Abstract
Background
Attention should be paid to endoscopy-related complications and safety-related accidents that may occur in the endoscopy unit. This study investigated the current status of complications associated with diagnostic and therapeutic endoscopy in Korea.
Methods
A questionnaire survey on endoscopy-related complications was conducted in a total of 50 tertiary or general hospitals in Korea. The results were compared to the population-level claims data from the Health Insurance Review & Assessment Service (HIRA), which analyzed endoscopy procedures conducted in 2017 in Korea.
Results
The incidences of bleeding associated with diagnostic and therapeutic esophagogastroduodenoscopy (EGD) and with diagnostic and therapeutic colonoscopy were 0.224% and 3.155% and 0.198% and 0.356%, respectively, in the 2017 HIRA claims data, compared to 0.012% and 1.857%, and 0.024% and 0.717%, in the 50 hospitals surveyed. The incidences of perforation associated with diagnostic and therapeutic EGD and with diagnostic and therapeutic colonoscopy were 0.023% and 0.613%, and 0.007% and 0.013%, respectively, in the 2017 HIRA claims data compared to 0.001% and 0.325%, and 0.017% and 0.206%, in the 50 hospitals surveyed. In the HIRA claims data, the incidence of bleeding/perforation after diagnostic colonoscopy in clinics, community hospitals, general hospitals, and tertiary hospitals was 0.129%/0.000%, 0.088%/0.004%, 0.262%/0.009%, and 0.479%/0.030% respectively, and the corresponding incidence of bleeding/perforation after therapeutic colonoscopy was 0.258%/0.004%, 0.401%/0.007%, 0.408%/0.024%, and 0.731%/0.055%.
Conclusion
The incidences of complications associated with diagnostic and therapeutic EGD or colonoscopy tended to increase with the hospital volume in Korea.
Trial Registration
Clinical Research Information Service Identifier: KCT0001728
Keywords: Endoscopy, Colonoscopy, Bleeding, Perforation
Graphical Abstract
INTRODUCTION
Esophagogastroduodenoscopy (EGD) and colonoscopy are relatively safe procedures, but can sometimes lead to serious, life-threatening complications. As the indications for therapeutic endoscopic procedures continue to expand, the risk for complications is expected to increase. Based on the Korean National Health Insurance Service database from 2002 to 2013, the overall colonoscopy volume increased eightfold over 12 years, and the colon polypectomy rate is also continuously increasing every year.1 Based on the claims data of endoscopic submucosal dissection (ESD) for early gastric cancer in Korea between November 2011 and December 2014, although the number of gastric ESD trials increased every year, most of them were carried out in tertiary care hospitals in Korea.2
As safety-related issues of endoscopy are closely related to the quality of endoscopists and endoscopy units,3 many countries have emphasized and enhanced endoscopy quality management and have made efforts to improve quality at the national level. In the USA, the American Society for Gastrointestinal Endoscopy (ASGE)/American College of Gastroenterology (ACG) Task Force has been working to improve endoscopic quality with the establishment of the first set of quality indicators for gastrointestinal (GI) tract endoscopic procedures in 2006.4,5,6 In Korea, the National Cancer Screening Program has included nationwide screening for gastric and colorectal cancer since 1999. The Korean Society of Gastrointestinal Endoscopy (KSGE) has established the National Endoscopy Quality Improvement Program to improve and manage the quality of endoscopic procedures. This program consists of qualification of endoscopists, quality improvement for instruments available at the endoscopy unit and endoscopic procedures, and measurement of outcomes of endoscopy screening.7,8,9 Furthermore, KSGE implemented the Accredited Endoscopy Unit Program in 2012 to certify and encourage high-quality endoscopy practices.10 Specifically, the Accredited Endoscopy Unit Program is obligated to document the incidence and types of complications, such as bleeding and perforation. Despite these efforts, quality control assessment programs still assess the documentation of endoscopic complications, but do not assess the actual incidence and management of complications.
Recently, ASGE/ACG has established a performance target associated with colonoscopy related to post-process quality indicators, which recommends that the perforation rate should be < 1/500 overall and < 1/1,000 in screening. It also recommends a bleeding rate < 1% after polypectomy.11 However, there have been few studies on complications related to diagnostic and therapeutic EGD and colonoscopy in Korea, with neither a uniform definition nor standardized reporting system, so there seems to be discrepancies between real clinical practice and research results. Nonetheless, the accredited Endoscopic Unit Program’s assessment of high-quality endoscopic practices has a mandatory requirement for documentation of complication rates, which is expected to better reflect data from real practices.
This study assessed the current status of complications associated with diagnostic and therapeutic endoscopy in Korea, to utilize this information to develop safety management indicators and improve quality of care in the endoscopy unit in Korea.
METHODS
Survey of the safety of endoscopy
A PubMed literature search between June 1 and July 15, 2018, was performed to identify the international standard guidelines and quality indicators for the safety of endoscopy. Based on the literature review, items were organized in accordance with the recommended guidelines, and a questionnaire survey produced by members of the Endoscopy Quality Assurance Committee under KSGE was designed to investigate the actual and current safety status of endoscopy units in Korea. In addition, a questionnaire survey was conducted in a total of 50 KSGE member tertiary or general hospitals using the Survey Monkey questionnaire survey site (https://ko.surveymonkey.com/). Participating institutions consisted of two community hospitals (4%), 17 general hospitals (34%), and 31 tertiary hospitals (62%), and no clinics. These hospitals have certified the Accredited Endoscopy Unit Program reviewed by KSGE for high-quality endoscopy practices that have passed the evaluation of strict standards for overall quality assessment items, including the qualification of endoscopists, the status of endoscopy procedures, and the records of the occurrence of complications.10,12,13 In addition, as these hospitals include most of the institutions that perform very high quality and advanced therapeutic endoscopy procedures in Korea, these data reflect the status of leading groups related to endoscopy in Korea.
The items included in the questionnaire survey were as follows (survey data): 1) Current status of working for medical personnel, 2) Number of diagnostic and therapeutic EGD and colonoscopy procedures performed between 2013 and 2017, and 3) Number and incidence of serious procedure-related complications, such as bleeding, perforation, and death, which occurred during the same period; sedation-related complications (respiratory depression, hypotension, anaphylaxis, shock, and so forth); periprocedural complications (falls, and so forth); and progress of each event (death, surgery, inpatient care, cardiopulmonary resuscitation, intubation, defibrillation).
To increase accuracy, complication data were collected by contacting the endoscopist in charge of the endoscopic unit or endoscopists participating in endoscopic quality management in each hospital. In addition, we asked them to investigate records of disputes related to complications in hospitals. During this collection process, the name of the institution was deleted because safety-related accident reports represent sensitive information for the institutions, and only the type of institution (general hospital, tertiary hospital, and so forth) was recorded. To prevent data leaks to outside parties, the researchers were trained, and written confidentiality agreements were obtained. Each file was assigned a password and handled securely. All files were destroyed upon completion of the study.
Population-based analyses of safety of endoscopy
Data sources and study population
Endoscopic procedures performed in Korea in 2017 were analyzed based on the claims data from the Health Insurance Review & Assessment Service (HIRA). The HIRA dataset contains demographic information on the beneficiaries, along with the adjusted medical and pharmacy claims data for almost 98% of the total Korean population14; it also contains extensive administrative data of all insurance claims, provider information, care setting, and diagnostic codes defined by the International Classification of Diseases 10th revision (ICD-10). Similar to other claims databases, no information is available about the indications for treatments or procedures received or the results of medical investigations. The study population included beneficiaries aged 20 years and older who underwent EGD or colonoscopy between January 1, 2017, and December 31, 2017. Endoscopy consisted of EGD and colonoscopy was classified as diagnostic or therapeutic endoscopy using procedure codes. Diagnostic endoscopy was defined as no additional procedures other than biopsy. Therapeutic endoscopy included polypectomy, endoscopic mucosal resection (EMR), and ESD in EGD, and polypectomy and EMR in colonoscopy. Colorectal ESD was excluded from the 2017 claims data because it was not covered by Korean National Health Insurance in 2017. Healthcare settings were categorized as primary clinics (< 30 beds), community hospitals (≥ 30 beds), general hospitals (≥ 100 beds), or tertiary hospitals (a general hospital designated by the Ministry of Health and Welfare specializing in treating severe and difficult diseases) according to the level of patient’s capacity in accordance with Korean medical law.
Ascertainment of adverse events from the HIRA dataset
We identified two major adverse events, i.e., perforation and bleeding, within 30 days after endoscopy using ICD-10 diagnosis codes and procedure or surgery claim codes. Patients with claim codes related to adverse events within 1 month prior to endoscopy were excluded. In EGD, claim codes related to each adverse event were defined as follows: perforation included “endoscopic treatment of upper GI perforation” (Q7660) and “simple closure of perforated stomach and duodenum” (Q2540), while bleeding included “surgical clipping” (Q2510), “endoscopic hemostasis of upper GI tract” (Q7620), and “embolization” (M6644). In colonoscopy, perforation included “segmental resection of colorectum” (Q2673), “colectomy” (Q2679), and “repair of bowel and/or mesenteric injury” (Q2771–2773), while bleeding included “sigmoidoscopic hemostasis” (Q7730), “colonoscopic hemostasis” (Q7680) and “embolization” (M6644). During the study period, endoscopic closure for colonic perforation was noted as covered by the HIRA. All emergency department visits within 30 days after EGD and colonoscopy were ascertained. To exclude cases who underwent therapeutic endoscopy due to bleeding rather than as an endoscopy-related complication, we excluded patients with claim codes related to GI bleeding within 1 month prior to endoscopy. In addition, we selected only patients who had bleeding after therapeutic endoscopy and both the procedure-related codes (polypectomy, EMR, or ESD) and the hemostasis-related codes.
Ethical problems and statistical analysis
Descriptive statistics were used to summarize the number of endoscopic procedures performed and the incidence of endoscopy-related complications. Categorical data are expressed as number (percentage), whereas continuous data are expressed as the mean ± SD. Statistical analyses were performed using R software version 3.5.1 (http://cran.r-project.org).
Ethics statement
This study was approved by the Institutional Ethics Committee and is registered at the Clinical Research Information Service (https://cris.nih.go.kr/cris/en/index.jsp) (KCT0001728). This study was approved by the Institutional Review Board of Kyung Hee University Hospital (KHUH 2019-01-015). Informed consent was waived by the board.
RESULTS
Incidence of endoscopy-related complications in surveyed hospitals in 2013–2017
The results were from analyses of approximately 3 million endoscopic procedures performed in 50 institutions in 2013–2017. The incidences of bleeding and perforations associated with diagnostic EGD were 0.012% and 0.001%, respectively. The incidences of bleeding and perforations associated with therapeutic EGD, which included polypectomy, EMR, and ESD, were 1.857% and 0.325%, respectively. The incidences of bleeding and perforations related to diagnostic colonoscopy were 0.024% and 0.017%, respectively. The incidences of bleeding and perforations related to therapeutic colonoscopy, which included polypectomy, EMR, and ESD, were 0.717% and 0.206%, respectively (Tables 1 and 2). Sedation-related complications, such as hypersensitivity, drug cross-reactions, respiratory depression, and hypotension, occurred 169 times annually on average. Fall accidents also occurred 18.8 times per year on average.
Table 1. Total number of endoscopic procedures performed in 50 hospitals during 2013–2017.
| Endoscopic procedures | Year | Total | |||||
|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | |||
| Diagnostic EGD | |||||||
| Sedation | 248,993 | 262,154 | 253,164 | 278,882 | 286,073 | 1,329,266 | |
| Non-sedation | 162,365 | 163,294 | 155,426 | 162,436 | 155,420 | 798,941 | |
| Diagnostic colonoscopy | |||||||
| Sedation | 115,341 | 116,994 | 117,012 | 124,741 | 124,457 | 598,545 | |
| Non-sedation | 38,492 | 37,845 | 39,156 | 39,442 | 41,324 | 196,259 | |
| Therapeutic EGD | |||||||
| ESD | 9,225 | 10,149 | 5,118 | 5,548 | 5,356 | 35,396 | |
| EMR | 4,964 | 5,268 | 1,318 | 1,155 | 1,078 | 13,783 | |
| Polypectomy | 1,240 | 1,286 | 24,283 | 22,410 | 22,433 | 71,652 | |
| Therapeutic colonoscopy | |||||||
| Polypectomy | 27,304 | 25,738 | 24,611 | 28,455 | 31,898 | 138,006 | |
| EMR | 21,251 | 21,893 | 6,229 | 7,320 | 7,367 | 64,060 | |
| ESD | 6,716 | 6,853 | 5,118 | 5,548 | 5,356 | 29,591 | |
EGD = esophagogastroduodenoscopy, ESD = endoscopic submucosal dissection, EMR = endoscopic mucosal resection.
Table 2. Numbers of endoscopy-related complications in surveyed institutions during 2013–2017 by year.
| Complications | Year | Total | Mean | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | 2017 | |||||
| Bleeding | |||||||||
| Stomach | |||||||||
| Diagnostic | 58 | 55 | 40 | 59 | 45 | 257 | 51.4 | ||
| Therapeutic | 438 | 436 | 431 | 449 | 490 | 2,244 | 448.8 | ||
| Colon | |||||||||
| Diagnostic | 43 | 42 | 35 | 34 | 33 | 187 | 37.4 | ||
| Therapeutic | 301 | 327 | 328 | 346 | 360 | 1,662 | 332.4 | ||
| Perforation | |||||||||
| Stomach | |||||||||
| Diagnostic | 8 | 7 | 8 | 2 | 5 | 30 | 6.0 | ||
| Therapeutic | 64 | 89 | 89 | 75 | 76 | 393 | 78.6 | ||
| Colon | |||||||||
| Diagnostic | 25 | 34 | 27 | 18 | 30 | 134 | 26.8 | ||
| Therapeutic | 106 | 107 | 85 | 83 | 97 | 478 | 95.6 | ||
| Sedation-related accidents (hypotension, respiratory depression, etc.) | 174 | 162 | 164 | 178 | 167 | 845 | 169 | ||
| Falls | 13 | 15 | 15 | 27 | 24 | 94 | 18.8 | ||
| Deaths | 3 | 3 | 4 | 2 | 4 | 16 | 3.2 | ||
| Other safety-related accidents | 3 | 8 | 3 | 6 | 6 | 26 | 5.2 | ||
| Total | 1,236 | 1,285 | 1,229 | 1,279 | 1,337 | 6,366 | 1,273.2 | ||
Performance status of endoscopic procedures based on 2017 HIRA claims data
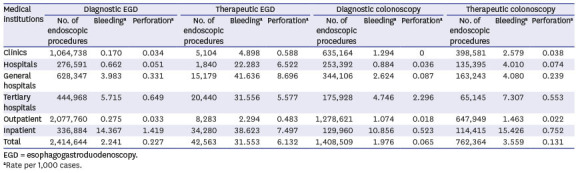
Excluding duplicate claims and cases of endoscopy for health screening, the numbers of EGD and colonoscopy procedures performed were 2,457,207 and 2,170,954, respectively. Diagnostic EGD was performed most often in clinics (44.1%), while therapeutic EGD (EMR or ESD) was performed most often in tertiary hospitals (48.0%). Diagnostic colonoscopy was also performed most often in clinics (45.1%), while therapeutic colonoscopy (polypectomy or EMR) was performed most often in clinics (52.3%), and only 8.5% of these procedures were performed in tertiary hospitals (Table 3).
Table 3. Rates of endoscopic procedures according to hospital classification based on 2017 claims data.
| Medical institutions | Diagnostic EGD | Therapeutic EGD | Diagnostic colonoscopy | Therapeutic colonoscopy | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of endoscopic procedures | Bleedinga | Perforationa | No. of endoscopic procedures | Bleedinga | Perforationa | No. of endoscopic procedures | Bleedinga | Perforationa | No. of endoscopic procedures | Bleedinga | Perforationa | |
| Clinics | 1,064,738 | 0.170 | 0.034 | 5,104 | 4.898 | 0.588 | 635,164 | 1.294 | 0 | 398,581 | 2.579 | 0.038 |
| Hospitals | 276,591 | 0.662 | 0.051 | 1,840 | 22.283 | 6.522 | 253,392 | 0.884 | 0.036 | 135,395 | 4.010 | 0.074 |
| General hospitals | 628,347 | 3.983 | 0.331 | 15,179 | 41.636 | 8.696 | 344,106 | 2.624 | 0.087 | 163,243 | 4.080 | 0.239 |
| Tertiary hospitals | 444,968 | 5.715 | 0.649 | 20,440 | 31.556 | 5.577 | 175,928 | 4.746 | 2.296 | 65,145 | 7.307 | 0.553 |
| Outpatient | 2,077,760 | 0.275 | 0.033 | 8,283 | 2.294 | 0.483 | 1,278,621 | 1.074 | 0.018 | 647,949 | 1.463 | 0.022 |
| Inpatient | 336,884 | 14.367 | 1.419 | 34,280 | 38.623 | 7.497 | 129,960 | 10.856 | 0.523 | 114,415 | 15.426 | 0.752 |
| Total | 2,414,644 | 2.241 | 0.227 | 42,563 | 31.553 | 6.132 | 1,408,509 | 1.976 | 0.065 | 762,364 | 3.559 | 0.131 |
EGD = esophagogastroduodenoscopy.
aRate per 1,000 cases.
When divided into age groups, diagnostic EGD was performed most often in patients aged 50–59 years, while therapeutic EGD was performed most often in patients aged 60–69 years. Both diagnostic and therapeutic colonoscopy procedures were performed most often in patients aged 50–59 years. Diagnostic EGD was performed mostly on an outpatient basis (86.0%), while therapeutic EGD was performed mostly on an inpatient basis upon diagnosis (80.5%). Both diagnostic and therapeutic colonoscopy procedures were performed primarily on an outpatient basis (90.8% and 85.0%, respectively) (Table 4).
Table 4. Number of endoscopic procedures according to age and type of care based on 2017 claims data.
| Age | EGD | Colonoscopy | ||
|---|---|---|---|---|
| Diagnostic | Therapeutic | Diagnostic | Therapeutic | |
| < 20 | 35,241 | 56 | 7,977 | 404 |
| 20–29 | 210,642 | 586 | 50,897 | 6,340 |
| 30–39 | 421,498 | 1,790 | 143,979 | 42,520 |
| 40–49 | 309,269 | 3,765 | 275,429 | 120,120 |
| 50–59 | 508,122 | 9,782 | 429,003 | 240,814 |
| 60–69 | 481,340 | 13,734 | 331,425 | 224,888 |
| 70–79 | 343,702 | 10,599 | 147,844 | 111,315 |
| > 80 | 104,830 | 2,251 | 22,036 | 15,963 |
| Outpatient | 2,077,760 | 8,283 | 1,278,621 | 647,949 |
| Inpatient | 336,884 | 34,280 | 129,969 | 114,415 |
| Total | 2,414,644 | 42,563 | 1,408,590 | 762,364 |
EGD = esophagogastroduodenoscopy.
Incidence of endoscopy-related complications based on 2017 HIRA claims data
The incidences of bleeding/perforation after therapeutic EGD occurring in clinics, community hospitals, general hospitals, and tertiary hospitals were 0.490%/0.059%, 2.228%/0.652%, 4.164%/0.870%, and 3.156%/0.558%. Both bleeding and perforation associated with therapeutic EGD showed the highest incidence rates in general hospitals. The incidences of bleeding/perforation after diagnostic colonoscopy occurring in clinics, community hospitals, general hospitals, and tertiary hospitals were 0.129%/0.000%, 0.088%/0.004%, 0.262%/0.009%, and 0.479%/0.030%. Both bleeding and perforation associated with diagnostic colonoscopy showed the highest incidence rates in tertiary hospitals. The incidences of bleeding/perforation after therapeutic colonoscopy occurring in clinics, community hospitals, general hospitals, and tertiary hospitals were 0.258%/0.004%, 0.401%/0.007%, 0.408%/0.024%, and 0.731%/0.055%. Unlike therapeutic EGD, the incidences of bleeding and perforation associated with therapeutic colonoscopy were highest in tertiary hospitals (Table 3).
DISCUSSION
Safety is one of the most important issues in quality management of endoscopy. However, the status of complications related to endoscopy is not well known. This is the first study in Korea to simultaneously analyze population-based data through insurance claims accounting for about 98% of the population and real-world data from 50 institutions certified by KSGE for high-quality endoscopic practices. The HIRA claims data were intended to be used to analyze the overall incidence of complications that occurred over a certain period for all volumes of hospitals in Korea and to analyze the incidence of complications according to the volume of the hospitals. The 50-hospital survey data were collected by tertiary or general hospitals that had performed certain procedures, such as gastric or colonic ESD, and had been certified by the Accredited Endoscopy Unit Program reviewed by KSGE for high-quality endoscopy practices.
Bleeding is a complication that occurs rarely in diagnostic EGD and is primarily associated with mechanical irritation generated by the tip of the endoscope during passage. The incidence of bleeding is approximately 0.15%.15 The risk for bleeding is higher in patients who have previously undergone gastrectomy and after multiple cold biopsies (8–15 biopsies) of the anastomotic site in Billroth I and Billroth II patients.16 A Mallory-Weiss tear may also occur due to excessive belching or retching during EGD.17 The incidences of bleeding associated with therapeutic EGD are 4% after EMR and 4.5% after ESD.18 In this study, the incidences of bleeding associated with diagnostic and therapeutic EGD were 0.224% and 3.155% in the 2017 HIRA claims data, and 0.012% and 1.857% in the 50 hospitals surveyed, respectively. Diagnostic and therapeutic EGD procedures were performed most frequently in clinics and tertiary hospitals, and the rates of bleeding associated with both procedures were relatively low compared to previous studies. The complications associated with EGD tended to increase as the hospital volume increased, probably due to the larger number of high-risk patients or higher rate of difficult procedures in general or tertiary hospitals.
Bleeding after polypectomy is one of the most common complications associated with colonoscopy. A recent meta-analysis showed that the incidence of bleeding in diagnostic colonoscopy without polypectomy was 0.06%, with rates of 0.98% after polypectomy,19 0.82% for immediate bleeding after colorectal ESD, and 1.7% for delayed bleeding.19 Another meta-analysis of the risk factors for bleeding associated with polypectomy showed that factors such as old age, high blood pressure, cardiovascular disease, right colon position, and polyp size > 1 cm were significantly associated with the occurrence of bleeding after polypectomy.20 In this study, the incidences of bleeding associated with diagnostic and therapeutic colonoscopy were 0.198% and 0.356% in the 2017 HIRA claims data, and 0.024% and 0.717% in the 50 hospitals surveyed, respectively. Both diagnostic and therapeutic colonoscopy procedures were most frequently performed in clinics. Similar to EGD-related bleeding, the diagnostic and therapeutic bleeding rates related to colonoscopy were relatively low compared to previous studies and tended to increase as the hospital volume increased, which was also probably due to the larger numbers of high-risk patients, such as those taking anticoagulant or antiplatelet drugs and with comorbidities, and the higher rate of difficult procedures, such as polypectomy for difficult location and large polyps, in general or tertiary hospitals.
Perforation during diagnostic EGD is extremely rare. A large prospective study reported that the incidence of perforation in diagnostic EGD was 0.05% and the associated mortality rate was 0.008%.21 The risk for perforation during diagnostic EGD was reported to be associated with Zenker’s diverticulum, esophageal stenosis, malignant tumors, duodenal diverticulitis, and the experience level of the endoscopist.21,22 Esophageal perforation can also occur during therapeutic procedures, such as balloon dilation with esophageal stenosis or achalasia and removal of sharp foreign bodies.22 In a meta-analysis, the incidences of esophageal perforation were 1.3% and 4.0% for EMR and ESD, respectively,23 and those for stomach perforation were 1.2% and 3.2%.23 In this study, the incidence rates of perforation associated with diagnostic and therapeutic EGD were 0.023% and 0.613% in the 2017 HIRA claims data, and 0.001% and 0.325% in the 50 hospitals surveyed. The incidences of diagnostic and therapeutic perforation associated with EGD were relatively low compared to previous studies, and the incidence of perforation in therapeutic EGD was lower in tertiary hospitals than in general hospitals.
The incidence of perforation associated with diagnostic colonoscopy was reported to be 0.05% with a mortality rate of 0.0029%, and that of perforation after colorectal polypectomy was 0.08% in a previous meta-analysis.19 The incidences of perforation related to colorectal ESD were reported to be 4.2% for immediate perforation and 0.22% for delayed perforation.24 During therapeutic colonoscopy, polyp location in the right colon or cecum, lateral spreading or nonpolypoid morphology, non-lifting polyp after submucosal injection due to submucosal fibrosis or deep layer involvement, polyps > 1 cm in size, and multiple polyps are risk factors for perforation.25,26,27,28 Diagnostic colonoscopy-associated perforations are relatively large and have a greater likelihood of requiring surgery than therapeutic colonoscopy-associated perforations.29 In this study, the incidences of perforation associated with diagnostic and therapeutic colonoscopy were 0.007% and 0.013% in the 2017 HIRA claims data, and 0.017% and 0.206% in the 50 hospitals surveyed, respectively. The incidences of diagnostic and therapeutic perforation associated with colonoscopy were also relatively low compared to previous studies and increased as the hospital volume increased, probably because most cases where perforation occurred in the clinic were transferred to tertiary hospitals for endoscopic management or surgery, and therefore the number of perforations in tertiary hospitals might be overestimated in analyses of HIRA data. The complication rates were higher in hospital survey data than HIRA claim data. This was because the hospital survey data were collected by general or tertiary hospitals that performed more in the way of high-level or high-risk procedures, hospital survey data included complications related to colorectal ESD, and a significant number of procedures might have been performed by GI fellows undergoing training. Also, because the occurrence of complications must be recorded to be certified by the Accredited Endoscopy Unit Program, it was likely that the hospital survey data reflected the occurrence of complications more accurately than the HIRA claim data.
This study had some limitations. We could not completely exclude cases who underwent therapeutic endoscopy due to bleeding rather than as an endoscopy-related complication due to limitations of use of claim data.
It might be impossible to define perforation accurately as a claim code because the clinical course of perforation differs among individuals, from conservative healing to endoscopic treatment to surgery, and coding for complications differs depending on the endoscopist or hospital. The amount of data was very large; therefore, we could not accurately evaluate the causal relationships, because we could not analyze the individual circumstances of each case. In the case of 2017 HIRA claims data, there were limitations with regard to the possible occurrence of complication code entry errors and unclaimed items after a complication had occurred. In the case of survey data, there were limitations with regard to the possible occurrence of missing records or varying definitions of a complication between institutions. Moreover, the investigation and recording of endoscopy-related complications may have been avoided in many cases because of the fear of legal issues arising with the reporting of complications. Thus, many cases of endoscopy-related complications may have been missing from the records.
Analyzing the results of this study, the largest numbers of diagnostic and therapeutic endoscopy procedures were performed in clinics, and the rate of complications was almost negligible. These results may be mistakenly taken to indicate the high degree of safety of endoscopy in clinics. The statistics in this study were not interpreted as absolute numbers because large numbers of complications in clinics were counted as occurring in general or tertiary hospitals because the patients were transferred to these hospitals for treatment and claims were made there. In addition, most procedures performed in clinics were simple, while tertiary hospitals had higher rates of more technically difficult procedures, which could lead to higher rates of complications. These factors may diminish the reliability of statistical analyses, and we cannot exclude the possible occurrence of large statistical errors in this study.
However, despite these limitations, the present study makes a significant contribution, as it is one of very few large-scale studies in Korea to investigate the incidence of endoscopy-related complications using data from HIRA claims and surveys over 5 years in 50 hospitals. Future research should consider various factors, such as diagnostic and therapeutic endoscopy indications, comorbidities, antithrombotic drug use, and experience of endoscopists related to complications according to the type of endoscopic procedure.
In conclusion, the incidences of diagnostic and therapeutic complications associated with EGD or colonoscopy tended to increase with the hospital volume in Korea. To obtain more reliable statistics, a system is needed to effectively report and manage complications at all types of hospital, from clinics to tertiary hospitals, in Korea.
Key message: 1) Diagnostic EGD was performed most often in clinics, while therapeutic EGD (EMR or ESD) was performed most often in tertiary hospitals in Korea. 2) Diagnostic colonoscopy and therapeutic colonoscopy (polypectomy, EMR, or ESD) were performed most often in clinics. 3) The incidences of complications associated with diagnostic and therapeutic EGD, or colonoscopy tended to increase with the hospital volume.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Jung Y, Kim JW, Im JP, Cho YK, Lee TH, Jang JY.
- Data curation: Jung Y, Kim JW, Im JP, Cho YK, Lee TH, Jang JY.
- Formal analysis: Jung Y, Kim JW, Im JP, Cho YK, Lee TH, Jang JY.
- Investigation: Jung Y, Jang JY.
- Methodology: Kim JW, Cho YK, Lee TH, Jang JY.
- Supervision: Jang JY.
- Visualization: Jung Y.
- Writing - original draft: Jung Y.
- Writing - review & editing: Kim JW, Jang JY.
References
- 1.Cha JM, Kwak MS, Kim HS, Kim SY, Park S, Park GU, et al. Real-world national colonoscopy volume in Korea: a nationwide population-based study over 12 years. Gut Liver. 2020;14(3):338–346. doi: 10.5009/gnl19108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kang HY, Kang HW, Kim SG, Kim JS, Park KJ, Jung HC, et al. Incidence and management of colonoscopic perforations in Korea. Digestion. 2008;78(4):218–223. doi: 10.1159/000190811. [DOI] [PubMed] [Google Scholar]
- 3.Cotton PB. Quality endoscopists and quality endoscopy units. J Interv Gastroenterol. 2011;1(2):83–87. doi: 10.4161/jig.1.2.15048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faigel DO, Pike IM, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for gastrointestinal endoscopic procedures: an introduction. Am J Gastroenterol. 2006;101(4):866–872. doi: 10.1111/j.1572-0241.2006.00677.x. [DOI] [PubMed] [Google Scholar]
- 5.Cohen J, Safdi MA, Deal SE, Baron TH, Chak A, Hoffman B, et al. Quality indicators for esophagogastroduodenoscopy. Am J Gastroenterol. 2006;101(4):886–891. doi: 10.1111/j.1572-0241.2006.00676.x. [DOI] [PubMed] [Google Scholar]
- 6.Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2006;101(4):873–885. doi: 10.1111/j.1572-0241.2006.00673.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee S, Jun JK, Suh M, Park B, Noh DK, Jung KW, et al. Gastric cancer screening uptake trends in Korea: results for the National Cancer Screening Program from 2002 to 2011: a prospective cross-sectional study. Medicine (Baltimore) 2015;94(8):e533. doi: 10.1097/MD.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cha JM. Quality improvement of gastrointestinal endoscopy in Korea: past, present, and future. Korean J Gastroenterol. 2014;64(6):320–332. doi: 10.4166/kjg.2014.64.6.320. [DOI] [PubMed] [Google Scholar]
- 9.Cha JM, Moon JS, Chung IK, Kim JO, Im JP, Cho YK, et al. National endoscopy quality improvement program remains suboptimal in Korea. Gut Liver. 2016;10(5):699–705. doi: 10.5009/gnl15623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim JW, Cho YK, Kim JO, Jang JY. Accredited endoscopy unit program of Korea: overview and qualification. Clin Endosc. 2019;52(5):426–430. doi: 10.5946/ce.2019.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rex DK, Schoenfeld PS, Cohen J, Pike IM, Adler DG, Fennerty MB, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81(1):31–53. doi: 10.1016/j.gie.2014.07.058. [DOI] [PubMed] [Google Scholar]
- 12.Lee TH, Yoon JY, Paik CN, Choi HS, Jang JY. Updates on the facilities, procedures, and performance of the accredited endoscopy unit. Clin Endosc. 2019;52(5):431–442. doi: 10.5946/ce.2019.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shin JE, Jung Y, Lee JH, Son BK, Jang JY, Kim HK, et al. Updates on the disinfection and infection control process of the accredited endoscopy unit. Clin Endosc. 2019;52(5):443–450. doi: 10.5946/ce.2019.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017;32(5):718–728. doi: 10.3346/jkms.2017.32.5.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Guideline on the management of anticoagulation and antiplatelet therapy for endoscopic procedures. Gastrointest Endosc. 2002;55(7):775–779. doi: 10.1016/s0016-5107(02)70402-1. [DOI] [PubMed] [Google Scholar]
- 16.Domellöf L, Enander LK, Nilsson F. Bleeding as a complication to endoscopic biopsies from the gastric remnant after ulcer surgery. Scand J Gastroenterol. 1983;18(7):951–954. doi: 10.3109/00365528309182121. [DOI] [PubMed] [Google Scholar]
- 17.Penston JG, Boyd EJ, Wormsley KG. Mallory-Weiss tears occurring during endoscopy: a report of seven cases. Endoscopy. 1992;24(4):262–265. doi: 10.1055/s-2007-1009122. [DOI] [PubMed] [Google Scholar]
- 18.Park YM, Cho E, Kang HY, Kim JM. The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and metaanalysis. Surg Endosc. 2011;25(8):2666–2677. doi: 10.1007/s00464-011-1627-z. [DOI] [PubMed] [Google Scholar]
- 19.Reumkens A, Rondagh EJ, Bakker CM, Winkens B, Masclee AA, Sanduleanu S. Post-colonoscopy complications: a systematic review, time trends, and meta-analysis of population-based studies. Am J Gastroenterol. 2016;111(8):1092–1101. doi: 10.1038/ajg.2016.234. [DOI] [PubMed] [Google Scholar]
- 20.Jaruvongvanich V, Prasitlumkum N, Assavapongpaiboon B, Suchartlikitwong S, Sanguankeo A, Upala S. Risk factors for delayed colonic post-polypectomy bleeding: a systematic review and meta-analysis. Int J Colorectal Dis. 2017;32(10):1399–1406. doi: 10.1007/s00384-017-2870-0. [DOI] [PubMed] [Google Scholar]
- 21.Quine MA, Bell GD, McCloy RF, Charlton JE, Devlin HB, Hopkins A. Prospective audit of upper gastrointestinal endoscopy in two regions of England: safety, staffing, and sedation methods. Gut. 1995;36(3):462–467. doi: 10.1136/gut.36.3.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ben-Menachem T, Decker GA, Early DS, Evans J, Fanelli RD, Fisher DA, et al. Adverse events of upper GI endoscopy. Gastrointest Endosc. 2012;76(4):707–718. doi: 10.1016/j.gie.2012.03.252. [DOI] [PubMed] [Google Scholar]
- 23.Guo HM, Zhang XQ, Chen M, Huang SL, Zou XP. Endoscopic submucosal dissection vs endoscopic mucosal resection for superficial esophageal cancer. World J Gastroenterol. 2014;20(18):5540–5547. doi: 10.3748/wjg.v20.i18.5540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akintoye E, Kumar N, Aihara H, Nas H, Thompson CC. Colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Endosc Int Open. 2016;4(10):E1030–E1044. doi: 10.1055/s-0042-114774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Panteris V, Haringsma J, Kuipers EJ. Colonoscopy perforation rate, mechanisms and outcome: from diagnostic to therapeutic colonoscopy. Endoscopy. 2009;41(11):941–951. doi: 10.1055/s-0029-1215179. [DOI] [PubMed] [Google Scholar]
- 26.Wada Y, Kudo SE, Tanaka S, Saito Y, Iishii H, Ikematsu H, et al. Predictive factors for complications in endoscopic resection of large colorectal lesions: a multicenter prospective study. Surg Endosc. 2015;29(5):1216–1222. doi: 10.1007/s00464-014-3799-9. [DOI] [PubMed] [Google Scholar]
- 27.Lee EJ, Lee JB, Choi YS, Lee SH, Lee DH, Kim DS, et al. Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg Endosc. 2012;26(6):1587–1594. doi: 10.1007/s00464-011-2075-5. [DOI] [PubMed] [Google Scholar]
- 28.Thirumurthi S, Raju GS. Management of polypectomy complications. Gastrointest Endosc Clin N Am. 2015;25(2):335–357. doi: 10.1016/j.giec.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Jung Y. Endoscopic management of iatrogenic colon perforation. Clin Endosc. 2020;53(1):29–36. doi: 10.5946/ce.2019.061. [DOI] [PMC free article] [PubMed] [Google Scholar]


