Abstract
Question
Mental disorders typically start in childhood and persist, causing high individual and collective burdens. To inform policymaking to address children’s mental health in high-income countries we aimed to identify updated data on disorder prevalence.
Methods
We identified epidemiological studies reporting mental disorder prevalence in representative samples of children aged 18 years or younger—including a range of disorders and ages and assessing impairment (searching January 1990 through February 2021). We extracted associated service-use data where studies assessed this. We conducted meta-analyses using a random effects logistic model (using R metafor package).
Findings
Fourteen studies in 11 countries met inclusion criteria, published from 2003 to 2020 with a pooled sample of 61 545 children aged 4–18 years, including eight reporting service use. (All data were collected pre-COVID-19.) Overall prevalence of any childhood mental disorder was 12.7% (95% CI 10.1% to 15.9%; I2=99.1%). Significant heterogeneity pertained to diagnostic measurement and study location. Anxiety (5.2%), attention-deficit/hyperactivity (3.7%), oppositional defiant (3.3%), substance use (2.3%), conduct (1.3%) and depressive (1.3%) disorders were the most common. Among children with mental disorders, only 44.2% (95% CI 37.6% to 50.9%) received any services for these conditions.
Conclusions
An estimated one in eight children have mental disorders at any given time, causing symptoms and impairment, therefore requiring treatment. Yet even in high-income countries, most children with mental disorders are not receiving services for these conditions. We discuss the implications, particularly the need to substantially increase public investments in effective interventions. We also discuss the policy urgency, given the emerging increases in childhood mental health problems since the onset of the COVID-19 pandemic (PROSPERO CRD42020157262).
Keywords: child & adolescent psychiatry
Background
Mental disorders typically start in childhood and adolescence (hereafter childhood) and significantly interfere with well-being and development.1 2 Now the leading cause of childhood disability globally,3 these disorders often persist into adulthood, adding greatly to the burden for individuals.4 5 The collective social and economic burdens are also high due to associated healthcare, education, child protection and justice system costs—and to the cost of lost human potential.6–9 Service shortfalls have compounded the burdens, even in high-income countries such as the UK, USA and Canada.10 This is despite growing health expenditures in these countries over the years.11–13 These shortfalls also persist despite longstanding recognition that all children have the right to adequate health, social and educational services—including mental health services14—and despite considerable research evidence describing effective interventions for preventing and treating childhood mental disorders.15–17
To address children’s mental health needs, policymakers require pooled prevalence data from multiple high-quality epidemiological studies using current or recent diagnostic standards.18 19 Studies using rigorous diagnostic measures in large representative/probabilistic samples and examining a range of mental disorders across multiple age groups provide accurate and comprehensive population estimates—and therefore the most accurate estimates of community burden. At the same time, data on associated patterns of mental health service use can also assist policymakers in identifying and remediating gaps.
Systematic review and meta-analysis methods are an optimal way of synthesising large bodies of research evidence to inform policymaking.20 21 However, recent reviews on the prevalence of childhood mental disorders have had policy-relevant limitations including: accepting less rigorous studies22–24; reporting on a relatively limited number of disorders25; and/or omitting service use data.22–26 As well, to our knowledge no reviews have included studies applying the latest diagnostic standards from the American Psychiatric Association’s (APA’s) Diagnostic and Statistical Manual of Mental Disorders (DSM) or the World Health Organization’s (WHO’s) International Classification of Diseases (ICD).27 28
Objective
To inform policymaking intended to address children’s mental health in high-income countries, we therefore conducted a systematic review and meta-analysis to identify comprehensive and updated data on the prevalence of childhood mental disorders and, where possible, associated service use. To ensure robust data, we aimed to identify recent high-quality epidemiological studies. We focused on high-income countries because most low- and middle-income countries have yet to mobilise children’s mental health services on a large scale—due to insufficient financial and human resources.29 30
Methods
Search strategy
We followed the Meta-analysis of Observational Studies in Epidemiology (MOOSE)31 and Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA)32 guidelines for this systematic review and meta-analysis. (Online supplemental appendix A provides MOOSE and PRISMA checklists.) We registered this review with PROSPERO (number CRD42020157262; see www.crd.york.ac.uk/PROSPERO/; no amendments added).
ebmental-2021-300277supp001.pdf (876.7KB, pdf)
To identify relevant studies, we searched EMBASE, MEDLINE and PsycINFO databases using the following terms: mental disorders; child; adolescent; epidemiology; prevalence; incidence; health survey; survey; population; community; representative; stratified; probability. (We did not conduct separate searches for service use because we aimed to extract these data from the prevalence studies that met our eligibility criteria.) Search dates were January 1990 through February 2021. The year 1990 was chosen to capture the WHO’s ICD 10th and later editions (1990–2020)28 and the APA’s DSM fourth and later editions (1994–2013).33 We limited our searches to prevalence studies conducted with children aged 18 years or younger and published in peer reviewed journals. We did not include language limiters and used Google Translate to assess studies published in languages other than English. We also hand-searched relevant systematic reviews retrieved through our database searches to identify additional publications (eg, Erskine et al 23 and Polancyzk et al 25). For applicability to policymaking in high-income countries, we excluded studies conducted in low- and middle-income countries (according to World Bank classifications).34 (Online supplemental appendix B gives search strategy details.)
Study selection
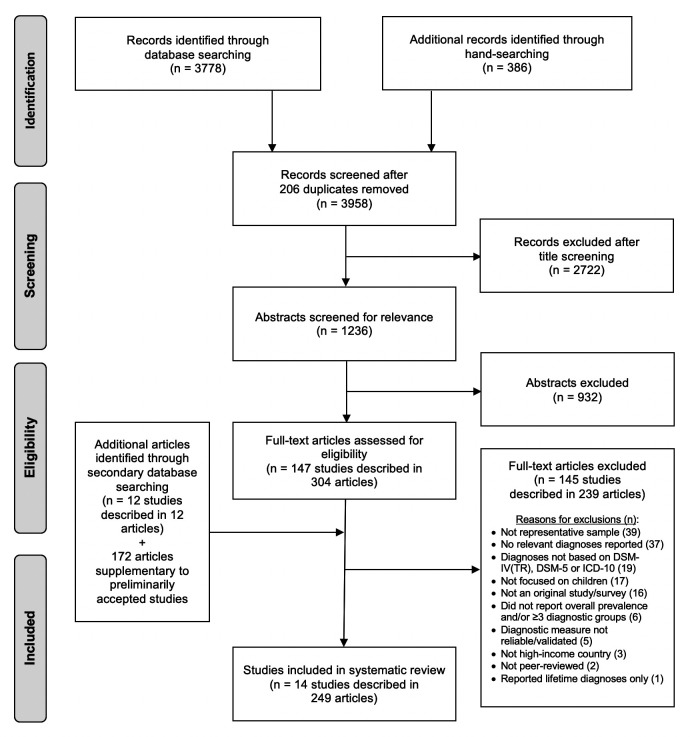
After title screening, two authors independently assessed all abstracts. Relevant studies were retrieved and independently assessed, again by two authors, identifying those that met all inclusion criteria, which were established a priori. To ensure inclusion of rigorous studies, we applied quality indicators requiring representative/probabilistic sampling and reliable and valid child diagnostic measures, including assessment of impairment; we excluded studies that used only clinical records for diagnoses. We required studies to provide overall prevalence for any disorder since this figure is particularly relevant for policymakers. For comprehensiveness, we also required studies to report on three or more individual disorders or disorder groups. We excluded studies that only reported lifetime prevalence because of potential recall bias and because such data provide less accurate estimates of current service needs.35 Next, we identified all supplemental publications making use of data from the accepted original studies, searching Web of Science by study names and/or titles and/or authors. Throughout the process, any disagreements were resolved by consensus involving two or more authors. (Online supplemental appendix C provides study inclusion criteria; figure 1 shows the search process; Online supplemental appendix D provides included studies.)
Figure 1.
Search process. DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Classification of Diseases.
Data extraction and quality assessment
We extracted data on the prevalence of any mental disorder and on the prevalence of individual disorders or disorder groups where possible. We also extracted data on potential moderators of prevalence including: overall study design; study location (continent); sampling area (national vs regional); data collection years; sampling frame; child age and sex; diagnostic standard; diagnostic measure; informants; diagnostic algorithm for reporting/combining data from different informants; and timeframes for assessing symptoms and impairment.25
To determine the prevalence of mental health-related service use, we extracted data from all accepted studies that assessed this variable among children who had mental disorders—including any service contacts for mental health needs regardless of type, setting or provider. One author extracted all salient data; a second author then independently verified this work, with input from other authors as needed. We also contacted study authors when we required additional information.
Beyond applying our inclusion criteria, we also assessed study quality using an adapted risk-of-bias tool developed by Hoy et al for prevalence studies.36 This tool assessed selection, non-response and measurement biases, as well as biases related to analysis. Scores of 0–3 were deemed low risk of bias, 4–6 moderate, and 7–10 high. (Online supplemental appendix E gives the quality assessment tool and results.)
Data synthesis
We conducted a meta-analysis using a random effects logistic model to calculate the pooled overall prevalence estimate for any mental disorder and its 95% confidence interval (95% CI). We performed the same analysis to calculate pooled prevalence estimates for individual disorders and service use among children with mental disorders when relevant data were available from at least two studies. For our meta-analyses, where possible we used prevalence data that study authors reported regardless of diagnostic algorithms used. These algorithms included: using clinical judgement; applying an ‘OR’ rule whereby disorders were counted if diagnostic thresholds were met by any informant (child OR parent); or relying on a single informant. Thirteen studies provided overall estimates for the whole sample, or a weighted average, that we used in our analyses. For one study that reported separate prevalence estimates by informant, with no weighted average for the whole sample, we selected estimates based on the most appropriate informant (for example, parent report for conduct disorder, child report for anxiety), then calculated a weighted average.37 s8
Regarding impairment, while precise definitions were not provided for all accepted studies, most reported definitions aligned with moderate-to-severe levels. Therefore, for the one study that reported separate estimates for mild, moderate and severe/‘serious’ impairment, we reported data that aligned with the other studies—in this case, ‘serious’ impairment which was defined as moderate impairment in most areas or severe impairment in at least one area.s1 Heterogeneity was assessed using I2. We conducted univariate meta-regression analyses to identify potential sources of heterogeneity for the pooled prevalence estimates for any mental disorder. We also performed a random effects meta-analysis to calculate pooled prevalence of mental health-related service use among children with mental disorders across studies. All statistical analyses were conducted using the metafor package for R.38
Findings
Study characteristics
We identified 159 studies for full-text assessment. Fourteen studies, described in 249 articles, met all inclusion criteria. Published between 2003 and 2020, these studies were conducted in 11 countries: the USA (four studies) and Australia, Canada, Chile, Denmark, Great Britain, Israel, Lithuania, Norway, South Korea and Taiwan (one study each). Sample sizes ranged from 957 to 10 438; child ages ranged from 4 to 18 years; 51.2% of participants were girls. Eleven of 14 studies used DSM-IV or DSM-IV-TR diagnostic standards, while two used ICD-10 and one used DSM-5. Most studies reported diagnoses using assessments of symptoms and impairment over one-year periods. (Table 1 describes the characteristics of the 14 included studies; online supplemental appendix F lists excluded studies.)
Table 1.
Childhood mental disorder prevalence study characteristics
| Study | Study location | Data collection year(s) | Sampling frame | Sample size* | Ages (years) | Diagnostic standard | Diagnostic measure† | Informant(s) | Timeframe‡ (months) |
| Canino 2004s2 | Puerto Rico (USA) | 1999–2000 | Households | 1897 | 4–17 | DSM-IV | DISC-IV | Child or parent | 12 |
| Chen 2020s3 | Taiwan | 2015–2017 | Schools | 4816 | 7–14 | DSM-5 | K-SADS-E | Child | 6 |
| Costello 2003s4 | North Carolina (USA) | 1993–2000 | Schools | 1420 | 9–16 | DSM-IV | CAPA | Child or parent | 3 |
| Elberling 2015s5 | Copenhagen (Denmark) | 2000 | Population registry | 1585 | 5–7 | ICD-10 | DAWBA | Parent + teacher | 1–12 |
| Farbstein 2010s6 | Israel | 2004–2005 | Population registry | 957 | 14–17 | DSM-IV | DAWBA | Child + parent | 1–12 |
| Ford 2003s7 | England, Scotland, Wales (Great Britain) | 1999 | Households | 10 438 | 5–15 | DSM-IV | DAWBA | Child + parent + teacher | 1–12 |
| Georgiades 2019s8 | Ontario (Canada) | 2014–2015 | Households | 6537 | 4–17 | DSM-IV-TR | MINI-KID | Child/parent | 6 |
| Heiervang 2007s9 | Bergen (Norway) | 2002–2003 | Schools | 6297 | 8–10 | DSM-IV | DAWBA | Parent + teacher | 1–12 |
| Kessler 2012s1, s10 | USA | 2001–2004 | Households + schools | 6483 | 13–17 | DSM-IV | CIDI | Child or parent | 12 |
| Lawrence 2016s11 | Australia | 2013–2014 | Households | 6310 | 4–17 | DSM-IV | DISC-IV | Parent§ | 12 |
| Lesinkiene 2018s12 | Lithuania | 2004–2007 | Schools | 3309 | 7–16 | ICD-10 | DAWBA | Parent + child + teacher | 1–12 |
| Merikangas 2010s13 | USA | 2001–2004 | Population registry | 3042 | 8–15 | DSM-IV | DISC-IV | Child or parent | 12 |
| Park 2015s14 | Seoul (South Korea) | 2005–2006 | Schools | 1645 | 6–12 | DSM-IV | DISC-IV | Parent | 12 |
| Vicente 2012s15 | Cautin, Conception, Iquique, Santiago (Chile) | 2007–2009 | Households | 1558 | 4–18 | DSM-IV | DISC-IV | Child/parent | 12 |
+ Diagnoses determined using clinical judgement combining information from multiple informants. / Diagnoses determined relying on a single informant based either on disorders and/or age ranges; figure 2 gives details on data used in meta-analysis. (Online supplemental appendix D lists references s1 to s15). 'or' Diagnoses determined applying ‘OR’ rule whereby disorders were counted if diagnostic thresholds met by any informant (either child or parent).
*51.2% of participants were girls.
†Fully structured measures included CAPA, CIDI, DISC-IV and MINI-KID; semi-structured measures included DAWBA and K-SADS-E.
‡Duration over which symptoms/impairment were assessed; when a range of timeframes were provided, 12 month prevalence was chosen.
§While 11- to 17-year-olds were informants for one disorder, only parent reported estimates were used in meta-analyses due to insufficient data for calculating overall rate for 11- to 17-year-olds.
CAPA, Child and Adolescent Psychiatric Assessment; CIDI, Composite International Diagnostic Interview; DAWBA, Development and Well-Being Assessment; DISC-IV, Diagnostic Interview Schedule for Children; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Statistical Classification of Diseases and Related Health Problems; K-SADS-E, Kiddie Schedule for Affective Disorders and Schizophrenia-Epidemiological; MINI-KID, Mini-International Neuropsychiatric Interview for Children and Adolescents.
Included studies determined diagnoses by interviewing children, parents and/or teachers using measures that included: Child and Adolescent Psychiatric Assessment; Composite International Diagnostic Interview; Development and Well-Being Assessment (DAWBA); Diagnostic Interview Schedule for Children-IV; Kiddie Schedule for Affective Disorders and Schizophrenia-Epidemiological; and Mini-International Neuropsychiatric Interview for Children and Adolescents. Among the seven studies that reported their specific criteria for assessing impairment, five required at least one severe or at least two moderate ratings of impairment in school achievement and/or relationships with family, friends or teachers,s1, s11, s13–s15 while two studies required moderate impairment in one of these domains.s2, s7
Studies also varied in their use of informants for determining diagnoses. For four studies, diagnoses were established using computer algorithms based on symptoms reported by either parents or children.s2, s4, s10, s13 For the five studies using DAWBA, symptom responses from all informants were considered, then diagnoses were made using clinical judgement.s5–s7, s9, s12 For the remaining studies, prevalence estimates were informed by a single source: one using child report onlys3; two using parent report onlys11, s14; and two using child and parent reports with estimates provided separately based on informant.s8, s15 All studies were deemed low risk regarding selection, non-response, measurement and analysis biases. (See online supplemental appendix E)
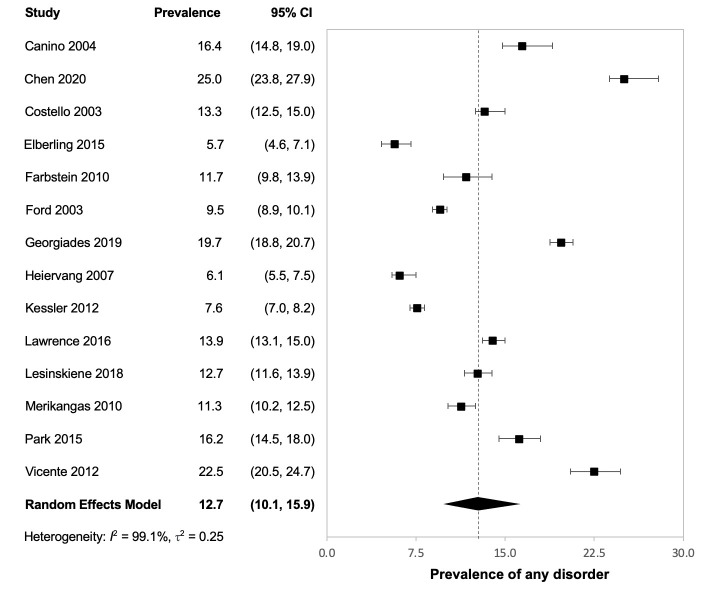
Pooled prevalence of any mental disorder
The pooled overall prevalence of any mental disorder was 12.7% (95% CI 10.1% to 15.9%; I2=99.1%), based on 14 studies with a pooled sample size of 61 545 children. The following covariates were identified as potential sources of heterogeneity: study location (continent); overall study design; diagnostic standard; diagnostic measure; informants; diagnostic algorithm for reporting/combining data from different informants; and timeframes for assessing symptoms and impairment. Covariates with no moderating effects on prevalence included: sampling area (national vs regional); sampling frame; data collection years; and child age and sex. (Figure 2 provides the forest plot for any disorder; online supplemental appendix G provides details on our meta-regression findings.)
Figure 2.
Forest plot for overall prevalence of any childhood mental disorder. Georgiades 2019s8 reported 18.2% of 4- to 11-year-olds (parent report) and 21.8% of 12- to 17-year-olds (child report) with any mental disorders. Vicente 2012s15 reported 27.8% of 4- to 11-year-olds (parent report) and 16.5% of 12- to 18-year-olds (child report) with any mental disorders. We report the weighted averages for these two studies in our meta-analysis.
Pooled prevalence of individual disorders and disorder groups
Pooled prevalence was calculated for individual disorders and/or disorder groups when such data were reported in two or more studies. The most common conditions were: any anxiety disorder, pooled prevalence 5.2% (95% CI 3.2% to 8.2%); attention-deficit/hyperactivity disorder (ADHD) 3.7% (95% CI 2.3% to 5.7%); oppositional defiant disorder 3.3% (95% CI 2.4% to 4.6%); any substance use disorder 2.3% (95% CI 2.1% to 2.6%); conduct disorder 1.3% (95% CI 0.8% to 2.3%); major depressive disorder 1.3% (95% CI 0.6% to 2.9%); and alcohol use disorder 1.2% (95% CI 1.0% to 1.4%). Prevalence rates for other conditions were: cannabis use disorder 0.6% (95% CI 0.4% to 1.0%); autism spectrum disorder 0.4% (95% CI 0.2% to 0.8%); obsessive-compulsive disorder 0.3% (95% CI 0.1% to 0.6%); bipolar disorder 0.3% (95% CI 0.1% to 1.1%); eating disorders 0.2% (95% CI 0.1% to 0.5%); post-traumatic stress disorder 0.1% (95% CI 0.02% to 0.5%); and schizophrenia 0.1% (95% CI 0.1% to 0.3%). Ten of 14 studies reported on concurrent disorders. Among children with mental disorders, 26.5% (weighted average; range 14.0–37.0%) had two or more disorders. (Table 2 presents pooled prevalence estimates for these disorders and/or disorder groups, including number of studies and pooled sample sizes; online supplemental appendix H presents forest plots for individual disorders and disorder groups.)
Table 2.
Pooled prevalence of childhood mental disorders
| Disorder | Age* (years) | Number of studies | Sample size | Prevalence (%) (95% CI) |
| Any anxiety disorder† | 4–18 | 12 | 53 663 | 5.2 (3.2 to 8.2) |
| Specific phobia | 4–18 | 7 | 37 170 | 3.4 (1.9 to 5.9) |
| Separation anxiety disorder | 4–18 | 10 | 46 935 | 1.6 (1.0 to 2.6) |
| Social anxiety disorder | 4–18 | 10 | 46 935 | 1.2 (0.6 to 2.3) |
| Generalised anxiety disorder | 4–18 | 11 | 49 977 | 0.9 (0.4 to 1.7) |
| Panic disorder | 4–18 | 9 | 38 881 | 0.1 (0.1 to 0.3) |
| Agoraphobia | 4–18 | 5 | 26 691 | 0.1 (0.04 to 0.4) |
| Attention-deficit/hyperactivity disorder | 4–18 | 14 | 61 545 | 3.7 (2.3 to 5.7) |
| Oppositional defiant disorder | 4–18 | 10 | 47 299 | 3.3 (2.4 to 4.6) |
| Any substance use disorder‡ | 12–18 | 4 | 15 788 | 2.3 (2.1 to 2.6) |
| Alcohol use disorder | 12–18 | 3 | 9114 | 1.2 (1.0 to 1.4) |
| Cannabis use disorder | 12–18 | 2 | 2631 | 0.6 (0.4 to 1.0) |
| Any depressive disorder§ | 4–18 | 7 | 31 737 | 1.8 (0.8 to 3.8) |
| Major depressive disorder | 4–18 | 11 | 45 696 | 1.3 (0.6 to 2.9) |
| Dysthymia | 4–18 | 4 | 8142 | 0.2 (0.1 to 0.7) |
| Conduct disorder | 4–18 | 13 | 59 960 | 1.3 (0.8 to 2.3) |
| Autism spectrum disorder | 4–18 | 4 | 21 629 | 0.4 (0.2 to 0.8) |
| Obsessive-compulsive disorder | 4–18 | 7 | 33 769 | 0.3 (0.1 to 0.6) |
| Bipolar disorder | 12–18 | 2 | 8128 | 0.3 (0.1 to 1.1) |
| Eating disorders | 12–18 | 5 | 21 194 | 0.2 (0.1 to 0.5) |
| Post-traumatic stress disorder | 4–18 | 8 | 35 839 | 0.1 (0.04 to 0.4) |
| Schizophrenia | 12–18 | 2 | 5500 | 0.1 (0.1 to 0.3) |
| Any disorder¶ | 4–18 | 14 | 61 545 | 12.7 (10.1 to 15.9) |
*Earliest age in the ranges provided reflects when disorders typically emerge.2
†For any anxiety disorder, 6 studies included post-traumatic stress and/or obsessive-compulsive disorders.
‡For any substance use disorder, 2 studies included alcohol, cannabis, nicotine and other substances; 1 included alcohol and drugs; and one did not specify.
§For any depressive disorder, 4 studies included major depressive disorder (MDD) and dysthymia; 1 included MDD and depression not specifie; 1 included MDD, dysthymia and bipolar; and 1 did not specify.
¶Overall estimate for children with any disorder is less than the sum of estimates for the specific disorders because 26.5% of children had two or more disorders concurrently.
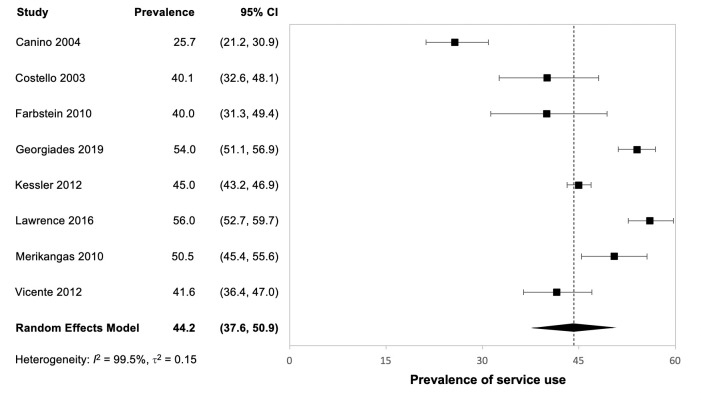
Pooled prevalence for service use
For children with mental disorders, we extracted data on any services accessed for mental health concerns, provided in eight studies.39–42 s2, s8, s13, s15 These studies varied considerably regarding measurement of services. Some included only mental healthcare, such as counselling provided by psychologists or psychiatric medications prescribed by physicians,42 s2, s13 while others included a much wider range, such as complementary medicine and youth justice services.39–41 s8, s15 Studies also varied regarding assessment of timeframes for service use. While most measured past-year use,40–42 s2, s13, s15 three-month39 and six-month uses8 were each assessed in a single study. Across these studies children were also defined as being recipients of services regardless of the intensity or duration of care provided. Informants also differed across the studies—involving childrens14, s15 or parents40 42 or both.39 41 s2, s8
Our meta-analysis found that only 44.2% children with mental disorders received any services for their mental health concerns (95% CI 37.6% to 50.9%; I2=95.5%).39–42 s2, s8, s13, s15 The one study that assessed service use by disorder severity found a gradient—with greater use for children with severe impairment relative to moderate impairment.42 (Figure 3 gives the forest plot for service use findings.)
Figure 3.
Forest plot for prevalence of service use. Service use data for Costello 2003,s4 Farbstein 2010,s6 Kessler 2012s10 and Lawrence 2016s11 were obtained from the separate articles by Burns 1995, Mansbach-Kleinfeld 2010, Costello 2014 and Johnson 2016,39–42 respectively. Costello 2003s4 and Merikangas et al 2010s13 reported that 40.3% and 50.6%, respectively, of children with mental disorders received any services for their mental health problems; we report slight variations in our meta-analysis due to rounding. Georgiades 2019s8 reported that 61.5% of 4- to 11-year-olds (parent report) and 43.7% of 12- to 17-year-olds (child report) with mental disorders received any services for their mental health problems; we report the weighted average in our meta-analysis.
Discussion
To inform policymaking to address children’s mental health in high-income countries, we conducted a systematic review and meta-analysis to determine the prevalence of childhood mental disorders and, where possible, associated service use. Fourteen high-quality studies from 11 high-income countries met the inclusion criteria, with a pooled sample of 61 545 children aged 4 to 18 years; eight studies also examined service use. The overall prevalence of any childhood mental disorder was 12.7%. The most common conditions were: any anxiety disorder 5.2%; ADHD 3.7%; oppositional defiant disorder 3.3%; any substance use disorder 2.3%; conduct disorder 1.3%; and major depressive disorder 1.3%. Among those with disorders, 26.5% had two or more disorders concurrently. Concerningly, only 44.2% of children with mental disorders received any services for these conditions.
These findings add to the extant literature in several ways that are salient for informing policymaking. To provide accurate population estimates, we have reported on only the most rigorous studies. To ensure comprehensiveness, we have included new studies not captured in previous reviews and have provided estimates for 12 of the most common disorders or disorder groups across a range of child ages. To inform service planning, we have also depicted the proportion of children in the general population who meet diagnostic disorder thresholds—including having both symptoms and impairment—and who therefore require mental health treatment services. As well, we have provided salient new data on service use by children with mental disorders.
We believe that our review can enable policymakers to better understand the mental health needs of children in high-income countries. In particular, policymakers can use our prevalence figures as benchmarks—calculating the numbers needing treatment at any given time within a given population or jurisdiction, then comparing the numbers in need with the numbers actually receiving mental health services. Service use does not always equate with need as defined by disorder prevalence. For example, families may seek services for children experiencing distress who do not meet diagnostic criteria. Consequently, prevalence data may under-represent service needs. However, prevalence data still provide critical population-level information for service planning. Importantly, our data cover children who are not receiving services—thereby providing a crucial supplement to administrative data on mental health service use.43 Beyond this, our data depict levels of need before the COVID-19 global pandemic. These pre-pandemic baseline data can facilitate planning, for example, to meet the increased children’s mental health needs that have emerged during the pandemic and that are predicted to continue.44 45
We acknowledge several limitations in the included studies. Our meta-regression analysis identified significant heterogeneity, particularly regarding measurement approaches used to determine diagnoses—underscoring longstanding methodological concerns about the use of differing measures and differing informants.25 46 47 While the studies we reported nevertheless arrived at robust estimates suitable for informing policymaking, future child mental health epidemiological research would benefit from better harmonisation of measures—including ensuring consistent and well-defined criteria for measuring impairment. As well, studies assessing service use mainly captured contacts (only). Future studies would benefit from adding more specific measures of intervention type, duration and intensity—data that would allow policymakers to gauge the reach, for example, of effective (vs unproven, ineffective or harmful) interventions.15–17 Such data could also inform more nuanced service planning, for example, informing tiered or layered approaches whereby more moderately-affected children might receive prevention services or services through schools and primary care, reserving specialised mental healthcare for those more severely affected.48
These limitations notwithstanding, we believe that urgent policy implications arise from our review. While it is not a new finding that high child mental disorder prevalence is coupled with severe service shortfalls, our updated data necessitate re-invigorated collective responses. Addressing children’s mental health first requires coherent central policy commitment and leadership—making this issue a priority and ensuring sustained engagement across all relevant public sectors including children’s services, healthcare, public health and education.48 49 Addressing children’s mental health also requires the development of comprehensive plans for: reducing avoidable adversities that contribute to the development of selected childhood mental disorders, such as socioeconomic disparities; preventing disorders in children at risk; providing treatment for all children with disorders; and tracking population outcomes through national surveillance programmes.30 48 As well, given that only an estimated 44.2% of children with mental disorders are receiving any services for these conditions, many countries will need to substantially increase children’s mental health budgets—and protect these budgets.48
Given severe service shortfalls, it is also crucial to consider quality assurance and efficiency. Quality assurance involves ensuring that effective—and only effective—interventions are offered, particularly given considerable high-quality research evidence on both prevention and treatment in the children’s mental health field.15–17 Quality assurance can also involve tracking child outcomes in general and clinical populations in order to evaluate the impact of policy efforts and to alter course and redeploy resources as needed.30 Efficiency, meanwhile, can involve building in prevention programming to avert avoidable individual burdens and to in turn reduce the burdens on treatment systems. While prevention programming has often been under-appreciated in the children’s mental health field, economic evaluation data suggest that preventing even just one case of a severe problem, such as childhood conduct disorder, may save an estimated $5.6 million (2021 USD equivalency) in lifetime costs—through averted healthcare, special education, child protection and justice system costs.9 In addition, adopting innovative service strategies and establishing tiers of service aligned with the type and intensity of need can help extend the reach of practitioners while also reaching more children—another form of efficiency.50 Beyond this, it is important to understand barriers to accessing services and how these may be addressed—to ensure that all children can access the mental health services they need when and where they need them.
Conclusions
We have depicted a high prevalence of childhood mental disorders coupled with unacceptable service shortfalls in high-income countries—to a degree that violates children’s rights.14 In essence, we have illuminated an invisible crisis in children’s mental health. In contrast, robust services are in place for child physical health problems such as cancer, diabetes and infectious diseases in most of these countries.11 12 Typical health expenditure levels indicate that high-income countries can also afford to do better.11–13 We therefore believe that our findings constitute a call to public action, taking the steps outlined above. This is particularly urgent given documented increases in children’s mental health needs since the onset of the COVID-19 pandemic—needs which are predicted to continue.44 45 The need for public action therefore could not be more urgent. Such action is essential if all children are to flourish. This collective flourishing will in turn benefit all—when fewer children needlessly experience mental disorders and associated disability, and when more children go on to thrive, contribute and meet their full potential.
Acknowledgments
KG holds the David R. (Dan) Offord Chair in Child Studies. During this project, CW was supported by a Canada Research Chair, Tier 2, in Children’s Health Policy. We also thank our reviewers, whose input greatly strengthened the manuscript.
Footnotes
Contributors: All authors contributed significantly to this manuscript, including the follow specific roles. Study concept and design: JLB, DY, CS and CW. Data acquisition: JLB, DY and CS. Data analysis: YZ, JLB and DY. Data interpretation: JLB, DY, CS, YZ, KG and CW. Drafting of manuscript: JLB, CS and CW. Revising of manuscript: JLB, DY, CS, YZ, KG and CW. All authors approved the final version.
Funding: The British Columbia Ministry of Children and Family Development, Child and Youth Mental Health Branch, funded this work (grant # BCMCFD#SL00444S01). (A short report summarizing the findings was provided to the funder).
Competing interests: KG and CW participated in the Ontario Child Health Study [reference s8] as Co-Principal Investigator and Co-Investigator, respectively. They therefore did not participate in decisions about inclusion, data extraction or interpretations regarding this study. KG was also an author on one other included study [reference s10] and did not participate in decisions about inclusion, data extraction or interpretation regarding this study. These two authors have no other conflicts to declare. All other authors declare no conflicts.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data covered in this systematic review and meta-analysis are available from the corresponding author, upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Copeland WE, Wolke D, Shanahan L, et al. Adult functional outcomes of common childhood psychiatric problems: a prospective, longitudinal study. JAMA Psychiatry 2015;72:892–9. 10.1001/jamapsychiatry.2015.0730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's world mental health survey initiative. World Psychiatry 2007;6:168–76. [PMC free article] [PubMed] [Google Scholar]
- 3. Erskine HE, Moffitt TE, Copeland WE, et al. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med 2015;45:1551–63. 10.1017/S0033291714002888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim-Cohen J, Caspi A, Moffitt TE, et al. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 2003;60:709–17. 10.1001/archpsyc.60.7.709 [DOI] [PubMed] [Google Scholar]
- 5. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 2007;20:359–64. 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lim K-L, Jacobs P, Ohinmaa A, et al. A new population-based measure of the economic burden of mental illness in Canada. Chronic Dis Can 2008;28:92–8. 10.24095/hpcdp.28.3.02 [DOI] [PubMed] [Google Scholar]
- 7. Fineberg NA, Haddad PM, Carpenter L, et al. The size, burden and cost of disorders of the brain in the UK. J Psychopharmacol 2013;27:761–70. 10.1177/0269881113495118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Olesen J, Gustavsson A, Svensson M, et al. The economic cost of brain disorders in Europe. Eur J Neurol 2012;19:155–62. 10.1111/j.1468-1331.2011.03590.x [DOI] [PubMed] [Google Scholar]
- 9. Cohen MA, Piquero AR. New evidence on the monetary value of saving a high risk youth. J Quant Criminol 2009;25:25–49. 10.1007/s10940-008-9057-3 [DOI] [Google Scholar]
- 10. Waddell C, Schwartz C, Andres C. Making children’s mental health a public policy priority: for the one and the many. Public Health Ethics 2018;11:191–200. 10.1093/phe/phx018 [DOI] [Google Scholar]
- 11. United Kingdom (UK) Office for National Statistics . Healthcare expenditure, UK health accounts, 2020. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/bulletins/ukhealthaccounts/2018 [Accessed Feb 2021].
- 12. Martin AB, Hartman M, Lassman D, et al. National health care spending in 2019: steady growth for the fourth consecutive year. Health Aff 2021;40:14–24. 10.1377/hlthaff.2020.02022 [DOI] [PubMed] [Google Scholar]
- 13. Canadian Institute for Health Information (CIHI) . National health expenditure trends, 2020. Ottawa, ON: CIHI, 2021. [Google Scholar]
- 14. United Nations General Assembly . Convention on the rights of the child, 1989. Available: https://www.unicef.org/child-rights-convention/convention-text [Accessed Apr 2021].
- 15. Waddell C, Schwartz C, Andres C, et al. Fifty years of preventing and treating childhood behaviour disorders: a systematic review to inform policy and practice. Evid Based Ment Health 2018;21:45–52. 10.1136/eb-2017-102862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schwartz C, Barican JL, Yung D, et al. Six decades of preventing and treating childhood anxiety disorders: a systematic review and meta-analysis to inform policy and practice. Evid Based Ment Health 2019;22:103–10. 10.1136/ebmental-2019-300096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schwartz C, Yung D, Barican J. Preventing and treating childhood mental disorders: effective interventions. Vancouver, BC: Children’s Health Policy Centre, Faculty of Health Sciences, Simon Fraser University, 2020. [Google Scholar]
- 18. Costello EJ, Burns BJ, Angold A, et al. How can epidemiology improve mental health services for children and adolescents? J Am Acad Child Adolesc Psychiatry 1993;32:1106–17. 10.1097/00004583-199311000-00002 [DOI] [PubMed] [Google Scholar]
- 19. Ford T. Practitioner review: how can epidemiology help us plan and deliver effective child and adolescent mental health services? J Child Psychol Psychiatry 2008;49:900–14. 10.1111/j.1469-7610.2008.01927.x [DOI] [PubMed] [Google Scholar]
- 20. Fox DM. Evidence and health policy: using and regulating systematic reviews. Am J Public Health 2017;107:88–92. 10.2105/AJPH.2016.303485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Greenhalgh T, Malterud K. Systematic reviews for policymaking: muddling through. Am J Public Health 2017;107:97–9. 10.2105/AJPH.2016.303557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barkmann C, Schulte-Markwort M. Prevalence of emotional and behavioural disorders in German children and adolescents: a meta-analysis. J Epidemiol Community Health 2012;66:194–203. 10.1136/jech.2009.102467 [DOI] [PubMed] [Google Scholar]
- 23. Erskine HE, Baxter AJ, Patton G, et al. The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiol Psychiatr Sci 2017;26:395–402. 10.1017/S2045796015001158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011;21:655–79. 10.1016/j.euroneuro.2011.07.018 [DOI] [PubMed] [Google Scholar]
- 25. Polanczyk GV, Salum GA, Sugaya LS, et al. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 2015;56:345–65. 10.1111/jcpp.12381 [DOI] [PubMed] [Google Scholar]
- 26. Williams NJ, Scott L, Aarons GA. Prevalence of serious emotional disturbance among U.S. children: a meta-analysis. Psychiatr Serv 2018;69:32–40. 10.1176/appi.ps.201700145 [DOI] [PubMed] [Google Scholar]
- 27. American Psychiatric Association (APA) . Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: APA, 2013. [Google Scholar]
- 28. World Health Organization . Classification of diseases (ICD), 2020. Available: https://www.who.int/standards/classifications/classification-of-diseases [Accessed Feb 2021].
- 29. Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011;378:1515–25. 10.1016/S0140-6736(11)60827-1 [DOI] [PubMed] [Google Scholar]
- 30. World Health Organization . Mental health atlas 2017, 2018. Available: https://www.who.int/publications/i/item/mental-health-atlas-2017 [Accessed Sep 2020].
- 31. Stroup DF, Berlin JA, Morton SC. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 32. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 33. American Psychiatric Association . DSM history, 2020. Available: https://www.psychiatry.org/psychiatrists/practice/dsm/history-of-the-dsm [Accessed Sep 2020].
- 34. World Bank Group . High income, 2021. Available: https://data.worldbank.org/country/XD [Accessed Jun 2021].
- 35. Merikangas KR, He J-P, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010;49:980–9. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012;65:934–9. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 37. Grills AE, Ollendick TH. Issues in parent-child agreement: the case of structured diagnostic interviews. Clin Child Fam Psychol Rev 2002;5:57–83. 10.1023/A:1014573708569 [DOI] [PubMed] [Google Scholar]
- 38. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010;36:1–48. 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 39. Burns BJ, Costello EJ, Angold A, et al. Children’s mental health service use across service sectors. Health Aff 1995;14:147–59. 10.1377/hlthaff.14.3.147 [DOI] [PubMed] [Google Scholar]
- 40. Mansbach-Kleinfeld I, Farbstein I, Levinson D, et al. Service use for mental disorders and unmet need: results from the Israel survey on mental health among adolescents. Psychiatr Serv 2010;61:241–9. 10.1176/ps.2010.61.3.241 [DOI] [PubMed] [Google Scholar]
- 41. Costello EJ, He J-ping, Sampson NA, et al. Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey-Adolescent. Psychiatr Serv 2014;65:359–66. 10.1176/appi.ps.201100518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johnson SE, Lawrence D, Hafekost J, et al. Service use by Australian children for emotional and behavioural problems: findings from the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2016;50:887–98. 10.1177/0004867415622562 [DOI] [PubMed] [Google Scholar]
- 43. Waddell C, Shepherd CA, Chen A, et al. Creating comprehensive children’s mental health indicators for British Columbia. Can J Commun Ment Health 2013;32:9–27. 10.7870/cjcmh-2013-003 [DOI] [Google Scholar]
- 44. Waddell C, Schwartz C, Barican J. COVID-19 and the impact on children’s mental health. Vancouver, BC: Children’s Health Policy Centre, Faculty of Health Sciences, Simon Fraser University, 2020. [Google Scholar]
- 45. Newlove-Delgado T, McManus S, Sadler K, et al. Child mental health in England before and during the COVID-19 lockdown. Lancet Psychiatry 2021;8:353–4. 10.1016/S2215-0366(20)30570-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Waddell C, Offord DR, Shepherd CA, et al. Child psychiatric epidemiology and Canadian public policy-making: the state of the science and the art of the possible. Can J Psychiatry 2002;47:825–32. 10.1177/070674370204700903 [DOI] [PubMed] [Google Scholar]
- 47. Roberts RE, Attkisson CC, Rosenblatt A. Prevalence of psychopathology among children and adolescents. Am J Psychiatry 1998;155:715–25. 10.1176/ajp.155.6.715 [DOI] [PubMed] [Google Scholar]
- 48. Waddell C, Georgiades K, Duncan L, et al. 2014 Ontario child health study findings: policy implications for Canada. Can J Psychiatry 2019;64:227–31. 10.1177/0706743719830033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Duncan L, Boyle MH, Abelson J, et al. Measuring children's mental health in Ontario: policy issues and prospects for change. J Can Acad Child Adolesc Psychiatry 2018;27:88–98. [PMC free article] [PubMed] [Google Scholar]
- 50. Hollis C, Falconer CJ, Martin JL, et al. Annual research review: digital health interventions for children and young people with mental health problems - a systematic and meta-review. J Child Psychol Psychiatry 2017;58:474–503. 10.1111/jcpp.12663 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ebmental-2021-300277supp001.pdf (876.7KB, pdf)
Data Availability Statement
Data covered in this systematic review and meta-analysis are available from the corresponding author, upon reasonable request.