Research from earlier waves of the COVID-19 pandemic shows that COVID-related stress—worry about becoming infected, socioeconomic concerns, xenophobia, compulsive checking behaviors, and traumatic stress reactions—waxes and wanes with rates of infection from SARS-CoV2 as well as the tightening and relaxing of public health measures (Asmundson and Taylor, 2020, Taylor, 2022). With the emergence of the highly transmissible Omicron variant, there has been a corresponding increase in COVID-related stress spanning the gamut of fears of infection to supply chain and essential service workers to over-capacity healthcare systems. Some of these stressors are similar to prior waves of the pandemic whereas others are unique or of higher intensity; as such, while the extant research may inform evidence-based responses to the current wave of infection, additional research is needed to guide interventions for pandemic-related stressors across waves and in unique circumstances. One group for which there has been little focus on the mechanisms through which the pandemic has impacted COVID-related stress levels is older adults.
Older adults have been disproportionally affected across the various waves of the COVID-19 pandemic, through increased risk of mortality, hospitalization, and intensive care unit admissions (e.g., De Pue et al., 2021; Modig, Ahlbom, & Ebeling, 2021; Sciensano, 2021; United Nations, 2020; Wiley et al., 2021; Zhang et al., 2021). Moreover, although all age groups have been impacted by public health measures and guidelines designed to mitigate the spread of COVID-19, given their heightened vulnerability to serious infection outcomes, extra regulations have been put in place that have had specific and unique impacts on older persons. For older adults in long-term care facilities, for example, the effect of public health measures has been more extreme and with potentially dire consequences (e.g., not allowing family visitors into long term care facilities, isolating older residents in their rooms for inordinate amounts of time with no social contact whatsoever). Compounding the restrictions imposed in long-term care settings, increased infection control demands combined with staff shortages have resulted in residents missing meals or being left in unsanitary conditions (Taylor, 2020), adding to potential COVID-related stress experienced by the long-term care residents as well as their family members.
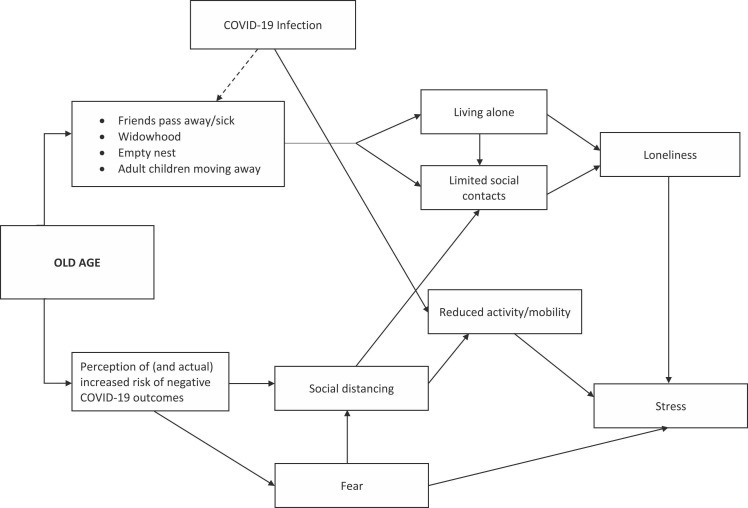
Although COVID-related stress and anxiety are not necessarily more elevated in community dwelling older persons compared to younger age groups (Klaiber et al., 2021, Taylor et al., 2020), possibly due to their resilience or other stress mitigating factors such relative financial stability (Vahia, Jeste, & Reynolds, 2020), we have conceptualized several ways in which the COVID-19 pandemic may uniquely impact stress levels in older individuals (see Fig. 1). Older persons, and especially older women, are more likely to be living alone due to factors such as widowhood or adult children moving away (Tang, Galbraith, & Truong, 2019). Moreover, with a disproportionally high number of deaths due to COVID-19 in the older population (e.g., Modig et al., 2021), the high prevalence of COVID-19 infections is a potential secondary contributor to an increased probability of living alone or becoming socially isolated as friends and older family members (e.g., spouses) die. In turn, living alone and social isolation is likely to result in feelings of loneliness, a known contributor to stress that has been associated with increased mortality (e.g., Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015).
Fig. 1.
Conceptual framework to guide understanding and research on COVID-related stress in older people. The dotted line indicates a secondary contribution.
Further contributing to COVID-related stress, older individuals are at increased risk of hospitalization and severe illness from SARS-CoV2 infection as well as other sources. Recognizing this risk, older persons experience increased fear of infection (Han, Mahendran, & Yu, 2021), which tends to lead to stricter adherence to social distancing and isolation-related public health guidance (Boyraz et al., 2020, Kowalczuk and Gębski, 2021). Older persons with dementia, who rely on others for their care, may similarly experience increased isolation due to avoidance behaviors of caregivers who have fears about passing the virus to their care recipient. Those with limited access to technology and the internet may be even more likely to feel isolated (e.g., Johnson, 2021). Regardless, reductions in in-person contacts have negative consequences that may not be easy to mitigate with other forms of communication. Fingerman et al. (2021) showed, for instance, that telephone contact did not confer the same types of affective benefits as in-person contact for older adults living alone during the pandemic.
In addition to increasing probability of social isolation, fear of becoming infected with COVID-19 has been associated with negative affect and increased illness risk perception in older adults (Han et al., 2021). Such fear exacerbates stress, both directly as well as indirectly, through more social isolation. In turn, social isolation has been associated with reduced mobility and activity in order individuals (Saraiva et al., 2021). Given the known benefits of physical activity on the psychological well-being of older persons during the pandemic, a significant reduction in mobility and activity is likely to result in increased stress and reduced quality of life, especially for those who experience frailty (Carriedo et al., 2020, Saraiva et al., 2021). As physical activity decreases, frailty is likely to become exacerbated, in part because reduced physical activity results in increased sarcopenia (i.e., progressive and generalized loss of muscle mass and strength; Yamada et al., 2020). The COVID-19 illness itself can contribute further to reductions in activity and mobility, even after infection resolves, due to lingering symptoms such as headaches and fatigue. The negative effects of loneliness and reduced physical activity and mobility may be short-lived, particularly as public health measures become relaxed with decreasing infection rates; however, with a persisting pandemic that requires continuing public health measures, impacts on older adults’ mental health may be long lasting (Stolz, Mayerl, & Freidl, 2021).
The mechanisms and outcomes outlined in Fig. 1 have been proposed to help explain a prominent dose-response association between COVID-related stress, loneliness, anxiety, and depression that have been identified in older persons during the pandemic (e.g., Robb et al., 2020). Compounding the disproportional impact of the COVID-19 pandemic on health outcomes, older adults are less likely to be referred for mental health services and are underrepresented among the recipients of such services (e.g., Chaplin, Farquharson, Clapp, & Crawford, 2015; Prina et al., 2014). With this in mind, we outline a series of recommendations to stimulate related and much needed research and identify potential strategies to mitigate these negative psychological outcomes.
-
1)
Public health campaigns should raise awareness regarding the impact of social isolation and loneliness on older adult COVID-related stress and well being. These campaigns should include guidance for health professionals and informal caregivers regarding best ways of recognizing social isolation, loneliness, and their negative effects on stress and coping and for selecting suitable interventions (Wu, 2020).
-
2)
Health professional continuing education initiatives on assessment, prevention, and management of loneliness, social isolation, and COVID-related stress should be pursued.
-
3)
Municipal, long-term care, and other organizations should develop, offer, and promote programming designed to increase safe and appropriate physical activity and social interaction in older persons while respecting COVID-19 public health protocols (e.g., outdoors where possible, using N-97 respirators and physical distancing). The benefits of physical activity for anxiety and stress reduction generally (Asmundson et al., 2013) and older adults specifically during the COVID-19 pandemic are well supported (Callow et al., 2020).
-
4)
Media stories could be designed to specifically highlight the special stressors and problems that older adults face during the pandemic as well as available resources aimed to help older adults combat stress.
-
5)
The augmentation of existing therapeutic resources with remotely-delivered interventions will be an important avenue of development and evaluation. Initial evidence suggests that older adults are able to form therapeutic bonds, through video-delivered evidence-based psychological interventions, that are as strong as those developed in face-to-face therapy and that they have a preference for video- over telephone-delivered approaches (Lichstein et al., 2013). Moreover, other evidence-based self-help initiatives (e.g., self-help workbooks) could be promoted and made widely available.
-
6)
The public could be encouraged via targeted media campaigns to check regularly with their older family members and offer them social support (Gorenko, Moran, Flynn, Dobson, & Konnert, 2021). The effectiveness of video calls with family in reducing psychological distress has been demonstrated (Tsai & Tsai, 2011) and such video calls could be facilitated and especially encouraged frequently and on a regular basis by long-term care facilities (Gorenko et al., 2021).
These are but a few targeted strategies that might serve to mitigate negative psychological outcomes in older adults, particularly in the face of prolonged and, with the highly transmissible Omicrom variant, increasing COVID-related stress. It will be important for any interventions specifically designed to alleviate COVID-related stress in older adults to be co-developed with older adults who have lived experience of COVID-19-related adjustment issues and who can advise on barriers and facilitators in the effective delivery of these interventions. Such interventions will also need to be evaluated systematically and implementation science principles, combined with large scale knowledge mobilization efforts, will be needed to facilitate their wide-spread adoption. While it is probable that the current issues specific to the Omicron variant will have passed by the time the suggested strategies are fully evaluated in systematic fashion, they may have important applications prior to the end of the COVID-19 pandemic and will most certainly hold relevance and better prepare us to address the specific mental health needs of older adults during the next pandemic.
Conflict of interest
We have no conflicts of interest to disclose.
References
- Asmundson G.J.G., Fetzner M.G., DeBoer L.B., Powers M.B., Otto M.W., Smits J.A.J. Let’s get physical: A contemporary review of the anxiolytic effects of exercise for anxiety and its disorders. Depression and Anxiety. 2013;30(4):362–373. doi: 10.1002/da.22043. [DOI] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. Coronaphobia revisted: A state-of-the-art on pandemic-related fear, anxiety, and stress. Journal of Anxiety Disorders. 2020;76 doi: 10.1016/j.janxdis.2020.102326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyraz G., Legros D.N., Tigershtrom A. COVID-19 and traumatic stress: the role of perceived vulnerability, COVID-19-related worries, and social isolation. Journal of Anxiety Disorders. 2020;76 doi: 10.1016/j.janxdis.2020.102307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callow D.D., Arnold-Nedimala N.A., Jordan L.S., Pena G.S., Won J., Woodard J.L., Smith J.C. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. The American Journal of Geriatric Psychiatry. 2020;28(10):1046–1057. doi: 10.1016/j.jagp.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carriedo A., Cecchini J.A., Fernandez-Rio J., Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. The American Journal of Geriatric Psychiatry. 2020;28(11):1146–1155. doi: 10.1016/j.jagp.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin R., Farquharson L., Clapp M., Crawford M. Comparison of access, outcomes and experiences of older adults and working age adults in psychological therapy: older adults and psychological therapy. International Journal of Geriatric Psychiatry. 2015;30(2):178–184. doi: 10.1002/gps.4122. [DOI] [PubMed] [Google Scholar]
- De Pue S., Gillebert C., Dierckx E., Vanderhasselt M.-A., De Raedt R., Van den Bussche E. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Scientific Reports. 2021;11(1):4636. doi: 10.1038/s41598-021-84127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman K.L., Ng Y.T., Zhang S., Britt K., Colera G., Birditt K.S., Charles S.T. Living alone during COVID-19: social contact and emotional well-being among older adults. The Journals of Gerontology: Series B. 2021;76(3):e116–e121. doi: 10.1093/geronb/gbaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorenko J.A., Moran C., Flynn M., Dobson K., Konnert C. Social isolation and psychological distress among older adults related to COVID-19: A narrative review of remotely-delivered interventions and recommendations. Journal of Applied Gerontology. 2021;40(1):3–13. doi: 10.1177/0733464820958550. [DOI] [PubMed] [Google Scholar]
- Han M.F.Y., Mahendran R., Yu J. Associations between fear of COVID-19, affective symptoms and risk perception among community-dwelling older adults during a COVID-19 lockdown. Frontiers in Psychology. 2021;12 doi: 10.3389/fpsyg.2021.638831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on Psychological Science. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Johnson, J., 2021, Share of adults in the United States who use the internet in 2021, by age group. 〈https://www.statista.com/statistics/266587/percentage-of-internet-users-by-age-groups-in-the-us/〉.
- Klaiber P., Wen J.H., DeLongis A., Sin N.L. The ups and downs of daily life during COVID-19: age differences in affect, stress, and positive events. The Journals of Gerontology: Series B. 2021;76(2):e30–e37. doi: 10.1093/geronb/gbaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalczuk I., Gębski J. Impact of fear of contracting COVID-19 and complying with the rules of isolation on nutritional behaviors of polish adults. International Journal of Environmental Research and Public Health. 2021;18(4):1631. doi: 10.3390/ijerph18041631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein K.L., Scogin F., Thomas S.J., DiNapoli E.A., Dillon H.R., McFadden A. Telehealth cognitive behavior therapy for co-occurring insomnia and depression symptoms in older adults: insomnia and depression. Journal of Clinical Psychology. 2013;69(10):1056–1065. doi: 10.1002/jclp.22030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prina A.M., Marioni R.E., Hammond G.C., Jones P.B., Brayne C., Dening T. Improving access to psychological therapies and older people: Findings from the Eastern Region. Behaviour Research and Therapy. 2014;56:75–81. doi: 10.1016/j.brat.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modig K., Ahlbom A., Ebeling M. Excess mortality from COVID-19: weekly excess death rates by age and sex for Sweden and its most affected region. European Journal of Public Health. 2021;31(1):17–22. doi: 10.1093/eurpub/ckaa218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robb C.E., de Jager C.A., Ahmadi-Abhari S., Giannakopoulou P., Udeh-Momoh C., McKeand J.…Middleton L. Associations of social isolation with anxiety and depression during the early COVID-19 Pandemic: a survey of older adults in London, UK. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.591120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraiva M.D., Apolinario D., Avelino-Silva T.J., De Assis Moura Tavares C., Gattás-Vernaglia I.F., Marques Fernandes C.…Romero Aliberti M.J. The impact of frailty on the relationship between life-space mobility and quality of life in older adults during the COVID-19 pandemic. The Journal of Nutrition, Health & Aging. 2021;25(4):440–447. doi: 10.1007/s12603-020-1532-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciensano, 2021, EPISTAT: Infectious Diseases Data Explorations & Visualizations—COVID-19. 〈https://epistat.wiv-isp.be/home/〉.
- Stolz E., Mayerl H., Freidl W. The impact of COVID-19 restriction measures on loneliness among older adults in Austria. European Journal of Public Health. 2021;31(1):44–49. doi: 10.1093/eurpub/ckaa238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J., Galbraith N., Truong J. Living Alone in Canada (Insights on Canadian Society) Statistics Canada. 2019 〈https://epe.lac-bac.gc.ca/100/201/301/weekly_acquisitions_list-ef/2019/19-10/publications.gc.ca/collections/collection_2019/statcan/75-006-x/75-006-2019-3-eng.pdf〉 [Google Scholar]
- Taylor G. Government of Canada; 2020. Canadian Armed Forces: JTFC Observations in Long Term Care Facilities in Ontario.〈https://s3.documentcloud.org/documents/6928480/OP-LASER-JTFC-Observations-in-LTCF-in-On.pdf〉 [Google Scholar]
- Taylor S. The psychology of pandemics. Annual Review of Clinical Psychology. 2022;18(1) doi: 10.1146/annurev-clinpsy-072720-020131. [DOI] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. COVID stress syndrome: concept, structure, and correlates. Depression and Anxiety. 2020;37(8):706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai H.-H., Tsai Y.-F. Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3-month videoconference program for older nursing home residents. Journal of Medical Internet Research. 2011;13(4) doi: 10.2196/jmir.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Policy Brief: The Impact of COVID-19 on older persons. 2020:1–16. 〈https://unsdg.un.org/sites/default/files/2020-05/Policy-Brief-The-Impact-of-COVID-19-on-Older-Persons.pdf〉 [Google Scholar]
- Vahia I.V., Jeste D.V., Reynolds C.F. Older adults and the mental health effects of COVID-19. JAMA. 2020;324(22):2253. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- Wiley Z., Kubes J.N., Cobb J., Jacob J.T., Franks N., Plantinga L., Lea J. Age, comorbid conditions, and racial disparities in COVID-19 outcomes. Journal of Racial and Ethnic Health Disparities. 2021 doi: 10.1007/s40615-020-00934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B. Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Global Health Research and Policy. 2020;5(1):27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada M., Kimura Y., Ishiyama D., Otobe Y., Suzuki M., Koyama S.…Arai H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: a cross-sectional online survey. The Journal of Nutrition, Health & Aging. 2020;24(9):948–950. doi: 10.1007/s12603-020-1501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Guo L., Huang L., Zhang C., Luo R., Zeng L.…Lian Q. Distinct disease severity between children and older adults with Coronavirus Disease 2019 (COVID-19): impacts of ACE2 expression, distribution, and lung progenitor cells. Clinical Infectious Diseases. 2021;73(11):e4154–e4165. doi: 10.1093/cid/ciaa1911. [DOI] [PMC free article] [PubMed] [Google Scholar]