Abstract
Arthrodesis of the proximal interphalangeal (PIP) joint of the finger is an established procedure for advanced osteoarthritis. As there are different techniques of fusion, it seems necessary to evaluate the results.
Primary outcome of this review was to evaluate different arthrodesis methods of the PIP joint and describe different numbers of non-unions. Secondary outcome was to evaluate time to consolidation. Respective complications, if mentioned, were listed additionally.
The review process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The selected databases were PubMed, Medline, Embase, Google Scholar and Cochrane Library. Studies reporting outcomes of the arthrodesis with a defined technique and radiological consolidation were included. Complication rates and types were recorded. In total, 6162 articles could be identified, 159 full-texts were assessed and 64 studies were included. Methodological quality was assessed using Methodological Index for Non-Randomized Studies.
A total of 1923 arthrodeses of the PIP joint could be identified. Twelve different surgical techniques were described, four of these techniques with compression at the arthrodesis site. The most frequently used techniques were K-wires (n = 743, 14 studies), tension-band (n = 313, 15 studies) and compression screws (n = 233, 12 studies). The lowest rate of described non-unions in compression techniques was 3.9% with the compression screw. The highest non-union rate of 8.6% was achieved by interosseous wiring.
All the described techniques can achieve the goal of fusing an osteoarthritic joint. There is a tendency in the more recent literature for the use of compression techniques.
Keywords: arthrodesis PIP joint, arthrodesis interphalangeal joint, fusion PIP joint, fusion interphalangeal joint, osteoarthritis PIP joint, osteoarthritis interphalangeal joint, treatment osteoarthritis finger
Introduction
Osteoarthritis of the proximal interphalangeal (PIP) joint, either primary or secondary, limits the range of motion and causes pain with or without instability, leading to significant global hand function impairment (1). Typical aetiologies leading to secondary osteoarthritis are posttraumatic changes, chronic instability or inflammatory diseases, for example rheumatoid arthritis or scleroderma. Operative treatment options include denervation, different arthroplasties, prosthesis or arthrodesis. The aim of arthrodeses is pain reduction in combination with a sufficient global hand function (2). With distinctive deformation of the joint and/or preexisting instability, there is a tendency to recommend arthrodesis because an unstable prothesis is prone to failure. In these cases, the fusion of the joint provides reliable results.
In posttraumatic osteoarthritis, especially of the radial digits with an instability not exceeding 30°, a prothesis could provide excellent results (3, 4). If more than one joint is affected, especially in patients with rheumatoid arthritis, and only a moderate instability exists, silicone arthroplasty is still the method of choice (5).
Arthrodesis of the PIP joint is an established technique for advanced osteoarthritis or when other reconstruction methods have failed. Different techniques for arthrodesis of the PIP joint have been described and their main difference is if there is compression on the arthrodesis or not (6). There is no clear indication in the current literature as to which technique shows the most promising results in terms of union. Typical major complications of PIP joint arthrodesis are non-union and mal-union; minor complications are superficial infections (61).
The aim of this first systematic review was to clarify the following questions: Do different arthrodesis methods of the PIP joint for primary and secondary causes of osteoarthritis or destruction of the joint show (i) different numbers of non-unions? (primary outcome) and (ii) different times to consolidation? (secondary outcome). The different complications of each technique were additionally included but not further evaluated.
Methods
Search methods
The review process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (7). Two reviewers (MM and HV) independently selected studies for inclusion. Disagreements were solved by discussion with a senior author (MR).
The search was conducted from January 1, 1946, to April 28, 2020, in the following databases: PubMed, Medline, Embase, Google Scholar and Cochrane Library by the main author. We initially searched without any language or publication type restrictions. The search algorithm is shown in Table 1.
Table 1.
The respective search string of the different included databases.
| Database | Search string |
|---|---|
| Pubmed | (((proximal interphalangeal joint[Title/Abstract]) OR (pij[Title/Abstract]) OR (pip-joint[Title/Abstract]) OR (finger[Title/Abstract]) OR (digital[Title/Abstract]) OR (pipj[Title/Abstract]) OR (proximal interphalangeal[Title/Abstract])) AND ((arthrodesis[Title/Abstract]) OR (fusion[Title/Abstract]))) NOT equine[Title/Abstract] |
| Embase | (‘proximal interphalangeal joint’/exp OR pij:ab,ti OR ‘pip joint’:ab,ti OR ‘proximal interphalangeal joint’:ti,ab OR ‘digital’:ab,ti OR ‘finger’:ab,ti) AND (‘arthrodesis’:ti,ab OR ‘fusion’:ab,ti) AND [embase]/lim |
| Cochrane Library | (pij OR pip joint OR pip-joint OR proximal-interpalangeal-joint OR proximal interphalangeal joint OR digital OR finger) AND (arthrodesis OR fusion) |
| Google Scholar | allintitle: (“pij” OR “pip joint” OR “proximal interphalangeal joint” OR “digital” OR “finger”) AND (“arthrodesis” OR “fusion”) |
Selection criteria
Full-text reports (original articles, randomized controlled trials, controlled clinical trials, retrospective or prospective observational studies, case series and technical descriptions) concerning PIP joint arthrodesis were screened.
Reference lists from included studies and reviews were screened for additional studies and included. Studies reporting outcomes of the arthrodesis with a defined technique and radiological consolidation were included. Complication rates and types were recorded. Clinical studies with an evidence level of I–IV were included. As there were studies which compared arthrodeses to other techniques of joint salvage, those reporting of five or less arthrodeses were also included.
Studies lacking original data, studies whose data were not doubtlessly concerning the PIP joint as well as studies whose full-text were not available were excluded. Doctoral theses were also excluded.
The search flowchart according to the PRISMA guidelines is depicted in Fig. 1. Initially, 6162 articles were identified. Thirteen additional records from reference lists were included. After removing 1914 duplicates, 4261 articles remained. By screening titles and abstracts, a further 4102 studies were excluded.
Figure 1.
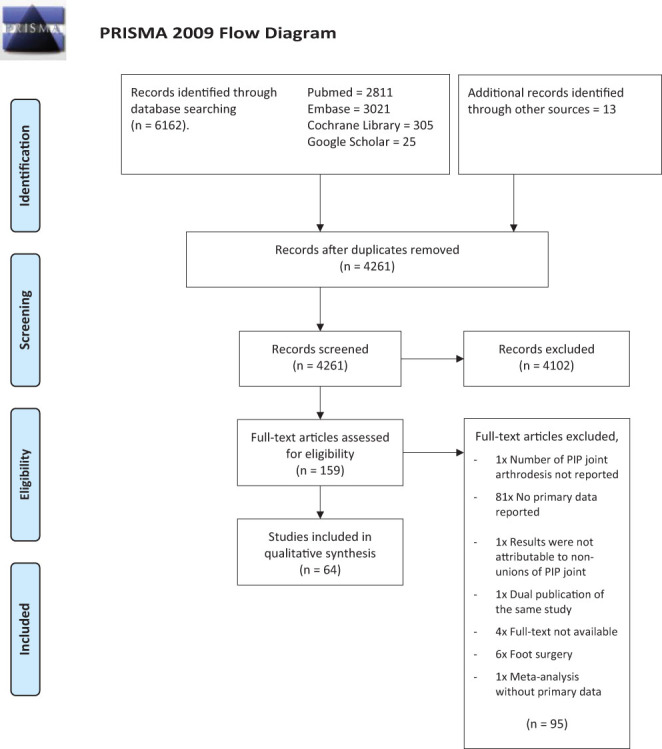
This PRISMA flowchart shows the numbers of articles identified as well as the inclusion and exclusion steps.
The full text of 159 articles was thoroughly assessed and evaluated for reporting the number of treated PIP joints, the technique used and the primary endpoint of consolidation. The 64 studies depicted in Table 2 were finally included, and data were extracted from these based on the inclusion criteria. Six studies that focused on diseases of connective tissue, for example rheumatoid arthritis, were mentioned separately from other indications.
Table 2.
Studies of arthrodeses of the PIP joint of the finger with different techniques.
| Reference | Year | LoE | MINORS score | Technique | Arthrodeses, n | Non-union, n | Consolidation (t) | Finger | IMM (t) | PROM (type, data) | Complications (Y/N) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Al-Qattan (9)1 | 2016 | IV | 11 | Interosseus + K-wire | 5 | 0 | 5 weeks | 5× DII | NR | NR | N |
| Allende & Engelem (10)2 | 1980 | IV | 8 | Tension-band | 16 | 0 | 4–6 weeks | 5× DII, 3× DIII, 4× DIV, 3× DV | Splint for discomfort | NR | Y – Lateral deviation; infection |
| Arata et al. (11) | 2003 | IV | 9 | Bioabsorbale rod | 1 | 0 | 7.9 weeks | NR | 3–4 weeks | NR | N |
| Ayres et al. (12) | 1988 | IV | 10 | Herbert screw | 51 | 1 | 6 weeks | NR | 2 weeks | NR | Y – 4× fracture dorsal cortex, 2× pain |
| Bansky & Racz (13) | 2005 | IV | 3 | Plate | 2 | 0 | NR | 2× DII | NR | NR | N |
| Baruch & Kahanovich (14)3 | 1980 | IV | 4 | Angulated bone peg | 5 | 0 | NR | NR | 3 weeks | NR | N |
| Biskop (15)4 | 1985 | IV | 11 | Tension-band | 25 | 0 | 12 weeks | 7× DII, 5× DIII, 9× DIV, 4× DV | – | NR | Y – 2× inflammation |
| Breyer et al. (16) | 2015 | III | 10 | Tension-band | 24 | 2 | 9.4 weeks | NR | 2–3 weeks | NR | Y – 5× superficial infection |
| Compression screw | 29 | 1 | 9.8 weeks | NR | 2–3 weeks | NR | Y – 1× superficial infection, 1× deep infection | ||||
| Buechler & Aiken (17) | 1987 | IV | 10 | Bone graft and plate | 25 | 2 | 45–90 days | 5× DII, 13 DIII, 6 DIV, 1 DV | NR | NR | Y – 1× infection |
| Buck-Gramcko & Oehme (18)5 | 1988 | III | 6 | Interosseus + K-wire | 84 | NR | 7 weeks | NR | NR | TAM | Y – 22× superficial infection, 3× osteoporotic fracture, three hardware failure |
| Lag screw | 6 | NR | 8.1 weeks | NR | NR | TAM | Y – 4× fracture dorsal cortex, 2× rotation, 1× tissue defect | ||||
| Tension-band | 20 | NR | 8.2 weeks | NR | NR | TAM | |||||
| K-wires | 8 | NR | 10.6 weeks | NR | NR | TAM | |||||
| Burton et al. (19) | 1986 | IV | 12 | K-wires | 34 | 0 | 9.2 weeks | NR | 3–4 weeks | NR | Y – 2× delayed union, 1× arterial spasm |
| Carroll & Hill (20) | 1969 | IV | 6 | Cup/cone + K-wire | 230 | 9 | 6–8 weeks | NR | 6–8 weeks | NR | Y – 4× rotational error |
| Faithfull & Herbert (21) | 1984 | IV | 4 | Herbert screw | 5 | 0 | NR | NR | – | NR | N |
| Goth & Konigsberger (22) | 1996 | IV | 9 | Lag screw | 23 | 0 | 7.5 weeks | NR | 2 weeks | PS-100° | N |
| Harrison & Nicolle (23) | 1974 | IV | 2 | Harrison–Nicolle peg | 35 | 1 | NR | NR | 2 weeks | NR | Y – 1× infection |
| Herzog (24) | 1961 | IV | 5 | Bone peg | 11 | 0 | 8–12 weeks | NR | 5 weeks | NR | N |
| Hoffmann & Rossack (25) | 1975 | IV | 6 | External fixation | 10 | 0 | NR | NR | 5 days | NR | N |
| Høgh & Jensen (26)6 | 1982 | IV | 9 | Interosseus + K-wire | 23 | NR | 8 weeks | NR | 6 weeks | NR | Y – 1× infection, 1× pain with amputation |
| Hohendorff et al. (27) | 2016 | IV | 9 | Tension-band | 16 | 1 | NR | 5× DII 4× DIII, 1× DIV, 6× DV | 6 weeks | Pain VAS, DASH, PS | Y – 1× infection |
| Jones et al. (28) | 2011 | III | 8 | K-wires | 2 | 1 | 9 months | 1× DII, 1× DIV | NR | MHOQ | Y – 2× malunion |
| Tension-band | 10 | 3 | 10 weeks | 4× DII, 4× DIII, 2× DIV | NR | ||||||
| Plate | 1 | 1 | 1× DV | NR | |||||||
| Khuri (29) | 1986 | IV | 8 | Tension-band | 10 | 0 | 6–8 weeks | 4× DII, 2× DIV, 4× DV | 7–10 days | NR | N |
| Kowalski & Manske (30) | 1988 | IV | 10 | K-wires | 6 | 0 | 6–12 weeks | 2× DII, 2× DIV, 2× DV | 6 weeks | NR | N |
| Kvasnička (31) | 2019 | IV | 8 | External fixation | 2 | 0 | 6.9 weeks | NR | NR | NR | N |
| Leibovic et al. (32) | 1994 | III | 10 | K-wires | 99 | 21 | 10 weeks | 49× DII, 63× DIII, 51× DIV, 61× DV | NR | NR | Y – 3x superficial infection, 1× osteomyelitis, 2× CRPS |
| Tension-band | 66 | 3 | 11 weeks | ||||||||
| Herbert screw | 35 | 0 | 9 weeks | ||||||||
| Plate | 4 | 2 | 12 weeks | ||||||||
| Leonard & Capen (33) | 1979 | IV | 8 | External fixation | 21 | 4 | 8 weeks | 3× DII, 2× DIII, 6× DIV, 10× DV | 8 weeks | NR | NR |
| Lewis et al. (34) | 1986 | IV | 8 | Cup/cone | 6 | 0 | NR | NR | 8 weeks | NR | N |
| Lister (35) | 1978 | IV | 8 | Interosseus + K-wire | 16 | 2 | 9.6 weeks | NR | – | NR | N |
| Martin (36)7 | 1981 | III | 10 | Lag screw | 89 | 9 | 7.1 weeks | NR | NR | NR | Y – 80× superficial infection, six fracture of dorsal cortex, 8× osteomyelitis, two breakage of wire |
| K-wires | 84 | 23 | 9.25 weeks | NR | NR | NR | |||||
| Tension-band | 19 | 1 | 10.3 weeks | NR | NR | NR | |||||
| Interosseus + K-wire | 4 | 0 | 10.7 weeks | NR | NR | NR | |||||
| Plate | 1 | 0 | 6.2 weeks | NR | NR | NR | |||||
| McGlynn et al. (37) | 1988 | IV | 8 | K-wires | 28 | 0 | 6–12 weeks | NR | 11× none, 14× 3–6 weeks, 3× 8–10 weeks | NR | Y – 2× superficial infection |
| Mikolyzk & Stern (38) | 2011 | IV | 7 | Interosseus + Steinmann Pin | 5 | 0 | NR | 1× DII, 3× DII, 1× DV | 6 weeks | NR | N |
| Moberg (39) | 1960 | III | 6 | K-wires | 15 | 1 | NR | NR | NR | NR | NR |
| Bone peg | 50 | 2 | 6 weeks | NR | 6 weeks | NR | |||||
| Netscher & Hamilton (40) | 2012 | IV | 6 | Bone peg + K-wires | 1 | 0 | 6 weeks | 1× DIV | 6 weeks | NR | N |
| Newman et al. (41) | 2018 | IV | 2 | Compression screw | 6 | 0 | NR | NR | NR | NR | N |
| Novoa-Parra et al. (42) | 2018 | IV | 10 | Compression screw | 6 | 0 | 8 weeks | 3× DIV, 3× DV | – | DASH, pain VAS | N |
| Ono et al. (43) | 2019 | IV | 8 | Plate | 1 | 1 | 8 weeks | 1× DII | NR | ROM, Grip | N |
| Pellegrini & Burton (44) | 1990 | IV | 7 | K-wires | 10 | 1 | NR | 5× DII, 2× DIII, 3× DIV | NR | Grip, pinch | N |
| Pfeiffer & Nigst (45) | 1970 | IV | 6 | Lag screw | 7 | 0 | 6 weeks | NR | – | NR | N |
| Popova & Yankov (46) | 1980 | IV | 6 | Staples | 10 | 0 | 6–8 weeks | NR | 4 weeks | NR | N |
| Pribyl et al. (47) | 1996 | IV | 9 | K-wires | 39 | 0 | 9 weeks | 9× DII, 6× DIII, 14× DIV, 10× DV | 8 weeks | NR | Y – 2× superficial infection, 1× mal-union |
| Prokes & Lutonsky (48) | 2005 | IV | 7 | External fixation | 9 | 0 | 6.7 weeks | NR | – | NR | N |
| Reill & Renne (49) | 1973 | IV | 5 | Lag screw | 20 | 0 | NR | NR | NR | NR | N |
| Robertson (50) | 1964 | IV | 2 | Interosseus wiring | 11 | 0 | NR | NR | 6 | NR | N |
| Sabbagh et al. (51) | 2001 | IV | 10 | Harrison–Nicolle peg | 20 | 1 | NR | NR | 2 weeks | NR | Y – 1× superficial infection, 1× deep infection |
| Sanderson et al. (52) | 1991 | IV | 9 | Harrison–Nicolle peg | 36 | 2 | NR | NR | 2 weeks | NR | N |
| Savvidou & Kutz (53) | 2013 | IV | 12 | X-Fuse | 2 | 0 | 8–12 weeks | 2× DV | 3 weeks | DASH | N |
| Seitz et al. (54) | 1994 | IV | 8 | External fixation | 7 | 0 | 4–6 weeks | NR | – | NR | N |
| Stahl & Rozen (55)7 | 2001 | IV | 9 | Tension-band | 41 | 0 | 7–14 weeks | 12× DII, 10× DIII, 8× DIV, 11× DV | 4–6 days | NR | Y – 2× superficial infection, 3× pain |
| Strzyzewski et al. (56) | 1971 | IV | 7 | External fixation | 10 | 0 | NR | NR | 6 weeks | NR | N |
| Tan et al. (57) | 2017 | III | 12 | Interosseus + K-wire | 2 | 1 | 12 weeks | 1× DIV, 1× DV | 1 weeks | ROM, DASH | NR |
| Lag screw | 1 | 0 | 13 weeks | 1× DIV | 1 weeks | ||||||
| Taylor & Spencer (58) | 1994 | IV | 8 | Harrison–Nicolle peg | 9 | 3 | NR | 2× DII, 2× DIII, 3× DIV, 2× DV | NR | NR | Y – 1× mal-union |
| Teoh et al. (59) | 1994 | IV | 8 | Lag screw | 9 | 0 | 8.2 weeks | 2× DII, 1× DIII, 2× DIV, 4× DV | – | NR | N |
| Uhl & Schneider (60) | 1992 | IV | 8 | Tension-band | 32 | 1 | 12 weeks | 3× DII, 6× DIII, 10× DIV, 13× DV | 1 week | NR | Y – 1× infection |
| Vitale et al. (61)4,8 | 2015 | III | 10 | Tension-band | 9 | 1 | NR | NR | NR | Grip, pinch, pain VAS, MHOQ | Y – 1× pain, 1× tendon adhesion |
| Plate | 3 | 0 | NR | NR | NR | ||||||
| Compression screw | 2 | 0 | NR | NR | NR | ||||||
| Reference | Year | LoE | MINORS score | Technique | Arthrodeses, n | Non-union, n | Consolidation (t) | Finger | IMM (t) | PROM (type, data) | Complications (Y/N) |
| Vorderwinkler et al. (62)4 | 2011 | III | 8 | Tension-band | 6 | 0 | NR | NR | NR | NR | N |
| External fixation | 1 | 0 | NR | NR | NR | NR | N | ||||
| Wexler et al. (63) | 1977 | IV | 8 | External fixation | 31 | 2 | 4–6 weeks | NR | 1 week | NR | Y – 5× infection |
| Wright & McMurtry (64) | 1983 | IV | 10 | Plate | 35 | 0 | 6 weeks | NR | – | NR | N |
| Wuestner et al. (65) | 1986 | IV | 6 | PDS peg | 2 | 0 | 6 weeks | 1× DII, 1× DIV | 2–3 weeks | NR | NR |
| Zolotov (66) | 2004 | IV | 6 | Tension-band | 6 | 0 | NR | 1× DII, 1× DIII, 2× DIV, 2× DV | 2–3 weeks | NR | N |
| Indication rheumatoid inflammatory diseases | |||||||||||
| Belsky et al. (67)9 | 1982 | IV | 7 | K-wires | 50 | 0 | NR | NR | NR | NR | N |
| Bracey et al. (68)10 | 1980 | IV | 12 | Plate | 24 | 0 | NR | NR | – | NR | N |
| Gilbart et al. (69)11 | 2004 | IV | 13 | Tension-band | 13 | 0 | NR | 1× DII, 3× DIII, 4× DIV, 5× DV | NR | NR | Y – 3× local irritation |
| Granowitz & Vainio (70)10 | 1966 | IV | 9 | K-wires | 122 | 8 | 6 weeks | 19× DII, 29× DIII, 43× DIV, 31× DV | – | NR | Y – 3× infection |
| Jones et al. (71)11 | 1987 | IV | 10 | Interosseus + K-wire | 53 | 3 | 6–8 weeks | NR | 6 weeks | NR | N |
| Lipscomb et al. (72)11 | 1969 | IV | 6 | K-wires | 16 | 0 | 5–8 weeks | 3× DII, 4× DIII, 4× DIV, 5× DV | NR | NR | Y – 5× superficial infection |
1 1x only Kwire; 2Unclear description of complications, might have occurred ad thumb; 31x additional Kwires; 4Personal communication with author; 5Non-union not differentiated between PIP- and other arthrodesis as well as techniques; 6Non-union and complication not differentiated between PIP- and other arthrodeses; 7Complications not differentiated between PIP- and other arthrodesis; 8Complications not differentiated between different methods; 9Psoriac arthritis; 10Rheumatoid arthritis; 11Systematic sclerosis.
DASH, disabilities of Arm, Shoulder and Hand Questionnaire; DII, index finger; DIII, long finger; DIV, ring finger; DV, little finger; IMM, immobilization; LoE, level of evidence; MHOQ, Michigan Hand Outcomes Questionnaire; nr, not reported; PROM, patient-reported outcome measure; PS, palm spacing; ROM, range of movement; TAM, total active movement; VAS, visual analogue scale.
Data extraction
Data were extracted from the included studies by two authors independently (MM and HV) according to a predefined data extraction sheet. The level of evidence, quality and risk of bias assessed with the standardized critical appraisal instrument, Methodological Index for Non-Randomized Studies (MINORS) score, where applicable, were recorded (8). The methodological quality score MINORS shows a mean of 8 with a global ideal score of 16. Fifty-five articles had level IV evidence, and nine articles had level III evidence. Nearly all studies were retrospective data analysis. We extracted the number of PIP joint arthrodesis, the technique used, time of immobilization, number of non-unions, time to radiological consolidation, and the incidence and type of complications. All patients regardless of their age with arthrodesis were included in this review.
Results
Included studies
A total of 1923 arthrodeses of the PIP joint could be extracted from the included papers (Table 2). The main indications for the arthrodesis of the PIP joint were primary or secondary osteoarthritis, joint infection or traumatic destruction. Included are six studies that consisted only of patients with rheumatic disease, for example rheumatoid arthritis or systemic sclerosis. These results are presented separately in Table 2.
Surgical techniques
Twelve different surgical techniques were described. Four of these techniques with compression at the arthrodesis site: interosseus wiring with/without K-wire, tension-band, cannulated screw as well as a lag screw – combined a total of 805 arthrodeses. The plate, external fixation and K-wire might hold some applied compression during the arthrodesis but do not hold any compression potential themselves. The most frequently used techniques were, with the number of arthrodesis in descending order, K-wires (n = 743, 14 studies), tension-band (n = 313, 15 studies) and compression screws (n = 233, 12 studies). The included studies cover a time span of 74 years of publication, and that there is an obvious trend towards techniques with compression of the arthrodesis, especially with compression screws.
Non-unions and mean consolidation times
Non-unions were reported in all studies. Two studies included other finger joints besides the PIP and did not report the exact numbers of non-unions concerning the fused joint. In these cases, the studies were only included for the consolidation time, for they reported that explicitly. The lowest non-union rate in compression techniques was 3.9% with the compression screw. Interestingly, the non-union rate for the peg fixations (without compression) was even lower 3.6%. The highest non-union rate showed the interosseous wiring with 8.6% (Table 3).
Table 3.
Amount of non-union joint arthrodeses because of osteoarthritis by technique – only studies which described the number of non-unions of the PIP joint with respective technique were included.
| Technique | Studies (n) | Individuals (n) | Non-union (n(%)) |
|---|---|---|---|
| Tension-band | 14 | 293 | 12 (4.1) |
| K-wires | 13 | 735 | 64 (8.7) |
| Compression screw | 12 | 282 | 11 (3.9) |
| Interosseus wiring | 8 | 105 | 9 (8.6) |
| Pin fixation | 9 | 102 | 6 (5.9) |
| Peg fixation | 8 | 165 | 6 (3.6) |
| Plate | 6 | 93 | 4 (4.3) |
| Total | 70 | 1775 | 112 (6.3) |
Table 4 depicts the mean consolidation times. Further information on how non-uniions were stratified by technique is presented in the Supplementary information and the results are presented in supplementary figures 1 and 2.
Table 4.
Consolidation time by technique – only studies included with joints affected by osteoarthritis. The table depicts the consolidation times (mean ± s.d.) in weeks. Again, there were no statistically significant differences between any analyzed technique in comparison to K-wires. Also, we made a comparison of compression vs non-compression techniques of the mean consolidation time, without statistically significant difference (P = 0.830).
| Technique | Studies (n) | Individuals (n) | Consolidation times (weeks) |
|---|---|---|---|
| Tension-band | 10 | 263 | 9.5 ± 2.2 |
| K-wires | 11 | 668 | 8.6 ± 1.5 |
| Compression screw | 9 | 255 | 7.7 ± 1.3 |
| Interosseus wiring | 7 | 187 | 8.5 ± 2.4 |
| Pin fixation | 7 | 82 | 6.9 ± 1.7 |
| Peg fixation | 3 | 63 | 7.3 ± 2.3 |
| Plate | 3 | 64 | 9.2 ± 3.0 |
| Total | 50 | 1582 | 8.2 ± 2.0 |
Complications
Four studies did not describe complications. All others either stated that they had no complications or did not describe them in detail. Most complications besides the non-unions were infections (mostly superficial), pain caused by the implant or mal-unions. The consequences of these complications, that is, if revisionary surgery had to be performed or if superficial infections could be treated by antibiotics, were not reported.
Discussion
A wide range of different surgical techniques for achieving fusion of the PIP joint have been published. Moberg already stated in 1960 that ‘the prime requisite of a good digital arthrodesis is a painless and stable union in proper position occurring in a reasonable space of time’ (39). Nevertheless, a proper comparison, although needed, proves to be difficult because of the variable quality of published studies, different indications for joint fusion, varying definitions of consolidation (radiological vs clinical) as well as lacking important data in large but older studies, where a personal communication with the author is no longer possible (73).
The two main groups of joint fusion techniques which can be differentiated, are techniques with and without compression of the arthrodesis site respectively (6). The most important advantage of the compression is the assumed shorter consolidation time because of higher primary stability, consolidation by primam intentionem with fewer non-unions as well as early functional occupational therapy (60, 64). In this systematic review, the assumption that techniques with compression are more reliable, as demonstrated by Leibovic in 1994, could not be clearly proven (32). One possible reason might be that the compression techniques are surgically more difficult and might tend to non-union if there are no ideal operative results. For example, there is the possibility that a tension-band fusion does not apply the compression to the whole arthrodesis site and therefore renders it unstable. The compression screw however might be easier and more forgiving to implant than tension-band or intraosseus wiring. That might be the reason why the superiority of this implant in contrast to K-wires is evident in different studies in the literature (32, 36).
Nevertheless, in the studies included in this systematic review, there is a trend towards techniques with compression over the course of time, especially towards compression screws (41, 42). With further development of the implants, the diameter of the screws got progressively smaller, as 8 mm diameter screws are commercially available now. Thus, these days they can be used in small bones too.
Newer implants like the Apex IP fusion device so far lack any evidence that they are easier to implant or provide a better outcome, maybe because they have not been available in the market long enough (42).
The most reported complications besides the primary outcome of non-unions were infection, mostly superficial. As there is typically very little soft tissue around the PIP joint, protruding implants, like a tension-band, can cause irritation and subsequently a superficial infection. This emphasizes the need for a proper handling of soft tissues (36).
Rheumatoid arthritis and connective tissue diseases
Rheumatoid inflammatory diseases commonly affect the joint, especially the PIP joint, which may lead to contractures and deviations that are both disabling as well as cosmetically unacceptable (74). These diseases could affect the quality of the bones and therefore the stability of arthrodeses as well as the healing of soft tissues. The referenced papers by Gilbart et al. (69), Jones et al. (71)and Lipscomb et al. (72) relate to patients with systemic sclerosis. From a pragmatic point of view, one might state that if something works for this challenging group of patients it will probably work for a patient with osteoarthritis. Interestingly and somewhat counterintuitively, Lipscomb et al. (72) found quicker healing compared to other studies dealing with posttraumatic osteoarthritis.
Biomechanical properties and primary stability
The primary stability of different fusion techniques or implants could provide an interesting insight into the ability of the implant itself to withstand the forces of early function therapy as well as a short or even no immobilization. There are only few papers that have tried to compare the results of different biomechanical studies (75, 76). Therefore, it seems reasonable to conduct a biomechanical study for comparing the different implants and techniques of interphalangeal arthrodesis so that postsurgical treatment can be standardized.
Strengths and limitations
There are several limitations of the existing literature as well as of this study. In order to do a reasonable meta-analysis and statistical evaluation of the different techniques, randomized controlled trials (RCT) are required. On the topic of arthrodesis of the PIP joint, there is no RCT published at all. Therefore, we did a qualitative systematic review with only descriptive data pooling of the different studies with respect to their published technique for greater clearness instead of a meta-analysis. Another limitation is that the literature review for this systematic review showed that there are predominantly studies with an evidence level IV, with a heterogenous MINORS score but a satisfying mean of 8. As the risk of bias as depicted in the MINORS score exists, one might suspect that the published technique makes the apparent effect appear better than it is. There were nine evidence level III studies which could be included. Nevertheless, these results imply a lack of good quality data to statistically compare the different techniques and to achieve recommendations.
Especially the complications of different techniques, which we extracted from the studies, were reported very heterogeneously with no clear evidence on how to avoid them or of their consequences.
Strengths of this systematic review is its novelty and uniqueness, since there are no systematic reviews with a high quality, like PRISMA methodology. It includes a very long-time span of nearly 74 years and covers the most extensive databases. A very large number of abstracts were screened to achieve the most complete systematic review.
Conclusion
The compression screw shows superior results with respect to non-unions in comparison to K-wires. There is a tendency of more published techniques with compression in the last 10 years which might implicate a shift towards compression techniques. Given the limited evidence of the available studies on arthrodesis of the PIP joint, there is a lack of clear indications for other special techniques. The three most often used techniques are K-wires, tension-band and compression screws. The K-wires still have their place in acute trauma with soft tissue defects or replantation. Only large multi-center RCTs can answer the question on which technique for arthrodesis of the PIP joint is the best.
Supplementary Material
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the work reported here.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author contribution statement
H-C Vonderlind and M Ruettermann: both authors contributed equally to this manuscript.
Acknowledgements
The authors would like to thank Stefanie Karpik for her support in preparing and correcting the manuscript with respect to spelling and grammar.
References
- 1.Murray PM.Treatment of the osteoarthritic hand and thumb. In Green’s Operative Hand Surgery, 7th ed., pp. 345–372. Eds Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS. Philadelphia: Elsevier Inc., 2017. [Google Scholar]
- 2.Herren D.The proximal interphalangeal joint: arthritis and deformity. EFORT Open Reviews 20194254–262. ( 10.1302/2058-5241.4.180042) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schindele SF, Hensler S, Audigé L, Marks M, Herren DB. A modular surface gliding implant (CapFlex-PIP) for proximal interphalangeal joint osteoarthritis: a prospective case series. Journal of Hand Surgery 201540334–340. ( 10.1016/j.jhsa.2014.10.047) [DOI] [PubMed] [Google Scholar]
- 4.Reischenboeck V, Marks M, Herren DB, Schindele S. Surface replacing arthroplasty of the proximal interphalangeal joint using the CapFlex-PIP implant: a prospective study with 5-year outcomes. Journal of Hand Surgery, European Volume 202146496–503. ( 10.1177/1753193420977244) [DOI] [PubMed] [Google Scholar]
- 5.Boeckstyns MEH.My personal experience with arthroplasties in the hand and wrist over the past four decades. Journal of Hand Surgery, European Volume 201944129–137. ( 10.1177/1753193418817172) [DOI] [PubMed] [Google Scholar]
- 6.Jones BF, Stern PJ. Interphalangeal joint arthrodesis. Hand Clinics 199410267–275. ( 10.1016/S0749-0712(2101289-0) [DOI] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG. & PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal of Surgery 20108336–341. ( 10.1016/j.ijsu.2010.02.007) [DOI] [PubMed] [Google Scholar]
- 8.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ Journal of Surgery 200373712–716. ( 10.1046/j.1445-2197.2003.02748.x) [DOI] [PubMed] [Google Scholar]
- 9.Al-Qattan MM.Pollicization of the index finger requiring secondary fusion of the new metacarpophalangeal joint. Journal of Hand Surgery, European Volume 201641295–300. ( 10.1177/1753193415587242) [DOI] [PubMed] [Google Scholar]
- 10.Allende BT, Engelem JC. Tension-band arthrodesis in the finger joints. Journal of Hand Surgery 19805269–271. ( 10.1016/s0363-5023(8080012-8) [DOI] [PubMed] [Google Scholar]
- 11.Arata J, Ishikawa K, Sawabe K, Soeda H, Kitayama T. Osteosynthesis in digital replantation using bioabsorbable rods. Annals of Plastic Surgery 200350350–353. ( 10.1097/01.SAP.0000041482.24205.D7) [DOI] [PubMed] [Google Scholar]
- 12.Ayres JR, Goldstrohm GL, Miller GJ, Dell PC. Proximal interphalangeal joint arthrodesis with the Herbert screw. Journal of Hand Surgery 198813600–603. ( 10.1016/s0363-5023(8880105-9) [DOI] [PubMed] [Google Scholar]
- 13.Bansky R, Racz N. The use of titanium miniplates in arthrodesis of the interphalangeal joints and a metacarpal neck fracture. Bratislavske Lekarske Listy 2005106287–290. [PubMed] [Google Scholar]
- 14.Baruch A, Kahanovich S. Angulated bone peg. Plastic and Reconstructive Surgery 198066471–473. ( 10.1097/00006534-198066030-00033) [DOI] [PubMed] [Google Scholar]
- 15.Biskop M, Neumann HW. Tension-wire arthrodesis of the proximal interphalangeal joint in chronic polyarthritis. Beiträge zur Orthopadie und Traumatologie 19853222–25. [PubMed] [Google Scholar]
- 16.Breyer JM, Vergara P, Parra L, Sotelo P, Bifani A, Andrade F. Metacarpophalangeal and interphalangeal joint arthrodesis: a comparative study between tension band and compression screw fixation. Journal of Hand Surgery, European Volume 201540374–378. ( 10.1177/1753193413514362) [DOI] [PubMed] [Google Scholar]
- 17.Buechler U, Aiken MA. Arthrodesis of the proximal interphalangeal joint by solid bone grafting and plate fixation in extensive injuries to the dorsal aspect of the finger. Journal of Hand Surgery 198813589–594. ( 10.1016/s0363-5023(8880103-5) [DOI] [PubMed] [Google Scholar]
- 18.Buck-Gramcko D, Oehme S. Finger joint arthrodeses with intraosseous wire suture and Kirschner wire. A comparative study of 309 operations. Handchirurgie, Mikrochirurgie, Plastische Chirurgie 19882099–106. [PubMed] [Google Scholar]
- 19.Burton RI, Margles SW, Lunseth PA. Small-joint arthrodesis in the hand. Journal of Hand Surgery 198611678–682. ( 10.1016/s0363-5023(8680011-9) [DOI] [PubMed] [Google Scholar]
- 20.Carroll RE, Hill NA. Small joint arthrodesis in hand reconstruction. Journal of Bone and Joint Surgery: American Volume 1969511219–1221. ( 10.2106/00004623-196951060-00020) [DOI] [PubMed] [Google Scholar]
- 21.Faithfull DK, Herbert TJ. Small joint fusions of the hand using the Herbert Bone Screw. Journal of Hand Surgery 19849167–168. ( 10.1016/S0266-7681(8480021-2) [DOI] [PubMed] [Google Scholar]
- 22.Goth D, Konigsberger H. Arthrodesis of finger joints using the Lagscrew principle. Operative Orthopädie und Traumatologie 19968118–128. ( 10.1007/BF02512776) [DOI] [Google Scholar]
- 23.Harrison SH, Nicolle FV. A new intramedullary bone peg for digital arthrodesis. British Journal of Plastic Surgery 197427240–241. ( 10.1016/s0007-1226(7490081-2) [DOI] [PubMed] [Google Scholar]
- 24.Herzog KH.Indication and technic of finger arthrodesis. Langenbecks Archiv fur Klinische Chirurgie Vereinigt mit Deutsche Zeitschrift Fur Chirurgie 1961297172–178. [PubMed] [Google Scholar]
- 25.Hoffmann P, Rossak K. 2 Kirschner wires as simplified external fixation devices in finger joint arthrosis. Handchirurgie 1975791–93. [PubMed] [Google Scholar]
- 26.Høgh J, Jensen PO. Compression-arthrodesis of finger joints using Kirschner wires and cerclage. Hand 198214149–152. ( 10.1016/s0072-968x(8280006-5) [DOI] [PubMed] [Google Scholar]
- 27.Hohendorff B, Franke J, Spies CK, Mueller LP, Ries C. Arthrodesis of the proximal interphalangeal joint of fingers with tension band wire. Operative Orthopädie und Traumatologie 201729385–394. ( 10.1007/s00064-016-0471-7) [DOI] [PubMed] [Google Scholar]
- 28.Jones Jr DB, Ackerman DB, Sammer DM, Rizzo M. Arthrodesis as a salvage for failed proximal interphalangeal joint arthroplasty. Journal of Hand Surgery 201136259–264. ( 10.1016/j.jhsa.2010.10.030) [DOI] [PubMed] [Google Scholar]
- 29.Khuri SM.Tension band arthrodesis in the hand. Journal of Hand Surgery 19861141–45. ( 10.1016/s0363-5023(8680099-5) [DOI] [PubMed] [Google Scholar]
- 30.Kowalski MF, Manske PR. Arthrodesis of digital joints in children. Journal of Hand Surgery 198813874–879. ( 10.1016/0363-5023(8890263-8) [DOI] [PubMed] [Google Scholar]
- 31.Kvasnička J.Arthrodesis of interphalangeal joints of the hand by an external fixator in managing conditions resulting from septic arthritis. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 201986358–361. [PubMed] [Google Scholar]
- 32.Leibovic SJ, Strickland JW. Arthrodesis of the proximal interphalangeal joint of the finger: comparison of the use of the Herbert screw with other fixation methods. Journal of Hand Surgery 199419181–188. ( 10.1016/0363-5023(9490002-7) [DOI] [PubMed] [Google Scholar]
- 33.Leonard MH, Capen DA. Compression arthrodesis of finger joints. Clinical Orthopaedics and Related Research 1979145193–198. ( 10.1097/00003086-197911000-00029) [DOI] [PubMed] [Google Scholar]
- 34.Lewis RC, Nordyke MD, Tenny JR. The tenon method of small joint arthrodesis in the hand. Journal of Hand Surgery 198611567–569. ( 10.1016/s0363-5023(8680201-5) [DOI] [PubMed] [Google Scholar]
- 35.Lister G.Intraosseous wiring of the digital skeleton. Journal of Hand Surgery 19783427–435. ( 10.1016/s0363-5023(7880135-x) [DOI] [PubMed] [Google Scholar]
- 36.Martin L.Arthrodeses of the thumb and long finger joints. Handchirurgie 198113221–230. [PubMed] [Google Scholar]
- 37.McGlynn JT, Smith RA, Bogumill GP. Arthrodesis of small joint of the hand: a rapid and effective technique. Journal of Hand Surgery 198813595–599. ( 10.1016/s0363-5023(8880104-7) [DOI] [PubMed] [Google Scholar]
- 38.Mikolyzk DK, Stern PJ. Steinmann pin arthrodesis for salvage of failed small joint arthroplasty. Journal of Hand Surgery 2011361383–1387. ( 10.1016/j.jhsa.2011.05.027) [DOI] [PubMed] [Google Scholar]
- 39.Moberg E.Arthrodesis of finger joints. Surgical Clinics of North America 196040465–470. ( 10.1016/s0039-6109(1636053-4) [DOI] [PubMed] [Google Scholar]
- 40.Netscher DT, Hamilton KL. Interphalangeal joint salvage arthrodesis using the lister tubercle as bone graft. Journal of Hand Surgery 2012372145–2149. ( 10.1016/j.jhsa.2012.05.043) [DOI] [PubMed] [Google Scholar]
- 41.Newman EA, Orbay MC, Nunez Jr FA, Nunez Sr F. Minimally invasive proximal interphalangeal joint arthrodesis using headless screw: surgical technique. Techniques in Hand and Upper Extremity Surgery 20182239–42. ( 10.1097/BTH.0000000000000189) [DOI] [PubMed] [Google Scholar]
- 42.Novoa-Parra CD, Montaner-Alonso D, Pérez-Correa JI, Morales-Rodríguez J, Rodrigo-Pérez JL, Morales-Suarez-Varela M. Arthrodesis of the proximal interphalangeal joint of the 4th and 5th finger using an interlocking screw device to treat severe recurrence of Dupuytren’s disease. Revista Espanola de Cirugia Ortopedica y Traumatologia 201862216–221. ( 10.1016/j.recot.2017.10.012) [DOI] [PubMed] [Google Scholar]
- 43.Ono R, Komura S, Hirakawa A, Hirose H, Tsugita M, Masuda T, Ito Y, Akiyama H. Staged arthrodesis using the Masquelet technique for osteomyelitis of the finger with articular destruction: a report of two cases. Archives of Orthopaedic and Trauma Surgery 20191391025–1031. ( 10.1007/s00402-019-03197-5) [DOI] [PubMed] [Google Scholar]
- 44.Pellegrini Jr VD, Burton RI. Osteoarthritis of the proximal interphalangeal joint of the hand: arthroplasty or fusion? Journal of Hand Surgery 199015194–209. ( 10.1016/0363-5023(9090096-a) [DOI] [PubMed] [Google Scholar]
- 45.Pfeiffer KM, Nigst H. Finger joint arthrodesis with surgical screws. Handchirurgie 19702149–151. [PubMed] [Google Scholar]
- 46.Popova B, Yankov E. Arthrodesis of the interphalangeal joints of fingers using an inverted U-shaped staple. Ortopediya i Travmatologiya 19801760–66. [Google Scholar]
- 47.Pribyl CR, Omer GE, McGinty L. Effectiveness of the chevron arthrodesis in small joints of the hand. Journal of Hand Surgery 1996211052–1058. ( 10.1016/S0363-5023(9680315-7) [DOI] [PubMed] [Google Scholar]
- 48.Prokes L, Lutonský M. Arthrodesis of interphalangeal joints by means of external frame fixation. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 200572111–115. [PubMed] [Google Scholar]
- 49.Reill P, Renné J. Indication and technic of finger joint arthrodesis for middle and distal joints using the AO-screw. Zeitschrift fur Orthopadie und Ihre Grenzgebiete 1973111475–478. [PubMed] [Google Scholar]
- 50.Robertson DC.The fusion of interphalangeal joints. Canadian Journal of Surgery 19647433–437. [PubMed] [Google Scholar]
- 51.Sabbagh W, Grobbelaar AO, Clarke C, Smith PJ, Harrison DH. Long-term results of digital arthrodesis with the Harrison-Nicolle peg. Journal of Hand Surgery 200126568–571. ( 10.1054/jhsb.2001.0649) [DOI] [PubMed] [Google Scholar]
- 52.Sanderson PL, Morris MA, Fahmy NR. A long-term review of the Harrison-Nicolle peg in digital arthrodesis. Journal of Hand Surgery 199116283–285. ( 10.1016/0266-7681(9190055-s) [DOI] [PubMed] [Google Scholar]
- 53.Savvidou C, Kutz J. Interphalangeal and thumb metacarpophalangeal arthrodesis with an intramedullary implant. Annals of Plastic Surgery 20137034–37. ( 10.1097/SAP.0b013e31821d0757) [DOI] [PubMed] [Google Scholar]
- 54.Seitz Jr WH, Sellman DC, Scarcella JB, Froimson AI. Compression arthrodesis of the small joints of the hand. Clinical Orthopaedics and Related Research 1994304116–121. ( 10.1097/00003086-199407000-00019) [DOI] [PubMed] [Google Scholar]
- 55.Stahl S, Rozen N. Tension-band arthrodesis of the small joints of the hand. Orthopedics 200124981–983. ( 10.3928/0147-7447-20011001-19) [DOI] [PubMed] [Google Scholar]
- 56.Strzyzewski H, Woźny W, Jurczyk A. Value of compression arthrodesis of finger joints. Chirurgia Narzadow Ruchu i Ortopedia Polska 197136741–745. [PubMed] [Google Scholar]
- 57.Tan M, Ho SWL, Sechachalam S. Acute arthrodesis of interphalangeal joints of the hand in traumatic injuries. Journal of Hand and Microsurgery 2018101–5. ( 10.1055/s-0037-1608691) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Taylor MF, Spencer JD. Complications of the use of the Harrison-Nicolle intramedullary Peg in digital arthrodesis. Journal of Hand Surgery 199419205–207. ( 10.1016/0266-7681(9490167-8) [DOI] [PubMed] [Google Scholar]
- 59.Teoh LC, Yeo SJ, Singh I. Interphalangeal joint arthrodesis with oblique placement of an AO lag screw. Journal of Hand Surgery 199419208–211. ( 10.1016/0266-7681(9490168-6) [DOI] [PubMed] [Google Scholar]
- 60.Uhl RL, Schneider LH. Tension band arthrodesis of finger joints: a retrospective review of 76 consecutive cases. Journal of Hand Surgery 199217518–522. ( 10.1016/0363-5023(9290365-v) [DOI] [PubMed] [Google Scholar]
- 61.Vitale MA, Fruth KM, Rizzo M, Moran SL, Kakar S. Prosthetic arthroplasty versus arthrodesis for osteoarthritis and posttraumatic arthritis of the index finger proximal interphalangeal joint. Journal of Hand Surgery 2015401937–1948. ( 10.1016/j.jhsa.2015.05.021) [DOI] [PubMed] [Google Scholar]
- 62.Vorderwinkler KP, Muehldorfer M, Pillukat T, van Schoonhoven J. Treatment of bacterial infection in the interphalangeal joints of the hand. Operative Orthopädie und Traumatologie 201123192–203. ( 10.1007/s00064-011-0024-z) [DOI] [PubMed] [Google Scholar]
- 63.Wexler MR, Rousso M, Weinberg H. Arthrodesis of finger joints by dynamic external compression using dorsoventral Kirschner wires and rubber bands. Plastic and Reconstructive Surgery 197760882–885. ( 10.1097/00006534-197712000-00006) [DOI] [PubMed] [Google Scholar]
- 64.Wright CS, McMurtry RY. AO arthrodesis in the hand. Journal of Hand Surgery 19838932–935. ( 10.1016/s0363-5023(8380099-9) [DOI] [PubMed] [Google Scholar]
- 65.Wuestner MC, Partecke BD, Buck-Gramcko D. Resorbable PDS splints in fracture stabilization and for arthrodeses of the hand. Handchirurgie, Mikrochirurgie, Plastische Chirurgie 198618298–301. [PubMed] [Google Scholar]
- 66.Zolotov AS.Finger joint fusion with the aid of an aluminum template. Techniques in Hand and Upper Extremity Surgery 20048193–196. ( 10.1097/01.bth.0000134707.51560.cc) [DOI] [PubMed] [Google Scholar]
- 67.Belsky MR, Feldon P, Millender LH, Nalebuff EA, Phillips C. Hand involvement in psoriatic arthritis. Journal of Hand Surgery 19827203–207. ( 10.1016/s0363-5023(8280090-7) [DOI] [PubMed] [Google Scholar]
- 68.Bracey DJ, McMurtry RY, Walton D. Arthrodesis in the rheumatoid hand using the AO technique. Orthopedic Reviews 1980965–69. [Google Scholar]
- 69.Gilbart MK, Jolles BM, Lee P, Bogoch ER. Surgery of the hand in severe systemic sclerosis. Journal of Hand Surgery 200429599–603. ( 10.1016/j.jhsb.2004.03.013) [DOI] [PubMed] [Google Scholar]
- 70.Granowitz S, Vainio K. Proximal interphalangeal joint arthrodesis in rheumatoid arthritis. A follow-up study of 122 operations. Acta Orthopaedica Scandinavica 196637301–310. ( 10.3109/17453676608989418) [DOI] [PubMed] [Google Scholar]
- 71.Jones NF, Imbriglia JE, Steen VD, Medsger TA. Surgery for scleroderma of the hand. Journal of Hand Surgery 198712391–400. ( 10.1016/s0363-5023(8780012-6) [DOI] [PubMed] [Google Scholar]
- 72.Lipscomb PR, Simons GW, Winkelmann RK. Surgery for sclerodactylia of the hand. Experience with six cases. Journal of Bone and Joint Surgery: American Volume 1969511112–1117. ( 10.2106/00004623-196951060-00006) [DOI] [PubMed] [Google Scholar]
- 73.Vonderlind HC, Eisenschenk A, Juergensen I, Kim S, Millrose M. Arthrodesis of the proximal interphalangeal joint – a review. Handchirurgie, Mikrochirurgie, Plastische Chirurgie 2019516–18. ( 10.1055/a-0833-8729) [DOI] [PubMed] [Google Scholar]
- 74.Nalebuff EA.Surgery in patients with systemic sclerosis of the hand. Clinical Orthopaedics and Related Research 199936691–97. ( 10.1097/00003086-199909000-00012) [DOI] [PubMed] [Google Scholar]
- 75.Vonderlind HC, Zach A, Eichenauer F, Kim S, Eisenschenk A, Millrose M. Proximal interphalangeal joint arthrodesis using a compression wire: a comparative biomechanical study. Hand Surgery and Rehabilitation 201938307–311. ( 10.1016/j.hansur.2019.07.002) [DOI] [PubMed] [Google Scholar]
- 76.Millrose M, Zach A, Kim S, Güthoff C, Eisenschenk A, Vonderlind HC. Biomechanical comparison of the proximal interphalangeal joint arthrodesis using a compression wire. Archives of Orthopaedic and Trauma Surgery 2019139577–581. ( 10.1007/s00402-019-03119-5) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 This work is licensed under a
This work is licensed under a