Abstract
Background
Acceptance of the role of the fallopian tube in ‘ovarian’ carcinogenesis and the detrimental sequelae of surgical menopause in premenopausal women following risk-reducing salpingo-oophorectomy (RRSO) has resulted in risk-reducing early-salpingectomy with delayed oophorectomy (RRESDO) being proposed as an attractive alternative risk-reducing strategy in women who decline/delay oophorectomy. We present the results of a qualitative study evaluating the decision-making process among BRCA carriers considering prophylactic surgeries (RRSO/RRESDO) as part of the multicentre PROTECTOR trial (ISRCTN:25173360).
Methods
In-depth semistructured 1:1 interviews conducted using a predeveloped topic-guide (development informed by literature review and expert consultation) until informational saturation reached. Wording and sequencing of questions were left open with probes used to elicit additional information. All interviews were audio-recorded, transcribed verbatim, transcripts analysed using an inductive theoretical framework and data managed using NVIVO-v12.
Results
Informational saturation was reached following 24 interviews. Seven interconnected themes integral to surgical decision making were identified: fertility/menopause/cancer risk reduction/surgical choices/surgical complications/sequence of ovarian-and-breast prophylactic surgeries/support/satisfaction. Women for whom maximising ovarian cancer risk reduction was relatively more important than early menopause/quality-of-life preferred RRSO, whereas those more concerned about detrimental impact of menopause chose RRESDO. Women managed in specialist familial cancer clinic settings compared with non-specialist settings felt they received better quality care, improved hormone replacement therapy access and were more satisfied.
Conclusion
Multiple contextual factors (medical, physical, psychological, social) influence timing of risk-reducing surgeries. RRESDO offers women delaying/declining premenopausal oophorectomy, particularly those concerned about menopausal effects, a degree of ovarian cancer risk reduction while avoiding early menopause. Care of high-risk women should be centralised to centres with specialist familial gynaecological cancer risk management services to provide a better-quality, streamlined, holistic multidisciplinary approach.
Keywords: surgical oncology, gynecology, genetics
Introduction
BRCA1/BRCA2 mutation carriers have a ~70% lifetime risk of breast cancer (BC) and ~17%–44% lifetime risk of ovarian cancer (OC).1 RAD51C/RAD51D/BRIP1/PALB2 are newer moderate penetrance OC genes, whose risks were recently validated (5%–13% lifetime cumulative OC risk) with RAD51C/RAD51D/PALB2 also associated with increased BC risk (20%–53%).2 3 BC risk management options include annual (eg, MRI) breast screening;4 chemoprevention (eg, Tamoxifen/Anastrazole))5 6 and surgical prevention (risk-reducing mastectomy (RRM)).7 Risk-reducing salpingo-oophorectomy (RRSO), usually recommended from 35 to 40 years, is the most effective surgical prevention option for OC-risk reduction, especially given the absence of an effective national (or even approved) high-risk OC-screening programme. However, premenopausal RRSO leads to early surgical menopause which has detrimental long-term health sequelae (increased risk of coronary heart disease, osteoporosis, vasomotor symptoms, sexual dysfunction, neurocognitive decline) particularly in women unable to use hormone replacement therapy (HRT).8–13 Widespread acceptance of a central role for the fallopian tube in the development of high-grade serous carcinoma (HGSC), the most common type of OC has led to early salpingectomy (ES) followed by delayed oophorectomy (DO) proposed as an attractive alternative two-step OC surgical prevention strategy in premenopausal women who have completed their family but decline/wish to delay RRSO. Epidemiological studies show 70% of occult lesions identified in high-risk women undergoing RRSO occur in the tube and that salpingectomy may reduce ovarian cancer risk in low-risk women by 42%–65%. Thus, it is anticipated that risk-reducing early-salpingectomy with delayed oophorectomy (RRESDO) will provide some level of risk reduction while conserving ovarian function to avoid the negative impact of early menopause.
Three trials in the UK (PROTECTOR), Netherlands (TUBA) and US (WISP) are currently offering RRESDO within a controlled research setting. Absence of prospective data strengthens offering RRESDO currently solely within a research setting. The precise estimate of OC risk reduction and the long-term health outcomes associated with ES remain unclear. Salpingectomy will not prevent OC arising outside the tube. Residual fimbrial tissue (most HGSC arise from tubal fimbria) may remain implanted on the ovarian surface postsalpingectomy in 9.8% cases14 and represents a possible site of malignant transformation. The natural history of different types of serous-tubal intraepithelial carcinoma (STIC), the precursor of tubal HGSC and rate-limiting step in OC development remain unknown.15 STICs may not be precursors to all OC.16 The long-term impact of salpingectomy on sexual function, endocrine function and menopause onset is unknown. Concerns remain regarding attrition from DO and uncertainties persist around cost effectiveness.17
There is a paucity of qualitative data on the decision-making process for RRESDO in BRCA carriers.18 Limited data suggest that the seriousness of OC, family history (FH), previous BC, uncertainty around effect of ES and ease of decision to undergo RRSO are barriers to undergoing RRESDO.18 The main facilitator is longer preservation of ovarian function.18 RRESDO appears acceptable particularly to women concerned about sexual dysfunction.19 Barriers to RRSO include early menopause, sexual dysfunction and loss of fertility; facilitators include FH, fear of dying, concurrent benign gynaecological issues, ineffective screening and physician recommendation.18 20–22
Current medical decision making encourages clinicians to respect patients’ preferences and be guided by them for treatment decisions.23 Policy makers and commissioners increasingly use qualitative data to inform guideline development and care pathways, as it enables care provision according to user insights by gaining a better understanding of, and reasons for the choices made. We report on the decision making of high-risk UK women undergoing/considering prophylactic surgery in the PROTECTOR trial (ISRCTN 25173360). This study aims to evaluate the decision-making process among BRCA carriers considering prophylactic surgeries. We offer novel insights for healthcare professionals providing decision support to BRCA carriers and for development of clinical management pathways for these women.
Methods
Study design
Qualitative substudy nested within a multicentre, observational cohort trial (PROTECTOR: Preventing Ovarian Cancer through early Excision of Tubes and late Ovarian Removal, ISRCTN:25173360) with three arms: RRESDO; RRSO; no surgery.24 Premenopausal women (follicle stimulating hormone (FSH) levels<40), >30 years, at increased risk of OC (BRCA1/BRCA2/RAD51C/RAD51D/BRIP1 carriers or due to a strong family history) were recruited to the PROTECTOR trial (www.protector.org.uk) through specialist high-risk familial cancer clinics (FCC), genetics, gynaecology/gynaecological oncology clinics. Exclusion criteria included being postmenopausal, previous bilateral salpingectomy or bilateral oophorectomy, pregnancy, future plan of childbearing (surgical arms only), prior OC/peritoneal malignancy, <12 months from cancer treatment, OC suspicion at baseline. Participants self-selected their chosen study arm following informed counselling.
In-depth semistructured one-to-one telephone interviews were conducted (by FG) using a predeveloped topic-guide (online supplemental material 1). Topic-guide development was informed by a literature review and expert consultation. Wording and sequencing of questions were left open with probes used to elicit more information as appropriate. Questions were refined following a pilot interview, and topics covered included: background (family structure, support network, occupation, hobbies); risk-reducing surgery for OC/BC prevention; health values; satisfaction-and-regret. Following informed consent, interviewees were recruited based on sociodemographics (age, ethnicity, marital status, postcode), parity, BC history, trial arm (RRESDO, RRSO, no surgery) and ascertainment location (high-risk FCC, gynaecology clinic, gynaecological oncology clinic, genetics clinic) to ensure adequate representation across the PROTECTOR cohort. Field notes were made, interviews audio-recorded and transcribed verbatim. Interviews were conducted (before OC prevention surgery) between November 2018 and October 2019 until data saturation was reached.
jmedgenet-2020-107501supp001.pdf (65KB, pdf)
Data analysis
Transcripts were analysed using a grounded-theory approach and data managed using NVIVO V.12 software. The analysis aimed to directly reflect the views and experiences of participants’ and not those predetermined by the researchers. Two researchers (FG, SG) independently coded all transcripts, following a three-step process: open coding, axial coding and selective coding. Meaningful text was labelled starting with a line-by-line analysis (open coding). Open codes were categorised, grouping similar codes, refined and combined into larger themes (axial coding). Through multiple, iterative discussions, we reflected on potential relationships between codes within and across cases and developed an in-depth understanding of themes. Coding disagreements were resolved through discussion with further transcript review until reaching consensus. Transcripts were re-reviewed to ensure themes reflected the data and important ideas/views had not been missed/over-represented. Selective coding involved integrating and refining themes. Analysis was performed in parallel with data collection and finalised once theoretical saturation was reached.
Results
Participant characteristics
Twenty-four women were interviewed, with no interview refusals. Participant characteristics are summarised in table 1. Participants ranged from 34 to 46 years; 22 were Caucasian, 19 married, 4 nulliparous, 4 had previously BC themselves, 9 had undergone RRM, 14 were BRCA1 carriers, 10 BRCA2 carriers, 11 self-selected RRESDO, 7 RRSO and 6 no surgery. Interviews lasted 40–70 (mean=55) min.
Table 1.
Participant characteristics
| ID | Study arm | Age (years) | Ethnicity | Marital status | Parity | Carrier status | Personal history of BC | RRM | Number of relatives with OC | Number of relatives with BC | Ascertainment | Postcode |
| ID-01 | No surgery | 40 | Caucasian | Single | 0 | BRCA1 | No | Yes | 0 | 1 SDR | High-risk FCC | London |
| ID-02 | RRSO | 41 | Caucasian | Married | 0 | BRCA2 | No | Yes | 0 | 1 FDR, 1 SDR | High-risk FCC | Essex |
| ID-03 | RRESDO | 37 | Caucasian | Married | 3 | BRCA2 | No | No | 1 SDR | 1 FDR, 1 SDR | High-risk FCC | Essex |
| ID-04 | RRSO | 46 | Caucasian | Married | 0 | BRCA1 | No | No | 0 | 0 | High-risk FCC | London |
| ID-05 | RRESDO | 43 | Caucasian | Single | 2 | BRCA1 | No | No | 1 SDR | 3 SDR | High-risk FCC | London |
| ID-06 | RRESDO | 38 | Caucasian | Married | 2 | BRCA1 | No | Yes | 0 | 3 SDR | High-risk FCC | Sussex |
| ID-07 | No-surgery | 36 | Asian | Single | 1 | BRCA1 | No | No | 1 SDR | 3 SDR | High-risk FCC | London |
| ID-08 | RRESDO | 46 | Caucasian | Married | 3 | BRCA2 | No | Yes | 0 | 1 FDR, 1 SDR | High-risk FCC | Cambridge |
| ID-09 | RRESDO | 39 | Caucasian | Married | 2 | BRCA1 | No | Yes | 1 FDR, 1 SDR | 1 FDR | High-risk FCC | London |
| ID-10 | No-surgery | 39 | Caucasian | Married | 0 | BRCA1 | No | No | 1 SDR | 1 FDR | High-risk FCC | London |
| ID-11 | RRESDO | 35 | Caucasian | Married | 2 | BRCA2 | No | No | 1 FDR | 0 | High-risk FCC | Hertfordshire |
| ID-12 | No-surgery | 36 | Caucasian | Married | 1 | BRCA1 | No | No | 2 SDR | 1 SDR | High-risk FCC | London |
| ID-13 | RRSO | 45 | Caucasian | Married | 1 | BRCA2 | No | Yes | 0 | 0 | General gynaecology clinic | Durham |
| ID-14 | No-surgery | 38 | Caucasian | Married | 1 | BRCA1 | Yes* | No† | 0 | 0 | High-risk FCC | London |
| ID-15 | RRESDO | 38 | Caucasian | Married | 2 | BRCA2 | No | No | 0 | 0 | High-risk FCC | Hertfordshire |
| ID-16 | RRESDO | 44 | Caucasian | Married | 2 | BRCA2 | No | No | 2 SDR | 1 SDR | High-risk FCC | Hampshire |
| ID-17 | RRESDO | 39 | Caucasian | Married | 2 | BRCA1 | Yes‡ | No† | 0 | 0 | GO clinic | Newport |
| ID-18 | RRESDO | 44 | Caucasian | Single | 2 | BRCA2 | No | Yes | 0 | 1 FDR, 2 SDR | High-risk FCC | London |
| ID-19 | No surgery | 34 | Caucasian | Married | 2 | BRCA1 | No | No | 0 | 1 SDR | Genetics clinic | Surrey |
| ID-20 | RRSO | 46 | Asian | Married | 2 | BRCA1 | No | No | 1 FDR, 2 SDR | 2 SDR | GO clinic | Aberdeen |
| ID-21 | RRESDO | 44 | Caucasian | Married | 2 | BRCA2 | Yes* | Yes§ | 1 FDR | 1 FDR, 1 SDR | GO clinic | Devon |
| ID-22 | RRSO | 39 | Caucasian | Married | 2 | BRCA2 | No | No | 0 | 1 FDR | GO clinic | Liverpool |
| ID-23 | RRSO | 40 | Caucasian | Single | 2 | BRCA1 | No | No | 1 FDR, 1SDR | 0 | High-risk FCC | Surrey |
| ID-24 | RRSO | 40 | Caucasian | Married | 1 | BRCA1 | Yes‡ | Yes*§ | 0 | 2 FDR | General gynaecology clinic | Cleveland |
*Oestrogen receptor positive breast cancer.
†Bilateral therapeutic mastectomies.
‡Triple negative breast cancer.
§Unilateral therapeutic mastectomy followed by contralateral risk reducing mastectomy.
BC, breast cancer; FCC, familial cancer clinic; FDR, first degree relative; GO, gynaecological oncology; OC, ovarian cancer; RRESDO, risk-reducing early salpingectomy with delayed oophorectomy; RRM, risk-reducing mastectomy; RRSO, risk-reducing salpingo-oophorectomy; SDR, second degree relative.
Themes
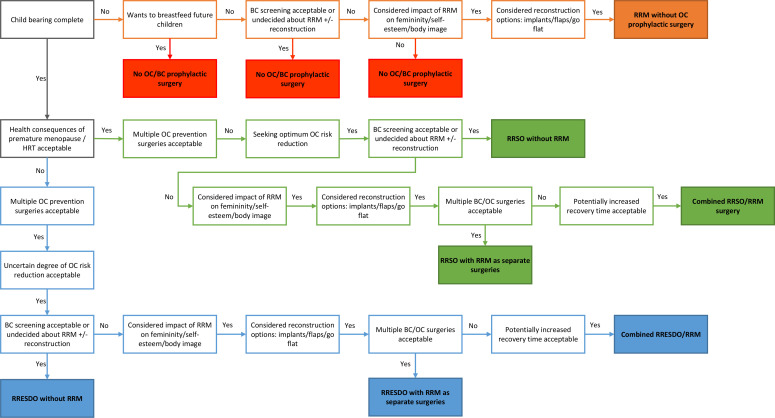
Seven themes pertinent to decision making emerged: fertility; menopause; cancer risk reduction: surgical choices; surgical complications; sequence of ovarian and breast prophylactic surgeries; support with decision making; satisfaction with treatment choices. Table 2 summarises the facilitators and table 3 the barriers per-theme and surgical prevention strategy. Figure 1 maps the decision-making options for premenopausal BRCA carriers considering risk-reducing surgery.
Table 2.
Thematised facilitators to uptake of risk reducing surgeries
| Themes | Facilitators | Quotes |
| RRESDO | ||
| Surgical complications; satisfaction with treatment choices | Positive experience with previous surgery | ‘…the trade-off between having two surgeries as opposed to one, that does feel absolutely fine to me, and that’s maybe because I've had positive experiences with surgery before.’ (ID-18) |
| Menopause; satisfaction with treatment choices | Flexible timing of delayed oophorectomy | ‘I know that there is no guarantee that it prevents ovarian cancer but I see it as being a positive thing I can do for myself for now, at my age and I know that if I had any concerns in the future, even before I hit menopause, that I could come back and approach you about having my ovaries removed, no-one’s telling me, “If you have your tubes out, you have to wait X, we won’t take your ovaries out for this”, so I think everyone’s been very open to discussing it and it’s been very focused around how I feel and what I want, which is very encouraging.’ (ID-16) |
| Menopause; satisfaction with treatment choices | Avoiding early menopause | ‘…what I was most interested in was the fact that it would be two-step because I feel personally, I'm too young to be put into menopause, I don’t want to go down that road.’ (ID-03) |
| Menopause | Avoiding the need to take HRT |
‘I'd rather just have a little surgery and deal with that for a small amount of time than have to take HRT all the time, I'm quite loathed to take drugs really.’ (ID-16) ‘I was worried about the financial implications of having to take something for life.’ (ID-18) |
| Menopause; satisfaction with treatment choices | Concerns HRT may not adequately alleviate menopausal symptoms and improve QoL | ‘…HRT perhaps hasn’t worked out quite as expected or planned or it’s needed a lot of tweaking or maybe they haven’t received the level that they’ve needed to and, they haven’t regretted the decision because actually they’ve reduced their risk but they’ve actually noticed a significant drop in their quality of life that they didn’t actually expect. And, I think it’s really important for people to know that that might happen…’ (ID-05) |
| Cancer risk reduction: surgical choices; satisfaction with treatment choices | To reduce anxiety of doing nothing | ‘Sometimes you just have to make a decision between two difficult things, where you don’t really want to do either of them and doing something is better than doing nothing…’ (ID-16) |
| Cancer risk reduction: surgical choices | Empowerment | ‘…I just see it as being something positive that I can do for myself, to hopefully reduce my risk of cancer.’ (ID-08) |
| Cancer risk reduction: surgical choices; sequence of ovarian and breast prophylactic surgeries; satisfaction with treatment choices | Stronger FH of BC than OC | ‘There’s more breast than ovary cancer in my family, so I’m probably at higher risk of breast cancer.’ (ID-18) |
| Fertility | Childbearing complete | ‘I have finished having children so it was an easy decision to make.’ (ID-06) |
| RRSO | ||
| Surgical complications | Single surgery and concerns over future health | ‘…I think while you’re fit and well, it’s the time to have surgery. The longer you wait, who knows what happens when you get older.’ (ID-13) |
| Surgical complications | Straightforward day case surgery | ‘…it (salpingo-oophorectomy)sounds like quite a straightforward minor operation and I can go home the same day…’ (ID-13) |
| Cancer risk reduction: surgical choices | Wanting maximum OC risk reduction | ‘I just want the surgery that will protect me from developing ovarian cancer the most.’ (ID-22) |
| Menopause | Taking HRT acceptable | ‘I don’t have any issue taking HRT.’ (ID-20) |
| Cancer risk reduction: surgical choices | Strong family history of OC | ‘So many of my relatives have died from ovarian cancer.’ (ID-23) |
| Fertility | Childbearing complete | ‘I’m finished having children.’ (ID-20) |
| Cancer risk reduction: surgical choices | No NHS OC screening programme | ‘There is no screening on the NHS for ovarian cancer and that means my only other option is to have my ovaries out.’ (ID-20) |
| Cancer risk reduction: surgical choices | Inability to self-examine ovaries | ‘From the very beginning I felt I was more concerned more about the ovarian cancer risk than the breast cancer risk, because I felt like I could effectively examine my own breasts and keep a check on that, but I can’t check my ovaries.’ (ID-04) |
| Cancer risk reduction: surgical choices | Poor OC prognosis | ‘…it’s very hard to detect ovarian cancer and it has a very poor prognosis, it seemed to make complete sense.’ (ID-04) |
| Support with decision making; cancer risk reduction: surgical choices; sequence of ovarian and breast prophylactic surgeries | Physician recommendation | ‘Counselling from my doctor really helped. She was knowledgeable, supportive and sympathetic of my situation. She recommended surgery as I have had all my kids, am 46 and because my aunt died of ovarian cancer at 45.’ (ID-04) |
| RRM | ||
| Cancer risk reduction: surgical choices | BC screening anxiety | ‘I never went away thinking, “I've got the all clear”, I went away feeling like, “As far as anyone can tell I've got the all clear”, and then the anxiety would start to rise again as we headed towards the next five month [screening] mark point when I could see it looming in the diary.’ (ID-13) |
| Fertility | Completion of childbearing and breast feeding | ‘I have finished having kids, so I don’t really need them anymore.’ (ID-02) |
| Cancer risk reduction: surgical choices; sequence of ovarian and breast prophylactic surgeries | Strong FH of BC | ‘I know that the risk is greater for cancer in the breast as compared to the ovaries because of my family history.’ (ID-02) |
| Combined breast and ovarian cancer prevention surgeries | ||
| Sequence of ovarian and breast prophylactic surgeries | Fewer surgeries | ‘Just throw everything at it, and let’s just get it all sorted in one.’ (ID-11) |
| Sequence of ovarian and breast prophylactic surgeries | Less anxiety associated with waiting for individual surgeries | ‘It’s stressful waiting for all the appointment to see different specialists at different times. I would be happier if I could have got it all sorted in one go.’ (ID-05) |
| Sequence of ovarian and breast prophylactic surgeries | Fewer hospital appointments | ‘The fewer times I need to visit hospital, the better.’ (ID-05) |
| Sequence of ovarian and breast prophylactic surgeries | Less delays waiting for individual surgeries | ‘I guess there’s no thinking of delaying one or the other, if I've made a decision to reduce my risk, I think it would make sense to do them both at the same time.’ (ID-22) |
| Sequence of ovarian and breast prophylactic surgeries; support with decision making | Less time off work | ‘I’m self employed, so the less time off work, the better.’ (ID-22) |
| Sequence of ovarian and breast prophylactic surgeries | Single postoperative recovery | ‘I would prefer to recover just once from surgery.’ (ID-18) |
| Sequence of ovarian and breast prophylactic surgeries; fertility | Childbearing complete | ‘Because I’m done having kids, I just want it all out.’ (ID-23) |
BC, breast cancer; HRT, hormone replacement therapy; OC, ovarian cancer; QoL, quality of life; RRESDO, risk-reducing early salpingectomy with delayed oophorectomy; RRM, risk-reducing mastectomy; RRSO, risk-reducing-salpingo-oophorectomy.
Table 3.
Thematised barriers to uptake of risk reducing surgeries
| Themes | Barriers | Quotes |
| RRESDO | ||
| Menopause; satisfaction with treatment choices | Approaching the age of natural menopause | ‘I think my age, I think it’s the fact that they [surgeries] might have ended up being within two or three years, it just didn’t make that much sense to me…’ (ID-20) |
| Cancer risk reduction; sequence of ovarian and breast prophylactic surgeries | Strong family history of OC | ‘I am more concerned about protecting myself from ovarian cancer because I have more relatives with ovarian cancer than breast cancer and so I just want the lot [tubes and ovaries] out.’ (ID-23) |
| Cancer risk reduction: surgical choices | Two staged surgery | ‘To be honest, I think if you’re going to go and have it done, have it done in one. Why would I want, in another 10 years, to go and have surgery again?’ (ID-23) |
| Surgical complications | Concerns over future poor health | ‘I don’t know what my health would be like in 10 years’ time, I might not be up for surgery. I just think get it done, get it over and done with now.’ (ID-20) |
| Cancer risk reduction: surgical choices; satisfaction with treatment choices | More effective surgery to reduce OC risk | ‘…I just want to eliminate as much [risk] as possible…’ (ID-20) |
| Fertility | Childbearing not complete | ‘I have not finished having children…’ (ID-01) |
| RRSO | ||
| Fertility | Childbearing not complete | ‘I have not finished having children…’ (ID-14) |
| Fertility | Not wanting to remove healthy tissue | ‘It’s also quite difficult to decide to go through an operation when there’s nothing wrong, so obviously it’s preventative but part of you is like “I'm perfectly healthy, why would I do this?”’(ID-01) |
| Menopause; satisfaction with treatment choices | Early menopause | ‘I was very off put by that [oophorectomy] because I feel I'm too young to be put into the menopause and I'm aware, probably through training as a nurse, the symptoms associated with that, the increased risk of, I would be decreasing my risk obviously of ovarian cancer but then have an increased risk of osteoporosis and all the other things, it was trying to weigh up the best option and I didn’t feel that that’s something I wanted to think of at this moment in time.’ (ID-01) |
| RRM | ||
| Cancer risk reduction: surgical choices | Loss of femininity and self esteem | ‘My breasts are my womanhood and loosing them I think would really effect my self esteem and not in a good way.’ (ID-15) |
| Fertility | Childbearing and breastfeeding not complete | ‘I still need my breasts to breastfeed. I’ve not finished having kids.’ (ID-03) |
| Surgical complications; satisfaction with treatment choices | Major operation with long recovery | ‘…it’s a major operation, psychologically and physically with long recovery.’ (ID-03) |
| Cancer risk reduction: surgical choices | Effective BC screening programme | ‘There is such an effective screening programme, I wouldn’t want surgery unless there was something picked up on a scan.’ (ID-04) |
| Cancer risk reduction: surgical choices | Good prognosis from early screen detected BC | ‘…breast cancer is quite treatable and has often a good prognosis.’ (ID-04) |
| Combined ovarian and breast cancer prevention surgeries | ||
| Sequence of ovarian and breast prophylactic surgeries; satisfaction with treatment choices | Increased duration of postoperative recovery | ‘I would be worried that recovery from such a big operation would be really long.’ (ID-23) |
| Sequence of ovarian and breast prophylactic surgeries; satisfaction with treatment choices | Concerns over increased number of complications | ‘…primarily it will be around the additional risk of complications and side effects from the various elements of the two different surgeries…’ (ID-23) |
| Sequence of ovarian and breast prophylactic surgeries; satisfaction with treatment choices | Psychological distress | ‘I don’t think I would cope well with going into menopause the same time as losing my breasts and all the implications that would have on me feeling like a woman.’ (ID-22) |
BC, breast cancer; HRT, hormone replacement therapy; OC, ovarian cancer; QoL, quality of life; RRESDO, risk-reducing early salpingectomy with delayed oophorectomy; RRSO, risk-reducing salpingo-oophorectomy.
Figure 1.
Decision making aid for premenopausal BRCA carriers considering risk reducing surgery. BC, breast cancer; HRT, hormone replacement therapy; OC, ovarian cancer; RRESDO, risk reducing early salpingectomy with delayed oophorectomy; RRM, risk reducing mastectomy; RRSO, risk reducing salpingo-oophorectomy.
Fertility
ID-03 (RRESDO-arm): ‘I just think because I know that I’ve completed my family and I don’t want these old tubes anymore anyway, I just see it [surgery] as being something positive that I can do for myself, to hopefully reduce my risk of cancer.’
Fertility was an important consideration for all women. For 18 women choosing surgery (RRESDO/RRSO), 16 completed childbearing and two didn’t want children. Once fertility was not a barrier, deciding to undergo surgery was less complex and a natural next step. Four women had not completed childbearing, wished to delay surgery and joined the control arm. Two control arm women despite completing childbearing delayed surgery. One was undecided what to choose and the second had strong beliefs against removing healthy tissue and any risk-reducing surgery.
Two women opted to conceive through in vitro fertilisation (IVF) and preimplantation genetic diagnosis (PGD). Both acknowledged PGD/IVF was physically and mentally stressful with multiple hospital visits and additional procedures but considered it an acceptable tradeoff to prevent their children being BRCA carriers and facing similar difficult decisions. One participant felt she may have not proceeded with a natural conception if IVF/PGD had failed.
Menopause
ID-06 (RRESDO-arm): ‘I wasn’t happy with the impact of going in to menopause straight away and although you obviously have HRT options which might be offered if you go to a good gynaecologist, I just, I wasn’t convinced that HRT brings you back up to an even keel or level, the way that I’m feeling right now which is basically very balanced.’
Interviewees who chose RRESDO (n=11) did so because of concerns about detrimental consequences of early menopause following oophorectomy, particularly low mood, sexual dysfunction and poorer QoL. All RRESDO interviewees found the uncertainty regarding long-term health implications (eg, possibility of earlier menopause following ES) an acceptable risk. Interviewees rationalised RRESDO as a preferential strategy to delay early menopause and its long-term consequences while benefiting from some OC risk reduction. Two women would have delayed risk-reducing surgery until they were near/at natural menopause if RRESDO was unavailable, whereas another would have undergone RRSO instead. Two RRESDO women found avoiding need for HRT and repeat prescription costs more appealing. RRESDO interviewees wanted to be in control of choosing the timing of DO (with their clinician) and felt a fixed timing for DO was a barrier to RRESDO uptake. Menopause was a lesser concern to older premenopausal women (nearer the age of natural menopause) self-selecting RRSO because RRESDO would only delay menopause by a few years and require an additional operation.
RRSO women managed outside specialist high-risk clinics reported receiving conflicting advice on HRT safety, lack of information on HRT efficacy for symptom relief and struggling with HRT access. A number of gynaecologists/gynaecological oncologists do not routinely counsel women about health consequences of early menopause, lack awareness of HRT safety and do not offer HRT to BRCA carriers undergoing premenopausal RRSO (particularly those near natural menopause age). Women attending BRCA support forums felt unsupported without follow-up after surgery and reported persistent menopausal symptoms detrimentally affecting QoL despite HRT. Women managed within a high-risk FCC reported being more reassured with their planned follow-up and access to a menopause specialist post-RRSO.
Cancer risk reduction: surgical choices
Ovarian-cancer risk-reducing surgery
ID-08 (RRESDO-arm): ‘It’s [RRESDO] acceptable because it’s my decision making as well, it’s not at the fault of any health professional, no-one is making me do it this way, it’s my decision and I'm aware of that.’
Women who prioritised avoiding menopause and preserving QoL selected RRESDO. While, women concerned about the precision of risk reduction and who prioritised maximising OC risk reduction, selected RRSO. Women with a strong FH of OC selected RRSO, and with strong FH of BC preferred RRESDO.
RRESDO interviewees felt comfortable and empowered with the tradeoff between an uncertain degree of OC risk reduction and avoidance of early menopause. They rationalised they were doing ‘…something to reduce risk as opposed to nothing…’ while avoiding early menopause and preserving their QoL.
A few interviewees reported being counselled/reading they were at increased endometrial cancer risk and were offered/requested a concomitant hysterectomy.
Breast-cancer risk-reducing surgery
ID-01 (No-surgery-arm): ‘…it’s also quite difficult to decide to go through a major operation when there’s nothing wrong, so obviously it’s preventative but part of you is like “I'm perfectly healthy, why would I do this?”, and there’s something quite emotional about the idea of having your breast removed as well, whereas the ovaries aren’t seen, it’s about appearance as well and just having implants and things like that.’
Interviewees considered RRM decision making much harder compared with RRSO/RRESDO. Women were conflicted with wanting to optimise BC prevention while preserving breasts for femininity and self-esteem. They preferred delaying RRM until finishing childbearing and breastfeeding.
ID-13 (RRSO-arm): ‘I never went away thinking, “I've got the all clear”, I went away feeling like, “As far as anyone can tell I've got the all clear”, and then the anxiety would start to rise again as we headed towards the next five month mark point when I could see it looming in the diary.’
Some women reported anxiety/stress with breast s
Nine women underwent RRM and five struggled with decision making on reconstruction with flaps or implants; and consideration of nipple-sparing versus non-nipple-sparing surgeries. Two highlighted lack of healthcare professional support for women opting against reconstruction. One interviewee regretted her decision of flap reconstruction due to resultant cosmetic appearance and chronic pain but did not regret RRM.
All BC-affected interviewees selected OC-prevention surgery purely for preventing OC. They felt alternative treatments were available to improve BC survival. Women selecting RRESDO did not consider the potential loss of improved BC-survival from oophorectomy a barrier.
Surgical complications
ID-18 (RRESDO-arm): ‘…the trade-off between having two surgeries as opposed to one, that does feel absolutely fine to me, and that’s maybe because I've had positive experiences with surgery before.’
Women with previous positive surgical experiences (good relationship with surgeon, postoperative care, no complications) and/or good health found two-staged RRESDO acceptable, without concerns for increased surgical complications or hospital appointments. Inspection of pelvis/abdomen for OC at RRES was reassuring for one patient. One RRSO interviewee highlighted concerns of two surgeries as future health may deteriorate with age and increase risks of surgical complications.
Sequence of ovarian and breast prophylactic surgeries
Sequential surgery
ID-16 (RRESDO-arm): ‘Because I’ve never had an operation, I thought it would be better to have a minor operation first, just to kind of prepare me rather than going straight into major surgery, that was one reason but the other was the ovarian cancer prevention felt more pressing because I'm on the breast screening programme and it didn’t feel quite so urgent.’
Interviewees reported preferring OC prevention surgery before RRM because of lack of an OC screening programme; poorer prognosis of OC; being a laparoscopic procedure with quick recovery; inability to self-examine ovaries. Women with a stronger FH of OC preferred RRSO first and those with a FH of BC chose undergoing RRM first. Sequence was also dependent on surgical referral and appointment times with some experiencing shorter waiting times for seeing a breast surgeon than a gynaecologist/gynaecological oncologist.
Combined ovarian and breast prophylactic surgery
ID-11 (RRESDO-arm): ‘Just throw everything at it, and let’s just get it all sorted in one.’
Fifteen women would have preferred a single combined risk-reducing procedure involving RRM±reconstruction along with OC preventative surgery. Reasons included fewer surgeries, less anxiety, less waiting, fewer appointments, less time off work and single surgical recovery. However, nine women expressed concerns over possible increased recovery time and increased psychological distress from early menopause impacted by RRM associated body image issues.
Support with decision making
Clinical support
ID-05 (RRESDO-arm): ‘…my experience of [gynaecology] appointments is that people just present things to you, and very quickly you have to make a decision, and there isn’t a way to just, some of the decisions take a lot of discussion, and coming back to it, and rethinking, and I just feel that there isn’t that space for it…’
Interviewees expressed preference for multiple appointments with gynaecologists/gynaecological oncologists for discussing risk-reducing surgery. Decision making was a complex/dynamic process, with one visit being inadequate to absorb/assimilate complex information, and make an informed decision. Interviewees felt more supported with RRM decision making, given access to a psychologist and multiple breast surgical appointments before RRM. Interviewees wished to be routinely offered an ‘optional’ (not compulsory) consultation with a psychologist prior to OC preventative surgery.
Interviewees who had done personal research (reading literature, speaking to BRCA carriers, online support groups (OSGs)) felt their decision was validated following counselling from healthcare professionals. Counselling received aided decision making of women who had not done any personal research. Counselling lacked information on communicating genetic test results to children and complex decisions carriers faced.
Patient support groups
ID-05 (RRESDO-arm): ‘I know there are [online] forums, but a lot of it, there’s a lot of fearful ideas there, and my cousin was saying that she just had to stop going on those forums.’
Continuous availability/access and anonymity were advantages of online BRCA support groups/forums reported by our cohort. However, interviewees also highlighted negative personal experiences (and anxiety) given poor surgical outcomes/negative experiences discussed at these outlets which were not balanced with positive outcomes. Interviewees used online forums for an ad-hoc-specific query rather than for regular support. Clinician-led educational days with experts’ talks about management options, opportunities to ask questions, share experiences and meet other BRCA carriers appeared preferable.
Lifestyle support
ID-22 (RRSO-arm): ‘When I realised that I’d have to go through with a number of operations to help reduce the risk, I made sure that I was in the best possible health beforehand to deal with those and I was really glad that I did.’
RRESDO/RRSO women were eating healthier, losing weight and exercising regularly to minimise postoperative complications and shorten recovery time. Even no-surgery interviewees made healthier choices (smoking cessation, reduced alcohol, exercise, diet) to increase their conception chances.
Satisfaction with treatment choices
ID-16 (RRESDO-arm): ‘I'm at peace over the situation, and it’s not something that has caused me anxiety, although I don’t really like procedures and hospitals as I've said, but I feel that it’s something that I can manage.’
Interviewees felt it difficult to state outright satisfaction with their decision to have/not have preventative surgery but rationalised their decision making. Women delaying surgery were concerned about developing cancer. Women undergoing surgery were also concerned about developing cancer along with surgical complications, impact on QoL and psychological health. However surgery reduced OC/BC anxiety.
ID-18 (RRESDO-arm): ‘I’d done quite a bit of research myself. I found all of the people that I’ve met within the team have been fantastic and haven’t just treated me like Patient X who doesn’t know anything at all.’
Interviewees managed within high-risk multidisciplinary FCC appeared more satisfied than those managed in genetics/gynaecology/gynaecological oncology clinics. Reasons included a more personalised approach, information tailored to the individual’s pre-existing knowledge base, same-day consultations with multiple specialists and continuity of care. The combination of specialists supporting FCCs varied but included: geneticists, gynaecologists, breast surgeons, menopause specialists, fertility specialists, psychologists. All seven women previously under the care of non-specialist clinics reported higher satisfaction levels when subsequently managed in the FCC setting.
ID-13 (RRSO-arm): ‘…it does take time, like relieve yourself of that sense of pressure of having to come to a decision…’
Interviewees would advise fellow BRCA carriers to avoid time-pressure with surgical decision making, talk to other BRCA carriers, do personal research, ask for second opinions if not satisfied.
No-surgery interviewees would regret their decision to delay/avoid surgery if they developed OC. Women undergoing surgery would regret it if a life-changing surgical complication occurred.
Discussion
We identified seven interconnected themes integral to surgical prevention decision making in BRCA carriers. To the best of our knowledge, this is the first qualitative study that has mapped all aspects of the decision-making process of BRCA carriers undergoing/considering all ovarian (RRESDO/RRSO)/breast (RRM)/combined risk-reducing surgical options (figure 1). Women for whom maximising OC risk reduction was relatively more important than early menopause/QoL preferred RRSO, whereas those more concerned about impact of menopause chose RRESDO.
While some facilitators/barriers we describe for RRESDO are similar to those reported earlier, we found some differences too.18 19 25 Unlike a Dutch study reporting a personal history of BC as a barrier, we report that BC-affected BRCA carriers found RRESDO acceptable despite potential for improved BC survival afforded by premenopausal oophorectomy. BC-affected and unaffected BRCA carriers selecting RRESDO were equally concerned about avoiding early menopause/maintaining QoL. This apparent difference in RRESDO acceptability among UK and Dutch women may be attributed to differences in counselling, risk-management options available, population differences, evolving scientific evidence base, its interpretation by clinicians and patients and changing practices. Oophorectomy may not reduce primary/contralateral BC risk26–29 and effective adjunct treatments to improve BC outcomes are available including contralateral mastectomy, GnRH analogues, selective estrogen receptor modulators etc.
Approaching the age of natural menopause and concerns over future poor health were new barriers to RRESDO we elicited. Previously unreported RRESDO facilitators identified include avoiding the need for HRT and significant concerns about not adequately alleviating menopausal symptoms or improving QoL. This highlights women’s unease and apprehension related to effects of menopause.30 Premenopausal women concerned about sexual dysfunction are more likely to opt for RRESDO.19 Despite HRT, symptom levels following premenopausal oophorectomy, particularly for sexual dysfunction, remain above those retaining their ovaries.31 As part of RRSO decision making all premenopausal women should be involved in formulating an individualised presurgical HRT plan and fully counselled on menopausal issues along with the benefits and limitations of HRT.
Other RRESDO facilitators we identified include positive experience with previous surgery, reducing the anxiety of doing nothing and flexible timing of DO. The Dutch-TUBA,32 and US-PSDO (Prophylactic Salpingectomy with Delayed Oophorectomy)33 studies undertake DO well before onset of menopause (without the option to delay until natural menopause). This could have been a barrier for UK women. However, in the UK PROTECTOR, and US WISP (Women Choosing Surgical Prevention)6 trials, women can choose when to undergo DO but are encouraged to do this by natural menopause. The facilitator and barriers to RRSO/RRM elicited in our cohort are similar to those reported earlier.22 33–37
We too found undergoing preventative surgery reduced anxiety.18 34 35 Although RRM decision making was more complex than OC preventative surgery, women felt more supported in their decision to undergo RRM (than OC prevention) due to psychology input and multiple breast surgical appointments. This reflects the well-established tertiary care BC risk-management pathways in the UK.38 We found disparities in OC risk management care across the UK. Women managed in high-risk FCC settings were more satisfied with their care and received better support and HRT access. The lower satisfaction in women managed in non-specialist clinics was linked to non-streamlined clinical pathways, need for multiple referrals, delays in seeing different specialists, lack of continuity of care and difficulties in assimilating large volumes of information in a single appointment. Others too have reported low satisfaction with poorly developed care pathways.36 39 Of particular concern was poor HRT counselling and management, also reported previously.20 High-risk women need to be supported by a multidisciplinary team comprising geneticists, gynaecologists/gynae-oncologists with a special interest, breast oncologists, oncoplastic surgeons, menopause specialists, fertility specialists, psychologists and specialist nurses. Our findings support centralising care of high-risk women to centres which have specialist high-risk multidisciplinary FCC services and the need to develop more such services/centres with well-defined care pathways.
Our data suggest that women engage concurrently in both OC and BC prevention decision making in contrast to some studies suggesting that women prioritise decisions and make them one at a time.36 40 41 We identified a demand for combined OC-and-BC prevention surgery. However, only few centres currently offer this, the psychological/QoL effects following combined BC/OC prophylactic surgery are unknown and not all women may be suitable candidates. Combined surgery offers logistical practicality for busy working women with dependent families by limiting the hospital appointments/surgeries/postoperative recoveries and has high satisfaction.40 Initial data suggest that a combined approach has lower costs than separate procedures40 but formal cost-utility analysis including sensitivity analysis is needed. Additionally, RRESDO may be more acceptable than RRSO for combined surgery given the potential for menopausal symptoms while recovering from effects of mastectomy.
Benefits of OSGs42–44 include fluid informational exchange, continuous availability, greater access/anonymity and were also reported by our cohort. Our cohort reported increasing anxiety with OSGs and a preference for educational support groups (ESGs). ESGs involve face-to-face group activities where participants and clinicians share their experiences and expertise, along with a patient representative acting as the group spokesperson. Women found the opportunity to ask experts questions and meet other BRCA carriers face-to-face more helpful than OSGs. Although small randomised controlled trials (RCTs) have shown lower anxiety/depression with OSGs (compared with clinical care) in BC women,45 these results may not be generalisable to BRCA previvors unaffected by cancer. Large, well-designed RCTs comparing OSG with ESG are needed. Another gap we identified was support women needed to communicate to their children genetic test results and the complex decisions they faced. Options to address this may include customised information sheets/decision aids, offering family counselling. While family counselling is established for informing children of a parent’s cancer diagnosis,46 outcome data and pathways for this in a previvor setting are needed.
Strengths of our study include a robust methodological approach using semistructured in-depth interviews until reaching data saturation, independent data analysis by two researchers and a comprehensive three-step coding process. Our sample was broad-based and included women who declined surgery, had a personal history of BC, parous/nulliparous, ascertainment from a variety of outpatient settings and different UK geographical locations. Limitations include that only two interviewees were non-Caucasian and there may be cultural nuances affecting the decision-making process in ethnic minorities. Also, women who had undergone RRM were interviewed retrospectively, ensuing a risk of recall bias.
Medical, physical, psychological and social contextual factors influence the timing of risk-reducing surgeries. RRESDO offers premenopausal women who would otherwise delay/decline premenopausal oophorectomy a degree of OC risk reduction while avoiding the detrimental sequelae of early menopause. The addition of RRESDO as a two-stage surgical alternative to RRSO, adds an additional dimension to an already complex decision-making process, so it is possible it may increase length of time for women to come to a decision regarding OC prevention surgery. Women who prioritise maximising OC risk reduction favour selecting RRSO, whereas those who prioritised maintaining QoL and avoiding menopause preferred RRESDO. Our cohort of women expressed a clear interest in combined breast-and-ovarian prophylactic surgeries. Women managed in specialist FCC settings compared with non-specialist settings received better quality care, better HRT access and were more satisfied. There is need for centralising the care of women at risk of familial gynaecological cancers to centres within specialist-FCC services which are able to provide a more streamlined, holistic multidisciplinary approach.
Acknowledgments
We are grateful to all women took part in the interviews. We are grateful to the central trials coordinating team at the Centre for Experimental Cancer Medicine at QMUL, led by Kelly Mousa. We are grateful to the independent members of the trial steering committee (chaired by Mr Tim Mould) and the data monitoring committee (chaired by Professor Richard Edmondson) and central pathology committee (Professor Naveena Singh (chair), Professor W Glenn McCluggage, Dr Raji Ganesan, Dr Gareth Bryson, Dr Gareth Rowlands, Dr Rupali Arora). We acknowledge support provided by a number of charities and stakeholders including BRCA Umbrella (Caroline Presho), The Eve Appeal, Ovacome, Target Ovarian Cancer and Ovarian Cancer Action. GDE is supported through the NIHR Manchester Biomedical Research Centre (IS-BRC-1215–20007). We are grateful to all our collaborators of the PROTECTOR study: Dr Munaza Ahmed (North East Thames Cancer Genetics Service, Great Ormond Street Hospital NHS Foundation Trust), Dr Aarti Sharma (Cardiff and Vale UHB), Dr Gautam Mehra (Guy’s and St Thomas’ NHS Foundation Trust), Dr Adam Rosenthal (University College London Hospitals NHS Foundation Trust), Dr Ian Harley (Belfast Health & Social Care Trust), Dr Michelle Mackintosh & Prof Emma Crosbie (Manchester University NHS Foundation Trust), Professor Sadaf Ghaem-Maghami (Imperial College Healthcare NHS Trust), Professor Omer Devaja (Maidstone and Tunbridge Wells NHS Trust), Professor Sudha Sundar and Mr Janos Balega (Sandwell and West Birmingham Hospitals NHS Trust), Dr Tim Duncan (Norfolk and Norwich University Hospitals NHS Foundation Trust), Dr Iain Cameron (Gateshead Health NHS Foundation Trust), Dr Claire Newton (University Hospitals Bristol NHS Foundation Trust), Dr Sonali Kaushik (Brighton and Sussex University Hospitals NHS Trust), Dr Angela Brady (London North West Healthcare NHS Trust), Dr Supratik Chattopadhyay (University Hospitals of Leicester NHS Trust), Dr Natalia Povolotskaya (Portsmouth Hospitals NHS Trust), Dr Rema Iyer (East Kent Hospitals University NHS Trust), Dr Lucy Side (University Hospital Southampton NHS Foundation Trust), Dr Katie Snape (St George’s University Hospitals NHS Foundation Trust), Dr Anil Tailor (Royal Surrey County Hospital Foundation Trust), Dr Manon van Seters (Worcestershire Acute Hospital Trust), Dr Katherine Edey (Royal Devon & Exeter NHS Foundation Trust), Dr Sian Taylor (Liverpool Women’s Hospital NHS Foundation Trust), Dr Suma Kodiathodi (North Tees and Hartlepool NHS Foundation Trust), Dr Partha Sengupta (County Durham and Darlington NHS Foundation Trust), Dr Scott Fegan (NHS Lothian), Dr Karin Williamson (Nottingham University Hospitals NHS Trust), Dr Andrew Phillips (University Hospitals of Derby and Burton NHS Foundation Trust), Dr Mark Willett (East Lancashire Hospitals NHS Trust), Dr Tony Chalhoub (The Newcastle upon Tyne Hospitals NHS Foundation Trust), Dr Sanjay Rao (South Tees Hospitals NHS Foundation Trust), Dr Nicholas Matthews (South Tyneside and Sunderland NHS Foundation Trust), Dr Beena Abdul (Northampton General Hospitals NHS Trust), Dr Ibraheem Hamoodi (Northumbria Healthcare NHS Foundation Trust), Dr Claire Park (Royal United Hospitals Bath NHS Foundation Trust), Dr Jane Borley (Royal Cornwall Hospitals NHS Trust), Dr Richard Hutson (Leeds Teaching Hospitals NHS Trust), Dr Kerryn Lutchman-Singh (Swansea Bay University Health Board), Dr Richard Peevor (Betsi Cadwaladr University Health Board), Dr Mahalakshmi Gurumurthy (NHS Grampian), Dr Kalpana Ragupathy (NHS Tayside).
Footnotes
Twitter: @ProfManchanda
Collaborators: The PROTECTOR team: Raji Ganesan; Gareth Bryson; Gareth Rowlands; Rupali Arora; Munaza Ahmed; Aarti Sharma; Gautam Mehra; Adam Rosenthal; Michelle Mackintosh; Sadaf Ghaem-Maghami; Omer Devaja; Sudha Sundar; Janos Balega; Tim Duncan; Claire Newton; Sonali Kaushik; Angela Brady; Supratik Chattopadhyay; Natalia Povolotskaya; Iain Cameron; Rema Iyer; Lucy Side; Katie Snape; Anil Tailor; Kavitha Thumuluru Madhuri; Katherine Edey; Sian Taylor; Manon van Seters; Suma Kodiathodi; Partha Sengupta; Scott Fegan; Karin Williamson; Andrew Phillips; Mark Willett; Tony Chalhoub; Sanjay Rao; Nicholas Matthews; Beena Abdul; Claire Park; Jane Borley; Ibraheem Hamoodi; Richard Hutson; Kerryn Lutchman-Singh; Richard Peevor; Mahalakshmi Gurumurthy; Kalpana Ragupathy; Emma Crosbie.
Contributors: Conception of qualitative study: FG, RM. Qualitative design and development: FG, RM, DM. Qualitative data collection: FG. Trial management: FG, SR, CT, NS, GDE, UM, RL, ES, WGM, HH, RM. Data analysis: FG, SG, RM, DM. Preparation of tables and figures: FG, OE. Initial draft of manuscript: FG, RM, DM. Manuscript writing and approval: all authors.
Funding: The study is supported by researchers at the Wolfson Institute of Preventive Medicine, Queen Mary University of London (C16420/A18066). This work was supported and funded by Barts and The London Charity and Rosetrees Trust.
Disclaimer: The funding bodies had no role in the study design, data collection, analysis, interpretation or writing of the report or decision to submit for publication. The research team was independent of funders.
Competing interests: RM declares research funding from Cancer Research UK and The Eve Appeal outside this work, an honorarium for grant review from Israel National Institute for Health Policy Research and honorarium for advisory board membership from Astrazeneca/MSD. RM is supported by an NHS Innovation Accelerator (NIA) Fellowship for population testing.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
the PROTECTOR team:
Raji Ganesan, Gareth Bryson, Gareth Rowlands, Rupali Arora, Munaza Ahmed, Aarti Sharma, Gautam Mehra, Adam Rosenthal, Michelle Mackintosh, Sadaf Ghaem-Maghami, Omer Devaja, Sudha Sundar, Janos Balega, Tim Duncan, Claire Newton, Sonali Kaushik, Angela Brady, Supratik Chattopadhyay, Natalia Povolotskaya, Iain Cameron, Rema Iyer, Lucy Side, Katie Snape, Anil Tailor, Kavitha Thumuluru Madhuri, Katherine Edey, Sian Taylor, Manon van Seters, Suma Kodiathodi, Partha Sengupta, Scott Fegan, Karin Williamson, Andrew Phillips, Mark Willett, Tony Chalhoub, Sanjay Rao, Nicholas Matthews, Beena Abdul, Claire Park, Jane Borley, Ibraheem Hamoodi, Richard Hutson, Kerryn Lutchman-Singh, Richard Peevor, Mahalakshmi Gurumurthy, Kalpana Ragupathy, and Emma Crosbie
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The PROTECTOR Study received full ethics approval from London-Bloomsbury Research Ethics Committee (18/LO/0555). The study was registered with the International Standard Randomised Controlled Trial Number Register-ISRCTN 25173360 (https://doi.org/10.1186/ISRCTN25173360).
References
- 1. Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips K-A, Mooij TM, Roos-Blom M-J, Jervis S, van Leeuwen FE, Milne RL, Andrieu N, Goldgar DE, Terry MB, Rookus MA, Easton DF, Antoniou AC, McGuffog L, Evans DG, Barrowdale D, Frost D, Adlard J, Ong K-R, Izatt L, Tischkowitz M, Eeles R, Davidson R, Hodgson S, Ellis S, Nogues C, Lasset C, Stoppa-Lyonnet D, Fricker J-P, Faivre L, Berthet P, Hooning MJ, van der Kolk LE, Kets CM, Adank MA, John EM, Chung WK, Andrulis IL, Southey M, Daly MB, Buys SS, Osorio A, Engel C, Kast K, Schmutzler RK, Caldes T, Jakubowska A, Simard J, Friedlander ML, McLachlan S-A, Machackova E, Foretova L, Tan YY, Singer CF, Olah E, Gerdes A-M, Arver B, Olsson H, BRCA1 and BRCA2 Cohort Consortium . Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 2017;317:2402–16. 10.1001/jama.2017.7112 [DOI] [PubMed] [Google Scholar]
- 2. Yang X, Leslie G, Doroszuk A, Schneider S, Allen J, Decker B, Dunning AM, Redman J, Scarth J, Plaskocinska I, Luccarini C, Shah M, Pooley K, Dorling L, Lee A, Adank MA, Adlard J, Aittomäki K, Andrulis IL, Ang P, Barwell J, Bernstein JL, Bobolis K, Borg Åke, Blomqvist C, Claes KBM, Concannon P, Cuggia A, Culver JO, Damiola F, de Pauw A, Diez O, Dolinsky JS, Domchek SM, Engel C, Evans DG, Fostira F, Garber J, Golmard L, Goode EL, Gruber SB, Hahnen E, Hake C, Heikkinen T, Hurley JE, Janavicius R, Kleibl Z, Kleiblova P, Konstantopoulou I, Kvist A, Laduca H, Lee ASG, Lesueur F, Maher ER, Mannermaa A, Manoukian S, McFarland R, McKinnon W, Meindl A, Metcalfe K, Mohd Taib NA, Moilanen J, Nathanson KL, Neuhausen S, Ng PS, Nguyen-Dumont T, Nielsen SM, Obermair F, Offit K, Olopade OI, Ottini L, Penkert J, Pylkäs K, Radice P, Ramus SJ, Rudaitis V, Side L, Silva-Smith R, Silvestri V, Skytte A-B, Slavin T, Soukupova J, Tondini C, Trainer AH, Unzeitig G, Usha L, van Overeem Hansen T, Whitworth J, Wood M, Yip CH, Yoon S-Y, Yussuf A, Zogopoulos G, Goldgar D, Hopper JL, Chenevix-Trench G, Pharoah P, George SHL, Balmaña J, Houdayer C, James P, El-Haffaf Z, Ehrencrona H, Janatova M, Peterlongo P, Nevanlinna H, Schmutzler R, Teo S-H, Robson M, Pal T, Couch F, Weitzel JN, Elliott A, Southey M, Winqvist R, Easton DF, Foulkes WD, Antoniou AC, Tischkowitz M. Cancer Risks Associated With Germline PALB2 Pathogenic Variants: An International Study of 524 Families. J Clin Oncol 2020;38:Jco1901907:674–85. 10.1200/JCO.19.01907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang X, Song H, Leslie G, Engel C, Hahnen E, Auber B, Horváth J, Kast K, Niederacher D, Turnbull C, Houlston R, Hanson H, Loveday C, Dolinsky JS, LaDuca H, Ramus SJ, Menon U, Rosenthal AN, Jacobs I, Gayther SA, Dicks E, Nevanlinna H, Aittomäki K, Pelttari LM, Ehrencrona H, Borg Åke, Kvist A, Rivera B, Hansen TVO, Djursby M, Lee A, Dennis J, Bowtell DD, Traficante N, Diez O, Balmaña J, Gruber SB, Chenevix-Trench G, Investigators kConFab, Jensen A, Kjær SK, Høgdall E, Castéra L, Garber J, Janavicius R, Osorio A, Golmard L, Vega A, Couch FJ, Robson M, Gronwald J, Domchek SM, Culver JO, de la Hoya M, Easton DF, Foulkes WD, Tischkowitz M, Meindl A, Schmutzler RK, Pharoah PDP, Antoniou AC. Ovarian and breast cancer risks associated with pathogenic variants in RAD51C and RAD51D. J Natl Cancer Inst 2020;112:1242–50. 10.1093/jnci/djaa030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. NICE, Familial Breast Cancer . Classification and care of people at of familial breast cancer and management of breast cancer and related risks in people with a family history of breast cancer (CG164). London, UK: National Institute for Health and Care Excellence, 2013. [Google Scholar]
- 5. Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, Saunders C, Roche N, Mansel RE, von Minckwitz G, Bonanni B, Palva T, Howell A, IBIS-II investigators . Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): an international, double-blind, randomised placebo-controlled trial. Lancet 2014;383:1041–8. 10.1016/S0140-6736(13)62292-8 [DOI] [PubMed] [Google Scholar]
- 6. Cuzick J, Forbes JF, Sestak I, Cawthorn S, Hamed H, Holli K, Howell A, International Breast Cancer Intervention Study I Investigators . Long-term results of tamoxifen prophylaxis for breast cancer--96-month follow-up of the randomized IBIS-I trial. J Natl Cancer Inst 2007;99:272–82. 10.1093/jnci/djk049 [DOI] [PubMed] [Google Scholar]
- 7. Rebbeck TR, Friebel T, Lynch HT, Neuhausen SL, van 't Veer L, Garber JE, Evans GR, Narod SA, Isaacs C, Matloff E, Daly MB, Olopade OI, Weber BL. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 2004;22:1055–62. 10.1200/JCO.2004.04.188 [DOI] [PubMed] [Google Scholar]
- 8. Parker WH, Feskanich D, Broder MS, Chang E, Shoupe D, Farquhar CM, Berek JS, Manson JE. Long-term mortality associated with oophorectomy compared with ovarian conservation in the nurses' health study. Obstet Gynecol 2013;121:709–16. 10.1097/AOG.0b013e3182864350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fakkert IE, Abma EM, Westrik IG, Lefrandt JD, Wolffenbuttel BHR, Oosterwijk JC, Slart RHJA, van der Veer E, de Bock GH, Mourits MJE. Bone mineral density and fractures after risk-reducing salpingo-oophorectomy in women at increased risk for breast and ovarian cancer. Eur J Cancer 2015;51:400–8. 10.1016/j.ejca.2014.11.022 [DOI] [PubMed] [Google Scholar]
- 10. Fakkert IE, van der Veer E, Abma EM, Lefrandt JD, Wolffenbuttel BHR, Oosterwijk JC, Slart RHJA, Westrik IG, de Bock GH, Mourits MJE. Elevated bone turnover markers after risk-reducing salpingo-oophorectomy in women at increased risk for breast and ovarian cancer. PLoS One 2017;12:e0169673. 10.1371/journal.pone.0169673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shuster LT, Gostout BS, Grossardt BR, Rocca WA. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause Int 2008;14:111–6. 10.1258/mi.2008.008016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rocca WA, Bower JH, Maraganore DM, Ahlskog JE, Grossardt BR, de Andrade M, Melton LJ. Increased risk of cognitive impairment or dementia in women who underwent oophorectomy before menopause. Neurology 2007;69:1074–83. 10.1212/01.wnl.0000276984.19542.e6 [DOI] [PubMed] [Google Scholar]
- 13. Gaba F, Manchanda R. Systematic review of acceptability, cardiovascular, neurological, bone health and HRT outcomes following risk reducing surgery in BRCA carriers. Best Pract Res Clin Obstet Gynaecol 2020;65:46–65. 10.1016/j.bpobgyn.2020.01.006 [DOI] [PubMed] [Google Scholar]
- 14. Gan C, Chenoy R, Chandrasekaran D, Brockbank E, Hollingworth A, Vimplis S, Lawrence AC, Jeyarajah AR, Oram D, Deo N, Saravanamuthu J, Lam SS, Faruqi A, Singh N, Manchanda R. Persistence of fimbrial tissue on the ovarian surface after salpingectomy. Am J Obstet Gynecol 2017;217:425.e1–16. 10.1016/j.ajog.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 15. Howitt BE, Hanamornroongruang S, Lin DI, Conner JE, Schulte S, Horowitz N, Crum CP, Meserve EE. Evidence for a dualistic model of high-grade serous carcinoma: BRCA mutation status, histology, and tubal intraepithelial carcinoma. Am J Surg Pathol 2015;39:287–93. 10.1097/PAS.0000000000000369 [DOI] [PubMed] [Google Scholar]
- 16. Eckert MA, Pan S, Hernandez KM, Loth RM, Andrade J, Volchenboum SL, Faber P, Montag A, Lastra R, Peter ME, Yamada SD, Lengyel E. Genomics of ovarian cancer progression reveals diverse metastatic trajectories including intraepithelial metastasis to the fallopian tube. Cancer Discov 2016;6:1342–51. 10.1158/2159-8290.CD-16-0607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gaba F, Piek J, Menon U, Manchanda R. Risk-reducing early salpingectomy and delayed oophorectomy as a two-staged alternative for primary prevention of ovarian cancer in women at increased risk: a commentary. BJOG 2019;126:831–9. 10.1111/1471-0528.15651 [DOI] [PubMed] [Google Scholar]
- 18. Arts-de Jong M, Harmsen MG, Hoogerbrugge N, Massuger LF, Hermens RP, de Hullu JA. Risk-reducing salpingectomy with delayed oophorectomy in BRCA1/2 mutation carriers: patients' and professionals' perspectives. Gynecol Oncol 2015;136:305–10. 10.1016/j.ygyno.2014.12.031 [DOI] [PubMed] [Google Scholar]
- 19. Gaba F, Blyuss O, Chandrasekaran D, Osman M, Goyal S, Gan C, Izatt L, Tripathi V, Esteban I, McNicol L, Ragupathy K, Crawford R, Evans DG, Legood R, Menon U, Manchanda R. Attitudes towards risk-reducing early salpingectomy with delayed oophorectomy for ovarian cancer prevention: a cohort study. BJOG 2020. 10.1111/1471-0528.16424. [Epub ahead of print: 16 Aug 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hallowell N. A qualitative study of the information needs of high-risk women undergoing prophylactic oophorectomy. Psychooncology 2000;9:486–95. [DOI] [PubMed] [Google Scholar]
- 21. Hallowell N, Jacobs I, Richards M, Mackay J, Gore M. Surveillance or surgery? A description of the factors that influence high risk premenopausal women's decisions about prophylactic oophorectomy. J Med Genet 2001;38:683–91. 10.1136/jmg.38.10.683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Babb SA, Swisher EM, Heller HN, Whelan AJ, Mutch DG, Herzog TJ, Rader JS. Qualitative evaluation of medical information processing needs of 60 women choosing ovarian cancer surveillance or prophylactic oophorectomy. J Genet Couns 2002;11:81–96. 10.1023/A:1014571420844 [DOI] [PubMed] [Google Scholar]
- 23. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns 2006;60:301–12. 10.1016/j.pec.2005.06.010 [DOI] [PubMed] [Google Scholar]
- 24. Finch A, Shaw P, Rosen B, Murphy J, Narod SA, Colgan TJ. Clinical and pathologic findings of prophylactic salpingo-oophorectomies in 159 BRCA1 and BRCA2 carriers. Gynecol Oncol 2006;100:58–64. 10.1016/j.ygyno.2005.06.065 [DOI] [PubMed] [Google Scholar]
- 25. Holman LL, Friedman S, Daniels MS, Sun CC, Lu KH. Acceptability of prophylactic salpingectomy with delayed oophorectomy as risk-reducing surgery among BRCA mutation carriers. Gynecol Oncol 2014;133:283–6. 10.1016/j.ygyno.2014.02.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Basu NN, Ingham S, Hodson J, Lalloo F, Bulman M, Howell A, Evans DG. Risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a 30-year semi-prospective analysis. Fam Cancer 2015;14:531–8. 10.1007/s10689-015-9825-9 [DOI] [PubMed] [Google Scholar]
- 27. Heemskerk-Gerritsen BAM, Seynaeve C, van Asperen CJ, Ausems MGEM, Collée JM, van Doorn HC, Gomez Garcia EB, Kets CM, van Leeuwen FE, Meijers-Heijboer HEJ, Mourits MJE, van Os TAM, Vasen HFA, Verhoef S, Rookus MA, Hooning MJ, Hereditary Breast and Ovarian Cancer Research Group Netherlands . Breast cancer risk after salpingo-oophorectomy in healthy BRCA1/2 mutation carriers: revisiting the evidence for risk reduction. J Natl Cancer Inst 2015;107:djv033. 10.1093/jnci/djv033 [DOI] [PubMed] [Google Scholar]
- 28. Kotsopoulos J, Huzarski T, Gronwald J, Singer CF, Moller P, Lynch HT, Armel S, Karlan B, Foulkes WD, Neuhausen SL, Senter L, Tung N, Weitzel JN, Eisen A, Metcalfe K, Eng C, Pal T, Evans G, Sun P, Lubinski J, Narod SA, The Hereditary Breast Cancer Clinical Study Group . Bilateral Oophorectomy and Breast Cancer Risk in BRCA1 and BRCA2 Mutation Carriers. J Natl Cancer Inst 2017;109. 10.1093/jnci/djw177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kotsopoulos J, Lubinski J, Lynch HT, Tung N, Armel S, Senter L, Singer CF, Fruscio R, Couch F, Weitzel JN, Karlan B, Foulkes WD, Moller P, Eisen A, Ainsworth P, Neuhausen SL, Olopade O, Sun P, Gronwald J, Narod SA, Hereditary Breast Cancer Clinical Study Group . Oophorectomy and risk of contralateral breast cancer among BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat 2019;175:443–9. 10.1007/s10549-019-05162-7 [DOI] [PubMed] [Google Scholar]
- 30. Madalinska JB, Hollenstein J, Bleiker E, van Beurden M, Valdimarsdottir HB, Massuger LF, Gaarenstroom KN, Mourits MJE, Verheijen RHM, van Dorst EBL, van der Putten H, van der Velden K, Boonstra H, Aaronson NK. Quality-Of-Life effects of prophylactic salpingo-oophorectomy versus gynecologic screening among women at increased risk of hereditary ovarian cancer. J Clin Oncol 2005;23:6890–8. 10.1200/JCO.2005.02.626 [DOI] [PubMed] [Google Scholar]
- 31. Madalinska JB, van Beurden M, Bleiker EMA, Valdimarsdottir HB, Hollenstein J, Massuger LF, Gaarenstroom KN, Mourits MJE, Verheijen RHM, van Dorst EBL, van der Putten H, van der Velden K, Boonstra H, Aaronson NK. The impact of hormone replacement therapy on menopausal symptoms in younger high-risk women after prophylactic salpingo-oophorectomy. J Clin Oncol 2006;24:3576–82. 10.1200/JCO.2005.05.1896 [DOI] [PubMed] [Google Scholar]
- 32. Harmsen MG, Arts-de Jong M, Hoogerbrugge N, Maas AHEM, Prins JB, Bulten J, Teerenstra S, Adang EMM, Piek JMJ, van Doorn HC, van Beurden M, Mourits MJE, Zweemer RP, Gaarenstroom KN, Slangen BFM, Vos MC, van Lonkhuijzen LRCW, Massuger LFAG, Hermens RPMG, de Hullu JA, salpingectomy E. Early salpingectomy (TUbectomy) with delayed oophorectomy to improve quality of life as alternative for risk-reducing salpingo-oophorectomy in BRCA1/2 mutation carriers (tuba study): a prospective non-randomised multicentre study. BMC Cancer 2015;15:593. 10.1186/s12885-015-1597-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Manchanda R, Burnell M, Abdelraheim A, Johnson M, Sharma A, Benjamin E, Brunell C, Saridogan E, Gessler S, Oram D, Side L, Rosenthal AN, Jacobs I, Menon U. Factors influencing uptake and timing of risk reducing salpingo-oophorectomy in women at risk of familial ovarian cancer: a competing risk time to event analysis. BJOG 2012;119:527–36. 10.1111/j.1471-0528.2011.03257.x [DOI] [PubMed] [Google Scholar]
- 34. Braude L, Kirsten L, Gilchrist J, Juraskova I. A systematic review of women's satisfaction and regret following risk-reducing mastectomy. Patient Educ Couns 2017;100:2182–9. 10.1016/j.pec.2017.06.032 [DOI] [PubMed] [Google Scholar]
- 35. Brown SL, Whiting D, Fielden HG, Saini P, Beesley H, Holcombe C, Holcombe S, Greenhalgh L, Fairburn L, Salmon P. Qualitative analysis of how patients decide that they want risk-reducing mastectomy, and the implications for surgeons in responding to emotionally-motivated patient requests. PLoS One 2017;12:e0178392. 10.1371/journal.pone.0178392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Howard AF, Bottorff JL, Balneaves LG, Kim-Sing C. Women's constructions of the 'right time' to consider decisions about risk-reducing mastectomy and risk-reducing oophorectomy. BMC Womens Health 2010;10:24. 10.1186/1472-6874-10-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mai PL, Piedmonte M, Han PK, Moser RP, Walker JL, Rodriguez G, Boggess J, Rutherford TJ, Zivanovic O, Cohn DE, Thigpen JT, Wenham RM, Friedlander ML, Hamilton CA, Bakkum-Gamez J, Olawaiye AB, Hensley ML, Greene MH, Huang HQ, Wenzel L. Factors associated with deciding between risk-reducing salpingo-oophorectomy and ovarian cancer screening among high-risk women enrolled in GOG-0199: an NRG Oncology/Gynecologic Oncology Group study. Gynecol Oncol 2017;145:122–9. 10.1016/j.ygyno.2017.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. NICE, Familial breast cancer . Classification and care of people at risk of familial breast cancer and management of breast cancer and related risks in people with a family history of breast cancer. In: Nice clinical guideline CG164. London, UK: National Institute for Health and Care Excellence, 2013. [Google Scholar]
- 39. Myklebust M, Gjengedal E, Strømsvik N. Experience of Norwegian female BRCA1 and BRCA2 Mutation-Carrying participants in educational support groups: a qualitative study. J Genet Couns 2016;25:1198–206. 10.1007/s10897-016-9954-9 [DOI] [PubMed] [Google Scholar]
- 40. Khadim MF, Eastwood P, Price J, Morrison P, Khan K. Multidisciplinary one-stage risk-reducing gynaecological and breast surgery with immediate reconstruction in BRCA-gene carrier women. Eur J Surg Oncol 2013;39:1346–50. 10.1016/j.ejso.2013.09.018 [DOI] [PubMed] [Google Scholar]
- 41. Hunsinger V, Marchac AC, Derder M, Hivelin M, Lecuru F, Bats A-S, Lantieri L. A new strategy for prophylactic surgery in BRCA women: combined mastectomy and laparoscopic salpingo-oophorectomy with immediate reconstruction by double DIEP flap. Ann Chir Plast Esthet 2016;61:177–82. 10.1016/j.anplas.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 42. Huber J, Muck T, Maatz P, Keck B, Enders P, Maatouk I, Ihrig A. Face-To-Face vs. online peer support groups for prostate cancer: a cross-sectional comparison study. J Cancer Surviv 2018;12:1–9. 10.1007/s11764-017-0633-0 [DOI] [PubMed] [Google Scholar]
- 43. Gold KJ, Normandin MM, Boggs ME. Are participants in face-to-face and Internet support groups the same? comparison of demographics and depression levels among women bereaved by stillbirth. Arch Womens Ment Health 2016;19:1073–8. 10.1007/s00737-016-0657-x [DOI] [PubMed] [Google Scholar]
- 44. Hu A. Reflections: the value of patient support groups. Otolaryngol Head Neck Surg 2017;156:587–8. 10.1177/0194599817697030 [DOI] [PubMed] [Google Scholar]
- 45. McCaughan E, Parahoo K, Hueter I, Northouse L, Bradbury I. Online support groups for women with breast cancer. Cochrane Database Syst Rev 2017;3. 10.1002/14651858.CD011652.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Antoniou AC, Pharoah PPD, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer 2004;91:1580–90. 10.1038/sj.bjc.6602175 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jmedgenet-2020-107501supp001.pdf (65KB, pdf)
Data Availability Statement
Data are available on reasonable request.