Abstract
Objectives
The present study aimed to demonstrate the efficacy of splash block using lidocaine to provide additional analgesia during ovariectomy in bitches. To identify an acute intraoperative nociceptive response, three clinical parameters were used: increased blood pressure, heart rate and respiratory rate.
Material and Methods
Forty healthy bitches were randomly assigned to receive 2% lidocaine (L group) topical application (splash block) on both ovaries (2 mg/kg each), or an equal volume of NaCl 0.9% at the same sites (C group). A fentanyl bolus (2 µg/kg) was administered intraoperatively in response to an increase in blood pressure, heart rate or respiratory rate during surgery (> 30% compared with the pre‐incisional values).
Results
Local lidocaine administration significantly reduced the need for supplementary fentanyl. Dogs in the L group showed greater intraoperative hemodynamic stability and lower surgical pain than those in the C group. In addition to the routine anaesthetic protocol, the local anaesthesia used in the present study was safe and caused no cardiopulmonary suppression. In addition, it significantly reduced the need for mandatory systemic or rescue analgesia.
Clinical Significance
Ovariectomy is a common surgical procedure in bitches. Analgesia during this procedure is important because intraoperative pain can cause negative effects that prevent patient recovery. This study aimed to demonstrate the analgesic efficacy of lidocaine splash block in video‐assisted ovariectomy in dogs. The results showed that splash block improved surgical analgesia during canine laparoscopic ovariectomy. Considering its relative simplicity, low cost, and safety, splash block could be used in daily clinical practice.
Keywords: laparoscopic ovariectomy, lidocaine, ovariectomy analgesia, splash block
Splash block of lidocaine to provide additional analgesia during ovariectomy in bitches. Splash block could be used in daily clinical practice
1. INTRODUCTION
Ovariectomy (OVH) is one of the most common elective surgical procedures in dogs (Gaynor & Muir, 2015, Leoci et al., 2019, Teixeira et al., 2013) and requires effective analgesia (Ansón et al., 2017, Mathews, 2000, Tranquili et al., 2007). The surgery involves both somatic and visceral pathways, resulting in extensive tissue damage (Hansen, 2005). Therefore, intraoperative analgesia is important because pain causes negative effects that prevent recovery (Cicirelli et al., 2021, Cicirelli et al., 2021, Gaynor, 1999, Gwendolyn & Carrol, 1996). Local anaesthetic drugs added to general anaesthesia may help control pain, develop multimodal analgesia, and reduce the need for rescue analgesia during surgery (Adin, 2011, Epstein, 2015). Because they can decrease intraoperative nociception, local anaesthetic drugs have been recommended in most surgical procedures by recent veterinary pain management guidelines (Epstein, 2015). The splash block has already been described by several authors (Grubb & Lobprise, 2020, Grubb & Lobprise, 2020, Wenger et al., 2005, Zilberstein et al., 2008). It consists of a lidocaine injection into the mesovarium to provide adequate analgesia during video‐assisted OVH in dogs (Zilberstein et al., 2008). Local anaesthetic drugs can completely block the transmission of pain, thus providing good analgesia and low incidence of adverse effects (Grubb & Lobprise, 2020, Grubb & Lobprise, 2020). This is in line with human studies, in which topical local anaesthesia significantly reduced intraoperative discomfort in patients who underwent OVH (Garwood et al., 2002, Zohar et al., 2001). General and local anaesthesia have been combined in a variety of veterinary surgical procedures (Taylor & Robertson, 2004). A mesovarian injection of lidocaine during standing laparoscopic OVH has been used in mares and cats to reduce pain responses during resection of the ovaries (Farstvedt & Hendrickson, 2005, Zilberstein et al., 2008). Bubalo showed minimal analgesic benefit of lidocaine in the mesovarium during OVH in dogs using an open technique (Bubalo et al., 2008). To our knowledge, the use of lidocaine in the mesovarium during canine OVH in laparoscopy has not yet been described, although it is to be expected that additional local anaesthesia confers better analgesia. In particular, arousal during painful ligation of the ovarian pedicles may be avoided, reducing the need for supplementary anaesthesia (Farstvedt & Hendrickson, 2005). The present study aimed to demonstrate the efficacy of splash block using lidocaine to provide additional analgesia during OVH in dogs.
2. MATERIALS AND METHODS
2.1. Patient selection
Forty bitches meeting the following requirements were recruited: age 1–3 years, weight 10–32 kg, no known previous pathologies, and low anaesthetic risk (American Society of Anesthesiology class 1). The patients arrived at the clinic early in the morning and returned to their owner on the same day. The day before surgery, patients underwent general pre‐operative examinations and routine blood tests (complete blood count, platelet count, total plasma proteins (TPP) and serum, creatinine, albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (FA) and urea). The 40 bitches were randomly assigned to receive either 8 mg/kg of 1% lidocaine or an equal volume of NaCl 0.9% as the splash block using StatView statistical software (JMP). Informed consent was obtained from pet owners prior to participation in the study.
2.2. Anaesthesia
All dogs were pre‐medicated 20 min before surgery using intramuscular dexmedetomidine (3 µg/kg; Dexdomitor®; Vetoquinol Italia SRL, Bertinoro, Italy) and methadone hydrochloride (0.25 mg/kg; Semfortan®; Eurovet Animal Health BV, Bladel, The Netherlands) mixed in the same syringe. When the sedative effect was achieved using sedation scale validate by Wagner (Farokhzad et al., 2021), a 24‐G intravenous catheter was inserted into the cephalic vein to start standard maintenance fluid therapy, and to allow for rapid drug administration, if necessary. This was followed by administration of 100% oxygen via a face mask using a Mapleson F circuit. Anaesthesia was induced in all dogs using intravenous propofol (Vetofol®, Esteve, Barcelona, Spain) at 5mg/kg (DS 1 mg). When anaesthesia was achieved, the patients were intubated and connected to the anaesthesia trolley using a Mapleson F respiratory circuit. Anaesthesia was maintained throughout the surgery using sevoflurane (EtSev 2,5%; SevoFlo®; Ecuphar Italia S.r.l., Milano, Italy) through the respiratory circuit. Systemic analgesia was administered as a 1 µg/kg bolus of fentanil (Fentadon®, Eurovet Animal Health BV at 50 µg/mL), followed by a maintenance dose, constant‐rate intravenous infusion of 1.5 µg/kg/h until the surgery was completed. Prior to manipulation of the ovarian pedicles, lidocaine (L group) or 0.9% NaCl (C group) was instilled onto the mesovarium using a 2.5 mL syringe (23‐G) from the side of the dog (Figure 1). Following lidocaine application, surgical manipulation was discontinued for 90 s (Zilberstein et al., 2008). The following vital parameters were monitored throughout surgery: heart rate (HR), respiratory rate, and non‐invasive blood pressure measured by pressure cuff (GE‐Datex Ohmeda Carestation 620 Anaesthesia Cart; GE‐Datex Ohmeda B 450 Monitor). In the immediate postoperative period, all bitches received subcutaneous meloxicam (Metacam; Boehringer Ingelheim Italia S.p.A.) at a dosage of 0.20 mg.
FIGURE 1.
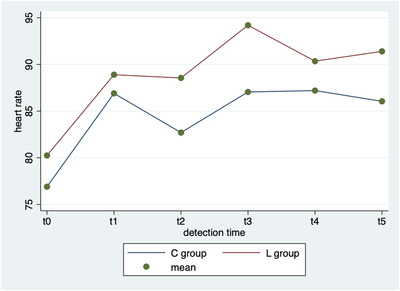
Repeated‐measures ANOVA. Average heart rate values by group (Control vs. Lidocaine) and detection time
2.3. Surgical procedure
A standardised surgical protocol was used, and the duration of all procedures was recorded. The skin at the surgical site was shaved and aseptically prepared, and the animals were placed in the dorsal decubitus position. Throughout the procedure, heat dispersion was minimised by placing the patient on an air‐heated mat (Bair Hugger model 505; 3M Italia). The first portal (8 mm) was positioned in the umbilical scar region, with an incision of approximately 0.5 cm made on the skin, subcutaneous tissue, and midline using scalpel No. 22. Pneumoperitoneum with medicinal CO2 was initiated at a speed of 1.5 L/min and with a maximum pressure of 8 mmHg for cavity inspection under guidance of a rigid endoscope of approximately 4.5 mm and 27° angulation. Under laparoscopic visualisation, the second 6‐mm portal was positioned in the midline in the pre‐pubic region. Lateralisation of the patients was promoted by rotation of the trunk to locate the ovaries. Subsequently, the uterine horn was elevated to the muscle wall using laparoscopic Kelly forceps. For fixation, an Assufil 2‐0 (Assut Europe) transparietal suture was performed. Haemostasis of both the uterine vessels and a small segment of the uterus, near the ovary, was achieved by cauterisation using 5‐mm bipolar forceps (PowerBlade Linea). A section of this structure was then occluded using 5‐mm Metzenbaum scissors. Finally, the suspended ligament of the ovary was cauterised and sectioned, allowing removal of the organ through the second portal. Both ovaries were excised in the same manner. The wounds were sutured in three planes using Assufil 2‐0 (Assut Europe). In the abdominal musculature and subcutaneous tissue, a cross‐mattress pattern was used. For dermorraphy, a simple interrupted pattern was made using an Assufil 0.
2.4. Intraoperative pain evaluation
To assess acute nociceptive response, physiological signs during surgery can be evaluated, such as increased blood pressure, HR, and respiratory rate (Farokhzad et al., 2021, Wagner et al., 2017). These parameters were registered at five time periods: grasping of the ovary (time 1), dissection of the mesosalpinx (time 2), tightening of the first loop ligature (time 3), tightening of the second loop ligature (time 4), and transection of the ovarian pedicle (time 5) by one individual who was blinded to the treatment. When one or more of these parameters exceeded pre‐incisional values by 30%, a bolus of fentanyl was administered intravenously at 2 µg/kg.
2.5. Data
Compiled forms were entered into a database created using an Excel spreadsheet, and data were analysed using Stata MP17 software.Continuous variables were described as mean (standard deviation [SD]) and range, while categorical variables were described as proportions. The skewness and kurtosis tests were used to evaluate the normality of continuous variables; all continuous variables were normally distributed. The Student's t‐test for independent data was used to compare continuous variables between groups, the ANOVA for repeated measures test was used to compare continuous variables between groups, and the Fisher's exact test was used to compare proportions. In all tests, a 2‐sided p‐value of < 0.05 was considered statistically significant.
3. RESULTS
All operations were performed by the same surgeon and the same surgical team, in full compliance with the leges artis, and lasted 45 min (SD: 6 min). The population consisted of 40 bitches: 20 (50.0%) in the C group and 20 (50.0%) in the L group. The characteristics of the population according to group are presented in Table 1.
TABLE 1.
Characteristics of the population according to group. Mean ± standard deviation and range of sample characteristics (age and weight) by Control and Lidocaine group
| Variable | C (n=20) | L (n=20) | Total (n=40) | p‐value |
|---|---|---|---|---|
| Age (months) | 23.1±8.1 (12‐36) | 22.4±8.0 (12‐36) | 22.7±8.0 (11‐16) | 0.770 |
| Weight (kg) | 24.1±7.6 (10‐36) | 24.3±7.7 (12‐33) | 24.2±7.5 (10‐36) | 0.920 |
Repeated‐measures ANOVA showed significant differences in the comparison of heart rate among different times (p < 0.0001), but not between groups (p = 0.175) or in the interaction between time and group (p = 0.683; Figure 1).
Repeated‐measures ANOVA showed a significant difference in blood pressure values among the various times (p < 0.0001), but not between groups (p = 0.149) or in the interaction between time and group (p = 0.775; Figure 2).
FIGURE 2.
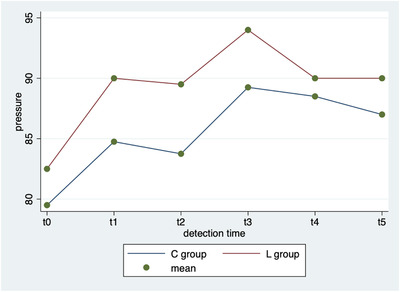
Repeated‐measures ANOVA. Average blood pressure values by group (Control vs. Lidocaine) and detection time
Repeated‐measures ANOVA showed no significant differences in respiratory rate among various times (p = 0.063), between groups (p = 0.660), or in the interaction between time and group (p = 0.675; Figure 3).
FIGURE 3.
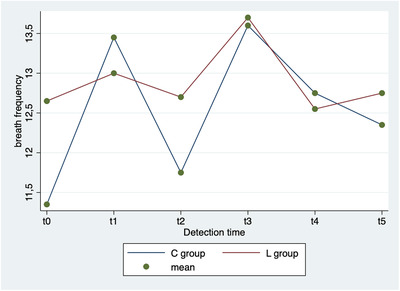
Repeated‐measures ANOVA. Average respiratory rate by group (Control vs. Lidocaine) and detection time
The proportion of dogs undergoing rescue analgesia according to group and detection time are described in Table 2.
TABLE 2.
Proportion of dogs undergoing rescue analgesia by group (Control and Lidocaine group) and detection time
| Variable | C (n=20) | L (n=20) | Total (n=40) | p‐value |
|---|---|---|---|---|
| T1 | 4 (20.0%) | 1 (5.0%) | 5 (12.5%) | 0.342 |
| T2 | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ‐ |
| T3 | 3 (15.0%) | 2 (10.0%) | 5 (12.5%) | 1.000 |
| T4 | 1 (5.0%) | 0 (0.0%) | 1 (2.5%) | 1.000 |
| T5 | 1 (5.0%) | 0 (0.0%) | 1 (2.5%) | 1.000 |
4. DISCUSSION
While laparoscopic ovariectomy has been utilized and reported by many authors to be less invasive compared to open surgical approaches (Hellyer et al., 2007), it is considered a moderately painful abdominal surgery. The present study suggested that lidocaine splash may provide intraoperative analgesia in dogs that have undergone OVH and video‐assisted OVH. Surgical pain management is better achieved using multimodal analgesia, with different drugs and techniques that target multiple sites in pain pathways (Dongaonkar et al., 2019, Hellyer et al., 2007). One simple way to deliver multimodal analgesia in OVH is local anaesthetic incorporation combined with systemic analgesic drugs (Gurney, 2012). Lidocaine is extensively used as an analgesic in veterinary medicine because it completely blocks the sensory nerve. When lidocaine is combined with general anaesthesia during surgery, it has significant analgesic benefits and an anaesthetic‐sparing effect (Lemke & Dawson, 2000). Lidocaine has a fast onset (< 2 min) and short duration of action (1–2 h), so it is very useful in ovarian manipulation (Collins et al., 2013). In addition, the correlation between physiological parameters used in this study (blood pressure, HR, and respiratory rate) and intraoperative nociception is commonly used (Gordan et al., 2015). In fact, when the sympathoadrenal system is triggered by a nociceptive stimulus, HR, respiratory rate, and blood pressure increase. Therefore, increased HR and arterial pressure may represent a response to a nociceptive stimulus during surgery (Weary et al., 2006, Zbinden et al., 1994). Our study demonstrated that splash block of lidocaine onto the ovarian ligament provides beneficial intraoperative analgesia in bitches subjected to video‐assisted OVH. We opted to exclude incisional analgesia to ensure a more specific evaluation of local anaesthesia injection into the mesovarium. Lidocaine infiltration in local tissues resolves perioperative pain; it is also simple to use, safe, and low cost (Michaloliakou et al., 1996, Oh et al., 2018). For this reason, Carpenter et al. (Carpenter et al., 2004) stated that lidocaine should be used in reproductive system surgical procedures. The combination of local and general anaesthesia reduced the need for supplementary drug doses or rescue analgesia. Anaesthetic sparing effect, compared to a control, illustrates the analgesic potential of a drug, technique, or anaesthetic protocol (Otto, 2001). Our results are in line with reports in humans, in which topical local anaesthetic significantly reduced intraoperative and postoperative discomfort in patients undergoing laparoscopic sterilisation (Garwood et al., 2002, Zohar et al., 2001). Irrigation of ovaries and their pedicles with lidocaine has been suggested during several surgical procedures in small animals (Deschamps, 2001). In terms of mechanism, the local anaesthetic likely blocks the ascending afferent input, interfering with the ion channels of the nerves. Ovaries receive sympathetic fibres from the intermesenteric and caudal mesenteric plexus, and parasympathetic fibres from the vagus nerve (Fink & Schofield, 1970). Excessive local anaesthetic absorption can cause systemic toxicity (Kip, 2007). The dose of lidocaine that produces central nervous system toxicity in dogs is 20.8 ± 4 mg/kg (Feldman et al., 1989). In the present study, the total dose of lidocaine administered was 4 mg/kg during the entire surgical procedure; therefore, it was unlikely to be associated with systemic toxicity.
5. CONCLUSIONS
The present study demonstrated that splash block using lidocaine confers satisfactory intraoperative analgesia during OVH in bitches. Considering the cost, availability, restrictions, and side effects of lidocaine, routine splash is considered desirable in bitches subjected to video‐assisted OVH.
ETHICS
The present study was performed in accordance with the ethical guidelines of the Animal Welfare Committee, and Institutional Review Board approval of the study was obtained (approval number: 02/21 [31/03/2021]). Animal procedures were performed following Directive 2010/63/EU of the European Parliament (Italian DL 26/2014).
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/vms3.637
Cicirelli, V. , Lacalandra, G. M. , & Aiudi, G. G. (2022). The effect of splash block on the need for analgesia in dogs subjected to video‐assisted ovariectomy. Veterinary Medicine and Science, 8, 104–109. 10.1002/vms3.637
All authors collaborated in the same way for the drafting of this work. Prof Aiudi supervised the team work. The authors declare that they have no competing interests.
REFERENCES
- Adin, C. A. (2011). Complications of ovariohysterectomy and orchiectomy in companion animals. Veterinary Clinics: Small Animal Practice, 41(5), 1023–1039. [DOI] [PubMed] [Google Scholar]
- Ansón, A. , Laredo, F. G. , Gil, F. , Soler, M. , Belda, E. , & Agut, A. (2017). Evaluation of an ultrasound‐guided technique for axillary brachial plexus blockade in cats. Journal of Feline Medicine and Surgery., 19(2), 146‐152. 10.1177/1098612X15618703. Epub 2016 Jul 10. PMID: 26620649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bubalo, V. , Moens, Y. P. , & Holzmann, A. (2008). Anaesthetic sparing effect of local anaesthesia of the ovarian pedicle during ovariohysterectomy in dogs. Veterinary Anaesthesia and Analgesia 35, 537–542. [DOI] [PubMed] [Google Scholar]
- Carpenter, R. E. , Wilson, D. V. , & Evans, A. T. (2004). Evaluation of intraperitoneal and incisional lidocaine or bupivacaine for analgesia following ovariohysterectomy in the dog. Veterinary Anaesthesia and Analgesia, 31(1), 46‐52. [DOI] [PubMed] [Google Scholar]
- Cicirelli, V. , Debidda, P. , Maggio, N. , Caira, M. , Mrenoshki, D. , Aiudi, G. G. , & Lacalandra, G M. (2021). Use of Spinal Anaesthesia with Anaesthetic Block of Intercostal Nerves Compared to a Continuous Infusion of Sufentanyl to Improve Analgesia in Cats Undergoing Unilateral Mastectomy. Animals, 11(3), 887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicirelli, V. , Debidda, P. , Maggio, N. , Caira, M. , Lacalandra, G. M. , & Aiudi, G G. (2021). Ultrasound‐Guided Funicular Block: Ropivacaine Injection into the Tissue around the Spermatic Cord to Improve Analgesia during Orchiectomy in Dogs. Animals, 11(5), 1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, J. B. , Song, M. D. , & Mahabir, R C. (2013). Onset and duration of intradermal mixtures of bupivacaine and lidocaine with epinephrine. The Canadian Journal of Plastic Surgery, 21(1), 51–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deschamps, J. (2001). Technique d'anesthesie locoregionale. In: Deschamps, J.Y. (Ed.), Vade´me´cum de gestion de la douleur chez le chien et le chat. Med'Com Editions, France: [Google Scholar]
- Dongaonkar, K. R. , Gulavane, S. U. , Chariar, V. M. , & Shelar, K R. (2019). Laparoscopic ovariectomy in dogs in late gestation. BMC Vet Res., 15(1), 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein, M. E. (2015). 2015–2015 AAHA/AAFP pain management guidelines for dogs and cats. Journal of the American Animal Hospital Association, 51, 67–84. [DOI] [PubMed] [Google Scholar]
- Farokhzad, B. , Sabiza, S. , Razi Jalali, M. , & Baniadam, A. (2021). Intraperitoneal administration of lidocaine or tramadol alone or in combination on postoperative pain after ovariohysterectomy in dogs. Veterinary Medicine and Science, 7(3), 634‐641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farstvedt, E. , & Hendrickson, D. , (2005). Intraoperative pain responses following intraovarian versus mesovarian injection of lidocaine in mares undergoing laparoscopic ovariectomy. Journal of American Veterinary Medical Association, 34, 646–650. [DOI] [PubMed] [Google Scholar]
- Feldman, H. S. , Arthur, G. R. , & Covino, B G. (1989). Comparative systemic toxicity on convulsant and supraconvulsant doses of intravenous ropivacaine, bupivacaine, and lidocaine in the conscious dog. Anesthesia and Analgesia, 69, 794‐801. [PubMed] [Google Scholar]
- Fink, G. , Schofield, C. (1970). Innervation of the ovary in cats. Journal of Anatomy 106(1), 191 [PubMed] [Google Scholar]
- Garwood, S. , Reeder, M. , Mackenzie, I. , & Guillebaud, J. , (2002). Tubal surface lidocaine mediates pre‐emptive analgesia in awake laparoscopic sterilization: A prospective randomized clinical trial. American Journal of Obstetrics and Gynecology, 186, 383–388 [DOI] [PubMed] [Google Scholar]
- Gaynor, J S. (1999). Is postoperative pain management important in dogs and cats? Veterinary Medicine, 3, 254‐257. [Google Scholar]
- Gaynor, J. S. , Muir, W. W. (2015). Handbook of veterinary pain management. Third edition. Missouri (USA), Elsevier. Pp. 620. [Google Scholar]
- Gordan, R. , Gwathmey, J. K. , & Xie, L ‐ H. (2015). Autonomic and endocrine control of cardiovascular function. World J Cardiol, 7, 204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubb, T. , & Lobprise, H. (2020). Local and regional anaesthesia in dogs and cats: Descriptions of specific local and regional techniques (Part 2), Veterinary Medicine and Science, 6, 2218‐234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubb, T. , & Lobprise, H. (2020). Local and regional anaesthesia in dogs and cats: Overview of concepts and drugs (Part 1), Veterinary Medicine and Science, 6(2), 209‐217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurney, M. (2012). Pharmacological options for intra‐operative and early postoperative analgesia: an update. Journal of Small Animal Practice, 53, 377–386. [DOI] [PubMed] [Google Scholar]
- Gwendolyn, L. C. , & Carrol, M. S. (1996). How to manage perioperative pain. Veterinary Medicine, 51, 353‐357. [Google Scholar]
- Hansen, B. D. Analgesia and sedation in the critically ill. (2005). Journal of Veterinary Emergency and Critical Care, 15, 285‐294. [Google Scholar]
- Hellyer, P. , Rodan, I. , & Brunt, J. (2007). AAHA/AAFP pain management guidelines for dogs and cats. Journal of Feline Medicine and Surgery, 9, 466–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kip, L. , 2007. Pain management II: local and regional anaesthetic techniques. In: Seymour, C. , Duke, T. (Eds.), BSAVA Manual of Canine and Feline Anaesthesia and Analgesia. Quedgeley, Gloucester, United Kingdom, pp. 104–114 [Google Scholar]
- Lemke, K. A. , & Dawson, S D. (2000). Local and regional anesthesia. Veterinary Clinics of North America. Small Animal Practice, 30, 839–857. [DOI] [PubMed] [Google Scholar]
- Leoci, R. , Aiudi, G. , Cicirelli, V. , Brent, L. , Iaria, C. , & Lacalandra, G. M. (2019). Effects of intratesticular vs. intraepididymal calcium chloride sterilant on testicular morphology and fertility in dogs. Theriogenology, 127, 153‐160. [DOI] [PubMed] [Google Scholar]
- Mathews, K. A. (2000). Pain assessment and general approach to management. Veterinary Clinics of North America. Small Animal Practice, 30, 729–755. [DOI] [PubMed] [Google Scholar]
- Michaloliakou, C. , Chung, F. , & Sharma, S. (1996). Preoperative multimodal analgesia facilitates recovery after ambulatory laparoscopic cholecystectomy. Anesthesia & Analgesia, 82(1), 44. [DOI] [PubMed] [Google Scholar]
- Oh, K. J. , Lee, J. Y. , Nam, E. J. , Kim, S. , Kim, Y. T. , & Kim, S. W. (2018). Periumbilical infiltration of lidocaine with epinephrine for postoperative pain reduction in single‐port laparoscopic adnexal surgery. Journal of Obstetrics and Gynecology, 1‐5. [DOI] [PubMed] [Google Scholar]
- Otto, K. (2001). Schmertztherapie bei Klein‐, first ed. Heim‐ und Versuchtieren Parey Buchverlag, Berlin. [Google Scholar]
- Taylor, P. , & Robertson, S. , (2004). Pain management in cats – past, present and future Part 1. The cat is unique. Journal of Feline Medicine and Surgery, 6, 313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira, L. R. , Luna, S. P. L. , Taffarel, M. O. , Lima, A. F. M. , Sousa, N. R. , & Joaquim, J. G. F. , (2013). PMC.FreitasComparison of intrarectal ozone, ozone administered in acupoints and meloxicam for postoperative analgesia in bitches undergoing ovariohysterectomy. Veterinary Journal., 197, 794–799. [DOI] [PubMed] [Google Scholar]
- Tranquili, W. J. , Thurmon, J. C. , & Grimm, K. A. (2007). Lumb & Jones Veterinary Anesthesia and Analgesia, Blackwell Publishing. 4th edit. Iowa, USA, p.1096. [Google Scholar]
- Wagner, M. C. , Hecker, K. G. , & Pang, D S J. (2017). Sedation levels in dogs: a validation study. BMC Vet Res., 13(1), 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weary, D. M. , Niel, L. , & Flower, F C. (2006). Identifying and preventing pain in animals. Appl Anim Behav Sci, 100, 64–76. [Google Scholar]
- Wenger, S. , Moens, Y. , Jäggin, N. , & Schatzmann, U. (2005). Evaluation of the analgesic effect of lidocaine and bupivacaine used to provide a brachial plexus block for forelimb surgery in 10 dogs. Veterinary Record, 156, 639–642. [DOI] [PubMed] [Google Scholar]
- Zbinden, A. , Petersen‐Felix, S. , & Thomson, D. (1994). Anesthetic depth defined using multiple noxious stimuli during isoflurane/oxygen anesthesia. II. Hemodynamic responses. Anesthesiology, 80, 261–267. [DOI] [PubMed] [Google Scholar]
- Zilberstein, L. F. , Moens, Y. P. , & Leterrier, E. (2008). The effect of local anaesthesia on anaesthetic requirements for feline ovariectomy. The Veterinary Journal, 178, 212–216. [DOI] [PubMed] [Google Scholar]
- Zohar, E. , Fredman, B. , Philipov, A. , Jedeikin, R. , & Shapiro, A. , (2001). The analgesic efficacy of patient‐controlled bupivacaine wound instillation after total abdominal hysterectomy whit bilateral salpingo‐oophorectomy. Anesthesia and Analgesia, 93, 482–487. [DOI] [PubMed] [Google Scholar]


