INTRODUCTION
Sepsis contributes to 1.7 million U.S. hospitalizations annually and has a 25–30% in-hospital mortality rate (1,2). Prompt management is important as hourly delays in antibiotics are associated with increased mortality (3,4). For this reason, sepsis quality improvement initiatives have focused on early recognition and treatment upon hospital presentation. However, there has been less attention to opportunities for identification and treatment in the pre-hospital setting.
Despite the current focus on early hospital care, many patients seek evaluation in other healthcare settings prior to hospital presentation. More than 45% of patients hospitalized for sepsis see a physician in the prior week (5), nearly 50% contact their primary care physician within 72 hours of admission (6), and 10–20% are seen in the outpatient setting on the day of admission (5). Yet, little is known about these outpatient visits. It remains unclear whether they represent an opportunity for earlier detection of impending sepsis, or conversely, whether they are unrelated to sepsis hospitalization and simply reflect the high burden of comorbid disease among sepsis patients.
We sought to understand the circumstances of clinic visits immediately preceding sepsis hospitalization—specifically, to measure (1) illness severity and symptoms, (2) the proportion of patients referred to the emergency department (ED) or hospital, and (3) the average time delay and change in illness severity from clinic to ED/hospital presentation.
METHODS
Setting and Cohort
Michigan Medicine (MM) is a tertiary academic center with 1,000 beds and 49,000 hospitalizations annually. We identified all adult medical and surgical hospitalizations with an ICD10 diagnosis of severe sepsis (R65.20) or septic shock (R65.21) discharged in 2017. We limited our cohort to patients with an established outpatient provider at Michigan Medicine so that outpatient visits could be examined in the electronic health record.
Chart Abstractions
Through manual chart review, we determined whether patients had a clinic visit within one calendar day of admission and then abstracted data from the clinic visit and ED/hospital presentation. Study definitions are presented in Table S2. Illness severity was measured by qSOFA score and vital sign abnormalities relative to a patient’s own baseline. Change in illness severity was measured by increasing qSOFA score or change in vitals from clinic to ED/hospital presentation (e.g. increase in heart rate by 20+ beats per minute). Time lapse from clinic to ED/hospital presentation was calculated from vital sign timestamps. Cohort demographics and comorbidities were extracted using DataDirect, a query tool for our electronic health record.
We present data as number (%), mean (SD) or median (interquartile range). All analyses were conducted using Stata/MP version 15 (College Station, TX). This study was approved by University of Michigan IRB (HUM00146288).
RESULTS
We identified 1,450 adult sepsis discharges in 2017, including 1,150 (79.3%) patients with an established outpatient provider. Of these 1,150 patients, 118 (10.3%) were seen in clinic—88 (74.6%) on day of and 30 (25.4%) on the day prior to admission. The majority (73.7%) of these visits were routine, while 26.3% were acute. Patients were a median 58 years old (IQR 49-70), majority male (61.0%) with a moderate-high comorbidity burden (median Charlson score 6, IQR 3–9) (Table 1).
Table 1:
Patient, clinic visit, and ED/hospital characteristics
| Patient Characteristics | |
|---|---|
| Age, median (IQR) | 58 (49–70) |
| Race, n (%) | |
| African American | 12 (10.2) |
| Caucasian | 95 (80.5) |
| Other | 11 (9.3) |
| Male, n (%) | 72 (61.0) |
| Comorbid conditions | |
| Chronic pulmonary disease, n (%) | 28 (23.7) |
| Diabetes, n (%) | 56 (47.5) |
| Liver disease, n (%) | 22 (18.6) |
| Metastatic cancer, n (%) | 25 (21.2) |
| Chronic kidney disease, n (%) | 32 (27.1) |
| Clinic Visit Characteristics | |
| Clinic Visit Type, n (%) | |
| Specialty care | 80 (67.8) |
| Primary care | 33 (28.0) |
| Urgent care | 5 (4.2) |
| Specialist Visits, n (%) | |
| Gastroenterology/Hepatology | 16 (13.6) |
| Hematology | 5 (4.2) |
| Oncology | 23 (19.5) |
| Physical Medicine and Rehabilitation | 5 (4.2) |
| Surgical subspecialist | 11 (9.3) |
| Other internal medical subspecialista | 16 (13.6) |
| Other specialistb | 4 (3.4) |
| Acuity of clinic visit, n (%) | |
| Acute or urgent visit | 31 (26.3) |
| Routine visit | 87 (73.7) |
| Most common symptoms documented in clinicc, n (%) | |
| Fatigue | 31 (26.3) |
| Fever | 28 (23.7) |
| Decreased oral intake | 25 (21.2) |
| Cough | 23 (19.5) |
| Shortness of breath | 21 (17.8) |
| Weakness | 18 (15.3) |
| Chills | 16 (13.6) |
| Skin edema or erythema | 15 (12.7) |
| Abdominal pain | 13 (11.0) |
| Nausea | 12 (10.2) |
| None | 23 (19.5) |
| qSOFA upon clinic presentation, n (%) | |
| qSOFA 0 | 71 (60.2) |
| qSOFA 1 | 37 (31.4) |
| qSOFA 2 | 10 (8.5) |
| qSOFA 3 | 0 (0.0) |
| Most common vital sign abnormalities documented in clinicd, n (%) | |
| Elevated heart rate | 40 (33.9) |
| Decreased systolic blood pressure | 28 (23.7) |
| Decreased diastolic blood pressure | 17 (14.4) |
| Altered mentation | 17 (14.4) |
| qSOFA abnormalities in clinic, n (%) | |
| Decreased systolic blood pressure | 35 (29.7) |
| Tachypnea | 5 (4.2) |
| Altered mentation | 18 (15.3) |
| Clinic triage decision, n (%) | |
| Refer to the ED | 64 (54.2) |
| Admit directly to the hospital | 10 (8.5) |
| Outpatient evaluation/treatment | 9 (7.6) |
| Discharge home without further evaluation/treatment | 35 (29.7) |
| ED/hospital characteristics | |
| qSOFA upon hospital presentation, n (%) | |
| qSOFA 0 | 49 (41.5) |
| qSOFA 1 | 44 (37.3) |
| qSOFA 2 | 21 (17.8) |
| qSOFA 3 | 4 (3.4) |
| Changes in illness severity from clinic to ED/hospital, n (%) | |
| Decrease in systolic blood pressure | 23 (19.5) |
| Increase in heart rate | 23 (19.5) |
| New tachynpea | 21 (17.8) |
| Newly altered mental status | 14 (11.9) |
| Decrease in diastolic blood pressure | 13 (11.0) |
| New hypoxia or oxygen requirement | 5 (4.2) |
| Length of hospital stay (days) | |
| Median | 6 |
| Mean | 9.47 |
| ICU characteristics, n (%) | |
| Admitted to an ICUe | 37 (31.4) |
| Treated with vasopressors | 19 (16.1) |
| Received mechanical ventilation | 21 (17.8) |
Other internal medicine subspecialist included Allergy, Cardiology, Endocrinology, Infectious Disease, and Sleep Medicine.
Other specialists included Dermatology, Ophthalmology, Radiation Oncology.
Additional symptoms documented in <10% of clinic visits: diarrhea, dizziness or lightheadedness, exertional dyspnea, vomiting, confusion, painful skin lesion, nasal congestion, urinary frequency, urinary urgency, flank pain, sore throat, myalgias, dysuria, purulent skin lesion, malodorous urine.
Additional vital signs abnormalities documented in <10% of clinic visits: hypoxemia or new oxygen requirement, abnormal temperature, tachypnea.
27 patients were admitted directly to an ICU, while an additional 10patients were transferred to an ICU later during hospitalization.
In clinic, most patients (65.2%) had abnormal vitals and/or a qSOFA ≥1. Specifically, 37 (31.3%) had qSOFA of 1, 10 (8.5%) had qSOFA of 2, and 59 (50%) had abnormal vitals. Of the 47 patients with an abnormal qSOFA, only 9 had an abnormal qSOFA in prior clinic visits. Symptoms of infection or sepsis were documented in 95 (80.5%) patients, most commonly fatigue (n=31, 26.3%), fever (n=28, 23.7%), and decreased oral intake (n=25, 21.2%) (Table 1). Of the 41 patients with normal vitals and qSOFA, 28 (68.3%) reported symptoms in clinic.
The majority (74, 62.7%) of patients were referred directly to the ED/hospital. Of the 44 patients not referred to the hospital/ED, 9 (7.6%) were treated in the outpatient setting, and 35 (29.7%) were sent home without intervention.
Upon arrival to the ED/hospital, 62 (52.5%) patients had worsening illness severity; 42 (35.6%) had an increased qSOFA (Figure 1), 23 (19.5%) had an increased heart rate, 23 (19.5%) had decreased systolic blood pressure, and 27 (22.9%) had worsening of multiple parameters. Illness severity worsened in 37.8% of patients instructed to present vs 77.3% not instructed to present to the ED/hospital (Figure 1).
FIGURE 1: qSOFA at Clinic and ED/hospital Presentation.
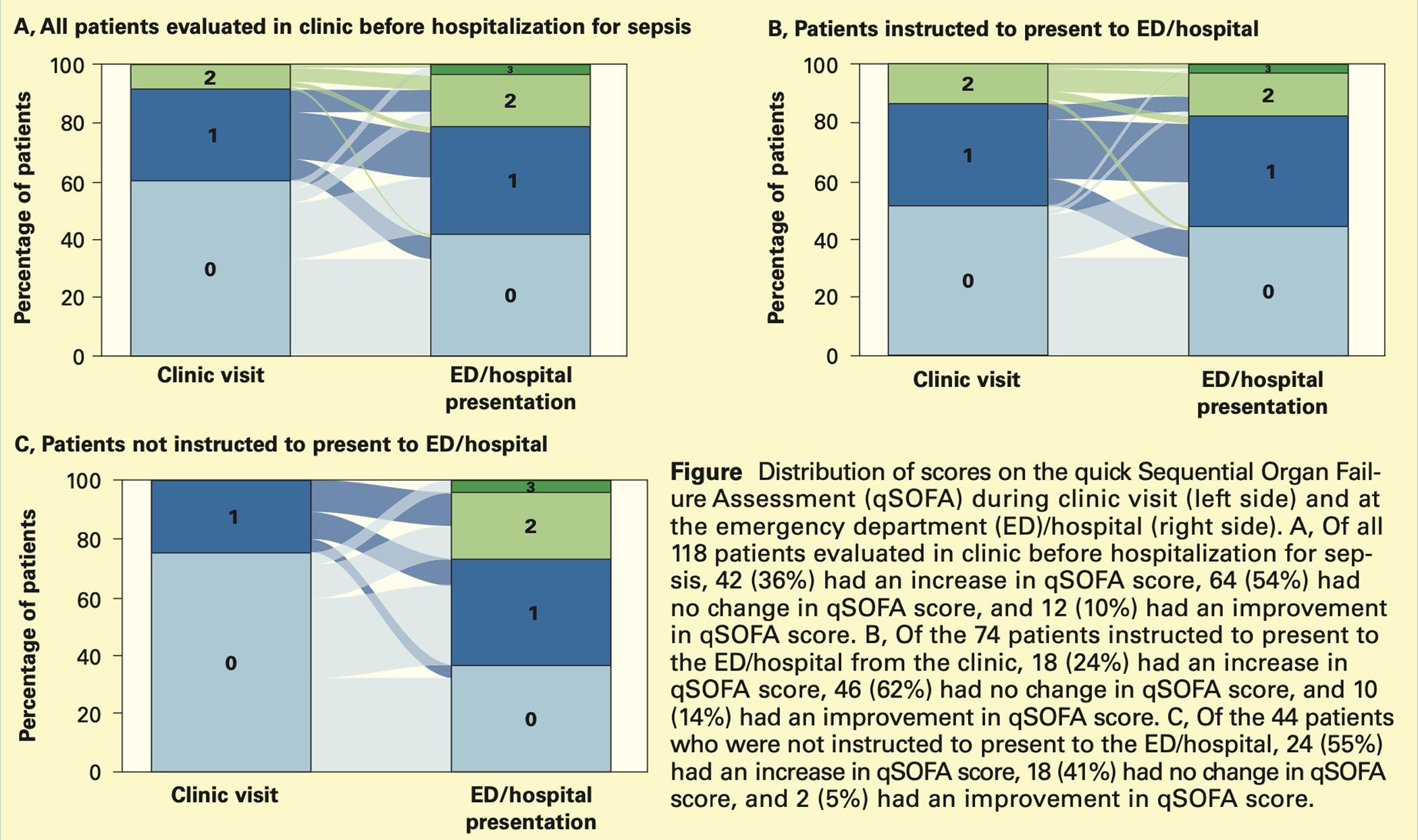
Figure 1a: Total Cohort
Figure 1b: Patients instructed to present to the ED/hospital
Figure 1c: Patients not instructed to present to the ED/hospital
This figure depicts the distribution of qSOFA scores during clinic (left column) versus ED/hospital presentation (right column). Of 118 patients evaluated in clinic prior to sepsis hospitalization, 42 (35.6%) had an increase in qSOFA, 64 (54.2%) had no change, and 12 (10.2%) had an improvement in qSOFA (1a). Of the 74 patients instructed to present to the ED/hospital from clinic, 18 (24.3%) had an increase in qSOFA, 46 (62.2%) had no change, and 10 (13.5%) had an improvement in qSOFA (1b). Of the 44 patients who were not instructed to present to the ED/hospital, 24 (54.5%) had an increase in qSOFA, 18 (40.9%) had no change in qSOFA, and 2 (4.5%) had an improvement in qSOFA (1c).
The median time lapse from clinic to ED/hospital was 3.2 hours (mean 8.3); 1.8 hours (mean 2.5) for patients instructed to present vs. 18.1 hours (mean 18.4) for patients not instructed to present. Ten (8.5%) patients died during hospitalization, of which 8 (80%) were instructed to present, and 5 (50%) had a clinic qSOFA of 0. Median time lapse for this subgroup was 1.4 hours (mean 4.2).
DISCUSSION
In this study, we found that 10% of patients hospitalized for sepsis were seen in clinic within one day of admission. In clinic, 80% had symptoms consistent with infection, and 64% had a qSOFA ≥1 or abnormal vital signs relative to his or her baseline. Most patients (63%) were referred to the ED/hospital, and over half of patients experienced worsening illness severity from clinic to ED/hospital presentation. The high burden of symptoms, abnormal vitals, and qSOFA ≥1 suggest that signs of impending sepsis were present in clinic for many patients.
Our results identify two populations that deserve attention. First, approximately one-half of patients experienced worsening illness severity over several hours between clinic and ED/hospital presentation, suggesting a trajectory of rapid deterioration requiring urgent action. These patients would benefit from an accelerated transfer and ED triage process. Second, one-third of patients had qSOFA of 0 and normal vital signs in clinic but were nonetheless hospitalized for sepsis shortly after the clinic visit. Majority of these patients reported symptoms consistent with infection, suggesting that it may still be possible to detect an increased risk for sepsis in clinic. Risk stratification algorithms incorporating non-vital sign-based features (e.g. symptoms consistent with infection, recent hospitalizations, repeated visits for unresolved symptoms) may assist physicians in identifying patients at high risk for deterioration.
Our study has several limitations. First, as a single-center study, it may not generalize to other settings. Second, mental status and respiratory rate were missing for many clinic visits. In these instances, we assumed normality, which may underestimate qSOFA in clinic and overestimate deterioration from clinic to ED/hospital. Finally, our study examined only patients who were ultimately hospitalized with sepsis.
In the future, we hope to compare our cohort to patients who were also evaluated in outpatient clinic during the same time frame, instructed to present to the ED for subjective or objective symptoms/signs concerning for infection but ultimately discharged home without admission. We hope that this will further delineate risk factors to identify those patients at highest likelihood of clinical deterioration. We anticipate that such work will contribute to the development of risk-stratification algorithms for sepsis identification in the outpatient setting.
In conclusion, 10% of patients were evaluated in clinic prior to sepsis hospitalization, the majority of whom had symptoms consistent with infection and objective evidence of illness. Potential opportunities to improve sepsis care in the outpatient setting include accelerated transfer to ED and risk-stratification algorithms that incorporate non-vital-sign based features.
Supplementary Material
Conflicts of Interest and Source of Funding:
Dr. Prescott was supported by K08 GM115859 from the National Institutes of Health; Dr Liu was supported by R35 GM128672 from the National Institutes of Health. The views in this manuscript do not reflect the position or policy of the US government or Department of Veterans Affairs.
REFERENCES
- 1.Rhee C, Dantes R, Epstein L, et al. ; CDC Prevention Epicenter Program. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA 2017;318(13):1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen J, Vincent JL, Adhikari NK, et al. Sepsis: a roadmap for future research. Lancet Infect Dis 2015;15:581–614. [DOI] [PubMed] [Google Scholar]
- 3.Seymour CW, Gesten F, Prescott HC, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 2017;376:2235–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu VX, Fielding-Singh V, Greene JD, et al. The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med 2017;196:856–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu VX, Escobar GJ, Chaudhary R, et al. Healthcare utilization and infection in the week prior to sepsis hospitalization. Crit Care Med 2018;46(4):513–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loots FJ, Smits M, van Steensel C, et al. Management of sepsis in out-of-hours primary care: a retrospective study of patients admitted to the intensive care unit. BMJ Open 2018;8:e022832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer M, Deutschman CS, Seymour CW et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315(8):801–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu V, Escobar GJ, Greene JD, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA 2014;312(1):90–92. [DOI] [PubMed] [Google Scholar]
- 9.Walkey AJ, Lagu T, Lindenauer PK. Trends in sepsis and infection sources in the United States. A population-based study. Ann Am Thorac Soc 2015;12:216–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


