Abstract
Purpose
Adolescence is characterized by dramatic physical, social, and emotional changes, making teens particularly vulnerable to the mental health effects of the COVID-19 pandemic. This longitudinal study identifies young adolescents who are most vulnerable to the psychological toll of the pandemic and provides insights to inform strategies to help adolescents cope better in times of crisis.
Methods
A data-driven approach was applied to a longitudinal, demographically diverse cohort of more than 3,000 young adolescents (11–14 years) participating in the ongoing Adolescent Brain Cognitive Development Study in the United States, including multiple prepandemic visits and three assessments during the COVID-19 pandemic (May–August 2020). We fitted machine learning models and provided a comprehensive list of predictors of psychological distress in individuals.
Results
Positive affect, stress, anxiety, and depressive symptoms were accurately detected with our classifiers. Female sex and prepandemic internalizing symptoms and sleep problems were strong predictors of psychological distress. Parent- and youth-reported pandemic-related psychosocial factors, including poorer quality and functioning of family relationships, more screen time, and witnessing discrimination in relation to the pandemic further predicted youth distress. However, better social support, regular physical activities, coping strategies, and healthy behaviors predicted better emotional well-being.
Discussion
Findings highlight the importance of social connectedness and healthy behaviors, such as sleep and physical activity, as buffering factors against the deleterious effects of the pandemic on adolescents' mental health. They also point to the need for greater attention toward coping strategies that help the most vulnerable adolescents, particularly girls and those with prepandemic psychological problems.
Keywords: Adolescents, Children, Mental-health, COVID-19, Pandemic, Sleep, Sex differences
Implications and Contribution.
Positive affect, perceived stress, anxiety, and depressive symptoms were accurately detected by a data-driven classification scheme. Findings highlight the importance of social connectedness and healthy lifestyle behaviors, such as sleep and physical activity, as buffering factors against the deleterious effects of the pandemic on adolescents' mental health.
Coronavirus disease (COVID-19) emerged in late 2019 and rapidly escalated into a global pandemic, leading to uncertainty, widespread restrictions, school and business closures, social isolation, financial loss, and drastic life changes [1]. These major stressors contributed to psychological distress in the general population [2,3], children and adolescents [4,5] (for review see [6]).
Early adolescence (11–14 years) is a sensitive period in life, characterized by dramatic cognitive and physical changes, as well as changes in social and emotional development [7], including shifts in social and emotional support from parents to peers, which leads to a greater autonomy [8]. These developmental shifts could make young adolescents vulnerable to the mental health effects of the pandemic, particularly girls, who are at increased risk for emotional problems [9]. The COVID-19 pandemic has curtailed in-person peer-to-peer social connections, in addition to inducing other stresses such as worry about health and future uncertainty, which can impact emotional wellbeing, especially for adolescents who were already at risk for experiencing emotional difficulties when the pandemic started [10]. Adverse effects of the pandemic on adolescent mental health are likely, particularly among those at high risk for developing sleep disorders or mental health problems, and in relation to dramatic pandemic-related changes, such as the rapid transition to remote learning practices, decrease in routines, and loss of in-person activities and peer relationships [11]. However, adolescents may leverage adaptive coping strategies to buffer the effect of stressors and enhance adaptation following stressful encounters [12]. Maintenance of daily routines, healthy behaviors, and engaging in social exchange are advocated to help adolescents cope with stress during the pandemic [13] but there is little research showing what behaviors are most effective. Maintaining digital social connections with peers is also encouraged; however, findings linking more digital media use with poor mental health have led to uncertainty about the positive or negative effects of specific components of screen time [14]. Most studies rely on convenience samples and cross-sectional designs [4,14] with limited longitudinal evidence of the psychological effects of the pandemic in adolescents. Recent longitudinal studies reported elevated rates of anxiety, depression, and stress among adolescents [15], especially in girls [16,17] and highlighted the risk effects of school-related concerns [17] and the importance of social connectedness (parent-child discussions and peer support) [16,17].
Here, we took advantage of the population-based, demographically, and geographically diverse Adolescent Brain Cognitive Development (ABCD) study (https://abcdstudy.org/), which has been following US youth before and during the COVID-19 pandemic. We fitted machine learning models to identify potentially modifiable psychosocial and lifestyle risk factors for psychological distress (anxiety, depression, and stress symptoms) and emotional wellbeing (represented by positive affect) during the pandemic. Machine learning tools offer a unique [18] and integrative approach to identify the independent risk and protective factors, to optimize early recognition and treatment for high-risk groups.
Methods
Participants
Data were obtained from the US-based, multisite ABCD study (21 research sites from 17 states; https://abcdstudy.org/study-sites/), that is, tracking >11,000 children, aged 9–10 years at baseline [19]. We included data from adolescents who completed the ABCD protocol (ABCD 3.0 data release) at prepandemic visits and online COVID-19 surveys [20] (May–August 2020).
ABCD data from the 3.0 data release included all participants who had completed the Year 2 assessment by February 2020 (Year 2 data from 5,500 participants were not yet available). Appendix A provides details of inclusion/exclusion criteria and Figure A1 provides an overview of the study design and measures included in the analysis.
Written informed consent and assent were obtained from a parent/guardian and the child, respectively. Procedures were approved by a centralized Institutional Review Board (University of California, San Diego, protocol number: #160091AW). Sample demographics are described in Table 1 . Compared to the full ABCD study sample at study entry, youth completing surveys during the pandemic were less likely to be Hispanic/Latino (16% vs. 20%), less likely to be Black (7% vs. 15%), more likely to be Asian (5% vs. 4%), and their parents were more likely to have higher education (e.g., having postgraduate degree 42% vs. 34%).
Table 1.
Demographics of ABCD study participants and the subset included in the current analysis
| Variable | Release 3.0 baseline data (N = 11,878) | Survey 1 (N = 3,091) | Survey 2 (N = 3,193) | Survey 3 (N = 2,934) |
|---|---|---|---|---|
| Age (years), mean (range) | 9.91 (9–11) | 12.86 (11–14) | 12.94 (11–14) | 13.05 (11–14) |
| Sex | ||||
| Female | 5,682 (47.8%) | 1,530 (49.3%) | 1,562 (48.9%) | 1,435 (48.9%) |
| Male | 6,196 (52.1%) | 1,561 (50.6%) | 1,631 (51.0%) | 1,499 (51.1%) |
| Racea | ||||
| White | 8,244 (69.4%) | 2,481 (80.2%) | 2,521 (78.9%) | 2,365 (80.6%) |
| Black | 1,895 (15.9%) | 213 (6.8%) | 267 (8.3%) | 216 (7.36%) |
| Asian | 498 (4.1%) | 170 (5.4%) | 172 (5.3%) | 168 (5.7%) |
| Multiracial/Multiethnic | 184 (1.5%) | 27 (0.8%) | 32 (1%) | 26 (0.8%) |
| Other | 852 (7.1%) | 167 (5.4%) | 168 (5.2%) | 128 (4.36%) |
| Unknown/Not reported | 205 (1.7%) | 34 (1.0%) | 33 (1.0%) | 29 (0.9%) |
| Ethnicity | ||||
| Hispanic/Latino | 2,411 (20.3%) | 512 (16.5%) | 523 (16.3%) | 457 (15.5%) |
| Not Hispanic | 9,314 (78.4%) | 2,545 (82.3%) | 2,638 (82.5%) | 2,446 (8.36%) |
| Unknown/Not reported | 143 (1.2%) | 33 (1%) | 34 (1%) | 31 (1%) |
| Parental education | ||||
| <High school diploma | 1,395 (11.7%) | 40 (1.2%) | 32 (1.0%) | 32 (1.0%) |
| High school diploma/GED | 330 (2.7%) | 174 (5.6%) | 182 (5.5%) | 160 (5.4%) |
| Some college | 3,080 (25.9%) | 615 (19.8%) | 673 (21.0%) | 587 (20.0%) |
| Bachelor's degree | 3,015 (25.3%) | 934 (30.2%) | 978 (30.6%) | 923 (31.4%) |
| Postgraduate degree | 4,044 (34.0%) | 1,325 (42.8%) | 1,323 (41.4%) | 1,230 (42.1%) |
| Unknown/not reported | 14 (0.1%) | 3 (<0.1%) | 5 (<0.1%) | 2 (<0.1%) |
ABCD = Adolescent Brain Cognitive Development; GED = General Educational Development Test.
Categories for race for the ABCD cohort were defined as in Goldstone et al. 2020.
Shelter-in-place orders were put into place by the majority of US states, starting in mid-March 2020, resulting in school and business closures. In May–August 2020 (the period of survey administration), infection/deaths due to COVID-19 and the associated economic impact persisted, although varied across regions of the United States. For a more detailed description of the COVID-19 pandemic in the period of May-August 2020, see Gold et al. [21].
Predictor variables: measures included in the models
Demographics
Sex, race, ethnicity, number of siblings, research site, educational attainment of parents/caregiver, and number of people living at the same address, reported at the prepandemic baseline year, were included. Age in months was based on the respective survey (Table 1).
Prepandemic measures
Internalizing and externalizing symptoms
From the most recent prepandemic assessment of the ABCD study (Year 2), we used parent/caregiver reports of externalizing problems (aggressive, rule-breaking behavior) from the Child Behavioral Checklist [22] and youth reports of internalizing problems (e.g., anxious, depressive) from the Achenbach System of Empirically Based Assessment Brief Problem Monitor [23].
Sleep
From the most recent ABCD assessment (Year 2), we used parent/caregiver reports of sleep disturbance (Sleep Disturbance Scale for Children [24]) with six subscales, including difficulty initiating and maintaining sleep and sleep breathing disorders. We also considered the importance of changes over time in these subscales, by including difference scores (%) between consecutive years (i.e., from Baseline to Year 1, and Year 1 to Year 2). For youth report, we used variables from the Munich Chronotype questionnaire [25] (Year 2). Variables included sleep timing, duration, sleep onset latency, sleep inertia (time taken to get out of bed) on school and free days, and chronotype-proxy.
Pandemic measures
Youth and parents were separately invited to complete three online surveys between May and August 2020, approximately 40 days apart. Surveys assessed effects of the COVID-19 pandemic on youth and their families and included >200 items across psychosocial and lifestyle domains (See Appendix B for details).
Outcome measures: pandemic mental health
In the COVID-19 survey, adolescents completed four scales about psychological distress and wellbeing (see Appendix B for details). National Institutes of Health (NIH) toolbox measures designed for those aged 8–17 years were used to assess emotional wellbeing (Survey 2: Positive affect, nine items about feelings that reflect pleasurable engagement with the environment [26]) and negative affect (Survey 1 and 3: Depressive symptoms: eight items about symptoms that are affective and cognitive indicators of depression; Survey 2: Anxiety: eight items about symptoms of anxiety and perceptions of threat) during the past week [27,28]. The 4-item Perceived Stress Scale (Survey 2: PSS) provides a brief measure of stress perceptions during the last month [29]. We developed classification models for positive affect, anxiety, and stress from Survey 2, and depressive symptoms from Survey 1 and 3 (Figure A2). For NIH toolbox batteries and scoring instructions, see https://www.healthmeasures.net/explore-measurement-systems/nih-toolbox/intro-to-nih-toolbox/emotion.
Since we assessed depressive scores at two timepoints, we also compared the potential change in the number of participants who scored above the cutoff using a McNemar chi-squared test.
Training and evaluation of classification models
Respondents with insufficient survey completion (below 65% completion rate for both youth and parent report) were removed. Using these criteria ∼20% of youth data and ∼7% of parent data were excluded (see Appendix A for more details). During the feature selection process, we removed features having missing records above 98% and dropped quasi-constant (>99%) features from the dataset. To identify redundant features and reduce collinearity among variables, we calculated the Spearman's rho (ρ) correlation matrix and identified pairs of variables with large correlation values (|ρ|>0.6). We compared these features with the outcome variable and kept in the model the feature that showed a higher correlation with the outcome.
To predict mental health risk, we used classification prediction, which requires that outcomes be classified into one of two or more classes. Outcomes were, therefore, coded into binary values where 1 represents high scores and 0 represents scores under the cutoff. Optimal thresholds were determined from the distribution of the normalized T-scores (Figure A2). T-scores are standard scores with a mean of 50 and standard deviation of 10 in the US general population. A T-score (standard score) of 60 for positive affect, depressive symptoms, and anxiety was used as a cutoff, representing one standard deviation above the mean of the US general population of adolescents [26]. For the Perceived Stress Score (PSS), the cutoff point was defined based on the distribution of the values in our sample (raw scores >10).
Model performance depends on the selection of their hyper-parameters (e.g., learning rate). To find the best-performing hyper-parameter configuration, we performed a grid search by evaluating all possible configurations in a predefined range. The aim was to obtain a model with high interpretability, therefore, keeping model complexity low. We trained regularized logistic regression (LogReg) [30] and XGBoost models (GBT) separately with several possible parameters to find the best fitting model targeting positive affect, depressive symptoms, stress, and anxiety. Extreme gradient boosting (XGBoost) is a relatively new gradient boosting implementation that has been successfully applied for the prediction of diabetes risk [31], risk of mortality from COVID-19 [32], and insomnia [33]. For model evaluation, we used area under the receiver operating characteristic curve (AUC) metrics.
For model comparison we used nested cross-validation (see Figure A3 for details). We fitted the final model on the entire dataset using the implementation in scikit-learn [34] (version 18.2) and Python 3.6.8. Results of the nested cross-validation indicated acceptable prediction performance (mean AUC ≥ 0.70) for both GBT and LogReg models (Table A1). Since we achieved higher, or roughly equal, performance using gradient boosting than with logistic regression in all four models, we chose to present the decision tree based GBT algorithm to explore feature importance, given that it is a powerful, widely recognized nonlinear tool [35] that inherently incorporates interactions among independent variables, which is appropriate here since features from the high-dimensional survey data likely interact. Furthermore, GBT has high generalization ability considering that the training data are sparse.
Feature importance in final models
We analyzed the feature importance values of the fine-tuned GBT models that we trained on the entire dataset with the best hyperparameters identified. To interpret these nonlinear models, we relied on SHapley Additive exPlanations (SHAP) values (φ) [36]. For XGBoost models, the SHAP algorithm computes the contribution of the individual variables in log odds values, providing an overall ranking of features according to their importance (mean absolute SHAP value). For the sake of interpretability, we categorized the top features into eight domains: demographics (e.g., age, sex); coping behaviors (e.g., having a regular meal time); physical activities (e.g., outdoor activities); relationships (e.g., relationship quality with friends, family); resources (e.g., unable to afford food), screen time (e.g., time spent on social media); sleep (e.g., prepandemic sleep disturbances); and other (e.g., prepandemic psychological problems).
Results
Feature importance in classification models
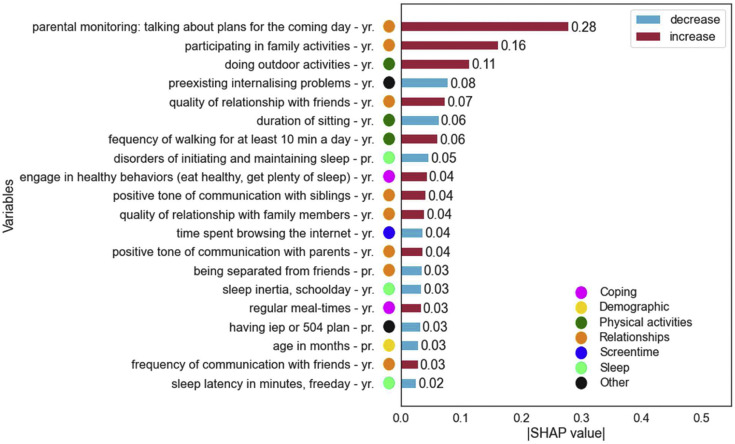
Positive affect
The final GBT model included 231 features. Figure 1 shows the top 20 features by mean absolute SHAP value for predicting positive affect during the pandemic. The top ranked variables were parent monitoring (φ = 0.28; i.e., “talking to a parent/guardian about daily plans”) and participating in family activities (φ = 0.16), followed by outdoor activities (φ = 0.11) during the pandemic. As shown, relationships with family and friends and better social support (8 of the top 20 features) are strong indicators for adolescents' positive affect in the pandemic. Additionally, healthy behaviors during the pandemic (more physical activities, less screen time), and younger age predicted high positive affect. Of note, having an Individualized Education Program or 504 plan, more prepandemic sleep problems, and higher pre-existing internalizing symptoms were associated with lower positive affect.
Figure 1.
Feature importance of the GBT model trained to predict positive affect in young adolescents during the pandemic (n = 2,896). Top 20 features are sorted by mean absolute SHAP value. The color of the bars represents the direction of the effect (red: higher values associated with higher SHAP scores). In variable names, “yr” = youth report; “pr” = parent report.
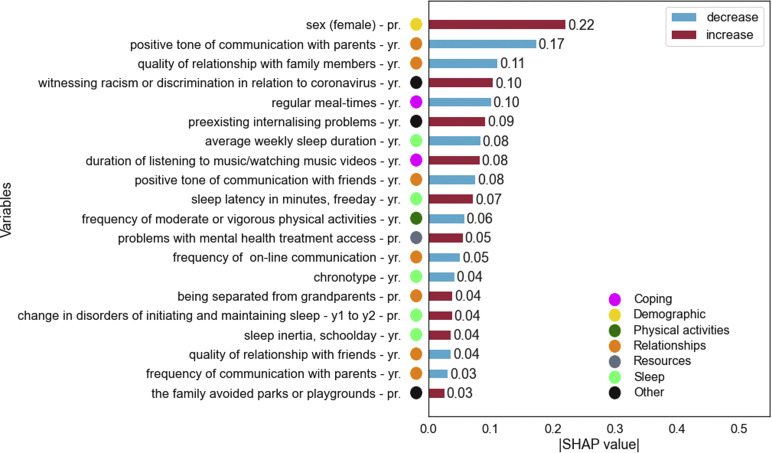
Perceived stress
The final GBT model included 228 features. Figure 2 shows the top 20 features by mean absolute SHAP value for predicting stress during the pandemic. Sex was the most important predictor (φ = 0.22), showing that girls were more likely than boys to have high stress levels in the pandemic. Variables reflecting relationships (7 of the top ranked variables) and prepandemic sleep problems were again strong predictors. Other important features were “witnessing discrimination in relation to coronavirus” (φ = 0.10), not having “regular meal times' (φ = 0.10), and pre-existing internalizing problems (φ = 0.09).
Figure 2.
Feature importance of the GBT model trained to predict stress in young adolescents during the pandemic (n = 3,193). Top 20 features are sorted by mean absolute SHAP value. The color of the bars represents the direction of the effect (red: higher values associated with higher SHAP scores). In variable names, “yr” = youth report; “pr” = parent report.
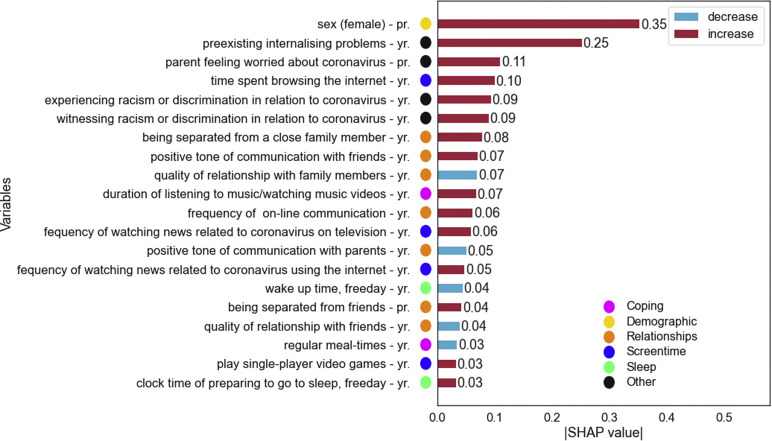
Anxiety
The final GBT model included 228 predictor variables. Figure 3 shows the top 20 features by mean absolute SHAP value for predicting anxiety during the pandemic. The top ranked variables were sex (φ = 0.35) and pre-existing internalizing problems (φ = 0.25), followed by “parent worry about coronavirus” (φ = 0.11). Relationship variables were important, with better quality family relationships and more positive tone of communication with family predicting less anxiety. Counterintuitively, more positive tone of communication with friends was associated with anxiety. Several screen time variables appeared in the top predictors of anxiety, with higher frequency of “watching news related to coronavirus,” more time “playing single-player video games,” or “browsing the internet,” predicting anxiety.
Figure 3.
Feature importance of the GBT model trained to predict anxiety in young adolescents during the pandemic (n = 3,193). Top 20 features are sorted by mean absolute SHAP value. The color of the bars represents the direction of the effect (red: higher values associated with higher SHAP scores). In variable names, “yr” = youth report; “pr” = parent report.
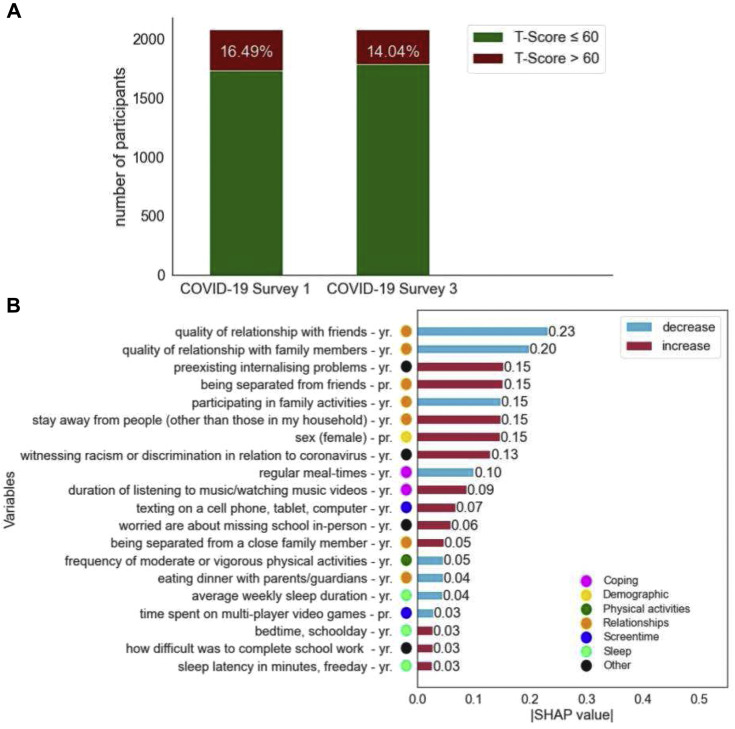
Depressive symptoms
The number of participants showing depressive symptom scores above the cutoff point decreased (N = 2,080, χ2(1) = 9.803, p = .001) from May (16.49%) to August (14.04%) 2020 (Figure 4 A).
Figure 4.
(A) Differences in the number and percentage of participants who exceeded the cutoff for high depressive symptoms (standard T-Score > 60) at COVID-19 Survey 1 and COVID-19 Survey 3. (B) Feature importance of the GBT model trained to predict depressive symptoms based on the dataset from Survey 1 (n = 3,063) in young adolescents during the pandemic. Top 20 features are sorted by mean absolute SHAP value. The color of the bars represents the direction of the effect (red: higher values associated with higher SHAP scores). In variable names, “yr” = youth report; “pr” = parent report.
The final GBT model using predictors and depressive score from Survey 1 included 240 features. Figure 4B shows the top 20 features by mean absolute SHAP value. The final model based on data from Survey 3 (see Supplementary Figure A4) included 223 features.
Predictive features largely overlapped between the two timepoints. Female sex, pre-existing internalizing problems, and “witnessing racism due to coronavirus,” not having “regular meal times,” and “listening to music” during the pandemic were in the top features associated with depressive symptoms at both timepoints. Family and peer relationships, during the pandemic and prepandemic sleep indicators were also in the top 20 features for both. On the other hand, school-related predictors (“worried about missing school in person,” “how easy or difficult it was to complete school work”) ranked high only in Survey 1 (May 2020).
Discussion
A broad analysis of psychosocial and lifestyle factors in the longitudinal ABCD study of adolescents in the United States found that social connectedness and family relationships were among the strongest predictors of emotional wellbeing in adolescents during the COVID 19 pandemic. Importantly, our data consistently showed girls were at higher risk for the negative effects of the pandemic on mental health. Also, adolescents who entered the pandemic having pre-existing internalizing symptoms and sleep problems were more vulnerable to psychological distress. Results suggest that increased physical activity, maintaining routines, and taking breaks from news stories—all predictors of emotional wellbeing during the pandemic, but also modifiable lifestyle factors—could be targets for prevention of mental health problems in youth during a major life stress, like a pandemic.
The prediction models for stress, anxiety, and depression identified sex as an important feature, with girls being more likely to experience psychological distress during the pandemic. Results support emerging studies, including in adolescents [16], showing greater vulnerability of the female sex to psychological distress during the pandemic [4,15,16]. Mental health problems are more prevalent in girls, with this sex difference emerging after puberty [9]. We did not examine predictors of psychological distress separately for boys and girls; however, others have shown that women are more sensitive than men to the depressogenic effects of low levels of social support [37]. Possibly, girls may be more affected by social isolation (particularly from peers) imposed by the pandemic.
Pre-existing internalizing symptoms strongly predicted psychological distress during the pandemic, which could reflect persistence of internalizing symptoms over time [38] and increased vulnerability of adolescents with these symptoms to pandemic-related stressors. Adolescents with mental health problems are less likely to tolerate lockdown and may have disruption to psychological services [13].
A concerning finding was that experiencing or witnessing discrimination in relation to COVID-19 disease predicted stress, anxiety, and depression. Others reported that Black and Asian Americans are vulnerable to COVID-19 racial discrimination, which was associated with poorer mental health in youth [39]. From our analysis we did not identify the context of discrimination, and work is needed to explore this relationship further. Public health and educational strategies are needed to decrease stigmatization of, and discrimination against, vulnerable groups. Multiple indicators of social connectedness with family and friends, including quality of relationships, more family activities, and less isolation from friends, were associated with better mental health, underscoring the social-emotional benefit of turning to one's family and friends to cope with stress. Although prediction does not indicate causality, the results here are in line with other studies showing that adolescents with high levels of social connection during COVID-19 had fewer depressive symptoms and anxiety [16], and prior research linking social connectedness with adolescent well-being [40]. Although peer social connections have been dramatically curtailed in the pandemic, companionship in the family context may protect adolescents' mental health [14].
Screen time variables were important predictors of anxiety and depression: greater consumption of pandemic-related news predicted anxiety, supporting ample evidence linking disaster-related media exposure, and negative outcomes in youth [41]. Connecting digitally and screen time use predicted anxiety and depression, similar to findings of others [4], although digital connections have also been associated with reduced loneliness [14]. Although interactions online can mimic in-person dynamics, they might also bring increased risk of ostracism, amplification of existing interpersonal struggles, or excessive rumination on negative emotions, which could increase depression [14]. On the other hand, screen time activities might reflect coping or seeking social support for those with depression (for review see [42]). Similarly, greater time spent listening to music/watching music videos could reflect coping in those with mental health symptoms. As emphasized elsewhere [14,43], mindful use of supportive virtual interactions with peers can enhance adolescent socialization during times of reduced physical peer-to-peer connections.
Pre-existing sleep problems predicted greater psychological distress in adolescents during the pandemic. There is a bidirectional relationship between sleep and mood, although sleep disturbances more often preceded depression than the reverse [44], supporting sleep as a modifiable target to reduce risk for poor mental health [45], including during stressful times like the pandemic. We also found that getting plenty of sleep, having regular meal times, and engaging in healthy behaviors during the pandemic, such as physical or outdoor activities, had a protective role for adolescent mental health. These data provide evidence of the benefits of routines, especially maintaining healthy sleep habits, which have been recommended as ways for adolescents to cope with stress and potentially prevent mood disorders during the pandemic [13]. While few prior studies examined the importance of prepandemic sleep health for psychological wellbeing during the pandemic, others reported found that in adolescents, parent-reported difficulty initiating/maintaining sleep increased, and sleep/wake behaviors became more delayed, compared to before the pandemic, with these effects associated with more sadness/loneliness and COVID-19-related worries/fears, respectively [46]. Adolescents in that study also reported less daytime sleepiness and longer school-night sleep duration during, compared to before, the pandemic, reflecting some positive changes in sleep [46].
Strengths of the current analysis lie in the ABCD study dataset, from participants across 21 sites in the United States, which contributes to the robustness of results, reducing the possibility that county-specific restrictions, health care resources, or differences in educational systems might impact our findings. However, generalizability is limited by the fact that the sample is not necessarily representative of the US population, and we only included a subsample here who had sufficient data from the prepandemic ABCD assessments and COVID-19 surveys. Results therefore need to be interpreted with caution. Second, participants self-reported their mental health during a period characterized by a quickly changing environment. Our results do not reveal the causal relationship between the predictors and youth's mental health, or the temporal relationship between predictors and the outcomes that were assessed cross-sectionally. We showed a reduction in risk of depressive symptoms from the first to the third assessment during the pandemic but further studies are needed to track longer term changes in mental health of this group across the course of the pandemic and into the future.
We provided a comprehensive list of independent predictors for each model; however, low variable importance for other factors does not necessarily imply that they are weakly related to the outcome, just that they do not contribute to outcome prediction given all the other variables in the simultaneous model. Furthermore, in their current form, our prediction models do not identify the root cause of mental health outcomes and do not test the causal relationships; some predictors might reflect coping or behavior induced by the outcome variable.
America's youth, especially those entering the pandemic with pre-existing mental health problems, as well as girls, are particularly vulnerable to the psychological impact of the COVID-19 pandemic. To limit the long-term adverse consequences of the pandemic, it is important that all adolescents receive regular and convenient access to mental health care or social/community-based support programs. Although cognitive behavioral therapies are the first-line treatment for mental health disorders, they are limited in availability and affordability, and adolescents with subclinical symptoms, in particular, may benefit from alternative services such as telehealth. In addition, it is critical to raise awareness of the potential psychological long-term sequelae of the COVID-19 pandemic among at-risk populations. Although social ties may serve as protective factors for maintaining stable mental wellbeing during the pandemic, modifiable lifestyle-related factors such as sleep may be the first approach to improving adolescents' psychological wellness, for example, by promoting regular sleep routines with educational programs. Collaborative work among scientists, governments, communities, and clinicians can help provide adolescents and their families with the tools and support to better cope with major life crises such as pandemics, environmental stressors (e.g., natural disasters), or other sources of global trauma.
Acknowledgments
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development℠ (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from: The ABCD data used in this report came from the ABCD 3.0 data release (https://doi.org/10.15154/1519007) and the ABCD COVID-19 Survey First Data Release (https://doi.org/10.15154/1520584). DOIs can be found at https://nda.nih.gov/study.html?id=901 and https://nda.nih.gov/study.html?&id=1041. Dr. Gayathri Dowling was substantially involved in all of the cited grants consistent with her role as Scientific Officer. The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
This study also benefited from Stanford Institute for Human-Centered AI (HAI) AWS Cloud Credit.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2021.11.023.
Author Contributions
O.K. cleaned and analyzed the data, constructed the figures, and wrote the first draft of the manuscript. Conception and design of experiments and analysis: F.C.B., O.K., E.A., D.Y., K.M.P., M.Z., E.M.M., W.E.P., C.J.M., M.R.G., S.A.B., N.E.W., A.T.M., E.R.S., F.J.B., K.M.L., A.S.D., C.S.S., B.D.M., M.J.G., A.M.V.R., G.J.D., S.F.T. Recruitment, data collection: D.P., I.D. All authors contributed data, critically reviewed the manuscript, and approved the final manuscript for submission.
Funding Sources
The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript. The corresponding author had full access to all the data and had the final responsibility for the decision to submit for publication. The codes used for the data analysis are available from the corresponding author upon reasonable request.
Supplementary data
References
- 1.Liu C.H., Doan S.N. Psychosocial stress contagion in children and families during the COVID-19 pandemic. Clin Pediatr (Phila) 2020;59:853–855. doi: 10.1177/0009922820927044. [DOI] [PubMed] [Google Scholar]
- 2.Alzueta E., Perrin P., Baker F.C., et al. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J Clin Psychol. 2020;77:556–570. doi: 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- 3.Yuksel D., McKee G.B., Perrin P.B., et al. Sleeping when the world locks down: Correlates of sleep health during the COVID-19 pandemic across 59 countries. Sleep Health. 2021;7:134–142. doi: 10.1016/j.sleh.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Omari O., Al Sabei S., Al Rawajfah O., et al. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: An online cross-sectional multicountry study. Depress Res Treat. 2020;2020:8887727. doi: 10.1155/2020/8887727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gotlib I.H., Borchers L.R., Chahal R., et al. Early life stress predicts depressive symptoms in adolescents during the COVID-19 pandemic: The mediating role of perceived stress. Front Psychol. 2021;11:3864. doi: 10.3389/fpsyg.2020.603748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiao W.Y., Wang L.N., Liu J., et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinberg L. Cognitive and affective development in adolescence. Trends Cogn Sci. 2005;9:69–74. doi: 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Steinberg L., Morris A.S. Adolescent development. Annu Rev Psychol. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 9.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 10.Chahal R., Kirshenbaum J.S., Miller J.G., et al. Higher executive control network coherence buffers against puberty-related increases in internalizing symptoms during the COVID-19 pandemic. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:79–88. doi: 10.1016/j.bpsc.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becker S.P., Gregory A.M. Editorial Perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. J Child Psychol Psychiatry. 2020;61:757–759. doi: 10.1111/jcpp.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suldo S.M., Shaunessy E., Hardesty R. Relationships among stress, coping, and mental health in high-achieving high school students. Psychol Schools. 2008;45:273–290. [Google Scholar]
- 13.Guessoum S.B., Lachal J., Radjack R., et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52:177–187. [Google Scholar]
- 15.Mayne S.L., Hannan C., Davis M., et al. COVID-19 and adolescent depression and suicide risk screening outcomes. Pediatrics. 2021;148 doi: 10.1542/peds.2021-051507. e2021051507. [DOI] [PubMed] [Google Scholar]
- 16.Magson N.R., Freeman J.Y.A., Rapee R.M., et al. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hawes M.T., Szenczy A.K., Klein D.N., et al. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2021:1–9. doi: 10.1017/S0033291720005358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orrù G., Monaro M., Conversano C., et al. Machine learning in psychometrics and psychological research. Front Psychol. 2020;10:2970. doi: 10.3389/fpsyg.2019.02970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garavan H., Bartsch H., Conway K., et al. Recruiting the ABCD sample: Design considerations and procedures. Developmental Cogn Neurosci. 2018;32:16–22. doi: 10.1016/j.dcn.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dataset: COVID rapid response research (RRR) survey first data release. Edition: The ABCD Consortium; 2020. NIMH Data Archive, Available at: https://nda.nih.gov/edit_collection.html?id=2573&tab=Associated%20Studies. Accessed December 30, 2021. [Google Scholar]
- 21.Gold J.A., Rossen L.M., Ahmad F.B., et al. Race, ethnicity, and age trends in persons who died from COVID-19—United States, May–August 2020. Morbidity Mortality Weekly Rep. 2020;69:1517. doi: 10.15585/mmwr.mm6942e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Achenbach T.M. In: Encyclopedia of Clinical Neuropsychology. Kreutzer J.S., DeLuca J., Caplan B., editors. Springer; New York, NY: 2011. Child behavior checklist; pp. 546–552. [Google Scholar]
- 23.Piper B.J., Gray H.M., Raber J., et al. Reliability and validity of brief problem monitor, an abbreviated form of the child behavior checklist. Psychiatry Clin Neurosci. 2014;68:759–767. doi: 10.1111/pcn.12188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bruni O., Ottaviano S., Guidetti V., et al. The Sleep Disturbance Scale for Children (SDSC) construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–261. doi: 10.1111/j.1365-2869.1996.00251.x. [DOI] [PubMed] [Google Scholar]
- 25.Roenneberg T., Wirz-Justice A., Merrow M. Life between clocks: Daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18:80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 26.Gershon R.C., Wagster M.V., Hendrie H.C., et al. NIH toolbox for assessment of neurological and behavioral function. Neurology. 2013;80:S2–S6. doi: 10.1212/WNL.0b013e3182872e5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irwin D.E., Stucky B., Langer M.M., et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res. 2010;19:595–607. doi: 10.1007/s11136-010-9619-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quinn H., Thissen D., Liu Y., et al. Using item response theory to enrich and expand the PROMIS pediatric self report banks. Health Qual Life Outcomes. 2014;12:160. doi: 10.1186/s12955-014-0160-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 30.Mohammadi F., Pourzamani H., Karimi H., et al. Artificial neural network and logistic regression modelling to characterize COVID-19 infected patients in local areas of Iran. Biomed J. 2021;44:304–316. doi: 10.1016/j.bj.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang L., Wang X., Chen A., et al. Prediction of type 2 diabetes risk and its effect evaluation based on the XGBoost model. Healthcare (Basel) 2020;8:247. doi: 10.3390/healthcare8030247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Domínguez-Olmedo J.L., Gragera-Martínez Á., Mata J., et al. Machine learning applied to clinical laboratory data in Spain for COVID-19 outcome prediction: Model development and validation. J Med Internet Res. 2021;23:e26211. doi: 10.2196/26211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ge F., Zhang D., Wu L., et al. Predicting psychological state among Chinese undergraduate students in the COVID-19 epidemic: A longitudinal study using a machine learning. Neuropsychiatr Dis Treat. 2020;16:2111–2118. doi: 10.2147/NDT.S262004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pedregosa F., Varoquaux G., Gramfort A., et al. Scikit-learn: Machine learning in Python. J Mach Learn Res. 2011;12:2825–2830. [Google Scholar]
- 35.Chen T., Guestrin C. Association for Computing Machinery; San Francisco, California, USA: 2016. XGBoost: A scalable tree boosting system. Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining; pp. 785–794. [Google Scholar]
- 36.Lundberg S.M., Erion G., Chen H., et al. From local explanations to global understanding with explainable AI for trees. Nat Mach Intel. 2020;2:56–67. doi: 10.1038/s42256-019-0138-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kendler K.S., Myers J., Prescott C.A. Sex differences in the relationship between social support and risk for major depression: A longitudinal study of opposite-sex twin pairs. Am J Psychiatry. 2005;162:250–256. doi: 10.1176/appi.ajp.162.2.250. [DOI] [PubMed] [Google Scholar]
- 38.Goldstone A., Javitz H.S., Claudatos S.A., et al. Sleep disturbance predicts depression symptoms in early adolescence: Initial findings from the adolescent brain cognitive development study. J Adolesc Health. 2020;66:567–574. doi: 10.1016/j.jadohealth.2019.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheah C.S.L., Wang C., Ren H., et al. COVID-19 racism and mental health in Chinese American families. Pediatrics. 2020;146 doi: 10.1542/peds.2020-021816. [DOI] [PubMed] [Google Scholar]
- 40.Stavrova O., Luhmann M. Social connectedness as a source and consequence of meaning in life. J Positive Psychol. 2016;11:470–479. [Google Scholar]
- 41.Comer J.S., DeSerisy M., Greif Green J. Caregiver-reports of internet exposure and posttraumatic stress among Boston-area youth following the 2013 marathon bombing. Evid Based Pract Child Adolesc Ment Health. 2016;1:86–102. doi: 10.1080/23794925.2016.1203737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keles B., McCrae N., Grealish A. A systematic review: The influence of social media on depression, anxiety and psychological distress in adolescents. Int J Adolesc Youth. 2020;25:79–93. [Google Scholar]
- 43.Nagata J.M., Abdel Magid H.S., Pettee Gabriel K. Screen time for children and adolescents during the coronavirus disease 2019 pandemic. Obesity. 2020;28:1582–1583. doi: 10.1002/oby.22917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lovato N., Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Med Rev. 2014;18:521–529. doi: 10.1016/j.smrv.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 45.Blake M.J., Allen N.B. Prevention of internalizing disorders and suicide via adolescent sleep interventions. Curr Opin Psychol. 2020;34:37–42. doi: 10.1016/j.copsyc.2019.08.027. [DOI] [PubMed] [Google Scholar]
- 46.Becker S.P., Dvorsky M.R., Breaux R., et al. Prospective examination of adolescent sleep patterns and behaviors before and during COVID-19. Sleep. 2021:44. doi: 10.1093/sleep/zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.