Abstract
Background
Most older adults do not meet recommended guidelines for physical activity. Referrals from physical therapists (PTs) to community- and evidence-based physical-activity programs like Enhance®Fitness have potential to address this gap. We tested an intervention intended to increase referrals of older adults to Enhance®Fitness programs offered at YMCAs.
Materials and methods
We developed a capacity-building intervention that included a structured toolkit and technical-assistance calls. From April 2016 to September 2018, using stratified randomization, we conducted a trial with 20 YMCA Associations randomized into intervention and control arms. The primary outcome was the number of new Enhance®Fitness enrollees during the trial period. Using both quantitative and qualitative methods, we also conducted process and intermediate-outcome evaluations to assess intervention implementation and Association outreach activities, barriers, and facilitators.
Results
The intervention was implemented as intended, but PT outreach was similar for both intervention and control YMCA Associations. The intervention arm had similar enrollment (1695 new enrollees) to the control arm (1326 new enrollees; 95% confidence interval, −47%–199%, P = 0.61). Interviews revealed that barriers, including lack of staff and time for outreach, limited capacity for Enhance®Fitness program growth, and competing priorities, outweighed facilitators, including existing partnerships, presence of an outreach team, senior leadership support, and infrastructure for referrals.
Conclusions
YMCA Associations in the intervention arm were unable to increase their outreach to PTs and enrollment in Enhance®Fitness. Our evaluation findings indicate that community organizations that prioritize program growth, have support at all organizational levels, and allocate staff and time for outreach and partnership development may be more successful in creating sustainable linkages with clinical partners and increasing evidence-based-program reach.
Keywords: Aged, Capacity building, Exercise, Physical therapists, Random allocation, Referral and consultation
Highlights
-
•
Physical therapists (PTs) may help older adults increase their physical activity by referring them to physical-activity programs.
-
•
In a randomized trial, we helped YMCA Associations build capacity to increase referrals by PTs of older adults to YMCA Enhance®Fitness programs.
-
•
The YMCA Associations encountered barriers and were unable to increase PT outreach and Enhance®Fitness enrollment.
-
•
We did, however, identify facilitators that may help community organizations create linkages with clinical partners and increase program reach.
-
•
Facilitators include prioritizing program growth, having senior-leadership support, and setting aside staff and time for outreach.
List of abbreviations
- CCL
community-clinical linkage
- CEO
chief executive officer
- EF
Enhance®Fitness
- ODES
Online Data Entry System
- PA
physical activity
- PT
physical therapist
- PT-REFER
Physical Therapists–Recommending Enhance®Fitness to Expand Reach
- RCT
randomized, controlled trial
- REDCap
Research Electronic Data Capture system
- UW
University of Washington
- YMCA
Young Men's Christian Association
- Y-USA
YMCA of the USA
1. Trial registration
The trial was registered on ClinicalTrials.gov on May 4.2017 and received registry number NCT03139461.
2. Background
Most adults aged 65 years and older do not meet recommended physical activity (PA) guidelines [1]. Previous studies have found that medical-provider support and encouragement can increase PA participation among older adults [[2], [3], [4], [5]]. These studies have mostly focused on primary care physicians; less is known about other provider types such as physical therapists (PTs). PTs work with patients to improve their mobility and fitness, are trained on how to increase PA among patients to improve health [6], and have been described as “ideally placed” to promote population health and well-being through PA [7].
Given this role, clinical-community linkages (CCL) that connect PTs with community-based organizations offering evidence-based PA programming are a promising approach to increasing older-adult reach, defined as “the absolute number, proportion, and representativeness of individuals who are willing to participate in a given initiative, intervention, or program” [8]. CCLs are partnerships between the clinical and community sectors to improve population health [9]. CCLs have the potential to better support patient care [9] and increase healthy behaviors such as PA [10] by providing patients a continuum of care connected to resources in their communities. CCLs can also address known barriers to older adult PA such as pain, cost, lack of transportation, and lack of interest [11], as well as lack of awareness of available and suitable programs [12].
We report here the outcomes of the Physical Therapists–Recommending Enhance®Fitness to Expand Reach (PT-REFER) trial, testing a capacity-building intervention with Young Men's Christian Association (YMCA) Associations (hereafter referred to as Associations) to form CCLs with physical-therapy clinics, thereby increasing PT referrals to Enhance®Fitness (EF). EF is an evidence-based PA program designed for older adults and delivered by Associations and other community organizations across the country [[13], [14], [15]]. We hypothesized that implementing the intervention would lead to increased older adult enrollment in EF compared to usual delivery of EF. Specifically, we hypothesized that Associations receiving the intervention would increase their time on, and their effectiveness with, outreach to PTs, and these PTs would then refer their older-adult clients to EF. Results may inform future efforts to develop capacity, create sustainable CCLs, and increase the reach of evidence-based programs.
3. Materials and Methods
We present an overview of study methods, including a description of the intervention, study measures, and data-analysis plan. We follow CONSORT guidelines for reporting and have provided a checklist in an “additional file” [16]. A more detailed description of the methods was published separately [17]. The University of Washington (UW) Institutional Review Board approved all protocols for this study. The clinical-trial registry number is NCT03139461.
3.1. Study design
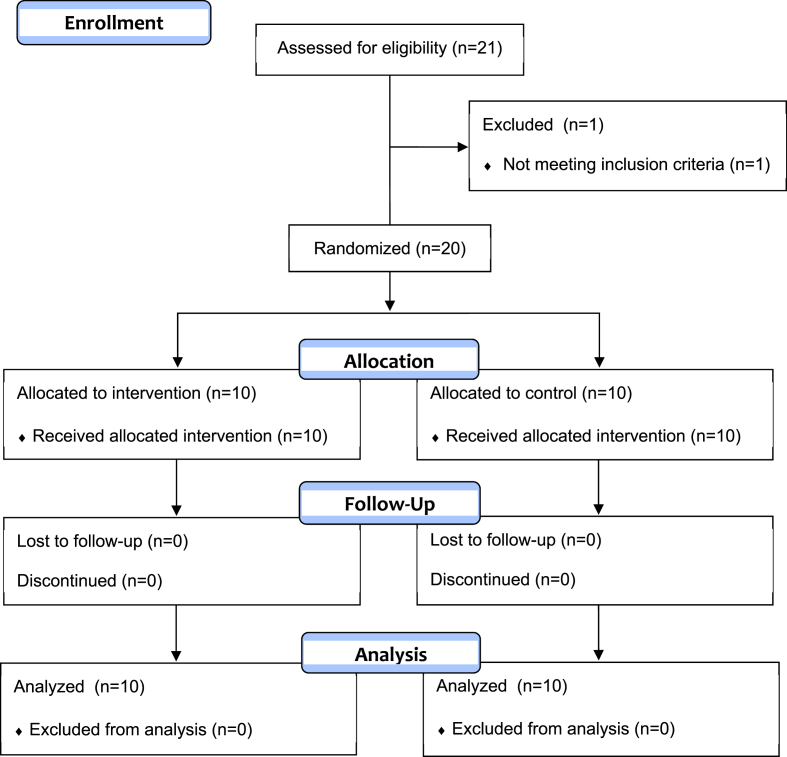
We conducted a two-arm, randomized, controlled trial (RCT). Our sample included 20 Associations from 13 states across the country (Fig. 1, Appendix X). Associations were the unit of randomization because each Association is an independent 501(c)(3) organization that serves a metropolitan or small-city area. These areas correspond well to the service areas of medical providers. Stratified randomization was used to reduce the chance of imbalance between treatment arms [18].We sorted the Associations in decreasing order of predicted EF enrollment, which we calculated based on EF enrollment in the year preceding the trial, March 2015 to February 2016. We then created 10 consecutive pairs of Associations (strata), and randomized the two Associations in each stratum to treatment and control conditions in a 1:1 ratio. We co-designed the study with staff of the YMCA of the USA (Y-USA), the national resource office of YMCAs. For example, Y-USA chose to focus outreach on PTs, as opposed to primary-care providers. The Associations in the intervention arm received the capacity-building intervention detailed below. The Associations in the control arm conducted their operations as usual, and had access to EF-related resources that were available to any YMCA Association delivering the program.
Fig. 1.
CONSORT flow diagram, PT-REFER randomized trial, April 2016 to September 2018.
The research team employed a limited blinding approach. Initially, the principal investigator (JH), health economist (SZ), and data analyst (MK) were blinded to the intervention assignments. This blinding remained in place through the intervention and booster phases. Blinding was enforced by using de-identified data and restricting discussion of intervention sites to unblinded research-team members. During the maintenance-phase data collection, the data analyst (MK) was unblinded to facilitate research operations. The biostatistician and health economist were provided de-identified data files for outcomes analysis.
3.2. Study dates
We recruited Associations in November and December 2014, enrolled them in the study in December 2014, conducted formative work with enrolled Associations and developed the intervention in 2015, and randomized them to treatment arms in March 2016. The period between enrollment and randomization was necessary to accurately stratify the Associations on predicted enrollment, which was calculated on actual enrollment in the year preceding the trial, March 2015 to February 2016. The 30-month trial launched in April 2016 and ended in September 2018.
3.3. Recruitment and study setting
We recruited Associations through Y-USA [19]. To be eligible, Associations had to be compliant with the National Council of YMCAs Constitution (Qualifications of Membership), be a current EF provider whose clients include community-dwelling older adults, and comply with national EF-license requirements. Of 21 eligible Associations, we enrolled 20 (95%). These 20 included 17 of 18 that applied in response to a national call for Associations interested in participation (the other was considered unprepared and thus ineligible), as well as an additional 3 that did not respond to the call but that Y-USA staff felt were well prepared for participation. With this sample size, we could detect a 50% difference in enrollment in the intervention arm compared to the control arm, with 91% power.
3.4. Intervention
The capacity-building intervention included two primary components: a structured toolkit, and technical-assistance calls. Capacity-building is an approach to cultivating and leveraging community organizations’ skills, leadership, resources, and commitment for a purpose [20]. Our purpose was to improve Association linkages to PT organizations and providers to increase older adult PA via EF enrollment. Although we initially planned to have only one active intervention phase at the beginning of the trial, a trial-midpoint evaluation showed that Associations were not able to sustain outreach activities beyond this initial active phase. As a result, we decided to add another active intervention phase during the second year of the trial (hereafter referred to as the “intervention booster”). As incentive for participation in the trial, both intervention and control Associations received payments totaling $2500 during the course of the RCT. Additional details about the recruitment and review process are available elsewhere [17].
3.4.1. Toolkit
Consistent with past YMCA practices, we based the toolkit structure on the Institute for Healthcare Improvement's Breakthrough Series Collaborative model of organizational change and quality improvement [21]. The toolkit contained seven modules, and Associations enrolled in the intervention arm received one toolkit module per month. Each monthly module built on work from prior months and included specific tasks: convening the toolkit team and engaging senior leaders (pre-work, month 1); partnership and capacity planning (month 2); data collection and management (month 3); outreach planning (month 4); conducting PT outreach (months 5 and 6); and review and quality improvement (month 7). Prior formative work with PTs informed toolkit development, such that Association staff, during outreach, could address PTs' priorities and how EF addresses those priorities [22]. The toolkit is available upon request.
3.4.2. Technical-assistance calls
Associations enrolled in the intervention arm participated in group technical-assistance calls with a Y-USA technical advisor, a staff member focused on implementation of evidence-based interventions like EF. Associations received support from the technical advisor and shared with each other experiences related to toolkit implementation. Associations participated in monthly calls during the toolkit implementation period (months 1–7 of the trial) and quarterly calls during the first maintenance period (months 8–19 of the trial).
3.4.3. Intervention booster
We provided the intervention booster from November 2017 to April 2018. A midpoint evaluation we conducted during April–May 2017 showed that YMCAs were not able to sustain outreach activities to providers and identified three barriers to outreach: lack of support and involvement from senior leadership, competing priorities, and difficulty establishing a feedback loop with providers. The intervention booster consisted of five monthly technical-assistance calls focused on addressing these barriers and providing a refresher of applicable toolkit modules. To address the perceived lack of leadership support, we also conducted one call with chief executive officers (CEOs) of intervention Associations as part of the booster.
3.5. Measures
3.5.1. Primary outcome measure
The primary outcome variable was the total number of new EF enrollees during the 30-month trial period (April 2016 to September 2018). These data were available through the Online Data Entry System (ODES), the online administrative-data management system for EF. ODES is housed and maintained by Sound Generations, a not-for-profit organization that licenses and disseminates EF nationally.
3.5.2. Process and intermediate outcome measures
Three online surveys hosted in the Research Electronic Data Capture system (REDCap) [23] collected information about Association outreach practices to providers (annually), staff-time allocation across all job duties including outreach (quarterly), and detailed outreach activities (monthly). Using a structured interview guide, we conducted 10 interviews on toolkit implementation with intervention Associations during the active intervention period (July 2016 and November 2016). For each element of the intervention toolkit, we asked participants: whether they had completed the activity (Yes, No, Partially completed, or Not yet at this element of the toolkit); whether they used the toolkit to complete the activity (Yes, No); how much time was spent completing the activity (<1 h; 1–2 h; >2 h); and how useful the activity was in building connection to physical therapists (Not at all useful, Not very useful, Somewhat useful, Very useful). We also captured additional contextual content as part of the interview. Using a structured interview guide, we conducted evaluation interviews with all 20 enrolled Associations at the end of trial year 1 (May 2017) and year 2 (May 2018); questions focused on facilitators and barriers to establishing CCLs with PTs. We digitally recorded all interviews and had them professionally transcribed verbatim. Using Excel, we summarized the responses to the quantitative questions about toolkit implementation. Using Atlas.ti, we conducted a content analysis of the transcripts to identify emergent themes.
3.5.3. Cost measures
We collected data on non-research-related intervention costs at Associations, Y-USA, and UW. At Associations, we measured time spent by staff on outreach to PTs from both intervention and control sites; this allowed us to assess differential costs between intervention implementation and business-as-usual. For PT outreach by Association staff, we used hourly time estimates, collected in the quarterly REDCap reports as “hours conducting outreach in a typical week,” and extrapolated them to total hours across the 30-month intervention period. We used national salary information obtained from Y-USA for each Association job category involved in PT outreach and matched to specific staff conducting outreach. We observed an average salary of $27 per hour across the job categories conducting outreach during the first 6 months of the trial and used this salary during the maintenance period of the intervention. We also reviewed time invoiced by the Y-USA technical advisor and likewise used invoiced salary information to calculate time spent by the UW team to support intervention activities (research administration and regulatory activities were not included in cost measures).
We estimated fringe and benefits at 30% for all staff. We used each institution's normal rates for facilities costs (information technology, office space, utilities, and other costs necessary to conduct the outreach activities); these were 17% for Associations, 20% for Y-USA, and 26% for UW. Additional costs included financial incentives to both intervention and control sites, as well as the cost of printed resources, such as posters and brochures provided during outreach.
3.6. Data analysis
3.6.1. Outcome measures
We used Poisson regression analysis to compare enrollment rates in the intervention and control arms, with Association as the unit of analysis. We included treatment assignment and stratum as independent variables. The treatment effect was expressed as the ratio of new enrollment for the intervention arm relative to the control arm. To avoid the need for distributional assumptions in the context of a small sample size [24], we used permutation test procedures to calculate P-values and 95% confidence intervals for the treatment effect.
We performed sensitivity analyses to assess the robustness of our findings to adjustment for covariates, the choice of unit of analysis (EF site versus Association), and the form of the regression model (linear versus log-linear). The Poisson regression model was modified, first by adding baseline EF enrollment as a covariate, and secondly by adding as covariates the number of YMCA branches and number of licensed EF sites within Associations. We also conducted analyses using EF site as the unit of analysis, as well as analyses using linear (as opposed to Poisson log-linear) regression models. In addition, we compared treatment arms on average weekly PT-outreach hours using t-tests. Using linear regression, we assessed the association between average outreach hours and enrollment. We used the statistical program R for all analyses [25].
3.6.2. Cost analyses
Cost data for the intervention and control Associations for the active intervention period and the maintenance period were summarized using Excel and Stata 15 (College Park, TX). The costs of the Y-USA technical advisor and the academic team are reported individually and not allocated to either the intervention or control sites because all sites had access to the Y-USA technical advisor, and the main support from the research team was for data collection required for both intervention and control sites.
4. Results
Intervention and control Associations were similar at baseline (Table 1). During the 11-month baseline period, the intervention Associations reported higher EF enrollment in 5 of the 10 strata, but the control Associations reported higher enrollment in the other 5. The number of EF sites per Association ranged from 1 to 30 and was similar for both arms.
Table 1.
Descriptive statistics (N = 20), YMCA Associations, baseline and trial period (April 2015 to September 2018).
| Stratuma | Group | Baseline Enrollmentb | Total Enrollment During Trialc |
|---|---|---|---|
| 1 | Control | 56 | 485 |
| 1 | Intervention | 65 | 284 |
| 2 | Control | 36 | 125 |
| 2 | Intervention | 135 | 597 |
| 3 | Control | 12 | 48 |
| 3 | Intervention | 92 | 234 |
| 4 | Control | 96 | 116 |
| 4 | Intervention | 10 | 237 |
| 5 | Control | 20 | 116 |
| 5 | Intervention | 49 | 127 |
| 6 | Control | 35 | 100 |
| 6 | Intervention | 33 | 30 |
| 7 | Control | 21 | 43 |
| 7 | Intervention | 16 | 49 |
| 8 | Control | 29 | 65 |
| 8 | Intervention | 9 | 27 |
| 9 | Control | 27 | 170 |
| 9 | Intervention | 43 | 60 |
| 10 | Control | 23 | 58 |
| 10 | Intervention | 11 | 50 |
| Control (mean) | 35.5 | 132.6 | |
| Intervention (mean) | 46.3 | 169.5 | |
| Ratio (Intervention/Control) | 1.30 | 1.28 |
d Number of Enhance®Fitness sites (both baseline and trial period sites included).
e Mean number of enrollees during the trial period, per site.
Number of new Enhance®Fitness enrollees during baseline period (April 2015 to February 2016).
Number of new Enhance®Fitness enrollees during the trial period (April 2016 to September 2018).
The capacity-building intervention was delivered as intended. Staff from all 10 Associations assigned to the intervention arm participated in the 7-month intervention; eight completed all modules, one completed parts of all modules, and one did not complete any module elements during the capacity-building intervention period (April–October 2016) because their EF class was not running due to loss of funding. Attendance at the monthly technical-assistance calls was high. Staff from three Associations attended all 7 calls, those from two attended 6, and those from five attended 5. The first 6 calls had staff from at least eight Associations in attendance. The last call, which covered plans for maintaining outreach after the active intervention, had the lowest attendance, with staff from only six Associations participating.
Participation in the intervention booster was variable. Staff from nine Associations attended at least one of the 5 booster technical-assistance calls focused on trouble-shooting barriers but ranged from attending 1 to 4 calls. Staff from five Associations attended the call for CEOs.
4.1. Primary outcome analysis
The intervention arm had 28% higher enrollment (1695 new enrollees) than the control arm (1326 new enrollees; 95% confidence interval, −47%–199%, P = 0.61). Sensitivity analyses yielded non-statistically significant treatment-effect estimates of similar magnitude (results not shown).
4.2. Intermediate outcome data
All 20 enrolled Associations reported on their outreach practices, including use of staff time, during the first 15 months of the trial; one Association stopped providing these data afterwards (Table 2). Completion of surveys exceeded 95%. The potential for outreach, as measured by the reported numbers of PT and healthcare partners, was similar for intervention and control Associations. The presence of an outreach team and the number of people on the team were similar for intervention and control Associations during the capacity-building and booster intervention periods in years 1 and 2. During the same time periods, the time spent on outreach to PTs was low, never more than 1.5 h per week, and was similar for intervention and control Associations.
Table 2.
Intermediate-outcome measures (N = 20), YMCA Associations, April 2016 to September 2018.
| Intervention (n = 10) |
Control (n = 10) |
|||||
|---|---|---|---|---|---|---|
|
Variable |
Baseline |
Year 1 |
Year 2 |
Baseline |
Year 1 |
Year 2 |
| n (%) or Mean (SD) | n (%) or Mean (SD) | |||||
| Provider-outreach practices | ||||||
| Total number of healthcare partners | 15.0 (30.2) | 9.6 (9.3) | 10.3 (18.9) | 27.7 (43.8) | 40.4 (50.8) | 20.8 (47.0) |
| Total number of PT partners | 1.5 (1.6) | 2.6 (2.1) | 2.6 (2.1) | 2.1 (2.5) | 6.5 (5.6) | 1.8 (1.9) |
| Have an outreach teama | 6 (60%) | 4(44%) | 3 (38%) | 4 (40%) | 3 (30%) | 2 (22%) |
| Number of people on outreach team | 2.8 (2.6) | 2.2 (0.5) | 2.0 (1.0) | 1.8 (0.5) | 1.0 (0.0) | 4.5 (2.1) |
| Sufficient time to conduct outreach, | ||||||
| Agree/strongly agree | 4 (40%) | 1 (11%) | 1 (13%) | 1 (10%) | 1 (10%) | 1 (11%) |
| Major barriers to outreachb | ||||||
| Staff turnover | 4 (40%) | 3 (30%) | 4 (44%) | 2 (20%) | 3 (30%) | 3 (30%) |
| Limited time | 9 (90%) | 8 (80%) | 8 (89%) | 10 (100%) | 10 (100%) | 7 (70%) |
| Competing demands | 9 (90%) | 6 (60%) | 6 (67%) | 3 (30%) | 4 (40%) | 1 (10%) |
| Poor provider response | 3 (30%) | 5 (50%) | 2 (22%) | 2 (20%) | 2 (20%) | 2 (20%) |
| Limited materials | 3 (30%) | 1 (10%) | 1 (11%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Other | 1 (10%) | 1 (10%) | 0 (0%) | 1 (10%) | 0 (0%) | 3 (30%) |
| Leadership support for outreachc | 3.8 (0.8) | 3.5 (1.4) | 3.9 (0.9) | 4.2 (1.0) | 4.0 (0.9) | 4.0 (1.1) |
| Staff time | ||||||
| Total hours worked per week | 37.6 (15.4) | 36.7 (13.5) | 38.8 (7.9) | 42.4 (16.7) | 46.5 (16.3) | 38.3 (18.4) |
| Hours spent on tasks, average week | ||||||
| Outreach to PTs | 2.0 (5.0) | 0.9 (1.6) | 1.5 (2.5) | 0.6 (0.8) | 0.8 (1.6) | 0.4 (0.7) |
| Outreach to other providers | 2.6 (2.4) | 2.7 (4.7) | 1.8 (2.0) | 2.1 (3.0) | 3.0 (2.0) | 1.1 (1.7) |
| YMCA member recruitment | 1.2 (1.6) | 1.8 (2.1) | 2.0 (2.0) | 5.2 (5.3) | 7.7 (9.0) | 5.44 (5.8) |
| Personnel and administration | 18.4 (15.4) | 19.2 (12.8) | 18.4 (13.3) | 18.0 (9.0) | 16.4 (9.3) | 15.3 (12.9) |
| Program duties | 5.8 (8.0) | 8.0 (6.87) | 8.4 (8.1) | 12.4 (7.6) | 12.4 (5.1) | 12.6 (11.2) |
Abbreviations: SD, standard deviation; PT, physical therapist.
Denominators varied slightly from measure to measure because of missing data.
Having an outreach team was defined as having staff who contributed to or participated in provider-outreach activities, including preparing or distributing outreach materials, contacting potential partners, and meeting with potential partners.
This variable indicates how many of the associations listed each item as a barrier.
Range = 1–5, where higher values indicate greater leadership support.
The most common barrier to outreach, reported by 70%–100% of Associations across both years and arms, was limited time for outreach to PTs regarding EF. Other barriers cited by at least half the Associations included competing demands and provider non-responsiveness to outreach. Fewer control than intervention Associations listed competing demands as a barrier to outreach, especially in year 2. The mean level of senior leadership support for outreach ranged between 3 and 4 (out of 5) across both years and arms. Very few Associations (n = 2 for both years 1 and 2, split equally between intervention and control arms) agreed that they had sufficient time to adequately conduct outreach for EF.
4.3. Intervention cost
Cost data showed that the intervention led to minor increases in effort on PT-outreach activities among intervention Associations (Table 3). Intervention and control Associations reported 1879 and 1449 total hours of outreach to PTs, respectively. Total costs associated with PT outreach were $105,110 and $84,172, respectively, with similar estimates of cost-per-new-enrollee for intervention ($62.01) and control Associations ($63.48).
Table 3.
Cost measures (N = 20), YMCA Associations, April 2016 to September 2018.a
| Intervention |
Control |
Difference |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Y-Staff Hours | Months 1–6 | Months 7–30 | Total | Months 1–6 | Months 7–30 |
Total | Months 1–6 | Months 7–30 |
Total |
| PT-related effortb | 499 | 1380 | 1879 | 150 | 1298 | 1449 | 349 | 82 | 430 |
| Costs | |||||||||
| Staff wagesc | $19,623 | $54,252 | $73,875 | $5900 | $51,046 | $56,945 | $13,723 | $3206 | $16,930 |
| Incentives | $5000 | $20,000 | $25,000 | $5000 | $20,000 | $25,000 | $0 | $0 | $0 |
| Printing/Supplies/Other | $1054 | $1230 | $2284 | $266 | $1961 | $2227 | $788 | -$731 | $57 |
| Booster effort | $0 | $3951 | $3951 | $0 | $0 | $0 | $0 | $3951 | $3951 |
| Total costs | $25,677 | $79,433 | $105,110 | $11,166 | $73,007 | $84,172 | $14,511 | $6426 | $20,938 |
| Y-USA Interventionist time | $16,526 | ||||||||
| Research team support | $43,534 | ||||||||
The active intervention phase occurred during months 1–6. The maintenance phase and intervention booster occurred during months 7–30.
Calculated as the total number of hours across sites.
Calculated as total hours of PT-related effort multiplied by $27/hour wages, plus benefits and facility-overhead costs.
4.4. Intervention facilitators and barriers from qualitative data
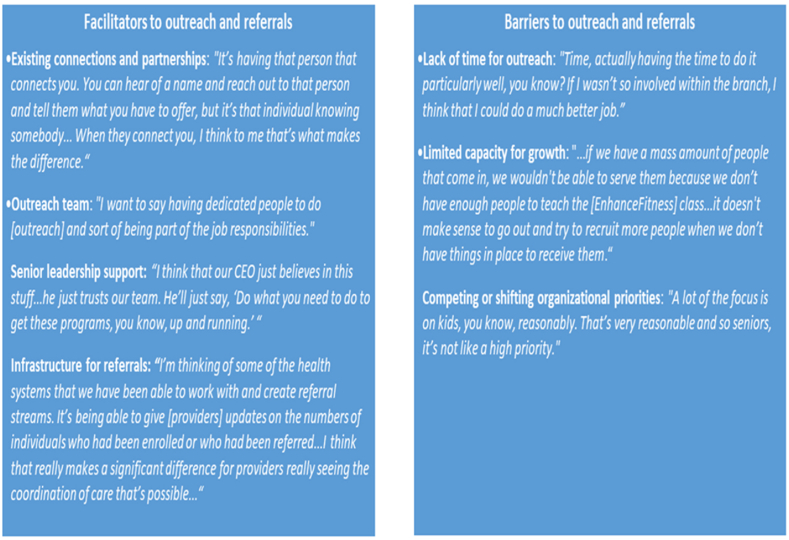
Our thematic analysis of qualitative data from the interviews with Associations at the end of trial year 2 identified facilitators and barriers to establishing CCLs with providers (Fig. 2). Facilitators described included existing connections and partnerships and having an outreach team. Existing connections were sometimes leveraged by participants to facilitate the development of new provider partnerships. Some participants shared facilities (e.g., a pool) with their clinical partners, and this facilitated patient referrals to YMCA programs by these partners. Having a team of staff whose job responsibilities included outreach helped make outreach efforts possible. Other facilitators included senior leadership support to do this type of work and a strong infrastructure for referrals (e.g., use of electronic medical records or other systems to enable bidirectional communication with providers about referrals).
Fig. 2.
Illustrative quotes from qualitative data analysis.
Participants reported that barriers outweighed the facilitators. Barriers to outreach and referrals included lack of staff and time for outreach, limited capacity for EF growth, and competing or shifting organizational priorities. Participants noted a lack of additional YMCA staff to conduct outreach or run EF classes; fitting outreach into their own workload was seen as a “juggling act.” Some Associations lacked the physical space to grow their EF program, and this made trying to increase referrals to the program fruitless. Finally, implementation of other programs like the Diabetes Prevention Program funded by the Centers for Medicare and Medicaid Services, or youth programs, also made it challenging to prioritize conducting outreach for EF.
5. Discussion
This RCT tested an intervention (PT-REFER) to increase patient referrals to EF, an evidence-based group-exercise program for older adults, by building CCL capacity between Associations and PTs. Our capacity-building intervention was designed collaboratively with Y-USA, and the focus on PTs rather than primary-care providers was their choice. The intervention had high participation and completion. Despite this collaborative approach and successful implementation, the intervention did not lead to a significant increase in the number of outreach hours to PTs in the intervention versus the control arm, nor did it significantly increase the number of new EF enrollees at YMCAs. Our cost analysis did reveal, however, that the cost of adding new enrollees was modest, less than $64 per enrollee in both arms.
The ability of Associations to sustain targeted outreach activities was hampered by organizational barriers such as insufficient staff and time dedicated for outreach, and competing or shifting organizational priorities. Competing priorities may have been particularly important, as Associations nationwide were simultaneously attempting new implementation of the Diabetes Prevention Program, and the same staff teams were implementing both EF and the Diabetes Prevention Program. The PT-REFER intervention was not able to overcome these barriers.
On the other hand, we did learn that outreach activities were facilitated by leveraging existing connections and partnerships, having a designated team for outreach, and having an infrastructure for referrals. These findings are consistent with previous research on facilitators and barriers to the development and sustainability of CCLs [26,27].
Based on our findings and those of others, we recommend several actions that may help organizations sustain outreach activities and increase patient referrals to evidence-based programs such as EF. First, the organization should have staff who can routinely dedicate time in their workday to outreach. This may require hiring additional staff, or having existing responsibilities reassigned from current staff to ensure adequate time for building and maintaining clinical partnerships. Second, organizations should place a strategic focus on outreach and program growth to ensure that these activities are a priority for the organization and that there is capacity for growth. Because senior leaders at both local and national levels are heavily involved in organizational priority-setting, clear communication of the buy-in and commitment from this group is critical. Lastly, having a referral structure (e.g., electronic health record connection) could help organizational staff communicate with partners more effectively. Developing a formal agreement to determine expectations for communication will make sure that each entity understands its role in the partnership and referral process [9].
5.1. Strengths and limitations
Our study employed a randomized-controlled-trial design, and we collected extensive quantitative and qualitative process and intermediate-outcome data, allowing us to shed light on the factors that influenced intervention implementation and resulting actions. However, the study had a number of limitations. First, our small sample size affected our ability to detect small-to-moderate intervention effects. Second, the intervention focused on increasing Association capacity for outreach to PTs and did not involve working directly with PTs or PT practices. While our approach was informed by feedback from both YMCAs and PTs, working with both groups to improve capacity for outreach might have led to stronger partnerships and greater EF enrollment.
Third, participating Associations were more limited than we and they realized in their capacity to expand PT outreach and to grow their EF programs. Associations that applied to participate in the study described their desire and capacity to grow their EF programs as part of their application. At the time of outreach, however, operational realities limited the capacity of the Associations. More discussion with senior Association leaders at the outset about capacity and competing priorities might have helped us choose Associations with room for program growth, choose a better time for intervention implementation, or design an intervention better suited to the realities of the Associations [28].
Finally, we conducted the study with YMCA Associations, which are different from other community-based organizations, both because they offer a wide range of fitness, youth, and chronic-disease-prevention programming, and because they are supported by Y-USA. As a result, the findings of this study may not be generalizable to other types of community organizations. Given that capacity for EF growth and competing priorities were two of the barriers to conducting outreach we identified in the study, community organizations with missions more aligned with serving older adults may be better able to allocate staff time and other resources to conducting outreach and increasing referrals to EF.
6. Conclusions
We collaborated with PTs and Y-USA to develop and implement a capacity-building intervention to increase CCLs that would support increased enrollment in EF programs offered by Associations through increased outreach to, and referrals from, PTs. Staff at intervention Associations had competing demands, however, and spent only marginally more time performing outreach to PTs. Enrollment in EF did not significantly increase. Our evaluation findings indicate that community organizations that prioritize growth of evidence-based programs, have support at all organizational levels, and set aside staff and time to invest in outreach and partnership development, may be more successful in creating sustainable linkages with clinical partners and increasing evidence-based-program reach.
Declarations
Ethics approval and consent to participate
The University of Washington (UW) Institutional Review Board approved all protocols for this study.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
This publication is a product of a Prevention Research Center and was supported by Cooperative Agreement Number U48DP005013 from the Centers for Disease Control and Prevention. The findings and conclusions in this paper are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Authors’ contributions
MPP was the co-principal investigator of the study and led writing of the first draft. JH was the co-principal investigator of the study and led writing of the final draft. BL was the biostatistician for the study. MK was the data manager and played a major role in data analysis and in writing. CK played a major role in data analysis and in writing. SZ led the cost analysis for the study. LS led development of the capacity-building intervention. SF led field operations for the study. BB served as the expert on Enhance®Fitness and advised on study design and implementation. MG was a YMCA technical advisor who worked with YMCA Associations during the study. PH is principal investigator of the Health Promotion Research Center, where the study was housed and advised on study design and implementation. All authors read and approved the final manuscript.
Trial registration
Name of the registry: clinicaltrials.gov.
Trial registration number: NCT03139461.
Date of registration: May 4, 2017, Retrospectively registered.
URL of registry record: https://clinicaltrials.gov/ct2/show/NCT03139461.
Declaration of interests
☒ The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
☐The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Acknowledgements
We also acknowledge the enduring advice and support of Maureen Pike of YMCA of the USA, as well as our Project Advisory Group members: Terry Brady, member-at-large; Jennifer Bruning, Kansas State Alliance of YMCAs; Paige Denison, Sound Generations; Lianna Fry, Greater Wichita YMCA; and Lori Schrodt, Western Carolina University and the Academy of Geriatric Physical Therapy, a component of the American Physical Therapy Association.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2022.100888.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.National Center for Health Statistics Summary health statistics: national health interview survey, 2016. 2018. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_A-14.pdf Available from:
- 2.Harris T., Kerry S.M., Limb E.S., Victor C.R., Iliffe S., Ussher M., et al. Effect of a primary care walking intervention with and without nurse support on physical activity levels in 45-to 75-year-Olds: the Pedometer and Consultation Evaluation (PACE-UP) cluster randomised clinical trial. PLoS Med. 2017;14(1) doi: 10.1371/journal.pmed.1002210. PubMed PMID: WOS:000395719900007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boehm J., Franklin R.C., Newitt R., McFarlane K., Grant T., Kurkowski B. Barriers and motivators to exercise for older adults: a focus on those living in rural and remote areas of Australia. Aust. J. Rural Health. 2013;21(3):141–149. doi: 10.1111/ajr.12032. PubMed PMID: 23782281. [DOI] [PubMed] [Google Scholar]
- 4.King A.C. Interventions to promote physical activity by older adults. J Gerontol A Biol Sci Med Sci. 2001;56:36–46. doi: 10.1093/gerona/56.suppl_2.36. Spec No 2(suppl_2) PubMed PMID: 11730236. [DOI] [PubMed] [Google Scholar]
- 5.Chiang K., Seman L., Belza B., Tsai J.H. It is our exercise family": experiences of ethnic older adults in a group-based exercise program. Prev. Chronic Dis. 2008;5(1):A05. PubMed Central PMCID: PMCPMC2248786. [PMC free article] [PubMed] [Google Scholar]
- 6.American Physical Therapy Association The role of the physical therapist in national health care reform. 2011. https://www.apta.org/uploadedFiles/APTAorg/Advocacy/Federal/Health_Care_Reform/APTA_Position/RoleofPTinHealthCareReform.pdf [cited 2018 October 26]. Available from:
- 7.Verhagen E., Engbers L. The physical therapist's role in physical activity promotion. Br. J. Sports Med. 2009;43(2):99–101. doi: 10.1136/bjsm.2008.053801. PubMed PMID: 18838405. [DOI] [PubMed] [Google Scholar]
- 8.Glasgow R.E., Harden S.M., Gaglio B., Rabin B., Smith M.L., Porter G.C., et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front. Public Health. 2019;7:64. doi: 10.3389/fpubh.2019.00064. PubMed PMID: 30984733; PubMed Central PMCID: PMCPMC6450067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Atlanta, GA: 2016. Community-clinical Linkages for the Prevention and Control of Chronic Diseases: A Practitioner's Guide. [Google Scholar]
- 10.Porterfield D.S., Hinnant L.W., Kane H., Horne J., McAleer K., Roussel A. Linkages between clinical practices and community organizations for prevention: a literature review and environmental scan. Am. J. Publ. Health. 2012;102(Suppl 3):S375–S382. doi: 10.2105/AJPH.2012.300692. PubMed PMID: 22690974; PubMed Central PMCID: PMCPMC3478082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gillette D.B., Petrescu-Prahova M., Herting J.R., Belza B. A pilot study of determinants of ongoing participation in EnhanceFitness, a community-based group exercise program for older adults. J. Geriatr. Phys. Ther. 2015;38(4):194–201. doi: 10.1519/JPT.0000000000000041. PubMed PMID: 25695473; PubMed Central PMCID: PMCPMC4540700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bethancourt H.J., Rosenberg D.E., Beatty T., Arterburn D.E. Barriers to and facilitators of physical activity program use among older adults. Clin. Med. Res. 2014;12(1–2):10–20. doi: 10.3121/cmr.2013.1171. PubMed PMID: 24415748; PubMed Central PMCID: PMCPMC4453303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohn M.J., Belza B., Petrescu-Prahova M., Miyawaki C.E., Hohman K.H. Participant variation by delivery site type in an evidence-based physical activity program. J. Aging Phys. Activ. 2015;23(3):401–408. doi: 10.1123/japa.2013-0252. PubMed PMID: 25134641; PubMed Central PMCID: PMCPMC4783154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belza B., Shumway-Cook A., Phelan E.A., Williams B., Snyder S.J., LoGerfo J.P. The effects of a community-based exercise program on function and health in older adults: the EnhanceFitness Program. J. Appl. Gerontol. 2006;25(4):291–306. doi: 10.1177/0733464806290934. PubMed PMID: WOS:000239244200002. [DOI] [Google Scholar]
- 15.Smith M.L., Belza B., Braun K.L., King S., Palmer R.C., Sugihara N.S., et al. National reach and dissemination of EnhanceFitness. Health Behav Policy Rev. 2014;1(2):150–160. doi: 10.14485/hbpr.1.2.7. [DOI] [Google Scholar]
- 16.Schulz K.F., Altman D.G., Moher D., Consort Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Ann. Intern. Med. 2010;11(152):726–732. doi: 10.1186/1745-6215-11-32. PubMed PMID: 20334632; PubMed Central PMCID: PMCPMC2857832. [DOI] [PubMed] [Google Scholar]
- 17.Petrescu-Prahova M., Kohn M., Leroux B., Steinman L., Fishleder S., Pike M., et al. Building community-clinical linkages to increase older adult physical activity: the PT-REFER trial protocol and participant baseline characteristics. Contemp Clin Trials Commun. 2019:100373. doi: 10.1016/j.conctc.2019.100373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donner A. Some aspects of the design and analysis of cluster randomization trials. J R Stat Soc C-Appl. 1998;47(1):95–113. doi: 10.1111/1467-9876.00100. PubMed PMID: WOS:000072828100007. [DOI] [Google Scholar]
- 19.Ymca of the Usa The Y: YMCA of the USA website. 2021. https://www.ymca.net [cited 2021 January 29]. Available from:
- 20.Simmons A., Reynolds R.C., Swinburn B. Defining community capacity building: is it possible? Prev. Med. 2011;52(3–4):193–199. doi: 10.1016/j.ypmed.2011.02.003. PubMed PMID: 21320524. [DOI] [PubMed] [Google Scholar]
- 21.Institute for Healthcare Improvement The Breakthrough Series: IHI's collaborative model for achieving Breakthrough improvement. Diabetes Spectr. 2004;17(2):97–101. doi: 10.2337/diaspect.17.2.97. [DOI] [Google Scholar]
- 22.Fishleder S., Petrescu-Prahova M., Harris J.R., Steinman L., Kohn M., Bennett K., et al. Bridging the gap after physical therapy: clinical-community linkages with older adult physical activity programs. Innov Aging. 2018;2(1) doi: 10.1093/geroni/igy006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. PubMed PMID: 18929686; PubMed Central PMCID: PMCPMC2700030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ernst M.D. Permutation methods: a basis for exact inference. Stat. Sci. 2004;19(4):676–685. doi: 10.1214/088342304000000396. PubMed PMID: WOS:000228784100014. [DOI] [Google Scholar]
- 25.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2016. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 26.Payán D.D., Sloane D.C., Illum J., Vargas R.B., Lee D., Galloway-Gilliam L., et al. Catalyzing implementation of evidence-based interventions in safety net settings: a clinical-community partnership in South Los Angeles. Health Promot. Pract. 2017;18(4):586–597. doi: 10.1177/1524839917705418. PubMed PMID: 28443342; PubMed Central PMCID: PMCPMC5593854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vogel M.T., Petrescu-Prahova M., Steinman L., Clegg-Thorp C., Farmer C., Sarliker S.E., et al. Partnerships for blood pressure control in Washington State, December 2016-July 2017. Health Promot. Pract. 2019 doi: 10.1177/1524839919853819. PubMed PMID: 31185742; PubMed Central PMCID: PMCPMC7582015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Thiele Schwarz U., Aarons G.A., Hasson H. The Value Equation: three complementary propositions for reconciling fidelity and adaptation in evidence-based practice implementation. BMC Health Serv. Res. 2019;19(1):868. doi: 10.1186/s12913-019-4668-y. PubMed PMID: 31752846; PubMed Central PMCID: PMCPMC6873662. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.