Abstract
Introduction:
Many mothers have the goal to breastfeed. However, more than 50% will have breastfeeding difficulty by the 3rd day of life. Mothers who are unable to meet their breastfeeding goals are at higher risk for anxiety, depression, embarrassment, and guilt. Those who stop breastfeeding need support and help resolving these feelings. This case study aims to describe one woman’s difficulty with mental health surrounding breastfeeding, her decision to bottle feed, and her successful transition back to direct breastfeeding.
Main Issue:
Barriers to the participant’s success with breastfeeding were pre-existing history of depression/anxiety, forceps delivery, uncontrolled perineal pain, infant physical trauma, and nipple/flow confusion. The decision to discontinue direct breastfeeding and start bottle feeding came after 2 months of anxiety, frustration, and persistence.
Management:
The participant followed her healthcare team’s recommendations of triple feeding, lactation support groups, pediatric chiropractic adjustments, and prescribed galactagogues. After 2 months of exhaustion and deliberation, she made the difficult decision to stop breastfeeding for nutritional benefits and switched to breastfeeding only for her infant’s pleasure and comfort. Lowered expectations allowed the dyad to heal and her son to transition to nearly exclusive breastfeeding at 4 months of life.
Conclusion:
Clinicians must be aware of the delicate balance between promoting breastfeeding for its nutritional value and health benefits and supporting a struggling mother with mental health needs.
Keywords: breastfeeding, breastfeeding barriers, breastfeeding difficulties, breastfeeding duration, breastfeeding experience, case study, mother–infant dyad, oral motor dysfunction, postpartum depression
*Editor’s Note
JHL has a policy of not publishing references from predatory publishers. The references in the Reference List with * were published in journals whose publishers have been criticized by some academics for low standards of peer review as well as some allegations of academic misconduct. Others have felt these publishers have done their due diligence. Due to the importance of the topic covered in this review, we left the inclusion of these articles to the authors’ discretion. The authors have reviewed all references and take responsibility for their quality.
Introduction
Most new mothers are concerned about feeding their infant (Brown et al., 2016). Many believe that breastfeeding is the more “natural” or “healthiest” feeding plan (Demirci et al., 2018; Woollard & Porter, 2017). While 83.2% of mothers attempt to breastfeed their newborns in the United States, only 57.6% are still breastfeeding at 6 months, with 24.9% exclusively breastfeeding (Centre for Disease Control and Prevention [CDC], 2020).
The reality of breastfeeding often becomes much harder than mothers had thought it would be (CDC, 2020). More than 63% of mothers have breastfeeding difficulty during the 1st month of life (Gianni et al., 2019). Mothers who do not meet their breastfeeding goals can feel sadness, depression, embarrassment, and guilt (Demirci et al., 2018), negatively affecting their mental health. Conversely, a mother’s mental health also affects her duration of any breastfeeding (Ritchie-Ewing et al., 2019). Mothers who stop breastfeeding may need support from many sources (Jackson et al., 2021).
We present a nulliparous mother with prior depression and anxiety who struggled to breastfeed. She made a deliberate and thoughtful (yet difficult) decision to stop breastfeeding at 2 months of life, providing her son with her own milk and formula by bottle, while breastfeeding only for his pleasure and comfort. By 4 months of life, however, she progressed to exclusive direct breastfeeding at home (Figure 1).
Figure 1.
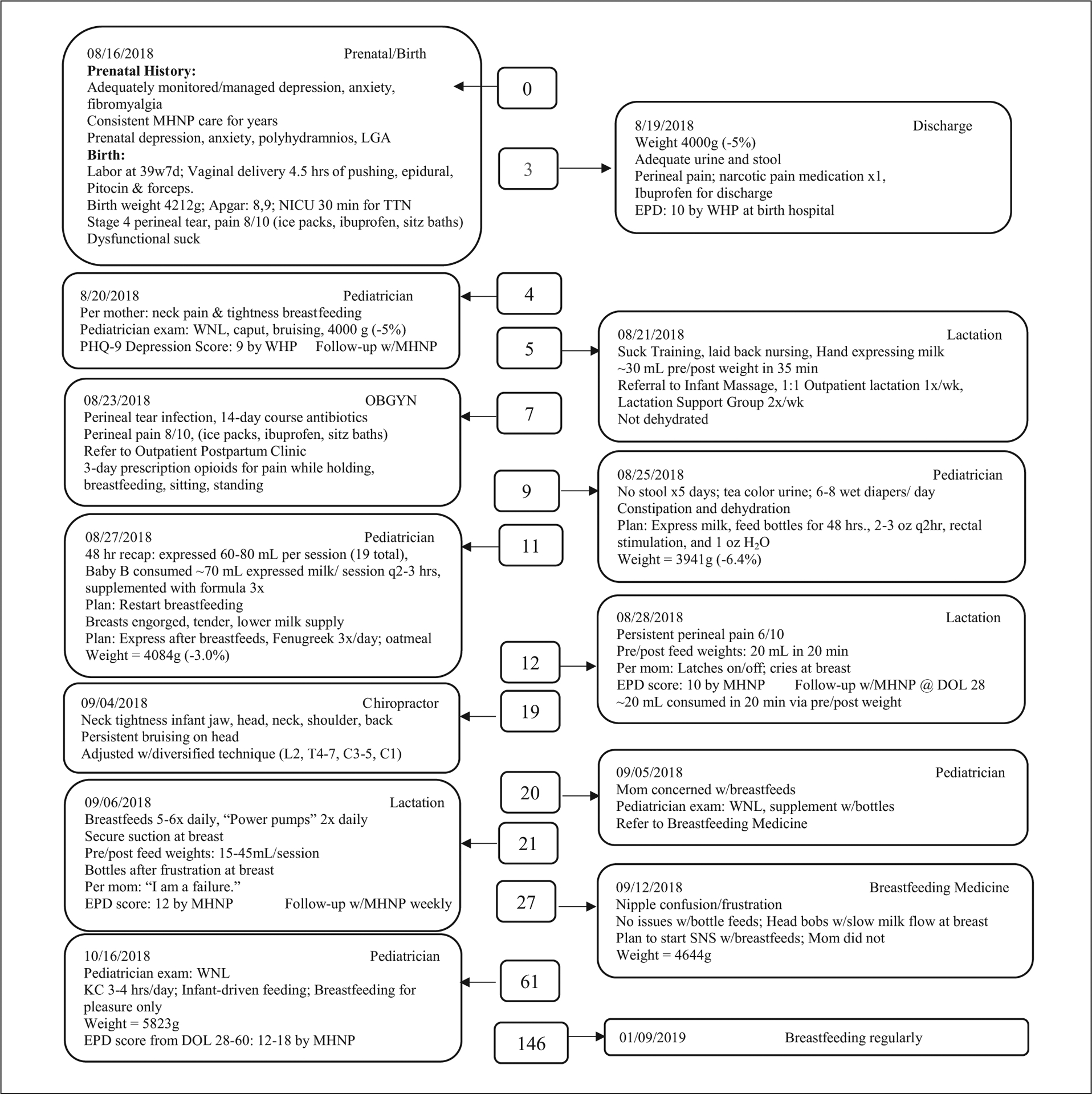
Timeline of Case Study on Delayed Breastfeeding and Interventions.
Note. MHNP = Mental Health Nurse Practitioner; LGA = Large for Gestational Age; NICU = Neonatal Intensive Care Unit; TTN = Transient Tachypnea of\urgh Postpartum Depression scale; WHP = Women’s Health Provider; WNL = Within normal limits; PHQ-9 = Patient Health Questionnaire-9; DOL = Day of Life; SNS = Supplemental Nursing System; KC = Kangaroo Care; w/ = with.
We discuss strategies for supporting mothers in their difficult decisions to stop breastfeeding for mental health concerns. For the purposes of this case study, we used breastfeeding terms based on Labbok and Starling’s (2012) work, which defines breastfeeding as the “child has received breastmilk (direct from the breast or expressed)” (p. 399). Exclusive breastfeeding is defined as the infant not receiving anything other than human milk directly and/or expressed human milk. Bottle feeding is defined as, receiving liquid (formula or human milk) from a bottle with a nipple (Labbok & Starling, 2012). We received Intsitutional Review Board (IRB) approval and the participant discussed in this case has given written consent for publication of the case. To ensure rigor of the research, the authors reviewed the official obstetrical, pediatric, psychiatric, chiropractic, and lactation health records of the participants from January 1, 2018–January 1, 2019. The authors also reviewed lactation log data electronically tracked by the participant from August 16, 2018–October 15, 2018. The participant (a co-author) has reviewed and approved of the case as submitted (FWA# 00003152).
History and Observational Assessment
The participant was a married, 30-year-old G1P1 Neonatal Intensive Care Unit (NICU) registered nurse, with a long-standing history of depression, anxiety, and fibromyalgia. The participant’s difficult labor included an epidural, Pitocin, a long second stage (4.5 hr), and a forceps delivery with a Stage 4 perineal tear (Figure 1). Following delivery, the participant immediately held her baby using skin-to-skin care (SSC). He attempted to migrate to the breast but was ineffective in latching. After 15 min of SSC, he was transferred to the neonatal intensive care unit (NICU) for 30 min and received suctioning and positive pressure ventilation.
At 3 hours of life, the International Board Certified Lactation Consultant (IBCLC®) helped facilitate the first breastfeed. The infant had an uncoordinated suck, notable facial/head bruising, caput succedaneum, light sensitivity, molding, and unilateral neck rotation. The IBCLC taught the participant how to hand express colostrum into a cup and feed her baby.
On Day of Life (DOL) 2, after a few minutes of breastfeeding, the infant pulled away crying, and was unable to latch. A different IBCLC recommended that the participant hold him close to her nipple for a few minutes, even while he cried. The infant roomed with the participant and did not receive any formula. Postpartum nurses observed the participant breastfeed several times without providing any additional guidance and continued to refer her to the lactation team for further problem solving.
The participant and her son were discharged on DOL 3. She experienced perineal pain that interfered with her mobility and her ability to hold her son. She scored close to minor/major depression on her Edinburgh Postpartum Depression screen (EPD score = 10). An EPD score of 10 signifies that depression may be present; an EPD score of 13 or higher signifies a positive depression screen (Cox et al., 1987). On DOL 4, the participant raised concerns with her primary pediatrician that her son seemed to be in pain during breastfeeding and had muscle tightness.
Management
On DOL 5, the participant attended an Outpatient Lactation Clinic. She was worried that her baby was not getting enough milk, despite breastfeeding 6–8 times a day and expressing an additional 25–45 ml of milk via pump 4 times daily. If her baby was crying and still showing hunger cues after breastfeeding, she then provided 25–50 ml of her milk or formula by bottle. On that day (DOL 5), she supplemented after breastfeeding, with her expressed milk 4 times and with formula twice. The IBCLC assured the participant that the first days of life are always overwhelming. She assisted with laid-back breastfeeding position, taught her to perform suck training, and referred her to an infant massage therapist class. The infant transferred ~30 ml in a 35-min feed. The participant followed up with the Lactation Clinic once a week and lactation support group twice weekly.
On DOL 9, the participant visited the on-call pediatrician because her baby had not stooled in 4 days and his urine was tea-colored. The pediatrician advised the participant to express and feed her own milk every 2–3 hr by bottle for 48 hr. After following this recommendation, the infant had more frequent wet diapers, stools, and increased alertness. However, the participant’s breasts were engorged, and she felt her milk supply had decreased. The pediatrician advised the participant to triple feed (breastfeed, express, bottle feed), take fenugreek, and eat oatmeal to increase her milk supply, which the participant found to be effective.
On DOL 12, during her lactation appointment, the participant reported that she was still in significant perineal pain. This made it difficult for her to sit, stand, walk, and hold her baby. Her pain threshold may have been altered due to her fibromyalgia, which can cause pain to be felt more intensely. Women’s health provider (WHP) notes revealed that her EPD screen was 10 (borderline depression). During breastfeeding, the infant would pull away from the breast and did not have satiety. The participant noted that after 48 hr of bottles, the baby would cry, flail, and become dysregulated at the breast. The IBCLC encouraged the participant to continue suck training, provide tummy time, and review a written handout on laid-back breastfeeding. She referred the baby to a pediatric chiropractor.
On DOL 19 the pediatric chiropractor diagnosed the infant with bilateral suboccipital, rhomboid, right masseter, and shoulder capsule tightness, and persistent bruising related to forceps. The chiropractor adjusted the infant using diversified technique (Alcantara et al., 2015). The participant attended an infant massage course and continued both chiropractic and massage exercises at home. On DOL 20, the participant’s husband took the baby to his 3-week well visit where the pediatrician referred him to Breastfeeding Medicine.
On DOL 21, the participant attended her weekly lactation appointment. The infant had a secure suction at the breast, evidenced by milk in his mouth and a deep latch. He transferred 15–45 ml of human milk and appeared satisfied. At home, if the infant was inconsolable prior to feeds, the participant provided 1–2 oz of her expressed milk. She would then switch to the breast, but the infant showed frustration with not getting milk quickly. The participant stated, “I feel like a failure.” The participant disclosed concerns about her and her baby’s safety if she was home alone without the support of her husband. The IBCLC did not share or follow up on this information. The participant met weekly with a mental health nurse practitioner (EPD score was 12 at that time).
On DOL 27, a Breastfeeding Medicine specialist diagnosed the infant with nipple confusion, as he latched and drank from a bottle without any issues, but had difficulty at the breast. He would pull off and cry with frustration from slow milk flow (Figure 1 & 2). The participant shared feelings of embarrassment regarding trying to relate to peers and colleagues who had great breastfeeding journeys. The physician emphasized that the participant “was a great mother,” and praised her for “doing a marvelous job,” recognizing that “getting any mother’s milk is a fabulous accomplishment.” She assured the participant that the team would support whatever feeding option she chose.
Figure 2.
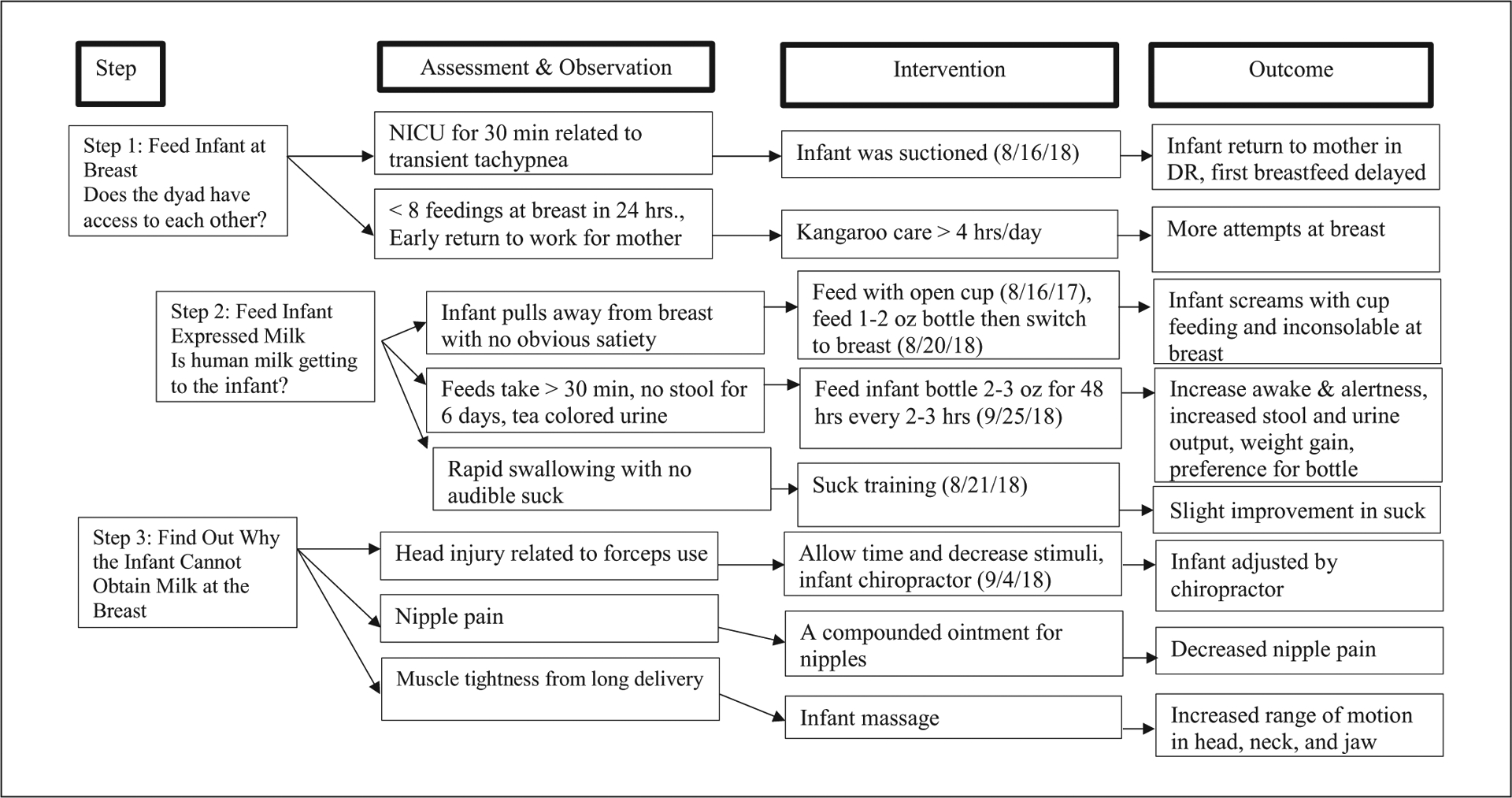
Breastfeeding Management and Interventions.
Note. These interventions were based on Smith’s Assistance, Breastmilk, Contact (ABC) Protocol. NICU = Neonatal Intensive Care Unit; DR = Delivery Room. Figure is based on Smith’s ABC Protocol (2007).
Between DOL 28–60, the participant increased her working hours. At work, she would pump 4–5 times while other caregivers bottle-fed her baby. The participant stopped attending outpatient private lactation visits and support groups. Appointments increased the participant’s stress because her IBCLCs often invalidated her feelings and were not able to offer the type of emotional support and troubleshooting she needed. Her IBCLCs mentioned that she no longer needed to attend appointments because feedings during appointments tended to go smoothly. The participant disagreed that she no longer needed support but stopped attending appointments because she felt dismissed for her feelings. Apart from her postpartum pain specialist and WHP, none of her providers communicated with each other or coordinated a team approach to care.
The participant was discouraged, and quickly became exhausted from triple feeding. Her EPD scores continued to increase (major depression: 13–18). At her 2-month mental health appointment, the participant noticed her severe postpartum depression and its relationship to her breastfeeding experience. She then prioritized strengthening her relationship with her son over “fighting to breastfeed.” This prioritization allowed the space for both the participant and infant to grow and heal.
Outcomes
The participant adhered to 2 months of breastfeeding interventions while returning to work (Figure 2). She tolerated a triple-feeding regimen for some time but not without physical and emotional cost. She decided to stop direct breastfeeding and turned her focus toward pumping. At her 4-month mental health appointment, the participant shared that she took pride in expressing her milk at work. Her colleagues praised her for “being a good mother” and she felt supported by them.
During evenings, nights, and weekends, the participant would SSC with her infant for several hours with opportunities to migrate to the breast if desired. If her infant showed hunger cues and frustration at the breast, the participant would bottle-feed him in SSC. The participant explained, “I don’t place any expectations on myself or my son to breastfeed. Feedings are driven by him. We focus on enjoying feeding, whatever the source.” By 4 months of life, the infant was predominantly feeding directly at the breast. The transition back to breast happened so gradually over the course of 2 months, and at an infant-led pace, that the participant did not notice that it had occurred.
Discussion
There were multiple risk factors present in the participant’s peripartum period that could have impeded her ability to exclusively breastfeed. This included a difficult, instrument-assisted delivery that resulted in both maternal and infant physical trauma and severe uncontrolled pain; diagnosed pre- and postpartum depression and anxiety, and the need to triple feed her infant due to severe nipple confusion.
Difficult Delivery and Breastfeeding
In this case study, the participant had a large for gestational age (LGA) infant and a long second stage of labor, resulting in forceps delivery and physical birth trauma. Instrument-assisted delivery has been repeatedly associated with breastfeeding difficulties (Bonilla & Riggs, 2020) like higher odds of infant feeding problems (Peters et al., 2018), shorter breastfeeding durations, and lower breastfeeding rates (Kendall-Tackett et al., 2015). The use of forceps causes lateral compression of the infant’s facial and cranial bones, which may result in bruising, bleeding, swelling (e.g., caput succedaneum), and infant suck dysfunction due to trigeminal nerve damage (Smith, 2007, Bonilla & Riggs, 2020). The infant’s injuries could have taken months to heal, which could explain why he felt more comfortable bottle-feeding and gradually made the transition from near exclusive bottle feeds to near exclusive breastfeeding.
A careful evaluation of the infant’s suck dysfunction may have diagnosed the breastfeeding problems sooner (Smith, 2007). A significant limitation in the participant’s management was that she was not informed and did not understand the significant perinatal risk factors she had experienced that could have result in her breastfeeding difficulties. Informing the participant about the significant risk factors could have reduced her anxiety and guilt. IBCLCs need to closely follow these dyads and provide a specific, written plan before hospital discharge about how to express milk, assess infant latch, suck, and swallow, and where to access outpatient lactation support (Supplementary Figures 1 and 2).
Pain and Breastfeeding
In this case study, the participant’s perineal Stage 4 tear and chronic fibromyalgia pain was persistent and uncontrolled, evidenced by difficulty holding and breastfeeding her son. Women who have severe perineal pain often report difficulty sitting, standing, holding, breastfeeding, and providing general care to their infant (Beck, 2021). Pain inhibits oxytocin activity and milk transfer (Brown et al., 2016; Jobst et al., 2016; Pereira et al., 2017, Reece-Stremtan, 2017), and is also significantly associated with symptoms of depression during the postpartum period (Jobst et al., 2016; Nguyen et al., 2019; Swenson et al., 2018).
A limitation in the participant’s management approach was a lack of continuity of care with the same IBCLC to provide the participant with a better understanding of her breastfeeding barriers. A telehealth conference between the mother, IBCLC, a mental health provider, and WHP could have helped the team better understand and address the participant’s pain, mental health, and breastfeeding needs. The team could then have created an individualized plan of care with a consistent, supportive message.
Depression and Anxiety: During Pregnancy and Postpartum
The participant suffered from a history of depression and anxiety before, during, and after her pregnancy. Both pre- and postpartum depression (Dias & Figueiredo, 2015; Payne & Maguire, 2019) and postpartum anxiety (Fallon et al., 2016; Hoff et al., 2019) predict shorter durations of breastfeeding. Maternal stress and frustration due to ongoing disparities between breastfeeding expectations and challenging realities can also make mothers more prone to postpartum depression (Stark et al., 2021). For mothers who highly value breastfeeding, difficult experiences with breastfeeding heighten the risk for low self-esteem and feelings of maternal role failure (Feenstra et al., 2018; Gianni et al., 2019). There is tremendous societal pressure surrounding mothering and breastfeeding expectations. Breastfeeding challenges are often viewed as a personal problem rather than a systemic failure to provide mothers with the support they need. As a result, mothers often report feeling as if their worth is defined by a feeding method (Jackson et al., 2021; Woollard & Porter, 2017).
In the participant’s case, all providers were aware of her history and current treatment. A significant limitation in her management approach was that her IBCLCs did not recognize the enormous stress that breastfeeding placed on the participant. While her providers were empathetic with her struggles and supportive of her decision to reduce direct breastfeeding, they did not provide adequate psychosocial support to help her actively work through her feelings. The participant’s providers viewed her mental health issues as another discipline’s responsibility and deferred her care to her mental health nurse practitioner, without continuity of care or coordination with the mental health team. A significant strength of the participant’s management approach was the support of her mental health practitioner, whom she had seen for several years. As a working mother who had also breastfed her children, the participant’s practitioner was able to provide her with a better understanding of the struggles that working mothers face when trying to breastfeed. This support helped the participant to cope with the stress of societal pressures and personal expectations as a health care professional and new mother.
Since there are often strong feelings and emotional struggles directly related to breastfeeding, IBCLCs can be a vital source of support by addressing these feelings. First, IBCLCs can help the patient identify her feelings in a nonjudgmental space by simply asking, “How are you feeling about breastfeeding right now?” Additionally, IBCLCs should directly ask about feelings of anger, guilt, embarrassment, or anxiety and how they affect the patient and their relationship to the infant, providing reassurance that it is OK to have these feelings and that they are not alone in them. Once the patient’s feelings are acknowledged, the IBCLC can introduce interventions to change their frame of mind, refocus their thoughts into constructive encouragement, and promote self-acceptance (Supplemental Figure 2).
IBCLCs can also provide paraprofessional psychological interventions to support lactating mothers (Diebold et al., 2020; Grover et al., 2020; Nation et al., 2018). IBCLCs can receive training and resources to address mental health issues when mothers do not meet their breastfeeding goals (Jackson et al., 2021). Breastfeeding does not define “good” motherhood, and IBCLCs can emphasize a mother’s worth is not determined by a feeding method (Jackson et al., 2021; Woollard & Porter, 2017).
Conclusion
As breastfeeding initiation rates continue to rise, so do cases of breastfeeding successes and difficulties. When mothers experience difficulties, IBCLCs can help identify and redefine unrealistic expectations that exacerbate breastfeeding problems and contribute to poor maternal mental health. A successful breastfeeding relationship can take several forms.
Supplementary Material
Acknowledgments
The authors would like to thank Danielle Toth for her technical writing and editorial assistant with this work.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number K23NR019081 with Dr. Weber as Principal Investigator. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures and Conflicts of Interest
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Weber is the subject of the paper. Ms. Murphy was Dr. Weber’s mental health care provider. Ms. Notestine is an IBCLC who was not involved in Dr. Weber’s care. Ms. Elder is a research assistant in Dr. Weber’s lab.
Supplementary Material
Supplementary Material may be found in the “Supplemental material” tab in the online version of this article.
References
- Alcantara J, Alcantara JD, & Alcantara J (2015). The Chiropractic care of infants with breastfeeding difficulties. Explore, 11(6), 468–474. 10.1016/j.explore.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Beck CT (2021). Effects of fourth-degree perineal lacerations on women’s physical and mental health. Journal of Obstetric, Gynecologic & Neonatal Nursing, 0(0). 10.1016/j.jogn.2020.10.009 [DOI] [PubMed] [Google Scholar]
- Bonilla EP, & Riggs J (2020). Forceps delivery. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK538220/ [PubMed] [Google Scholar]
- Brown A, Rance J, & Bennett P (2016). Understanding the relationship between breastfeeding and postnatal depression: The role of pain and physical difficulties. Journal of Advanced Nursing, 72(2), 273–282. 10.1111/jan.12832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020, September 28). Facts about nationwide breastfeeding goals. https://www.cdc.gov/breastfeeding/data/facts.html
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry: The Journal of Mental Science, 150, 782–786. [DOI] [PubMed] [Google Scholar]
- Demirci J, Caplan E, Murray N, & Cohen S (2018). “I just want to do everything right:” Primiparous women’s accounts of early breastfeeding via an app-based diary. Journal of Pediatric Health Care, 32(2), 163–172. 10.1016/j.pedhc.2017.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias CC, & Figueiredo B (2015). Breastfeeding and depression: A systematic review of the literature. Journal of Affective Disorders, 171, 142–154. 10.1016/j.jad.2014.09.022 [DOI] [PubMed] [Google Scholar]
- Diebold A, Ciolino JD, Johnson JK, Yeh C, Gollan JK, & Tandon SD (2020). Comparing fidelity outcomes of paraprofessional and professional delivery of a perinatal depression preventive intervention. Administration and Policy in Mental Health, 47(4), 597–605. 10.1007/s10488-020-01022-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallon V, Groves R, Halford JCG, Bennett KM, & Harrold JA (2016). Postpartum anxiety and infant-feeding outcomes. Journal of Human Lactation, 32(4), 740–758. 10.1177/0890334416662241 [DOI] [PubMed] [Google Scholar]
- Feenstra MM, Jørgine Kirkeby M, Thygesen M, Danbjørg DB, & Kronborg H (2018). Early breastfeeding problems: A mixed method study of mothers’ experiences. Sexual & Reproductive Healthcare, 16, 167–174. 10.1016/j.srhc.2018.04.003 [DOI] [PubMed] [Google Scholar]
- Gianni ML, Bettinelli ME, Manfra P, Sorrentino G, Bezze E, Plevani L, Cavallaro G, Raffaeli G, Crippa BL, Colombo L, Morniroli D, Liotto N, Roggero P, Villamor E, Marchisio P, & Mosca F (2019). Breastfeeding difficulties and risk for early breastfeeding cessation. Nutrients, 11(10). 10.3390/nu11102266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover S, Avasthi A, & Jagiwala M (2020). Clinical practice guidelines for practice of supportive psychotherapy. Indian Journal of Psychiatry, 62(Suppl. 2), S173–S182. 10.4103/psychiatry.IndianJPsychiatry_768_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff CE, Movva N, Rosen Vollmar AK, & Pérez-Escamilla R (2019). Impact of maternal anxiety on breastfeeding outcomes: A systematic review. Advances in Nutrition, 10(5), 816–826. 10.1093/advances/nmy132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson L, De Pascalis L, Harrold J, & Fallon V (2021). Guilt, shame, and postpartum infant feeding outcomes: A systematic review. Maternal & Child Nutrition, e13141. 10.1111/mcn.13141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobst A, Krause D, Maiwald C, Härtl K, Myint A-M, Kästner R, Obermeier M, Padberg F, Brücklmeier B, Weidinger E, Kieper S, Schwarz M, Zill P, & Müller N (2016). Oxytocin course over pregnancy and postpartum period and the association with postpartum depressive symptoms. Archives of Women’s Mental Health, 19(4), 571–579. 10.1007/s00737-016-0644-2 [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K, Cong Z, & Hale TW (2015). Birth interventions related to lower rates of exclusive breastfeeding and increased risk of postpartum depression in a large sample. Clinical Lactation, 6(3), 87–97. 10.1891/2158-0782.6.3.87 [DOI] [Google Scholar]
- Labbok MH, & Starling A (2012). Definitions of breastfeeding: Call for the development and use of consistent definitions in research and peer-reviewed literature. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 7(6), 397–402. 10.1089/bfm.2012.9975 [DOI] [PubMed] [Google Scholar]
- Nation JA, Wertheim EH, & Worthington EL (2018). Evaluation of an online self-help version of the REACH forgiveness program: Outcomes and predictors of persistence in a community sample. Journal of Clinical Psychology, 74(6), 819–838. 10.1002/jclp.22557 [DOI] [PubMed] [Google Scholar]
- Nguyen AJ, Hoyer E, Rajhans P, Strathearn L, & Kim S (2019). A tumultuous transition to motherhood: Altered brain and hormonal responses in mothers with postpartum depression. Journal of Neuroendocrinology, 31(9), e12794. 10.1111/jne.12794 [DOI] [PubMed] [Google Scholar]
- Payne JL, & Maguire J (2019). Pathophysiological mechanisms implicated in postpartum depression. Frontiers in Neuroendocrinology, 52, 165–180. 10.1016/j.yfrne.2018.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira TRC, Souza FGD, & Beleza ACS (2017). Implications of pain in functional activities in immediate postpartum period according to the mode of delivery and parity: An observational study. Brazilian Journal of Physical Therapy, 21(1), 37–43. 10.1016/j.bjpt.2016.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters LL, Thornton C, de Jonge A, Khashan A, Tracy M, Downe S, Feijen-de Jong EI, & Dahlen HG (2018). The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age: A linked data population-based cohort study. Birth, 45(4), 347–357. 10.1111/birt.12348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reece-Stremtan S, Campos M, Kokajko L, & Academy of Breastfeeding Medicine. (2017). ABM Clinical Protocol #15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeeding Medicine, 12(9), 500–506. 10.1089/bfm.2017.29054.srt [DOI] [PubMed] [Google Scholar]
- Ritchie-Ewing G, Mitchell AM, & Christian LM (2019). Associations of maternal beliefs and distress in pregnancy and postpartum with breastfeeding initiation and early cessation. Journal of Human Lactation, 35(1), 49–58. 10.1177/0890334418767832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LJ (2007). Impact of birthing practices on the breastfeeding dyad. Journal of Midwifery & Women’s Health, 52(6), 621–630. 10.1016/j.jmwh.2007.07.019 [DOI] [PubMed] [Google Scholar]
- Stark EL, Shim J, Ross CM, & Miller ES (2021). The association between positive antenatal depression screening and breastfeeding initiation and continuation. American Journal of Perinatology, 38(2), 171–175. 10.1055/s-0039-1695775 [DOI] [PubMed] [Google Scholar]
- Swenson CW, DePorre JA, Haefner JK, Berger MB, & Fenner DE (2018). Postpartum depression screening and pelvic floor symptoms among women referred to a specialty postpartum perineal clinic. American Journal of Obstetrics and Gynecology, 218(3), 335.e1–335.e6. 10.1016/j.ajog.2017.11.604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woollard F, & Porter L (2017). Breastfeeding and defeasible duties to benefit. Journal of Medical Ethics, 43(8), 515–518. 10.1136/medethics-2016-103833 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


