Abstract
Background
Both medial pivot (MP) and rotating platform (RP) mobile-bearing (MB) total knee arthroplasty (TKA) have been developed to better mimic the natural knee kinematics and femoral roll back in flexion. The purpose of this retrospective study was to compare the mid-term functional outcomes and range of motion (ROM) of MP and RP types of total knee arthroplasty.
Methods
116 patients (mean age of 66.3 years) undergoing TKA (52 Medial pivot design and 64 Rotating Platform design) were evaluated retrospectively with Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) knee score, knee society score (KSS) with its subgroups namely, Knee Score (KSKS) and Functional Score (KSFS) and forgotten joint score (FJS) at a mean follow-up of 7.1 years. Range of motion (ROM) and tibiofemoral anatomic angle on the radiographs were also compared.
Results
Mean ROM, WOMAC and KSKS improved significantly from pre-operative to postoperative knees in both the groups. There was, however, no significant difference between the two groups at the final follow-up. In contrast, mean KSFS score improved to 89.5 ± 8.1 in MP group and 86.3 ± 7.1 in RP Group (p = 0.025), while mean FJS was 85.6 ± 4.1 and 80.9 ± 5.4 in the MP and RP groups, respectively (p = < 0.0001).
Conclusion
Satisfactory clinical and functional outcomes can be obtained using either a MP or RP knee joint in tricompartmental osteoarthritis of knee. The MP design scores better on the KSFS score and FJS than the RP-TKA.
Keywords: Knee, Osteoarthritis, Arthroplasty, Medial pivot, Mobile bearing
Introduction
Total knee Arthroplasty (TKA) is one of the most effective surgical interventions to relieve pain and restore function in patients with osteoarthritis (OA) of the knee. A factor that plays a vital role in the implant designing is the longevity. Each new design aims to improve patient outcomes, knee function, and implant survival. In the early 1990s, medial pivot (MP) design was developed [1]. This design consists of an asymmetric tibial insert which provide a deeper, highly constraint medial compartment and a less congruent lateral side of knee to allow relative freedom of antero-posterior movement of the lateral condyle [2]. Kinematics studies reveal that the knee moves with the medial compartment staying very nearly stable like a ball and socket joint, while the lateral femoral condyle moves front to back rotating around the center of the medial side during knee flexion [3]. This way it shifts the rotational axis medially and reproduces medial pivot motion of the normal knee.
The mobile-bearing (MB) design TKA was first developed in 1980s as the meniscal bearing concept which was later modified into rotating platform (RP) design. This design offers many theoretical advantages. First, it involves antero-posterior translation of the femur and internal rotation of the tibia with deep knee flexion which reproduces and can accommodate a more physiologic pattern of movement [4]. Second, it reduces the polyethylene contact stresses and wears resulting in a lower rate of aseptic loosening as it reduces the forces transferred to the tibial component and bone–cement interfaces [5, 6]. Wear is also reduced as the rolling/sliding curvilinear motion is separated from the transverse axial rotation motion onto two separate articulating surfaces [7]. Finally, it self-corrects the rotational mismatch between the tibia and femur which optimizes patella-femoral tracking and reduces the anterior knee pain [8, 9].
Although the outcomes for both the designs have described widely, their comparison is scarcely studied. Further, the data comparing the MP design with other designs of TKA in the Indian population are very limited with no mid- or long-term study having compared the two. The authors wished to answer this question and, thus, designed the study to assess and compare the clinical and functional outcomes of the MP-TKA and RP-TKA in the Indian population at a mid-term follow-up.
Materials and Methods
A retrospective, comparative, single-center study was performed at a tertiary care hospital in Western India after the approval from the institutional ethics committee to compare medial pivot (MP) and rotating platform (RP) mobile-bearing designs of TKA with a minimum 6 years of follow-up. All the patients who underwent TKA with either of the two implants were included in the study. We used our prospectively collected institutional joint registry and examined the electronic medical records of all the patients who underwent a primary TKA between January 2013 and May 2015. The patients were then divided into two groups based on the implant design used for the respective patient. The decision to use either an MP or RP design was based solely on the availability of the implants at our institution. Informed consent was obtained from all patients before the study.
We included all the patients between 50 and 80 years of age with a minimum follow-up of 6 years who were operated with a primary total knee arthroplasty using either the MP or the RP design for an established diagnosis of primary knee osteoarthritis grade 4 according to the Kellgren and Lawrence system of classification of OA of knee joint. All the patients were ambulatory before surgery. Exclusion criteria included medio-lateral instability and fixed flexion deformity greater than 15 degrees, previous surgery of knee joint, traumatic knee arthritis, presence of active infection or secondary arthritis due to inflammatory diseases and patients with diagnosed systemic disease such as bone diseases, immunologically suppressed conditions, neuromuscular deficits and Complex Regional Pain Syndrome that would have affected the overall outcome of the study.
Operative Technique
All the medial pivot implants were Advance® Medial-Pivot Knee System from Wright Medical Technology, Inc. whereas mobile-bearing implant were P.F.C.® Sigma™ Rotating platform Mobile-bearing Total Knee System from Depuy-Synthes. All the surgeries were performed by a single surgeon using a midline skin incision. A tourniquet was used in all the cases and a medial para-patellar approach was used. The bone cuts were made using a measured resection technique. Proximal tibial cut was performed using extra-medullary tibial cutting guide by taking 0° of posterior slope for mobile-bearing TKA, while three degrees of posterior slope used for medial pivot design (angle of the tibial cutting guide provided by the manufacturer). All osteophytes were removed. The tibial cut was followed by distal femoral cut using intramedullary guide. Anterior-referencing method was used to select the size of the femoral component. The rotation of the femoral component was determined as 3°–5° of external rotation using the trans-epicondylar axis, Whiteside’s line and posterior condylar axis.
The posterior cruciate ligament (PCL) was sacrificed in all TKAs. The patella was selectively resurfaced when it was deformed by arthritis or when erosion of the native articular cartilage involved > 50% of the surface (Outerbridge grade III or IV). Normal patellar tracking was confirmed using the no-thumb technique.
In all cases, fixation of the components (femoral and tibial) was performed using a cemented technique. All patients followed a similar standard postoperative rehabilitation protocol including postoperative antibiotics for 5 days, postoperative range of motion exercises, and weight bearing as tolerated with crutches on postoperative day 1. Deep vein thrombosis prophylaxis was given to all patients.
Assessment
Patients were contacted on a regular basis and postoperative examinations were performed at 3, 6 months, and 1 year after surgery, and annually thereafter. Clinical and radiological data were obtained from these patients.
Two independent investigators repetitively performed all clinical and radiological data obtained at each follow-up to reduce observational bias and mean of two values obtained by both the observers were taken into consideration. Knee ROM of all the patients was evaluated in the supine position using a standard long arm goniometer preoperatively and a mean flexion angle was obtained [10]. Functional evaluation was done using WOMAC, Knee society score and forgotten joint score preoperatively and at each follow-up [11, 12]. Patient satisfaction was also assessed with the visual analog scale (VAS). The patients were asked about their satisfaction with the surgery at the last follow-up from either fully dissatisfied, somewhat dissatisfied, somewhat satisfied or fully satisfied. A Minimal Clinically Important Difference was also calculated for the WOMAC score at 1 year and Knee Society Objective and Functional Scores. The MCID was defined as per the published literature [13, 14].
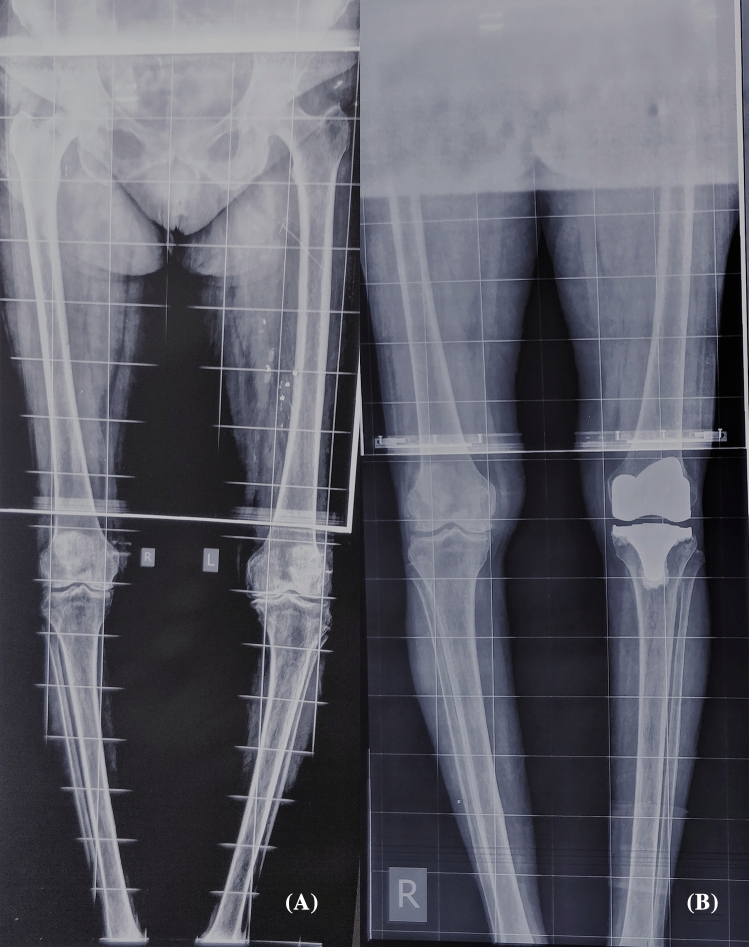
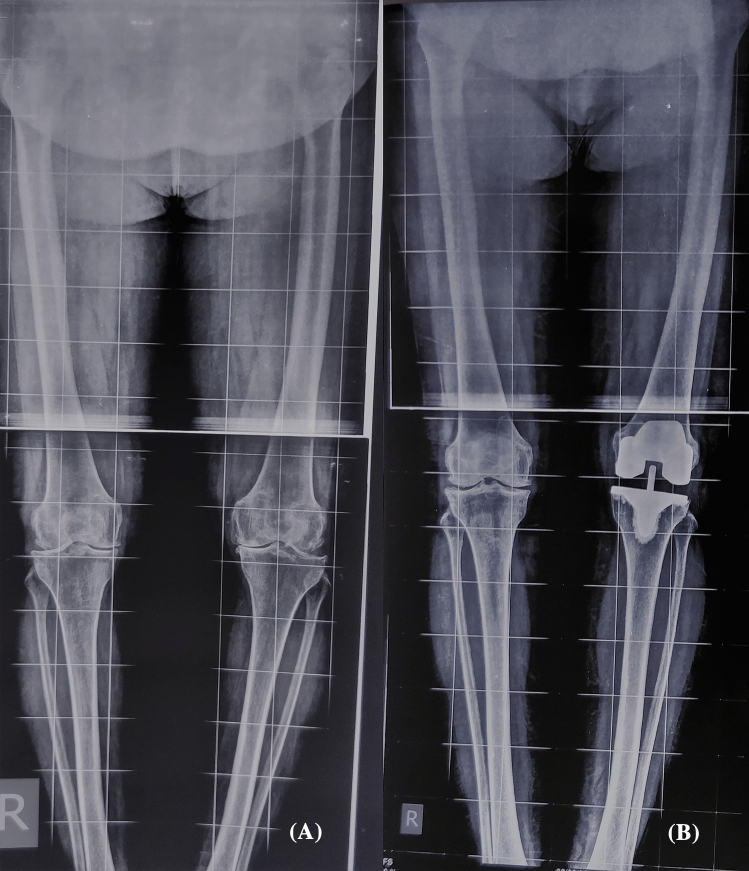
Standard radiographs were obtained before and after surgery which included antero-posterior and lateral view in supine and standing position. Skyline view and hip–knee–ankle scannogram views were obtained for assessment of the alignment of the limb. Radiographs were assessed for the position of the component, presence and location of all radiolucent lines at the bone–cement interface and any osteolysis around the components (Figs. 1, 2).
Fig. 1.
A Preoperative radiographs of a 57-year-old female show osteoarthritis of knees. B Postoperative radiographs of left-side TKA with medial pivot implant design
Fig. 2.
A Preoperative radiographs of a 64-year-old female show osteoarthritis of knees. B Postoperative radiographs of left-side TKA with mobile-bearing rotating platform implant design
Statistical Analysis
The statistical analysis was performed by SPSS 23.0 version. Continuous variables were described as mean and variation of each observation from the mean value represented as mean ± standard deviation (analyzed using independent t test). Categorical variables were described by taking percentages and were analyzed using Chi square test or Fisher exact test when appropriate. Intragroup variable analysis was done using paired t test. Variables with p value < 0.05 was considered as statistically significant.
Results
Total 116 patients were included of which 54 patients belonged to the MP group and 62 to the RP group. The average follow-up period was 7.1 ± 1.1 years (range 6.0–8.3 years). The mean age, gender distribution, side of the surgery and BMI were comparable among the two groups. Patella was resurfaced in 36 and 40 patients in MP and RP groups, respectively (p = 0.57) (Table 1).
Table 1.
Patient demographics
| Variable | MP (n = 52) | RP (n = 64) | p value |
|---|---|---|---|
| Age in years (mean ± standard deviation) | 67.1 ± 5.6 | 65.9 ± 6.1 | 0.28 |
| Gender (M:F) | 24:28 | 26:38 | 0.68 |
| Side (R:L) | 27:25 | 34:30 | 0.95 |
| BMI in kg/m2 (mean ± standard deviation) | 26.9 ± 3.5 | 27.5 ± 3.0 | 0.32 |
| Comorbidities | |||
| Hypertension | 19 | 20 | 0.69 |
| Diabetes mellitus | 16 | 20 | 0.88 |
| Cardiac disease | 14 | 19 | 0.90 |
| COPD | 7 | 5 | 0.49 |
| Thyroid disorder | 4 | 4 | 0.95 |
| Dyslipidaemia | 13 | 16 | 0.83 |
| Smoking | 9 | 12 | 0.97 |
| Patellar resurfacing | 36 | 40 | 0.57 |
| Follow-up (mean ± standard deviation) | 7.3 ± 1.1 | 7.0 ± 1.2 | 0.18 |
A p value < 0.05 is considered to be significant
MP medial pivot, RP rotating platform, BMI body mass index, R:L right:left, M: F male:female, COPD chronic obstructive pulmonary disorder
The range of motion was improved significantly post-operatively in both the groups. At the last follow-up, the ROM had increased to 119.6 ± 10.1 from 101.7 ± 12.2 preoperatively in the MP group (p < 0.0001). Similarly, the ROM in the RP group improved to 120.5 ± 8.4 at the last follow-up from 103.2 ± 13.9 preoperatively. The improvement was comparable among the groups (p < 0.0001). VAS score too was significantly improved in both the groups at each follow-up but was comparable on the inter-group comparison (p = 0.28). A similar trend was observed for WOMAC score and Objective Knee Score. This implied that VAS, WOMAC and Objective KSS were not affected by the design of implants used in TKA (Tables 2, 3).
Table 2.
Preoperative clinical and functional scores:
| MP (n = 52) | RP (n = 64) | p value | |
|---|---|---|---|
| Visual analog scale | 7.2 ± 0.6 | 7.0 ± 0.8 | 0.14 |
| Preoperative range of motion (°) | 101.7 ± 12.2 | 103.2 ± 13.9 | 0.54 |
| WOMAC score | 36.3 ± 2.5 | 36.9 ± 3.1 | 0.26 |
| Knee Society objective score | 34.0 ± 7.9 | 35.5 ± 9.2 | 0.35 |
| Knee Society functional score | 43.9 ± 11.2 | 44.3 ± 9.6 | 0.60 |
| Femorotibial angle (°) | Varus 14.1 ± 3.1 | Varus 13.5 ± 2.8 | 0.28 |
Values are presented as mean ± standard deviation. A p value < 0.05 is considered to be significant
MP medial pivot, RP rotating platform, WOMAC Western Ontario and McMaster Universities Osteoarthritis Index
Table 3.
Clinical and functional scores at the final follow-up
| MP (n = 52) | RP (n = 64) | p value | |
|---|---|---|---|
| Range of motion (°) | 119.6 ± 10.1 | 120.5 ± 8.4 | 0.60 |
| Visual analog scale | 1.3 ± 1.1 | 1.5 ± 0.9 | 0.28 |
| WOMAC score | 84.5 ± 4.2 | 83.9 ± 3.8 | 0.42 |
| Knee Society Knee score | 91.1 ± 6.0 | 90.9 ± 5.5 | 0.85 |
| Knee Society functional score | 89.5 ± 8.1 | 86.3 ± 7.1 | 0.025 |
| Forgotten joint score | 85.6 ± 4.1 | 80.9 ± 5.4 | < 0.0001 |
| Femorotibial angle (°) | Valgus 5.0 ± 3.1 | Valgus 5.3 ± 2.2 | 0.60 |
| Patient satisfaction rating | |||
| Fully satisfied | 47 | 56 | 0.84 |
| Somewhat satisfied | 2 | 4 | |
| Somewhat dissatisfied | 3 | 4 | |
| Fully dissatisfied | 0 | 0 | |
Values are presented as mean ± standard deviation. A p value < 0.05 is considered to be significant
MP medial pivot, RP rotating platform, WOMAC Western Ontario and McMaster Universities Osteoarthritis Index
In contrast, the improvement in the Functional knee society score was significantly better in the MP group as compared to the RP group (p = 0.025). It improved from a pre-operative score of 43.9 ± 11.2 to 89.5 ± 8.1 (p < 0.0001) at the final follow-up in the MP group compared to an improvement from 44.3 ± 9.6 to 84.3 ± 7.1 in the RP group (p < 0.0001) (Tables 2, 3). The MCID attainment for the WOMAC and Knee Society Objective and Functional scores was seen in all the patients thus showing that the improvement in the outcomes necessary for a positive patient perception was seen in all the patients. The overall satisfaction rating was also similar at the final follow-up among the two groups.
We found a statistically significantly better overall mean Forgotten joint score in the MP group as compared to the RP group (Table 3) (p = < 0.0001). We also noted that patients in MP group scored more on the question “Are you aware of your artificial joint when you are standing up from a low-sitting position”. The mean score for the question was 2.6 ± 1.3 for the MP group and 3.4 ± 1.6 for the RP group (p = 0.004).
Mean pre-operative anatomical femorotibial angle was found to be in varus for all the patients. It was 14.1° ± 3.1° and 13.5° ± 2.8° in the MP and RP groups, respectively (p = 0.28). Mean anatomical femorotibial angle at the last follow-up was 5.0° ± 3.1° valgus and 5.3° ± 2.2° of valgus, respectively, in the MP and RP groups (p = 0.60), indicating a significant correction of the deformity in both the groups (p < 0.001).
In terms of the complications observed, three patients in each group had a residual flexion deformity in the range of 5°–15°. One patient in each group had wound gaping which was managed with local debridement which eventually healed by secondary intention. Two patients in the MP group and three patients in the RP group had non-progressive radiolucent lines measuring < 1 mm at the final follow-up which were not associated with any clinical finding. There were no cases of progressive osteolysis or aseptic loosening in any of the patients included in this study. There were no clinically significant complications during the follow-up.
Discussion
The search for an ideal implant for knee arthroplasty that can completely mimic the native knee biomechanics and, thus, result in a better outcome and at the same time lead to an acceptable longevity has led to the wide variety of implant designs for TKA seen presently. Although each design has its own theoretical advantages and disadvantages, the overall patient satisfaction has been found to be variable with every design. One such design is the Medial Pivot TKA that is modeled to provide a higher stability and lead to a better longevity by decreasing the polyethylene wear and osteolysis using a highly conforming design. The present study thus compared the MP design with the other design used very commonly, i.e., Posterior-stabilized mobile-bearing TKA.
A number of researchers have showed that the MP design provides better outcomes at mid-term and long term [15–19]. Bordini et al. reported good outcomes of the Advance MP-TKA, having a 10-year survivorship estimate of 96.6% for the MP-TKA, higher than all other cemented TKA types [15]. Fan et al. observed a significant improvement in the pain score, ROM and KSS at a minimum 5-year follow-up. They achieved a mean ROM of 115.4° [16]. Similarly, Karachalios and Chinzei noted significant improvements in the functional scores at a mean of 13.4 and 8 years, respectively [17, 19]. This was attributed to its ability to mimic the natural kinematics of the knee, specifically more natural femoral rollback. It is also said to reduce contact stresses and polyethylene wear on medial side due to its large contact area, and thus providing better outcomes at mid- and long terms [2].
The MP design has also been compared to the other commonly used designs for TKA. However, no mid- or long-term study comparing the two in the Indian population is available in the literature and the present study is the first one to compare the mid-term outcomes of MP design with any other design of TKA. Kulshrestha et al. compared the outcomes between MP and fixed-bearing PS designs in the Indian population over a 2-year follow-up and found comparable KSS and FJS [20]. Bae et al. using KSS scores and WOMAC score found no significant difference in the functional outcome between the MP-TKA and PS-TKA [21]. Similarly, Shi et al. reported similar improvements in the KSS and WOMAC scores for both the MP and PS groups in the Chinese population at mid-term follow-up [22]. Hossain et al. in his study reported that MP-TKA has a more favorable outcome over the Fixed-bearing PS-TKA in terms of physical elements of the SF-36 and Total Knee Function Questionnaire scoring [23]. Samy et al. in his retrospective study reported an improvement in the FJS in the medial pivot TKA group comparing with PS prosthesis group of patients particularly with regards to deep knee flexion and stability of the prosthesis [24]. It is comparable to the present study which also concludes that mean FJS scores are favorable in MP-TKA group compared to RP-TKA patients. We have included FJS as a tool to measure functional outcome as it provides a better measure of high-end functionality post arthroplasty.
Benjamin et al. compared the MP-TKA with a PS single-radius design and found similar results in the gait analysis and the functional outcome scores [25]. Another study comparing the MP and RP designs found similar kinematic gait analysis [26]. On the contrary Kim et al. in his randomized clinical trial of consecutive series of bilateral single-stage TKAs on 92 patients found worse early clinical outcome in terms of Knee Society (p = 0.021) and Hospital for Special Surgery knee scores (p = 0.023) for medial Pivot fixed-bearing prosthesis while comparing with the PFC Sigma mobile-bearing prosthesis [27]. In their long-term analysis as well, they observed worse functional and radiological outcomes as well as an inferior ROM and patient satisfaction [28]. They speculated that the inferior results in the MP group could be due to the high constraint secondary to the fully congruent medial tibiofemoral articulation that in turn hampers the restoration of the normal knee kinematics. Our results were, however, in contrast and could be due to a different patient profile and the higher rate of infections in the MP group as compared to the RP group which would negatively affect the outcome measures.
We also compared the functional outcomes in terms of the achievement of a minimal clinically important difference (MCID). The MCID is defined as the difference in the mean change in the individual score between patients with no improvement compared with those with little improvement according to the anchor question. It signifies the minimal change in the respective score that was perceived by the patient as beneficial. It was reported to be 10 for the WOMAC score, 6.4 for Knee society functional score and 5.9 for Knee society subjective score [13, 14]. We estimated the MCID attainment for KSFS and KSOS at 2 years and for WOMAC at 1 year post-operatively as described by the respective authors. MCID was attained for all the patients for all the scores which further showed that each patient experienced at least some perceived improvement.
The significantly better KSFS and FJS and similar WOMAC and KSKS at the final follow-up in the MP group when compared to the RP group is an interesting finding. We believe that the difference could have arisen due to the variability in the individual components of the various scoring systems. For example, WOMAC score measures the outcomes in terms of pain, stiffness and other symptoms in addition to the functional outcomes. Similarly, KSKS mainly involves the measurement of various objective criteria. In contrast, KSFS and FJS involve the quantification of the subjective outcomes and do not take into account the specific objective clinical measurements. An individual may be able to tolerate better the issues of swelling, stiffness and slight pain as long as his/her functional demands are met, thus scoring better on systems that measure the functional outcome as compared to those that measure mainly the objective criteria. The abovementioned observation, thus, implies that the MP design, due to its design characteristics, leads to better subjective outcomes compared to the RP design. The objective and other clinical criteria, however, remain similar. Moreover, the older age patient population in our study may hold significance as they tend to have limited functional demands compared to a relatively younger population who have relatively higher functional demands.
In our study, ROM improved post-operatively in both the groups but showed no significant difference between the MP-TKA and RP-TKA designs. Shakespeare et al. reported a mean flexion angle of 111° in the MP group while 109° flexion in the PS group at one-year follow-up (p = 0 0.110) [29]. These mean angles are lower than other clinical studies. However, the patients in this study had lower pre-operative flexion angles which could be a responsible factor for these results. Similarly, Vecchini et al. in their study reported that mean range of motion was improved from 97.7° to 112.5°, respectively (p < 0.001), using the Advance medial pivot prosthesis at mean 7-year follow-up [30]. On the contrary, another study showed that regression analysis of an individual knee revealed a small (average, 2.9°) but greater loss of flexion at 12-month follow-up with the medial pivot fixed-bearing prosthesis [27]. Kulshrestha et al., however, observed that a Fixed-bearing PS design provided a greater gain in knee flexion as compared to the MP group [20].
In all our medial pivot design cases, we sacrificed posterior cruciate ligament. Initially, in literature, there was a controversy regarding PCL, whether its retention is necessary or not. Karachalios T et al. reported no significant differences in functional outcomes when PCL was either retained or sacrificed, provided appropriate soft tissue balance was obtained during the surgery [17]. Similarly, Bae et al. in his study reported satisfactory clinical results in medial pivot TKA, whether PCL is sacrificed or not [31]. However, knees with PCL sacrificed showed better ROM compared to knees with PCL retention but that was not statistically significant. Authors also noted that accurate soft tissue balancing in both extension and flexion is more important. If such a balance is not possible, then the posterior cruciate ligament should be resected.
One interesting finding in our study we noted was that the patients with medial pivot design prosthesis were more comfortable when they were asked to stand from low-sitting position and climbing stairs up and down as compared to the PS RP design. This was also seen by Samy et al. [24]. It was supposed to be due to a higher mid-flexion instability seen in the PS design. In contrast, the MP design has an inherent stability due its design which leads to a better mid-flexion stability. PS design generates very high contact stress at the post-cam mechanism and can, thus, lead to instability when the knee is extended from high flexion as in the action of getting up from the sitting position [32].
In our study, we encountered some limitations. First, it represents a retrospective comparison of two cohorts undergoing total knee arthroplasty with use of two different designs. Although the groups were similar in age, sex, clinical characteristics, and pre-operative function, a prospective randomized study would have limited the bias and other potentially confounding variables. Second, sample size is limited and thus could provide less power to detect small changes in clinical function. Third, there could be an element of selection bias while selecting the cohort for 2 groups in the form of unknown confounding variables; however, as there was no statistically significant difference in pre-operative ROM and functional score between the two groups, it could be negligible. We have also not analyzed the radiographic variables in detail which could further shed light on the association between the clinical, functional and radiological outcomes. Finally, other issues such as selective patellar resurfacing in both groups could have affected the results. A long-term, prospective, randomized comparative study with a larger sample size to provide adequate power to the study will be very helpful in demonstrating the advantages in terms of the functional and satisfaction scores as well as the longevity of the implant design, if any. In this study, a single surgeon had performed all TKA who had good expertise in using both the designs (MP-TKA and RP-TKA) before starting this study. The surgeon did not use any selective criteria for the use of a specific implant for a specific patient. All patients in this study were consistent with their long-term follow-up. These factors offer great strength to this study. The authors also plan to follow up the patients for an analysis of the long-term outcomes.
In conclusion, we found that there is no significant difference in the improvement of the ROM post-operatively between MP-TKA and RP-TKA. However, patients with MP-TKA scored better on functional knee society score and forgotten joint score owing to better mid-flexion stability compared to RP-TKA group. Other clinical and radiological outcome were comparable.
Abbreviations
- TKA
Total knee arthroplasty
- ROM
Range of motion
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
- KSS
Knee society score
- FJS
Forgotten joint score
- OA
Osteoarthritis
- MP
Medial pivot
- MB
Mobile bearing
- RP
Rotating platform
- PCL
Posterior cruciate ligament
- VAS
Visual analog scale
- BMI
Body mass index
- PS
Posterior stabilized
Author Contributions
AS had designed this study, Vijay Singh had performed all surgeries which are included in this study, RA and AS had substantively revised the manuscript, NM had analyzed and interpreted the patient data. VW and AJ had collected all data for this study, AS and RA had drafted the article. All authors had read and approved the final manuscript.
Funding
Nil.
Availability of Data and Material
We had used our prospectively collected institutional total joint registry and examined the electronic medical records of all patients who underwent a primary TKA from January 2013 to April 2015.
Declarations
Conflict of interest
Akash Shakya, Vijay Singh, Romit Agrawal, Ayush Sharma, Nilesh Mangale, Venkatramana Wadgave, Ajay Jaiswal declare that they have no conflict of interest.
Ethics approval and consent to participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Akash Shakya, Email: akashshakya.gmc@gmail.com.
Vijay Singh, Email: vijay201080@gmail.com.
Romit A. Agrawal, Email: romitagrawal2588@gmail.com
Ayush Sharma, Email: drayush@gmail.com.
Nilesh Mangale, Email: nbmangale28@gmail.com.
Venkatramana Wadgave, Email: venkatwadgave28@gmail.com.
Ajay Jaiswal, Email: jaisajay66@gmail.com.
References
- 1.Dalury DF, Barrett WP, Mason JB, Goldstein WM, Murphy JA, Roche MW. Midterm survival of a contemporary modular total knee replacement: a multicentre study of 1970 knees. The Journal of Bone and Joint Surgery British volume. 2008;90:1594–1596. doi: 10.1302/0301-620X.90B12.21064. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt, R., Komistek, R. D., Blaha, J. D., Penenberg, B. L., & Maloney, W. J. (2003). Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clinical Orthopaedics and Related Research, (410), 139–147. 10.1097/01.blo.0000063565.90853.a4 [DOI] [PubMed]
- 3.Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. Journal of Biomechanics. 2005;38:197–208. doi: 10.1016/j.jbiomech.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Nakamura E, Banks SA, Tanaka A, Sei A, Mizuta H. Three-dimensional tibiofemoral kinematics during deep flexion kneeling in a mobile-bearing total knee arthroplasty. Journal of Arthroplasty. 2009;24(7):1120–1124. doi: 10.1016/j.arth.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Argenson JN, O’Connor JJ. Polyethylene wear in meniscal knee replacement. A one to nine-year retrieval analysis of the Oxford knee. The Journal of Bone and Joint Surgery British volume. 1992;74(2):228–232. doi: 10.1302/0301-620X.74B2.1544958. [DOI] [PubMed] [Google Scholar]
- 6.Buechel FF, Insall JN, Scott WN, Scuderi GR. Low contact stress meniscal bearing knee replacement: design concepts, failure mechanisms and long-term survivorship. Current concepts in primary and revision total knee arthroplasty. Lippincott-Raven; 1996. pp. 47–64. [Google Scholar]
- 7.Jones VC, Barton DC, Fitzpatrick DP, Auger DD, Stone MH, Fisher J. An experimental model of tibial counterface polyethylene wear in mobile bearing knees: The influence of design and kinematics. BioMedical Materials and Engineering. 1999;9:189–196. [PubMed] [Google Scholar]
- 8.Li YL, Wu Q, Ning GZ, Feng SQ, Wu QL, Li Y, Hao Y. No difference in clinical outcome between fixed- and mobile-bearing TKA: A meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(3):565–575. doi: 10.1007/s00167-012-2313-y. [DOI] [PubMed] [Google Scholar]
- 9.Capella M, Dolfin M, Saccia F. Mobile bearing and fixed bearing total knee arthroplasty. Annals of Translational Medicine. 2016;4(7):127. doi: 10.21037/atm.2015.12.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gogia PP, Braatz JH, Rose SJ, Norton BJ. Reliability and validity of goniometric measurements at the knee. Physical Therapy. 1987;67:192–195. doi: 10.1093/ptj/67.2.192. [DOI] [PubMed] [Google Scholar]
- 11.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clinical Orthopaedics and Related Research. 1989;248:13–14. doi: 10.1097/00003086-198911000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: Validation of a new patient-reported outcome measure. The Journal of Arthroplasty. 2012;27:430.e1–436.e1. doi: 10.1016/j.arth.2011.06.035. [DOI] [PubMed] [Google Scholar]
- 13.Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. What is the minimum clinically important difference for the WOMAC Index after TKA? [published correction appears in Clin Orthop Relat Res. 2020 Apr; 478(4):922] Clinical Orthopaedics and Related Research. 2018;476(10):2005–2014. doi: 10.1097/CORR.0000000000000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(11):3354–3359. doi: 10.1007/s00167-016-4208-9. [DOI] [PubMed] [Google Scholar]
- 15.Bordini B, Ancarani C, Fitch DA. Long-term survivorship of a medial-pivot total knee system compared with other cemented designs in an arthroplasty registry. Journal of Orthopaedic Surgery and Research. 2016;11:44. doi: 10.1186/s13018-016-0388-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fan CY, Hsieh JT, Hsieh MS, Shih YC, Lee CH. Primitive results after medial pivot knee arthroplasties: a minimum 5-year follow-up study. The Journal of Arthroplasty. 2010;25:492–496. doi: 10.1016/j.arth.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 17.Karachalios T, Roidis N, Giotikas D, Bargiotas K, Varitimidis S, Malizos KN. A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. The Knee. 2009;16:484–488. doi: 10.1016/j.knee.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Fitch DA, Sedacki K, Yang Y. Mid- to long-term outcomes of a medial-pivot system for primary total knee replacement: A systematic review and metaanalysis. Bone and Joint Research. 2014;3:297–304. doi: 10.1302/2046-3758.310.2000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chinzei N, Ishida K, Tsumura N, Matsumoto T, Kitagawa A, Iguchi T, et al. Satisfactory results at 8 years mean follow-up after ADVANCE® medial-pivot total knee arthroplasty. The Knee. 2014;21:387–390. doi: 10.1016/j.knee.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Kulshrestha V, Sood M, Kanade S, Kumar S, Datta B, Mittal G. Early outcomes of medial pivot total knee arthroplasty compared to posterior-stabilized design: A randomized controlled trial. Clinics in Orthopedic Surgery. 2020;12(2):178–186. doi: 10.4055/cios19141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bae DK, Cho SD, Im SK, Song SJ. Comparison of midterm clinical and radiographic results between total knee arthroplasties using medial pivot and posterior-stabilized prosthesis-a matched pair analysis. The Journal of Arthroplasty. 2016;31:419–424. doi: 10.1016/j.arth.2015.09.038. [DOI] [PubMed] [Google Scholar]
- 22.Shi W, Jiang Y, Wang C, Zhang H, Wang Y, Li T. Comparative study on mid- and long-term clinical effects of medial pivot prosthesis and posterior-stabilized prosthesis after total knee arthroplasty. Journal of Orthopaedic Surgery and Research. 2020;15(1):421. doi: 10.1186/s13018-020-01951-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hossain F, Patel S, Rhee SJ, Haddad FS. Knee arthroplasty with a medially conforming ball-and-socket tibiofemoral articulation provides better function. Clinical Orthopaedics and Related Research. 2011;469:55–63. doi: 10.1007/s11999-010-1493-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samy, D. A., Wolfstadt, J. I., Vaidee, I., & Backstein, D. J. (2018). A retrospective comparison of a medial pivot and posterior-stabilized total knee arthroplasty with respect to patient-reported and radiographic outcomes. The Journal of Arthroplasty, 33(5), 1379–1383. 10.1016/j.arth.2017.11.049 [DOI] [PubMed]
- 25.Benjamin B, Pietrzak JRT, Tahmassebi J, Haddad FS. A functional comparison of medial pivot and condylar knee designs based on patient outcomes and parameters of gait. The Bone and Joint Journal. 2018;100-B(1 Supple A):76–82. doi: 10.1302/0301-620X.100B1.BJJ-2017-0605.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Papagiannis GI, Roumpelakis IM, Triantafyllou AI, Makris IN, Babis GC. No differences identified in transverse plane biomechanics between medial pivot and rotating platform total knee implant designs. Journal of Arthroplasty. 2016;31(8):1814–1820. doi: 10.1016/j.arth.2016.01.050. [DOI] [PubMed] [Google Scholar]
- 27.Kim YH, Yoon SH, Kim JS. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clinical Orthopaedics and Related Research. 2009;467(2):493–503. doi: 10.1007/s11999-008-0221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim YH, Park JW, Kim JS. Clinical outcome of medial pivot compared with press-fit condylar sigma cruciate-retaining mobile-bearing total knee arthroplasty. Journal of Arthroplasty. 2017;32(10):3016–3023. doi: 10.1016/j.arth.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 29.Shakespeare D, Ledger M, Kinzel V. Flexion after total knee replacement. A comparison between the medial pivot knee and a posterior stabilised implant. The Knee. 2006;13:371–373. doi: 10.1016/j.knee.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Vecchini E, Christodoulidis, Magnan B, Ricci M, Regis D, Bartolizzi Clinical and radiologic outcomes of total knee arthroplasty using the Advance Medial Pivot prosthesis. A mean 7 years follow-up. The Knee. 2012;19:851–855. doi: 10.1016/j.knee.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Bae DK, Song SJ, Cho SD. Clinical outcome of total knee arthroplasty with medial pivot prosthesis. The Journal of Arthroplasty. 2011;26:693–698. doi: 10.1016/j.arth.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 32.Nakayama K, Matsuda S, Miura H, Iwamoto Y, Higaki H, Otsuka K. Contact stress at the post-cam mechanism in posterior-stabilised total knee arthroplasty. The Journal of Bone and Joint Surgery British. 2005;87:483–488. doi: 10.1302/0301-620X.87B4.15684. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We had used our prospectively collected institutional total joint registry and examined the electronic medical records of all patients who underwent a primary TKA from January 2013 to April 2015.