Key Points
Question
What is the risk of myocarditis after mRNA-based COVID-19 vaccination in the US?
Findings
In this descriptive study of 1626 cases of myocarditis in a national passive reporting system, the crude reporting rates within 7 days after vaccination exceeded the expected rates across multiple age and sex strata. The rates of myocarditis cases were highest after the second vaccination dose in adolescent males aged 12 to 15 years (70.7 per million doses of the BNT162b2 vaccine), in adolescent males aged 16 to 17 years (105.9 per million doses of the BNT162b2 vaccine), and in young men aged 18 to 24 years (52.4 and 56.3 per million doses of the BNT162b2 vaccine and the mRNA-1273 vaccine, respectively).
Meaning
Based on passive surveillance reporting in the US, the risk of myocarditis after receiving mRNA-based COVID-19 vaccines was increased across multiple age and sex strata and was highest after the second vaccination dose in adolescent males and young men.
Abstract
Importance
Vaccination against COVID-19 provides clear public health benefits, but vaccination also carries potential risks. The risks and outcomes of myocarditis after COVID-19 vaccination are unclear.
Objective
To describe reports of myocarditis and the reporting rates after mRNA-based COVID-19 vaccination in the US.
Design, Setting, and Participants
Descriptive study of reports of myocarditis to the Vaccine Adverse Event Reporting System (VAERS) that occurred after mRNA-based COVID-19 vaccine administration between December 2020 and August 2021 in 192 405 448 individuals older than 12 years of age in the US; data were processed by VAERS as of September 30, 2021.
Exposures
Vaccination with BNT162b2 (Pfizer-BioNTech) or mRNA-1273 (Moderna).
Main Outcomes and Measures
Reports of myocarditis to VAERS were adjudicated and summarized for all age groups. Crude reporting rates were calculated across age and sex strata. Expected rates of myocarditis by age and sex were calculated using 2017-2019 claims data. For persons younger than 30 years of age, medical record reviews and clinician interviews were conducted to describe clinical presentation, diagnostic test results, treatment, and early outcomes.
Results
Among 192 405 448 persons receiving a total of 354 100 845 mRNA-based COVID-19 vaccines during the study period, there were 1991 reports of myocarditis to VAERS and 1626 of these reports met the case definition of myocarditis. Of those with myocarditis, the median age was 21 years (IQR, 16-31 years) and the median time to symptom onset was 2 days (IQR, 1-3 days). Males comprised 82% of the myocarditis cases for whom sex was reported. The crude reporting rates for cases of myocarditis within 7 days after COVID-19 vaccination exceeded the expected rates of myocarditis across multiple age and sex strata. The rates of myocarditis were highest after the second vaccination dose in adolescent males aged 12 to 15 years (70.7 per million doses of the BNT162b2 vaccine), in adolescent males aged 16 to 17 years (105.9 per million doses of the BNT162b2 vaccine), and in young men aged 18 to 24 years (52.4 and 56.3 per million doses of the BNT162b2 vaccine and the mRNA-1273 vaccine, respectively). There were 826 cases of myocarditis among those younger than 30 years of age who had detailed clinical information available; of these cases, 792 of 809 (98%) had elevated troponin levels, 569 of 794 (72%) had abnormal electrocardiogram results, and 223 of 312 (72%) had abnormal cardiac magnetic resonance imaging results. Approximately 96% of persons (784/813) were hospitalized and 87% (577/661) of these had resolution of presenting symptoms by hospital discharge. The most common treatment was nonsteroidal anti-inflammatory drugs (589/676; 87%).
Conclusions and Relevance
Based on passive surveillance reporting in the US, the risk of myocarditis after receiving mRNA-based COVID-19 vaccines was increased across multiple age and sex strata and was highest after the second vaccination dose in adolescent males and young men. This risk should be considered in the context of the benefits of COVID-19 vaccination.
This descriptive study compares the effect of mRNA-based COVID-19 vaccination with BNT162b2 (Pfizer-BioNTech) vs mRNA-1273 (Moderna) on the reported cases of myocarditis in the US after each vaccination dose.
Introduction
Myocarditis is an inflammatory condition of the heart muscle that has a bimodal peak incidence during infancy and adolescence or young adulthood.1,2,3,4 The clinical presentation and course of myocarditis is variable, with some patients not requiring treatment and others experiencing severe heart failure that requires subsequent heart transplantation or leads to death.5 Onset of myocarditis typically follows an inciting process, often a viral illness; however, no antecedent cause is identified in many cases.6 It has been hypothesized that vaccination can serve as a trigger for myocarditis; however, only the smallpox vaccine has previously been causally associated with myocarditis based on reports among US military personnel, with cases typically occurring 7 to 12 days after vaccination.7
With the implementation of a large-scale, national COVID-19 vaccination program starting in December 2020, the US Centers for Disease Control and Prevention (CDC) and the US Food and Drug Administration began monitoring for a number of adverse events of special interest, including myocarditis and pericarditis, in the Vaccine Adverse Event Reporting System (VAERS), a long-standing national spontaneous reporting (passive surveillance) system.8 As the reports of myocarditis after COVID-19 vaccination were reported to VAERS, the Clinical Immunization Safety Assessment Project,9 a collaboration between the CDC and medical research centers, which includes physicians treating infectious diseases and other specialists (eg, cardiologists), consulted on several of the cases. In addition, reports from several countries raised concerns that mRNA-based COVID-19 vaccines may be associated with acute myocarditis.10,11,12,13,14,15
Given this concern, the aims were to describe reports and confirmed cases of myocarditis initially reported to VAERS after mRNA-based COVID-19 vaccination and to provide estimates of the risk of myocarditis after mRNA-based COVID-19 vaccination based on age, sex, and vaccine type.
Methods
Data Sources
VAERS is a US spontaneous reporting (passive surveillance) system that functions as an early warning system for potential vaccine adverse events.8 Co-administered by the CDC and the US Food and Drug Administration, VAERS accepts reports of all adverse events after vaccination from patients, parents, clinicians, vaccine manufacturers, and others regardless of whether the events could plausibly be associated with receipt of the vaccine. Reports to VAERS include information about the vaccinated person, the vaccine or vaccines administered, and the adverse events experienced by the vaccinated person. The reports to VAERS are then reviewed by third-party professional coders who have been trained in the assignment of Medical Dictionary for Regulatory Activities preferred terms.16 The coders then assign appropriate terms based on the information available in the reports.
This activity was reviewed by the CDC and was conducted to be consistent with applicable federal law and CDC policy. The activities herein were confirmed to be nonresearch under the Common Rule in accordance with institutional procedures and therefore were not subject to institutional review board requirements. Informed consent was not obtained for this secondary use of existing information; see 45 CFR part 46.102(l)(2), 21 CFR part 56, 42 USC §241(d), 5 USC §552a, and 44 USC §3501 et seq.
Exposure
The exposure of concern was vaccination with one of the mRNA-based COVID-19 vaccines: the BNT162b2 vaccine (Pfizer-BioNTech) or the mRNA-1273 vaccine (Moderna). During the analytic period, persons aged 12 years or older were eligible for the BNT162b2 vaccine and persons aged 18 years or older were eligible for the mRNA-1273 vaccine. The number of COVID-19 vaccine doses administered during the analytic period was obtained through the CDC’s COVID-19 Data Tracker.17
Outcomes
The primary outcome was the occurrence of myocarditis and the secondary outcome was pericarditis. Reports to VAERS with these outcomes were initially characterized using the Medical Dictionary for Regulatory Activities preferred terms of myocarditis or pericarditis (specific terms are listed in the eMethods in the Supplement). After initial review of reports of myocarditis to VAERS and review of the patient’s medical records (when available), the reports were further reviewed by CDC physicians and public health professionals to verify that they met the CDC’s case definition for probable or confirmed myocarditis (descriptions previously published and included in the eMethods in the Supplement).18 The CDC’s case definition of probable myocarditis requires the presence of new concerning symptoms, abnormal cardiac test results, and no other identifiable cause of the symptoms and findings. Confirmed cases of myocarditis further require histopathological confirmation of myocarditis or cardiac magnetic resonance imaging (MRI) findings consistent with myocarditis.
Deaths were included only if the individual had met the case definition for confirmed myocarditis and there was no other identifiable cause of death. Individual cases not involving death were included only if the person had met the case definition for probable myocarditis or confirmed myocarditis.
Statistical Analysis
We characterized reports of myocarditis or pericarditis after COVID-19 vaccination that met the CDC’s case definition and were received by VAERS between December 14, 2020 (when COVID-19 vaccines were first publicly available in the US), and August 31, 2021, by age, sex, race, ethnicity, and vaccine type; data were processed by VAERS as of September 30, 2021. Race and ethnicity were optional fixed categories available by self-identification at the time of vaccination or by the individual filing a VAERS report. Race and ethnicity were included to provide the most complete baseline description possible for individual reports; however, further analyses were not stratified by race and ethnicity due to the high percentage of missing data. Reports of pericarditis with evidence of potential myocardial involvement were included in the review of reports of myocarditis. The eFigure in the Supplement outlines the categorization of the reports of myocarditis and pericarditis reviewed.
Further analyses were conducted only for myocarditis because of the preponderance of those reports to VAERS, in Clinical Immunization Safety Assessment Project consultations, and in published articles.10,11,12,19,20,21 Crude reporting rates for myocarditis during a 7-day risk interval were calculated using the number of reports of myocarditis to VAERS per million doses of COVID-19 vaccine administered during the analytic period and stratified by age, sex, vaccination dose (first, second, or unknown), and vaccine type. Expected rates of myocarditis by age and sex were calculated using 2017-2019 data from the IBM MarketScan Commercial Research Database. This database contains individual-level, deidentified, inpatient and outpatient medical and prescription drug claims, and enrollment information submitted to IBM Watson Health by large employers and health plans. The data were accessed using version 4.0 of the IBM MarketScan Treatment Pathways analytic platform. Age- and sex-specific rates were calculated by determining the number of individuals with myocarditis (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] codes B33.20, B33.22, B33.24, I40.0, I40.1, I40.8, I40.9, or I51.4)22 identified during an inpatient encounter in 2017-2019 relative to the number of individuals of similar age and sex who were continually enrolled during the year in which the myocarditis-related hospitalization occurred; individuals with any diagnosis of myocarditis prior to that year were excluded. Given the limitations of the IBM MarketScan Commercial Research Database to capture enrollees aged 65 years or older, an expected rate for myocarditis was not calculated for this population. A 95% CI was calculated using Poisson distribution in SAS version 9.4 (SAS Institute Inc) for each expected rate of myocarditis and for each observed rate in a strata with at least 1 case.
In cases of probable or confirmed myocarditis among those younger than 30 years of age, their clinical course was then summarized to the extent possible based on medical review and clinician interviews. This clinical course included presenting symptoms, diagnostic test results, treatment, and early outcomes (abstraction form appears in the eMethods in the Supplement).23
When applicable, missing data were delineated in the results or the numbers with complete data were listed. No assumptions or imputations were made regarding missing data. Any percentages that were calculated included only those cases of myocarditis with adequate data to calculate the percentages.
Results
Case Characteristics
Between December 14, 2020, and August 31, 2021, 192 405 448 individuals older than 12 years of age received a total of 354 100 845 mRNA-based COVID-19 vaccines. VAERS received 1991 reports of myocarditis (391 of which also included pericarditis) after receipt of at least 1 dose of mRNA-based COVID-19 vaccine (eTable 1 in the Supplement) and 684 reports of pericarditis without the presence of myocarditis (eTable 2 in the Supplement).
Of the 1991 reports of myocarditis, 1626 met the CDC’s case definition for probable or confirmed myocarditis (Table 1). There were 208 reports that did not meet the CDC’s case definition for myocarditis and 157 reports that required more information to perform adjudication (eTable 3 in the Supplement). Of the 1626 reports that met the CDC’s case definition for myocarditis, 1195 (73%) were younger than 30 years of age, 543 (33%) were younger than 18 years of age, and the median age was 21 years (IQR, 16-31 years) (Figure 1). Of the reports of myocarditis with dose information, 82% (1265/1538) occurred after the second vaccination dose. Of those with a reported dose and time to symptom onset, the median time from vaccination to symptom onset was 3 days (IQR, 1-8 days) after the first vaccination dose and 74% (187/254) of myocarditis events occurred within 7 days. After the second vaccination dose, the median time to symptom onset was 2 days (IQR, 1-3 days) and 90% (1081/1199) of myocarditis events occurred within 7 days (Figure 2).
Table 1. Characteristics of Reports to VAERS After mRNA-Based COVID-19 Vaccination That Met the CDC’s Case Definition for Myocarditis Between December 14, 2020, and August 31, 2021.
| Vaccination with BNT162b2 | Vaccination with mRNA-1273 | Overall | |||||
|---|---|---|---|---|---|---|---|
| First dose | Second dose | Dose unknown | First dose | Second dose | Dose unknown | ||
| No. of myocarditis reports to VAERS | 147 | 928 | 61 | 126 | 337 | 27 | 1626 |
| No. of vaccination doses administered | 114 246 837 | 95 532 396 | 78 158 611 | 66 163 001 | 354 100 845 | ||
| Age, median (IQR), y | 19 (16-37) | 18 (16-25) | 22 (16-35) | 31 (23-47) | 26 (21-36) | 29 (22-39) | 21 (16-31) |
| Time to symptom onset, median (IQR), d | 3 (1-8) | 2 (2-3) | 3 (2-4) | 3 (2-9) | 2 (1-3) | 2 (1-5) | 2 (1-3) |
| Reported sex, No. (%) | (n = 147) | (n = 928) | (n = 61) | (n = 125) | (n = 337) | (n = 27) | (n = 1625) |
| Male | 111 (76) | 795 (86) | 53 (87) | 89 (71) | 265 (79) | 21 (78) | 1334 (82) |
| Female | 36 (24) | 133 (14) | 8 (13) | 36 (29) | 72 (21) | 6 (22) | 291 (18) |
| Reported race and ethnicity, No. (%)a | (n = 123) | (n = 772) | (n = 40) | (n = 100) | (n = 277) | (n = 18) | (n = 1330) |
| American Indian or Alaska Native | 1 (1) | 4 (1) | 0 | 1 (1) | 0 | 0 | 6 (<1) |
| Asian | 10 (8) | 58 (8) | 1 (3) | 5 (5) | 10 (4) | 0 | 84 (6) |
| Black | 11 (9) | 31 (4) | 3 (8) | 5 (5) | 14 (5) | 4 (22) | 68 (5) |
| Hispanic | 28 (23) | 127 (16) | 9 (23) | 23 (23) | 36 (13) | 5 (28) | 228 (17) |
| Multiple races | 1 (1) | 10 (1) | 0 | 0 | 5 (2) | 1 (6) | 17 (1) |
| Native Hawaiian or Pacific Islander | 0 | 5 (1) | 1 (3) | 1 (1) | 0 | 0 | 7 (1) |
| White | 72 (59) | 531 (69) | 26 (65) | 65 (65) | 212 (77) | 8 (44) | 914 (69) |
| Otherb | 0 | 6 (1) | 0 | 0 | 0 | 0 | 6 (<1) |
Abbreviations: CDC, US Centers for Disease Control and Prevention; VAERS, Vaccine Adverse Event Reporting System.
Categories without ethnicity were either non-Hispanic or had no ethnicity reported.
Individuals were able to choose this category without further specification.
Figure 1. Cases of Myocarditis After mRNA-Based COVID-19 Vaccination by Age at Onset of Myocarditis.
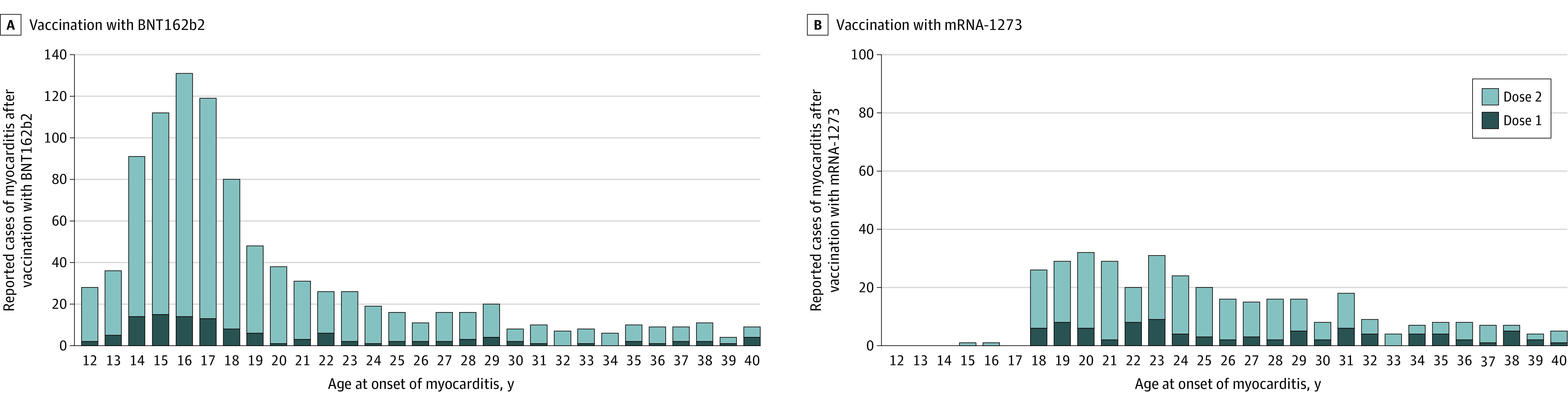
The reports to the Vaccine Adverse Event Reporting System met the case definition of myocarditis (reported cases). Among individuals older than 40 years of age, there were no more than 8 reports of myocarditis for any individual age after receiving either vaccine. For the BNT162b2 vaccine, there were 114 246 837 first vaccination doses and 95 532 396 second vaccination doses; and for the mRNA-1273 vaccine, there were 78 158 611 and 66 163 001, respectively. The y-axis range differs between panels A and B.
Figure 2. Cases of Myocarditis After mRNA-Based COVID-19 Vaccination by Time From Vaccination to Symptom Onset.
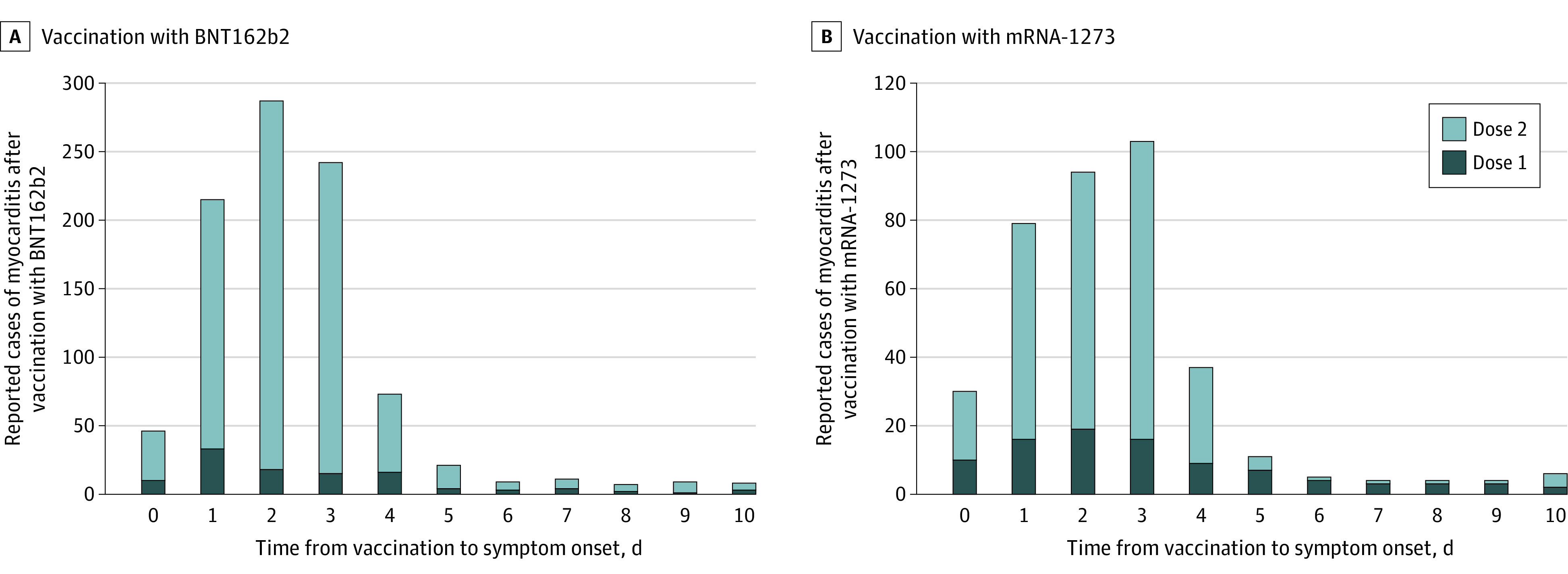
The reports to the Vaccine Adverse Event Reporting System met the case definition of myocarditis (reported cases). Among recipients of either vaccine, there were only 13 reports or less of myocarditis beyond 10 days for any individual time from vaccination to symptom onset. The y-axis range differs between panels A and B.
A, For the BNT162b2 vaccine, there were 138 reported cases of myocarditis with known date for symptom onset and dose after 114 246 837 first vaccination doses and 888 reported cases after 95 532 396 second vaccination doses.
B, For the mRNA-1273 vaccine, there were 116 reported cases of myocarditis with known date for symptom onset and dose after 78 158 611 first vaccination doses and 311 reported cases after 66 163 001 second vaccination doses.
Males comprised 82% (1334/1625) of the cases of myocarditis for whom sex was reported. The largest proportions of cases of myocarditis were among White persons (non-Hispanic or ethnicity not reported; 69% [914/1330]) and Hispanic persons (of all races; 17% [228/1330]). Among persons younger than 30 years of age, there were no confirmed cases of myocarditis in those who died after mRNA-based COVID-19 vaccination without another identifiable cause and there was 1 probable case of myocarditis but there was insufficient information available for a thorough investigation. At the time of data review, there were 2 reports of death in persons younger than 30 years of age with potential myocarditis that remain under investigation and are not included in the case counts.
Reporting Rates of Myocarditis Within 7 Days After COVID-19 Vaccination
Symptom onset of myocarditis was within 7 days after vaccination for 947 reports of individuals who received the BNT162b2 vaccine and for 382 reports of individuals who received the mRNA-1273 vaccine. The rates of myocarditis varied by vaccine type, sex, age, and first or second vaccination dose (Table 2). The reporting rates of myocarditis were highest after the second vaccination dose in adolescent males aged 12 to 15 years (70.73 [95% CI, 61.68-81.11] per million doses of the BNT162b2 vaccine), in adolescent males aged 16 to 17 years (105.86 [95% CI, 91.65-122.27] per million doses of the BNT162b2 vaccine), and in young men aged 18 to 24 years (52.43 [95% CI, 45.56-60.33] per million doses of the BNT162b2 vaccine and 56.31 [95% CI, 47.08-67.34] per million doses of the mRNA-1273 vaccine). The lower estimate of the 95% CI for reporting rates of myocarditis in adolescent males and young men exceeded the upper bound of the expected rates after the first vaccination dose with the BNT162b2 vaccine in those aged 12 to 24 years, after the second vaccination dose with the BNT162b2 vaccine in those aged 12 to 49 years, after the first vaccination dose with the mRNA-1273 vaccine in those aged 18 to 39 years, and after the second vaccination dose with the mRNA-1273 vaccine in those aged 18 to 49 years.
Table 2. Reports to VAERS After mRNA-Based COVID-19 Vaccination That Met the CDC’s Case Definition for Myocarditis Within a 7-Day Risk Interval per Million Doses of Vaccine Administered.
| Reported cases of myocarditis within a 7-d risk interval per million doses of vaccine administered (95% CI)a | Expected cases of myocarditis in a 7-d risk interval per million doses (95% CI)c | ||||
|---|---|---|---|---|---|
| Vaccination with BNT162b2 | Vaccination with mRNA-1273b | ||||
| First dose | Second dose | First dose | Second dose | ||
| Males | |||||
| Age group, y | |||||
| 12-15 | 7.06 (4.88-10.23) | 70.73 (61.68-81.11) | 0.53 (0.40-0.70) | ||
| 16-17 | 7.26 (4.45-11.86) | 105.86 (91.65-122.27) | 1.34 (1.05-1.72) | ||
| 18-24 | 3.82 (2.40-6.06) | 52.43 (45.56-60.33) | 10.73 (7.50-15.34) | 56.31 (47.08-67.34) | 1.76 (1.58,1.98) |
| 25-29 | 1.74 (0.78-3.87) | 17.28 (13.02-22.93) | 4.88 (2.70-8.80) | 24.18 (17.93-32.61) | 1.45 (1.21-1.74) |
| 30-39 | 0.54 (0.20-1.44) | 7.10 (5.26-9.57) | 3.00 (1.81-4.97) | 7.93 (5.61-11.21) | 0.63 (0.54.0.73) |
| 40-49 | 0.55 (0.21-1.48) | 3.50 (2.28-5.36) | 0.59 (0.19-1.82) | 4.27 (2.69-6.78) | 0.78 (0.67-0.90) |
| 50-64 | 0.42 (0.17-1.01) | 0.68 (0.33-1.43) | 0.62 (0.28-1.39) | 0.85 (0.41-1.79) | 0.77 (0.68-0.86) |
| ≥65 | 0.19 (0.05-0.76) | 0.32 (0.10-1.00) | 0.18 (0.05-0.72) | 0.51 (0.21-1.23) | |
| Females | |||||
| Age group, y | |||||
| 12-15 | 0.49 (0.12-1.98) | 6.35 (4.05-9.96) | 0.17 (0.11-0.29) | ||
| 16-17 | 0.84 (0.21-3.37) | 10.98 (7.16-16.84) | 0.42 (0.27-0.66) | ||
| 18-24 | 0.18 (0.03-1.31) | 4.12 (2.60-6.54) | 0.96 (0.31-2.96) | 6.87 (4.27-11.05) | 0.38 (0.30-0.49) |
| 25-29 | 0.26 (0.04-1.84) | 2.23 (1.07-4.69) | 0.41 (0.06-2.94) | 8.22 (5.03-13.41) | 0.48 (0.35-0.65) |
| 30-39 | 0.72 (0.32-1.60) | 1.02 (0.49-2.14) | 0.74 (0.28-1.98) | 0.68 (0.22-2.10) | 0.47 (0.39-0.57) |
| 40-49 | 0.24 (0.06-0.97) | 1.73 (0.98-3.05) | 0.18 (0.02-1.25) | 1.89 (0.98-3.63) | 0.89 (0.77-1.04) |
| 50-64 | 0.37 (0.15-0.88) | 0.51 (0.23-1.14) | 0.65 (0.31-1.36) | 0.43 (0.16-1.15) | 1.00 (0.89-1.13) |
| ≥65 | 0.08 (0.01-0.54) | 0.35 (0.13-0.92) | 0.26 (0.08-0.81) | ||
Abbreviations: CDC, US Centers for Disease Control and Prevention; VAERS, Vaccine Adverse Event Reporting System.
Of 1453 cases of myocarditis with known vaccination dose and time to symptom onset, 1267 had symptom onset within the 7-day risk interval.
The observed estimates were not calculated for the strata with 0 cases of myocarditis. In addition, the observed estimates were not calculated for the strata with cases of myocarditis after administration of mRNA-1273 in those younger than aged 18 years. The mRNA-1273 vaccine had not been authorized for use in the US in this age group.
Estimated using data from the IBM MarketScan Commercial Research Database for 2017-2019. Rates were not calculated for those aged 65 years or older due to the limitations of the database.
The reporting rates of myocarditis in females were lower than those in males across all age strata younger than 50 years of age. The reporting rates of myocarditis were highest after the second vaccination dose in adolescent females aged 12 to 15 years (6.35 [95% CI, 4.05-9.96] per million doses of the BNT162b2 vaccine), in adolescent females aged 16 to 17 years (10.98 [95% CI, 7.16-16.84] per million doses of the BNT162b2 vaccine), in young women aged 18 to 24 years (6.87 [95% CI, 4.27-11.05] per million doses of the mRNA-1273 vaccine), and in women aged 25 to 29 years (8.22 [95% CI, 5.03-13.41] per million doses of the mRNA-1273 vaccine). The lower estimate of the 95% CI for reporting rates of myocarditis in females exceeded the upper bound of the expected rates after the second vaccination dose with the BNT162b2 vaccine in those aged 12 to 29 years and after the second vaccination dose with the mRNA-1273 vaccine in those aged 18 to 29 years.
Clinical Course of Myocarditis After COVID-19 Vaccination in Persons Younger Than 30 Years of Age
Among the 1372 reports of myocarditis in persons younger than 30 years of age, 1305 were able to be adjudicated, with 92% (1195/1305) meeting the CDC’s case definition. Of these, chart abstractions or medical interviews were completed for 69% (826/1195) (Table 3). The symptoms commonly reported in the verified cases of myocarditis in persons younger than 30 years of age included chest pain, pressure, or discomfort (727/817; 89%) and dyspnea or shortness of breath (242/817; 30%). Troponin levels were elevated in 98% (792/809) of the cases of myocarditis. The electrocardiogram result was abnormal in 72% (569/794) of cases of myocarditis. Of the patients who had received a cardiac MRI, 72% (223/312) had abnormal findings consistent with myocarditis. The echocardiogram results were available for 721 cases of myocarditis; of these, 84 (12%) demonstrated a notable decreased left ventricular ejection fraction (<50%). Among the 676 cases for whom treatment data were available, 589 (87%) received nonsteroidal anti-inflammatory drugs. Intravenous immunoglobulin and glucocorticoids were each used in 12% of the cases of myocarditis (78/676 and 81/676, respectively). Intensive therapies such as vasoactive medications (12 cases of myocarditis) and intubation or mechanical ventilation (2 cases) were rare. There were no verified cases of myocarditis requiring a heart transplant, extracorporeal membrane oxygenation, or a ventricular assist device. Of the 96% (784/813) of cases of myocarditis who were hospitalized, 98% (747/762) were discharged from the hospital at time of review. In 87% (577/661) of discharged cases of myocarditis, there was resolution of the presenting symptoms by hospital discharge.
Table 3. Symptoms, Treatment, and Outcomes in 826 Patients Younger Than 30 Years of Age With Myocarditis.
| Cases of myocarditis, No./total (%) |
|
|---|---|
| Presenting symptoms | |
| Chest pain, pressure, or discomfort | 727/817 (89.0) |
| Dyspnea or shortness of breath | 242/817 (29.6) |
| Palpitations | 65/817 (8.0) |
| Abnormal findings | |
| Elevated troponin levela | 792/809 (97.9) |
| Electrocardiogram | 569/794 (71.7) |
| Echocardiogram | 123/721 (17.1) |
| Decreased LVEF (<50%) on echocardiogram | 84/721 (11.7) |
| Cardiac magnetic resonance imagingb | 223/312 (71.5) |
| Hospitalized | 784/813 (96.4) |
| Treatment | |
| Nonsteroidal anti-inflammatory drugs | 589/676 (87.1) |
| Glucocorticoids | 81/676 (12.0) |
| Anticoagulant therapy | 54/676 (8.0) |
| Antiarrhythmic therapy | 18/676 (2.7) |
| Low- or high-flow nasal cannula oxygen support | 12/676 (1.8) |
| Diuretics | 11/676 (1.6) |
| Intensive therapy | |
| Intravenous immunoglobulin | 78/676 (11.5) |
| Vasoactive medications | 12/676 (1.8) |
| Intubation or mechanical ventilation | 2/676 (0.3) |
| Heart transplant | 0 |
| Extracorporeal membrane oxygenation or ventricular assist device | 0 |
| Outcome among those who were hospitalized | |
| Discharged from the hospital | 747/762 (98.0) |
| Still hospitalized at time of review | 15/762 (2.0) |
| Died | 0 |
| Resolution of presenting symptoms by hospital discharge | 577/661 (87.3) |
Abbreviation: LVEF, left ventricular ejection fraction.
Abnormal per the reference range for the hospital or laboratory where the test was performed.
Consistent with myocarditis.
Discussion
In this review of reports to VAERS between December 2020 and August 2021, myocarditis was identified as a rare but serious adverse event that can occur after mRNA-based COVID-19 vaccination, particularly in adolescent males and young men. However, this increased risk must be weighed against the benefits of COVID-19 vaccination.18
Compared with cases of non–vaccine-associated myocarditis, the reports of myocarditis to VAERS after mRNA-based COVID-19 vaccination were similar in demographic characteristics but different in their acute clinical course. First, the greater frequency noted among vaccine recipients aged 12 to 29 years vs those aged 30 years or older was similar to the age distribution seen in typical cases of myocarditis.2,4 This pattern may explain why cases of myocarditis were not discovered until months after initial Emergency Use Authorization of the vaccines in the US (ie, until the vaccines were widely available to younger persons). Second, the sex distribution in cases of myocarditis after COVID-19 vaccination was similar to that seen in typical cases of myocarditis; there is a strong male predominance for both conditions.2,4
However, the onset of myocarditis symptoms after exposure to a potential immunological trigger was shorter for COVID-19 vaccine–associated cases of myocarditis than is typical for myocarditis cases diagnosed after a viral illness.24,25,26 Cases of myocarditis reported after COVID-19 vaccination were typically diagnosed within days of vaccination, whereas cases of typical viral myocarditis can often have indolent courses with symptoms sometimes present for weeks to months after a trigger if the cause is ever identified.1 The major presenting symptoms appeared to resolve faster in cases of myocarditis after COVID-19 vaccination than in typical viral cases of myocarditis. Even though almost all individuals with cases of myocarditis were hospitalized and clinically monitored, they typically experienced symptomatic recovery after receiving only pain management. In contrast, typical viral cases of myocarditis can have a more variable clinical course. For example, up to 6% of typical viral myocarditis cases in adolescents require a heart transplant or result in mortality.27
In the current study, the initial evaluation and treatment of COVID-19 vaccine–associated myocarditis cases was similar to that of typical myocarditis cases.28,29,30,31 Initial evaluation usually included measurement of troponin level, electrocardiography, and echocardiography.1 Cardiac MRI was often used for diagnostic purposes and also for possible prognostic purposes.32,33 Supportive care was a mainstay of treatment, with specific cardiac or intensive care therapies as indicated by the patient’s clinical status.
Long-term outcome data are not yet available for COVID-19 vaccine–associated myocarditis cases. The CDC has started active follow-up surveillance in adolescents and young adults to assess the health and functional status and cardiac outcomes at 3 to 6 months in probable and confirmed cases of myocarditis reported to VAERS after COVID-19 vaccination.34 For patients with myocarditis, the American Heart Association and the American College of Cardiology guidelines advise that patients should be instructed to refrain from competitive sports for 3 to 6 months, and that documentation of a normal electrocardiogram result, ambulatory rhythm monitoring, and an exercise test should be obtained prior to resumption of sports.35 The use of cardiac MRI is unclear, but it may be useful in evaluating the progression or resolution of myocarditis in those with abnormalities on the baseline cardiac MRI.36 Further doses of mRNA-based COVID-19 vaccines should be deferred, but may be considered in select circumstances.37
Limitations
This study has several limitations. First, although clinicians are required to report serious adverse events after COVID-19 vaccination, including all events leading to hospitalization, VAERS is a passive reporting system. As such, the reports of myocarditis to VAERS may be incomplete, and the quality of the information reported is variable. Missing data for sex, vaccination dose number, and race and ethnicity were not uncommon in the reports received; history of prior SARS-CoV-2 infection also was not known. Furthermore, as a passive system, VAERS data are subject to reporting biases in that both underreporting and overreporting are possible.38 Given the high verification rate of reports of myocarditis to VAERS after mRNA-based COVID-19 vaccination, underreporting is more likely. Therefore, the actual rates of myocarditis per million doses of vaccine are likely higher than estimated.
Second, efforts by CDC investigators to obtain medical records or interview physicians were not always successful despite the special allowance for sharing information with the CDC under the Health Insurance Portability and Accountability Act of 1996.39 This challenge limited the ability to perform case adjudication and complete investigations for some reports of myocarditis, although efforts are still ongoing when feasible.
Third, the data from vaccination administration were limited to what is reported to the CDC and thus may be incomplete, particularly with regard to demographics.
Fourth, calculation of expected rates from the IBM MarketScan Commercial Research Database relied on administrative data via the use of ICD-10 codes and there was no opportunity for clinical review. Furthermore, these data had limited information regarding the Medicare population; thus expected rates for those older than 65 years of age were not calculated. However, it is expected that the rates in those older than 65 years of age would not be higher than the rates in those aged 50 to 64 years.4
Conclusions
Based on passive surveillance reporting in the US, the risk of myocarditis after receiving mRNA-based COVID-19 vaccines was increased across multiple age and sex strata and was highest after the second vaccination dose in adolescent males and young men. This risk should be considered in the context of the benefits of COVID-19 vaccination.
eMethods. Medical Dictionary for Regulatory Activities Preferred Terms, Definitions of Myocarditis and Pericarditis, Myocarditis medical review form
eFigure. Flow diagram of cases of myocarditis and pericarditis reported to Vaccine Adverse Event Reporting System (VAERS) after receiving mRNA-based COVID-19 vaccine, United States, December 14, 2020-August 31, 2021.
eTable 1. Characteristics of all myocarditis cases reported to Vaccine Adverse Event Reporting System (VAERS) after mRNA-based COVID-19 vaccination, United States, December 14, 2020–August 31, 2021.
eTable 2. Characteristics of all pericarditis cases reported to Vaccine Adverse Event Reporting System (VAERS) after mRNA-based COVID-19 vaccination, United States, December 14, 2020–August 31, 2021.
eTable 3. Characteristics of myocarditis cases reported to Vaccine Adverse Event Reporting System after mRNA-based COVID-19 vaccination by case definition status.
References
- 1.Cooper LT Jr. Myocarditis. N Engl J Med. 2009;360(15):1526-1538. doi: 10.1056/NEJMra0800028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vasudeva R, Bhatt P, Lilje C, et al. Trends in acute myocarditis–related pediatric hospitalizations in the United States, 2007-2016. Am J Cardiol. 2021;149:95-102. doi: 10.1016/j.amjcard.2021.03.019 [DOI] [PubMed] [Google Scholar]
- 3.Arola A, Pikkarainen E, Sipilä JO, Pykäri J, Rautava P, Kytö V. Occurrence and features of childhood myocarditis: a nationwide study in Finland. J Am Heart Assoc. 2017;6(11):e005306. doi: 10.1161/JAHA.116.005306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kytö V, Sipilä J, Rautava P. The effects of gender and age on occurrence of clinically suspected myocarditis in adulthood. Heart. 2013;99(22):1681-1684. doi: 10.1136/heartjnl-2013-304449 [DOI] [PubMed] [Google Scholar]
- 5.Dasgupta S, Iannucci G, Mao C, Clabby M, Oster ME. Myocarditis in the pediatric population: a review. Congenit Heart Dis. 2019;14(5):868-877. doi: 10.1111/chd.12835 [DOI] [PubMed] [Google Scholar]
- 6.Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis—diagnosis, treatment options, and current controversies. Nat Rev Cardiol. 2015;12(11):670-680. doi: 10.1038/nrcardio.2015.108 [DOI] [PubMed] [Google Scholar]
- 7.Halsell JS, Riddle JR, Atwood JE, et al. ; Department of Defense Smallpox Vaccination Clinical Evaluation Team . Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. JAMA. 2003;289(24):3283-3289. doi: 10.1001/jama.289.24.3283 [DOI] [PubMed] [Google Scholar]
- 8.Gubernot D, Jazwa A, Niu M, et al. US population-based background incidence rates of medical conditions for use in safety assessment of COVID-19 vaccines. Vaccine. 2021;39(28):3666-3677. doi: 10.1016/j.vaccine.2021.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Centers for Disease Control and Prevention . Clinical Immunization Safety Assessment project. Accessed August 24, 2021. https://www.cdc.gov/vaccinesafety/ensuringsafety/monitoring/cisa/index.html
- 10.Marshall M, Ferguson ID, Lewis P, et al. Symptomatic acute myocarditis in 7 adolescents after Pfizer-BioNTech COVID-19 vaccination. Pediatrics. 2021;148(3):e2021052478. doi: 10.1542/peds.2021-052478 [DOI] [PubMed] [Google Scholar]
- 11.Kim HW, Jenista ER, Wendell DC, et al. Patients with acute myocarditis following mRNA COVID-19 vaccination. JAMA Cardiol. 2021;6(10):1196-1201. doi: 10.1001/jamacardio.2021.2828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Montgomery J, Ryan M, Engler R, et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 2021;6(10):1202-1206. doi: 10.1001/jamacardio.2021.2833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A. Myocarditis and pericarditis after vaccination for COVID-19. JAMA. 2021;326(12):1210-1212. doi: 10.1001/jama.2021.13443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mevorach D, Anis E, Cedar N, et al. Myocarditis after BNT162b2 mRNA vaccine against Covid-19 in Israel. N Engl J Med. 2021;385(23):2140-2149. doi: 10.1056/NEJMoa2109730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Witberg G, Barda N, Hoss S, et al. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med. 2021;385(23):2132-2139. doi: 10.1056/NEJMoa2110737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MedDRA . Medical Dictionary for Regulatory Activities. Accessed June 30, 2021. https://www.meddra.org
- 17.US Centers for Disease Control and Prevention . CDC COVID-19 data tracker. Accessed June 30, 2021. https://covid.cdc.gov/covid-data-tracker
- 18.Gargano JW, Wallace M, Hadler SC, et al. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the Advisory Committee on Immunization Practices—United States, June 2021. MMWR Morb Mortal Wkly Rep. 2021;70(27):977-982. doi: 10.15585/mmwr.mm7027e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abu Mouch S, Roguin A, Hellou E, et al. Myocarditis following COVID-19 mRNA vaccination. Vaccine. 2021;39(29):3790-3793. doi: 10.1016/j.vaccine.2021.05.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larson KF, Ammirati E, Adler ED, et al. Myocarditis after BNT162b2 and mRNA-1273 vaccination. Circulation. 2021;144(6):506-508. doi: 10.1161/CIRCULATIONAHA.121.055913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosner CM, Genovese L, Tehrani BN, et al. Myocarditis temporally associated with COVID-19 vaccination. Circulation. 2021;144(6):502-505. doi: 10.1161/CIRCULATIONAHA.121.055891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boehmer TK, Kompaniyets L, Lavery AM, et al. Association between COVID-19 and myocarditis using hospital-based administrative data—United States, March 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(35):1228-1232. doi: 10.15585/mmwr.mm7035e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium . The REDCap Consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahrholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114(15):1581-1590. doi: 10.1161/CIRCULATIONAHA.105.606509 [DOI] [PubMed] [Google Scholar]
- 25.Mason JW, O’Connell JB, Herskowitz A, et al. ; Myocarditis Treatment Trial Investigators . A clinical trial of immunosuppressive therapy for myocarditis. N Engl J Med. 1995;333(5):269-275. doi: 10.1056/NEJM199508033330501 [DOI] [PubMed] [Google Scholar]
- 26.Saji T, Matsuura H, Hasegawa K, et al. Comparison of the clinical presentation, treatment, and outcome of fulminant and acute myocarditis in children. Circ J. 2012;76(5):1222-1228. doi: 10.1253/circj.CJ-11-1032 [DOI] [PubMed] [Google Scholar]
- 27.Ghelani SJ, Spaeder MC, Pastor W, Spurney CF, Klugman D. Demographics, trends, and outcomes in pediatric acute myocarditis in the United States, 2006 to 2011. Circ Cardiovasc Qual Outcomes. 2012;5(5):622-627. doi: 10.1161/CIRCOUTCOMES.112.965749 [DOI] [PubMed] [Google Scholar]
- 28.Caforio ALP, Pankuweit S, Arbustini E, et al. ; European Society of Cardiology Working Group on Myocardial and Pericardial Diseases . Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636-2648. doi: 10.1093/eurheartj/eht210 [DOI] [PubMed] [Google Scholar]
- 29.Yancy CW, Jessup M, Bozkurt B, et al. ; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines . 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-e239. doi: 10.1016/j.jacc.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 30.Law YM, Lal AK, Chen S, et al. ; American Heart Association Pediatric Heart Failure and Transplantation Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young and Stroke Council . Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. 2021;144(6):e123-e135. doi: 10.1161/CIR.0000000000001001 [DOI] [PubMed] [Google Scholar]
- 31.US Centers for Disease Control and Prevention . Clinical considerations: myocarditis and pericarditis after receipt of mRNA COVID-19 vaccines among adolescents and young adults. Accessed August 24, 2021. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html
- 32.Sachdeva S, Song X, Dham N, Heath DM, DeBiasi RL. Analysis of clinical parameters and cardiac magnetic resonance imaging as predictors of outcome in pediatric myocarditis. Am J Cardiol. 2015;115(4):499-504. doi: 10.1016/j.amjcard.2014.11.029 [DOI] [PubMed] [Google Scholar]
- 33.Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72(24):3158-3176. doi: 10.1016/j.jacc.2018.09.072 [DOI] [PubMed] [Google Scholar]
- 34.US Centers for Disease Control and Prevention . Investigating long-term effects of myocarditis. Accessed August 24, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myo-outcomes.html
- 35.Maron BJ, Udelson JE, Bonow RO, et al. ; American Heart Association Electrocardiography and Arrhythmias Committee of Council on Clinical Cardiology, Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and American College of Cardiology . Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: a scientific statement from the American Heart Association and American College of Cardiology. Circulation. 2015;132(22):e273-e280. doi: 10.1161/CIR.0000000000000239 [DOI] [PubMed] [Google Scholar]
- 36.Aquaro GD, Ghebru Habtemicael Y, Camastra G, et al. ; Cardiac Magnetic Resonance Working Group of the Italian Society of Cardiology . Prognostic value of repeating cardiac magnetic resonance in patients with acute myocarditis. J Am Coll Cardiol. 2019;74(20):2439-2448. doi: 10.1016/j.jacc.2019.08.1061 [DOI] [PubMed] [Google Scholar]
- 37.US Centers for Disease Control and Prevention . Interim clinical considerations for use of COVID-19 vaccines currently authorized in the United States. Accessed August 24, 2021. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html
- 38.Shimabukuro TT, Nguyen M, Martin D, DeStefano F. Safety monitoring in the Vaccine Adverse Event Reporting System (VAERS). Vaccine. 2015;33(36):4398-4405. doi: 10.1016/j.vaccine.2015.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.US Centers for Disease Control and Prevention . HIPAA privacy rule and public health: guidance from CDC and the US Department of Health and Human Services. MMWR Suppl. 2003;52:1-17, 19-20. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Medical Dictionary for Regulatory Activities Preferred Terms, Definitions of Myocarditis and Pericarditis, Myocarditis medical review form
eFigure. Flow diagram of cases of myocarditis and pericarditis reported to Vaccine Adverse Event Reporting System (VAERS) after receiving mRNA-based COVID-19 vaccine, United States, December 14, 2020-August 31, 2021.
eTable 1. Characteristics of all myocarditis cases reported to Vaccine Adverse Event Reporting System (VAERS) after mRNA-based COVID-19 vaccination, United States, December 14, 2020–August 31, 2021.
eTable 2. Characteristics of all pericarditis cases reported to Vaccine Adverse Event Reporting System (VAERS) after mRNA-based COVID-19 vaccination, United States, December 14, 2020–August 31, 2021.
eTable 3. Characteristics of myocarditis cases reported to Vaccine Adverse Event Reporting System after mRNA-based COVID-19 vaccination by case definition status.


