Abstract
Background
Lipoprotein(a) (Lp(a)) is a highly proatherogenic lipid fraction that is a clinically significant risk modifier. Patients wanting to learn more about Lp(a) are likely to use online patient educational materials (OPEMs). However, the readability of OPEMs may exceed the health literacy of the public.
Objective
This study aims to assess the readability of OPEMs related to Lp(a). We hypothesized that the readability of these online materials would exceed the sixth grade level recommended by the American Medical Association.
Methods
Using an online search engine, we queried the top 20 search results from 10 commonly used Lp(a)-related search terms to identify a total of 200 websites. We excluded duplicate websites, advertised results, research journal articles, or non–patient-directed materials, such as those intended only for health professionals or researchers. Grade level readability was calculated using 5 standard readability metrics (automated readability index, SMOG index, Coleman-Liau index, Gunning Fog score, Flesch-Kincaid score) to produce robust point (mean) and interval (CI) estimates of readability. Generalized estimating equations were used to model grade level readability by each search term, with the 5 readability scores nested within each OPEM.
Results
A total of 27 unique websites were identified for analysis. The average readability score for the aggregated results was a 12.2 (95% CI 10.9798-13.3978) grade level. OPEMs were grouped into 6 categories by primary source: industry, lay press, research foundation and nonprofit organizations, university or government, clinic, and other. The most readable category was OPEMs published by universities or government agencies (9.0, 95% CI 6.8-11.3). The least readable OPEMs on average were the ones published by the lay press (13.0, 95% CI 11.2-14.8). All categories exceeded the sixth grade reading level recommended by the American Medical Association.
Conclusions
Lack of access to readable OPEMs may disproportionately affect patients with low health literacy. Ensuring that online content is understandable by broad audiences is a necessary component of increasing the impact of novel therapeutics and recommendations regarding Lp(a).
Keywords: lipoprotein(a), readability, online patient education material, health education, health literacy
Introduction
Lipoprotein(a) (Lp(a)) is a highly proatherogenic lipid fraction that is increasingly recognized as a clinically significant risk modifier. The 2018 American College of Cardiology and the American Heart Association guidelines recommend using Lp(a) as a risk-enhancing factor favoring initiation of statin therapy in persons with intermediate atherosclerotic cardiovascular disease (ASCVD) risk [1]. This recommendation is based on data in recent years showing a strong genetic determination of Lp(a) levels; limited modifiability with diet, exercise, and medication; and an increased risk of ASCVD independent of traditional risk factors [2]. National cohort studies using Mendelian randomization estimate that reducing Lp(a) by 50 mg/dl and 99 mg/dl could reduce major adverse cardiac events by 20% and 40%, respectively [3]. Statins do not lower Lp(a), and there are currently no Food and Drug Administration–approved therapies to lower Lp(a) specifically. PCSK-9 inhibitors result in a modest reduction in Lp(a) and may be associated with a reduction in major adverse cardiovascular events for patients with elevated baseline Lp(a) who have experienced acute coronary syndrome [4,5]. Antisense oligonucleotides targeting expression of Lp(a) are in phase III clinical trials [6,7]. The National Lipid Association published guidance in 2019 for clinicians using Lp(a) in clinical practice, and as novel therapeutics are approved, interest in this biomarker is expected to increase in the coming years [8]. Patients may be especially interested in learning their Lp(a) levels after encountering stories of public figures experiencing early ASCVD in the setting of an elevated Lp(a) [9].
Patients wanting to learn more about Lp(a) are likely to use online patient educational materials (OPEMs) [10]. However, patient health literacy may influence utilization of evidence-based OPEMs [11,12]. The American Medical Association (AMA) recommends writing health information for patients at the sixth grade level or below to ensure broad comprehension [13]. Although OPEMs influence patient decision-making, the readability of OPEMs generally exceeds the health literacy of the public [14-16]. Patients with lower health literacy have been noted to have poorer overall health and higher mortality, and this is notably true as well among patients from racial and ethnic minority backgrounds, partially explaining the racial disparities in some outcomes [17]. The disparate impact of elevated Lp(a) in racial/ethnic groups and the lack of standardization of the use of this biomarker in clinical practice make it even more pressing to ensure that evidence-based materials are appropriately written for the public. Thus, we sought to quantify the readability of frequently accessed OPEMs about Lp(a).
Methods
Data Acquisition and Refinement
We used Google, the largest online search engine, to query the first 20 results for each of the following 10 search terms: “lipoprotein(a),” “lipoprotein(a) cardiovascular risk,” “lipoprotein(a) elevated,” “lipoprotein(a) high,” “lipoprotein(a) levels,” “lipoprotein(a) screening,” “lipoprotein(a) test,” “Lp little a,” “Lp(a),” and “Lp(a) screening” [18]. Location, cookies, and user account information were disabled beforehand to avoid search bias. All 200 websites were accessed and downloaded as PDFs on November 5 to 6, 2020. OPEMs were defined as materials intended for patients and the public. Two independent reviewers reviewed each source’s mission statement or informational page to determine whether it was patient-facing. Research journal articles, advertised results, results failing to contain material on Lp(a), and non–patient-directed sources such as those intended only for health professionals or researchers were excluded.
This research is exempt from human participant institutional review board approval as no human participant data were used, and only publicly available OPEMs were included in the analysis.
OPEMs were grouped into 6 categories by primary source. Industry OPEMs were published by for-profit companies or offered a proprietary test or service related to Lp(a). Lay press OPEMs were published by news organizations and health care reporters that do not have a specific research or scientific focus. Research foundations and nonprofit OPEMs were published by health-related organizations that have a specific research or scientific focus. University or government OPEMs were published by academic institutions or national, state, or local government agencies. Clinic OPEMs were published by Williams Integracare clinic, an independently owned family medicine, chiropractic, and physical therapy clinic in St. Cloud, MN. Other includes Wikipedia.org, a crowdsourced online free encyclopedia, which published an article on Lp(a).
Readability Assessment
Websites meeting the criteria for OPEMs were converted into plain text in separate Word (Microsoft Corporation) documents and prepared in accordance with recommendations from the Centers for Medicare and Medicaid Services prior to scoring readability [19]. Using methods consistent with prior readability assessment studies we removed advertisements, videos, images, figures, captions, hyperlinks, disclaimers, copyright notices, acknowledgments, and citations. Periods were used to denote the end of all sentences; all other punctuation were removed. Symbols and numerals were spelled out to avoid artificial increases in reading level. Readability was assessed with Readable.com, as done in prior literature [16].
Statistical Methods
Similar to prior readability studies, grade-level readability was calculated using 5 standard readability metrics (automated readability index, SMOG index, Coleman-Liau index, Gunning Fog score, Flesch-Kincaid score) to produce robust point (mean) and interval (CI) estimates of readability. Averaging across multiple readability metrics has been demonstrated to yield more reliable results than relying on a single readability metric [20]. This was done to minimize bias because no single readability metric has been established as a “gold standard”; each readability metric is calculated differently and varies in limitations [21]. Generalized estimating equations were used to model grade-level readability by each search term, with the 5 readability scores nested within each OPEM [16]. Readability analyses were conducted with SAS Software 9.4 (SAS Institute), with sandwich estimation and the GLIMMIX procedure. All interval estimates were calculated for 95% confidence. The interval estimates reflect the variability of readability for the 5 readability metrics for each OPEM.
Results
Figure 1 summarizes the selection Lp(a) OPEMs for analysis. From an initial sample of 200 total search results across all 10 search terms, 102 results met inclusion criteria. A total of 75 duplicate results were then removed. There were 27 unique OPEMs included in the readability analysis.
Figure 1.
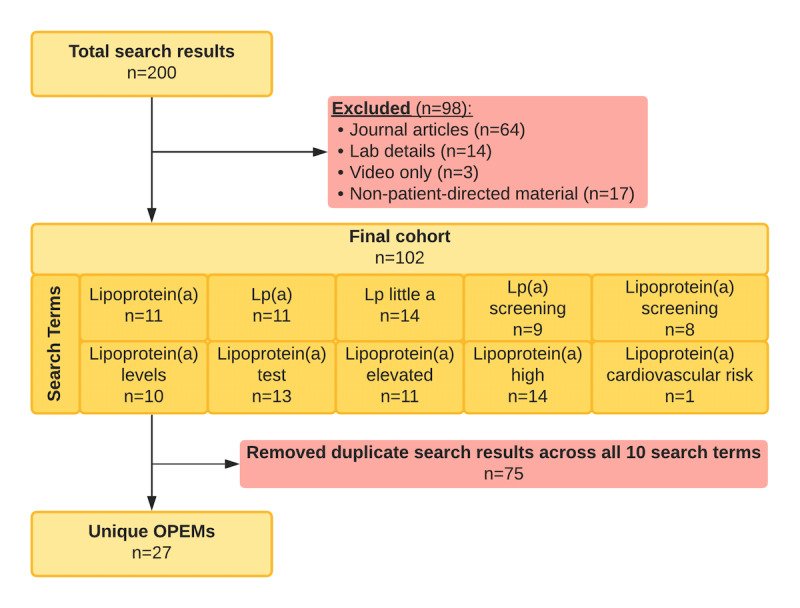
Material selection and exclusion for OPEMs related to lipoprotein(a). OPEM: online patient education material.
Among the 27 OPEMs, the largest category of were university and government sources, which included 30% (n=8) of unique search results. The next largest categories were research and nonprofit foundations and industry publications, which each comprised 22% (n=6) of the results. The third largest category of OPEMs were articles in the lay press, which comprised 19% (n=5/27) of results. The smallest categories were clinic publications and other, both of which had 1 (3%) website (Williams Integracare Clinic and Wikipedia, respectively).
The average readability score across unique websites was at a 12.2 (95% CI 10.9798-13.3978) grade level. The most readable category was OPEMs published by universities or government agencies (9.0, 95% CI 6.8-11.3). The least readable OPEMs on average were the ones published by lay press (13.0, 95% CI 11.2-14.8). Research and nonprofit foundations (12.8, 95% CI 11.0-14.6) and industry (12.1, 95% CI 10.9-13.3) had intermediate readability. Clinic (10.2) and other publications (14) had 1 site per category and therefore are not averaged figures. Figure 2 summarizes the readability scores by category of OPEMs.
Figure 2.
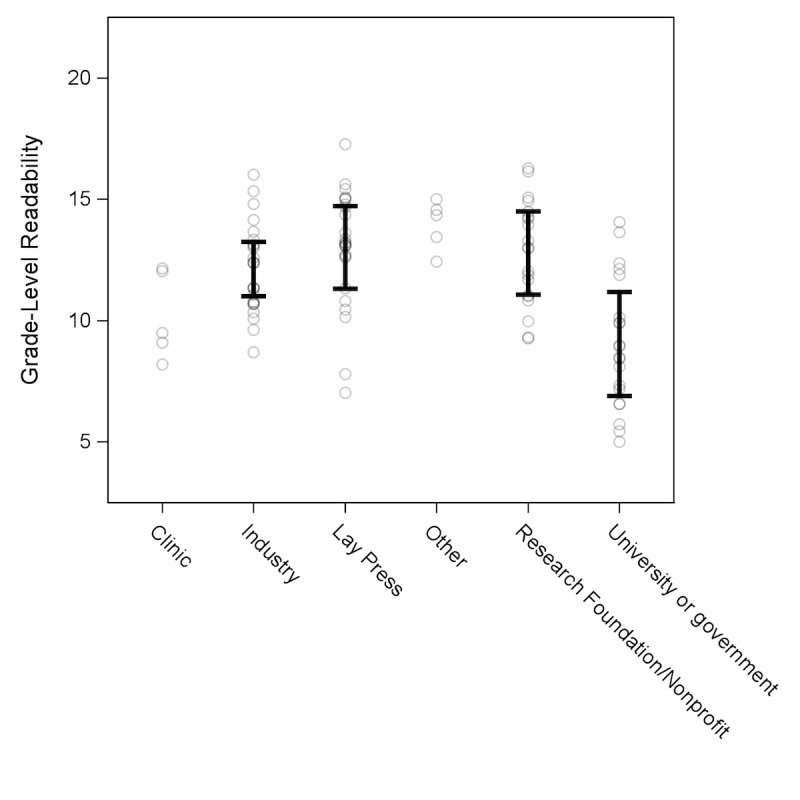
Average grade level readability of online patient education material (OPEM) by category of publication. Each circle represents a readability score for one OPEM, with a total of five readability scores for each unique OPEM. 95% CIs are included for all categories except “Clinic” and “Other,” which only had one unique OPEM each. University and government sources were significantly more readable than research and nonprofit foundation, industry, and lay press sources.
Of the 27 unique search results, only 1 site, the University of Rochester Medical Center (7.0, 95% CI 5.7-8.3), had the sixth grade level recommended by the AMA within its 95% CI. The least readable OPEM was the HEART UK’s Lp(a) general information site (15.7, 95% CI 14.8-16.6). The readability of each unique website is shown in Figure 3.
Figure 3.
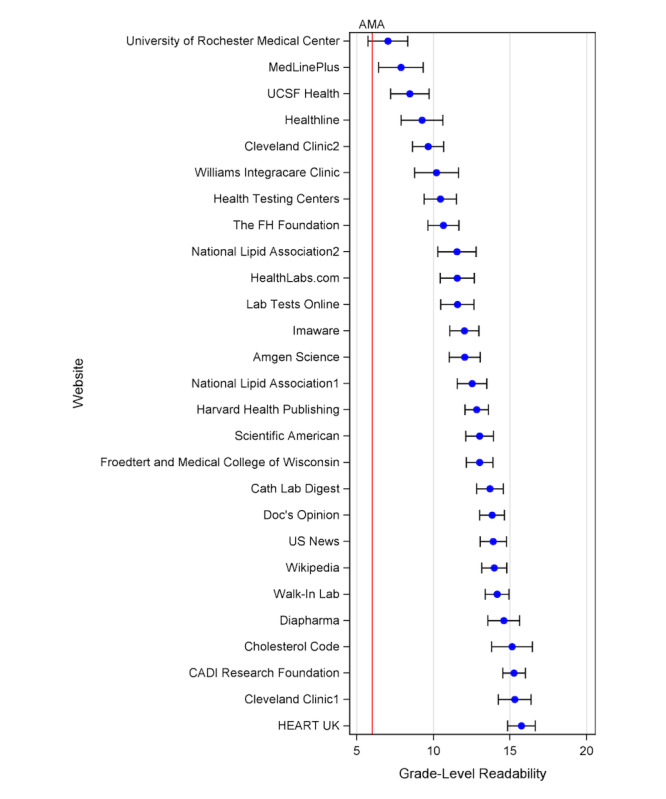
Readability rankings by search result. Each blue dot corresponds to the mean readability based on the average of five standard readability scores (automated readability index, SMOG index, Coleman-Liau index, Gunning fog score, Flesch-Kincaid score) with whiskers representing the range of readability scores. The red vertical line corresponds to the AMA sixth grade level readability target. Cleveland Clinic1: Elevated Lipoprotein(a): Is a Long-Sought Treatment Finally on the Way?; Cleveland Clinic2: Why Would My Doctor Order a Lipoprotein(a) Blood Test?; National Lipid Association1: lipoprotein(a) Screening for Individuals at High ASCVD Risk; National Lipid Association2: Elevated Lipoprotein (a) Patient-Centered Education From the National Lipid Association. AMA: American Medical Association.
Table 1 highlights excerpts from Lp(a) OPEMs across readability levels.
Table 1.
Search concepts and excerpts of readable and nonreadable quotes from OPEM.
| Concept | Excerpt from less readable OPEMa | Excerpt from more readable OPEM |
| Lp(a)b contains both a lipid and a protein carrier | “Lipoprotein(a), or Lp(a), is a distinctive particle with two components: a lipoprotein core that resembles LDL, along with a shell that contains apolipoprotein(a), or apo(a).” [22] | “Lipoproteins are substances made up of protein and fat” [23] |
| Lp(a) is a proatherogenic lipoprotein fraction | “High levels of LP(a) have now been identified as an independent risk factor in cardiovascular disease, with a causal link to atherosclerosis (furring up of arteries), heart attacks, strokes, aortic valve disease and heart failure.” [24] | “High levels of Lp(a) can create plaque in your blood vessels.” [25] |
| High-risk populations should be screened for Lp(a) | “Measurement of lipoprotein(a) is now recommended in several patient subgroups… patients with premature atherosclerosis; patients with a strong family history of premature coronary heart disease (CHD); patients with elevated LDL-C and greater than or equal to two risk factors; patients who have had coronary angioplasty in whom lipoprotein(a) excess may increase the risk of restenosis; patients who have undergone coronary bypass graft surgery in whom Lp(a) excess may be associated with graft stenosis.” [26] | “You may need this test if you have: Heart disease, despite normal results on other lipid tests, High cholesterol, despite maintaining a healthy diet A family history of heart disease, especially heart disease that has occurred at an early age and/or sudden deaths from heart disease.” [27] |
| There is no widely implemented standard for measuring Lp(a) | “Although the reference material for the accurate measurement of Lp(a) … has been available for many years, many commercial laboratories have not changed their reagents and testing methods and continue to use old reagents and methods resulting in inaccurate results. Accordingly, results of Lp(a) measurements by different labs are not comparable and some of them are clearly inaccurate.” [28] | “Note: Normal value ranges may vary slightly among different laboratories. Talk to your doctor about the meaning of your specific test results.” [29] |
| There are no drugs demonstrated to improve outcomes in patients with elevated Lp(a) | “Results using statin medications have been mixed in most trials … In severe cases, such as familial hypercholesterolemia or treatment- resistant hypercholesterolemia, lipid apheresis may dramatically reduce Lp(a) … Other medications that are in various stages of development include thyromimetics, cholesterol-ester-transfer protein (CETP inhibitors), anti-sense oligonucleopeptides, and proprotein convertase subtilisin/kexin type 9 (PCSK-9) inhibitors.” [30] | “Medications/treatments in current use that lower Lp(a) also lower cholesterol. There are apheresis and niacin. These both have substantial side effects. PCSK9 inhibitors lower Lp(a) while lowering LDL cholesterol. Statins have no effect on Lp(a).” [31] |
aOPEM: online patient educational material.
bLp(a): lipoprotein(a).
A list of the OPEM sources used for this study can be found in Multimedia Appendix 1.
Discussion
Principal Results
We found that the average reading grade level of OPEMs pertaining to Lp(a) generally exceeded AMA readability recommendations that OPEMs be written at or below a sixth grade reading level to be accessible to the public. Average grade-level readability of OPEMs on Lp(a) was a 12.2 (95% CI 10.9798-13.3978) grade level, exceeding the average reading level of US adults (eighth grade) [13]. Of 27 unique websites reviewed, only 1 website had a lower bound of reading grade level (5.7) that was below the sixth grade reading level recommendation. Our results suggest that the overwhelming majority of Lp(a) OPEMs are written at a reading level that is too high for the minimally health literate members of the public.
These findings have several important implications for how patients may make decisions about this important, proatherogenic lipid fraction that is receiving increased attention. Patients frequently use the internet to supplement health information from their clinicians [32]. If presented clearly, online health information can be a valuable patient resource. Patients who feel more informed are more comfortable asking their provider questions and report better understanding of their providers’ explanations and greater self-confidence in making health care decisions [33]. A 2018 cross-sectional survey found that patients who searched online for health information to solve their medical problems were also significantly more likely to change their medical decision based on information gathered [34]. It is noteworthy that OPEMs in the academic and government categories were the most readable. Academic and government sites are regarded as reliable sources given that many organizations seek to advance public health and knowledge [35]. Given the major influence of online health information on decision-making, these academic and government websites may also benefit from direct guidance to craft OPEMs with readability targets in view. Despite the importance of these OPEMs in reaching the lay community, research foundations and nonprofit sites demonstrate the largest gaps between patient reading skills and OPEMs reading level on Lp(a).
The less readable OPEMs tend to cover topics in greater depth, including nuances around Lp(a) measurement and standardization, and the role of Lp(a) in thrombogenesis and wound healing. Thus, there appears to be a trade-off between readability and comprehensiveness in OPEMs.
These findings align with results from prior studies across a broad range of health conditions that show OPEMs commonly exceed the recommended readability level. Ayyaswami et al [36] showed that greater than 99% of OPEMs relating to cardiovascular disease were written above the grade level recommended by the AMA [35]. OPEMs are frequently written at a reading level too difficult for the public to comprehend, and low readability levels have been documented across disciplines including common topics related to surgery, oncology, and radiology [37,38].
The percentage of adults with below basic health literacy is considerably higher for populations who identify as Black (24%), Hispanic (41%), American Indian/Alaska Native (25%), and Asian/Pacific Islander (13%) compared to non-Hispanic White (9%) [39]. Similarly, over half of adults older than 65 years were found to have less than a basic health literacy level [39]. These are the very populations known to face a disproportionate burden of cardiovascular risk. Our current risk prediction models such as the Pooled Cohort Equations do not adequately capture the risk to heterogenous racial/ethnic groups [1,40-42]. The importance of reaching these populations is further increased given that Lp(a) is known to circulate at higher levels in patients of African and South Asian descent [43,44].
Many clinical preventive and screening services are underused by historically marginalized racial/ethnic communities and older adults due to inadequate health care access and low health literacy, but we suggest that providing more readable OPEMs may help bridge this gap in care. In the interim, our study findings remind clinicians to consider the readability of OPEMs and patient literacy when recommending Lp(a) evaluation. Shared decision-making requires adequate understanding of the risks and benefits of any diagnostic testing or risk stratification procedure. Actionability of OPEMs on Lp(a) is presently limited by the lack of approved therapies; however, with changes in emerging therapies and practice guidelines, understandability and actionability will be important parameters to assess systematically using the Patient Education Materials Assessment Tool in future studies.
A strength of our study is that we incorporated readability results from five different standard readability metrics, which allows us to have a robust evaluation of readability regardless of the number of websites evaluated. All of the reading grade level estimates supported our hypothesis that Lp(a) OPEMs are written above the recommended sixth grade reading level. We also included a thorough review of possible patient queries by analyzing 200 search results for 10 commonly used search terms. Finally, we included examples of communication of a concept from both more readable and less readable OPEMs. This may serve as a real-world, practical guide for creators of OPEMs seeking to choose words and phrases that will be accessible to a broad audience.
Limitations
Our study should be interpreted in the context of certain limitations. We did not account for other search engines besides Google. This limitation is somewhat mitigated by the fact that 88% of global internet users use Google as their most frequent search engine [18]. As with other OPEM readability studies, the readability metrics used here do not consider the inherent complexity of some medical terms. Polysyllabic words and longer words are automatically rated as more complex and less understandable than short or monosyllabic words, which in medicine does not always hold true.
Conclusions
In conclusion, we found that the grade level readability of OPEMs relating to Lp(a) generally substantially exceeded the sixth grade reading level recommended by the AMA. This gap in readability may disproportionately affect patients with low health literacy. Creators of OPEMs should be mindful of the readability of their content. Ensuring that online content is understandable by broad audiences is a necessary component of increasing the impact of novel therapeutics and recommendations regarding Lp(a).
Acknowledgments
The authors of the study thank the Family Heart Foundation for assistance in reviewing the early drafts of this paper.
Abbreviations
- AMA
American Medical Association
- ASCVD
atherosclerotic cardiovascular disease
- Lp(a)
lipoprotein(a)
- OPEM
online patient educational material
Included online patient educational materials URLs.
Footnotes
Authors' Contributions: KP, SN, FR, and GB designed the study. GB performed all statistical analysis. SN performed all searches and filtered the online patient education materials, as well as conducted the initial readability analysis. KP and AS reviewed the websites for patient-centeredness. KP and SN wrote the manuscript. EE designed all figures and tables. FR, JK, and AS provided editorial review.
Conflicts of Interest: None declared.
References
- 1.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082–e1143. doi: 10.1161/CIR.0000000000000625. https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000000625?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pearson K, Rodriguez F. Lipoprotein(a) and cardiovascular disease prevention across diverse populations. Cardiol Ther. 2020 Dec;9(2):275–292. doi: 10.1007/s40119-020-00177-4. http://europepmc.org/abstract/MED/32451810 .10.1007/s40119-020-00177-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madsen CM, Kamstrup PR, Langsted A, Varbo A, Nordestgaard BG. Lipoprotein(a)-lowering by 50 mg/dL (105 nmol/L) may be needed to reduce cardiovascular disease 20% in secondary prevention: a population-based study. Arterioscler Thromb Vasc Biol. 2020 Jan;40(1):255–266. doi: 10.1161/ATVBAHA.119.312951. https://www.ahajournals.org/doi/abs/10.1161/ATVBAHA.119.312951?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 4.O'Donoghue ML, Fazio S, Giugliano RP, Stroes ESG, Kanevsky E, Gouni-Berthold I, Im K, Lira Pineda A, Wasserman SM, Češka R, Ezhov MV, Jukema JW, Jensen HK, Tokgözoğlu SL, Mach F, Huber K, Sever PS, Keech AC, Pedersen TR, Sabatine MS. Lipoprotein(a), PCSK9 inhibition, and cardiovascular risk. Circulation. 2019 Mar 19;139(12):1483–1492. doi: 10.1161/CIRCULATIONAHA.118.037184. [DOI] [PubMed] [Google Scholar]
- 5.Bittner VA, Szarek M, Aylward PE, Bhatt DL, Diaz R, Edelberg JM, Fras Z, Goodman SG, Halvorsen S, Hanotin C, Harrington RA, Jukema JW, Loizeau V, Moriarty PM, Moryusef A, Pordy R, Roe MT, Sinnaeve P, Tsimikas S, Vogel R, White HD, Zahger D, Zeiher AM, Steg PG, Schwartz GG, ODYSSEY OUTCOMES Committees and Investigators Effect of alirocumab on lipoprotein(a) and cardiovascular risk after acute coronary syndrome. J Am Coll Cardiol. 2020 Jan 21;75(2):133–144. doi: 10.1016/j.jacc.2019.10.057. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(19)38464-5 .S0735-1097(19)38464-5 [DOI] [PubMed] [Google Scholar]
- 6.Santos RD, Raal FJ, Catapano AL, Witztum JL, Steinhagen-Thiessen E, Tsimikas S. Mipomersen, an antisense oligonucleotide to apolipoprotein B-100, reduces lipoprotein(a) in various populations with hypercholesterolemia: results of 4 phase III trials. Arterioscler Thromb Vasc Biol. 2015 Mar;35(3):689–99. doi: 10.1161/ATVBAHA.114.304549. http://europepmc.org/abstract/MED/25614280 .ATVBAHA.114.304549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsimikas S, Viney NJ, Hughes SG, Singleton W, Graham MJ, Baker BF, Burkey JL, Yang Q, Marcovina SM, Geary RS, Crooke RM, Witztum JL. Antisense therapy targeting apolipoprotein(a): a randomised, double-blind, placebo-controlled phase 1 study. Lancet. 2015 Oct 10;386(10002):1472–83. doi: 10.1016/S0140-6736(15)61252-1.S0140-6736(15)61252-1 [DOI] [PubMed] [Google Scholar]
- 8.Wilson DP, Jacobson TA, Jones PH, Koschinsky ML, McNeal CJ, Nordestgaard BG, Orringer CE. Use of Lipoprotein(a) in clinical practice: a biomarker whose time has come. A scientific statement from the National Lipid Association. J Clin Lipidol. 2019;13(3):374–392. doi: 10.1016/j.jacl.2019.04.010.S1933-2874(19)30086-8 [DOI] [PubMed] [Google Scholar]
- 9.O’Connor A. A heart risk factor even doctors know little about. The New York Times. 2018. Jan 9, [2021-03-07]. https://www.nytimes.com/2018/01/09/well/heart-risk-doctors-lipoprotein.html .
- 10.Rice RE. Influences, usage, and outcomes of Internet health information searching: multivariate results from the Pew surveys. Int J Med Inform. 2006 Jan;75(1):8–28. doi: 10.1016/j.ijmedinf.2005.07.032.S1386-5056(05)00146-2 [DOI] [PubMed] [Google Scholar]
- 11.Ilic D. The role of the internet on patient knowledge management, education, and decision-making. Telemed J E Health. 2010;16(6):664–9. doi: 10.1089/tmj.2010.0003. [DOI] [PubMed] [Google Scholar]
- 12.Hersh L, Salzman B, Snyderman D. Health literacy in primary care practice. Am Fam Physician. 2015 Jul 15;92(2):118–24. https://www.aafp.org/link_out?pmid=26176370 .d12016 [PubMed] [Google Scholar]
- 13.Weiss B. Health Literacy and Patient Safety: Help Patients Understand: Manual for Clinicians Internet. Chicago, IL: AMA Foundation; 2007. [Google Scholar]
- 14.Imoisili OE, Levinsohn E, Pan C, Howell BA, Streiter S, Rosenbaum JR. Discrepancy between patient health literacy levels and readability of patient education materials from an electronic health record. Health Lit Res Pract. 2017 Oct;1(4):e203–e207. doi: 10.3928/24748307-20170918-01. http://europepmc.org/abstract/MED/31294265 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kapoor K, George P, Evans MC, Miller WJ, Liu SS. Health literacy: readability of ACC/AHA online patient education material. Cardiology. 2017;138(1):36–40. doi: 10.1159/000475881.000475881 [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez F, Ngo S, Baird G, Balla S, Miles R, Garg M. Readability of online patient educational materials for coronary artery calcium scans and implications for health disparities. J Am Heart Assoc. 2020 Sep 15;9(18):e017372. doi: 10.1161/JAHA.120.017372. https://www.ahajournals.org/doi/10.1161/JAHA.120.017372?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011 Jul 19;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005.155/2/97 [DOI] [PubMed] [Google Scholar]
- 18.Worldwide desktop market share of leading search engines from January 2010 to September 2021. Statista. [2021-11-24]. https://www.statista.com/statistics/216573/worldwide-market-share-of-search-engines/
- 19.Toolkit for making written material clear and effective: section 4: special topics for writing and design: part 7: using readability formulas: a cautionary note. Centers for Medicare and Medicaid Services. 2010. Sep 30, [2021-11-25]. https://www.cms.gov/Outreach-and-Education/Outreach/WrittenMaterialsToolkit/Downloads/ToolkitPart07.pdf .
- 20.Mailloux SL, Johnson ME, Fisher DG, Pettibone TJ. How reliable is computerized assessment of readability? Comput Nurs. 1995;13(5):221–5. [PubMed] [Google Scholar]
- 21.Zhou S, Jeong H, Green PA. How consistent are the best-known readability equations in estimating the readability of design standards? IEEE Trans Professional Commun. 2017 Mar;60(1):97–111. doi: 10.1109/tpc.2016.2635720. [DOI] [Google Scholar]
- 22.Elevated lipoprotein(a): is a long-sought treatment finally on the way? Consult QD. [2021-11-25]. https://consultqd.clevelandclinic.org/elevated-lipoproteina-is-a-long-sought-treatment-finally-on-the-way/
- 23.Lipoprotein-A test. Healthline. [2021-11-25]. https://www.healthline.com/health/lipoprotein-a .
- 24.High lipoprotein (a) HEART UK. [2021-11-25]. https://www.heartuk.org.uk/genetic-conditions/high-lipoproteina .
- 25.Lipoprotein(a) cholesterol. University of Rochester Medical Center. [2021-11-25]. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=lpa_cholesterol#:~:text=Lp(a)%20is%20a%20type,%2Ddensity%20lipoprotein%20(LDL).&text=A%20high%20level%20of%20Lp,risk%20factor%20for%20heart%20disease .
- 26.Lipoprotein (a) blood test. Walk-In Lab. [2021-11-25]. https://www.walkinlab.com/products/view/lipoprotein-a-blood-test .
- 27.Lipoprotein (a) blood test. MedlinePlus. [2021-11-25]. https://medlineplus.gov/lab-tests/lipoprotein-a-blood-test/
- 28.Lp (a) testing and standardization. Cadi. [2021-11-25]. https://cadiresearch.org/topic/lipoproteina/lpa-testing-2 .
- 29.Lipoprotein-a. UCSF Health. [2021-11-25]. https://www.ucsfhealth.org/medical-tests/lipoprotein-a .
- 30.Lipoprotein(a) Wikipedia. [2021-11-25]. https://en.wikipedia.org/wiki/Lipoprotein(a)
- 31.Lp(a) and familial hypercholesterolemia. FH Foundation. [2021-11-25]. https://thefhfoundation.org/lpa-and-familial-hypercholesterolemia#:~:text=What%20is%20Lp(a)%3F,levels%20than%20the%20general%20population .
- 32.Lagan BM, Sinclair M, Kernohan WG. Internet use in pregnancy informs women's decision making: a web-based survey. Birth. 2010 Jun;37(2):106–15. doi: 10.1111/j.1523-536X.2010.00390.x.BIR390 [DOI] [PubMed] [Google Scholar]
- 33.Empowerment and Engagement Among Low-income Californians: Enhancing Patient-Centered Care. San Francisco, CA: Blue Shield of California Foundation; 2021. p. E. [Google Scholar]
- 34.Chen Y, Li C, Liang J, Tsai C. Health information obtained from the internet and changes in medical decision making: questionnaire development and cross-sectional survey. J Med Internet Res. 2018 Feb 12;20(2):e47. doi: 10.2196/jmir.9370. https://www.jmir.org/2018/2/e47/ v20i2e47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bergeron B. Online patient-education options. MedGenMed. 2004 Apr 28;6(2):54. https://www.medscape.com/viewarticle/470749 .470749 [PMC free article] [PubMed] [Google Scholar]
- 36.Ayyaswami V, Padmanabhan D, Patel M, Prabhu AV, Hansberry DR, Agarwal N, Magnani JW. A readability analysis of online cardiovascular disease-related health education materials. Health Lit Res Pract. 2019 Apr;3(2):e74–e80. doi: 10.3928/24748307-20190306-03. https://journals.healio.com/doi/abs/10.3928/24748307-20190306-03?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miles RC, Choi P, Baird GL, Dibble EH, Lamb L, Garg M, Lehman C. Will the effect of new federal breast density legislation be diminished by currently available online patient educational materials? Acad Radiol. 2020 Oct;27(10):1400–1405. doi: 10.1016/j.acra.2019.11.008.S1076-6332(19)30577-X [DOI] [PubMed] [Google Scholar]
- 38.Miles RC, Baird GL, Choi P, Falomo E, Dibble EH, Garg M. Readability of online patient educational materials related to breast lesions requiring surgery. Radiology. 2019 Apr;291(1):112–118. doi: 10.1148/radiol.2019182082. [DOI] [PubMed] [Google Scholar]
- 39.White S, Bennett I, Cordell T, Baxter S. Health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy. PsycEXTRA Dataset. 2006 Sep 06;:A. doi: 10.1037/e530912012-001. [DOI] [Google Scholar]
- 40.Tota-Maharaj R, Blaha MJ, Blankstein R, Silverman MG, Eng J, Shaw LJ, Blumenthal RS, Budoff MJ, Nasir K. Association of coronary artery calcium and coronary heart disease events in young and elderly participants in the multi-ethnic study of atherosclerosis: a secondary analysis of a prospective, population-based cohort. Mayo Clin Proc. 2014 Oct;89(10):1350–9. doi: 10.1016/j.mayocp.2014.05.017. http://europepmc.org/abstract/MED/25236430 .S0025-6196(14)00539-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC, Sorlie P, Stone NJ, Wilson PWF, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen W, Smith SC, Tomaselli GF, American College of Cardiology/American Heart Association Task Force on Practice Guidelines 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Jun 24;129(25 Suppl 2):S49–73. doi: 10.1161/01.cir.0000437741.48606.98. https://www.ahajournals.org/doi/abs/10.1161/01.cir.0000437741.48606.98?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .01.cir.0000437741.48606.98 [DOI] [PubMed] [Google Scholar]
- 42.Rodriguez F, Chung S, Blum MR, Coulet A, Basu S, Palaniappan LP. Atherosclerotic cardiovascular disease risk prediction in disaggregated Asian and Hispanic subgroups using electronic health records. J Am Heart Assoc. 2019 Jul 16;8(14):e011874. doi: 10.1161/JAHA.118.011874. https://www.ahajournals.org/doi/10.1161/JAHA.118.011874?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Enas EA, Varkey B, Dharmarajan TS, Pare G, Bahl VK. Lipoprotein(a): an underrecognized genetic risk factor for malignant coronary artery disease in young Indians. Indian Heart J. 2019;71(3):184–198. doi: 10.1016/j.ihj.2019.04.007. https://linkinghub.elsevier.com/retrieve/pii/S0019-4832(19)30019-7 .S0019-4832(19)30019-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Virani SS, Brautbar A, Davis BC, Nambi V, Hoogeveen RC, Sharrett AR, Coresh J, Mosley TH, Morrisett JD, Catellier DJ, Folsom AR, Boerwinkle E, Ballantyne CM. Associations between lipoprotein(a) levels and cardiovascular outcomes in black and white subjects: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2012 Jan 17;125(2):241–9. doi: 10.1161/CIRCULATIONAHA.111.045120. http://europepmc.org/abstract/MED/22128224 .CIRCULATIONAHA.111.045120 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Included online patient educational materials URLs.


