Abstract
Greater understanding of molecular pathophysiology has led to the recognition that an excessive type 2 inflammatory response is at the basis of the pathophysiology of several inflammatory diseases including atopic dermatitis (AD), asthma, and chronic rhinosinusitis with nasal polyps (CRSwNP). Given the availability of biological agents that can permit management of specific disease endotypes, this reinforces the need for detailed characterization of these diseases through a multidisciplinary approach. Herein, these three conditions are briefly overviewed and practical guidance for a multidisciplinary approach to management is presented. Since type 2 inflammation is suppressed by steroids, drugs such as glucocorticoids have long been the workhorse of medical therapy. However, steroids have well-known local and systemic adverse effects, especially when used at high doses over prolonged periods of time, which is problematic when treating chronic diseases such as AD, asthma, and CRSwNP. Moreover, a substantial proportion of patients remain refractive to therapy. In the attempt to overcome these limitations, greater understanding of the molecular mechanisms of type 2 inflammation have led to the development of targeted biological drugs such as dupilumab, a fully human monoclonal antibody that targets the α chain of the IL-4 receptor. Dupilumab represents a unique therapy for type 2 inflammatory diseases and to date is the only therapy approved for AD, asthma, and CRSwNP. In terms of multidisciplinary management of type 2 inflammatory conditions, the main healthcare professionals involved include a dermatologist, pneumologist or allergologist, and ENT specialist. The model proposed herein takes into account the complex management of patients with type 2 inflammatory conditions and the new biological agents available. A multidisciplinary team can provide a central point for patient management, improve outcomes and specialist referrals, reduce costs, and guarantee that the most appropriate therapeutic decisions are made, as well as aid in management of adverse events. The multidisciplinary model should be structured and dedicated, but at the same time simple and flexible in order to not risk slowing down the patient's care. At present, it is believed that a structured multidisciplinary approach is currently the best means to optimize care of patients with type 2 inflammatory conditions.
Key words: Atopic dermatitis, type 2 comorbidities, asthma, nasal polyps
Introduction
Multidisciplinary approaches are increasingly advocated in many fields of medicine given the mounting complexity of diagnosis and management as well as the multitude of new therapies. In asthma, for example, multidisciplinary care has been shown to reduce hospitalizations and costs in difficult to treat patients who are frequently admitted to hospital [1,2]. A multidisciplinary approach is also considered useful in evaluating triggers and response to treatment, and to address factors such as sleep patterns that can negatively affect the quality of life [3]. Patients with difficult- to-treat asthma often require support from multiple specialist services such as asthma specialists and pulmonary specialists, with possible referrals for psychological support, physiotherapy, and social care [1]. Thus, the care pathway can differ greatly depending on the individual characteristics of the patient, disease, and comorbidities. In addition, to further complicate management, some biological therapies, such as dupilumab, are indicated for more than one condition, and more than one specialist may be needed to evaluate and manage the individual patient.
Greater understanding of molecular pathophysiology has led to the recognition that an excessive type 2 inflammatory response, related to an overactive immune system response, is at the basis of the pathophysiology of several inflammatory diseases including atopic dermatitis (AD), asthma, and chronic rhinosinusitis with nasal polyps (CRSwNP) [4-6]. The availability of biological agents that can permit management of specific disease endotypes, reinforces the need for detailed characterization of these diseases through a multidisciplinary approach [7]. In this regard, GINA now recommends that an integrated approach should be taken towards management of asthma, favoring personalization of therapy [8]. The importance of a multidisciplinary approach has also been highlighted in consensus recommendations from the ARIAITALIA group on nasal polyposis when using biological agents to manage the disease [9]. In AD, a consensus group recently concluded that given the complexity of the disease and its comorbidities, a multidisciplinary approach is potentially useful [10]. For AD, it has been further suggested that multidisciplinary treatment approaches should include medical evaluation and management by an AD specialist, along with education and nursing care, psychological support, and nutritional assessment [11]. In CRSwNP, active collaboration between otolaryngologists and allergists/immunologists has also been recently advocated in order to optimize management [12]. However, despite such recommendations, a multidisciplinary approach is not currently implemented in a large proportion of settings. Thus, there is clear need to identify specific strategies for integrated management not only of adult patients, but also for pediatric patients given the difficulties in transitioning to adult care.
With the overall objective of optimizing therapy for type 2 inflammatory diseases, the present report provides a brief overview of these conditions and gives guidance for multidisciplinary approaches to management using the practical model developed at Verona.
Type 2 inflammatory diseases and management
A type 2 immune response refers to a response that involves both the innate and adaptive arms of the immune system (reviewed in [5]). Type 2 immunity is characterized by activation of T helper 2 (TH2) CD4+ T cells and production of IgE antibodies by B cells. The innate cellular response includes innate lymphoid cells, eosinophils, basophils, and mast cells, as well as interleukin-4 (IL- 4)- and/or IL-13-activated macrophages. A type 2 response has been linked several cytokines such as IL-4, IL-5, IL-9, IL-13, IL- 25, and IL-33. Allergy is a systemic type 2 inflammatory response to an allergen, and is a result of the complex interaction between both genetic and environmental factors, with production of IgE and anomalous immune responses [13]. As mentioned, it is now well documented that type 2 inflammatory responses are at the basis of atopic dermatitis (AD), asthma, and CRSwNP, as well as for eosinophilic esophagitis, some forms of COPD, and other conditions [4-6]. Given this, it is clear that the management of the individual patient requires distinct approaches.
In this regard, since type 2 inflammation is suppressed by steroids, these drugs have long been the workhorse of medical therapy. However, steroids have well-known local and systemic adverse effects, especially when used at high doses over prolonged periods of time, which is problematic when treating chronic diseases such as AD, asthma, and CRSwNP. Moreover, a substantial proportion of patients remain refractive to therapy. In the attempt to overcome these limitations, greater understanding of the molecular mechanisms of type 2 inflammation have led to the development of targeted biological drugs. A leading example is dupilumab, a fully human monoclonal antibody that targets the α chain of the IL-4 receptor [14]. The IL-4Rα subunit is shared by both IL-4 and IL-13, which are key drivers in the TH2 response, and thus the actions of both cytokines are diminished by dupilumab, thereby decreasing TH2-mediated inflammation. Dupilumab represents a unique therapy for type 2 inflammatory diseases and to date is the only therapy approved for AD, asthma, and CRSwNP. Dupilumab is now considered as the one of the most successful therapies that target the IL-4R axis [15]. The availability of dupilumab can provide several benefits in terms of simplifying patient management, but with the need to coordinate care among various specialists. Dupilumab is thus an interesting alternative to more traditional approaches and represents a new way to confer clinical benefits to patients who present with more than one type 2 inflammatory disease.
Multidisciplinary approaches and multidimensional assessment
There are many theoretical benefits of a multidisciplinary approach, which include the reduced need for documents to make referrals, access to services and treatments that would otherwise be inaccessible (e.g., radiological examinations, new biological treatments), optimized flow of patients from primary to secondary to tertiary care, management of adverse events, and obtaining a detailed overview of the management of multiple therapies for more than one pathology. Multidisciplinary care teams ensure patient centrality, improvement of direct and indirect outcomes, cost reduction, and more appropriate therapeutic decisions [16-18]. Patients with CRS also report higher rates of satisfaction with multidisciplinary care compared to standalone clinics [19] with evidence of improved QoL (Quality of Life) and better control of exacerbations in asthma patients [20]. Once a multidisciplinary team is formed, there is a need for coordination of meetings and communication between the various members. This sharing of information and close follow up of the patient by a cross functional team also promotes continuous education and an opportunity for professional development, leading to better quality of patient care.
Considering multidisciplinary management, it should be highlighted that several registries in Italy have helped to shed light on treatments offered and prevalence of comorbidities in patients with type 2 inflammatory diseases. Analysis of data from the AIPO (Associazione Italiana Pneumologi Ospedalieri) registry revealed that out of about 1,300 patients with asthma, roughly 10% have asthma in association with CRSwNP. In contrast, data from the same registry suggest that an association of asthma with AD is rare (and vice versa). It will be interesting, and some efforts are currently being made, to put together data from different national registries [21]. AtopyReg, together with SANI (Severe Asthma Network in Italy), is a project that intends to create a single national register of cases of moderate and severe atopic dermatitis in adults, regardless of the age at which the disease appeared [22]. Another such registry is RINET (Rhinosinusitis Italian Network) [23]. For each patient in these registries, information is being collected on onset of the disease, severity, comorbidities, clinical data, and therapeutic management. All these registries thus highlight the need for evaluation of comorbidities in patients with type 2 inflammatory disease, possibly by multiple specialists.
A model for multidisciplinary management
Notwithstanding the definite clinical need, there is little practical guidance in the literature on how to implement a multidisciplinary approach in daily practice for type 2 inflammatory diseases. A shared diagnostic and therapeutic approach for management of type 2 inflammatory disease should be based on welldefined objectives (Table 1). The expert group further proposed a flow chart for multidisciplinary management based on five steps, as shown in Figure 1. The scheme firstly considers that the healthcare professional leading the team is different: pneumologist or allergologist for asthma, ENT (Ear, Nose and Throat specialist) for CRSwNP, dermatologist for atopic dermatitis, and pediatrician for severe pediatric asthma. In step 1, patients are evaluated for the signs and symptoms of severe type 2 inflammatory comorbidities. For example, patients with asthma are assessed for signs of polyposis and atopic dermatitis. Step 2 consists of multidisciplinary evaluation and staging of any suspected comorbidities, where patients are sent to the most appropriate specialist for further assessment, and the team leader is informed about diagnosis, staging, and recommended therapy. Step 3 has the important multidisciplinary objective of identifying patients with a severe type 2 inflammatory disease who are potential candidates for a biological therapy, wherein all specialists involved can make a shared treatment recommendation. This can help ensure that the most appropriate therapy is being given, and that choice of suitability for a biological therapy is carefully assessed [24]. Step 4 involves periodic follow up assessment and evaluation by all specialists involved in the patient’s care. Lastly, step 5 has the aim of multidisciplinary evaluation to confirm the recommended treatment plan or change it at predefined intervals. The model proposed takes into account the complex management of patients with type 2 inflammatory conditions and the new biological agents available. For this reason, the main healthcare professionals involved in the multidisciplinary team include a dermatologist, pneumologist or allergologist, and ENT specialist. It is thus important to increase collaboration between these specialists in the management of type 2 inflammatory diseases. The model should be structured, but at the same time simple and flexible in order to not risk slowing the patient’s care. Of particular importance are the type of dialogue tools between specialists who should guarantee speed in sharing information and dedicated paths to avoid entering waiting lists for various visits or exams.
Table 1.
Primary objectives of a shared management plan.
| A management plan for severe asthma should ensure |
|---|
| • Accessibility and appropriateness of therapy |
| • Homogeneity of care and quality of assistance |
| • Reduction of clinical and organizational inappropriateness |
| • Consolidate continuity of care |
| • Accountability |
Figure 1.
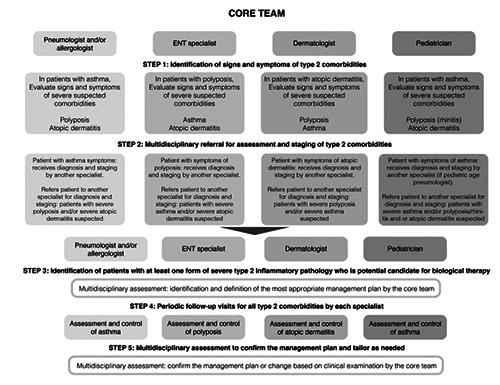
Flow chart for multidisciplinary management: a proposed model.
A multidisciplinary approach for pediatric patients
Well-defined management approaches are especially important for pediatric patients who are making the transition to an adult care setting, and were also included in the proposed scheme (Figure 1). As an example of multidisciplinary collaboration in management of patients with type 2 inflammatory disease, recent efforts in asthma are outlined below. A group called GIPAET (Gruppo Interdisciplinare Asma nell’Età di Transizione) was recently established which was approved by hospital management. The GIPAET will be opening a dedicated “Transitional Outpatient Clinic” to better address the critical issues in management of the most severe pediatric patients with asthma who are transitioning to adult care. A transition approach organizes days dedicated to patients at a “threshold” age for the transition from a pediatric setting to an adult one. This is based on the belief that it is important to support patients during the transitional phase to ensure better control of asthma and allergic diseases. Transitional management includes discussion between specialists from various pediatric/adult clinical areas on clinical cases. While the transition from pediatric to adult management is generally decided on the basis of age, in reality this is not always well defined. Patients in the 15-18-year age group are considered as “borderline” for assuming responsibility for their disease, even if generally after 16 years they transition to adult management, and before 12-14 years all are pediatric patients. An important difference in the management of asthma between childhood/ adolescence and adulthood regards the fact that younger patients often do not take combination therapies, while adults rarely take only a steroid: if the treating physicians are in agreement with the time and modality of the transition between the levels of treatment foreseen by guidelines, the transition from pediatric to adult management is much simpler.
Beyond a multidisciplinary approach
Several additional factors were considered to be useful. These included theoretical-practical multidisciplinary training events on diagnosis and therapy, which will attract considerable interest from otolaryngologists, pulmonologists, allergists, and pediatricians. Such events could be based on previous successful events, i.e., 2- day meetings with lectures on key theoretical aspects and workshops that are focused on clinical, instrumental, cytological diagnosis, etc. It was held that the teaching staff can include reference specialists of the structure in which the course is carried out. Educational events were also considered to be important since the diagnostic-therapeutic approach to type 2 inflammatory diseases is evolving rapidly, and the number of treatment options is expanding. For example, a drug such as dupilumab can significantly change the way these diseases are managed, and multidisciplinary training events are a potent stimulus for the specialists who treat them to improve the care of their patients.
In addition to concerted care, it should also be stressed that educational initiatives for patients can be useful in understanding more about the disease and the importance of adherence to therapy. Patients can also be empowered to take a more active role in the choice of therapy, given the increasing number of treatments for type 2 inflammatory diseases.
Conclusions
Herein, a group of experts had the aim of defining strategies for integrated management of patients with type 2 inflammatory diseases. The multidisciplinary involvement management plan described favors exchange of information and understanding of roles among professionals. A multidisciplinary team can provide a central point for patient management, improve outcomes and specialist referrals, reduce costs, and guarantee that the most appropriate therapeutic decisions are made, as well as aid in management of adverse events. In addition, when a patient has a pathology that is comorbid with asthma, even if mild or moderate in severity, it is important that the dermatologist or ENT specialist consults a pneumologist/ allergologist for the correct evaluation and management of asthma, since the condition could potentially place the patient’s life at risk. At the same time, it is important that the pneumologist/allergologist consults with the ENT specialist and dermatologist in the case of polyposis/atopic dermatitis for correct assessment of all comorbid pathologies. Multidisciplinary management can help to achieve better outcomes in terms of QoL when all aspects of the patient’s condition are considered together. The availability of a therapy that targets type 2 inflammation, which underlies all these pathologies, allows for optimal management and better control of symptoms and QoL outcomes. Last but not least, a multidisciplinary approach is likely to be associated with cost savings, especially in the long-term.
The experts considered that the availability of an integrated and structured outpatient clinic will have clear advantages over traditional approaches, and effective multidisciplinary interaction between specialists can make a difference in the appropriate management of patients and help to obtain the best outcomes. It is clear that the proposed model for multidisciplinary management will continue to evolve based on the availability of new therapeutic agents, increasing experience among centers, better understanding of the optimal care pathways, and changing patterns in waiting lists. However, at present, it is believed that a dedicated and structured, but at the same time easy and flexible, multidisciplinary approach is currently the best means to optimize care of patients with type 2 inflammatory conditions.
Acknowledgements
We thank Patrick Moore, Adriatic Health Communications, for writing and editorial assistance with the manuscript.
Abbreviations
- AD:
atopic dermatitis;
- CRSwNP:
chronic rhinosinusitis with nasal polyps.
Funding Statement
Funding: Sanofi s.r.l. provided unrestricted funding for the editorial support of this article.
References
- 1.Burke H, Davis J, Evans S, Flower L, Tan A, Kurukulaaratchy RJ. A multidisciplinary team case management approach reduces the burden of frequent asthma admissions. ERJ Open Res 2016;2:00039-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patil V, Townshend C, Kurukulaaratchy R, Dyke B, Rahman T, Joshi V. The impact of a specialist multi-disciplinary approach to difficult asthma on healthcare outcomes in a district hospital. Eur Respir J 2013;42:P2023. [Google Scholar]
- 3.Boguniewicz M, Nicol N, Kelsay K, Leung YM. A multidisciplinary approach to evaluation and treatment of atopic dermatitis. Semin Cutan Med Surg 2008;27:115-27. [DOI] [PubMed] [Google Scholar]
- 4.Carr S, Chan ES, Watson W. Eosinophilic esophagitis. Allergy Asthma Clin Immunol 2018;14:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gandhi NA, Bennett BL, Graham NM, Pirozzi G, Stahl N, Yancopoulos GD. Targeting key proximal drivers of type 2 inflammation in disease. Nat Rev Drug Discov 2016;15:35-50. [DOI] [PubMed] [Google Scholar]
- 6.Steinke JW, Wilson JM. Aspirin-exacerbated respiratory disease: pathophysiological insights and clinical advances. J Asthma Allergy 2016;9:37-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vlastos I, Gkouskou K, Doulaptsi M, Karatzanis A, Prokopakis EP. Precision medicine in rhinosinusitis. Curr Allergy Asthma Rep 2019;19:12. [DOI] [PubMed] [Google Scholar]
- 8.Global Initiative for Asthma (GINA). Available from: https://ginasthma.org [Google Scholar]
- 9.Lombardi C, Passalacqua G, Asero R, Bagnasco D, Blasi F, Bonini M, et al. [Consensus Multidisciplinare ARIA-ITALIA: poliposi nasale e farmaci biologici].[Document in Italian]. Available from: http://www.sipirs.it/cms/wp-content/uploads/2020/04/Documento-ARIA-polipsi-final.pdf [Google Scholar]
- 10.Calzavara Pinton P, Cristaudo A, Foti C, Canonica GW, Balato N, Costanzo A, et al. Diagnosis and management of moderate to severe adult atopic dermatitis: a Consensus by the Italian Society of Dermatology and Venereology (SIDeMaST), the Italian Association of Hospital Dermatologists (ADOI), the Italian Society of Allergy, Asthma and Clinical Immunology (SIAAIC), and the Italian Society of Allergological, Environmental and Occupational Dermatology (SIDAPA). G Ital Dermatol Venereol 2018;153:133-45. [DOI] [PubMed] [Google Scholar]
- 11.LeBovidge JS, Elverson W, Timmons KG, Hawryluk EB, Rea C, Lee M, et al. Multidisciplinary interventions in the management of atopic dermatitis. J Allergy Clin Immunol 2016;138:325-34. [DOI] [PubMed] [Google Scholar]
- 12.Lal D, Borish L, Detwiller KY, Gray ST, Joshi S, Kern EC, et al. The rationale for multidisciplinary management of chronic rhinosinusitis with nasal polyposis. J Allergy Clin Immunol Pract 2020;8:1565-6. [DOI] [PubMed] [Google Scholar]
- 13.Pascual M, Davila I, Isidoro-Garcia M, Lorente F. Epigenetic aspects of the allergic diseases. Front Biosci (Schol Ed) 2010;2815-24. [DOI] [PubMed] [Google Scholar]
- 14.Sastre J, Davila I. Dupilumab: A new paradigm for the treatment of allergic diseases. J Investig Allergol Clin Immunol 2018;28:139-50. [DOI] [PubMed] [Google Scholar]
- 15.Licari A, Castagnoli R, Marseglia A, Olivero F, Votto M, Ciprandi G, et al. Dupilumab to treat type 2 inflammatory diseases in children and adolescents. Paediatr Drugs 2020;22:295-310. [DOI] [PubMed] [Google Scholar]
- 16.Nolte E, McKee M. Caring for people with chronic conditions. A health system perspective. Open University Press. Available from: https://www.euro.who.int/__data/assets/pdf_file/0006/96468/E91878.pdf [Google Scholar]
- 17.Gance-Cleveland B, Ozkaynak M. Multidisciplinary teams are essential for developing clinical decision support to improve pediatric health outcomes: An exemplar. J Pediatr Nurs 2021;58104-6. [DOI] [PubMed] [Google Scholar]
- 18.Holmes LJ, Sheehan R, Elsey L, Allen D. The multidisciplinary team severe asthma day case assessment and its impact on patient care. Br J Hosp Med (Lond) 2021;82:1-7. [DOI] [PubMed] [Google Scholar]
- 19.Li KL, Fang CH, Ferastraoaru D, Akbar NA, Jerschow E, Abuzeid WM. Patient satisfaction and efficiency benefits of a novel multidisciplinary rhinology and allergy clinic. Ann Otol Rhinol Laryngol 2020;129:699-706. [DOI] [PubMed] [Google Scholar]
- 20.Clark VL, Gibson PG, Genn G, Hiles SA, Pavord ID, McDonald VM. Multidimensional assessment of severe asthma: A systematic review and meta-analysis. Respirology 2017;22:1262-75. [DOI] [PubMed] [Google Scholar]
- 21.Maio S, Baldacci S, Cecchi L, Viegi G. The severe asthma registries: a way to better know and fight the disease. Eur Ann Allergy Clin Immunol 2021;53:99-102. [DOI] [PubMed] [Google Scholar]
- 22.Canonica GW, Colombo GL, Bruno GM, Di Matteo S, Martinotti C, Blasi F, et al. Shadow cost of oral corticosteroidsrelated adverse events: A pharmacoeconomic evaluation applied to real-life data from the Severe Asthma Network in Italy (SANI) registry. World Allergy Organ J 2019;12:100007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rhinosinusitis Italian Network (RINET). Available from: https://redcap.studi-ricerche.it/surveys/index.php?s=3MAWHNJ7HH [Google Scholar]
- 24.Bush A. Which child with asthma is a candidate for biological therapies? J Clin Med 2020;9:1237. [DOI] [PMC free article] [PubMed] [Google Scholar]


