Visual Abstract
Abstract
Noninfectious lung diseases contribute to nonrelapse mortality. They constitute a spectrum of diseases that can affect the parenchyma, airways, or vascular pulmonary components and specifically exclude cardiac and renal causes. The differential diagnoses of these entities differ as a function of time after hematopoietic cell transplantation. Specific diagnosis, prognosis, and optimal treatment remain challenging, although progress has been made in recent decades.
Learning Objectives
Describe the different pulmonary toxicities that occur after HCT and their timing post HCT as well as risk factors and recommended treatments
Describe the workup of lung toxicity and the current challenges to diagnosis and treatment of noninfectious lung injury after HCT
Introduction
Noninfectious lung complications after hematopoietic cell transplantation (HCT) are uncommon but associated with significant morbidity and mortality.1 Lung compromise may be due to intrapulmonary injury to the parenchyma, airways, or vascular structures and excludes that due to extrapulmonary, renal, or cardiac causes. Identifying the correct diagnosis is critical but can be challenging with available tools, though timing after HCT narrows the differential. This review thus presents the differential diagnoses and key findings as a function of time post transplant.
CLINICAL CASE 1
A 9-month-old, who was transplanted for a nonmalignant condition with a mismatched cord-blood donor after a reduced-intensity busulfan-based preparative regimen and had recently engrafted, developed acute hypoxic respiratory distress 28 days after HCT, in the setting of sinusoidal obstructive syndrome treated with defibrotide. Fresh blood was noted on bronchoalveolar lavage (BAL) that did not clear, as well as a new infiltrate on chest x-ray and rapid progression to respiratory failure. An infectious and cardiac workup was not revealing. Sadly, despite attempting high-frequency oscillatory ventilation, this patient succumbed.
Pulmonary differential of Case 1
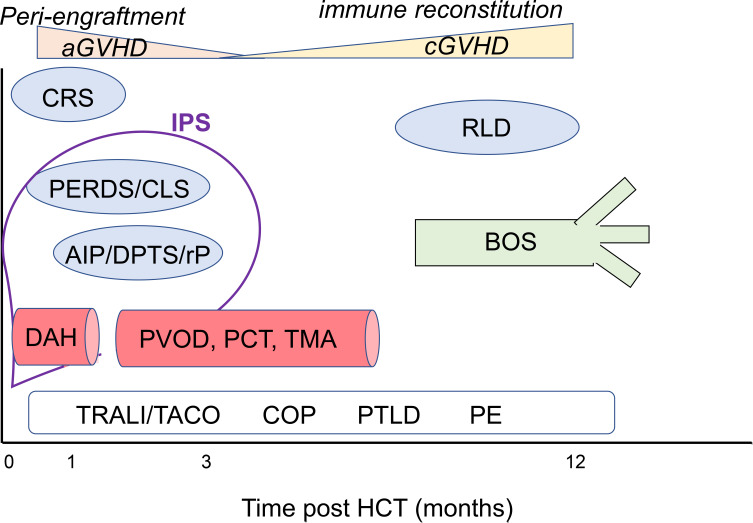
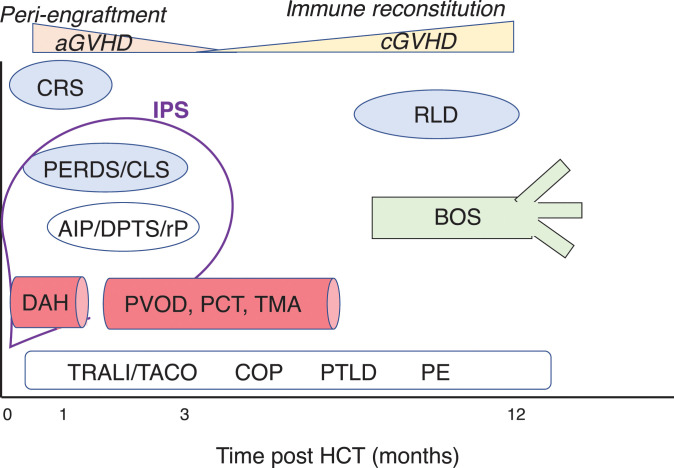
The differential diagnosis of noninfectious lung injury early after HCT largely reflects alveolar injury, many mediated by endothelial dysfunction. These early lung injuries include peri-engraftment respiratory distress syndrome (PERDS), capillary leak syndrome (CLS), diffuse alveolar hemorrhage (DAH), acute interstitial pneumonitis (AIP), or toxic pneumonitis/injuries, collectively termed idiopathic pneumonia syndrome (IPS). Additionally, vascular injury, such as pulmonary veno-occlusive disease (PVOD), can lead to respiratory decline early after HCT (Table 1 and Figure 1). These diagnoses are associated with respiratory distress, include radiographic abnormalities, and although pulmonary function tests (PFTs) are rarely performed, would demonstrate a restrictive defect. The diagnosis of Case 1 is DAH.
Table 1.
Diagnoses, key points, and treatments of noninfectious lung injury after HCT
| Diagnosis | Peak time post HCT/structure | Key findings | Additional diagnosis | Proposed treatments |
|---|---|---|---|---|
| DAH | <day 30 post HCT endothelial | Hypoxia, new infiltrate, bloody BAL | Hemosiderin-laden macrophages | Inhaled transexamic acid, intrapulmonary recombinant factor VIIa |
| PERDS (IPS) | Pre-engraftment Alveolar (from endothelial damage) |
Respiratory distress/hypoxia | Multilobar infiltrates | Steroids/etanercept |
| CLS (IPS) | Engraftment to day
15 Alveolar (from endothelial damage) |
Dyspnea/hypoxia, >3% weight gain | Multilobar infiltrates | Steroids/etanercept |
| AIP and toxin-related lung injuries, DPTC | 50 days post
HCT Alveolar |
Fever, dyspnea, cough | Ground glass on imaging/bilateral
infiltrates, restrictive PFT |
|
| IPS (PERDS, CLS, DAH, AIP, DPTC) | 45 days post
HCT Alveolar |
Hypoxia, pulmonary infiltrates | Steroids/etanercept | |
| CRS | <7 days postcellular
therapy Alveolar |
Respiratory compromise, hypoxia | Infiltrates | Tociluzumab |
| PVOD, PCT, TA-TMA | 15-120 days post
HCT Endothelial |
Hypoxia, dyspnea, vascular occlusion, may
progress to pulmonary hypertension Biopsy diagnosis |
Sildenafil (PVOD, TA-TMA), nitric oxide (TA-TMA) prostacyclins, calcium channel blockers (PVOD) Steroids (PCT)? | |
| RLD after HCT | Day 100-1
year Alveolar |
Decreased FEV1, normal FEV1/VC ratio, fibrosis on CT (upper lobes) | PPFE, NSIP interstitial pneumonia; can include other diagnoses | Etanercept Poor response to steroids |
| BOS | Day 100-1.5
years Airway |
FEV1 < 75%, ≥10% decline, FEV1/VC LL of the 90% CI, absence of infection and either preexisting cGVHD, air trapping by expiratory CT or by PFT, or circumferential fibrosis of bronchioles on biopsy | Newer modalities: PRM and xenon-129 MRI | FAM: inhaled fluticasone, azithromycin,
montelukast +1 mg/kg/d prednisone with rapid taper; ECP, etanercept, GERD tx, nutrition, infection prophylaxis |
| Non-HCT-specific
complications: TRALI/TACO, PE, ARDS, A1AT, cancer/PTLD, pneumothorax |
Alveolar (ARDS,
PTLD)
Airway (A1AT) Endothelial (TRALI/TACO, PE) |
TRALI/TACO: temporal association blood
products, fever, acute dyspnea PE: dyspnea/hypoxia, V/Q+ ARDS: fever, dyspnea, hypoxia, bilateral infiltrates |
A1AT: obstructive disease, emphysema,
bronchiectasis PTLD: nodules/EBV+ |
TRALI/TACO: supportive care PE: anticoagulants ARDS: treat underlying cause (often antimicrobial) and supportive care A1AT: A1AT infusion, inhaled steroids PTLD: rituximab, cellular therapy Pneumothorax: chest tube |
EBV, Epstein-Barr virus; ECP, extracorporeal photopheresis; FAM, inhaled fluticasone, azithromycin, and montelukast + 1 mg/kg/d steroid burst and rapid taper; GERD tx, gastro-esophageal reflux disease treatment; PRM; parametric response mapping; V/Q, ventilation/perfusion scan.
Figure 1.
Illustrated HCT noninfectious lung complications in terms of structure and peak timing after HCT. The time after HCT is shown on the x-axis (in months) with the diseases. Light blue bubbles, parenchymal processes (CRS; PERDS; CLS, capillary leak syndrome from endothelial damage; AIP; rP; DPTS; RLD). Red vessels, the endothelial processes (DAH; PVOD; PCT; TA-TMA). Green airway, airway disease (BOS). IPS, which is most often defined early post HCT, includes these diagnoses (defined by hypoxia, infiltrates, alveolar injury, and excludes later diagnoses that often do not present with these features). White box, pulmonary noninfectious diagnoses not specific to HCT (TRALI; TACO; COP; PE; PTLD), which can occur throughout the HCT trajectory. Above the table are key events occurring during HCT aGVHD and cGVHD.
Diffuse alveolar hemorrhage
Hallmarks of this diagnosis include hypoxia, respiratory distress, and new radiographic infiltrates in the perihilar and lower lobes, with the diagnosis being confirmed by bloody BAL that does not clear, along with hemosiderin-laden macrophages. The incidence is 2% to 5% in allogeneic recipients and 1% in autologous. This patient had risk factors for DAH, including status as a cord-blood recipient, defibrotide treatment, delayed engraftment, though not sirolimus prophylaxis, total body irradiation (TBI), and myeloablation.2,3 Patients often present <30 days after HCT and do poorly, with <25% of adults and <16% of children surviving a year.4,5 While the pathogenesis is incompletely understood, DAH is thought to reflect accumulated damage from conditioning regimens, aberrant immune response, and subsequent damage to the endothelium, resulting in hemorrhage into alveolar spaces. DAH can occur as a result of infections, and thus a full infectious workup is advised (Table 2).6 Treatment historically included steroids, though multiple studies have demonstrated a lack of benefit, and some have shown harm.6-8 Similarly, aminocaproic acid and systemic recombinant factor VIIa have not benefited DAH.8,9 In contrast, small series have supported the use of intrapulmonary administration of recombinant factor VIIa and inhaled transexamic acid. A small case series showed improved survival in patients receiving intrabronchi recombinant factor VIIa compared with historical patients who received steroids,10,11 which is consistent with my experience. For patients too sick to interrupt the ventilatory circuit, inhaled transexamic acid, an antifibrinolytic agent, can be used with conventional ventilation. We have used this in several DAH patients with improvement (without steroids), based on published retrospective data.12 Finally, extracorporeal membrane oxygenation has been rarely employed.13 DAH is consistently diagnosed, while its etiology and optimal treatment are unknown, though local therapies may offer the greatest benefit, and high-dose steroid use has waned.
Table 2.
Workup considerations of noninfectious lung injury after HCT
| Type | Test | Considerations |
|---|---|---|
| Radiographic | CT-inspiratory | Noncontrast sufficient for most; bronchiectasis, enlarged pulmonary vessels may be seen in some diagnoses |
| CT-added expiratory | Valuable to assess air trapping (BOS or RLD) | |
| MRI/MRA | May identify vascular disease | |
| V/Q scan | Evaluate for PE | |
| Chest x-ray | Less valuable if air trapping is present | |
| BAL | PCP (PJP) PCR Explify PCR Respiratory virus PCR Gram stain/culture Fungal stain/culture Cytology (silver stain) Nocardia culture AFB smear/culture CMV PCR HSV PCR Mycoplasma pneumoniae PCR Legionella pneumophilia culture Galactomannan |
PCR tests are increasingly
valuable Explify can detect multiple pathogens by NGS and may detect organisms at low levels not evident in culture, which may be most valuable for pretreated patients or distal lesions Blood return that does not clear is diagnostic for DAH Visual inspection can identify fungal lesions or other indicators Because BAL fluid quantity is per kilogram and return is diminished in severe lung injury, it may be important to prioritize tests in children |
| Blood | Blood culture Karius Blood gas |
Karius uses NGS and can detect lung
organisms with good sensitivity, though data suggest that some
pulmonary infections may be missed (eg, fungal
nodules) Consider methemoglobin if hypoxic and medications at risk |
| Urine | Histoplasmosis antigen | |
| PFTs | FEV1, FEV1/VC ratio, RV and RV/TLC, DLCO, +/−albuterol | Lung clearance index may be
valuable 6 minutes' walk time is a measure of endurance for BOS FEV1 slope of decline can be valuable for prognosis in BOS |
| Lung biopsy | Pathology, stains, and cultures | High morbidity should prompt careful consideration of risk/benefit analysis |
| Echocardiogram/+/−angiography | Pulmonary hypertension | May also identify pericardial effusions |
AFB, acid fast bacillus; CMV, cytomegalovirus; DLCO, diffusion capacity of lung for carbon monoxide; HSV, herpes simplex virus; MRA, magnetic resonance angiography; PJP/PCP, Pneumocystis jirovecii pneumonia (formerly Pneumocystis carinii pneumonia); TLC, total lung capacity.
AIP and toxin-related lung injury
Pneumonitis, an inflammation of the alveoli, can occur early after HCT due to infections, the preparative regimen, or be idiopathic. The presentation is nonspecific, including fever, dyspnea, cough, and ground-glass opacities on imaging. These toxin-induced injuries have had several terms linked to them, including AIP, radiation pneumonitis, carmustine pneumonitis, or delayed pulmonary toxicity syndrome (DPTS from chemotherapy). Overall, the incidence of radiation and chemotherapy pneumonitis has decreased with modifications to chemotherapy regimens and the advent of lung blocking and fractionated TBI.14,15 The recent overall incidence of noninfectious pneumonitis was 5% one year after HCT, with a median onset of 1.6 months in children.5 Risk factors included cancer indication and myeloablative conditioning.5 There was also an association with cord blood transplantation, which may reflect the increased use in TBI in this cohort, though it was not discussed. After myeloablative TBI in adults, the incidence of noninfectious radiation-induced IP is 7.4%, with a median onset of 2.5 months, and less after chemotherapy conditioning.14 The overall survival for adults and children is 50% and 40%, respectively.5,14 Reducing lung exposure during TBI has decreased the rates of radiation-induced IP further.16 Other toxin-mediated early lung complications can include cyclophosphamide-induced, eosinophilic pneumonia linked to fludarabine; IP or DAH with rituximab; DAH after alemtuzumab; or pneumonitis after checkpoint inhibitors.15,17 While steroids are often cited for treatment of these pneumonitis and toxin-induced injuries, data suggest that they have fallen out of favor, given the sparce data for benefit and the relative risks of infection and cancer recurrence. Collectively, these AIP- or toxin-induced lung injuries are uncommon complications of HCT that would benefit from specific diagnostic criteria and investigation into steroid-sparing therapeutic approaches.
PERDS and CLS
PERDS and CLS lead to alveolar damage through endothelial injury, with pulmonary edema as a downstream event. The manifestations include respiratory distress and hypoxemia, the presence of multilobar infiltrates by imaging, and the absence of infections, with PERDS typically occurring within 5 days of engraftment, and some suggesting even a week earlier, and CLS occurring in the first 15 days and accompanied by fluid overload (>3% weight gain). Recent data suggest PERDS occurs in nearly 5% of autologous HCTs and 7% of allogeneic HCTs.18,19 Several elevations in systemic cytokines have been associated with engraftment syndrome, including ST2 protein (an IL-33 receptor), IL-2Rα, tumor necrosis factor 1 between baseline and day 14, and procalcitonin at day 0.19,20 Engraftment syndrome is associated with increased mortality after HCT, though PERDS was not analyzed separately.19 A similar incidence is reported for CLS, which affected approximately 5% of allogeneic HCT patients in a case series, though all but 0.6% of these cases were due to sepsis and associated with mortality.21 A risk factor for CLS may be preexisting vascular dysregulation and cord blood transplant.22 PERDS and noninfectious CLS are rarer causes of lung dysfunction early after HCT, characterized by endothelial dysfunction and cytokine abnormalities, with increased mortality.
IPS—a unifying diagnosis
IPS is an umbrella diagnosis that has historically incorporated several of the above diagnoses. Most definitions have included PERDS, CLS, DAH, AIP, and DPTC in this terminology, with diagnostic criteria of noninfectious, noncardiogenic, nonrenal pulmonary injury after HCT with associated pulmonary infiltrates and hypoxemia due to alveolar injury.23-26 The term is an important unifying diagnosis, permitting key clinical trials of rare diagnoses that collectively comprise early noninfectious lung injury. The incidence of IPS is 3.7% of allogeneic adult HCT patients, with a median onset of 43 days, though later onset is described, and risk factors of myeloablative conditioning, high-dose TBI, lower-respiratory tract viruses pre-HCT, and inborn errors of metabolism as indication for HCT.25,27 In children, the most recent data (2014) showed a rate of 6.7% in allogeneic recipients.28 Approximately 5% of autologous transplant recipients incur IPS.29 Notably, this rate is lower than the rate of the composite diagnoses combined and may reflect the heterogeneity of disorders and patients included under the IPS umbrella. Outcomes remain poor after allogeneic HCT, with <16% to 30% of children and adults surviving a year.25,28,30,31 Many studies have linked elevated BAL levels of tumor necrosis growth factor, ST2, and IL-6 to IPS at diagnosis.26,32-34 Some studies, though not all, have shown a benefit from etanercept with corticosteroids, although less of an impact on long-term survival.26,31,35 The risk of death was higher in patients with prior pulmonary impairment, those who required ventilatory support, or those who had concurrent renal or hepatic injury.25 IPS is a beneficial umbrella diagnosis of early life-threatening noninfectious pulmonary injury after HCT without consensus on its optimal treatment.
Cytokine release syndrome
A new diagnosis has emerged related to the administration of genetically modified T cells (chimeric antigen receptor T-cell therapy; CAR-T). Cytokine release syndrome (CRS) can include respiratory compromise, with infiltrates, hypoxia, and endothelial dysfunction that closely mimics CLS.36-38 A large international study showed that 25% of patients with CAR-T had significant pulmonary compromise.39 Risk factors for CRS include high disease burden, concurrent infections, and lymphodepletion prior to CAR-T.37,38 The role of IL-6 in this process has been established and blockade (via tocilizumab) has mitigated toxicity, sometimes with steroid coadministration.37,38 These data beg the question of whether IL-6 blockade could be valuable in IPS as well, though as yet this treatment remains untested.
PVOD, pulmonary cytolytic thrombi, and transplant- associated thrombotic microangiopathy
PVOD disease, PCT, and transplant-associated thrombotic microangiopathy (TA-TMA) are endothelial lung complications rarely described after HCT that are identified by pathology and usually result in poor outcomes. PVOD is due to intimal fibrosis and venule hypertrophy and obstruction.40 While the pathologic findings are similar to those found in the liver of hepatic VOD (sinusoidal obstructive syndrome; SOS), the literature is lacking regarding co-incidence, and the peak timing differs for these diseases (earlier after HCT for SOS and later for PVOD).41 PVOD is difficult to diagnose, with dyspnea and nonspecific findings on imaging that eventually manifest as right ventricular dysfunction.42 PVOD has been linked to myeloablative HCT and acute graft-versus-host disease (aGVHD) and other airway diseases.40 Treatment with nitrates may be deleterious, while calcium channel blockers, prostacyclins, and sildenafil have suggested possible benefit.42 Defibrotide, an antithrombotic and fibrinolytic agent that stabilizes the endothelium, has yet to be investigated for PVOD after HCT, though the mechanism of action and success in SOS would support its use. Rare reports of pulmonary cytolytic thrombi (PCT) after HCT appeared in the early 2000s, with presentation marked by fever, often in patients with active aGVHD who had nodules on imaging and biopsy showing leukocytes and basophilic occlusions.43 TA-TMA is a syndrome disorder after HCT of endothelial dysfunction most commonly affecting the kidney and is difficult to diagnose without biopsy. It can lead to pulmonary arterial hypertension and hypoxemia, has been demonstrated on biopsy with fibrin occlusion of small pulmonary vessels, and has been treated with sildenafil and nitric oxide.44,45 Given the similarities among these diagnoses, it is unclear if they are separate entities or a spectrum of disease processes. Collectively, these rare endothelial diseases would benefit from further study, refined diagnostic criteria, and systematic evaluation of treatment approaches.
Other pulmonary diagnoses after HCT
HCT recipients are at risk for pulmonary problems that commonly occur in critical illness. These include inflammatory conditions, acute respiratory distress syndrome (ARDS), transfusion-associated acute lung injury (TRALI), transfusion-associated circulatory overload (TACO), and cryptogenic organizing pneumonia (COP; previously termed bronchiolitis obliterans and organizing pneumonia), which is responsive to steroids and restrictive on PFTs and often linked to infections. Other conditions can contribute to pulmonary dysfunction, including alpha-1-antitrypsin deficiency (A1AT), pneumothorax, pulmonary embolism, and, finally, cancer relapse or posttransplant lymphoproliferative disorders (PTLDs).
CLINICAL CASE 2
One year after matched-sibling HCT for relapsed acute leukemia, with busulfan conditioning, complicated by severe aGVHD and cytomegalovirus reactivation before day 100, a 12-year-old girl presented with dyspnea on exertion and ocular chronic GVHD (cGVHD). She underwent lung biopsy, which confirmed bronchiolitis obliterans (forced expiratory volume in 1 second [FEV1]/VC ratio >0.7). Although she had mycobacteria, FEV1 failed to fully recover with protracted antimicrobials consistent with biopsy findings of bronchiolitis obliterans syndrome (BOS), improving from 46% to 59% but then plateauing while still on sirolimus treatment. She was treated in a trial with montelukast with rising FEV1 (to 73%, with FEV1 of 1.56-1.87 L at 2 years). Now, over a decade later, her FEV1 is 2.08 L, 85% predicted, and she remains on montelukast and treatment for mycobacteria (which recurred after 2 antimicrobial cessations).
Pulmonary differential in Case 2
Late-onset noninfectious lung disease affects nearly 20% of 100-day HCT survivors.46 Overall risk factors include chest radiation prior to HCT, lung infection within the first 100 days after HCT, and a reduced mean forced expiratory flow at 25% to 75% (FEF25-75) at 100 days after HCT.46 BOS is the diagnosis of Case 2.
Bronchiolitis obliterans syndrome
BOS is the accepted pulmonary manifestation of cGVHD, diagnosed by an FEV1 < 75% predicted and an irreversible ≥10% decline in <2 years, an FEV1/vital capacity (VC) ratio <0.7 or the lower limit (LL) of the 90% CI of the ratio, an absence of infection, and either preexisting cGVHD, air trapping by expiratory computerized tomography (CT) or by PFT, or circumferential fibrosis of bronchioles on biopsy.47,48 This case highlights several important aspects of the revised definition of BOS, including the ability to diagnose obstructive disease in children for whom the LL of normal is far higher than 0.7. Now this child could be diagnosed without biopsy. As the FEV1/VC ratio declines with age, this is also a key modification for older individuals for whom 0.7 may be a normal value, and a diagnosis of BOS is not warranted. In addition, this case highlights the value of BAL, which could have diagnosed mycobacteria and excluded rare diseases, eg, bronchial obliterans.49 Case 2 has several risk factors linked to BOS, including busulfan conditioning, viral infections early after HCT, and aGVHD, with peripheral blood stem cell donor and ABO incompatibility not present.47,50 A recent study suggests that pre-HCT viruses may confer increased risk as well.27 The current incidence is approximately 3% in pediatric and 3% to 6% in adult HCT.1,51-53 A challenge of this disease has been its insidious nature leading to moderate decline at diagnosis. The frequent use of home devices to detect early declines in lung function and the use of FEF25-75 as an indicator may aid in the earlier identification of BOS.52,54,55 Newer imaging and serum markers show promise for BOS diagnosis, including parametric response mapping (with recent data for machine-learning algorithms), xenon-129 magnetic resonance imaging (MRI), and serum MMP3, though the data are insufficient to replace PFTs.56-59 This may be most critical for children who cannot perform PFTs in the future.60 Therapy for BOS consistently has striven for disease stabilization because the natural history of BOS is steady decline, with severe FEV1 declines associated with highest mortality.61 A prospective, multi-institutional study of inhaled fluticasone, azithromycin, and montelukast with a brief steroid burst (to 1 mg/kg/d prednisone equivalent with rapid tapering off in 1 month) showed stabilization or improvement in 64% of patients with new-onset BOS at 6 months.62 Immunosuppression with calcineurin inhibitor or sirolimus was continued. This approach has been endorsed by the European Society for Blood and Marrow Transplantation as first-line therapy for BOS after HCT.63 One of these agents, azithromycin, came under scrutiny due to increased relapse rates in a randomized trial of azithromycin prior to HCT,64 which were not confirmed in a larger study of azithromycin in established BOS, though a higher rate of secondary neoplasms was observed.65 At this time, the benefits of azithromycin likely outweigh the risks for most BOS patients, though steroids and other risks for secondary neoplasms should also be minimized and personalized risks evaluated. In patients with ongoing pulmonary decline, extracorporeal photopheresis may improve survival, which builds upon prior retrospective data of a response rate of approximately 60%.47,66 Etanercept has shown some success for BOS (32%), while ruxolitinib has not had an impact on BOS progression.67 A challenge to evaluating therapeutic success is the relapsing-remitting nature of BOS, though rapid declines have consistently been associated with poorer outcomes, and the FEV1 slope can thus guide prognosis.68 Lung transplantation remains a final option, and recent data suggest improved survival of 80% at a median of 5 years.69 Overall, the survival of patients with BOS has improved to 40% to 50% at 5 years, which likely reflects the incorporation of newer therapies, a reduction of protracted high-dose steroids, and improvements in supportive care.47 As highlighted by our case, children may experience an unique trajectory of recovery, which I have observed after significant growth and which was recently published in a retrospective cohort.51
Restrictive lung disease
Restrictive lung disease (RLD) after HCT is less well characterized. RLD has a much larger differential to exclude, such as infections, COP, and extrapulmonary constraints, eg, sclerosis or myositis. Intraparenchymal pathology can include elastic fibrosis of the pleura or parenchyma, typically in the upper lobes, termed pleural parenchymal fibroelastosis (PPFE) or nonspecific interstitial pneumonia (NSIP). A study of lung explants suggested that late RLD was due to parenchymal fibrosis with 20% to 30% of small airways obstructed (a much lower proportion than patients with BOS, in which 70% were obstructed).70 These RLD findings can occur with many other HCT-associated lung pathologies, including BOS, PVOD, and lymphocytic bronchiolitis.71 Because chemotherapy can induce PPFE or NSIP, the contribution of cGVHD has been difficult to discern. However, a recent meta-analysis compared the incidence of PPFE in patients with chemotherapy or autologous HCT to those with allogeneic HCT and showed a higher rate in allogeneic HCT (71% vs 25%), suggesting that alloimmunity plays a role in this process.72 A long-term survivor pediatric study showed an association between RLD and GVHD as well as pre-HCT pulmonary dysfunction.73 There are no diagnostic criteria for RLD after HCT, though these findings have been reported: fibrosis on CT (especially the upper lobes) and reduced diffusion capacity and an increased residual volume (RV)/total lung capacity ratio, a 20% decline in FEV1 with a normal FEV1/VC ratio, and reduced VC.74,75 From adult series, the incidence of RLD would seem rarer than BOS, up to 2.6% to 5%.46,74 However, interestingly, pediatric reports of long-term survivors (>6 years) suggest RLD is common, in up to 50% of survivors, highlighting the need for consensus diagnostic criteria.73,76 Little is known to guide treatments of RLD; approximately one-third of patients responded to etanercept, while ruxolitinib did not affect disease.67,77 While newer studies have granted insight into the variable pathology of this disease, the clinical diagnostic criteria and etiology remain ill-defined.
The changing landscape of lung injury after HCT
Infections and lung injury
The definition of noninfectious lung injury is a moving target. Polymerase chain reaction (PCR) studies have improved the detection of viral, bacterial, and fungal pathogens, which has been further enhanced by next-generation sequencing (NGS) with high sensitivity and specificity.78-81 Using such PCR methods from a retrospective cohort, 57% of IPS patients had a detectable pathogen in the BAL.82 By improving infection diagnostics, the role of infections will be better elucidated.
We may need to modify our approach to the consideration of infections with lung injury. Some noninfectious lung injuries are likely late sequelae from an acute infectious process, eg, BOS, linked to viral infections after HCT, and progression has been linked to infections as well.83
Challenges to diagnosis, treatment, and prevention
There are significant diagnostic challenges to noninfectious lung injuries. The diagnostic criteria for BOS and IPS have changed over time, leading to challenges in comparing studies, though both have published consensus criteria.15,23,24,48,84-86 RLD lacks diagnostic criteria altogether. It will be critical to continue to use these standardized diagnostic criteria for these challenging diagnoses and refine with consensus to permit broad application.
Similarly, many of these diagnoses lack specific diagnostic criteria. The endothelial syndromes of PERDS, CLS, and TA-TMA are particularly plagued by this issue, such that a recent review made a “plea” for consensus definitions.86 While there are subtle differences in the findings and risk factors of PERDS/CLS and idiopathic or toxin-related pneumonitis, there is no way to distinguish these diagnoses clinically. It is also unclear whether these lung injuries result from a final common immunologic pathway or result from distinct mechanisms. Addressing this critical question could enhance our ability to identify biomarkers and targeted therapies for these components of IPS as well as the pulmonary vascular diagnoses.
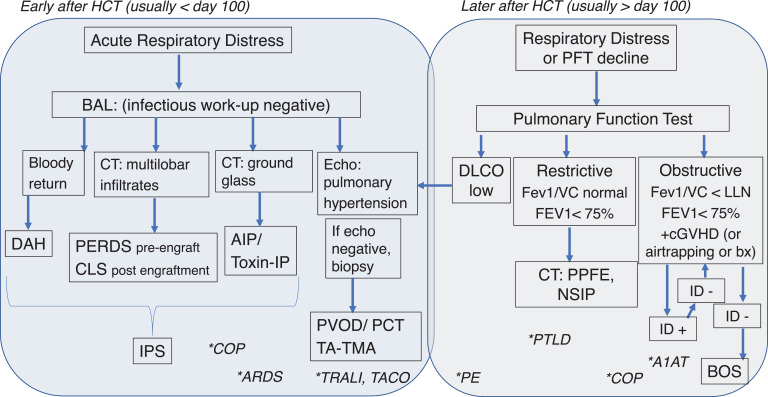
Accurate and noninvasive diagnostic tools that identify lung diagnoses remain an elusive goal. Lung biopsy yields the diagnosis in 50% of patients but is associated with morbidity and mortality.87 BAL yields fewer diagnoses with fewer complications and likely a higher yield with newer modalities (eg, NGS).87 Figure 2 and Table 2 summarize a data-driven workup approach. As is highlighted in Figure 2, many providers attempt a diagnosis through noninvasive means (imaging, BAL, serum testing) and reserve lung biopsy for those patients with nonspecific results from these tests. Notably, these tests typically require over a week to yield results, prompting most practitioners to preemptively treat broadly for infections and for a noninfectious diagnosis of high suspicion. Biopsy is still often required to diagnose vascular complications, though some centers have tried treatments for the pulmonary VOD or TA-TMA without biopsy and used response as a method of diagnosis (often while awaiting results from the BAL tests). Given the high rate of pneumothoraxes in patients with BOS, attempting to make this diagnosis without biopsy is advantageous. Because this remains a clinical challenge, hopefully, imaging or blood biomarkers will be valuable for noninvasive diagnosis in the future.
Figure 2.
Flow diagram for workup and diagnosis of noninfectious lung diseases after HCT. Blue box, diseases commonly diagnosed in the first 100 days after HCT. Gray box, those diseases occurring usually beyond day 100 after HCT. Noninfectious lung injury workup and diagnoses are in boxes. *Additional pulmonary diagnoses are denoted by stars and listed in the column in which these diagnoses would be included in the differential. Notably, other processes can exhibit low DLCO, which is often reduced in RLD, but isolated DLCO reduction should prompt evaluation for vascular diseases of the lung. For the workup of obstructive disease, infection is often diagnosed, which should prompt repeat testing after treatment to ascertain BOS diagnosis (arrows). bx, biopsy; DLCO, diffusion capacity of lung for carbon monoxide; ID, infectious disease workup; PE, pulmonary embolism; toxin-IP, toxin associated interstitial pneumonitis, including that from radiation or chemotherapy.
The prevention of lung injuries after HCT is largely an unattainable end point because of the lack of knowledge of the mechanisms underpinning these diseases. The reduction of lung injury through targeted dosing (of radiation or chemotherapy) has diminished the pneumonitis related to these insults. However, most of the noninfectious lung injuries lack known modifiable inciting factors. Further, the lack of objective specific diagnostic criteria, the rarity of these diseases, and the relative paucity of animal models that mimic the clinical condition have hampered progress in understanding these diseases to develop preventive strategies. Finally, the unintended consequences of diminishing some known risk factors, eg, aGVHD, can lead to increased life-threatening risks, eg, relapse and infections, constraining some efforts due to the need to balance these risks.88,89
Conclusion
Noninfectious lung injury contributes to nonrelapse mortality and morbidity. It usually develops in the first year after HCT and can affect the parenchyma, airways, or vascular structures. Timing, presentation, and imaging can aid in distinguishing the diagnosis, and multiple diagnoses can coexist. However, diagnosis and treatment are areas of critical need. A better understanding of the etiology and immune dysregulation may inform both new diagnostic tools and better treatments to improve outcomes.
Acknowledgments
Drs. Jennifer Holter Chakrabarty, James George, Gregory Yanik, and Guang-Shing Cheng are acknowledged for their expert counsel during this article's preparation.
Conflict-of-interest disclosure
Kirsten M. Williams: no competing financial interests to declare.
Off-label drug use
Kirsten M. Williams: All drugs recommended in this manuscript constitute off-label use with the exception of tociluzumab for CRS. Drugs that are used off label in non-infectious lung treatments include steroids, etanercept, fluticasone, azithromycin, montelukast, inhaled transexamic acid, recombinant factor VII.
References
- 1.Duque-Afonso J, Ihorst G, Waterhouse M, et al.. Impact of lung function on bronchiolitis obliterans syndrome and outcome after allogeneic hematopoietic cell transplantation with reduced-intensity conditioning. Biol Blood Marrow Transplant. 2018;24(11):2277-2284. doi: 10.1016/j.bbmt.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 2.Fan K, McArthur J, Morrison RR, Ghafoor S. Diffuse alveolar hemorrhage after pediatric hematopoietic stem cell transplantation. Front Oncol. 2020;10 (9 September):1757. doi: 10.3389/fonc.2020.01757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keklik F, Alrawi EB, Cao Q, et al.. Diffuse alveolar hemorrhage is most often fatal and is affected by graft source, conditioning regimen toxicity, and engraftment kinetics. Haematologica. 2018;103(12):2109-2115. doi: 10.3324/haematol.2018.189134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Z, Wang C, Peters SG, et al.. Epidemiology, risk factors, and outcomes of diffuse alveolar hemorrhage after hematopoietic stem cell transplantation. Chest. 2021;159(6):2325-2333. doi: 10.13039/100000871. [DOI] [PubMed] [Google Scholar]
- 5.Broglie L, Fretham C, Al-Seraihy A, et al.. Pulmonary complications in pediatric and adolescent patients following allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2019;25(10):2024-2030. doi: 10.1016/j.bbmt.2019.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Majhail NS, Parks K, Defor TE, Weisdorf DJ. Diffuse alveolar hemorrhage and infection-associated alveolar hemorrhage following hematopoietic stem cell transplantation: related and high-risk clinical syndromes. Biol Blood Marrow Transplant. 2006;12(10):1038-1046. doi: 10.1016/j.bbmt.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Haider S, Durairajan N, Soubani AO. Noninfectious pulmonary complications of haematopoietic stem cell transplantation. Eur Respir Rev. 2020; 29(156):190119. doi: 10.1183/16000617.0119-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rathi NK, Tanner AR, Dinh A, et al.. Low-, medium- and high-dose steroids with or without aminocaproic acid in adult hematopoietic SCT patients with diffuse alveolar hemorrhage. Bone Marrow Transplant. 2015; 50(3):420-426. doi: 10.1038/bmt.2014.287. [DOI] [PubMed] [Google Scholar]
- 9.Elinoff JM, Bagci U, Moriyama B, et al.. Recombinant human factor VIIa for alveolar hemorrhage following allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20(7):969-978. doi: 10.1016/j.bbmt.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker MS, Diab KJ, Carlos WG, Mathur P. Intrapulmonary recombinant factor VII as an effective treatment for diffuse alveolar hemorrhage: a case series. J Bronchology Interv Pulmonol. 2016;23(3):255-258. doi: 10.1097/LBR.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 11.Park JA, Kim BJ. Intrapulmonary recombinant factor VIIa for diffuse alveolar hemorrhage in children. Pediatrics. 2015;135(1):e216–e220. doi: 10.1542/peds.2014-1782. [DOI] [PubMed] [Google Scholar]
- 12.O'Neil ER, Schmees LR, Resendiz K, Justino H, Anders MM. Inhaled tranexamic acid as a novel treatment for pulmonary hemorrhage in critically ill pediatric patients: an observational study. Crit Care Explor. 2020;2(1):e0075. doi: 10.1097/CCE.0000000000000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fan K, Hurley C, McNeil MJ, et al.. Case report: management approach and use of extracorporeal membrane oxygenation for diffuse alveolar hemorrhage after pediatric hematopoietic cell transplant. Front Pediatr. 2020;8(13 January):587601. doi: 10.3389/fped.2020.587601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiang Y, Tsai CH, Kuo SH, et al.. Reduced incidence of interstitial pneumonitis after allogeneic hematopoietic stem cell transplantation using a modified technique of total body irradiation. Sci Rep. 2016;6:36730. doi: 10.1038/srep36730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahya VN. Noninfectious acute lung injury syndromes early after hematopoietic stem cell transplantation. Clin Chest Med. 2017;38(4):595-606. doi: 10.1016/j.ccm.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Durie E, Nicholson E, Anthias C, et al.. Determining the incidence of interstitial pneumonitis and chronic kidney disease following full intensity haemopoetic stem cell transplant conditioned using a forward-planned intensity modulated total body irradiation technique. Radiother Oncol. 2021;158(May):97-103. doi: 10.1016/j.radonc.2021.02.020. [DOI] [PubMed] [Google Scholar]
- 17.Vande Vusse LK, Madtes DK. Early onset noninfectious pulmonary syndromes after hematopoietic cell transplantation. Clin Chest Med. 2017;38(2):233-248. doi: 10.1016/j.ccm.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wieruszewski PM, May HP, Peters SG, et al.. Characteristics and outcome of peri-engraftment respiratory distress syndrome following autologous hematopoietic cell transplant. Ann Am Thorac Soc. 2020;18(6):1013-1019. doi: 10.1513/AnnalsATS.202008-1032OC. [DOI] [PubMed] [Google Scholar]
- 19.Chang L, Frame D, Braun T, et al.. Engraftment syndrome after allogeneic hematopoietic cell transplantation predicts poor outcomes. Biol Blood Marrow Transplant. 2014;20(9):1407-1417. doi: 10.1016/j.bbmt.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah NN, Watson TM, Yates B, et al.. Procalcitonin and cytokine profiles in engraftment syndrome in pediatric stem cell transplantation. Pediatr Blood Cancer. 2017;64(3):e26273. doi: 10.1002/pbc.26273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lucchini G, Willasch AM, Daniel J, et al.. Epidemiology, risk factors, and prognosis of capillary leak syndrome in pediatric recipients of stem cell transplants: a retrospective single-center cohort study. Pediatr Transplant. 2016;20(8):1132-1136. doi: 10.1111/petr.12831. [DOI] [PubMed] [Google Scholar]
- 22.Reikvam H, Grønningsæter IS, Ahmed AB, Hatfield K, Bruserud O. Metabolic serum profiles for patients receiving allogeneic stem cell transplantation: the pretransplant profile differs for patients with and without posttransplant capillary leak syndrome. Dis Markers. 2015;2015(October):943430. doi: 10.1155/2015/943430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yanik G, Kitko C. Management of noninfectious lung injury following hematopoietic cell transplantation. Curr Opin Oncol. 2013;25(2):187-194. doi: 10.1097/CCO.0b013e32835dc8a5. [DOI] [PubMed] [Google Scholar]
- 24.Clark JG, Hansen JA, Hertz MI, Parkman R, Jensen L, Peavy HH. NHLBI workshop summary: idiopathic pneumonia syndrome after bone marrow transplantation. Am Rev Respir Dis. 1993;147(suppl 6, pt 1):1601-1606. doi: 10.1164/ajrccm/147.6_Pt_1.1601. [DOI] [PubMed] [Google Scholar]
- 25.Wenger DS, Triplette M, Crothers K, et al.. Incidence, risk factors, and outcomes of idiopathic pneumonia syndrome after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26(2):413-420. doi: 10.1016/j.bbmt.2019.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yanik GA, Ho VT, Levine JE, et al.. The impact of soluble tumor necrosis factor receptor etanercept on the treatment of idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Blood. 2008;112(8):3073-3081. doi: 10.1182/blood-2008-03-143412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Versluys B, Bierings M, Murk JL, et al.. Infection with a respiratory virus before hematopoietic cell transplantation is associated with alloimmune-mediated lung syndromes. J Allergy Clin Immunol. 2018;141(2):697-703.e8703e8. doi: 10.1016/j.jaci.2017.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sano H, Kobayashi R, Iguchi A, et al.. Risk factor analysis of idiopathic pneumonia syndrome after allogeneic hematopoietic SCT in children. Bone Marrow Transplant. 2014;49(1):38-41. doi: 10.1038/bmt.2013.123. [DOI] [PubMed] [Google Scholar]
- 29.Afessa B, Abdulai RM, Kremers WK, Hogan WJ, Litzow MR, Peters SG. Risk factors and outcome of pulmonary complications after autologous hematopoietic stem cell transplant. Chest. 2012;141(2):442-450. doi: 10.1378/chest.10-2889. [DOI] [PubMed] [Google Scholar]
- 30.Thompson J, Yin Z, D'Souza A, et al.. Etanercept and corticosteroid therapy for the treatment of late-onset idiopathic pneumonia syndrome. Biol Blood Marrow Transplant. 2017;23(11):1955-1960. doi: 10.1016/j.bbmt.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 31.Yanik GA, Horowitz MM, Weisdorf DJ, et al.. Randomized, double-blind, placebo-controlled trial of soluble tumor necrosis factor receptor: enbrel (etanercept) for the treatment of idiopathic pneumonia syndrome after allogeneic stem cell transplantation: Blood and Marrow Transplant Clinical Trials Network protocol. Biol Blood Marrow Transplant. 2014;20(6):858–864. doi: 10.1016/j.bbmt.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seo S, Yu J, Jenkins IC, et al.. Diagnostic and prognostic plasma biomarkers for idiopathic pneumonia syndrome after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2018;24(4):678-686. doi: 10.1016/j.bbmt.2017.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhargava M, Viken KJ, Dey S, et al.. Proteome profiling in lung injury after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2016;22(8):1383-1390. doi: 10.1016/j.bbmt.2016.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Varelias A, Gartlan KH, Kreijveld E, et al.. Lung parenchyma-derived IL-6 promotes IL-17A-dependent acute lung injury after allogeneic stem cell transplantation. Blood. 2015;125(15):2435-2444. doi: 10.1182/blood-2014-07-590232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tizon R, Frey N, Heitjan DF, et al.. High-dose corticosteroids with or without etanercept for the treatment of idiopathic pneumonia syndrome after allo-SCT. Bone Marrow Transplant. 2012;47(10):1332-1337. doi: 10.1038/bmt.2011.260. [DOI] [PubMed] [Google Scholar]
- 36.Gavriilaki E, Sakellari I, Gavriilaki M, Anagnostopoulos A. A new era in endothelial injury syndromes: toxicity of CAR-T cells and the role of immunity. Int J Mol Sci. 2020;21(11):3886. doi: 10.3390/ijms21113886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee DW, Santomasso BD, Locke FL, et al.. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transplant. 2019;25(4):625-638. doi: 10.1016/j.bbmt.2018.12.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maus MV, Alexander S, Bishop MR, et al.. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune effector cell-related adverse events. J Immunother Cancer. 2020;8(2):e001511. doi: 10.1136/jitc-2020-001511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Azoulay E, Castro P, Maamar A, et al; Nine-I Investigators. Outcomes in patients treated with chimeric antigen receptor T-cell therapy who were admitted to intensive care (CARTTAS): an international, multicentre, observational cohort study. Lancet Haematol. 2021;8(5):e355–e364. doi: 10.1016/S2352-3026(21)00060-0. [DOI] [PubMed] [Google Scholar]
- 40.Gazourian L, Spring L, Meserve E, et al.. Pulmonary clinicopathological correlation after allogeneic hematopoietic stem cell transplantation: an autopsy series. Biol Blood Marrow Transplant. 2017;23(10):1767-1772. doi: 10.1016/j.bbmt.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mandel J, Mark EJ, Hales CA. Pulmonary veno-occlusive disease. Am J Respir Crit Care Med. 2000;162(5):1964-1973. doi: 10.1164/ajrccm.162.5.9912045. [DOI] [PubMed] [Google Scholar]
- 42.Bunte MC, Patnaik MM, Pritzker MR, Burns LJ. Pulmonary veno-occlusive disease following hematopoietic stem cell transplantation: a rare model of endothelial dysfunction. Bone Marrow Transplant. 2008;41(8):677-686. doi: 10.1038/sj.bmt.1705990. [DOI] [PubMed] [Google Scholar]
- 43.Gulbahce HE, Pambuccian SE, Jessurun J, et al.. Pulmonary nodular lesions in bone marrow transplant recipients: impact of histologic diagnosis on patient management and prognosis. Am J Clin Pathol. 2004;121(2):205–210. doi: 10.1309/4HYN-1DEA-718R-DM6T. [DOI] [PubMed] [Google Scholar]
- 44.Jodele S, Hirsch R, Laskin B, Davies S, Witte D, Chima R. Pulmonary arterial hypertension in pediatric patients with hematopoietic stem cell transplant-associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2013;19(2):202-207. doi: 10.1016/j.bbmt.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 45.Nakamura Y, Mitani N, Ishii A, et al.. Idiopathic pneumonia syndrome with thrombotic microangiopathy-related changes after allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2013;98(4):496-498. doi: 10.1007/s12185-013-1413-x. [DOI] [PubMed] [Google Scholar]
- 46.Bergeron A, Chevret S, Peffault de Latour R, et al.. Noninfectious lung complications after allogeneic haematopoietic stem cell transplantation. Eur Respir J. 2018;51(5). doi: 10.1183/13993003.02617-2017. [DOI] [PubMed] [Google Scholar]
- 47.Williams KM. How I treat bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. Blood. 2017;129(4):448-455. doi: 10.1182/blood-2016-08-693507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams KM, Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation. JAMA. 2009;302(3): 306-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yokoi T, Hirabayashi N, Ito M, et al; Nagoya Bone Marrow Transplant Group. Broncho-bronchiolitis obliterans as a complication of bone marrow transplantation: a clinicopathological study of eight autopsy cases. Virchows Arch. 1997;431(4):275-282. doi: 10.1007/s004280050099. [DOI] [PubMed] [Google Scholar]
- 50.Zhou X, O'Dwyer DN, Xia M, et al.. First-onset herpesviral infection and lung injury in allogeneic hematopoietic cell transplantation. Am J Respir Crit Care Med. 2019;200(1):63-74. doi: 10.1164/rccm.201809-1635OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Walther S, Rettinger E, Maurer HM, et al.. Long-term pulmonary function testing in pediatric bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. Pediatr Pulmonol. 2020;55(7):1725-1735. doi: 10.1002/ppul.24801. [DOI] [PubMed] [Google Scholar]
- 52.Jamani K, He Q, Liu Y, et al.. Early post-transplantation spirometry is associated with the development of bronchiolitis obliterans syndrome after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26(5):943-948. doi: 10.1016/j.bbmt.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yomota M, Yanagawa N, Sakai F, et al.. Association between chronic bacterial airway infection and prognosis of bronchiolitis obliterans syndrome after hematopoietic cell transplantation. Medicine (Baltimore). 2019;98(1):e13951. doi: 10.1097/MD.0000000000013951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Turner J, He Q, Baker K, et al.. Home spirometry telemonitoring for early detection of bronchiolitis obliterans syndrome in patients with chronic graft-versus-host disease. Transplant Cell Ther. 2021;27(7):616.e1-616.e6. doi: 10.1016/j.jtct.2021.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abedin S, Yanik GA, Braun T, et al.. Predictive value of bronchiolitis obliterans syndrome stage 0p in chronic graft-versus-host disease of the lung. Biol Blood Marrow Transplant. 2015;21(6):1127-1131. doi: 10.1016/j.bbmt.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu X, Yue Z, Yu J, et al.. Proteomic characterization reveals that MMP-3 correlates with bronchiolitis obliterans syndrome following allogeneic hematopoietic cell and lung transplantation. Am J Transplant. 2016;16(8):2342-2351. doi: 10.1111/ajt.13750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cheng GS, Selwa KE, Hatt C, et al.. Multicenter evaluation of parametric response mapping as an indicator of bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. Am J Transplant. 2020;20(8):2198-2205. doi: 10.1111/ajt.15814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sharifi H, Lai YK, Guo H, et al.. Machine learning algorithms to differentiate among pulmonary complications after hematopoietic cell transplant. Chest. 2020;158(3):1090-1103. doi: 10.1016/j.chest.2020.02.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walkup LL, Myers K, El-Bietar J, et al.. Xenon-129 MRI detects ventilation deficits in paediatric stem cell transplant patients unable to perform spirometry. Eur Respir J. 2019;53(5):1801779. doi: 10.1183/13993003.01779-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cuvelier GDE, Nemecek ER, Wahlstrom JT, et al.. Benefits and challenges with diagnosing chronic and late acute GVHD in children using the NIH consensus criteria. Blood. 2019;134(3):304-316. doi: 10.1182/blood.2019000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kwok WC, Liang BM, Lui MMS, et al.. Rapid versus gradual lung function decline in bronchiolitis obliterans syndrome after haematopoietic stem cell transplantation is associated with survival outcome. Respirology. 2019;24(5):459-466. doi: 10.1111/resp.13472. [DOI] [PubMed] [Google Scholar]
- 62.Williams KM, Cheng GS, Pusic I, et al.. Fluticasone, azithromycin, and montelukast treatment for new-onset bronchiolitis obliterans syndrome after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2016;22(4):710-716. doi: 10.1016/j.bbmt.2015.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Penack O, Marchetti M, Ruutu T, et al.. Prophylaxis and management of graft versus host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2020;7(2):e157-e167. doi: 10.1016/S2352-3026(19)30256-X. [DOI] [PubMed] [Google Scholar]
- 64.Bergeron A, Chevret S, Granata A, et al; ALLOZITHRO Study Investigators. Effect of azithromycin on airflow decline-free survival after allogeneic hematopoietic stem cell transplant: the ALLOZITHRO randomized clinical trial. JAMA. 2017;318(6):557-566. doi: 10.1001/jama.2017.9938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cheng GS, Bondeelle L, Gooley T, et al.. Azithromycin use and increased cancer risk among patients with bronchiolitis obliterans after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26(2):392–400. doi: 10.1016/j.bbmt.2019.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hefazi M, Langer KJ, Khera N, et al.. Extracorporeal photopheresis improves survival in hematopoietic cell transplant patients with bronchiolitis obliterans syndrome without significantly impacting measured pulmonary functions. Biol Blood Marrow Transplant. 2018;24(9):1906-1913. doi: 10.1016/j.bbmt.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 67.Bondeelle L, Chevret S, Hurabielle C, et al.. Effect of ruxolitinib on lung function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2020;26(11):2115-2120. doi: 10.1016/j.bbmt.2020.07.033. [DOI] [PubMed] [Google Scholar]
- 68.Cheng GS, Storer B, Chien JW, et al.. Lung function trajectory in bronchiolitis obliterans syndrome after allogeneic hematopoietic cell transplant. Ann Am Thorac Soc. 2016;13(11):1932-1939. doi: 10.1513/AnnalsATS.201604-262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kliman DS, Kotecha SR, Abelson DC, Snell GI, Glanville AR, Ma DDF. Favorable outcome of lung transplantation for severe pulmonary graft versus host disease: an Australian multicenter case series. Transplantation. 2019;103(12):2602-2607. doi: 10.1097/TP.0000000000002693. [DOI] [PubMed] [Google Scholar]
- 70.Verleden SE, McDonough JE, Schoemans H, et al.. Phenotypical diversity of airway morphology in chronic lung graft vs. host disease after stem cell transplantation. Mod Pathol. 2019;32(6):817-829. doi: 10.1038/s41379-019-0203-2. [DOI] [PubMed] [Google Scholar]
- 71.Takeuchi Y, Miyagawa-Hayashino A, Chen F, et al.. Pleuroparenchymal fibroelastosis and non-specific interstitial pneumonia: frequent pulmonary sequelae of haematopoietic stem cell transplantation. Histopathology. 2015;66(4):536-544. doi: 10.1111/his.12553. [DOI] [PubMed] [Google Scholar]
- 72.Higo H, Miyahara N, Taniguchi A, Maeda Y, Kiura K. Cause of pleuroparenchymal fibroelastosis following allogeneic hematopoietic stem cell transplantation. Respir Investig. 2019;57(4):321-324. doi: 10.1016/j.resinv.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 73.Madanat-Harjuoja LM, Valjento S, Vettenranta K, Kajosaari M, Dyba T, Taskinen M. Pulmonary function following allogeneic stem cell transplantation in childhood: a retrospective cohort study of 51 patients. Pediatr Transplant. 2014;18(6):617-624. doi: 10.1111/petr.12313. [DOI] [PubMed] [Google Scholar]
- 74.Namkoong H, Ishii M, Mori T, et al.. Clinical and radiological characteristics of patients with late-onset severe restrictive lung defect after hematopoietic stem cell transplantation. BMC Pulm Med. 2017;17(1):123. doi: 10.1186/s12890-017-0466-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yang JY, Oh SY, Song JW, et al.. Restrictive chronic lung function decline after haematopoietic stem cell transplantation. Eur Respir J. 2016;47(1):336–339. doi: 10.1183/13993003.00180-2015. [DOI] [PubMed] [Google Scholar]
- 76.L'excellent S, Yakouben K, Delclaux C, Dalle JH, Houdouin V. Lung evaluation in 10 year survivors of pediatric allogeneic hematopoietic stem cell transplantation. Eur J Pediatr. 2019;178(12):1833-1839. doi: 10.1007/s00431-019-03447-z. [DOI] [PubMed] [Google Scholar]
- 77.Yanik GA, Mineishi S, Levine JE, et al.. Soluble tumor necrosis factor receptor: enbrel (etanercept) for subacute pulmonary dysfunction following allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2012; 18(7):1044-1054. doi: 10.1016/j.bbmt.2011.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Blauwkamp TA, Thair S, Rosen MJ, et al.. Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat Microbiol. 2019;4(4):663-674. doi: 10.1038/s41564-018-0349-6. [DOI] [PubMed] [Google Scholar]
- 79.Gwinn M, MacCannell D, Armstrong GL. Next-generation sequencing of infectious pathogens. JAMA. 2019;321(9):893-894. doi: 10.1001/jama.2018.21669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Armstrong AE, Rossoff J, Hollemon D, Hong DK, Muller WJ, Chaudhury S. Cell-free DNA next-generation sequencing successfully detects infectious pathogens in pediatric oncology and hematopoietic stem cell transplant patients at risk for invasive fungal disease. Pediatr Blood Cancer. 2019;66(7):e27734. doi: 10.1002/pbc.27734. [DOI] [PubMed] [Google Scholar]
- 81.Rossoff J, Chaudhury S, Soneji M, et al.. Noninvasive diagnosis of infection using plasma next-generation sequencing: a single-center experience. Open Forum Infect Dis. 2019;6(8):ofz327. doi: 10.1093/ofid/ofz327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Seo S, Renaud C, Kuypers JM, et al.. Idiopathic pneumonia syndrome after hematopoietic cell transplantation: evidence of occult infectious etiologies. Blood. 2015;125(24):3789-3797. doi: 10.1182/blood-2014-12-617035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zinter MS, Hume JR. Effects of hematopoietic cell transplantation on the pulmonary immune response to infection. Front Pediatr. 2021;9(26 January):634566. doi: 10.3389/fped.2021.634566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Panoskaltsis-Mortari A, Griese M, Madtes DK, et al; American Thoracic Society Committee on Idiopathic Pneumonia Syndrome. An official American Thoracic Society research statement: noninfectious lung injury after hematopoietic stem cell transplantation: idiopathic pneumonia syndrome. Am J Respir Crit Care Med. 2011;183(9):1262-1279. doi: 10.1164/rccm.2007-413ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Klein OR, Cooke KR. Idiopathic pneumonia syndrome following hematopoietic stem cell transplantation. J Pediatr Intensive Care. 2014;3(3):147–157. doi: 10.3233/PIC-14098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pagliuca S, Michonneau D, Sicre de Fontbrune F, et al.. Allogeneic reactivity-mediated endothelial cell complications after HSCT: a plea for consensual definitions. Blood Adv. 2019;3(15):2424-2435. doi: 10.1182/bloodadvances.2019000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chellapandian D, Lehrnbecher T, Phillips B, et al.. Bronchoalveolar lavage and lung biopsy in patients with cancer and hematopoietic stem-cell transplantation recipients: a systematic review and meta-analysis. J Clin Oncol. 2015;33(5):501-509. doi: 10.1200/JCO.2014.58.0480. [DOI] [PubMed] [Google Scholar]
- 88.Williams KM, Inamoto Y, Im A, et al.. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease, I: the 2020 Etiology and Prevention Working Group report. Transplant Cell Ther. 2021;27(6):452-466. doi: 10.1016/j.jtct.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kitko CL, Pidala J, Schoemans HM, et al.. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease, IIa: the 2020 Clinical Implementation and Early Diagnosis Working Group report. Transplant Cell Ther. 2021;27(7):545-557. doi: 10.1016/j.jtct.2021.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]