Introduction
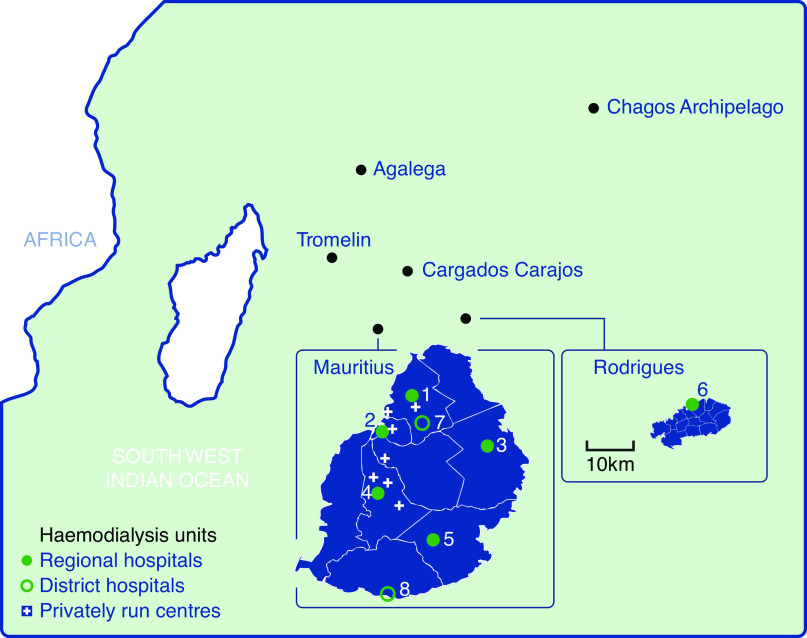
The Republic of Mauritius consists of several groups of small islands, spread over a large area of the south-west Indian Ocean. The largest two islands are Mauritius, 800 km east of Madagascar, and Rodrigues, a further 600 km east of Mauritius (Figure 1). Mauritius is well served by shipping routes and numerous daily international flights. Rodrigues is linked to Mauritius by several daily flights, and less frequently by cargo ships. It is geographically linked to the African continent, but most inhabitants are descended from immigrants from Asia. The main ethnicities are Indian, Creole, Chinese, and European. The population of Mauritius as of December 31,2019 was 1,265,475 people, and there is an ageing population structure compared with most African countries (1).
Figure 1.
The islands of Mauritius in the south-west Indian Ocean off the coast of East Africa, with details of the hemodialysis centers on the two larger islands. 1, Sir Seewoosagur Ramgoolam National Hospital; 2, Dr AG Jeetoo Hospital; 3, Dr Bruno Cheong Hospital; 4, Victoria Hospital; 5, Jawaharlal Nehru Hospital; 6, Queen Elizabeth Hospital; 7, Long Mountain Hospital; and 8, Souillac Hospital.
Mauritius, an upper-middle–income country for many years, was classified as a high income country (2) for the first time in July 2020, just as the devastating coronavirus disease 2019 pandemic struck. In 2017, the Mauritius Gini coefficient was 36.8 (3) and the health expenditure was 6% of GDP (4). The Mauritius welfare system provides a network of community and area health centers, mediclinics, district and specialized hospitals, administered from five larger regional hospitals. Although all aspects of health care are free of charge, a sizeable proportion of the population prefer to pay for the services of general practitioners, specialists, and clinics in the private sector.
Epidemiology
The burden of noncommunicable disease is considerable. Mauritius has ranked in the top five countries worldwide for diabetes prevalence for many years (5). The prevalence of diabetes and of hypertension in 2015 were 23% and 28%, respectively (6). Data on CKD in Mauritius is scarce. The National Noncommunicable Disease Survey (6,7) found a prevalence of eGFR <60 ml/min per 1.73 m2 of 8% in 2009 and of 6% in 2015, but the albuminuria prevalence was 12% in 2009 and 7% in 2015. These somewhat divergent figures do not allow us to confidently estimate a CKD prevalence rate for Mauritius. However, the Global Burden of Disease CKD Collaboration (8) estimated there were 218,000 patients with CKD in 2017 and placed Mauritius second both for CKD prevalence and death due to CKD. Local data for dialysis prevalence and especially incidence (see below) suggest these estimates are reliable.
Patients with CKD are followed up in the community and in physician-led hospital outpatient clinics. Most patients have CKD associated with longstanding diabetes or hypertension and, in these patients, a cutoff creatinine level of 300 μmol/l triggers referral to the nephrology team. Patients with uncertain or rarer diagnoses are referred regardless of renal function.
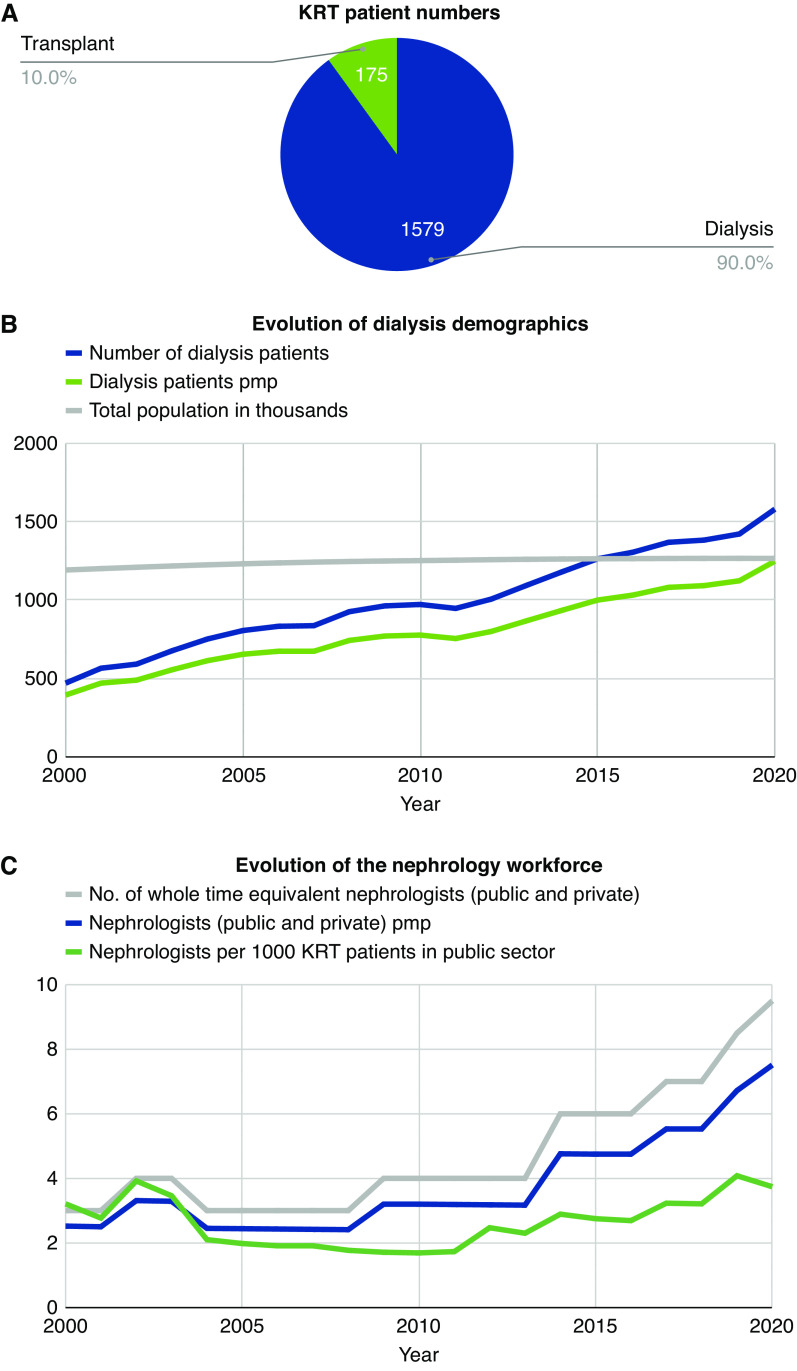
There were 1578 patients on hemodialysis (HD) and one patient on peritoneal dialysis (PD) on December 31, 2020, giving a prevalence rate of 1248 per million population (pmp) for patients on dialysis (9). Including the estimated 175 patients with functioning kidney transplants, the prevalence rate for patients on RRT was 1386 pmp. The incidence of patients going on long-term dialysis was estimated to be 486 pmp (615 patients) in 2020. Comparing the Mauritius 2018 data with the United States Renal Data System International Comparisons data for 2018 (10) places Mauritius in the top 15 countries in the world for prevalence, and in the top five for incidence of patients on RRT. Figure 2 shows the evolution in the prevalence of patients on HD in Mauritius.
Figure 2.
RRT patient numbers, evolution of dialysis demographics and of the nephrology workforce in Mauritius. (A) Number of patients on kidney replacement therapy (KRT) on the 31st December 2020. (B) Evolution of dialysis demographics between 2000 and 2020 as measured by number of dialysis patients, dialysis patients per million population (pmp) and total Mauritius population in thousands. (C) Evolution of the nephrology workforce in Mauritius between 2000 and 2020 as measured by number of whole time equivalent nephrologists (public and private), number of nephrologists (public and private) pmp and nephrologists per 1000 KRT patients in public sector. Source: Ministry of Health and Wellness, Mauritius.
The far smaller autonomous island of Rodrigues had a population of 43,538 on December 31, 2019 (1), of which 29 were on HD. The population, unlike that of Mauritius, is mainly of Creole ethnicity. The dialysis prevalence rate is about 60% that of Mauritius, with a lower rate of diabetes but higher rate of hypertension in the dialysis population. Another difference is the female predominance among patients on dialysis. Patients from Rodrigues are offered free air transfer to hospitals in Mauritius for tertiary medical care, including arteriovenous fistula surgery. Unfortunately, there is no outcome data for the dialysis population of the two islands.
Transplantation
The first form of RRT performed in Mauritius was kidney transplantation on December 17, 1980. Kidney transplantation in Mauritius has a checkered history. The first kidney transplantation was one of 17 performed in private clinics, although the series came to a stop after 2 years. Teams of foreign surgeons performed kidney transplants from 1992 to 1995 in public hospitals. Local surgeons carried out their first transplant in 1993 and took over the program at the end of 1995 (11). However, the local live kidney transplantation program came to a halt with the retirement of the transplant surgeons in 2017. Subsequently, 38 patients were sent to Chennai for transplantation, at a cost to the government of Mauritius, until the coronavirus disease 2019 pandemic struck.
It is estimated that about 550 kidney transplants have been performed on Mauritians, with 389 on Mauritius soil. The precise number of patients who have traveled abroad for a kidney transplant is unknown. There are presently about 175 patients with functioning transplants under follow-up in public hospitals.
Hemodialysis Services
The first HD session was performed in a private center in 1991 and HD only became totally free of charge in 1997. The first public HD unit opened in 1995 at Victoria Hospital and was gradually joined by an increasing number of similar units. Today, the five regional hospitals each have a dialysis unit and supervise smaller units in district hospitals and private clinics. Almost all patients on dialysis are on HD. Table 1 summarizes the main features of dialysis services in Mauritius, whereas Table 2 gives some characteristics of patients on HD in Mauritius.
Table 1.
Dialysis services in Mauritius at December 31, 2020
| Characteristic | Value |
| Number of patients on dialysis (total number and per million people in the general population) | 1579 patients (1578 HD, one PD) in total and 1248 pmp in general population |
| Percent of patients on home dialysis in your country | <0.1% |
| Government funded | Public hospitals 1252 patients |
| Privately run units 313 patients | |
| Patient funded | Privately run units 14 patients |
| Are all dialysis sessions covered by insurance, or do some patients have out-of-pocket expenses? | Public: costs fully covered by government |
| Private: costs fully covered by patient | |
| Are the dialysis units hospital based or freestanding? | Most units are hospital based, a few are freestanding |
| Are the dialysis units for-profit or non-profit? | Non-profit if government run |
| What is the reimbursement per dialysis session in US$? | Not applicable |
| Are all of the staff who deliver dialysis nurses, or do you also use patient care technicians? | Nurses only |
| What is the typical patient to RN ratio in the dialysis units? | 4:1 |
| What is the average length of a dialysis session? | 3 h (thrice weekly) |
| How many times per mo are patients seen by a nephrologist during dialysis sessions? | Once every 3 mo |
| What is the proportion of patients on HD in your country using an AVF, AVG and CVC? | AVF 87%, AVG 0%, CVC 13% |
HD, hemodialysis; PD, peritoneal dialysis; pmp, per million population; RN, registered nurse; AVF, arteriovenous fistula; AVG, arteriovenous graft; CVC, central venous catheter.
Table 2.
Characteristics of Mauritian patients on long term HD (at 1st November 2020)
| Characteristics | Values | |
| Diabetic, % | 55.5 | |
| Viral seropositivity rate, % | Hepatitis B 0.2 | |
| Hepatitis C 2.2 | ||
| HIV 0.5 | ||
| On ESA, % | 79.6 | |
| Using hospital transport, % | 65.3 | |
| Gender, % | Female 37.0 | |
| Female 37.0 | ||
| Age distribution/yra | % of male patients | % of female patients |
| < 20 | 0.9 | 0.9 |
| 20 - 30 | 3.1 | 2.9 |
| 31 - 40 | 6.3 | 7.6 |
| 41 - 50 | 14.4 | 17.6 |
| 51 - 60 | 34.7 | 25.6 |
| 61 - 70 | 28.3 | 32.3 |
| 71 - 80 | 11.4 | 11.4 |
| > 81 | 0.9 | 1.8 |
ESA, erythropoietin stimulating agent.
Based on 77% returns.
The government of Mauritius bears all of the costs for any patient dialyzing within the public scheme, without any restriction at all. Mauritius has a unique arrangement that came about because of a chronic shortage of dialysis space in public hospitals. The government pays a fee of US$20 per session and provides dialysis consumables to participating private units to allow free treatment of patients who cannot be accommodated in public hospitals. Less than 2% of patients on dialysis choose to pay for their treatment in selected private clinics, where the fee per session of dialysis is about US$115.
In addition to free dialysis treatment, patients on dialysis are offered free transport between their home and the dialysis center. They also receive a one-off grant of US$375 from the National Solidarity Fund and are eligible for monthly social security allowance. Drugs present on the hospital formulary (including erythropoietin) are provided free of charge.
A nephrologist determines each individual patient’s treatment plan and evaluating the patient in outpatient clinics every 3 months. Some dialysis units have a trainee physician in attendance. Only certified HD nurses are authorized to perform patient care. The prescription of HD in Mauritius is typically 3 hours, three times per week with bicarbonate dialysate. Both dialysis bloodlines and dialyzers are disposed of after a single use. Dialysis consumables are purchased in bulk by the government for all public patients, allowing economies of scale. Online haemodiafiltration and home HD are unavailable at present. However, all HD centers utilize standard water purification processes, including reverse osmosis systems, and water quality is rarely an issue.
Vascular Access
On November 1, 2020, 87% of patients on HD were dialyzed via an arteriovenous fistula. This is a reasonable performance in comparison with international registry data. Arteriovenous grafts have been used sporadically in the past. No data for vascular access at the start of HD exists, and it is likely that a temporary central venous catheter is the first dialysis access in a large proportion of new patients. Many patients present to nephrologists very late, and many of those who are followed from early on refuse to commit to timely dialysis preparation.
Peritoneal Dialysis
PD has been the modality of treatment for very few patients in Mauritius, with presently only one patient out of 1579 patients on dialysis. The rare patients and their carers are fully trained by the nephrology team and provided with all necessary supplies to carry out PD at home. Yet, there is great reluctance of patients to engage in self-care and poor compliance if they do try. Family members and health staff are expected to step in. The high numbers of dialysis crashlanders — patients presenting with advanced CKD requiring dialysis who weren’t previously under the care of a nephrologist — do not want to shift to PD once started on emergency HD. For many patients, their socioeconomic status is not conducive to PD home dialysis. There is no dedicated PD multidisciplinary team to maintain standards and confidence in the technique.
PD is usually offered as a last resort when options for a vascular access have run out. The failure rate in these unmotivated patients is high. Peritonitis occurs early. As a result, the perception of PD being a second-line therapy, offered only when HD access runs out, is prevalent both in patients and hospital staff. Given the low number of patients, PD costs are inevitably far higher than HD.
Home dialysis in the form of PD has the potential of offering better care at reduced costs, yet there has been no active initiative to increase its use. The entrenched HD dominance can only be challenged if both the government and clinicians campaign vigorously in favor of PD.
Nephrology Workforce
Although it is true that Mauritius has far more nephrologists pmp (npmp) than countries in sub-Saharan Africa, previously published figures of 10 npmp in 2012 and 8 npmp in 2015 are clear overestimates (12–14). The actual figure for 2020 is 7.5 npmp and was far lower previously (see Figure 2). Of note, the Mauritius nephrology workforce can be said to be smaller than that of South Africa (15,16), measured by the number of nephrologists per 1000 patients on RRT (5.4 versus 13.2).
It is also worth noting Mauritian nephrologists have no nephrology team to work with. There are no nephrology trainees and no specialist renal nurses (excluding dialysis nurses). Indeed, Mauritian nephrologists are part of the internal medicine team in the absence of a nephrology department. Presently, neither nephrologist training nor nephrology workforce planning exists. All current nephrologists are Mauritian born, but they have received nephrology training abroad in countries such as the United Kingdom, France, and China.
The Way Forward
Mauritius is a unique country in the African region. Patients with kidney failure are given free and unrestricted access to dialysis, medication, and financial support, despite a CKD prevalence that has climbed rapidly to one of the highest in the world. Unfortunately, a single-track approach has led to most patients being maintained on costly in-center HD. Relaunching and expanding transplantation and PD are priorities. A whole range of strategies is needed to effectively prevent, detect, and slow the progression of CKD, and offer better education and support to patients from an early stage. The National Renal Registry was set up in January 2021 to provide reliable data, essential for such planning. Research publications (17) on kidney disease in Mauritius have been virtually nonexistent and need to be promoted. Significant and sustained investment in infrastructure and the workforce is necessary to build a nephrology service fit to take on the daunting epidemic of kidney disease in Mauritius.
Acknowledgments
The authors thank Mr. Seewoonarain Jugroo (Dialysis Coordinator, Ministry of Health and Wellness, Mauritius) for providing historical and up-to-date data, Dr. S. B. M. Gaya for his valuable suggestions and proofreading the manuscript, and all of the nephrologists and dialysis unit managers in Mauritius for kindly collecting data.
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendations. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
Author Contributions
D. Ip Min Wan conceptualized the study and was responsible for the formal analysis; K. Fagoonee wrote the original draft; and both authors were responsible for data curation and reviewed and edited the manuscript.
Disclosures
D. Ip Min Wan reports having other interests or relationships as the Secretary of the Renal Association of Mauritius, Member of the International Society of Nephrology, and Member of the ISN Africa Regional Board. K. Fagoonee reports having other interests or relationships as the President of The Renal Association of Mauritius, Member of the International Society of Nephrology, and Member of the ISN Fellowship Committee.
Funding
None.
References
- 1.Mauritius S: Population and vital statistics - year 2019. Available at: https://statsmauritius.govmu.org/Documents/Statistics/ESI/2020/EI1505/Pop_Vital_Yr19.pdf. Accessed January 14, 2021
- 2.The World Bank: Mauritius overview, Washington, DC. Available at: https://www.worldbank.org/en/country/mauritius/overview. Accessed January 14, 2021 [Google Scholar]
- 3.The World Bank: World bank open data: GINI index (World Bank estimate) – Mauritius, Washington, DC. Available at: https://data.worldbank.org/indicator/SI.POV.GINI?locations=MU. Accessed January 14, 2021 [Google Scholar]
- 4.World Data Atlas: Mauritius - Current health expenditure as a share of GDP. Available at: https://knoema.com/atlas/Mauritius/Health-expenditure-as-a-share-of-GDP. Accessed January 14, 2021
- 5.International Diabetes Federation: IDF diabetes atlas, 9th Ed., Brussels, Belgium: 2019. Available at: https://www.diabetesatlas.org. Accessed January 14, 2021 [Google Scholar]
- 6.Baker IDI Heart and Diabetes Institute; Ministry of Health and Quality of Life: The trends in diabetes and cardiovascular disease risk in Mauritius-The Mauritius non communicable diseases survey 2009
- 7.Baker IDI Heart and Diabetes Institute; Ministry of Health and Quality of Life: The trends in diabetes and cardiovascular disease risk in Mauritius-The Mauritius non communicable diseases survey 2015
- 8.GBD Chronic Kidney Disease Collaboration: Global, regional, and national burden of chronic kidney disease, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 395: 709–733, 2020. 10.1016/S0140-6736(20)30045-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health and Wellness: Port Louis, Mauritius
- 10.United States Renal Data System: The United States renal data system 2020 annual data report. International comparisons. Available at: https://adr.usrds.org/2020/end-stage-renal-disease/11-international-comparisons
- 11.Gaya SB, Upadhyaya R, Kahn D: The evolution of renal transplantation in Mauritius (1980-1997). Transpl Int 14: 115–116, 2001. 10.1111/j.1432-2277.2001.tb00025.x [DOI] [PubMed] [Google Scholar]
- 12.Pozo ME, Leow JJ, Groen RS, Kamara TB, Hardy MA, Kushner AL: An overview of renal replacement therapy and health care personnel deficiencies in sub-Saharan Africa. Transpl Int 25: 652–657, 2012. 10.1111/j.1432-2277.2012.01468.x [DOI] [PubMed] [Google Scholar]
- 13.Barsoum RS, Khalil SS, Arogundade FA: Fifty years of dialysis in Africa: Challenges and progress. Am J Kidney Dis 65: 502–512, 2015. 10.1053/j.ajkd.2014.11.014 [DOI] [PubMed] [Google Scholar]
- 14.Benghanem Gharbi M: Chronic dialysis programs in African countries: Barriers and successes. World Congress of Nephrology, Cape Town, South Africa, 2015
- 15.Hassen M, Archer E, Pellizzon A, Chikte UME, Davids MR: Human resources for nephrology in South Africa: A mixed-methods study. PLoS One 15: e0228890, 2020. 10.1371/journal.pone.0228890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davids MR, Jardine T, Marais N, Zunza M, Jacobs JC, Sebastian S: South African renal registry annual report 2017. Afr J Nephrol. 22: 60–71, 2019 [Google Scholar]
- 17.Subratty AH, Peeroo K, Jowaheer V, Wah MF, Mohungoo AR: Quality of Life in End Stage Renal Failure Patients Undergoing Dialysis in Mauritius, Mauritius, University of Mauritius Research Journal, 2003, pp 10 [Google Scholar]