Figure 2.
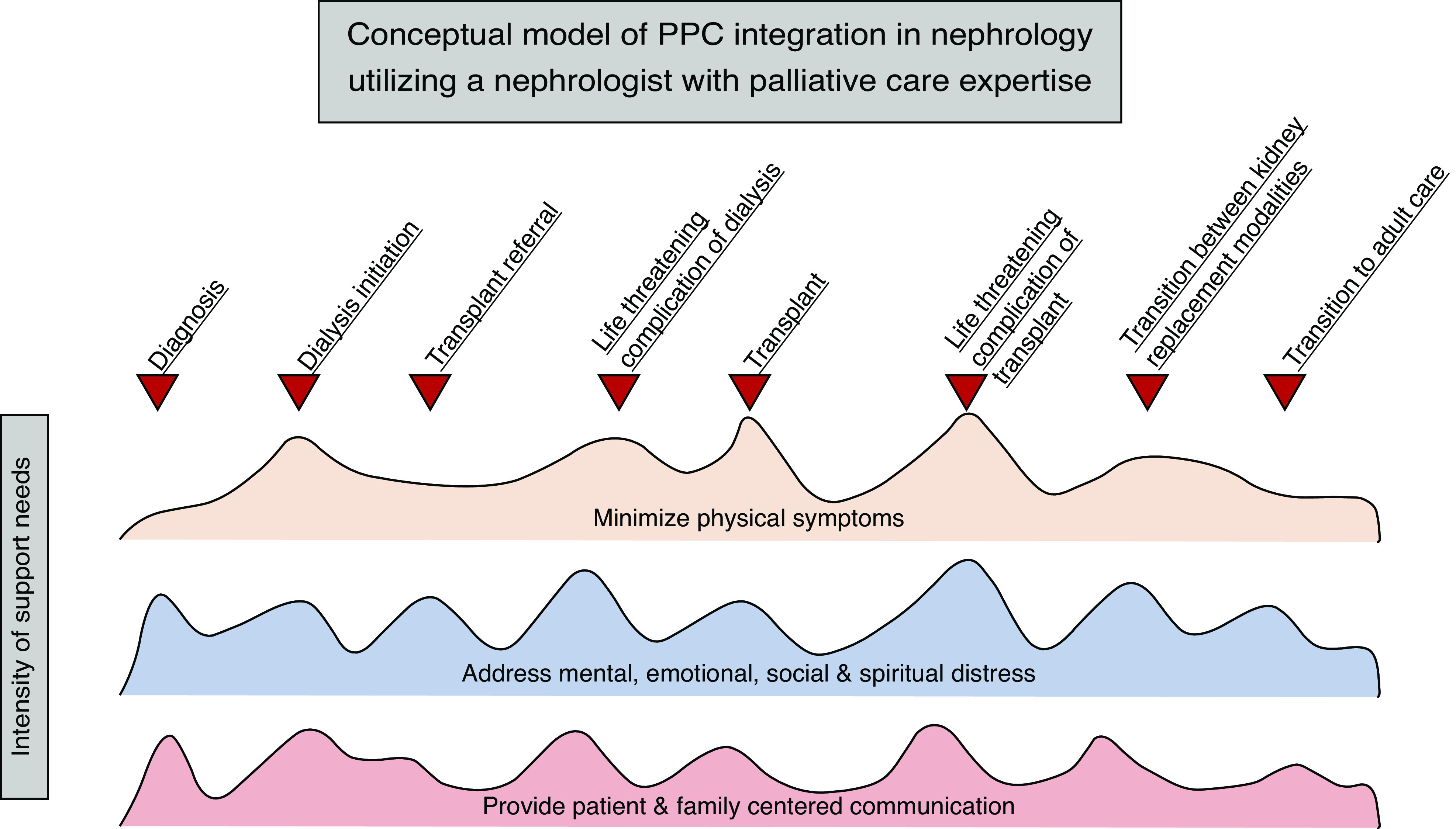
Conceptual model of pediatric palliative care (PPC) integration in nephrology utilizing a nephrologist with palliative care expertise. The domains of PPC should be addressed by the primary nephrologist and multidisciplinary team throughout the disease course, with the intensity of support individualized to the patient and family’s needs at that time in their care. A nephrologist with palliative care expertise is utilized at inflection points in care, when the patient and their family may experience significant changes in symptoms, experiences, burdens, and—ultimately—prognosis. With significant changes, goals of care may need to be revisited or revised, further reinforcing the benefit of additional PPC expertise. Although not every patient and family will experience each of these events, individualized inflection points of care may be identified that require additional burden alleviation. One example of an inflection point, where needs and burdens of patient and family can be more effectively addressed through integration of a nephrologist with palliative care expertise, includes diagnosis of CKD. The patient may already be experiencing resulting sleep disturbance. The patient and family may find it difficult to accept the diagnosis and feel grief that their hopes, goals, and dreams may be altered in the setting of CKD. Extensive questions about prognosis and care planning are likely. Another example of an inflection point that would benefit from integration of a nephrologist with palliative care expertise is at the time of transplant referral. A patient receiving a living, related kidney transplant may endorse emotional distress related to donation from a parent. The family may be anticipating significant financial burden associated with a parent’s donation, resulting in negative effects to the patient, parent, and siblings’ mental health and overall quality of life. Additionally, the patient and family may be overwhelmed with considering the potential complications of transplant, necessitating extra opportunities for patient- and family-centered communication. In both examples, the needs and burdens of the patient, and their family, can be more effectively met through enhanced palliative care provision by a nephrologist with PPC expertise.
