Abstract
Background:
Coaching-in-Context (CinC) is a conversation-based process for working with people that draws on the tenets of positive psychology, is solution-focused and strength-based, and uses evidence-informed coaching techniques that create opportunities for clients to be at their best when engaging in the roles and activities that are desired, required, or expected of them.
Objectives:
To explore the use of CinC with informal maternal care partners (mothers, grandmothers) of children with spinal cord injury (SCI).
Methods:
This study was a multicenter, single group, pre-post treatment design. Participants received up to 10 sessions of CinC over a 10-week period. The Canadian Occupational Performance Measure (COPM), Parenting Stress Index, Fourth Edition Short Form (PSI-4-SF), and Pediatric Measure of Participation Short Form (PMoP SF) were administered before and after coaching. The number of coaching sessions completed, missed, and rescheduled was recorded. Descriptive and nonparametric statistics were used to summarize sample characteristics and to evaluate changed COPM scores. PSI-4-SF stress percentiles were examined descriptively. Wilcoxon signed-rank test was used to determine whether there was a statistically significant change between baseline and postcoaching COPM and PMoP SF scores.
Results:
Nine caregivers enrolled in the study; two had face-to-face coaching, five had phone coaching, and two dropped out. The seven who completed were mothers with an average age of 37.14 (range, 32–45; SD = 5.15) years, with children an average age of 10 (range, 7–13; SD = 2.89) years with paraplegia (n = 4) or tetraplegia (n = 3) sustained an average of 6.71 (range, 2–13; SD = 3.73) years prior to the study. Fifty-five (average = 7.86, mode = 9; range, 3–10) coaching sessions were provided; two sessions were missed and nine were rescheduled. After coaching, mean COPM performance scores increased by 2.48 (SD = 2.01) (Z = −4.057, p < .001), mean COPM satisfaction scores increased by 2.81 (SD = 1.33) (Z = −4.812, p < .001), and PMoP self scores increased (Z = −2.023, p < .043).
Conclusion:
This study provides preliminary support for CinC with informal care partners of children with SCI. It also highlights several factors that are important to consider when implementing a coaching program, namely mode of delivery and time commitment.
Keywords: coaching, informal caregiving, pediatrics
Parents of infants and young children perform a variety of caregiving tasks until children can do these tasks on their own. Parents lift and carry children who are not yet mobile, feed them until they eat independently, change diapers until toilet training is successful, and provide help in many other caregiving routines until children no longer need their assistance. When a child has chronic health conditions or disabilities such as spinal cord injury (SCI), a parent’s role is redefined to include not only usual parenting practices but also practices associated with partnering with their child to address the needs of living and growing up with a chronic health condition.1,2 In addition to their role as informal care partner, parents of children with SCI must arrange and often jointly participate in their children’s activities such as recreation or leisure and orchestrate their children’s participation in family activities such as attending a place of worship and doing errands.3
The majority of informal care partners of children with SCI are mothers4–6 who are central to their children’s health and integration into family, school, and community life.1 Informal caregiving of children with SCI places the care partner and child who receives the care at risk for emotional stress, anxiety, depression and creates barriers to social, vocation, and personal pursuits.6–8 However, informal caregiving has also been described as prosocial behavior by persons who find value and satisfaction in serving and caring for others.9 Parents of children with disabilities have described the positive rewards and benefits of caring for a child with a disability, while acknowledging constraints and other challenges that require productive coping skills, attention to self-care, and solution-focused problem-solving.10–12
Coaching-in-Context (CinC)13,14 aligns with the perspective that informal caregiving can be positive, rewarding, and satisfying when caregiving demands do not exceed personal, social, and psychological resources.9 CinC is a conversation-based process for working with people that draws on the tenets of positive psychology, is solution-focused and strength-based, and uses evidence-informed coaching techniques that create opportunities for clients to be at their best when engaging in the roles and activities that are desired, required, or expected of them. CinC situates clients as resourceful experts and builds upon clients’ strengths to promote awareness and insights about factors that potentially impact their goals and to strengthen problem-solving skills that are solution-focused. CinC conversations are contextualized by the personal, physical, social, cultural, virtual, spiritual, and socioeconomic lived environments and by the requirements and innate desires for competent and satisfying everyday living. The purpose of this study was to explore CinC with informal maternal care partners of children with SCI and to explore its potential for influencing parent and child outcomes.
Methods
A multicenter, single group, pre-post treatment design was used to explore CinC with informal care partners of children and youth with SCI. Purposeful sampling was used to recruit one primary maternal care partner of children with SCI. Care partners were recruited from four pediatric rehabilitation facilities in the United States. They were eligible for study participation if they were a primary informal female care partner of a child with recent or long-standing SCI, willing to be coached over the phone or face-to-face, lived within 1 hour of their assigned coach, had access to a phone or tablet and were willing to use it for remote coaching, and spoke and understood English. Although many children with SCI have more than one informal care partner, we purposefully recruited only one primary maternal care partner. Male care partners were not invited to participate because the overwhelming number of primary informal care partners of children with SCI are female. As such, we sought to prioritize that group for this initial study. The study was approved by the Institutional Review Boards of all participating sites.
Coaching-in-Context
CinC has been discussed13,14 and is briefly described herein. CinC uses an overarching framework comprised of three components: connect, discover, and plan. During connection, a trusting and mutually respectful relationship is formed, and the focus of the coaching session is established. Although the connect component of CinC is predominant early in the coaching relationship, it continues throughout the duration of the coaching session to nourish the trusting and respectful relationship between the coach and client. Through skillful and reflective questions, the discovery component fosters clarity about bridges and barriers to goal achievement. During the discovery component, powerful but simple coaching questions and responses are used to help move the client to deeper awareness and new insights about factors that may influence goal achievement. With clarity, the client is better poised to recognize new opportunities, be receptive to new possibilities, expand awareness of available resources and supporting communities, and become resourceful in defining plans to guide actions toward solutions. Within a given coaching session, connect, discover, and plan components are interwoven seamlessly and are guided by clients’ responses to questions including content and tone of verbal responses, silences during thought and reflection, and other indicators of the client’s desire and readiness for action. Each session closes with an action plan defined by the client. Table 1 provides an overview of each component of CinC and examples of coaching questions, comments, and strategies.
Table 1.
Overview of purpose and general description of Coaching-in-Context (CinC)
| CinC framework | Purpose | General description | Examples of coaching questions/responsesa | Coaching strategies |
|---|---|---|---|---|
| Connect | Establish and maintain mutually trusting relationship Convey genuine belief in and respect for client Establish focus of coaching session | Occurs at the beginning of every coaching session More time is spent connecting earlier in coaching relationship. Seamlessly occurs throughout session, particularly during times when client appears to be shutting down, frustrated, etc. | What’s great in your life right now? What did you accomplish this week that you are most proud of? Last week you told me that you were looking forward to Saturday, how did it go? Sounds like you are having lots of successes, would you be willing to share more about them? That’s too bad the outcome wasn’t what you had planned, what did you learn anyway? Thanks for letting me coach you today, shall we get started? I would love to coach you on that! | Shares an experience that connects with client’s experience Shows gratitude Uses humor Believes in and affirms the client Recalls people, places, events that are important to client from previous sessions and asks about them Asks about actions and goals established at previous coaching sessions |
Table 1.
Overview of purpose and general description of Coaching-in-Context (CinC) (cont.)
| CinC framework | Purpose | General description | Examples of coaching questions/responsesa | Coaching strategies |
|---|---|---|---|---|
| Discover | Gain deeper awareness and new insights Recognize new opportunities and possibilities Strengthen resourcefulness and problem-solving skills Move client to place of readiness to develop actions and identify solutions | Curiosity is used and skillful coaching questions are asked that prompt the client to consider alternatives, reflect on needs, strengths, and values, and be receptive to new possibilities and perspectives. Coach’s responses and reactions are simple, yet powerful and sufficient for the client to deepen their own thinking, reflection, and perspective. These responses can include silence, one word affirmation, and simple questions. Client does the majority of talking. Coach never offers solutions or suggestions without permission. | Is this the problem or is it the solution? What’s stopping you? How can you find out? What have you learned from the situation? What’s the upside of the problem? How would you like it to be? Why does it matter? Of everything you just said, what is most important right now? What is the worst thing that could happen if you did nothing? What are you willing to do about it now? What are you willing to stop doing to improve the situation? If you are successful, who else may benefit? Sounds like a strength to me, what would you say? What persistence you showed! May I share an observation? | Uses silence to allow reflection Matches energy and tone with client’s energy and tone Uses questions that provide clarity: “Is it this or is it that, or is it something else?”, “Is this a should do or want to do?”, “Is this a need or a want?”, “Is this a priority for you or someone else?” Uses questions to mitigate rabbit holes and spiraling stories: “How does this story relate to your coaching goal, or does it?”, “Is this something you want to be coached on, or are you just sharing?” Restates what is heard to make sure it is what client meant Affirms client Checks in with client to make sure they feel like they are working toward session goals(s) Uses connecting questions and strategies to maintain trusting relationship |
Table 1.
Overview of purpose and general description of Coaching-in-Context (CinC) (cont.)
| CinC framework | Purpose | General description | Examples of coaching questions/responsesa | Coaching strategies |
|---|---|---|---|---|
| Plan | Establish actions that are solution focused, feasible, and embraced | Definitive actions are defined and goals made to be accomplished prior to next coaching session Asks client if coaching goals were accomplished | What is the first step you are willing to take? Which of these plans excite you? What strengths can you use or what do you need to accomplish this goal? What are potential barriers to accomplishing this goal, and how will you address them? When will you get started? How will you know if you are successful? That does not sound too convincing. | Affirms client Listens for inconsistencies and communicates them with the client Closes session with questions/comments such as: “What was most useful to you in today’s coaching session?”, “Thank you for allowing me to coach you.” |
Example questions and strategies are not all inclusive and illustrate the types of possible questions and strategies used throughout CinC.
One of four trained coaches was assigned to participants, who received up to ten 60-minute coaching sessions over a 10-week period between August 2018 and May 2019. Ten coaching sessions within a 10-week period was the most a participant could receive. If all coaching sessions were not completed in 10 weeks, follow-up assessments were administered, and coaching was stopped. Every coaching session was audio-recorded and transcribed verbatim.
Coaches and coach training
An occupational therapist, physical therapist, social worker, and psychologist were recruited and trained in CinC. All had experience working in the field of SCI. Although one had prior experience with motivational interviewing, CinC was a novel approach for each of them.
The senior authors (M.J.M., W.D.) are certified positive psychology coaches who provided virtual training on CinC. Training consisted of three 1-hour sessions focused on core coaching principles, the conceptual model for coaching, and the structure of coaching sessions. Between training sessions, coach trainees practiced coaching skills with one another and brought insights, questions, and feedback to subsequent training meetings. Supplemental coach training was provided midway through the study and consisted of three 90-minute sessions. Fidelity to coaching was monitored with a fidelity measure developed by the investigators of this study for purposes of informing the boost coach training. Preliminary psychometric evaluation of the fidelity measure indicated moderate to good interrater reliability, as evidenced by an intraclass correlation coefficient (ICC) of 0.760 with a 95% confidence interval (CI) between 0.682 and 0.827.15
Data collection
At baseline, a research assistant recorded participant characteristics and administered the Beck Anxiety Inventory (BAI).16,17 The BAI is a 21-item patient-reported assessment in which clients rate the degree to which they are bothered by symptoms on a 4-point scale (0 = not bothered at all; 1 = mildly bothered; 2 = moderately bothered; 3 = severely bothered). BAI item-level scores are summed to generate a total score between 0 and 63 that is interpreted as “minimal anxiety” (0–7), “mild anxiety” (8–15), “moderate anxiety” (16–25), and “potential for severe anxiety” (26–63). Participants also completed the beta form of the International SCI Basic Data Set for Caregivers,18 which records hours spent a week in paid employment, informal caregiving, rest and sleep, leisure and socializing, and a burden of caregiving rating between 0 (not at all straining in regard to how burdensome caregiver feels about caring for child with SCI or accompanying child with SCI) and 100 (too straining). These data were used to describe the study sample.
The Parenting Stress Index, Fourth Edition Short Form (PSI-4-SF)19 and the Pediatric Measure of Participation Short Form (PMoP SF)20 were administered before and after the completion of all coaching by a research assistant. The PSI-4 SF is a self-report screening tool that measures overall level of parenting stress (Total Stress Score), level of stress as a function of personal factors directly related to parenting (Parental Distress [PD]), extent to which parent perceives the child as not meeting expectations and interactions with the child not reinforcing the parent role (Parent-Child Dysfunctional Interaction [P-CDI]), and characteristics of the child that influence the parent-child relationship (Difficult Child [DC]). In this study, we focused on total parenting stress, which typically falls within the 15th to 80th percentile. Stress levels in the 81th to 89th and 90th to 100th percentiles are indicative of high and clinically significant stress, respectively.19
We used the parent-reported PMoP SFs to assess parent reports of child participation. The response categories of the parent-reported PMoP SFs are as follows: My child does it as much as they want (as much as their friends); my child does it a little less than they want (a little less than their friends); my child does it a lot less than they want (a lot less than their friends). PMoP SF raw scores are converted to a T-score, where the mean is 50, and standard deviation (SD) is 10.20
Coaches administered the Canadian Occupational Performance Measure (COPM)21 to establish coaching goals and to evaluate the outcomes of CinC. Consistent with the guidelines for administering the COPM, coaching goals were identified based on those that were most important to the participant and could but did not have to be goals directly related to their child with SCI. The COPM uses a 10-point scale (1 = unable to perform, low satisfaction; 10 = performs without a problem, satisfied), which the participant used to rate their current performance and satisfaction with each goal they identified. A change in 2 or more points in the mean score on the COPM indicates clinically significant change.22,23
The study team recorded the number of sessions completed, missed, and rescheduled.
Data management and analysis
Data were deidentified, transmitted to the lead site using Health Insurance Portability and Accountability Act (HIPAA)–compliant procedures, and entered into a secure study-specific database. Audio recordings were also transmitted to the lead site using HIPAA-compliant procedures, stored in a study-specific folder on a secure research drive, and transcribed verbatim. The quality and integrity of the data were monitored throughout the study by two research assistants who independently confirmed data. With the exception of the coaching transcriptions, data were exported to SPSS 26 (IBM Corp., Armonk, NY) for analysis.
Researchers summarized sample characteristics using descriptive statistics and examined relationships using the nonparametric Spearman rank correlation coefficient (rs). Correlation coefficients of .50 to .75 and >.75 were indicative of moderate and good association,24 respectively. Raw PSI-4-SF scores were converted into percentiles using the conversion tables provided in the manual,19 and changes between baseline and follow-up percentiles were examined descriptively. Mean changed COPM performance and satisfaction scores were calculated for each participant. Due to the small sample size, the Wilcoxon signed-rank test was used to determine whether there was a statistically significant change between baseline and postcoaching COPM performance and satisfaction scores and between baseline and postcoaching PMoP SF scores.
Results
As shown in Table 2, nine informal care partners of children with SCI consented and enrolled in the study; two had face-to-face coaching, five had phone coaching, and two dropped out (one phone, one face-to-face). Care partner participants were 38.44 (range, 32–45; SD = 5.25) years of age with children ages 7 to 13 years (mean = 9.56, SD = 2.65). Except for one who had moderate level of anxiety (ID 302), participants had minimal levels (ID 304, 306) or no anxiety. Two participants had high stress levels at the start of the study; one withdrew (ID 305) and the stress level of the other participant (ID 204) lowered after coaching but remained within the high percentile range (87% at baseline to 81% following coaching). On average, participants reported spending 48.06 (range, 0–100; SD = 34.10) hours a week caring for their child on SCI-specific needs, 38.83 (range, 0–80; SD = 30.66) hours a week caring for people other than the child with SCI, 25 (range, 0–65; SD = 21.70) hours in gainful employment, and only 3.56 (range, 0–7; SD = 2.65) and 5.44 (range, 1–15; SD = 4.16) hours in leisure and socializing with others, respectively. The average amount of time spent in rest and sleep each week was 43.33 (range, 28–56; SD = 11.01) hours. Perceived burden was neither low nor high (average score = 48.89; SD = 24.21), but the scores ranged between 10 and 70, with two participants (ID 203, 306) reporting low burden and four others (ID 201, 202, 301, 302, 305) reporting relatively high burden. There were inverse moderate associations between hours worked outside the home and stress (rs = -.709, p = .032) and between caregiver age and anxiety (rs = −.670, p = .049), in which lower levels of stress and anxiety were associated with hours spent in gainful employment and older age, respectively. There was a good and statistically significant association between hours spent in the informal caregiving role and perceived burden (rs = .794, p = .011), in which more time spent in informal caregiving was associated with higher perceived burden. Although not significant, the association between burden and stress was fair (rs = .478, p = .193). No other associations were remarkable, including hours worked outside of the house and burden (rs = −.254, p = .509).
Table 2.
Sample characteristics
| Participant characteristics | Child characteristics | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Modea | ID | Weekly hours spent | |||||||||||||||||
| Age, years | Race | Marital status | Highest education | Anxiety (0–63) | Burden (0–100) | Stress (%) | Paid work | Caring SCI | Caring for others not SCI | Leisure | Social with others | Rest & sleep | Age, years | LOI (AIS) | Cause | Years post SCI | |||
| Face | 301 | 35 | W | M | College | 6 | 70 | 54 | 20 | 67 | 56 | 3 | 4 | 56 | 7 | C6 (UK) | Trauma. | 7 | |
| 302 | 32 | B | NM | HS | 18b | 50 | 56 | 65 | 100 | 70 | 2 | 4 | 56 | 13 | T6 (A) | Infec | 13 | ||
| Phone | 202 | 45 | W | M | College | 7 | 60 | 74 | 24 | 6 | 10 | 5 | 3 | 42 | 11 | L2 (C) | Infec | 10 | |
| 203 | 43 | W | D | College | 5 | 10 | 14 | 40 | 1 | 1 | 7 | 6 | 56 | 12 | T4 (A) | MVA | 6 | ||
| 204 | 35 | B | M | Some college | 6 | 40 | 87† | 34 | 16 | 0 | 0 | 2 | 28 | 13 | T6 (A) | Fall | 2 | ||
| 304 | 32 | W | D | Some college | 15c | 50 | 60 | 0 | 50 | 24 | 7 | 7 | 30 | 7 | Tetra (UK) | Fall | 4 | ||
| 306 | 38 | W | M | Graduate school | 12c | 10 | 12 | 4 | 50 | 45 | 3 | 7 | 42 | 7 | Tetra (UK) | Iatro. | 5 | ||
| Withdrew | 201 | 45 | B | M | Lower than HS | 4 | 60 | 75 | 0 | 62.5 | 62.5 | 0 | 1 | 35 | 8 | C2 (C) | MVA | 5 | |
| 305 | 41 | W | D | HS | 6 | 70 | 81d | 6 | 80 | 80 | 5 | 15 | 45 | 8 | T1 (A) | Fall | 1 | ||
Note: AIS = American Spinal Injury Association Impairment Scale; B = Black/African American; D = divorced; HS = high school; ID = unique study identifier; Iatro = iatrogenic; Infec = infection; LOI = neurological level of injury; M = married; NM = never married; Tetra = tetraplegia; Trauma = traumatic; UK = unknown; W = White/Caucasian.
Mode refers to method of coaching-in-context.
Moderate anxiety.
Mild anxiety.
High stress.
The seven participants who completed the study were mothers with an average age of 37.14 (range, 32–45; SD = 5.15) years with children who were an average age of 10 (range, 7–13; SD = 2.89) years and who sustained paraplegia (n = 4) or tetraplegia (n = 3) from traumatic (n = 4) or nontraumatic (n = 3) SCI an average of 6.71 (range, 2–13; SD = 3.73) years prior to the study. Participants were predominantly White (n = 5), employed (n = 6), married (n = 4), and had a college degree (n = 4). There were no statistically significant differences in characteristics of participants who completed the study and those who did not complete the study.
Coaches completed a total of 55 (average = 7.86, mode = 9; range, 3–10) coaching sessions across the seven participants who completed the study, and participants established a total of 31 COPM goals for leisure (n = 11), self-care (n = 4), and productivity (n = 16). One phone and one face-to-face coaching session were missed, without prior notification. Nine coaching sessions (five face-to-face, four phone) were cancelled ahead of time and rescheduled due to conflicts in schedules. Table 3 shows changed COPM performance and satisfaction scores. After coaching, the mean COPM performance score increased by 2.48 (SD = 2.01) and mean COPM satisfaction score increased by 2.81 (SD = 1.33) (Figure 1). Leisure-related goals demonstrated greatest improvements in which mean performance score increased by 3.27 (Figure 2A) and mean satisfaction score increased by 2.91 (Figure 2B). Statistically significant improvement in both performance in and satisfaction with goals after coaching was evidenced by higher postcoaching median COPM performance (Z = -4.057, p < .001) and satisfaction (Z = -4.812, p < .001) scores. Participants’ report of participation indicated that their children with SCI were participating at levels comparable to other children with SCI as evidenced by baseline mean T-scores of 49.33 (SD = 8.93) and 47.63 (SD = 7.25) for self and friend participation, respectively. After coaching, there was a statistically significant increase in participation-self scores (Z = -2.023, p = .043).
Table 3.
Mean baseline, post coaching, and changed performance and satisfaction scores for participants who completed
| COPM performance scores | COPM satisfaction scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Post coaching | Changed score | Baseline | Post coaching | Changed score | |||||
| ID | Coaching sessions | Goals | Goals ≥ 2 points | Mean (SD) | Mean (SD) | Mean (SD) | Goals ≥ 2 points | Mean (SD) | Mean (SD) | Mean (SD) |
| 202 | 10 | 5 | 5a | 4.2 (1.64) | 7.4 (1.14) | 3.2 (1.10) | 5a | 3.2 (1.64) | 7.2 (0.84) | 4.0 (1.00) |
| 203 | 3 | 3 | 3a | 4.0 (2.00) | 7.3 (0.57) | 3.3 (1.53) | 2b | 4.3 (2.31) | 7.0 (1.00) | 2.7 (1.53) |
| 204 | 9 | 5 | 5a | 2.6 (1.82) | 5.3 (1.48) | 2.6 (0.89) | 4b | 3.4 (2.41) | 5.6 (2.07) | 2.2 (1.10) |
| 301 | 8 | 5 | 3b | 6.2 (1.30) | 8.4 (0.55) | 2.2 (1.30) | 3c | 6.0 (1.58) | 8.2 (0.45) | 2.2 (1.92) |
| 302 | 9 | 5 | 5a | 3.8 (2.17) | 7.8 (1.30) | 4.0 (1.41) | 5a | 4.8 (1.79) | 7.6 (1.52) | 2.8 (0.84) |
| 304 | 9 | 5 | 3d | 5.2 (0.84) | 5.6 (4.23) | 0.4 (3.65) | 4d | 5.4 (0.55) | 8.6 (0.89) | 3.2 (1.30) |
| 306 | 7 | 3 | 2b | 5.3 (0.58) | 7.0 (0.00) | 1.7 (0.58) | 2b | 5.0 (1.00) | 7.3 (0.58) | 2.3 (1.15) |
Note: With exception of performance for participants 304 and 306 (shaded cells), each mother achieved mean improvement in performance and satisfaction of at least 2 points, indicating a clinically meaningful improvement. COPM = Canadian Occupational Performance Measure; ID = participant identification.
Improvement of ≥2 points in every goal.
After coaching, remaining goals improved by 1 point.
After coaching, satisfaction in one goal improved by 1 point and was unchanged in another goal.
After coaching, performance in one goal dropped 5 points and satisfaction improved by 4 points; for another goal, performance dropped 4 points and satisfaction improved 1 point.
Figure 1.
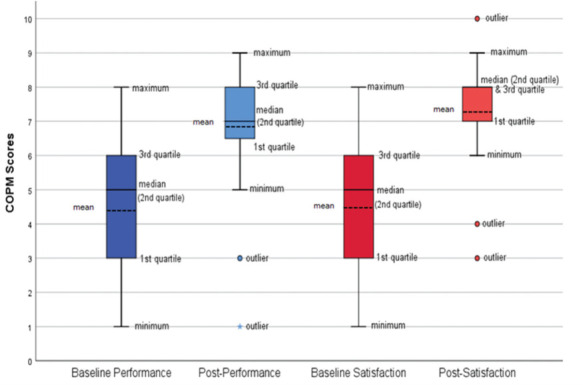
Box and whisker plots showing distribution of performance (blue) and satisfaction (red) scores before and after coaching (n = 31 goals). Upper and lower margins of the box indicate interquartile range. Center solid line sits at median score. Outer bars (whiskers) represent range of scores at each end of distribution, with circles and asterisks indicating outliers. COPM = Canadian Occupational Performance Measure.
Figure 2.
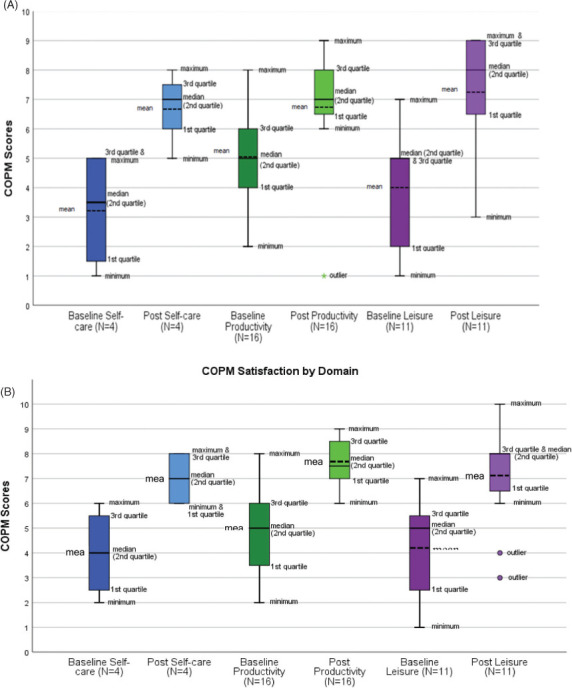
Box and whisker plots showing (A) distribution of performance and (B) satisfaction scores before and after coaching for self-care (blue), productivity (green), and leisure (purple) goals. Upper and lower margins of box indicate interquartile range. Center solid line sits at median score. Outer bars (whiskers) represent range of scores at each end of distribution, with circles and asterisks indicating outliers. COPM = Canadian Occupational Performance Measure.
Discussion
This study shows the potential of CinC for supporting participation of informal care partners in activities associated with leisure, self-care, and productivity. Every participant in this study showed clinically significant improvement (≥2 points) in performance and satisfaction in more than half of the activities identified as coaching goals; performance by three participants improved in every goal, two of whom also reported higher satisfaction with every goal. In addition to the clinical significance of the findings, improvements in performance and satisfaction after coaching were statistically significant.
Coaching outcomes of higher satisfaction despite decline in performance, as seen with two goals (ID 304), have previously been reported14 and may be attributed to new insights and understandings gained by the client through coaching. CinC enables clients to have new insights and heightened awareness of resources, supports, and opportunities that help to achieve goals in ways other than originally imagined. Coaching also helps clients to develop awareness of here-and-now experiences and persist or change behavior and thinking based on their highest values.25 Expanding awareness about values and resources opens the space for reflection to reinvent goals with renewed sense of satisfaction, which is a plausible explanation for lower performance scores and higher satisfaction scores after coaching.
At baseline, three participants reported having mild or moderate anxiety, and two reported having high stress. It is interesting to note that the participants with moderate anxiety and high stress reported clinically significant improvement in performance of every coaching goal, whereas the two mothers with mild anxiety did not reach clinically significant changes. Despite coaching findings that report reduction in parental stress among mothers of very young children with autism,24 the one participant who completed this study with high stress (ID 204) remained within the high percentile range (80%-89%). Because mothers of children with SCI do experience anxiety and stress that have been associated with negative child outcomes,6,7 future studies on CinC should include larger sample sizes that are representative of informal care partners and that provide an opportunity to examine the effects of coaching, not only on parental stress but also on parental anxiety.
CinC has the potential to address unmet needs of informal care partners and their children with SCI. It uses problem-solving, which is an approach that has been identified as highly relevant for care partners with SCI6 and one that has shown to be highly effective for care partners of children with other chronic conditions.26,27 It is also solution-focused. Through CinC, challenges that interfere with engaging in meaningful activities in real-world environments, which children with SCI and their parents report as being problematic,5,28,29 can be identified, understood, reappraised, and surpassed, creating the determination to persevere despite the challenges. In this study, at baseline there was an association between perceived burden and hours spent in the caregiving role and between hours spent in gainful employment and stress level. Perhaps one of the strongest advantages of CinC is its ability to support the prosocial nature of informal caregiving by fostering new behaviors and insights, expanding perspectives and thinking, and identifying resources that allow caregivers to engage in the activities that mitigate adverse outcomes and allow them to flourish in their informal care partner role. For example, in this study, participants identified coaching goals associated with reducing hours spent in the caregiving role (e.g.,“allow other adults to help with her [child’s] care,” “let him [child] take the school bus”) and goals associated with spending more time in leisure and productivity (e.g., “have a weekly parent date night,” “enroll in a class,” spend more time with friends,” “go to the gym”). Future studies should incorporate methods to evaluate outcomes of CinC on anxiety, perceived caregiving burden, satisfaction with the role as a care partner, parental sense of competency, health-related quality of life, and participation outcomes of care partners and the children who receive the care.
Because the health and wellness of informal care partners directly impacts the health and wellness of the child receiving care,7 we explored the outcomes of CinC on participants’ report of their children’s participation. After coaching, participants’ perceptions of their children’s participation improved, with statistically significant improvement in participation compared to what the child wants to do. Although it is possible that children’s participation did improve over the course of coaching, it is also possible that children’s participation remained unchanged but participants’ perspectives changed, and new insights and awareness about children’s participation were gained. It is also possible that children’s participation improved and participants’ perspectives also changed. In future studies on CinC, there is an opportunity to explore the benefits of coaching care partners on child outcomes of participation, as reported by both the care partner and child.
Important lessons were learned from this study. We originally sought to enroll 16 participants, eight for face-to-face coaching and eight for phone coaching, with no preconceived thoughts about which mode of coaching would be more successful or if there would be any differences between the two. Recruitment into the face-to-face group was difficult because participants were required to reside within an hour’s drive of the coach. During the period of open enrollment, the majority of potential participants resided farther away. Thus, only three participants received face-to-face coaching, and one withdrew after her child was discharged from in-patient rehabilitation due to time constraints. A fourth participant, who was assigned to the face-to-face coaching group, received it over the phone at her request. Among the six participants enrolled in phone coaching, one withdrew after three coaching sessions without reason. Another participant completed the study, but she only completed three phone coaching sessions due to her busy work schedule. Of the two participants who withdrew from the study, one was a mother and one was a grandmother. Both received three coaching sessions, one face-to-face and one via phone. Scheduling logistics may have been a contributing factor to their withdrawal from the study. Other factors may have been their relatively high burden, stress levels, and number of hours spent in informal caregiving. Because they did not complete the study, we do not know how or if the three coaching sessions improved performance of and satisfaction with their goals. Nonetheless, their decisions to withdraw from the study warrant consideration.
For successful coaching outcomes, clients must have the emotional and physical energy to engage in coaching conversations and the “readiness” to follow through with actions developed in coaching sessions. Time requirements needed for a coaching program are also a consideration. Coaching via phone or video-conferencing addresses time requirements needed for travel to face-to-face sessions and may provide greater access, especially for caregivers living in rural areas or at long distances from regional health care systems.30 Likewise, in this study we establish the CinC program as up to ten 60-minute coaching sessions over a 10-week period, which was largely based on previous studies of mothers of very young children with autism.26,27,31 Shorter coaching sessions and more flexibility with coaching frequency are important considerations and may make CinC more accessible for care partners. Additional studies on coaching will provide a better understanding about who, why, and when one might best benefit and about optimal “dosing” in terms of length of time and frequency of individual coaching sessions and duration of a coaching program.
The coaches in this study were novices but did receive coach training for this study. The supplemental training provided at mid-study was needed to reinforce several key principles of coaching, based on review of fidelity in audio-recordings. One of which was the use of open-ended questions and strategies to prevent unproductive “story-telling.” The majority of published studies investigating the efficacy of similar conversation-based coaching approaches do not describe the coaching training. Those that do32–36 primarily provided informal coaching training. Only four published studies14,37,38 reported having provided coaches formal training, which ranged from a 2-day workshop to 3 months of weekly 1-hour sessions. Coaching requires a distinct set of skills that are not taught in most entry-level clinical programs. These skills include the ability to craft open-ended questions and probes that foster a journey of self-discovery, active constructive responding, use of silence and short vocalizations to invite self-reflection, and the ability to articulate and use theories and models, such as CinC, to guide coaching conversations. Formal training in coaching is necessary.
There are limitations to this study. Recruitment was challenging due to the study design, which led to small sample size. The coaches in this study were novices. The fidelity measure was used to monitor, not measure, adherence to coaching principles, as it has recently been developed and the psychometric properties are not fully developed. Nonetheless, it served to document observations made while the audio-recordings were reviewed. Work is underway to validate the CinC fidelity measure so that it can be used in future studies.
Conclusion
This study provides preliminary support for CinC with informal care partners of children with SCI. It also highlights several factors that are important when implementing a coaching program, namely mode of delivery and time commitment. Future studies are necessary to better understand optimal timing for coaching post SCI. Studies are also needed to examine the outcomes of coaching children and of dyad coaching (care partner and child together). Improvement in everyday activities is a relevant primary endpoint for coaching outcomes, but secondary endpoints such as parental sense of competency in the informal caregiving role, caregiving burden, and child outcomes are also important and warrant further study.
Acknowledgments
Rebecca Sinko, OTD, Dawn Scheaffer, MSW, LSW, ACM-SW, Colleen Bechtel Driscoll, PhD, and Kristine Lopez, PT, NCS, served as coaches for this study. Hannah Dalton, OTD, and Maclain Capron, BS, are acknowledged for assisting with data analysis. Marie-Christine Potvin, PhD, is acknowledged for her thoughtful review of this manuscript.
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Support
The study was funded by the Craig H. Neilsen Foundation grant #533863 (Mulcahey, PI).
REFERENCES
- 1.Bourke-Taylor H, Howie L, Law M. Impact of caring for a school-aged child with a disability: Understanding mothers’ perspectives. Australian OTJ . 2010;57:127–136. doi: 10.1111/j.1440-1630.2009.00817.x. [DOI] [PubMed] [Google Scholar]
- 2.Nelson A. A metasynthesis: Mothering other than normal children. Qual Health Res . 2002;12(4):515–530. doi: 10.1177/104973202129120043. [DOI] [PubMed] [Google Scholar]
- 3.Kolakowsky-Hayner SA, Kishore R. Caregiver functioning after traumatic injury. NeuroRehabilitation . 1999;13:27–33. [Google Scholar]
- 4.House LA, Russell HF, Kelly EH et al. Rehabilitation and future participation of youth following spinal cord injury: Caregiver perspectives. Spinal Cord . 2009;47:882–886. doi: 10.1038/sc.2009.64. [DOI] [PubMed] [Google Scholar]
- 5.Gorzkowski J, Kelly EH, Klaas SJ, Vogel LC. Obstacles to community participation among youth with spinal cord injury. J Spinal Cord Med . 2011;34(6):576–585. doi: 10.1179/2045772311Y.0000000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly EH, Anderson CJ, Garma SI et al. Relationships between the psychological characteristics of youth with spinal cord injury and their primary caregivers. Spinal Cord . 2011;49:200–205. doi: 10.1038/sc.2010.78. [DOI] [PubMed] [Google Scholar]
- 7.Kelly EH, Riordan AL, Zebracki K et al. Relationships between caregiver characteristics and health-related quality of life among youth with spinal cord injury. Top Spinal Cord Inj Rehabil . 2016;22(2):149–157. doi: 10.1310/sci2016-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolais CJ, Perrin PB, Panyavin I et al. Family dynamics and psychosocial functioning in children with SCI/D from Colombia, South America. J Spinal Cord Med . 2016;39(1):58–65. doi: 10.1179/2045772314Y.0000000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roth DL, Fredman L, Haley WE. Informal caregiving and its impact on health: A reappraisal from population based studies. Gerontologist . 2105;55(2):309–319. doi: 10.1093/geront/gnu177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green SE. “We’re tired, not sad”: Benefits and burdens of mothering a child with a disability. Social Sci Med . 2007;64:150–163. doi: 10.1016/j.socscimed.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 11.Redquest BK, Reinders N, Bryden PJ, Schneider M, Fletcher PC. Raising a child with special needs: The perspective of caregivers. Clin Nurse Spec . 2015;29(3):E8–15. doi: 10.1097/NUR.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 12.Geuze L, Goossensen A. Parents caring for children with normal life span threatening disabilities: A narrative review of literature. Scand J Caring Sci . 2019;33(2):279–297. doi: 10.1111/scs.12643. [DOI] [PubMed] [Google Scholar]
- 13.Potvin MC, Prelock PA, Savard L. Supporting children with autism and their families: A culturally responsive family-driven interprofessional process. Pediatr Clin North Am . 2018;65(1):47–57. doi: 10.1016/j.pcl.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 14.Cadematori C, Alpajora B, Sivori T, Betz S, Gerhardt N, Dunn W, Mulcahey MJ. Preliminary examination of coaching in context with clients with spinal cord injury. Spinal Cord Ser Cases . 2021;17(1):27. doi: 10.1038/s41394-021-00391-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sivori T, Mulcahey MJ. Assessment of fidelity to health coaching in context Doctorate of Occupational Therapy Program Capstone Presentations. Paper 15. 2020. https://jdc.jefferson.edu/otdcapstones/15 .
- 16.Beck AT, Steer RA. Beck Anxiety Inventory Manual . San Antonio: Harcourt Brace and Company; 1993. [Google Scholar]
- 17.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol . 1988;56:893–897. doi: 10.1037/0022006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 18.Haywood C, Martin R, Mulcahey MJ;, The Pediatric International Spinal Cord Injury Basic Data Set Caregiver Workgroup Development of the International SCI Basic Data Set for Caregivers: Capturing data beyond the person with SCI/D. Top Spinal Cord Rehabil . 2018;24(Suppl 1):123–124. [Google Scholar]
- 19.Abidin RR. Parenting Stress Index Professional Manual . Lutz, FL: PAR; 2012. [Google Scholar]
- 20.Mulcahey M, Slavin M, Ni P et al. The Pediatric Measure of Participation (PMoP) short forms. Spinal Cord . 2016;54:1183–1187. doi: 10.1038/sc.2016.68. [DOI] [PubMed] [Google Scholar]
- 21.Law M, Baptiste S, Carswell A Canadian Occupational Performance Measure . 4th ed. Ottawa, ON: CAOT Publications ACE; 2005. [Google Scholar]
- 22.COPM used in research. https://www.thecopm.ca/faq/ Retrieved June 2017.
- 23.Eyssen IC, Steultjens MP, Oud TA et al. Responsiveness of the Canadian Occupational Performance Measure. J Rehabil Res Dev . 2011;48(5):517–528. doi: 10.1682/jrrd.2010.06.0110. [DOI] [PubMed] [Google Scholar]
- 24.Portney LG, Watkins MP. Foundations in Clinical Research Applications to Practice . 3rd ed. Philadelphia: FA Davis; 2015. [Google Scholar]
- 25.Pentland W, Heinz A. What is coaching. In: Pentland W, Isaacs-Young J, Gash J, Heinz A, editors. Enabling Positive Change Coaching Conversation in Occupational Therapy . Ottawa: CAOT Pub; 2016. [Google Scholar]
- 26.Graham F, Rodger S, Ziviani G. Effectiveness of occupational performance coaching in improving children’s and mothers’ performance and mothers’ self-competence. Am J Occup Ther . 2013;67:10–18. doi: 10.5014/ajot.2013.004648. [DOI] [PubMed] [Google Scholar]
- 27.Foster L, Dunn W, Lawson LM. Coaching mothers of children with autism: A qualitative study for occupational therapy. Phys Occup Ther Pediatr . 2013;33(2):253–263. doi: 10.3109/01942638.2012.747581. [DOI] [PubMed] [Google Scholar]
- 28.Mulcahey MJ, Calhoun C, Riley A, Haley S. Children’s reports of activity and participation after sustaining spinal cord injury: A cognitive interviewing study. Dev Neurorehabil . 2009;12(4):191–200. doi: 10.1080/17518420902998177. [DOI] [PubMed] [Google Scholar]
- 29.Mulcahey MJ, DiGiovanni N, Calhoun C et al. Children’s and parents’ perspectives of activity performance and participation following spinal cord injury. Am J Occup Ther . 2010;64(4):605–613. doi: 10.5014/ajot.2010.08148. [DOI] [PubMed] [Google Scholar]
- 30.Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One . 2019;14(8):e0221848. doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Angelin C, Sugi S, Rajendran K. Occupational performance coaching for mothers of children with disabilities in India. Can J Occup Ther . 2021;88(1):38–47. doi: 10.1177/0008417420972868. [DOI] [PubMed] [Google Scholar]
- 32.Graham F, Rodger S, Ziviani J. Effectiveness of occupational performance coaching in improving children’s and mothers’ performance and mothers’ self-competence. Am J Occup Ther . 2013;67(1):10–18. doi: 10.5014/ajot.2013.004648. [DOI] [PubMed] [Google Scholar]
- 33.Kahjoogh MA, Kessler D, Khankeh HR et al. Occupational performance coaching: Goal barriers and beneficial facilitators. Int J Ther Rehabil . 2020;27(3):1–10. [Google Scholar]
- 34.Kahjoogh MA, Kessler D, Hosseini SA et al. Randomized controlled trial of occupational performance coaching for mothers of children with cerebral palsy. Br J Occup Ther . 2019;82(4):213–219. doi: 10.1177/0308022618799944. [DOI] [Google Scholar]
- 35.Little LM, Pope E, Wallisch A, Dunn W. Occupation-based coaching by means of telehealth for families of young children with autism spectrum disorder. Am J Occup Ther . 2018;72(2):1–7. doi: 10.5014/ajot.2018.024786. [DOI] [PubMed] [Google Scholar]
- 36.Dunn W, Cox J, Foster L, Lawson LM, Tanquary J. Impact of a contextual intervention on child participation and parent competence among children with autism spectrum disorders: A pretest-posttest repeated-measures design. Am J Occup Ther . 2012;66(5):520–528. doi: 10.5014/ajot.2012.004119. [DOI] [PubMed] [Google Scholar]
- 37.Graham F, Boland P, Ziviani J, Rodger S. Occupational therapists’ and physiotherapists’ perceptions of implementing occupational performance coaching. Disabil Rehabil . 2018;40:1386–1392. doi: 10.1080/09638288.2017.1295474. [DOI] [PubMed] [Google Scholar]
- 38.Harrington E, Santos G, Potvin MCC. Students’ perceptions of occupational therapy-led coaching in post-secondary education. Open J Occup Ther . 2021;9(2):1–13. doi: 10.15453/2168-6408.1790. [DOI] [Google Scholar]


