Abstract
Objective
This study describes the radiographic diagnosis and nonoperative chiropractic management for a case of a chronic calcaneonavicular coalition in an adult patient.
Background
Calcaneonavicular coalition is a congenital/acquired condition of the tarsal bones often diagnosed in individuals 8–12 years old. Considering its rare presentation (less than 1% of the population), there remains little literature on the conservative management of this condition.
Case presentation
Chronic calcaneonavicular coalition in a 35-year-old recreational athlete is presented.
Management/outcome
Following radiographic diagnosis, the patient was placed in a walking boot for four-weeks. After removal of the boot, the patient was managed nonoperatively. They reported a full resolution of symptoms with noted return to all pre-injury activities.
Summary
Presentation of calcaneonavicular coalition may be dependent on many factors, including age, medical history, and chronicity of the condition. Previous medical background may include recurrent inversion ankle sprains, aggravated with activity, and alleviated with rest. Nonoperative management of calcaneonavicular coalition may be considered as a viable intervention.
Keywords: calcaneonavicular coalition, chiropractic, conservative, non-operative management, tarsal coalition
MOTS CLÉS: coalition calcanéo-naviculaire, chiropratique, conservateur, traitement non chirurgical, coalition tarsienne
Abstract
Objectif
Cette étude présente le diagnostic à l’aide de radiographies et la prise en charge non chirurgicale par la chiropratique d’un cas de coalition calcanéonaviculaire chronique chez un patient adulte.
Contexte
La coalition calcanéo-naviculaire est une affection congénitale ou acquise des tarses souvent diagnostiquée chez des individus âgés de 8 à 12 ans. Comme il s’agit d’une affection rare (moins de 1% de la population), il existe peu de littérature sur le traitement conservateur de cette affection.
Présentation du cas
Présentation d’une coalition calcanéo-naviculaire chronique chez un athlète amateur de 35 ans.
Prise en charge/résultat
Après le diagnostic établi à l’aide de radiographies, le patient a été placé dans une botte de marche orthopédique pendant quatre semaines. Après le retrait de la botte, le patient a été pris en charge de manière non chirurgicale. Tous ses symptômes sont disparus et il a pu reprendre toutes les activités qu’il avait avant sa blessure.
Résumé
La survenue d’une coalition calcanéonaviculaire peut dépendre de nombreux facteurs, dont l’âge, les antécédents médicaux et la chronicité de l’affection. Les antécédents médicaux peuvent inclure des entorses récurrentes de la cheville en inversion, aggravées par l’activité et soulagées par le repos. La prise en charge non chirurgicale de la coalition calcanéo-naviculaire peut être considérée comme une intervention viable.
Introduction
Calcaneonavicular coalition is an abnormal union bridge between the calcaneus and the navicular or tarsal scaphoid bone, and may be osseous (synostosis), cartilaginous (synchondrosis) or fibrous (synfibrosis or syndesmosis).1 It is a congenital or acquired condition of the foot that is usually diagnosed in individuals between the ages of eight to twelve years old2, when secondary ossification centres begin to fuse. While being the most common form of tarsal coalitions3, it presents symptomatically in less than 1% of the population4,5. Additionally, Kernbach et al.6 note that bilateral tarsal coalitions are quite common in the adolescent population, occurring in as many as 80% of patients with this condition.
Patients may typically present with a slight antalgic gait, with possible examination findings of a flattened medial longitudinal arch, peroneal spastic flat foot, and decreased subtalar motion.6,7 Pain will often be worsened with activity and improve with rest, and they may report recurrent ankle sprains.8 While high-quality evidence for conservative management of patients presenting with this condition remains scarce (consisting mostly of case reports/series)2, review of the literature involves mostly youth/adolescent patients, with adult population management poorly represented. Of the evidence found, some nonoperative treatment options include activity modification, non-steroidal anti-inflammatory drugs, orthotics, and immobilization in a walking boot.2 Considering thus far the efficacy of these interventions has been poorly established, many patients and healthcare providers still prefer resection surgery to non-operative interventions. Therefore, the purpose of this case report includes calcaneonavicular coalition and chronic pain presentations, key radiographic findings, along with additional diagnostic imaging options, and collaborative management for this condition.
Case presentation
A 35-year-old male presented to a chiropractor with a complaint of left lateral foot pain of nearly three years duration. The patient reported the pain originally presented on the dorsum of the foot during the first few steps of weightbearing. Examination revealed full ankle ranges of motion and pain was reproduced with only digital pressure between the third and fourth digits. In addition to the orthopaedic examination, x-rays were prescribed to rule out any osseus abnormalities. Due to various possible factors (including human error in foot positioning, or radiographic interpretation), the original radiographic report revealed an os trigonum to be the only abnormal finding, and thus the patient was diagnosed as having an interdigital neuroma.
Following intermittent resolution of his symptoms, the patient returned 18 months later to the same facility complaining of pain more laterally in the foot, aggravated by activities (soccer) involving running for any more than a few minutes. On this occasion examination findings were positive for left ankle instability (anterior drawer test) and cuboid syndrome (dorsal plantar cuboid shear test of cuboid on calcaneus), though were notably negative for any navicular tenderness/immobility. Of note, anterior drawer test has a sensitivity of 0.74 95% CI (0.58–0.86) and specificity of 0.38 95% CI (0.24–0.56).9 Attempts at determining the specificity and sensitivity of the shear test for cuboid syndrome were unsuccessful, with Curall noting a lack of any evidence-based guidelines for this condition.10
Intervention originally included soft tissue treatment (Achilles tendon, gastrocnemius/soleus complex, and peroneal musculature), laser (lateral ligaments), proprioception activities, and foot mobilizations to the cuboid as needed. Cuboid intervention was performed through the use of a toggle-board extremity drop piece. The patient’s foot was placed in a neutral position with slight eversion on the drop piece. The practitioner placed their second and third digits under the cuboid. Using a high-velocity low amplitude thrust on the dorsal surface of the foot (towards the floor), the cuboid is translated dorsally into its normal biomechanical position in relation to the surrounding tarsals and metatarsals (Figure 1). Additionally, taping of the cuboid was performed to provide additional support and stability to the lateral foot through the use of Leukotape rigid stressing tape and (since it cannot be applied directly on skin) generic surgical dressing tape. A loop of surgical dressing tape is applied around the midfoot area directly to the skin. The rigid tape is then applied on the plantar aspect of the midfoot, and tension is applied around the lateral aspect of the foot to the dorsum of the foot) to simulate proper dorsal stability for the cuboid. Given the ability of prolonged adherence of the surgical dressing tape, the tape job can safely remain for as long as the tape adheres (two to three days) or as needed (Figures 2a and 2b). Additionally, taping or bracing of the ankle was recommended for sporting activities.
Figure 1.
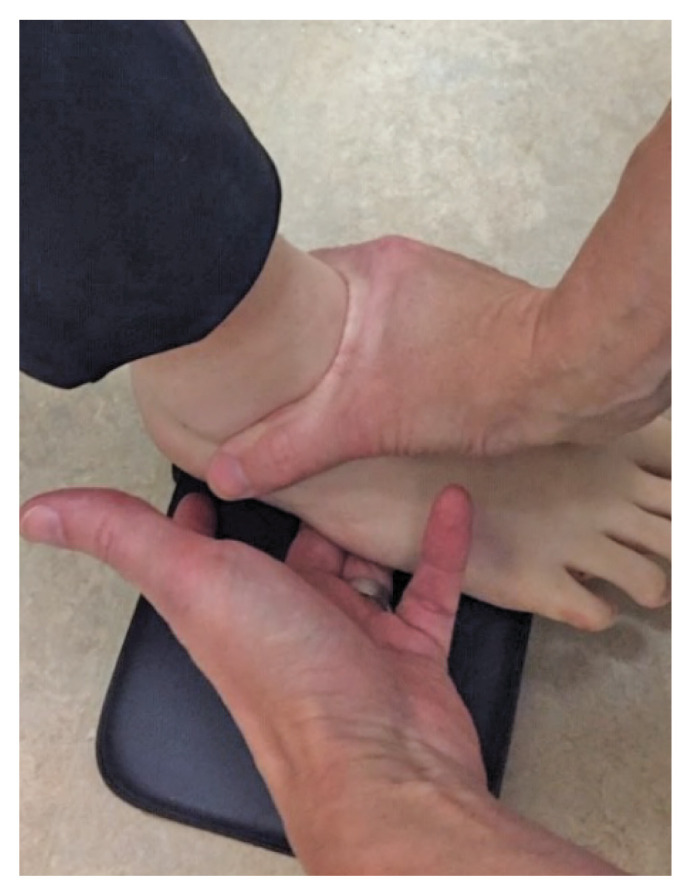
Cuboid EMT with use of toggle board drop piece.
Figure 2.
2A (left). Cuboid taping with noted beginning of tension direction (“B”).
2B (right). Cuboid taping with noted direction of tension (arrows) and end point (“E”).
After many months of recurrent intermittent foot pain and multiple inversion sprains, the patient’s subjective pain reporting would continue to vary. On some days they reported pain and difficulties with activities, and on others reported feeling as beginning to show moderate improvement under the authors’ care, even expressing during one visit they might be on the way to a “full recovery”. During this time the patient had also noted an increased sensitivity in the foot, with the area of pain changing and widening over time.
Management of the patient reached a turning point when the patient presented to the clinic unable to weight bear on the left foot after a soccer game the previous evening, with no reported mechanism. X-rays were immediately prescribed under the suspicion of a stress fracture. Radiographic interpretation revealed diagnosis of a calcaneonavicular coalition (see Figures 3 and 4), with no other findings. A walking boot was prescribed, along with referral to a sports medicine physician for further imaging and an orthopaedic consultation.
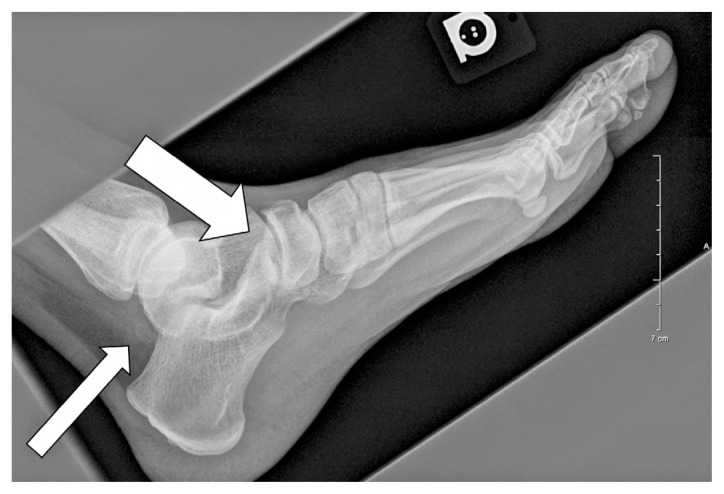
Figure 3.
AP and oblique radiograph views of a 35-year-old male with calcaneonavicular coalition. On the AP view note how the proximal portion of the navicular is wider than the talonavicular joint, and the lateral aspect of the navicular has a tapered, elongated appearance. On the oblique view, the accessory joint formed at the anterior calcaneal process and lateral aspect of the navicular (arrow), consistent with a cartilaginous calcaneonavicular coalition.
Figure 4.
A lateral radiograph of the same patient. Note the elongation of the superior calcaneus (arrow) and flattening of the longitudinal arch. Additionally, a non-united posterior talar process is detected, consistent with an os trigonum (thin arrow).
The sports medicine physician recommended continued use of the walking boot, along with referral for a bone scan and MRI (Figures 5–7) and orthopaedic consultation regarding possible surgical intervention. The patient remained in a walking boot for four weeks and continued to receive conservative care, while experiencing intermittent bouts of lateral foot pain.
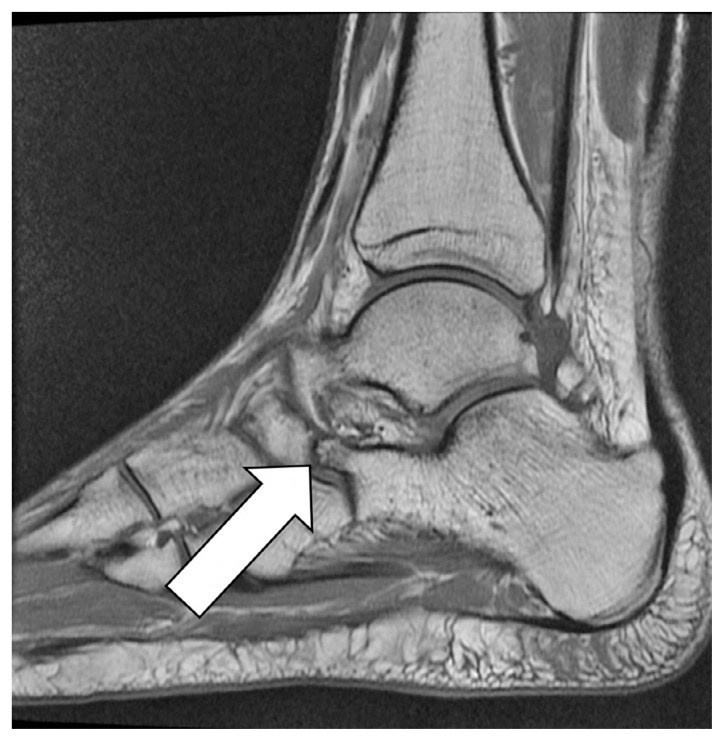
Figure 5.
Axial T1-weighted MRI image. As in Figure 3, note the proximal portion of the navicular is wider than the talonavicular joint, and the lateral aspect of the navicular has a tapered, elongated appearance. Unlike the radiograph, sclerosis, bone proliferation, and irregularity of the calcaneonavicular joint (arrow) more visibly demonstrates this non-osseous joint coalition.
Figure 6.
Sagittal T1-weighted MRI image. As in Figure 5, there is demonstration of a prominent anterior process of the calcaneus (arrow), equivalent to the radiographic anteater sign.
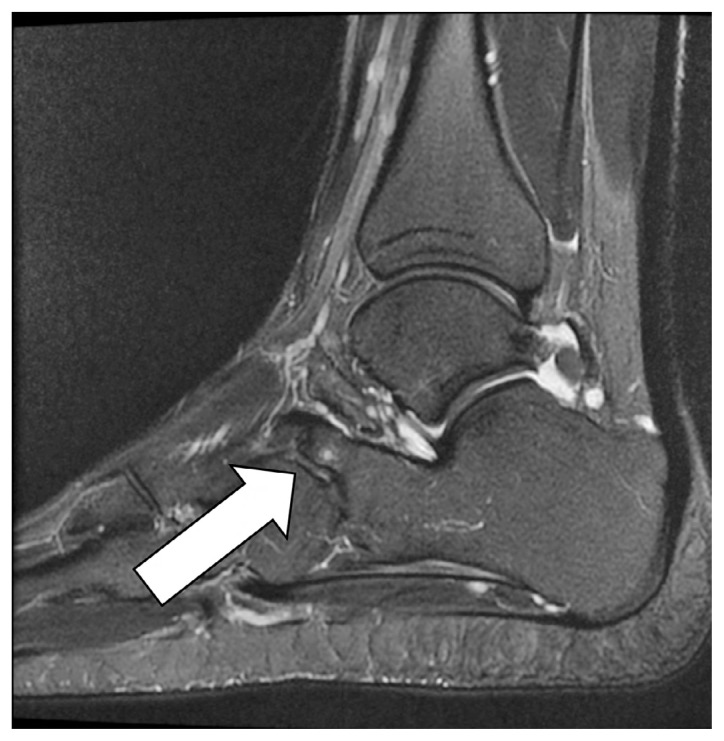
Figure 7.
Sagittal T2-weighted fat-suppressed MRI image. with a visualized joint and adjacent bone marrow edema (arrow), and a small subchondral cyst in the elongated process of the calcaneus.
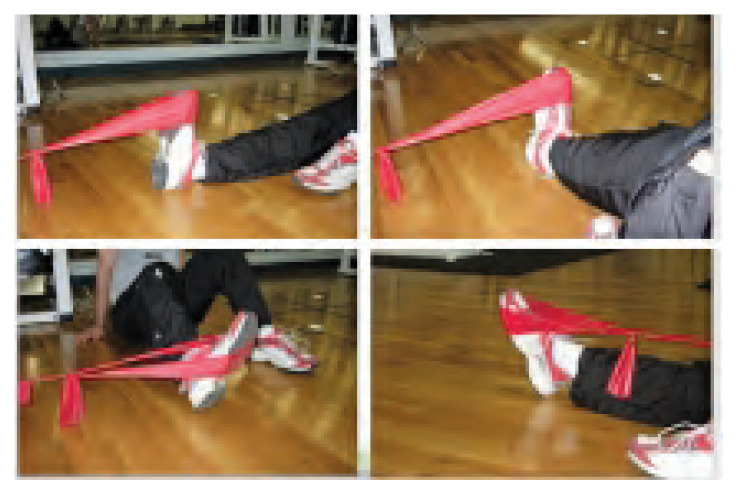
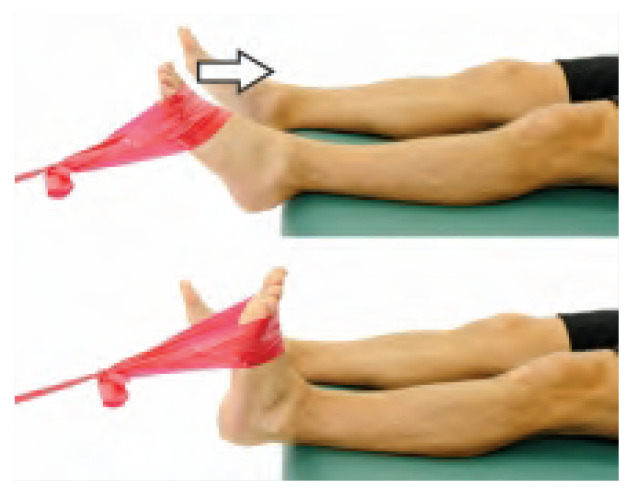
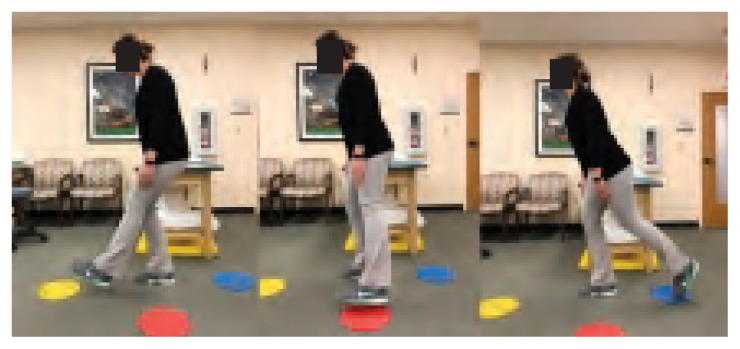
During boot immobilization, intervention involved soft tissue treatment as above, pain control (pre-modular interferential current), intrinsic foot exercises, and isometric ankle strengthening. The patient was also encouraged to continue with non-impact aerobic activities (stationary bike, swimming). Following removal of the walking boot, the patient’s rehabilitation consisted of resistance band strengthening (focusing on dorsi-flexion and eversion), single leg proprioception activities (one-legged stance, star excursions, progressing onto unstable surfaces), and closed kinetic chain strengthening (single-leg squat). All exercises began with a focus on functional strength increases (3 sets of 10–12 repetitions), with eventual progression to functional endurance (2 sets of 15–20 repetitions). The patient was instructed to perform these exercises daily (when not in clinic), and sets/reps and frequency were adjusted as the patient’s symptoms improved and objective measurement improved (See Table 1).
Table 1.
Rehabilitation exercise protocol
Passive management consisted of soft tissue treatment, mobilizations of the first ray and talus (ensuring normal accessory movements through the sagittal planes) and pain control (as needed). Upon re-evaluation of the foot a 90% improvement was noted, although with a new complaint of bilateral plantar fascial pain. In addition to above interventions, the patient was prescribed full-length custom orthotics for use in all footwear. Given confirmation of the radiological findings at re-evaluation (and the MRI results), the patient declined the option of coalition resection and decided to modify his activities. At the time, the patient opted for swimming as a primary aerobic activity as they were apprehensive that the impact of soccer would re-aggravate his foot pain. However, at one-year follow-up the patient was happy to report that they gradually returned to soccer, using the custom orthotic in their footwear. To date the patient has not experienced any foot discomfort with all activities.
Discussion
Pain presentation
In the adult population, many tarsal coalitions are discovered incidentally while a patient is being evaluated for a different condition.11 Varner et al.12 retrospectively reviewed 27 adult patients with a coalition and found that two-thirds of these were discovered during workup for symptoms such as an ankle instability and sinus tarsi pain, whereas one-third of the adult patients were completely asymptomatic. With a calcaneonavicular coalition restricting motion in the midfoot, forceful motion beyond the restricted range may result in partial or complete ligamentous injuries to the ankle. If hindfoot or midfoot motion is restricted, more trauma is inflicted to the ankle ligaments in an effort to dissipate the forces exerted. In cutting, pivoting, or decelerating, different mechanisms may result in different injuries.13
In addition to the added stress placed on other structures of the foot due to the coalition, one must also consider the chronic presentation of this condition over time. Osteoarthritic changes were observed on the Sagittal T2-weighted fat-supressed MRI in Figure 7 including: bone marrow edema and a small subchondral cyst. It is likely that these degenerative changes could have contributed to the recurrent bouts of pain experienced by the patient.
Additionally, due to the patient’s prolonged pain complaints and change in clinical presentation area, the possibility of nociceptive hypersensitivity was also considered. In states of chronic pain, nociceptive and non-nociceptive sensory afferents are sensitized.14 One mechanism used to describe the genesis of chronic pain is peripheral sensitization, which constitutes a decreased threshold and increased responsiveness of nociceptors due to post-translational changes in the area and altered trafficking of transducer receptors and ion channels.15 Also known as primary hyperalgesia, this sensitization of nociceptors is a protective action of the human body to prevent use and consequent further damage to traumatized area and surrounding tissues. However, with a diffuse pain distribution central sensitization, which is a process characterized by generalized hypersensitivity of the somatosensory system16,17. As Nijs et al.16 note, the longer pain persists, the more likely central sensitization becomes a more dominant component to the clinical presentation. Given the timelines of the patient’s complaint and the fact their pain location (lateral foot) was different from the area of coalition, the practitioner could therefore consider sensitization as an additional contributing factor in the clinical presentation.
Imaging diagnosis
Due to the different types of possible coalition, a review of literature revealed differing viewpoints on imaging for this condition. One review reported that as many as 94% of adult coalitions could be found on plain radiographs alone.12 However, Hochman et al.18 suggested CT is the best imaging technique for examining coalitions, based on its ease of use, allowance for bilateral comparison, and improved visualization of the location, size, and type of coalition. Yet another paper noted that despite suggestive clinical signs, standard X-rays may miss the diagnosis due to the lack of synostosis.1 MRI identified, located and characterized symptomatic lesions that were not necessarily visible on CT, enabling preoperative planning for adapted surgery.
In terms of radiographic diagnosis, one paper suggested routine anteroposterior and lateral unenhanced radiographs are a sensitive screening test for both talocalcaneal and calcaneonavicular coalitions, even with observers who had no prior experience.7 However, others opined that calcaneonavicular coalitions are difficult to visualize on radiographs due to the complex orientation of the joint; thus the best view to see the coalition is an internal oblique view as this lays the calcaneonavicular interface out for inspection and therefore best displays various signs of a calcaneonavicular coalition.6 In accordance to the literature, the coalition was best visualized in the AP oblique view (Figure 3).
Crim et al.8 note a calcaneonavicular bar can be seen on anteroposterior radiographs in a substantial number of coalition cases if careful attention is paid to the lateral margin of the navicular bone. The shape of the navicular bone is altered by the presence of a coalition.7 Therefore, in addition to showing the calcaneonavicular bar, the anteroposterior radiograph often reveals that the proximal portion of the navicular bone is wider than the talonavicular joint and that the lateral aspect of the navicular bone has a tapered, elongated appearance. Other radiographic features that have been shown to indicate the presence of a calcaneonavicular coalition (as seen in this case) include the “anteater nose”, seen on the lateral view as an elongation of the anterior process of the calcaneus toward the navicular for a calcaneonavicular coalition.19 Lawrence et al.7 note the presence of this elongated anterior calcaneal process is highly suggestive of a calcaneonavicular coalition, with a specificity of 94%.
Operative versus nonoperative management
In terms of management, most of the literature revealed management through surgical resection of the coalition. Cohen et al.4 noted that resection of a calcaneonavicular coalition in the adult (in the absence of significant degenerative changes of the talonavicular and subtalar joints), could be successful, providing an option to arthrodesis when nonoperative methods have failed. Additionally, Mahan et al.20 noted that although physician-based outcomes such as foot alignment are important in tarsal coalition surgery, patient-reported outcomes of pain, daily function, and return to high-level sports are of paramount importance in assessing whether tarsal coalition surgery can reliably offer a high-quality result. In their study, 73% of patients reported unlimited activity, with no difference in reported outcomes between the calcaneonavicular and talocalcaneal groups.
However, unlike adolescent coalitions, nonoperative treatment may be even more effective in the adult patient, as many are asymptomatic or discovered after injury.2,4 Various studies note the treatment of adult tarsal coalitions should begin with nonoperative treatment. This can include activity modification, physical therapy, orthotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and short leg cast immobilization for 4 to 6 weeks.2, 12 However, while some studies have shown a nonoperative treatment protocol to be effective, other authors’ results have been variable. In their review, Flynn et al.11 note differing success rates between 15% and 67% in non-operative management of subtalar coalitions12. Therefore, it may be difficult to draw any firm conclusions.
In this case, non-operative management was successful once a proper diagnosis was rendered. Given the myriad subjective pain reporting by the patient and undulating clinical presentations, prior interventions resulted in only temporary improvements. Achieving a proper diagnosis was the primary challenge in this case, and was reliant upon multi-disciplinary involvement, including various imaging modalities and chronic pain management.
Summary
Given its rare presentation in adults, differing etiologic factors, pain presentations (including possible pain sensitization), and differing views on imaging diagnosis and management, the evidence base regarding calcaneonavicular coalition, particularly in the adult population, remains quite poor. This case demonstrates the challenges experienced in the diagnosis and management of such a condition, and the options available to a practitioner. Additionally, as was noted earlier, the role of central sensitization contributing to the presentation should have been considered and could have resulted in earlier referral for diagnostic imaging and resolution of this complaint. Ultimately, a cooperative multi-disciplinary approach in diagnosing this condition, along with a nonoperative management, led to a favourable pain and functional outcome result for the patient. While this management protocol was sufficient for this patient, it is important to remember many factors (i.e. presence of arthritic change) not discussed can affect the decision making of such a case. An evidence-based practice approach involving clinical expertise, external evidence, and patient values and expectations must always be considered. Should nonoperative management not result in favourable outcome, then an algorithm for surgical management for adult subtalar coalition should be considered.11 Prior to implementing any such diagnostic or nonoperative management protocols in a condition such as this, further investigation in larger, controlled trials is recommended.
Footnotes
The authors have no disclaimers, competing interests, or sources of support or funding to report in the preparation of this manuscript. The involved patient provided consent for case publication.
References
- 1.Guignand D, Journeau P, Mainard-Simard L, Popkov D, Haumont T, Lascombes P. Child calcaneonavicular coalitions: MRI diagnostic value in a 19-case series. Orthopaed Traumatol Surg Res. 2011;97:67–72. doi: 10.1016/j.otsr.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Shirley E, Gheorghe R, Neal KM. Results of nonoperative treatment for symptomatic tarsal coalitions. Cureus. 2018;10(7):1–7. doi: 10.7759/cureus.2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masquijo J, Allende V, Torres-Gomez A, Dobbs MB. Fat graft and bone wax interposition provides better functional outcomes and lower reossification rates than extensor digitorum brevis after calcaneonavicular coalition resection. J Pediatr Orthop. 2017:1–5. doi: 10.1097/BPO.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 4.Cohen BE, Hodges Davis W, Anderson RB. Success of calcaneonavicular coalition resection in the adult population. Foot Ankle Intl. 1996;9(17):569–572. doi: 10.1177/107110079601700912. [DOI] [PubMed] [Google Scholar]
- 5.Mubarak SJ, Patel PN, Upasani VV, Moor MA, Wegner DR. Calcaneonavicular coalition: treatment by excision and fat graft. J Pediatr Orthop. 2009;29(5):418–426. doi: 10.1097/BPO.0b013e3181aa24c0. [DOI] [PubMed] [Google Scholar]
- 6.Kernbach KK. Tarsal coalitions: etiology, diagnosis, imaging, and stigmata. Clin Podiatr Med Surg. 2010;27:105–117. doi: 10.1016/j.cpm.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 7.Lawrence DA, Rolen MF, Haims AH, Zayour Z, Moukaddam HA. Tarsal coalitions: radiographic, CT, and MR imaging findings. HSS J. 2014;10:153–166. doi: 10.1007/s11420-013-9379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crim JR, Kjeldsberg KM. Radiographic diagnosis of tarsal coalition. Am J Roentgenol. 2004;182:323–328. doi: 10.2214/ajr.182.2.1820323. [DOI] [PubMed] [Google Scholar]
- 9.Croy T, Koppenhaver S, Saliba S, Hertel J. Anterior talocrural joint laxity: diagnostic accuracy of the anterior drawer test of the ankle. J Orthopaed Sports Phys Ther. 2013;43(12):911–919. doi: 10.2519/jospt.2013.4679. [DOI] [PubMed] [Google Scholar]
- 10.Curall CJ. Examination and treatment of cuboid syndrome: a literature review. Sports Health. 2011;3(6):514–519. doi: 10.1177/1941738111405965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flynn JF, Wukich DK, Conti SF, Hasselman CT, Hogan MV, Kline AJ. Subtalar coalitions in the adult. Foot Ankle Clin N Am. 2015;20:283–291. doi: 10.1016/j.fcl.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Varner KE, Michelson JD. Tarsal coalition in adults. Foot Ankle Intl. 2000;21:669–672. doi: 10.1177/107110070002100807. [DOI] [PubMed] [Google Scholar]
- 13.Snyder RB, Lipscomb B, Johnston RK. The relationship of tarsal coalitions to ankle sprains in athletes. Am J Sports Med. 1981;9(5):313–317. doi: 10.1177/036354658100900505. [DOI] [PubMed] [Google Scholar]
- 14.Gangadharan V, Kuner R. Pain hypersensitivity mechanisms at a glance. Disease Models Mech. 2013;6(4):889–895. doi: 10.1242/dmm.011502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiegel DR, Pattison A, Lyons A, Ansari U, McCroskey AL, Luehrs E, Barr L, Le S. The role and treatment implications of peripheral and central processing of pain, pruritus, and nausea in heightened somatic awareness: a review. Innov Clin Neurosci. 2017;14(5–6):11–20. [PMC free article] [PubMed] [Google Scholar]
- 16.Nijs J, Van Houdenhove B, Oostendorp RAB. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice (Masterclass) Man Ther. 2010;15:135–141. doi: 10.1016/j.math.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3):S2–15. doi: 10.1016/j.pain.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hochman M, Reed MH. Features of calcaneonavicular coalition on coronal computed tomography. Skelet Radiol. 2009;29:409–412. doi: 10.1007/s002560000211. [DOI] [PubMed] [Google Scholar]
- 19.Thorpe SW, Wukich DK. Tarsal Coalitions in the adult population. Does treatment differ from the adolescent? Foot Ankle Clin. 2012;17(2):195–204. doi: 10.1016/j.fcl.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Mahan ST, Spencer SA, Vezeridis PS, Kasser JR. Patient-reported outcomes of tarsal coalitions treated with surgical excisions. J Pediatr Orthopaed. 2015;35(6):583–588. doi: 10.1097/BPO.0000000000000334. [DOI] [PubMed] [Google Scholar]