Abstract
Aim
There is both favorable and controversial evidence on the application of telemedicine in the emergency department (ED), which has created uncertainty regarding the effectiveness of these systems. We performed a systematic review of the literature on systematic reviews to provide an overview of the benefits and challenges to the application of telemedicine systems for the ED.
Subject and methods
PubMed, Web of Science, Scopus, Cochrane Library, and Google Scholar databases were explored for systematic reviews of telemedicine applications for the ED. Each review was critically appraised by two authors for data items to be extracted and evaluated. The most highly recommended technology, feasibility, benefits, and challenges to the application of telemedicine systems were studied and reported.
Results
We identified 18 studies of varying methodological quality and summarized their key findings. Form these 18 studies, 12 papers yielded a high risk of bias in their investigation. Nine papers concluded that real-time video conferencing was the best method of delivery, eight papers found cost reduction as an outcome of implementing these systems, and six studies found technical and infrastructure issues as a challenge when implementing telemedicine for EDs.
Conclusion
There is strong evidence suggesting that the use of telemedicine positively impacts patient care. However, there are many challenges in implementing telemedicine that may impede the process or even impact patient safety. In conclusion, despite the high potential of telemedicine systems, there is still a need for better quality of evidence in order to confirm their feasibility in the ED.
Keywords: Benefit, Challenge, Telemedicine, Emergency department, Systematic review
Introduction
Emergency departments (ED) are one of the most critical and sensitive sections of the hospital, and how they function can have a considerable effect on other sections and patient satisfaction. The performance of the ED is a key measure in evaluating a hospital's role in providing services to the people. Each year, there are approximately 30 million critically ill patients in the United States, and the ED provides urgent healthcare for them. This massive number of admissions decreases the time providers can spend with a patient, leading to increased medical error rates (Trzeciak and Rivers 2003). Moreover, it increases the wait time for treatment, which results in ED overcrowding (Trzeciak and Rivers 2003).
Due to rising healthcare costs and patient expectations, and in light of technological advances that have reduced the cost of necessary equipment, the use of telemedicine for providing healthcare services has seen rapid development (Whitten et al. 2002).
Telemedicine is defined as “providing remote healthcare services using information and communication technologies,” where the information and communication technologies have great potential to be utilized (Sood et al. 2007). According to recent studies on the application of telemedicine for the ED, these applications include providing specialized services to rural areas (Mohr et al. 2018; Ray et al. 2017; Ward et al. 2015; Zachrison et al. 2019), reducing ED overcrowding (Letvak and Rhew 2015; Rademacher et al. 2019; Sun et al. 2018; Tolia et al. 2017), providing specialized services to paramedics, better crisis management, and reducing the time between accidents and patients’ arrival at the hospital (Cho et al. 2015; Doggett et al. 2018; Kim and Falcone 2017).
However, many studies in this area indicate that further research is needed and that current evidence is inadequate (Ward et al. 2015; Brainard et al. 2016; Salmoiraghi and Hussain 2015; Kelton et al. 2018; Marsh-Feiley et al. 2018; Pak and Pak 2015; Rogers et al. 2017; Kimmel et al. 2019).
Considering the benefits and challenges of applying telemedicine technology in the ED, which were mentioned in many articles, the usability of these systems seems to be uncertain, which has given rise to serious questions regarding their implementation.
Numerous studies have investigated the use of telemedicine in the ED, and many reviews have attempted to determine the feasibility of these systems for emergency settings. However, the results of these studies in many cases tend to be in disagreement. Hence we aim to reach a conclusion by presenting an overview of the systematic reviews performed.
The objective of this study is to provide an overview of systematic reviews regarding the use of telemedicine in the ED. The primary questions to be addressed are as follows:
-
I.
Is telemedicine technology feasible for the ED?
-
II.
What are the benefits of the application of telemedicine in the ED?
-
III.
What challenges arise when using this technology in emergency settings?
Material and methods
Search strategy
To investigate the feasibility of telemedicine in the ED and to provide an overview of studies on this topic, a systematic search was carried out in databases including PubMed, Scopus, Web of Science, Cochrane library, and Google Scholar. In addition, to identify gray literature, we searched OpenGrey and OpenDOAR databases. Additionally, manual searches were performed by searching reference lists from the included studies. This review was conducted in accordance with the PRISMA protocol.
The review was conducted using a combination of MeSH and relevant terms “Systematic Review,” “Telemedicine,” and “Emergency.” The last search was performed on September 15, 2020. The search method for each database is as follows (Table 1):
Table 1.
Search strategy
| Database | Search Strategy | Count |
|---|---|---|
| PubMed | (("Telemedicine"[Title/Abstract] OR "Teleconsultation"[Title/Abstract] OR "Remote Consultation"[Title/Abstract] OR "Telehealth"[Title/Abstract] OR "eHealth"[Title/Abstract] OR "Telepathology"[Title/Abstract] OR "Teleradiology"[Title/Abstract] OR "Telerehabilitation"[Title/Abstract] OR "Mobile Health"[Title/Abstract] OR "mHealth"[Title/Abstract]) AND ("Emergency"[Title/Abstract] OR "Emergency Department"[Title/Abstract] OR "Emergency medicine"[Title/Abstract] OR "Emergency Information systems"[Title/Abstract])) AND ("Systematic Review"[Title/Abstract]) | 68 |
| Scopus | ( TITLE-ABS-KEY ( "Telemedicine" OR "Teleconsultation" OR "Remote Consultation" OR "Telehealth" OR "eHealth" OR "Telepathology" OR "Teleradiology" OR "Telerehabilitation" OR "Mobile Health" OR "mHealth" ) AND TITLE-ABS-KEY ( "Emergency" OR "Emergency Department" OR "Emergency medicine" OR "Emergency Information systems" ) AND TITLE-ABS-KEY ( "Systematic Review" ) ) | 179 |
| Web of Science | TOPIC: (“Telemedicine” OR “Teleconsultation” OR “Remote Consultation” OR “Telehealth” OR “eHealth” OR “Telepathology” OR “Teleradiology” OR “Telerehabilitation” OR “Mobile Health” OR “mHealth”) AND TOPIC: (“Emergency” OR “Emergency Department” OR “Emergency medicine” OR “Emergency Information systems”) AND TOPIC: ("Systematic Review") | 74 |
| Cochrane Library | “Telemedicine” OR “Teleconsultation” OR “Remote Consultation” OR “Telehealth” OR “eHealth” OR “Telepathology” OR “Teleradiology” OR “Telerehabilitation” OR “Mobile Health” OR “mHealth” in Title Abstract Keyword AND “Emergency” OR “Emergency Department” OR “Emergency medicine” OR “Emergency Information systems” in Title Abstract Keyword AND "Systematic Review" in Title Abstract Keyword - (Word variations have been searched) | 15 |
| Google Scholar | intitle:(“Telemedicine” OR “Teleconsultation” OR “Remote Consultation” OR “Telehealth”) AND intitle:(“Emergency” OR “Emergency Department”) AND intitle:"systematic review" | 478 |
Eligibility criteria
Inclusion criteria for the studies were as follows:
Published between 2015 and 2020: because we only wanted the modern and most recent evidence regarding the feasibility of this technology
Published in the English language
Papers that were systematic reviews: because of the disparities among the results of studies regarding the feasibility of these systems, we decided to provide an overview of the studies performed in recent years and reach a conclusion.
Exclusion criteria for the studies were as follows:
Not concentrated on the application of telemedicine in the ED.
Date extraction and synthesis
Data regarding research characteristics and results were independently extracted by two authors. A narrative review was then performed, and its findings are presented in a table.
Data items
Data items that were extracted from the articles include the following:
Research’s main finding
Main research question
Number of articles included in systematic review
The most recommended technology
Journal of publication
Publication year
Telemedicine method
Telemedicine application example in its respective field
Benefits of telemedicine implementation
Challenges to telemedicine implementation
Risk of bias assessment
Two reviewers independently evaluated the quality of papers using the ROBIS tool (version 1.2) (Whiting et al. 2016). In the case of disagreement, the final decision was made based on consensus.
Results
The findings of this study are presented in two main sections:
-
A.
The benefits of telemedicine in the ED
-
B.
Challenges posed by application of telemedicine in the ED
Before these two sections, we first present information on article journals, telemedicine technologies, and the impact on patient care.
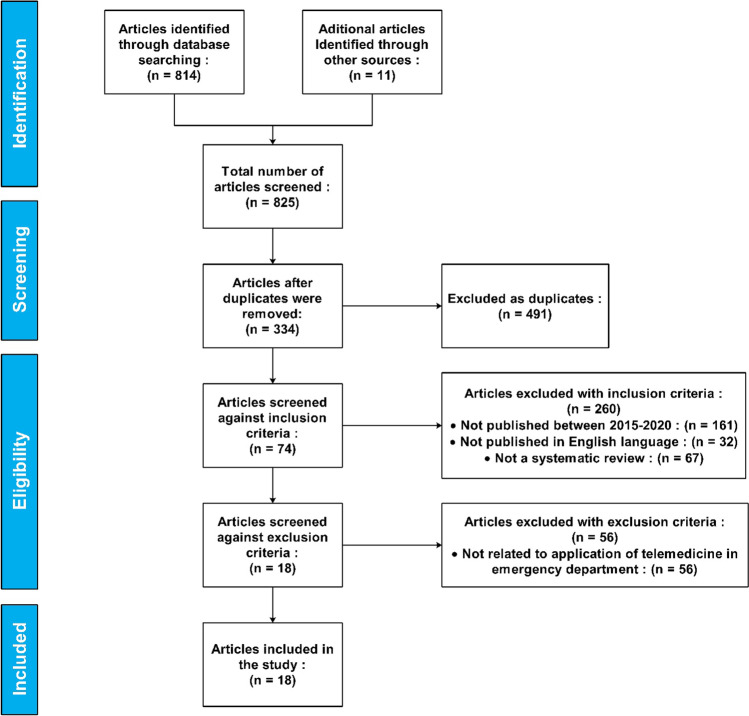
The initial search identified 825 articles. Of these, 491 articles were removed from the study as duplicates, leaving 334 papers to be screened against the inclusion criteria. After screening, 74 studies remained, of which 56 were removed by exclusion criteria. Finally, 18 articles were included in the study (Fig. 1).
Fig. 1.
PRISMA flow diagram
The year of publication for each of the included studies is presented in Fig. 2.
Fig. 2.
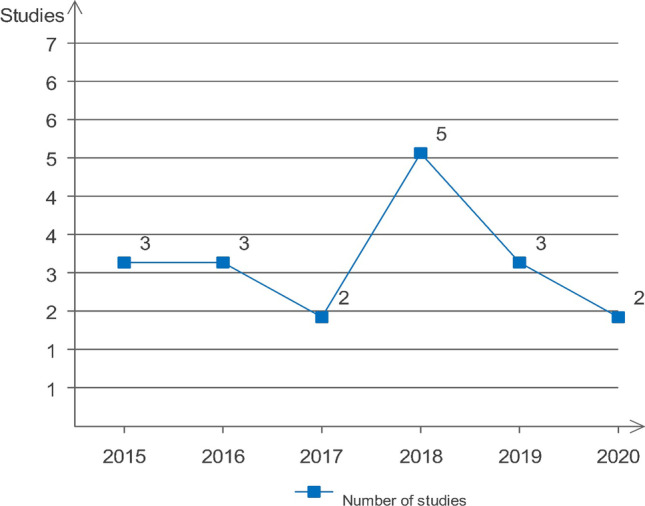
Publication year of articles included in the study
The journals with the highest number of articles were Telemedicine and e-Health (three articles) and Journal of Telemedicine and Telecare (two articles).
Technologies
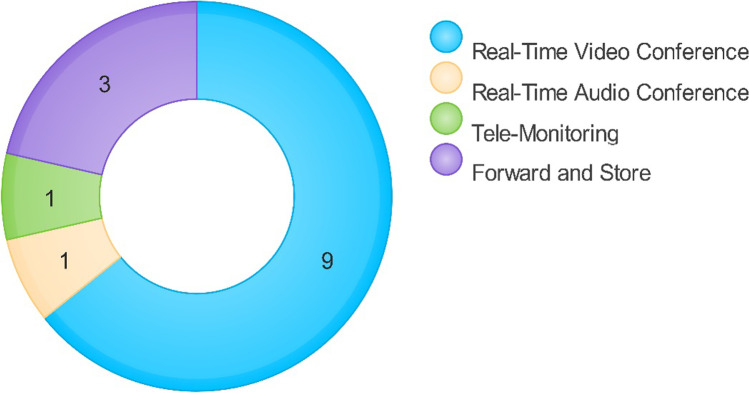
In most of the papers, one of the telemedicine technologies was chosen as the most feasible technology. Some articles pointed out that usability varied depending on the setting and the situation. For instance, in cardiovascular disease centers, the store and forward method, for supporting stroke patients before arriving at the hospital, and the video conference method (real-time video and audio) tended to be the best methods, and for primary care, consultation through real-time audio was found to be the best method (Winburn et al. 2018). In another review, it was established that the best and most cost-effective method was a combination of video conferencing and store and forward (Bashshur et al. 2016). In total, nine papers mentioned real-time video conferencing (du Toit et al. 2019; Eder et al. 2018; Gattu et al. 2016; Marsh-Feiley et al. 2018; Salmoiraghi and Hussain 2015; Ward et al. 2015; Winburn et al. 2018; Culmer et al. 2019; Nadar et al. 2018), three papers mentioned store and forward (Marsh-Feiley et al. 2018; Winburn et al. 2018; Lazarus et al. 2020), one paper discussed tele-monitoring (Kimmel et al. 2019), and one paper real-time audio conferencing (Winburn et al. 2018) as the most feasible technology, as presented in Fig. 3. Six papers did not mention anything concerning the issue (Brainard et al. 2016; Kelton et al. 2018; Pak and Pak 2015; Rogers et al. 2017; Guevorkian 2017; Boggan et al. 2020).
Fig. 3.
Most feasible technology
The benefits of telemedicine application in the ED
Table 2 provides a summary of the benefits reported in the included studies
Table 2.
Benefits of emergency department telemedicine
| Benefit | Source | Ratio |
|---|---|---|
| Cost reduction | (Brainard et al. 2016; Gattu et al. 2016; Kelton et al. 2018; Kimmel et al. 2019; Pak and Pak 2015; Rogers et al. 2017; Salmoiraghi and Hussain 2015; Culmer et al. 2019) | 8/18 |
| Improved quality of care | (Bashshur et al. 2016; Eder et al. 2018; Gattu et al. 2016; Kelton et al. 2018; Nadar et al. 2018; Culmer et al. 2019; Guevorkian 2017) | 7/18 |
| Decreased patient transfer rate from rural centers to major centers | (Brainard et al. 2016; du Toit et al. 2019; Kelton et al. 2018; Winburn et al. 2018; Nadar et al. 2018; Culmer et al. 2019) | 6/18 |
| Reduced mortality rate | (Eder et al. 2018; Kimmel et al. 2019; Guevorkian 2017; Nadar et al. 2018; Lazarus et al. 2020) | 5/18 |
| Reduced patient treatment time | (Kimmel et al. 2019; Rogers et al. 2017; Nadar et al. 2018; Lazarus et al. 2020; Culmer et al. 2019) | 5/18 |
| Reduced time between first contact and treatment | (Pak and Pak 2015; Rogers et al. 2017; Guevorkian 2017; Lazarus et al. 2020; Culmer et al. 2019) | 5/18 |
| Cost effectiveness | (Brainard et al. 2016; Kelton et al. 2018; Ward et al. 2015; Guevorkian 2017; Lazarus et al. 2020) | 5/18 |
| Medical staff practice and training | (Gattu et al. 2016; Kimmel et al. 2019; Marsh-Feiley et al. 2018; Lazarus et al. 2020) | 4/18 |
| Quick access to specialist | (Gattu et al. 2016; Marsh-Feiley et al. 2018; Salmoiraghi and Hussain 2015; Ward et al. 2015) | 4/18 |
| Reduced ED overcrowding | (Gattu et al. 2016; Kelton et al. 2018; Winburn et al. 2018) | 3/18 |
| improved capability of rural centers | (du Toit et al. 2019; Ward et al. 2015; Lazarus et al. 2020) | 3/18 |
| On-site diagnosis and prescription | (Eder et al. 2018; Rogers et al. 2017) | 2/18 |
| Reduced return visits for unnecessary cases | (Bashshur et al. 2016; Winburn et al. 2018) | 2/18 |
| Providing remote specialist care | (Salmoiraghi and Hussain 2015; Ward et al. 2015) | 2/18 |
| Preventing medication side effects and medical error | (Bashshur et al. 2016; Nadar et al. 2018) | 2/18 |
| Better management of emergency conditions | (Eder et al. 2018) | 1/18 |
As shown in the results above, telemedicine tends to be effective in many aspects through various approaches. For example, it can help to avoid unnecessary transfers from rural locations to central hospitals. Since the severity of the injury can be estimated using telemedicine consultation, not every potential patient transfer will need to take place (Rademacher et al. 2019). This consultation could vary from a 24-hour consulting nurse (Ray et al. 2017) to video evaluation, usually combined with radiology images (specifically in the diagnosis of minor fractures) (Cho et al. 2015). Furthermore, due to the high accuracy of telemedicine diagnosis either in an ambulance or on the scene, the patient’s treatment time also seems to be considerably shorter (Mohr et al. 2018).
Challenges posed by application of telemedicine in the emergency department
Although the benefits of telemedicine in EDs were demonstrated in every article included, its challenges, varying from technical and infrastructure issues (Brainard et al. 2016; Gattu et al. 2016; Pak and Pak 2015; Rogers et al. 2017; Culmer et al. 2019; Guevorkian 2017) to implementation costs (Rogers et al. 2017), remain. Addressing the challenges ahead for telemedicine programs to be applied most efficiently is just as vital as identifying its benefits that befit each center’s specific goals and needs. Accordingly, the table below outlines the possible challenges of implementing and applying telemedicine systems in the EDs, which are extracted from the included studies (Table 3).
Table 3.
Challenges of emergency department telemedicine
| Challenge | Source | Ratio |
|---|---|---|
| Technical issues and difficulties | (Brainard et al. 2016; Gattu et al. 2016; Pak and Pak 2015; Rogers et al. 2017; Guevorkian 2017; Culmer et al. 2019) | 6/18 |
| Legislative, ethical and policy issues | (Eder et al. 2018; Gattu et al. 2016; Marsh-Feiley et al. 2018; Salmoiraghi and Hussain 2015; Culmer et al. 2019) | 5/18 |
| Protecting patient privacy, confidentiality and security | (Gattu et al. 2016; Marsh-Feiley et al. 2018; Pak and Pak 2015) | 3/18 |
| Prolonged consultation time with telemedicine | (Gattu et al. 2016; Marsh-Feiley et al. 2018; Pak and Pak 2015) | 3/18 |
| Scarce and limited literature on technology implementation | (Kelton et al. 2018; Kimmel et al. 2019; Salmoiraghi and Hussain 2015) | 3/18 |
| Lack of cooperation from other departments | (Eder et al. 2018; Winburn et al. 2018) | 2/18 |
| Loss of skill in rural physician | (Kelton et al. 2018; Pak and Pak 2015) | 2/18 |
| Incompatible pre-existing health systems | (Kelton et al. 2018; Pak and Pak 2015) | 2/18 |
| Increased anxiety in hub physician | (Kelton et al. 2018; Pak and Pak 2015) | 2/18 |
| Possible loss of critical data | (Marsh-Feiley et al. 2018; Pak and Pak 2015) | 2/18 |
| Synchronizing the field of telemedicine and emergency care | (Bashshur et al. 2016; Pak and Pak 2015) | 2/18 |
| Increased workload in low staff areas | (du Toit et al. 2019; Boggan et al. 2020) | 2/18 |
| Lower inclination of rural residents for participation | (Brainard et al. 2016; Culmer et al. 2019) | 2/18 |
| Financial support | (Ward et al. 2015; Culmer et al. 2019) | 2/18 |
| Additional time needed for setting up equipment | (Pak and Pak 2015) | 1/18 |
| Disagreement between diagnosis and management between physician | (Pak and Pak 2015) | 1/18 |
| User support | (du Toit et al. 2019) | 1/18 |
| Difficulty of providing care in remote rural EDs | (du Toit et al. 2019) | 1/18 |
| Implementation costs | (Rogers et al. 2017) | 1/18 |
| Increased complexity of cases | (Ward et al. 2015) | 1/18 |
| Difficult system maintenance | (Kimmel et al. 2019) | 1/18 |
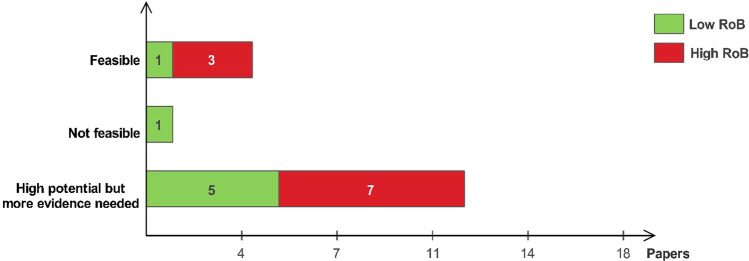
Feasibility
Overall, the use of telemedicine for emergency settings has shown much potential. Nevertheless, due to the weak study designs, most of the studies were unable to confirm the usability of telemedicine and concluded that further studies were required. Four papers suggested that ample evidence has demonstrated the feasibility and effectiveness of telemedicine in emergency care (Winburn et al. 2018; Brainard et al. 2016; Bashshur et al. 2016; Ward et al. 2015). However, three of these studies had a high risk of bias (RoB) (Ward et al. 2015; Winburn et al. 2018; Bashshur et al. 2016). Twelve papers found that despite the potential, further studies with better quality of evidence were still needed to confirm their findings and the feasibility of this technology (Eder et al. 2018; Rogers et al. 2017; Salmoiraghi and Hussain 2015; Kimmel et al. 2019; Kelton et al. 2018; Marsh-Feiley et al. 2018; Gattu et al. 2016; Pak and Pak 2015; Guevorkian 2017; Nadar et al. 2018; Lazarus et al. 2020; Culmer et al. 2019). Seven of these studies were determined to have a high RoB in their investigation (Rogers et al. 2017; Salmoiraghi and Hussain 2015; Kelton et al. 2018; Gattu et al. 2016; Pak and Pak 2015; Lazarus et al. 2020; Culmer et al. 2019). One paper, which had a low RoB, reported that limited evidence supported the feasibility of telemedicine; however, the paper’s main focus was on remote triage and not an overall assessment of all the methods involved (Boggan et al. 2020). Also, one paper did not report any outcome regarding feasibility and effectiveness (du Toit et al. 2019) (Fig. 4).
Fig. 4.
Feasibility and effectiveness
Table 4 presents the review results for each article included in the study. The application example column expands on telemedicine applications regarding the research field, and the findings column provides a brief summary of the studies’ main findings.
Table 4.
Data extracted from articles
| Reference | Research questions | Number of included articles | Method | Application | Findings |
|---|---|---|---|---|---|
| Eder et al. (2018) |
1- Which telemedicine services in acute trauma care are implemented, and what was the nature of intervention? 2- What are the reported effects of telemedicine on acute trauma care by EMS? 3- Which methodologies were used to produce knowledge about telemedicine in included studies? |
15 | Tele-consultation | Providing services using tele-consultation which a paramedic would not normally be able to do |
1- Tele-consultation and pre-notification systems have the most utilization for acute trauma care 2- Its application improves patient’s condition |
| Telemedical pre-notification | Hospital care team awareness of patient’s condition while transferring the patient | ||||
| Winburn et al. (2018) | What is the level of adoption, the format of delivery, and the clinical focus for telehealth in pre-hospital emergency care? | 68 | Tele-consultation | Providing pre-hospital counseling for stroke, cardiovascular disease, and trauma |
1- It is best to utilize forward and store for cardiovascular diseases 2- Tele-consultation is commonly used for stroke patient care |
| du Toit et al. (2019) |
1- How has telehealth been used to manage noncritical emergency presentations? 2- What were the telehealth program outcomes? |
15 | Tele-consultation | Linking a small rural ED to a major ED center and receiving services and tele-consultation from specialists there |
1- Tele-consultation systems tend to be more accepted in places where nurses are the main provider 2- Its acceptance seems low in places where doctors are the main provider |
| Rogers et al. (2017) | How is telemedicine implemented and what are its benefits and effects? | 23 | Tele-consultation | Providing tele-consultation for on-site and ambulance paramedics by a specialist physician | System implementation outcomes have been positive and beneficial |
| Brainard et al. (2016) | Which health service interventions reduce the unplanned use of healthcare by rural populations? | 33 | Tele-consultation | Utilizing skills and equipment of major centers in cities by rural EDs | The use of these systems is especially cost-effective in rural areas |
| Salmoiraghi and Hussain (2015) | What are the effects and qualities of tele-psychiatry in emergency settings? | 23 | Tele-consultation | Providing psychological counseling and management services in the case of emergency |
1- Tele-consultation improves accessibility 2- Cost reduction |
| Ward et al. (2015) | What is the impact of hospital-based telemedicine systems in emergency care settings? | 38 | Tele-consultation | Decision support for diagnosis and treatment |
1- Most studies have had positive and beneficial outcomes 2- Research design and statistic assessment of studies was not robust enough |
| Telepresence | The remote physician has the role of on-site physician | ||||
| Kimmel et al. (2019) | Which alert systems improve outcomes and which types of alerts are effective? | 10 | Telemedical notification | Integrating care plans with the electronic health record (EHR) and sending reminder to provider at the desired time |
1- Telemedical notification reduces costs 2- It improves resource consumption 3- The usability of telemedicine systems requires further research |
| Kelton et al. (2018) | – | 11 | Tele-consultation | Using less expensive care providers, e.g., a nurse, alongside a remote physician |
1- The highest rate of implementation of these systems is in countries with diffuse populations 2- The success of these systems seems to lie not in the specialized services provided but in the ability to support patients in need of urgent care who may not receive the necessary quality care in other ways |
| Marsh-Feiley et al. (2018) | Is tele-sonography feasible, diagnostically accurate, and clinically useful in emergency settings? | 28 | Tele-sonography | A nonspecialist sonographer connecting a specialist through the system, and either the examination is done in real time, or the pictures are taken and then sent to the specialist |
1- Tele-sonography is applicable to a wide range of situations 2- Asynchronous communication was the most accessible among the available methods |
| Bashshur et al. (2016) | What does the current evidence say about the feasibility, acceptance, and effect of telemedicine in primary care? | 86 | Tele-consultation | Consultation of two specialists or providing tele-consultation for chronic patients instead of referrals to the ED |
1- Tele-consultation is effective in primary care 2- It is acceptable for both patient and provider 3- It improves the quality of service 4- It reduces costs |
| Gattu et al. (2016) | – | Not stated | Tele-consultation | Linking two centers and providing consultation |
1- They are usable and reliable 2- Further investigation is required in the case of pediatric emergency care |
| Tele-monitoring | Real-time remote monitoring of the patient’s physiological status, including vital signs | ||||
| Pak and Pak (2015) |
Does telemedicine offer clinical benefits? Does telemedicine offer the same outcomes with reduced costs? |
7 | Tele-consultation | Provider surveillance, X-ray interpretation, and EKG transmission prior to patient transfer to the center |
1- No clinical benefits were observed 2- It was safe and satisfactory |
| Guevorkian (2017) | What potential does telemedicine have in pre-hospital care? | 15 | Tele-consultation | Augmenting the efforts of non-professional health workers in low-resource settings | Studies have shown promising results, but more robust studies are needed to confirm the findings |
| Nadar et al. (2018) | What is the effect of telemedicine on clinical outcomes in pediatric acute care? | 24 | Tele-consultation |
Assessing the patient in real time, checking clinical data and medical files, observing medical images and monitoring equipment, and providing a beneficial and helpful remote consultation |
The use of telemedicine showed positive impacts, but more studies are needed |
| Lazarus et al. (2020) | Is tele-stroke usable for acute stroke management in rural settings? | 15 | Tele-consultation (tele-stroke) | Providing treatment remotely to stroke victims in rural communities | Telemedicine showed promising results, but further studies are needed to confirm these findings |
| Boggan et al. (2020) | Is remote triage feasible and beneficial for acute settings? | 8 | Tele-consultation (remote triage) | Triaging patients to the appropriate level of care through the use of technological systems that facilitate remote decision-making | There is limited evidence supporting the feasibility of remote triage in acute settings |
| Culmer et al. (2019) | Is ambulance-based telemedicine effective? What is its effect on quality, cost, and satisfaction? | 13 | Tele-consultation |
Transmission of patient data from an ambulance to a hospital’s ED or physician |
1- Telemedicine is effective in reducing costs 2- Quality of care is as good or even better when using telemedicine 3- Increased efficiency when using telemedicine due to reduced number and time of travel and also time of care |
Risk of bias assessment
The included studies were evaluated using the ROBIS tool. This tool evaluates the quality of systematic reviews using four domains of questions: domain 1, study eligibility criteria; domain 2, identification and selection of studies; domain 3, data collection and study appraisal; and domain 4, synthesis and findings. In another phase, the tool then determines the risk of bias in the studies based on the answers to those questions (Table 5).
Table 5.
Risk of bias assessment
| Study | Domain 1 | Domain 2 | Domain 3 | Domain 4 | Risk of bias | FD | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | LoC | 1 | 2 | 3 | 4 | 5 | LoC | 1 | 2 | 3 | 4 | 5 | LoC | 1 | 2 | 3 | 4 | 5 | 6 | LoC | 1 | 2 | 3 | RoB | |||
| (Eder et al. 2018) | Evaluator 1 | Y | Y | Y | P-Y | P-Y | Low | Y | Y | Y | Y | Y | Low | P-Y | P-Y | Y | N | N-I | High | Y | P-Y | Y | Y | P-Y | N | UC | P-Y | Y | Y | Low | Low |
| Evaluator 2 | P-Y | P-Y | Y | P-N | P-Y | Low | Y | N-I | P-Y | Y | P-Y | Low | P-N | Y | P-Y | N | N-I | High | P-Y | P-Y | N-I | Y | P-Y | N | Low | P-Y | Y | P-Y | Low | ||
| (Winburn et al. 2018) | Evaluator 1 | Y | P-Y | P-Y | P-Y | P-Y | Low | P-Y | P-N | P-Y | P-N | P-Y | High | N-I | P-Y | P-Y | N | N | High | P-Y | Y | P-Y | Y | P-Y | N | UC | N | P-Y | Y | High | High |
| Evaluator 2 | P-Y | P-Y | P-N | P-Y | P-Y | Low | P-N | N | P-Y | P-N | N-I | High | N-I | P-Y | P-Y | N-I | N-I | UC | P-N | P-Y | N | Y | N-I | P-N | UC | P-N | P-Y | Y | High | ||
| (du Toit et al. 2019) | Evaluator 1 | Y | P-Y | Y | P-Y | P-Y | Low | Y | P-N | P-Y | N | P-Y | High | P-Y | Y | Y | N | N | High | Y | P-Y | P-Y | P-Y | Y | N | High | N | Y | P-Y | High | High |
| Evaluator 2 | P-Y | P-N | P-Y | P-N | P-N | High | P-Y | Y | P-Y | P-N | N-I | High | P-Y | P-Y | N-I | N | N | High | P-N | P-Y | P-Y | P-Y | N-I | N | High | N | P-Y | P-Y | High | ||
| (Rogers et al. 2017) | Evaluator 1 | N-I | P-Y | Y | P-Y | P-Y | Low | P-N | Y | P-Y | N | Y | High | Y | Y | Y | N | N | High | Y | P-Y | Y | Y | P-Y | N | High | N | P-Y | Y | High | High |
| Evaluator 2 | P-Y | P-Y | P-Y | P-Y | Y | Low | P-N | N-I | P-N | P-Y | Y | High | Y | P-Y | P-Y | N | N-I | UC | P-Y | P-Y | P-Y | Y | P-N | N-I | Low | P-Y | P-Y | P-Y | Low | ||
| (Brainard et al. 2016) | Evaluator 1 | Y | P-Y | Y | P-Y | P-Y | Low | Y | Y | Y | P-Y | P-Y | Low | N-I | P-Y | Y | Y | N-I | Low | Y | Y | Y | Y | P-Y | P-Y | Low | Y | Y | Y | Low | Low |
| Evaluator 2 | Y | P-Y | Y | Y | Y | Low | P-Y | Y | N-I | Y | P-Y | Low | P-Y | P-Y | P-Y | Y | P-Y | Low | P-Y | Y | P-Y | Y | N-I | P-N | Low | Y | P-Y | Y | Low | ||
| (Salmoiraghi and Hussain 2015) | Evaluator 1 | N-I | Y | P-Y | Y | Y | Low | Y | Y | P-Y | N | Y | High | N-I | P-N | Y | N | N | High | Y | P-Y | P-Y | Y | P-Y | N | High | N | Y | Y | High | High |
| Evaluator 2 | P-N | N-I | N | N-I | P-N | High | P-Y | P-Y | P-N | P-N | Y | High | N-I | P-N | P-N | N-I | N-I | High | N-I | N | P-N | N-I | N | N | High | N | P-N | P-N | High | ||
| (Ward et al. 2015) | Evaluator 1 | Y | P-Y | P-Y | Y | Y | Low | Y | N | P-Y | N | Y | High | Y | Y | Y | N | N | High | Y | P-Y | Y | Y | P-Y | N | High | N | Y | P-Y | High | High |
| Evaluator 2 | Y | P-Y | P-Y | Y | P-Y | Low | Y | N-I | P-Y | P-N | Y | High | N-I | P-Y | P-Y | N-I | N-I | UC | P-Y | Y | N-I | N-I | P-Y | N | High | P-N | P-Y | P-Y | High | ||
| (Kimmel et al. 2019) | Evaluator 1 | Y | Y | P-Y | P-Y | Y | Low | Y | P-Y | Y | Y | Y | Low | Y | Y | P-Y | Y | N-I | Low | Y | P-Y | Y | Y | P-Y | P-Y | Low | P-Y | P-Y | Y | Low | Low |
| Evaluator 2 | P-Y | P-Y | P-Y | P-N | Y | Low | Y | P-Y | N-I | P-Y | Y | Low | Y | P-Y | P-Y | Y | N-I | Low | P-N | P-Y | P-Y | Y | P-Y | P-Y | Low | P-Y | Y | P-Y | Low | ||
| (Kelton et al. 2018) | Evaluator 1 | Y | P-Y | Y | P-Y | Y | Low | Y | Y | Y | P-Y | Y | Low | N-I | Y | Y | N | N | High | Y | P-Y | Y | Y | P-Y | N | High | N | Y | Y | High | High |
| Evaluator 2 | Y | Y | P-Y | P-Y | P-Y | Low | Y | P-Y | P-Y | P-N | Y | Low | N-I | P-N | P-Y | N-I | N-I | UC | Y | N-I | P-N | N-I | N-I | N-I | UC | P-N | P-Y | P-Y | UC | ||
| (Marsh-Feiley et al. 2018) | Evaluator 1 | Y | Y | Y | P-Y | Y | Low | Y | Y | Y | Y | Y | Low | Y | P-Y | P-Y | Y | Y | Low | Y | Y | P-Y | Y | Y | Y | Low | P-Y | Y | Y | Low | Low |
| Evaluator 2 | Y | P-Y | Y | P-Y | P-Y | Low | Y | P-Y | P-Y | P-Y | P-Y | Low | N-I | P-Y | P-Y | Y | Y | Low | P-Y | Y | P-Y | P-Y | P-Y | P-Y | Low | Y | Y | P-Y | Low | ||
| (Bashshur et al. 2016) | Evaluator 1 | P-Y | P-Y | N | P-N | P-Y | High | N-I | N-I | N-I | N | N-I | High | N-I | P-Y | Y | N | N | High | P-Y | Y | P-Y | P-Y | Y | N | High | N | N-I | Y | High | High |
| Evaluator 2 | P-Y | P-N | P-N | P-N | N | High | N-I | N-I | N-I | P-N | N-I | High | N-I | N-I | P-N | N-I | N-I | High | P-Y | N-I | P-Y | N-I | N-I | N-I | UC | P-N | P-N | N-I | High | ||
| (Gattu et al. 2016) | Evaluator 1 | Y | Y | P-Y | N-I | P-Y | Low | N-I | N-I | N-I | P-Y | N-I | UC | N-I | P-Y | Y | N | N | High | P-Y | P-Y | P-Y | P-Y | N-I | N | High | N | P-Y | P-Y | High | High |
| Evaluator 2 | P-Y | Y | P-N | N-I | N-I | UC | N-I | N-I | N-I | N-I | N-I | UC | N-I | P-Y | N-I | N | N | High | P-Y | N-I | P-Y | P-N | N-I | N | High | N | P-Y | N-I | High | ||
| (Pak and Pak 2015) | Evaluator 1 | N-I | P-Y | Y | P-Y | P-Y | Low | Y | Y | Y | N | Y | High | Y | Y | Y | N | N | High | P-Y | P-Y | Y | P-Y | P-Y | N | High | N | P-Y | Y | High | High |
| Evaluator 2 | Y | P-Y | P-Y | P-Y | P-N | Low | Y | Y | P-Y | P-N | Y | Low | Y | P-Y | P-N | N-I | N-I | UC | P-N | N | P-Y | P-Y | P-Y | N-I | High | N | P-Y | P-Y | High | ||
| (Guevorkian 2017) | Evaluator 1 | N-I | P-Y | Y | P-Y | P-Y | Low | Y | P-Y | Y | P-Y | N | High | N | P-Y | Y | Y | N | High | Y | Y | P-Y | Y | P-Y | P-Y | Low | Y | P-Y | Y | Low | Low |
| Evaluator 2 | Y | P-Y | Y | P-Y | P-Y | Low | P-Y | P-Y | P-Y | P-Y | N | High | N | P-Y | P-Y | Y | N | High | P-Y | Y | P-Y | P-Y | P-Y | P-Y | Low | P-Y | P-Y | Y | Low | ||
| (Nadar et al. 2018) | Evaluator 1 | Y | P-Y | Y | P-Y | P-Y | Low | Y | Y | Y | P-Y | Y | Low | Y | P-Y | Y | Y | Y | Low | Y | Y | Y | Y | P-Y | Y | Low | P-Y | Y | P-Y | Low | Low |
| Evaluator 2 | Y | P-Y | Y | P-Y | P-N | Low | Y | Y | Y | P-Y | Y | Low | Y | P-Y | Y | P-Y | Y | Low | Y | P-Y | Y | Y | P-Y | Y | Low | Y | Y | P-Y | Low | ||
| (Lazarus et al. 2020) | Evaluator 1 | Y | Y | Y | P-Y | P-Y | Low | P-Y | Y | Y | N | N | High | N | Y | P-Y | Y | N | High | Y | Y | P-Y | Y | P-Y | Y | Low | N | P-Y | Y | High | High |
| Evaluator 2 | Y | Y | P-Y | P-Y | P-Y | Low | P-Y | Y | P-Y | P-N | P-N | High | N-I | P-Y | P-Y | Y | Y | Low | P-Y | Y | Y | Y | P-Y | Y | Low | P-N | P-Y | Y | UC | ||
| (Boggan et al. 2020) | Evaluator 1 | Y | P-Y | Y | P-Y | P-Y | Low | Y | P-Y | Y | P-Y | Y | Low | Y | Y | P-Y | Y | Y | Low | Y | P-Y | Y | P-Y | P-Y | P-Y | Low | Y | P-Y | P-Y | Low | Low |
| Evaluator 2 | P-Y | P-Y | P-Y | N-I | P-N | UC | P-Y | P-Y | Y | P-Y | Y | Low | Y | Y | P-Y | Y | Y | Low | P-Y | Y | Y | Y | P-Y | P-Y | Low | P-Y | P-Y | P-Y | Low | ||
| (Culmer et al. 2019) | Evaluator 1 | Y | P-Y | Y | P-Y | P-Y | Low | P-Y | N | P-Y | N | Y | High | Y | P-Y | Y | Y | N-I | Low | Y | P-Y | Y | Y | P-Y | P-Y | Low | N | P-Y | Y | High | High |
| Evaluator 2 | Y | P-Y | Y | P-Y | P-Y | Low | P-Y | N | P-N | N | Y | High | Y | Y | P-Y | Y | N-I | Low | P-Y | P-Y | Y | P-Y | P-Y | P-Y | Low | P-N | P-Y | Y | High | ||
LoC = level of concern, Y = yes , FD = final decision, UC = unclear, N-I = no information, RoB = risk of bias, N = no, P-Y = probably yes, P-N = probably no
Discussion
Overall, evidence indicates that although telemedicine in the ED is both practical and convenient, it presents its own challenges. Most of the studies concluded that despite the high potential of this technology, its feasibility is uncertain, and further research is needed (Eder et al. 2018; Kimmel et al. 2019; Rogers et al. 2017; Salmoiraghi and Hussain 2015; Kelton et al. 2018; Marsh-Feiley et al. 2018; Pak and Pak 2015; Gattu et al. 2016; Guevorkian 2017; Nadar et al. 2018; Lazarus et al. 2020; Culmer et al. 2019).
Most of the included reviews were published in Telemedicine and e-Health and the Journal of Telemedicine and Telecare (Bashshur et al. 2016; Kimmel et al. 2019; Rogers et al. 2017; Culmer et al. 2019; Winburn et al. 2018; du Toit et al. 2019). Most of the articles were also published in 2018, reflecting the recent interest of the researchers to this field (Eder et al. 2018; Kelton et al. 2018; Marsh-Feiley et al. 2018; Winburn et al. 2018; Nadar et al. 2018).
Real-time video conferencing was the most feasible technology used in this area, according to the studies (du Toit et al. 2019; Eder et al. 2018; Gattu et al. 2016; Marsh-Feiley et al. 2018; Salmoiraghi and Hussain 2015; Ward et al. 2015; Winburn et al. 2018; Nadar et al. 2018; Culmer et al. 2019). Although tele-monitoring has been investigated in previous years for emergency settings, it was mentioned the least in the included studies (Kimmel et al. 2019).
Many outcomes were reported as benefits of implementing such systems in the ED. Cost reduction (Brainard et al. 2016; Gattu et al. 2016; Kelton et al. 2018; Kimmel et al. 2019; Pak and Pak 2015; Rogers et al. 2017; Salmoiraghi and Hussain 2015), improved quality of care (Bashshur et al. 2016; Eder et al. 2018; Gattu et al. 2016; Kelton et al. 2018), decreased patient transfer rate (Brainard et al. 2016; du Toit et al. 2019; Kelton et al. 2018; Winburn et al. 2018), reduced mortality rate (Eder et al. 2018; Kimmel et al. 2019; Mong et al. 2019), and treatment time (Kimmel et al. 2019; Rogers et al. 2017) are only a few of these cases. Accordingly, implementing this technology can be beneficial for both organizations and patients, since it could greatly facilitate the management of chronic diseases that require consistent follow-ups to the hospital and especially the ED.
On the other hand, implementing this technology can have unwanted results and may pose some challenges to the organization and patients. Technical issues (Brainard et al. 2016; Gattu et al. 2016; Mong et al. 2019; Pak and Pak 2015; Rogers et al. 2017; Culmer et al. 2019; Guevorkian 2017), legislation, and ethical and policy issues (Eder et al. 2018; Gattu et al. 2016; Marsh-Feiley et al. 2018; Salmoiraghi and Hussain 2015; Culmer et al. 2019) tend to be the most commonly reported issues using this system. If using these systems delays service provision or endangers patients’ critical health information, they may think twice before using them.
This technology can be especially useful in rural areas where there is a shortage of specialist care and equipment. Remote consultation can improve access to specialist care, reduce mortality, and facilitate transfer from these areas to major hospitals, which itself can reduce costs and overcrowding. These systems have also shown high potential in trauma and stroke care. They can provide an opportunity to reduce severity and mortality, decrease response and treatment time, and provide specialist care on-site.
During the COVID-19 global pandemic, there has been a surge in the adoption of telemedicine worldwide as a means for remote delivery of non-urgent medical care (Bashshur et al. 2020; Vidal-Alaball et al. 2020). Increased practice of telemedicine has demonstrated that the infrastructure for widespread adoption of such technologies may have more availability than previously thought, mainly owing to the global adoption of smartphones (Bashshur et al. 2020; Vidal-Alaball et al. 2020). Many governments have temporarily ceased all restrictive regulations regarding telemedicine use, including licensing and reimbursement (Bashshur et al. 2020). However, security risks, confidentiality issues, and unauthorized access remain a major concern (Bashshur et al. 2020; Vidal-Alaball et al. 2020).
The demonstrated potential of telemedicine during the pandemic can lay the groundwork for further implementation of these technologies for managing chronic diseases such as diabetes, heart conditions, or asthma in routine clinical practice in the future (Portnoy et al. 2020; Vidal-Alaball et al. 2020).
Limitations
Our study had several limitations that might impact our investigation. Only English-language studies and those published between 2015 and 2020 were included in our review, since we wanted only the most recent and up-to-date evidence regarding the issue. Consequently, we did not include much of the early research on telemedicine use in EDs, especially that related to trauma. Hence, there were likely studies that should have been included and were not, and likewise also studies that were less relevant but were included. Another limitation of our study was that most of the papers included had a high RoB in their investigation. Hence, further research with higher quality of evidence is needed to reach a conclusion on the feasibility of telemedicine for emergency care.
Conclusion
The application of telemedicine for the ED still has a long way to go, and there are many unknown areas that have yet to be investigated. This review has highlighted the benefits and challenges faced while implementing and using telemedicine in the ED. The majority of reviews found evidence of cost reduction for both hospital and patient. For example, for chronic disease management, which requires constant follow-up, telemedicine can alleviate the issue by reducing the costs and overcrowding. Nevertheless, if the proper technical infrastructure is not available for these systems, the expected effectiveness cannot be realized, and may lead to reduced hospital productivity and even prolonged treatment time. Altogether, telemedicine for the ED has high potential to impact patient care; however, due to the low quality of studies and scarce clinical trials regarding the issue, its feasibility cannot be confirmed, and further studies with better quality of evidence are needed.
Future research suggestion
Future research should focus on providing better quality of evidence and more robust study designs. There is also a paucity of clinical trials regarding the implementation of telemedicine in EDs.
Glossary
- Real-time video & audio conference
Communications via an interactive conference between two or more participants at different sites, using computer networks or other telecommunication links to transmit audio, video, and data [1].
- Store and Forward
Store-and-forward telemedicine is also called “asynchronous telemedicine.” It is a method by which healthcare providers share patient medical information with a physician, radiologist, or specialist at another location. It is not unlike email, but it is done using a solution that has built-in, sophisticated security features to ensure patient confidentiality [2].
- Tele-monitoring
Transmission of patient vital and non-vital signs from patient site to the doctor. It is more suited for patients with chronic illnesses such as hypertension or diabetes [3].
- Telepresence
Feeling present in a remote but real environment through telecommunications in order to perform tasks [4].
- Tele-consultation
Synchronous or asynchronous consultation using information and communication technology to omit geographical and functional distance. Its goals are for diagnostics or treatment between two or more geographically separated health providers (for example, physicians or nurses) or between health providers and patients [5].
- Tele-psychiatry
The practice of delivering psychiatric care using communications technology as a remote linkage between health-care providers and patients. Enables the productive interaction for clinical assessment, diagnosis, medication management, and therapy [6].
- Tele-stroke
A network of audiovisual communication and computer systems providing the foundation for a collaborative, interprofessional care model focusing on acute stroke patients [7].
- Tele-sonography
Combination of the use of ultrasound with telemedicine, allows for off-site expert interpretation as a solution to the major disadvantage of ultrasound, namely the skill required to interpret images [8].
- 1.
LeRouge C, Garfield MJ, Hevner AR, editors. Quality attributes in telemedicine video conferencing. Proceedings of the 35th Annual Hawaii International Conference on System Sciences; 2002: IEEE.
- 2.
Houston MS, Myers JD, Levens SP, McEvoy MT, Smith SA, Khandheria BK, et al., editors. Clinical consultations using store-and-forward telemedicine technology. Mayo Clinic Proceedings; 1999: Elsevier.
- 3.
Omboni S, Ferrari R. The role of telemedicine in hypertension management: focus on blood pressure telemonitoring. Current hypertension reports. 2015;17(4):21.
- 4.
Draper JV, Kaber DB, Usher JM. Telepresence. Human factors. 1998;40(3):354-75.
- 5.
Deldar K, Bahaadinbeigy K, Tara SM. Teleconsultation and Clinical Decision Making: a Systematic Review. Acta Inform Med. 2016;24(4):286-92.
- 6.
Adaji A, Fortney J. Telepsychiatry in Integrated Care Settings. Focus (Am Psychiatr Publ). 2017;15(3):257-63.
- 7.
Demaerschalk BM, Berg J, Chong BW, Gross H, Nystrom K, Adeoye O, et al. American Telemedicine Association: Telestroke Guidelines. Telemed J E Health. 2017;23(5):376-89.
- 8.
Marsh-Feiley G, Eadie L, Wilson P. Telesonography in emergency medicine: A systematic review. PloS one. 2018;13(5):e0194840.
Author contributions
Leila Shahmordai prepared the study conception and design, reviewed the final manuscript, critically revised the paper, and approved the final version of manuscript. Material preparation, data collection, and analysis were performed by Ali Sharifi Kia and Mouna Rafizadeh. The first draft of the manuscript was written by Ali Sharifi Kia, and all authors commented on previous versions of the manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Availability of data and material
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted, and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Code availability
Not applicable
Declarations
Ethics approval
The authors declare that this review was completed in compliance with ethical standards.
Conflict of Interest
The authors have no relevant financial or nonfinancial interests to disclose.
Consent to participate
Not applicable
Consent for publication
Not applicable
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 Pandemic, Lessons for the Future. Telemed J E Health. 2020;26:571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR. The empirical foundations of telemedicine interventions in primary care. Telemed J E Health. 2016;22:342–375. doi: 10.1089/tmj.2016.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggan JC, Shoup JP, Whited JD, Van Voorhees E, Gordon AM, Rushton S, Lewinski AA, Tabriz AA, Adam S, Fulton J (2020) Effectiveness of acute care remote triage systems: a systematic review. J Gen Intern Med 1-10. 10.1007/s11606-019-05585-4 [DOI] [PMC free article] [PubMed]
- Brainard JS, Ford JA, Steel N, Jones AP. A systematic review of health service interventions to reduce use of unplanned health care in rural areas. J Eval Clin Pract. 2016;22:145–155. doi: 10.1111/jep.12470. [DOI] [PubMed] [Google Scholar]
- Cho SJ, Kwon IH, Jeong J. Application of telemedicine system to prehospital medical control. Healthc Inform Res. 2015;21:196–200. doi: 10.4258/hir.2015.21.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culmer N, Smith T, Stager C, Meyer H, Quick S, Grimm K (2019) Evaluation of the triple aim of medicine in prehospital telemedicine: A systematic literature review. J Telemed Telecare: 1357633X19853461. 10.1177/1357633X19853461 [DOI] [PubMed]
- Doggett S, Ragland DR, Felschundneff G (2018) Prehospital Response Time and Traumatic Injury—A Review. UC Berkeley: Safe Transportation Research & Education Center. https://escholarship.org/uc/item/8978m2pn
- du Toit M, Malau-Aduli B, Vangaveti V, Sabesan S, Ray RA (2019) Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: a systematic review. J Telemed Telecare 25: 3-16. 10.1177/1357633X17734239 [DOI] [PubMed]
- Eder PA, Reime B, Wurmb T, Kippnich U, Shammas L, Rashid A. Prehospital Telemedical Emergency Management of Severely Injured Trauma Patients. Methods Inf Med. 2018;57:231–242. doi: 10.1055/s-0039-1681089. [DOI] [PubMed] [Google Scholar]
- Gattu R, Teshome G, Lichenstein R. Telemedicine applications for the pediatric emergency medicine: a review of the current literature. Pediatr Emerg Care. 2016;32:123–130. doi: 10.1097/pec.0000000000000712. [DOI] [PubMed] [Google Scholar]
- Guevorkian M (2017) Is Prehospital Emergency Telemedicine Implementation Feasible In Non-Traditional EMS Settings: A Systematic Literature Review. University of Arizona. http://hdl.handle.net/10150/623626
- Kelton DK, Szulewski A, Howes D. Real-time video telemedicine applications in the emergency department: a scoping review of literature. CJEM. 2018;20:920–928. doi: 10.1017/cem.2017.382. [DOI] [PubMed] [Google Scholar]
- Kim PT, Falcone RA Jr (2017) The use of telemedicine in the care of the pediatric trauma patient. Semin Pediatr Surg 47-53. Elsevier. 10.1053/j.sempedsurg.2017.01.008 [DOI] [PubMed]
- Kimmel HJ, Brice YN, Trikalinos TA, Sarkar IN, Ranney ML. Real-Time Emergency Department Electronic Notifications Regarding High-Risk Patients: A Systematic Review. Telemed J E Health. 2019;25:604–618. doi: 10.1089/tmj.2018.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, G, Permana AF, Nugroho SW, Audrey J, Wijaya DN, Widyahening IS (2020) Telestroke strategies to enhance acute stroke management in rural settings: A systematic review and meta-analysis. Brain Behav e01787. 10.1002/brb3.1787 [DOI] [PMC free article] [PubMed]
- Letvak S, Rhew D (2015) Assuring quality health care in the emergency department. Healthcare (Basel) 3:726-32. 10.3390/healthcare3030726 [DOI] [PMC free article] [PubMed]
- Marsh-Feiley G, Eadie L, Wilson P. Telesonography in emergency medicine: A systematic review. PloS One. 2018;13:e0194840. doi: 10.1371/journal.pone.0194840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr NM, Priyanka Vakkalanka J, Harland KK, Bell A, Skow B, Shane DM, Ward MM. Telemedicine use decreases rural emergency department length of stay for transferred North Dakota trauma patients. Telemed J E Health. 2018;24:194–202. doi: 10.1089/tmj.2017.0083. [DOI] [PubMed] [Google Scholar]
- Mong R, Tiah L, Wong M, Tan C (2019) Improving telestroke treatment times through a quality improvement initiative in a Singapore emergency department. Singapore Med J 60:69. 10.11622/smedj.2018083 [DOI] [PMC free article] [PubMed]
- Nadar M, Jouvet P, Tucci M, Toledano B, Sicotte C (2018) Impact of synchronous telemedicine models on clinical outcomes in pediatric acute care settings: a systematic review. Pediatr Crit Care Med 19: e662-e71. 10.1097/PCC.0000000000001733 [DOI] [PubMed]
- Pak D, Pak K (2015) Effectiveness of telemedicine in acute/emergency care settings versus face to face patient care: A systematic literature review. J Med Internet Res 3: e14 (1-13)
- Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rademacher NJ, Cole G, Psoter KJ, Kelen G, Fan JWZ, Gordon D, Razzak J. Use of Telemedicine to Screen Patients in the Emergency Department: Matched Cohort Study Evaluating Efficiency and Patient Safety of Telemedicine. JMIR Med Inform. 2019;7:e11233. doi: 10.2196/11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray KN, Felmet KA, Hamilton MF, Kuza CC, Saladino RA, Schultz BR, Scott Watson R, Kahn JM. Clinician attitudes toward adoption of pediatric emergency telemedicine in rural hospitals. Pediatr Emerg Care. 2017;33:250–257. doi: 10.1097/PEC.0000000000000583. [DOI] [PubMed] [Google Scholar]
- Rogers H, Madathil KC, Agnisarman S, Narasimha S, Ashok A, Nair A, Welch BM, McElligott JT. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemed J E Health. 2017;23:707–717. doi: 10.1089/tmj.2016.0248. [DOI] [PubMed] [Google Scholar]
- Salmoiraghi A, Hussain S. A systematic review of the use of telepsychiatry in acute settings. J Psychiatr Pract. 2015;21:389–393. doi: 10.1097/PRA.0000000000000103. [DOI] [PubMed] [Google Scholar]
- Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, Merrell RC. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health. 2007;13:573–590. doi: 10.1089/tmj.2006.0073. [DOI] [PubMed] [Google Scholar]
- Sun S, Lu SF, Rui H (2018) Does Telemedicine Improve Operational Efficiency? Evidence from New York Emergency Departments
- Vaishal T, Castillo E, Guss D (2017) EDTITRATE (emergency department telemedicine initiative to rapidly accommodate in times of emergency). J Telemed Telecare 23: 484-88. 10.1177/1357633X16648535 [DOI] [PubMed]
- Trzeciak S, Rivers EP (2003) Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J 20: 402-05. 10.1136/emj.20.5.402 [DOI] [PMC free article] [PubMed]
- Vidal-Alaball J, Acosta-Roja R, Hernández NP, Luque US, Morrison D, Pérez SN, Perez-Llano J, Vèrges AS, Seguí FL. Telemedicine in the face of the COVID-19 pandemic. Aten Primaria. 2020;52:418–422. doi: 10.1016/j.aprim.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward MM, Jaana M, Natafgi N. Systematic review of telemedicine applications in emergency rooms. Int J Med Inform. 2015;84:601–616. doi: 10.1016/j.ijmedinf.2015.05.009. [DOI] [PubMed] [Google Scholar]
- Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–234. doi: 10.1016/j.jclinepi.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitten PS, Mair FS, Haycox A, May CR, Williams TL, Hellmich S. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ. 2002;324:1434–1437. doi: 10.1136/bmj.324.7351.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winburn AS, Brixey JJ, Langabeer J 2nd, Champagne-Langabeer T (2018) A systematic review of prehospital telehealth utilization. J Telemed Telecare 24: 473-81. 10.1177%2F1357633X17713140 [DOI] [PubMed]
- Zachrison KS, Boggs KM, Hayden EM, Espinola JA, Camargo Jr CA (2019) Understanding Barriers to Telemedicine Implementation in Rural Emergency Departments. Ann Emerg Med. 10.1016/j.annemergmed.2019.06.026 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted, and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Not applicable