Abstract
PURPOSE:
Emergency cancer care constitutes a significant health care and patient burden. The purpose of this study was to identify characteristics of patients most fitting for treatment in an oncology-dedicated emergency department (OED).
METHODS:
Electronic files of patients with cancer seeking emergency services between April and June 2017 were retrospectively obtained from the hospital registry. Efficacy parameters were compared between patients treated in the OED and those treated in the general emergency department (GED). Using descriptive statistics and logistic regressions, patient- and treatment-related factors were correlated with effective care in the OED.
RESULTS:
More than half of the total 799 patients presented initially to the OED, of which 10.4% required GED referral. Treatment in the GED was associated with a higher rate of consultations, imaging, and hospitalization (P < .001), with the cost of imaging alone four times that of the OED ($23,263 US dollars difference). The relative proportion of patients with cancer visiting the GED was reduced after founding the OED. In the OED, patient diagnoses included lung (33%), GI, and breast cancer, of which 85% were metastatic. Frequent chief complaints were pain (45%), GI, malaise, and respiratory symptoms. Referral to the GED was significant in those with genitourinary cancer, back pain (P < .001), and neurologic symptoms, on biologic therapy, and with suspected oncological emergencies; conversely, disease symptoms (30% admissions) were well-controlled in the OED (P = .003).
CONCLUSION:
Using minimal resources, the OED provides efficacious, cancer-focused care, suitable for the majority of acute admissions. Careful triage is recommended, as high-risk patients should be referred to the GED, where advanced multidisciplinary management is more readily available.
BACKGROUND
Patients with cancer face unique disease and treatment-related complications that prompt frequent visits to the emergency department (ED), constituting a significant patient and health care burden. Their utilization of emergency services exceeds that of the general population,1 they consume more resources in the ED,2 and more than half of their visits result in hospital admission, in contrast to 12.5% in noncancer patients.3 General emergency departments (GEDs) tend to be overcrowded and fast-paced, attending to large and heterogeneous populations, and emergency physicians often lack expertise in caring for complex cancer patients or knowledge of the rapidly evolving treatment landscape. This may hamper the administration of quality cancer-focused care and potentially lead to superfluous and costly evaluations. Emergency management of patients with cancer by general physicians, rather than oncologists, has been associated with delayed diagnoses, complications, and worse outcomes.4 Various models for cancer-specific emergency services are developing worldwide, designed to provide apt and efficient treatment. With predetermined opening hours, admission criteria, and staff specialization, these services range from EDs at large, dedicated cancer centers to cancer emergency units integrated within GEDs, to cancer EDs that function alongside the GED and share resources.5
In Rambam Medical Center, a pilot oncology-dedicated ED (OED) was created within the clinic to provide a more intimate setting for patients with cancer in need of urgent care. Rambam Medical Center is a large tertiary referral center for 12 district hospitals, serving approximately 20% of the total population of Israel, and patients with cancer have direct access to inpatient, outpatient, and emergency services covered by national health care. Patients presenting during clinic hours visit the OED pending an available bed; when the OED is closed, they visit the main GED, where an oncology consult can be obtained if needed. Located within the oncology day care unit, the OED contains 10-15 beds reserved for emergency patients, alongside those receiving intravenous therapy. Open during weekday morning hours (9 am until last bed or 12 pm), the OED is staffed with an oncologist and designated nurse. Because of physical proximity, acquaintance of staff, and integration of the clinic and day care, the oncologist may request consultation with radiation oncology, neuro-oncology, or palliative medicine, as well as an oncology-dedicated social worker, complementary medicine practitioner, or spiritual care counselor. External consultations are requested in a similar manner to the GED. Resources are shared with the day care, including drug and fluid administration, laboratory tests, and imaging in the general hospital. After treatment, patients are discharged, hospitalized in the oncology inpatient department, or referred to the GED for more advanced evaluation and care, usually after their specific care team is notified of their condition.
In this work, the unique and integrative nature of the OED is presented as an effective alternative to the GED during morning hours, providing cancer-focused care in a familiar environment and potentially reducing substantial burden from the GED and costs for the institution.
METHODS
Patients
Retrospective electronic medical record review was performed for all patients admitted to the GED and OED during the 3-month period between April 2017 and June 2017. Data for the GED were obtained only for days the OED was open, to establish similar groups and exclude confounders in weekend or holiday visits. During open hours, patients attended the OED without selection or triage until the last bed was filled and thereafter were referred to the GED. Patients could attend the GED at any hour and needed to have a documented oncology consult.
Full patient data were obtained from a representative cohort or the first 91 consecutive patients who met study inclusion criteria during the month of June. Patients referred to the GED from the OED remained in the OED group for evaluation of the sample population, but their transfer was taken into account for statistical analysis. Patients with hematologic malignancies were excluded since they are treated in a separate department. This study was approved by the Institutional Review Board and granted a waiver for obtaining patient consent because of its retrospective design. The study was approved by the institutional Independent Ethics Committee, registered as 0465-17-RMB.
Parameters
Baseline patient and cancer characteristics, workup in the ED (imaging and consultations), and disposition (hospitalization, discharge, and referral) were recorded. Full analysis of the representative cohort was performed on a case-by-case basis by an oncologist and not generated in an automated manner, to retroactively determine chief complaint and admission type using classifications created by the investigators. Patients could be allotted more than one chief complaint but only one admission type. Those admitted more than once were analyzed as distinct cases (Appendix Table A1, online only).
Data Analysis
Descriptive statistics and logistic regressions were performed. Statistical analysis was carried out using the χ2 test for nominal data, Mann-Whitney test for the medians of nonparametric data, and Student’s t test for the parametric data. All reported P values are two tailed, with P values < .05 considered statistically significant.
RESULTS
Comparison of Two Groups: Fully Treated in OED vs GED
This full cohort included 799 patients treated in either OED or GED on the 53 days that the OED was open. Sixty percent, or 479 patients, presented initially to the OED, and of these, 50 patients, or 10.4%, were subsequently referred to the GED, hence deemed unfit for the OED. In total, 429 patients (54%) received full treatment in the OED, from presentation until discharge or hospitalization, whereas the remaining 370 patients (46%) were treated in the GED, either as an initial admission or referral from the OED (Tables 1 and 2).
TABLE 1.
OED, GED Patient, and Efficacy Evaluation
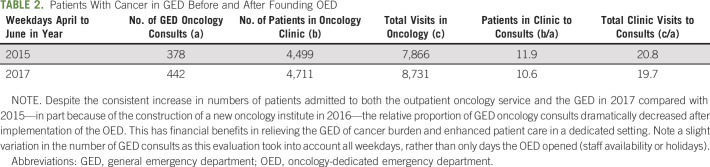
TABLE 2.
Patients With Cancer in GED Before and After Founding OED
The two groups of patients were equally matched in terms of demographics. However, those treated in the GED consumed more resources than those in the OED. Nononcologist physicians were more likely to be consulted from the GED (88% of the time or 327 of 370) than from the OED (11% or 48 of 429) (P < .001). The GED also used more imaging modalities, such as ultrasound in 9% versus 5% of patients in the GED and OED, respectively (P = .03); computed tomography scan in 28% versus 3% (P < .001); and x-ray in 43% versus 16% (P < .001). Using pricings from 2017, this translated into a $23,263 US dollars (USD) difference, making imaging in the GED four times more costly. For those with available data, more patients in the GED group were hospitalized compared with the OED group (88% v 16% P < .001).
Patient admission was compared with 2015, before founding the OED. Despite the consistent increase in numbers of patients admitted to both the outpatient oncology service and the GED—in part because of the construction of a new oncology institute in 2016—the relative proportion of GED oncology consults dramatically decreased after implementation of the OED. This has financial benefits in relieving the GED of cancer burden and enhanced patient care in a dedicated setting.
Who Presented to OED: Characteristics of Sample 91 Patients
Full data were obtained from the first consecutive 91 patients who were admitted to the OED during the month of June. Of these, 29 (32%) were found unfit for the OED and referred for further evaluation in the GED. Fifteen patients were hospitalized, and the remaining 47 were discharged from the OED.
Demographics.
Patient age ranged from 24 to 85, whereas 65% of patients were at least 60 years old. Nearly two thirds of patients were male. Most patients had lung cancer (33%), followed by GI (30%), breast (11%), and genitourinary (10%) cancers. The majority (85%) of patients had metastatic disease, and more than half of patients (59%) were on chemotherapy. Additional treatment modalities included immunotherapy (16%) and other biologic therapy including hormonal treatment (16%).
Chief complaint.
Pain was the most common chief complaint (45%); of these, 82% reported abdominal pain. Ten patients or 26% suffered from back pain. GI symptoms were also common (33%), as were malaise (18%) and respiratory complaints (15%). Other presenting problems included neurologic (11%) and dermatologic (10%) symptoms.
Admission type.
The most frequent type of emergency admission was for the management of disease symptoms (30% of patients). Treatment of side effects was second most common (18%), thereafter oncological emergencies (15%), nononcology-related problems (13%), infection (10%) and finally, for the purpose of medical procedures, namely, paracentesis of malignant ascites (7%).
Who Was Found Unfit for OED: 22 Patients Referred to GED
Basic demographic parameters did not differ between patients treated fully in the OED and those referred to the GED. Despite the small sample size, certain parameters were significantly associated with a referral to the GED (Fig 1). The presence of genitourinary cancer (56% referred; P = .031; 95% CI, 1.2 to 19.8) and treatment with biologic nonimmune therapy (64%; P < .001; 95% CI, 2.9 to 36) were each independently associated with a referral to the GED. Referral on biologic treatment was more likely than other treatment with an odds ratio of 10.15. No significant correlations were found for other cancer types: patients with lung cancer received full care in the OED in 73% of cases, GI cancer in 74%, and breast cancer in 80%. All 15 patients with other malignancies (melanoma, sarcoma, CNS, head-and-neck, and unknown primary) were fully treated in the OED.
FIG 1.
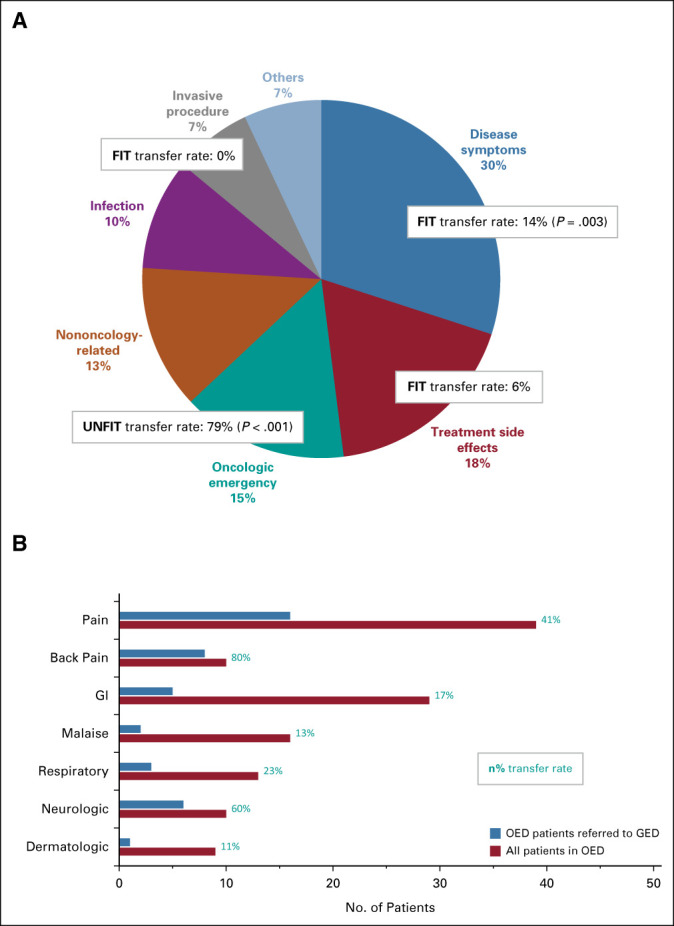
GED transfer rate by admission type and chief complaint. (A) Admission type: Of 91 patients who attended the OED, most were admitted for treatment of disease symptoms. Disease symptoms, treatment side effects, and invasive procedures were successfully treated in the OED; oncological emergencies were consistently referred to the GED. Significant parameters are marked with a P value. (B) Chief complaint: Red bars signify the number of patients with symptom in the OED, of representative 91 patients. Blue bars signify the number of patients with corresponding symptom who failed to complete treatment in the OED and required referral to the GED. The resulting ratio defines the referral rate for each symptom, marked to the right of the bars. GED, general emergency department; OED, oncology-dedicated emergency department.
Compared with those with other presenting symptoms, patients with back pain were most frequently unfit for the OED and sent for continuous care in the GED 80% of the time (P < .001; 95% CI, 3.7 to 100). Neurologic symptoms also led to referral (60%; P = .010; 95% CI, 1.6 to 24.8). Malaise was managed in the OED alone in 87% of cases, GI complaints in 83%, and respiratory symptoms in 77%. One patient of nine with dermatologic symptoms was referred to the GED.
When categorized by admission type, disease symptoms were fully treated in the oncology setting in 86% (P = .003). A similar trend was observed for the treatment of side effects and paracentesis, which were almost always managed in the OED alone (94% and 100%, respectively); however, because of small sample size, these were not statistically significant. Conversely, oncological emergencies were most frequently referred to the GED (79%; P < .001; 95% CI, 4.2 to 116), with an odds ratio of 22.
DISCUSSION
With tremendous progress attained in cancer diagnosis and treatment, patients live longer on diverse therapeutic modalities, and care teams are tasked with novel challenges in the acute setting. In this retrospective evaluation, although open for only a few morning hours, the OED fully managed more than half of all emergency admissions to the hospital, while using fewer costly resources alongside a higher discharge rate, as compared with the 24-hour GED. International studies have shown that acute care of patients with cancer should be guided by specialists and not GED physicians, to improve patient experience and safety, coordinate teams, and drive efficiency.4 Physicians from Korea described how the initiation of a cancer ED resulted in significantly reduced hospitalization rates (42% v 85.5%; P < .001) and cost per patient ($646 v $725 USD; P < .001), as compared with data obtained from the same hospital before founding the cancer ED.6 A regional study in the United States that obtained registry data from 2011 to 2015 found that more than a quarter of ED costs or $1,134,254 USD were potentially preventable by better symptom management.7
Patient profiles in the OED resembled those of previously described patients with cancer in emergency settings. Patients were slightly older, more male, and with more advanced disease than historical comparators, where the mean age was 58, 59% male, and 65% metastatic.8 The GED cohort was more consistent with the literature, suggesting an inherent patient selection in the OED toward those with poorer prognoses. Common diagnoses were ranked identically as lung, GI, and breast cancer,8 despite common diagnoses nationally being prostate cancer for men and breast cancer for women.9 Pain remains a dominant presenting symptom among patients with cancer, reinforcing the need for specialized care by an experienced caregiver.2,10 Previous investigations also ranked respiratory symptoms fourth,11 associated with poor prognoses.8,12 Fever ranked lower.10 Although other works described patients heavily treated with chemotherapy (more than 90%),6 the current study cohort was more often on immunotherapy and targeted agents, of these who were most admitted for adverse events and none with cancer symptoms—highlighting the relevance of the results in the present oncological landscape. When categorized by admission type, management of disease symptoms or progressive disease prevailed (42%) followed by treatment side effects (20%).8 True emergencies and nononcologic problems seem to be less frequent. Taken together, the majority of patients presenting for emergency management benefit from superior care by a dedicated oncological team, with experience in pain and disease symptom management, as well as up-to-date knowledge of adverse effects of new biologic agents, and where appropriate treatment can be initiated immediately.
The 10% GED referral rate of those unfit for services provided in the OED indicates that careful patient triage can enhance OED efficacy. A higher level of suspicion should be given to patients with prone underlying malignancies or symptomology. Genitourinary cancer, biologic nonimmune therapy, back pain, neurologic symptoms, and oncologic emergencies were parameters associated with higher referral rates. Often associated with impending emergent situations, such as spinal cord compression syndrome, symptomatic brain metastases, or superior vena cava syndrome, these require multidisciplinary evaluation and the expertise of specialists, such as a neurosurgeon and orthopedic surgeon, as well as timely imaging procedures, all of which are more available in the GED. An attempt to manage patients presenting with high-risk characteristics in the OED may be unfavorable, prolonging time to treatment initiation. Therefore, careful triage is key in any oncology-dedicated service and effective communication with the GED.
This study has various limitations. As a single center with limited sample size, the results might not be generalized. However, electronic medical records were reviewed individually and not automatically to ensure accuracy of data and account for multiple possible diagnoses and complaints. Logistic regressions were performed on a limited number of outcomes, which, however, significantly and logically define a specific subpopulation of patients who benefit from such an acute care setting. The main comparison is matched for general patient characteristics but not cancer- or admission-related parameters because of the manner in which information is recorded in database. The efficacy analysis is confounded by patient selection bias, as cases managed in the GED may be more complex that those in the OED, because of type or time of presentation (10% referred); however, the dramatic differences in resource utilization appear far greater than those accounted for by this alone and at least suggest that the OED relieved significant burden from the GED. A nationwide analysis found that patients with cancer attend emergency services more often during business hours and on weekdays and are more likely to be hospitalized during these times.2
The OED described in the present work is unique because of its integrative nature. It does not require separate facilities or equipment, but rather is created within the ongoing dynamic of a cancer clinic. Big or small, any cancer center can adapt this concept into daily practice, by designating a nurse and physician, who can rotate on a daily basis, and admit patients according to space and personnel availability. Paramedical professionals working in the day care can incorporate emergency patients. On busy days with high occupancy, or when staff is limited, the OED can treat a handful of patients or none at all; on days with less activity, the OED can attend to larger quantities. The results of this study highlight the importance of effective patient triage. When admitted according to criteria and pending OED availability, with effective cooperation with a GED that is close by or in the same institution, patients, caregivers, and the health care system as a whole benefit from quality and efficacious urgent cancer care.
We propose a prospective model for cooperation between emergency settings, designed to streamline patient care (Fig 2). Trained nurses in both the OED and the GED perform patient triage on the basis of predetermined admission criteria. Admission to the OED will be preferred for patients with general disease symptoms such as malaise, treatment side effects, or those in need of procedures like paracentesis. Admission to the GED will be preferred for those with suspected oncologic emergencies such those presenting with back pain or neurologic symptoms. We predict that effective patient sorting will lead to reduced resource consumption and enhanced patient outcomes.
FIG 2.
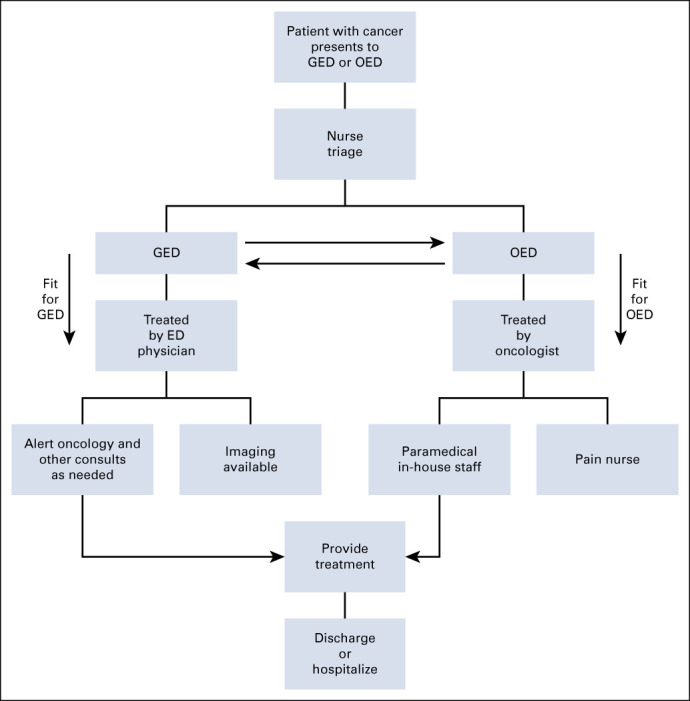
Proposed model to streamline patient admission. Trained nurses will perform triage. Patients with genitourinary cancer, back pain, neurologic symptoms, on biologic treatment, and those with suspected oncological emergencies will be considered high risk. Those with symptoms of cancer, known treatment side effects or in need of a basic procedure, will be directed to the OED. ED, emergency department; GED, general emergency department; OED, oncology-dedicated emergency department.
Appendix
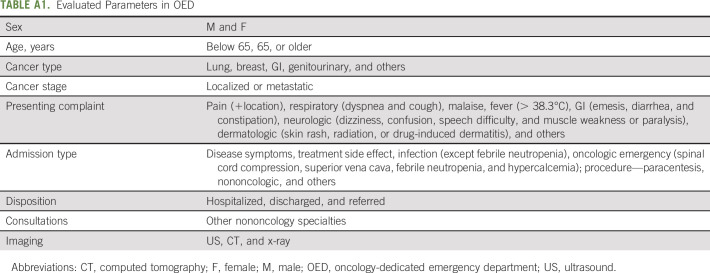
TABLE A1.
Evaluated Parameters in OED
Gil Bar-Sela
Honoraria: BMS, MSD Oncology, Novartis, Sanofi
No other potential conflicts of interest were reported.
SUPPORT
Supported by a resident grant by the Friends of Rambam organization awarded for this project, which was used only for statistical analysis of data.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Effective Patient Selection for an Oncology-Dedicated Emergency Service: A Retrospective Study
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Gil Bar-Sela
Honoraria: BMS, MSD Oncology, Novartis, Sanofi
No other potential conflicts of interest were reported.
REFERENCES
- 1.Lash RS, Bell JF, Reed SC, et al. : A systematic review of emergency department use among cancer Patients. Cancer Nurs 40:135-144, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang Z, Yang R, Kwak MJ, et al. : Oncologic emergencies in a cancer center emergency department and in general emergency departments countywide and nationwide. PLoS One 13:e0191658, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niska R, Bhuiya F, Xu J: National hospital ambulatory medical care survey: 2007 emergency department summary. Natl Cent Health Stat 1:32, 2010 [PubMed] [Google Scholar]
- 4.Young A, Marshall E, Krzyzanowska M, et al. : Responding to acute care needs of patients with cancer: Recent trends across continents. Oncologist 21:301-307, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rice TW, Klotz A, Neville-Webbe HL, et al. : Models of care for cancer emergencies, in: Todd KH, Thomas CRJ. (eds): Oncologic Emergency Medicine: Principles and Practice. Cham, Switzerland, Springer International, 2016, pp 3-12 [Google Scholar]
- 6.Ahn S, Lee YS, Lim KS, et al. : Emergency department cancer unit and management of oncologic emergencies: Experience in Asan Medical Center. Support Care Cancer 20:2205-2210, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Panattoni L, Fedorenko CR, Kreizenbeck KL, et al. : Costs of potentially preventable emergency department use during cancer treatment: A regional study. J Clin Oncol 35, 2017. (suppl; abstr 2) [Google Scholar]
- 8.Muallaoglu S, Karagün O, Mertsoylu H, et al. : Attributes of cancer patients admitted to the emergency department in one year. World J Emerg Med 5:85-90, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Agency for Research on Cancer: https://gco.iarc.fr/today/data/factsheets/populations/376-israel-fact-sheets.pdf
- 10.Mayer D, Travers D, Wyss A, et al. : Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 29:2683-2688, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Escalante CP, Martin CG, Elting LS, et al. : Dyspnea in cancer patients: Etiology, resource utilization, and survival—Implications in a managed care world. Cancer 78:1314-1319, 1996 [DOI] [PubMed] [Google Scholar]
- 12.Geraci JM, Tsang W, Valdres RV, et al. : Progressive disease in patients with cancer presenting to an emergency room with acute symptoms predicts short-term mortality. Support Care Cancer 14:1038-1045, 2006 [DOI] [PubMed] [Google Scholar]