Abstract
The CARLA study (Cardiovascular Disease, Living and Ageing in Halle) is a longitudinal population-based cohort study of the general population of the city of Halle (Saale), Germany. The primary aim of the cohort was to investigate risk factors for cardiovascular diseases based on comprehensive cardiological phenotyping of study participants and was extended to study factors associated with healthy ageing. In total, 1779 probands (812 women and 967 men, aged 45–83 years) were examined at baseline (2002–2005), with a first and second follow-up performed 4 and 8 years later. The response proportion at baseline was 64.1% and the reparticipation proportion for the first and second follow-up was 86% and 77% respectively. Sixty-four percent of the study participants were in retirement while 25% were full- or partially-employed and 11% were unemployed at the time of the baseline examination. The currently running third follow-up focuses on the assessment of physical and mental health, with an intensive 4 h examination program, including measurement of cardiovascular, neurocognitive, balance and gait parameters. The data collected in the CARLA Study resulted in answering various research questions in over 80 publications, of which two thirds were pooled analyses with other similar population-based studies. Due to the extensiveness of information on risk factors, subclinical conditions and evident diseases, the biobanking concept for the biosamples, the cohort representativeness of an elderly population, and the high level of quality assurance, the CARLA cohort offers a unique platform for further research on important indicators for healthy ageing.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10654-021-00824-7.
Keywords: Population-based cohort study, Elderly population, Cardiovascular diseases, Healthy ageing
Background
Cardiovascular diseases (CVDs) have long been considered the leading cause of death in Germany accounting for 37.4% of total deaths in 2018 [1]. In 2000, 10 years after the reunification of Germany, mortality from cardiovascular disease was still about 50% higher in East compared with West Germany [2]. Compared with other federal states in both former West and East Germany, Saxony-Anhalt has the highest cardiovascular disease morbidity and mortality from reunification until today [3]. The population of Saxony-Anhalt is in average older and shows higher rates of cardiovascular risk factors than those of the other German federal states [4]. In a study investigating regional differences in Germany with respect to life-time prevalence of major cardiovascular disease, Saxony-Anhalt was the most unfavorable state [5]. The Cardiovascular Risk Factors, Living and Ageing in Halle (CARLA) Study, a longitudinal population-based cohort study, was designed to address this gap by collecting detailed data on CVD risk factors and follow-up information on CVD morbidity and mortality in a region of eastern Germany characterized by a particularly pronounced CVD mortality. After the baseline examination, two additional follow-up examinations were performed, with a third follow-up currently taking place. Over time, the CARLA study evolved toward a broader research platform on ageing. Understanding the lifecourse trajectories pursued by an elderly population while maintaining an acceptable level of well-being and functionality could establish a useful route to recognize and plan good preventive approaches [6]. The aim of this article is to provide an overview of the CARLA study, and the main results obtained thus far. Additionally, we provide details on the current third follow-up examination of study participants.
Study design and methodology
Study population and recruitment
A total sample size of 1760 subjects was needed according to the sample size calculation for the study as per the primary outcome "Occurrence of reduced heart rate variability (RHRV)". Details of the sample size calculation have been described elsewhere [7]. A random sample of 2500 men and women each, with an age between 45 and 83 years was drawn from the population registry of the city of Halle (Saale), Saxony-Anhalt in 2002. The detailed recruitment procedure and response rate has been described elsewhere [7, 8]. In brief, the sampling was done using 5-year age strata, where residents in the age group of 75–80 years were oversampled, with twice as many invited from this stratum in comparison to the younger strata. The recruitment of study subjects has been done by inviting consecutive waves of random sub-samples of the original population sample. Accordingly, not all persons originally drawn from the population registry had to be invited in order to achieve a representative sample of the Halle population aged 45–80 years. Of the 3437 subjects invited to participate in the study, 1779 participants were recruited, of which 812 (46%) were women and 967 (54%) men, resulting in a final response proportion of 64.1% (68.6% for men and 59.5% for women) after exclusion of persons who deceased prior to the invitation, moved away or were unable to participate due to illness. The recuirtment process and reasons for non-participation in the study are presented in Fig. 1 and the study flowchart is presented in Fig. 2. Moreover, an analysis of non-respondents was implemented as a means to estimate non-response bias by obtaining information about prevalent diseases and selected behavioral and sociodemographic factors. Compared to the general population in Halle in the age of 45–85 years, CARLA study population had a higher proportion of subjects with university level education (11.8% in the general population in East Germany (2002) vs. 27.7% in CARLA-0) and also a higher proportion of unemployed subjects (for the age group 45–49 years old: 13,47% in the general population of Halle (2006) vs. 27% in the same age group in CARLA-0) [9, 10].
Fig. 1.
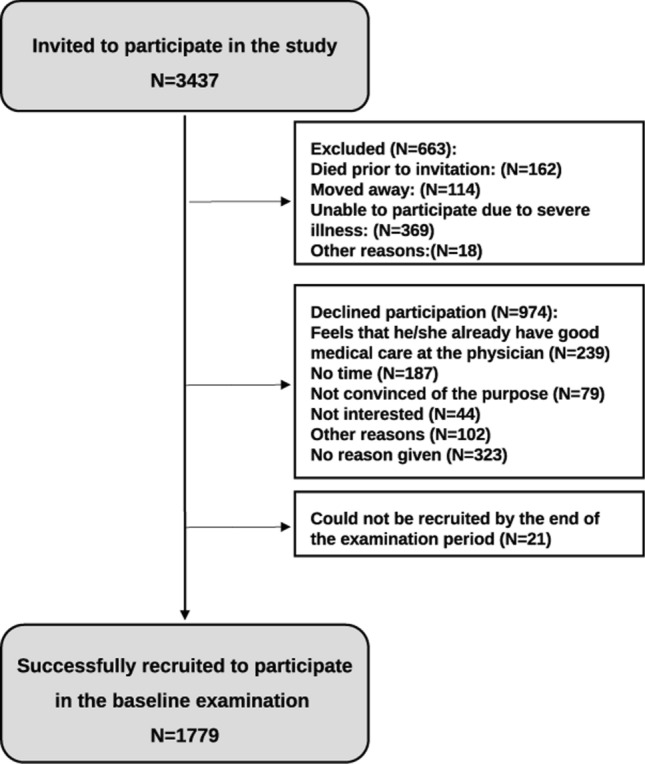
Flowchart of the number of subjects invited for participation in the CARLA study and reasons for exclusion and non-participation
Fig. 2.

Flowchart of the number of subjects attending examinations for the CARLA cohort and reasons for attrition
The local ethics commission of the Medical Faculty of the Martin Luther University Halle-Wittenberg approved the study and the follow-up examinations. All participants gave their written informed consent.
Baseline characteristics of the study population
Analyses of baseline data revealed that the study population suffered from high proportions of cardiovascular risk factors and diseases (Table 1). The study participants were characterized by a very high baseline prevalence of hypertension (74%), type 2 diabetes (15%) and a high average Body Mass Index (BMI) (28 kg/m2) [11]. In addition, there was a high prevalence of left ventricular hypertrophy and heart failure (HF) with preserved or reduced ejection fraction (HFpEF and HFrEF). The overall prevalence of symptomatic HF was 9.4% for men and 9.9% for women. Symptomatic HFrEF could be shown in 48% (n = 78), symptomatic HFpEF in 52% (n = 85) of subjects [12].
Table 1.
Demographic, clinical and laboratory characteristics of the CARLA cohort at baseline (CARLA-0), first (CARLA-1) and second (CARLA-2) follow-up examination
| Characteristics | Baseline (CARLA-0) | First Follow-up (CARLA-1) | Second Follow-up (CARLA-2) | |||
|---|---|---|---|---|---|---|
| n | Mean ± SD or n (%) | n | Mean ± SD or n (%) | n | Mean ± SD or n (%) | |
| Age (years) | 1779 | 64.4 ± 10.1 | 1436 | 67.3 ± 9.7 | 1140 | 70.2 ± 9.2 |
| Female | 1779 | 812 (45.6) | 1436 | 646 (44.9) | 1140 | 529 (46.4) |
| BMI (kg/m2) | 1779 | 28.3 ± 4.7 | 1423 | 28.3 ± 4.7 | 1040 | 28.9 ± 4.7 |
| Waist circumference (cm) | 1779 | 99.8 ± 12.7 | 1420 | 99.5 ± 13.6 | 0 | N/A |
| SBP (mmHg) | 1778 | 143.9 ± 21.3 | 1426 | 137.1 ± 19.6 | 1044 | 127.2 ± 18.4 |
| DBP (mmHg) | 1778 | 84.7 ± 11.1 | 1426 | 79.9 ± 10.2 | 1044 | 73.6 ± 10.4 |
| Triglycerides (mmol/L) | 1767 | 1.89 ± 1.5 | 1417 | 1.9 ± 1.2 | N/A | N/A |
| Total cholesterol (mmol/L) | 1767 | 5.5 ± 1.08 | 1417 | 5.4 ± 1.05 | N/A | N/A |
| HDL cholesterol (mmol/L) | 1767 | 1.4 ± 0.41 | 1417 | 1.3 ± 0.38 | N/A | N/A |
| LDL cholesterol (mmol/L) | 1767 | 3.4 ± 0.89 | 1416 | 3.3 ± 0.90 | N/A | N/A |
| Glucose (mmol/L) | 1767 | 5.99 ± 1.83 | 1417 | 5.8 ± 1.7 | N/A | N/A |
| HbA1c (%) | 1767 | 5.7 ± 0.8 | 1417 | 5.8 ± 0.7 | N/A | N/A |
| Creatinine (μmol/L) | 1767 | 75.2 ± 28.3 | 1417 | 80.4 ± 33.8 | N/A | N/A |
| eGFR (mL/min/1.73m2) | 1767 | 85.3 ± 16.6 | 1417 | 80.1 ± 17.9 | N/A | N/A |
| NT-proBNP (pg/mL) | 1722 | 216.1 ± 580.3 | 1416 | 253.3 ± 760.2 | N/A | N/A |
| CRP (mg/L) | 1695 | 3.2 ± 5.9 | 1417 | 3.5 ± 7.67 | N/A | N/A |
| IL-6 (pg/mL) | 1763 | 3.5 ± 4.6 | 1417 | 3.8 ± 7.4 | N/A | N/A |
| sTNF-R1 (pg/mL) | 1764 | 1180.3 ± 408.8 | 1417 | 1317.6 ± 509.4 | N/A | N/A |
| Current smoker | 1778 | 344 (19.3) | 1427 | 224 (15.7) | 1134 | 163 (14.3) |
| Current sport activity | 1777 | 643 (36.2) | 1426 | 667 (46.7) | 1106 | 540 (48.8) |
| Average years of education | 1779 | 14.9 ± 2.5 | 1431 | 14.8 ± 2.5 | N/A | N/A |
| University education | 1778 | 494 (27.7) | 1431 | 432 (30.1) | N/A | N/A |
| Unemployment | 1779 | 198 (11.0) | 1430 | 101 (7.1) | 1133 | 43 (3.8) |
| Retirement | 1779 | 1142 (64.1) | 1430 | 1011 (70.7) | 1133 | 852 (75.1) |
| Hypertensiona | 1779 | 1324 (74.4) | 1426 | 1084 (76.02) | 1041 | 736 (70.7) |
| Diabetes (self-reported) | 1778 | 274 (15.4) | 1431 | 258 (18.03) | 1130 | 216 (19.1) |
| Chronic heart failure | 1688 | 163 (9.6) | 1222 | 90 (7.3) | 1112 | 158 (14.2) |
| Antihypertensive medication | 1779 | 985 (55.3) | 1426 | 920 (64.5) | 1132 | 830 (73.3) |
| Lipid lowering medication | 1779 | 295 (16.5) | 1426 | 347 (24.3) | 1132 | 308 (27.2) |
| Anti-diabetic medication | 1779 | 218 (12.2) | 1426 | 203 (14.2) | 1132 | 181 (15.9) |
N/A not available, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, HDL high density lipoprotein, LDL low density lipoprotein, HbA1c hemoglobin A1c, eGFR estimated glomerular filtration rate, CRP C-reactive protein
aMeasured blood pressure > 140/90 or intake of antihypertensive medication
Follow‑up examinations
After a mean of 4.0 years (standard deviation [SD] = 0.3), 1436 (86%) subjects took part in the first follow-up examination. A second follow-up was performed after a mean of 8.8 years (SD = 0.7) with 1136 (77%) participants. Information on the vital status of participants is updated before the beginning of each follow-up and irregularly in between the follow-ups via a query at the residents' registration office. For deceased participants, a copy of the official death certificate is requested from the local health authority. The cause of death was defined as specified in the official death certificate compiled by the Federal Statistical Office. Initially, the cause of death was recorded by a medical doctor and subsequently reviewed by a certified coder at the Statistical State Office Saxony-Anhalt.
The third follow-up examination within the BioSALSA project (Biomarkers for Healthy Aging in Saxony-Anhalt) is currently taking place and will be finished by the end of 2021. For participants who are unable to come to the study center due to illness or fragility and whose address of residence was known, home visits with a reduced examination protocol are performed as in the first two follow-ups.
Data collection
Investigations performed at baseline, first follow-up and the current third follow-up included a standardized computer-assisted personal face-to-face interview, self-administered questionnaires, an extensive medical examination, and drawing of non-fasting venous blood samples (Tables 2, 3, 4). In the second follow-up, only an interview, self-administered questionnaires, blood pressure measurements, and anthropometry were performed. Standard operating procedures have been defined for each clinical examination which were then used at every follow-up. Interview and medical examinations were performed by trained and certified study nurses. At baseline and third-follow-up, echocardiographic examinations were conducted and evaluated by a specially trained and certified physician. At the first follow-up, echocardiography was performed by a trained and certified study nurse, and subsequently the stored echocardiographic recordings were evaluated by a trained physician. All echocardiographers underwent the same dedicated study certification procedures. The self-administered questionnaires were given to the participants to be filled at home. The baseline and first follow-up interview and examination took place at the previous CARLA study center in the University Hospital of the Martin-Luther-University Halle-Wittenberg. The second and ongoing third follow-up examinations are conducted at the current CARLA study center of the Institute of Medical Epidemiology of the Martin-Luther-University Halle-Wittenberg. The average duration was 3.5 h per participant.
Table 2.
Interview and questionnaire conducted at baseline (CARLA-0), first (CARLA-1), second (CARLA-2) and third (CARLA-3) follow-up examination
| Instrument | Time-points | |||
|---|---|---|---|---|
| CARLA-0 | CARLA-1 | CARLA-2 | CARLA-3 | |
| Interview | ||||
| Sociodemographic factors [16] | x | x | x | x |
| Utilization of medical services [14] | x | x | x | x |
| Medical history (self-reported) [13–15] | x | x | x | x |
| Family history [13–15] | x | x | – | – |
| Menopausal state and use of hormone replacement therapy | x | x | x | – |
| Medication use during the preceding 7 days [19] | x | x | x | x |
| Smoking, alcohol, and physical activity [14, 16, 17] | x | x | xa | xa |
| Food questionnaire [20] | x | x | xa | xa |
| Material circumstances [27] | x | x | x | xa |
| Social support [23] | x | x | x | x |
| Employment and personal financial situation after German reunification in 1990 | x | – | – | – |
| Unemployment, job insecurity [14, 27] | x | x | – | – |
| Health literacy [26] | – | – | x | – |
| Questionnaires | ||||
| Health-related quality of life (SF-12) [21, 22] | x | x | x | x |
| Perceived morale/attitude toward own aging [69] | x | x | x | |
| Hostility [70] | – | x | – | – |
| Social networks [23] | x | x | x | x |
| Job strain, effort-reward imbalance [71] | x | x | – | – |
| Depression scale [25] | x | x | x | x |
| Perceived security in neighborhood environments before and after German reunification in 1990 | x | – | – | – |
| Activities of daily Life (ADL) [24] | x | x | x | |
| Anxiety [46] | – | – | – | x |
| Resilience [44] | – | – | – | x |
| Cognitive Reserve [45] | – | – | – | x |
| Alcohol use—binge drinking [27] | x | – | – | – |
| Health beliefs | x | – | – | – |
| Sleep disorder | – | x | – | – |
aAs part of the questionnaires
Table 3.
Physical and medical examinations conducted and collected biosamples at baseline (CARLA-0), first (CARLA-1), second (CARLA-2) and third (CARLA-3) follow-up examination
| Instrument | Time-points | |||
|---|---|---|---|---|
| CARLA-0 (N = 1779) | CARLA-1 (N = 1436) | CARLA-2 (N = 1140) | CARLA-3 (N = ongoing) | |
| Anthropometry | ||||
| Body weight and body height (standing) [15, 72] | x | x | x | x |
| Waist and hip circumference | x | x | x | x |
| Body impedance analysis (BIA) [72] | – | – | – | x |
| 3D Body Scanner [72] | – | – | – | x |
| Cardiovascular system | ||||
| Blood pressure [15, 28] | x | x | x | x |
| Echocardiography, systolic and diastolic function | x | x | – | x |
| 12-leads Electrocardiogram (20-min and 10-s) [30, 31] | x | x | – | xa |
| Ankle–brachial index (ABI) [36)] | x | x | – | x |
| Pulse wave analysis (PWA) | xb | xb | ||
| AGE reader (skin autofluorescence) | – | x (N = 368) | – | x |
| Cognitive function | ||||
| Mini Mental State Examination | – | xc (N = 1020) | – | x |
| Semantic memory, episodic memory, working memory [35, 36] | – | – | – | x |
| Numerical reasoning (fluid intelligence), passive vocabulary (crystallized intelligence) [35] | – | – | – | x |
| Attention/executive, motor coordination [35] | – | – | – | x |
| Gait and balance assessment | ||||
| Timed up and Go Test (TMUG) [39] | – | – | – | x |
| Gait analysis using portable analysis system (Rehagait system) [40] | – | – | – | x |
| Balance assessment using pressure distribution measurement system (Zebris FM System) [41] | – | – | – | x |
| Sensory organ | ||||
| Olfactory test (Sniffin’ sticks 12) [38] | – | – | – | x |
| Bio-specimens | ||||
| Serum | x | x | – | x |
| EDTA whole blood | x | x | – | – |
| EDTA plasma | x | x | – | x |
| EDTA cellular components | x | x | – | x |
| MPA-stabilized EDTA plasma | x | x | – | – |
| Heparin plasma | – | x | – | x |
| Citrate plasma | x | x | – | x |
| Peripheral blood mononuclear cells | – | – | – | x |
| Urine | – | x | – | x |
| Stabilized stool | – | – | – | x |
| Physical activity, physical fitness | ||||
| Hand grip strength [42] | – | – | – | x |
| 7-Day accelerometry [43] | – | – | – | x |
a20-min ECG was not performed. Instead, a 5-min ECG was performed
bSphygmoCor device (CARLA-1) Vascular Explorer (CARLA-3)
cOnly in participants > = 60yrs
Table 4.
Blood and urine parameters determined at baseline (CARLA-0), first (CARLA-1) and third (CARLA-3) follow-up examination
| Parameter | CARLA-0 | CARLA-1 | CARLA-3 |
|---|---|---|---|
| Plasma and serum | |||
| Erythrocytes (RBC) | x | x | x |
| Nucleated red blood cells | – | – | x |
| Hemoglobin | x | x | x |
| Hematocrit | – | x | x |
| Leucocytes (WBC) | x | x | x |
| Lymphocytes | – | x | x |
| Neutrophilic granulocytes | – | x | x |
| Eosinophilic granulocytes | – | x | x |
| Basophilic granulocytes | – | x | x |
| Immature granulocytes | – | – | x |
| Monocytes | – | x | x |
| Platelets | – | x | x |
| Mean corpuscular volume | – | x | x |
| Mean corpuscular haemoglobin | – | x | x |
| Mean corpuscular haemoglobin concentration | – | x | x |
| Red cell distribution width | – | x | x |
| Mean platelet volume | – | x | – |
| Glucose | x | x | x |
| Glycated hemoglobin (Hba1c) | x | x | x |
| Creatinine | x | x | x |
| Triglycerides | x | x | x |
| Total cholesterol | x | x | x |
| High density lipoprotein cholesterol | x | x | x |
| Low density lipoprotein cholesterol (LDL) | x | x | x |
| Small dense LDL | – | x | – |
| Apolipoprotein A1 | – | x | x |
| Apolipoprotein B | – | x | x |
| Alanine aminotransferase | x | x | x |
| Aspartate aminotransferase | x | x | x |
| Gamma glutamyl transferase | x | x | x |
| α-Amylase | x | – | x |
| Lipase | x | – | x |
| N-terminal pro-brain-natriuretic peptide | x | x | x |
| (High-sensitivity) C reactive protein | x | x | x |
| Interleukin 1β (IL-1) | x | – | – |
| Interleukin 6 (IL-6) | x | x | x |
| Interferon γ | x | – | – |
| Tumor necrosis factor α (TNF-α) | x | – | – |
| soluble TNF-receptor 1 (sTNF-R1) | x | x | – |
| soluble TNF-receptor 2 (sTNF-R2) | x | – | – |
| Albumin | – | – | x |
| Insulin-like growth factor-1 | xa | – | x |
| Dehydroepiandrosterone sulfate | xa | – | x |
| Testosterone | xa | – | x |
| Prostate specific antigen (m) | xa | – | x |
| Ferritin (f) | xa | – | x |
| Sex hormone binding globulin | xa | – | x |
| Cystatin C | xa | – | x |
| Thyroid stimulating hormone | x | – | – |
| Free triiodothyonine | x | – | – |
| Total triiodothyonine | x | – | – |
| Free thyroxine | x | – | – |
| Total thyroxine | x | – | – |
| Antithyroglobulin antibodies | x | – | – |
| Antithyroperoxidase antibodies | x | – | – |
| Folate | x | – | – |
| Vitamin B12 | x | – | – |
| Soluble RAGE | x | xa | xa |
| AGE-specific fluorescence | x | xa | xa |
| Influenza A IgG | xa | ||
| Influenza B IgG | xa | ||
| CMV IgG/IgM | xa | ||
| Serum metabolites measured by targeted metabolomics AbsoluteIDQ p150 Kit | x | x | |
| Urine | |||
| Dip stick (bilirubin, erythrocytes, glucose, ketone, leucocytes, nitrite, pH, protein, spec. weight, urobilinogen) | x | x | x |
| Sediment (bacteria, erythrocytes, leucocytes) | – | – | x |
| Creatinine | – | – | x |
| Albumin | – | – | x |
| Uric acid | – | – | x |
aParameters determined from frozen samples as part of the third follow-up
Interview and questionnaires
The standardized, computer-assisted interview collected information regarding medical history (based on [13–15]), sociodemographic and socioeconomic variables (based on [16]), utilization of medical services (based on [14]), psychosocial and lifestyle factors (based on [14, 15, 17, 18]) (Table 2). The use of medication within the 7 days preceding examination was documented using the IDOM software to derive ATC codes [19]. Additionally, self-administered questionnaires were employed which included validated tools: a food frequency questionnaire adapted from / as in the EPIC Potsdam Study Follow-up [20], questionnaires on quality of life (based on [21, 22]), the adapted German version of the Berkman scale of social support and social networks [23], information on instrumental activities of daily living was collected based on a modified questionnaire from Lawton and Brody [24], physical activity was documented using the adapted Baecke questionnaire [17], smoking was recorded according to the recommendations of the German Epidemiological Association [16], depressed mood using the Center for Epidemiologic Studies Depression Scale (CES-D) (based on [25]), and health literacy as described by Sorensen [26]. Questionnaires on alcohol consumption, unemployment and job insecurity and material circumstances were adapted from the Study of Health In Pomerania (SHIP) [14] and the Health, Alcohol and Psychosocial factors in Eastern Europe (HAPIEE) [27] Study, respectively. Some elements were implemented in the interview at baseline and first follow-up and then were applied as self-administered questionnaires in the second and third follow-up (Table 2).
Examinations
The following examinations and measurements (Table 3) have been carried out in the CARLA Cohort:
Anthropometric parameters
The anthropometric measurements followed the procedures used in the MONICA/KORA and SHIP study [14, 15]. Weight and height were measured with the SECA 701 (seca GmbH & co.kg, Halle, Germany) digital scale and the SECA 220 (seca GmbH&Co.KG, Halle, Germany) height measuring system. Waist and hip circumference were measured using a flexible tape, with the study subject standing in front of a full-sized mirror, which allowed checking the horizontal position of the tape. Weight was recorded with a precision of 100 g, and height, waist and hip circumference to the nearest 0.1 cm.
Blood pressure measurement
After a resting period of at least five minutes, the measurement of systolic and diastolic blood pressure was performed. Blood pressure was measured with the OMRON HEM-705CP automated oscillometric blood pressure device [28] according to the procedure employed in the SHIP and KORA/MONICA Study [14, 29]. Three measurements were conducted on the left arm with a three-minute interval between measurements. The heart rate was counted manually during the resting time. In the third follow-up, we use the OMRON HEM-705IT, which is the successor device of OMRON HEM-705CP.
Electrocardiogram (ECG) recording
Two resting ECGs were recorded: one 10 s and one 20 min (5 min in third follow-up) 12-lead ECG. The participants were in a supine resting position for at least 20 min before the recording of the ECG began. Throughout the 20-min respectively the 5-min ECG, participants were instructed to breathe at a rate of 15/min (0.25 Hz). This was done to standardize the ECG recording with respect to the influence of the respiratory rate on the determination of spectral parameters of the heart rate variability (HRV). All 10-s ECGs were processed by the Modular ECG Analysis System (MEANS) [30] to obtain Minnesota Codes [31]. MEANS was additionally used to process the 20-min/5-min ECGs to obtain the locations and types of the QRS complexes, which were then used to compute standard time domain and frequency domain parameters of HRV. The method of computing HRV has been described in detail elsewhere [8, 32, 33].
Echocardiographic measurements
The analysis included parameters of left ventricular dimension (left ventricular mass) and of systolic and diastolic function derived from M-Mode and Doppler echocardiographic measurements.
Echocardiographic examinations at baseline and first follow-up were performed using the GE Vivid ultrasound system (GE Vivid 4 and 5 at baseline, GE vivid 5 at first follow-up). At the third follow-up, a Philips iE33 3D-echocardiographic device is used. Echocardiographic images are obtained in standardized parasternal and apical views using 2D, M-Mode, pulse wave and tissue doppler imaging. Echocardiographic measurements included parameters of left ventricular dimension, systolic and diastolic function. All acquired images and media are stored on a secured network server as digital clips, using a unique identification number, and analyzed on a dedicated workstation (EchoPAC PC, version 110.1.0, GE Healthcare and Philips IntelliSpace Cardiovascular 3.2).
Ankle–brachial index (ABI)
For ABI measurement in CARLA at baseline and first follow-up, the supine systolic blood pressure (BP) at the arm and ankle was measured after 5 min of rest using the OMRON HEM-705CP device. Measurement of BP was started simultaneously on the arm and ankle. Two measurements were conducted on the right ankle, followed by two measurements on the left ankle with a one-minute delay between each pair of measurements. To calculate the ABI, the mean systolic BP of that ankle side which was lowest was divided by the brachial systolic BP which was the highest. Further details are described elsewhere [34]. In the third follow-up, the Vascular Explorer (VaE) (Fa. Enverdis GmbH, Jena, Deutschland) is used to measure ABI as adapted from the NAKO study (National Cohort Study) [35]. For the determination of the ABI, the blood pressure is measured with the help of oscillometric blood pressure cuffs at both arms and legs as well as so-called occlusion pressure values at all four extremities through photo-plethysmographic measurement methods (SPO2 sensors).
Pulse wave analysis (PWA)
PWA was performed noninvasively in the first follow-up by applanation tonometry of the radial artery using SphygmoCor. During the third follow-up, PWA was perfomed using the VaE, according to the procedure employed in the NAKO Study [35, 36]. The following parameters of the vascular stiffness are determined via algorithms: pulse wave velocity, augmentation index and aortic blood pressure.
Advanced glycation end products (AGEs) analysis
Skin autofluorescence induced by the formation of AGEs was recorded in the first follow-up in a subgroup of N = 368 and will be measured in all participants in the third follow-up with the AGE Reader SU (DiagnOptics, The Netherlands).
Additional examinations in the third follow-up
In the third follow-up, our aim is to focus on aging processes from the perspective of a healthy aging (within the BioSALSA project: Biomarkers for Healthy Aging in Saxony Anhalt). It is envisaged that parameters of physiological, neurocognitive and immunological functioning as well blood biomarker profiles will allow a characterization of the (healthy) ageing process of the participants and their cardiovascular system. In addition to the examinations that were conducted at baseline and first follow-up, several further examinations are undertaken, such as the cognitive function test battery adapted from the German National Cohort (NAKO) [35, 36], an olfactory test [38], gait assessment using Timed up and Go test [39], an inertial-sensor based device [40], balance assessment using a pressure distribution plate [41], as well as the assessment of physical fitness using hand grip strength test [37, 42] and a 7-day accelerometry [43]. Using self-administered questionnaires, we will also measure psychosocial factors affecting ageing, such as resilience [44], cognitive reserve [45], depressed mood [25], and anxiety [46].
Laboratory analyses
Biosamples
Non-fasting, venous blood samples as well as other biomaterials were collected and processed following the standardized operating procedures of each examination by trained laboratory personnel at baseline and at the first follow-up. In general, samples were centrifuged, separated and immediately placed on ice for processing. Aliquoted samples were stored at -80 °C for future analyses. Detailed information about the collected biospecimens in each examination of the participants is given in Table 4.
In the third follow-up, Ethylenediaminetetraacetic acid (EDTA), citrate and heparin stabilized plasma as well as EDTA cellular components, serum, urine and stabilized stool will be collected and stored at − 80 °C to allow broad subsequent analyses. Furthermore, peripheral blood mononuclear cells (PBMCs) will be isolated by FICOLL gradient centrifugation utilizing BD Vacutainer CPT sodium citrate stabilized plasma tubes. Therefore, CPT vacutainers are centrifuged for 22 min at 1700×g, sodium citrate plasma is collected, replaced by phosphate-buffered saline (PBS) and the PBMCs are then decanted into 15 mL screw-cap tubes. After two washing steps with PBS, PBMCs are dissolved in freezing medium, aliquoted and stored at − 150 °C. The collected, corresponding sodium citrate plasma is also stored, allowing for direct pair-wise analyses of fluid and cells.
Analyses
An overview on the determined blood and urine parameters in baseline and first follow-up, as well as on the planned parameters of the third follow-up, is given in Table 4.
In the baseline examination, as well as in the first follow-up, blood samples were directly analyzed for a wide range of parameters including a hemogram, glucose, HbA1c, cholesterol levels, liver and pancreas enzymes, inflammatory markers, as well as kidney and thyroid function, as described before [7]. Additionally, advanced glycation end products (AGE)-specific fluorescence and their soluble receptor (sRAGE) levels were determined for non-fasting plasma samples collected at baseline [47]. Soluble tumor necrosis factor receptor R1 (TNF-R1) was determined in duplicates in serum samples of the baseline and the first follow-up using an antibody-based assay (Quantikine ELISA, R&D Systems) on an Epoch 2 Microplate Spectrophotometer [48].
Metabolite quantification was performed in the Genome Analysis Center at the Helmholtz Zentrum München using the AbsoluteIDQ™ p150 Kit (Biocrates Life Sciences AG, Austria). In more detail, a panel of 163 metabolites that includes free carnitine, 40 acylcarnitines, 14 amino acids, hexoses (sum of hexoses), 92 glycerophospholipids, and 15 sphingolipids was quantified by flow injection analysis-tandem mass spectrometry (FIA-MS/MS). The sample preparation and mass spectrometric measurements, as well as the metabolite nomenclature, have been described previously [49, 50].
In the third follow-up, measurements of most previously assessed blood parameters, as well as of additional blood and urine-parameters, are planned (Table 4). All measurements will be carried out in cooperation with the Central Laboratory of the University Hospital Halle (Saale) on Roche Cobas, Sysmex or ABL90 Flex Plus analytical platforms except for soluble RAGE and Influenza and CMV-reactive antibodies, which are determined manually by ELISA.
Findings to date
Results from the CARLA Study have been reported in 82 publications, out of which 34 publications were using only the CARLA cohort data and 48 publications were based on collaborations between CARLA and other national and international cohorts. More details are provided in the supplementary material. The in-depth data collection has been used for describing the prevalence and incidence of cardiovascular risk factors and diseases as well as for exploratory analyses on associations between cardiovascular risk factors and various phenotypes during a period spanning 11 years. Overall, we found a very high prevalence of all classic life-style-related cardiovascular risk factors and diseases, e.g. hypertension, overweight, diabetes mellitus, and heart failure. These findings were extraordinary even with respect to other population-based epidemiologic studies in Germany.
Key publications have reported the following specific findings:
Heart rate variability was shown to have a weak and inconsistent association with cardiovascular risk factors [8, 51, 52].
There was a high prevalence of symptomatic chronic heart failure. Women were more affected by heart failure with preserved ejection fraction, while men suffered from heart failure with reduced ejection fraction [12].
A decrease in systolic and diastolic blood pressure was observed between baseline and subsequent follow-ups, accompanied by an increase in anti-hypertensive medication consumption and a higher awareness of the condition. This decrease has been ascribed to a better hypertension control due to raised awareness of participants’ hypertension status after participation in the Study [53].
We showed that a higher health literacy score was associated with different health-related outcomes even after adjustment for educational level [54].
We found a direct association of the inflammation biomarker sTNF-R1 in the elderly male general population with renal failure development [55] and with echocardiographic parameters for ventricular hypertrophy [56], in addition to cardiovascular and all-cause mortality [48].
Recently, we showed that AGEs and their soluble receptor sRAGE measured in plasma samples were associated with limitations in physical functioning in women, but not in men [57]. However, we couldn’t find any association of plasma AGEs and sRAGE with overall or cardiovascular mortality [58].
We showed sex- specific effects of lifestyle risk factors [50] and ageing [59] on human metabolites. We also showed that the instability in an individuals’ own ‘metabolic space’ (metabotype) was associated with incident cardiovascular disease and all-cause mortality [60] thus, identifying metabotype instability represents a valuable indicator of pre-clinical disease.
Additionally, the data from the CARLA Study have been used in several pooled cohort analyses, such as the DIAB-CORE Consortium, which published findings on regional differences for diabetes mellitus in Germany [61] and describing the need for better blood pressure [62] and lipid-level management for subjects with diabetes [63]. The CARLA study was compared to other population-based cohorts in Germany to examine regional differences and disparities. For example, an analysis showed that the odds of type 2 diabetes prevalence were highest in the east (odds ratio = 1.98, 95% confidence interval: 1.81, 2.14) and northeast of Germany and decreased to the southwest after adjustment for individual variables [64]. In another analysis examining the incidence of type 2 diabetes, the results of an analysis of data from five population-based cohorts in Germany show that the regional incidence was highest in the East and lowest in the South of Germany with 16.9 (95% CI 13.3–21.8) vs 9.3 (95% CI 7.4–11.1)/1000 person-years, respectively [65]. The waist circumference as a measure of central obesity was also shown to be on average 3.4 and 6.7 cm higher among men and women with similar BMI in CARLA compared to a cohort from Bavaria [66].
In several genome-wide association studies, CARLA acted as a replication cohort, identifying 18 loci associated with CRP levels [67] and 4 loci associated with thyroid function [68]. The epidemiological lesson learned from a small cohort study, such as the CARLA cohort, is—when the primary goal is to examine real-life exposures, subject-related outcomes and their change, the focus should be on measures that can be standardized and replicated.
Strengths and limitations
The main strength of the CARLA Study is the comprehensive set of important clinical, biochemical, and lifestyle information collected during a long follow-up period in a representative sample of the elderly general population. The CARLA study is one of the last epidemiological studies in Germany that aimed for representativeness to the general population and indeed achieved response proportions of more than 60%. Nevertheless, we had to discuss problems and effects of selection bias on at least partly unexpected results. An analysis of non-responders (not shown here) indicated that selection bias due to non-participation led to an underestimation of disease prevalence and of risk factors in study participants as compared to the general population, which could have biased the associations of risk factors and disease towards the null as a result of a loss of highly susceptible subjects. The data has been used for answering several research questions in cardiology, endocrinology, and genetics. The stored bio-samples allow additional analyses. The harmonization of data collection with other cohort studies (KORA, SHIP, RECALL, EPIC Potsdam and HAPIEE) allows for pooled data analyses by including individual data of multiple cohorts. Self-reported information on a physician diagnosis of heart attack, stroke, cancer and diabetes were validated by general practitioners. The current data collection expands the focus into physical functioning in old age and mental health.
The main limitation is the relatively small sample size, making it difficult to study incident disease outcomes. Moreover, blood samples were not collected during the second follow-up period, and for examinations that are performed for the first time in CARLA subjects during the current third follow-up (e.g. gait and balance test), no preceding values exist.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the work of the medical and clerical staff at the Martin Luther University Halle-Wittenberg and all the study participants who made this study possible.
Authors' contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by Lamiaa Hassan, Ljupcho Efremov and Anne Großkopf and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The CARLA Study was funded by a grant from the Deutsche Forschungsgemeinschaft (DFG) as part of the Collaborative Research Centre 598 ‘Heart failure in the elderly – cellular mechanisms and therapy’, by an additional single funding grant from the DFG, by three grants of the Wilhelm-Roux-Programme of the Martin-Luther-University of Halle-Wittenberg (FKZ 14/41, 16/19 and 28/21), by the Federal Employment Office, by the Ministry of Education and Cultural Affairs of Saxony-Anhalt (MK-CARLA-MLU-2011). The project “Biosalsa” (ID: ZS/2019/07/99752) belongs to the Research Association „Autonomy in old Age“ (AiA) funded by the European Union (ERDF-European Regional Development Fund) and the State of Saxony-Anhalt, Germany.
Availability of data and materials
Researchers interested in a potential collaboration can apply for the data by sending an email to [carlastudie@uk-halle.de] or through submitting a form that is available on the CARLA study website https://webszh.uk-halle.de/carla-studie/. To access the data, a formal application must be submitted with a detailed research proposal consisting of a title, authors, research questions, brief scientific background, list of needed variables, and proposed statistical analyses. All proposals will be reviewed by the CARLA Study steering committee and a final decision on the use of data will be given.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethics approval was granted by the Ethics Committee of the Medical Faculty of the Martin Luther University Halle Wittenberg for the baseline study and follow-up examinations.
Consent to participate
All participants (or their legal guardians) provided written informed consent.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lamiaa Hassan, Ljupcho Efremov and Anne Großkopf joint first-authors.
Alexander Kluttig and Rafael Mikolajczyk joint last authors.
References
- 1.Bundesamt S. Todesursachenstatistik. 2020. https://www.destatis.de. Accessed 17.02.2021.
- 2.Muller-Nordhorn J, Rossnagel K, Mey W, Willich SN. Regional variation and time trends in mortality from ischaemic heart disease: East and West Germany 10 years after reunification. J Epidemiol Community Health. 2004;58(6):481–485. doi: 10.1136/jech.2003.013367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herzstiftung D. Deutscher Herzbericht 2016. Frankfurt: Deutsche Herzstiftung e.V.; 2016. [Google Scholar]
- 4.Roessner V, von Klitzing K. 25 years after the fall of the Berlin wall—what differences does child and adolescent psychiatry (still) see? Z Kinder Jugendpsychiatr Psychother. 2015;43(3):155–159. doi: 10.1024/1422-4917/a000350. [DOI] [PubMed] [Google Scholar]
- 5.Dornquast C, Kroll LE, Neuhauser HK, Willich SN, Reinhold T, Busch MA. Regional differences in the prevalence of cardiovascular disease. Dtsch Arztebl Int. 2016;113(42):704–711. doi: 10.3238/arztebl.2016.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franco OH, Karnik K, Osborne G, Ordovas JM, Catt M, van der Ouderaa F. Changing course in ageing research: the healthy ageing phenotype. Maturitas. 2009;63(1):13–19. doi: 10.1016/j.maturitas.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Greiser KH, Kluttig A, Schumann B, et al. Cardiovascular disease, risk factors and heart rate variability in the elderly general population: design and objectives of the CARdiovascular disease, Living and Ageing in Halle (CARLA) Study. BMC Cardiovasc Disord. 2005;5:33. doi: 10.1186/1471-2261-5-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greiser KH, Kluttig A, Schumann B, et al. Cardiovascular diseases, risk factors and short-term heart rate variability in an elderly general population: the CARLA study 2002–2006. Eur J Epidemiol. 2009;24(3):123–142. doi: 10.1007/s10654-009-9317-z. [DOI] [PubMed] [Google Scholar]
- 9.Bürgerservice F. Statistisches Jahrbuch der Stadt Halle (Saale) Stadt Halle (Saale): Die Oberbürgermeisterin; 2006. [Google Scholar]
- 10.Niedersachsen LfSuK. Sozioökonomische Grunddaten für die zwölf neuen EU-Mitgliedsstaaten. Deutschland und die Bundesländer; 2011.
- 11.Haerting J, Kluttig A, Greiser KH, Nuding S, Werdan K. Kohortenstudie zu Risikofaktoren für Herz-Kreislauf-Krankheiten in einer urbanen älteren ostdeutschen Allgemeinbevölkerung (CARLA-Studie) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55(6):795–800. doi: 10.1007/s00103-012-1493-4. [DOI] [PubMed] [Google Scholar]
- 12.Tiller D, Russ M, Greiser KH, et al. Prevalence of symptomatic heart failure with reduced and with normal ejection fraction in an elderly general population-the CARLA study. PLoS ONE. 2013;8(3):e59225. doi: 10.1371/journal.pone.0059225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med. 1977;31(1):42–48. doi: 10.1136/jech.31.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.John U, Greiner B, Hensel E, et al. Study of Health In Pomerania (SHIP): a health examination survey in an east German region: objectives and design. Soz Praventivmed. 2001;46(3):186–194. doi: 10.1007/BF01324255. [DOI] [PubMed] [Google Scholar]
- 15.Döring AFB, Holle R, et al. KORA-survey 2000. Manual of operation. Untersucher-handbuch. Neuherberg: GSF Neuherberg; 2000. [Google Scholar]
- 16.Jöckel KH, Babitsch B, Bellach BM. Messung und Quantifizierung soziodemographischer Merkmale in epidemiologischen Studien. München: MMV Medizin; 1998. pp. 7–38. [Google Scholar]
- 17.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 18.Kroke A, Klipstein-Grobusch K, Voss S, et al. Validation of a self-administered food-frequency questionnaire administered in the European Prospective Investigation into Cancer and Nutrition (EPIC) Study: comparison of energy, protein, and macronutrient intakes estimated with the doubly labeled water, urinary nitrogen, and repeated 24-h dietary recall methods. Am J Clin Nutr. 1999;70(4):439–447. doi: 10.1093/ajcn/70.4.439. [DOI] [PubMed] [Google Scholar]
- 19.Mühlberger N, Behrend C, Stark R. Datenbankgestützte Online-Erfassung von Arzneimitteln im Rahmen gesundheitswissenschaftlicher Studien, Erfahrungen mit der IDOM-Software. Informatik Biometrie und Epidemiologie in Medizin und Biologie. 2003;2003:601–611. [Google Scholar]
- 20.Mitry P, Wawro N, Six-Merker J, et al. Usual dietary intake estimation based on a combination of repeated 24-H food lists and a food frequency questionnaire in the KORA FF4 cross-sectional study. Front Nutr. 2019;6:145. doi: 10.3389/fnut.2019.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner-Bowker D, Hogue SJ. Short form 12 health survey (SF-12) In: Michalos AC, editor. Encyclopedia of quality of life and well-being research. Dordrecht: Springer Netherlands; 2014. pp. 5954–5957. [Google Scholar]
- 22.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 23.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 24.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. doi: 10.1093/geront/9.3_Part_1.179. [DOI] [PubMed] [Google Scholar]
- 25.Hautzinger M. Die CES-D Skala: Ein Depressionsm… sinstrument für Untersuchungen in der Allgemeinbevölkerung. Diagnostica. 1988.
- 26.Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bobak M, Room R, Pikhart H, et al. Contribution of drinking patterns to differences in rates of alcohol related problems between three urban populations. J Epidemiol Community Health. 2004;58(3):238–242. doi: 10.1136/jech.2003.011825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Brien E, Mee F, Atkins N, Thomas M. Evaluation of three devices for self-measurement of blood pressure according to the revised British Hypertension Society Protocol: the Omron HEM-705CP, Philips HP5332, and Nissei DS-175. Blood Press Monit. 1996;1(1):55–61. [PubMed] [Google Scholar]
- 29.Faulhaber HD, Luft FC. Treatment of high blood pressure in Germany. Am J Hypertens. 1998;11(6 Pt 1):750–753. doi: 10.1016/s0895-7061(98)00068-5. [DOI] [PubMed] [Google Scholar]
- 30.van Bemmel JH, Kors JA, van Herpen G. Methodology of the modular ECG analysis system MEANS. Methods Inf Med. 1990;29(4):346–353. doi: 10.1055/s-0038-1634805. [DOI] [PubMed] [Google Scholar]
- 31.Prineas RJCR, Blackburn H. The Minnesota code manual of electrocardiographic findings. Standard procedures for measurement and classification. Boston: John Wright PSB; 1982. [Google Scholar]
- 32.Bootsma M, Swenne CA, Van Bolhuis HH, Chang PC, Cats VM, Bruschke AV. Heart rate and heart rate variability as indexes of sympathovagal balance. Am J Physiol. 1994;266(4 Pt 2):H1565–H1571. doi: 10.1152/ajpheart.1994.266.4.H1565. [DOI] [PubMed] [Google Scholar]
- 33.Pluim BM, Swenne CA, Zwinderman AH, et al. Correlation of heart rate variability with cardiac functional and metabolic variables in cyclists with training induced left ventricular hypertrophy. Heart. 1999;81(6):612–617. doi: 10.1136/hrt.81.6.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ittermann T, Lorbeer R, Tiller D, et al. Serum thyrotropin concentrations are not associated with the ankle-brachial index: results from three population-based studies. Eur Thyroid J. 2015;4(Suppl 1):101–107. doi: 10.1159/000381309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schipf S, Schone G, Schmidt B, et al. The baseline assessment of the German National Cohort (NAKO Gesundheitsstudie): participation in the examination modules, quality assurance, and the use of secondary data. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020;63(3):254–266. doi: 10.1007/s00103-020-03093-z. [DOI] [PubMed] [Google Scholar]
- 36.German National Cohort C The German National Cohort: aims, study design and organization. Eur J Epidemiol. 2014;29(5):371–82. doi: 10.1007/s10654-014-9890-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trampisch US, Franke J, Jedamzik N, Hinrichs T, Platen P. Optimal Jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. J Hand Surg Am. 2012;37(11):2368–2373. doi: 10.1016/j.jhsa.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 38.Oleszkiewicz A, Schriever VA, Croy I, Hahner A, Hummel T. Updated Sniffin' Sticks normative data based on an extended sample of 9139 subjects. Eur Arch Otorhinolaryngol. 2019;276(3):719–728. doi: 10.1007/s00405-018-5248-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 40.Schwesig R, Leuchte S, Fischer D, Ullmann R, Kluttig A. Inertial sensor based reference gait data for healthy subjects. Gait Posture. 2011;33(4):673–678. doi: 10.1016/j.gaitpost.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 41.Kalron A, Achiron A. Postural control, falls and fear of falling in people with multiple sclerosis without mobility aids. J Neurol Sci. 2013;335(1–2):186–190. doi: 10.1016/j.jns.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 42.Roberts HC, Denison HJ, Martin HJ, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40(4):423–429. doi: 10.1093/ageing/afr051. [DOI] [PubMed] [Google Scholar]
- 43.Santos-Lozano A, Santin-Medeiros F, Cardon G, et al. Actigraph GT3X: validation and determination of physical activity intensity cut points. Int J Sports Med. 2013;34(11):975–982. doi: 10.1055/s-0033-1337945. [DOI] [PubMed] [Google Scholar]
- 44.Aiena BJ, Baczwaski BJ, Schulenberg SE, Buchanan EM. Measuring resilience with the RS-14: a tale of two samples. J Pers Assess. 2015;97(3):291–300. doi: 10.1080/00223891.2014.951445. [DOI] [PubMed] [Google Scholar]
- 45.León I, García-García J, Roldán-Tapia L. Estimating cognitive reserve in healthy adults using the cognitive reserve scale. PLoS ONE. 2014;9(7):e102632. doi: 10.1371/journal.pone.0102632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 47.Bartling B, Hofmann HS, Sohst A, et al. Prognostic potential and tumor growth-inhibiting effect of plasma advanced glycation end products in non-small cell lung carcinoma. Mol Med. 2011;17(9–10):980–989. doi: 10.2119/molmed.2011.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hassan L, Medenwald D, Tiller D, et al. The association between change of soluble tumor necrosis factor receptor R1 (sTNF-R1) measurements and cardiovascular and all-cause mortality-results from the population-based (Cardiovascular Disease, Living and Ageing in Halle) CARLA study 2002–2016. PLoS ONE. 2020;15(10):e0241213. doi: 10.1371/journal.pone.0241213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goek ON, Doring A, Gieger C, et al. Serum metabolite concentrations and decreased GFR in the general population. Am J Kidney Dis. 2012;60(2):197–206. doi: 10.1053/j.ajkd.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 50.Lacruz ME, Kluttig A, Tiller D, et al. Cardiovascular risk factors associated with blood metabolite concentrations and their alterations during a 4-year period in a population-based cohort. Circ Cardiovasc Genet. 2016;9(6):487–494. doi: 10.1161/CIRCGENETICS.116.001444. [DOI] [PubMed] [Google Scholar]
- 51.Kluttig A, Schumann B, Swenne CA, et al. Association of health behaviour with heart rate variability: a population-based study. BMC Cardiovasc Disord. 2010;10:58. doi: 10.1186/1471-2261-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Medenwald D, Swenne CA, Frantz S, et al. Longitudinal association of short-term, metronome-paced heart rate variability and echocardiographically assessed cardiac structure at a 4-year follow-up: results from the prospective, population-based CARLA cohort. Europace. 2017;19(12):2027–2035. doi: 10.1093/europace/euw296. [DOI] [PubMed] [Google Scholar]
- 53.Lacruz ME, Kluttig A, Hartwig S, et al. Prevalence and incidence of hypertension in the general adult population: results of the CARLA-cohort study. Medicine (Baltimore) 2015;94(22):e952. doi: 10.1097/MD.0000000000000952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tiller D, Herzog B, Kluttig A, Haerting J. Health literacy in an urban elderly East-German population—results from the population-based CARLA study. BMC Public Health. 2015;15:883. doi: 10.1186/s12889-015-2210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Medenwald D, Girndt M, Loppnow H, et al. Inflammation and renal function after a four-year follow-up in subjects with unimpaired glomerular filtration rate: results from the observational, population-based CARLA cohort. PLoS ONE. 2014;9(9):e108427. doi: 10.1371/journal.pone.0108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Medenwald D, Dietz S, Tiller D, et al. Inflammation and echocardiographic parameters of ventricular hypertrophy in a cohort with preserved cardiac function. Open Heart. 2014;1(1):e000004. doi: 10.1136/openhrt-2013-000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ebert H, Lacruz ME, Kluttig A, et al. Advanced glycation end products and their ratio to soluble receptor are associated with limitations in physical functioning only in women: results from the CARLA cohort. BMC Geriatr. 2019;19(1):299. doi: 10.1186/s12877-019-1323-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ebert H, Lacruz ME, Kluttig A, et al. Association between advanced glycation end products, their soluble receptor, and mortality in the general population: results from the CARLA study. Exp Gerontol. 2020;131:110815. doi: 10.1016/j.exger.2019.110815. [DOI] [PubMed] [Google Scholar]
- 59.Chak CM, Lacruz ME, Adam J, et al. Ageing investigation using two-time-point metabolomics data from KORA and CARLA studies. Metabolites. 2019 doi: 10.3390/metabo9030044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lacruz ME, Kluttig A, Tiller D, et al. Instability of personal human metabotype is linked to all-cause mortality. Sci Rep. 2018;8(1):9810. doi: 10.1038/s41598-018-27958-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schipf S, Werner A, Tamayo T, et al. Regional differences in the prevalence of known Type 2 diabetes mellitus in 45–74 years old individuals: results from six population-based studies in Germany (DIAB-CORE Consortium) Diabet Med. 2012;29(7):e88–95. doi: 10.1111/j.1464-5491.2012.03578.x. [DOI] [PubMed] [Google Scholar]
- 62.Ruckert IM, Baumert J, Schunk M, et al. Blood pressure control has improved in people with and without type 2 diabetes but remains suboptimal: a longitudinal study based on the German DIAB-CORE Consortium. PLoS ONE. 2015;10(7):e0133493. doi: 10.1371/journal.pone.0133493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ruckert IM, Schunk M, Holle R, et al. Blood pressure and lipid management fall far short in persons with type 2 diabetes: results from the DIAB-CORE Consortium including six German population-based studies. Cardiovasc Diabetol. 2012;11:50. doi: 10.1186/1475-2840-11-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Muller G, Kluttig A, Greiser KH, et al. Regional and neighborhood disparities in the odds of type 2 diabetes: results from 5 population-based studies in Germany (DIAB-CORE consortium) Am J Epidemiol. 2013;178(2):221–230. doi: 10.1093/aje/kws466. [DOI] [PubMed] [Google Scholar]
- 65.Schipf S, Ittermann T, Tamayo T, et al. Regional differences in the incidence of self-reported type 2 diabetes in Germany: results from five population-based studies in Germany (DIAB-CORE Consortium) J Epidemiol Community Health. 2014;68(11):1088–1095. doi: 10.1136/jech-2014-203998. [DOI] [PubMed] [Google Scholar]
- 66.Stang A, Doring A, Volzke H, et al. Regional differences in body fat distributions among people with comparable body mass index: a comparison across six German population-based surveys. Eur J Cardiovasc Prev Rehabil. 2011;18(1):106–114. doi: 10.1097/HJR.0b013e32833b3305. [DOI] [PubMed] [Google Scholar]
- 67.Dehghan A, Dupuis J, Barbalic M, et al. Meta-analysis of genome-wide association studies in >80 000 subjects identifies multiple loci for C-reactive protein levels. Circulation. 2011;123(7):731–738. doi: 10.1161/CIRCULATIONAHA.110.948570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rawal R, Teumer A, Volzke H, et al. Meta-analysis of two genome-wide association studies identifies four genetic loci associated with thyroid function. Hum Mol Genet. 2012;21(14):3275–3282. doi: 10.1093/hmg/dds136. [DOI] [PubMed] [Google Scholar]
- 69.Lawton MP. The Philadelphia Geriatric Center Morale Scale: a revision. J Gerontol. 1975;30(1):85–89. doi: 10.1093/geronj/30.1.85. [DOI] [PubMed] [Google Scholar]
- 70.Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB., Jr The Cook–Medley hostility scale: item content and ability to predict survival. Psychosom Med. 1989;51(1):46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- 71.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- 72.Fischer B, Sedlmeier AM, Hartwig S, et al. Anthropometrische Messungen in der NAKO Gesundheitsstudie – mehr als nur Größe und Gewicht. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020;63(3):290–300. doi: 10.1007/s00103-020-03096-w. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Researchers interested in a potential collaboration can apply for the data by sending an email to [carlastudie@uk-halle.de] or through submitting a form that is available on the CARLA study website https://webszh.uk-halle.de/carla-studie/. To access the data, a formal application must be submitted with a detailed research proposal consisting of a title, authors, research questions, brief scientific background, list of needed variables, and proposed statistical analyses. All proposals will be reviewed by the CARLA Study steering committee and a final decision on the use of data will be given.
Not applicable.


