Abstract
Background:
Medical errors were largely concealed prior to the landmark report “To Err Is Human”. The purpose of this systematic scoping review was to determine the extent pediatric surgery defines and studies errors, and to explore themes among papers focused on errors in pediatric surgery.
Methods:
The methodological framework used to conduct this scoping study has been outlined by Arksey and O’Malley. In January 2020, PubMed, the Cochrane Database of Systematic Reviews, and the Cochrane Central Register of Controlled Trials were searched. Oxford Level of Evidence was assigned to each study; only studies rated Level 3 or higher were included.
Results:
Of 3,064 initial studies, 12 were included in the final analysis: 4 cohort studies, and 8 outcome/audit studies. This data represented 5,442,000 aggregate patients and 8,893 errors. There were 6 different error definitions and 5 study methods. Common themes amongst the studies included a systems-focused approach, an increase in errors seen with increased complexity, and studies exploring the relationship between error and adverse events.
Conclusions:
This study revealed multiple error definitions, multiple error study methods, and common themes described in the pediatric surgical literature. Opportunities exist to improve the safety of surgical care of children by reducing errors.
Level of Evidence Rating:
1
Keywords: Medical error, surgical error, pediatric surgery, pediatric surgical error, scoping study, systematic review
1. Introduction:
Medical and surgical error was largely concealed from the public eye prior to the landmark report “To Err Is Human”1. This report triggered a shift in the practice of medicine toward emphasizing safety and quality of care delivered. Now over two decades since its release, numerous patient safety initiatives have originated and hospital quality standards have improved2. There have been systematic reviews published on surgical adverse events3, never events4, and single interventions such as implementation of checklists5. However, the amount of research on surgical errors has been scarce. Existing randomized controlled trials or systematic reviews focus on individual types of surgical error6-9. While there also have been systemic reviews studying errors in some surgical subspecialties10-13, there have been no systematic reviews on errors in pediatric surgery.
In order to conduct this study, we used Arksey and O’Malley’s strict methodological framework for systematic scoping reviews with validated additions, including an assessment of the quality of research14-17. This type of research follows rigorous guidelines in order to “map” existing literature on a topic, particularly when the topic is heterogenous, complex and not yet extensively reviewed, such as the topic of pediatric surgical errors14-17. Arksey and O’Malley identified four reasons for conducting a systematic scoping study, of which the following three applied to this study in particular: “to examine the extent, range and nature of research activity,” to “summarize and disseminate research findings” and to “identify research gaps in the existing literature”14. In conducting a systematic scoping review of pediatric surgical errors, our specific goals were to determine the extent pediatric surgery defines errors, the various methodological approaches to study pediatric surgical errors, and to explore common themes amongst the highest quality research available in this area.
2. Methods:
In conjunction with two medical librarians (KK, EA), the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, and PubMed databases were searched in January 2020 using the following terms: ((((("databases, factual"[MAJR] OR data[TIAB] OR measure[TIAB] OR measurement*[TIAB] OR statistics[TIAB] OR "statistics and Numerical Data"[SH] OR methods[SH] OR statistical[TIAB]) AND (medical errors[MAJR] OR "medical error*"[TIAB]) AND (surgery[MAJR] OR surgery[sh] OR surgery[TI] OR surgical[TI] OR surgical procedures, operative[MAJR]))))). No time limits were set. These search criteria were selected in order to capture all articles studying surgical error. Publications that were duplicates or unrelated to humans were immediately excluded. At least two reviewers (KMM, FET, XC, SV, RSJ) screened each title and abstract to select studies for full-text review. Studies that either seemed appropriate for inclusion, or those that could not clearly be excluded on title and abstract alone were carried forward for further evaluation. Conflicts were resolved jointly between the 5 article reviewers (KMM, FET, XC, SV, RSJ). Two authors (KMM, RSJ) then independently assessed each remaining full-text article to determine eligibility for inclusion in the study. Disagreement was resolved by consensus, and Institutional Board Review approval was not required.
Inclusion criteria:
Pediatric general surgery and all pediatric surgical subspecialties
Pre-, intra-, or post-operative phases of care
Definition of error
Error measurement method
Exclusion criteria:
Articles without pediatric patients
No full-text available
Full text in languages other than English
Failure to define error
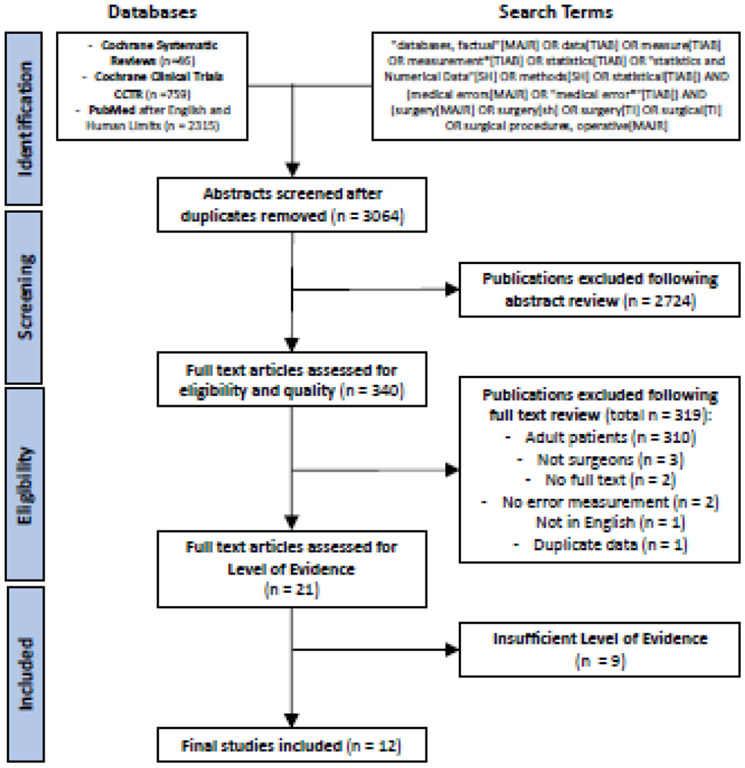
Of note, one text was excluded on the basis of utilizing a duplicate dataset. Following full-text review, two authors (KMM, RSJ) then independently determined Level of Evidence for each remaining study18. Disagreement on Level of Evidence was resolved by consensus. Studies that had a Level of Evidence of 4 or 5 were excluded. This full process is outlined in the PRISMA flowsheet (Figure 1).
Figure 1:
PRISMA Flow Diagram
Of the included articles, the following data were extracted: title, author names, author degrees, year published, journal, impact factor of journal, subspecialty, phase of care, nation, single or multi-institutional, financial support, type of study, number of patients, and number of errors. Several studies reviewed data in national databases. As a necessary clarification, if authors were from a single institution but reviewed a national data set from many institutions, these papers were categorized as “multi-institutional.”
To determine the extent pediatric surgery defines errors and the various methodological approaches to study pediatric surgical errors, the error definition and study methods used in each article were also recorded. Recurrent definitions and study methods were identified and grouped. Similarly, overall themes across multiple studies were recognized and described.
3. Results:
A total of 3,064 studies were identified for screening after excluding duplicates. After abstract review, 340 full-text articles were assessed for inclusion and exclusion criteria. Following full-text review and resolution of conflicts, 21 articles met inclusion criteria. Of these, 12 studies had sufficient Level of Evidence (Figure 1). There were 4 cohort studies and 8 outcome/audit studies (Table 1). No systematic reviews or randomized controlled clinical trials were found. The data represented 5,442,197 aggregate patients and 8,893 errors from five different nations. In addition to general pediatric surgery, pediatric surgical subspecialties were represented including cardiothoracic surgery, neurosurgery, urology, orthopedic surgery, otolaryngology, transplantation, and plastic surgery. Errors were examined in the preoperative (n = 8), intraoperative (n = 6), and postoperative (n = 5) phases of care, with five studies observing errors in more than one phase of care. Only 4 of these studies received funding: 2 federal, 1 foundational, and 1 departmental. There were 4 multi-institutional studies.
Table 1:
Included studies arranged by error category, type of study, level of evidence, surgical subspecialty, phase of care, and nation. Number of patients and number of errors captured in each study.
| Type of Study | Level of Evidence |
Subspecialty | Phase Of Care | Nation | Number of Patients |
Number of Errors |
|
|---|---|---|---|---|---|---|---|
| Medication Errors | |||||||
| King et al. 2003 | Cohort | 2 | Multiple | Pre/Post Op | Canada | 36,103 | 804 |
| Kaushal et al. 2008 | Cohort | 2 | Multiple | Pre/Post Op | USA | 1,924 | 32 |
| Engum et al. 2008 | Outcomes / Audit | 2 | Multiple | Pre/Post Op | USA | 757 | 1340 |
| Errors in Diagnosis | |||||||
| Smink et al. 2004 ~ * | Cohort | 2 | General Pediatric Surgery | Pre Op | USA | 37,109 | 3103 |
| Kutasy et al. 2010 | Cohort | 2 | General Pediatric Surgery | Pre Op | Ireland | 1228 | 153 |
| Bachur et al. 2012 ~ | Outcomes / Audit | 2 | General Pediatric Surgery | Pre Op | USA | 52,290 | 1882 |
| Technical Errors | |||||||
| Tang et al. 2004 | Outcomes / Audit | 2 | General Pediatric Surgery | Intra Op | Netherlands | 50 | 310 |
| Never Events | |||||||
| Shah et al. 2009 ~ | Outcomes / Audit | 2 | Multiple | Intra Op | USA | 3,365,317 | 103 |
| Camp et al. 2010 ~ * | Outcomes / Audit | 2 | Multiple | Intra Op | USA | 1,946,831 | 413 |
| Comprehensive | |||||||
| Proctor et al. 2003 | Outcomes / Audit | 2 | General Pediatric Surgery | Pre/Intra/Post Op | Canada | 64 | 108 |
| Catchpole et al. 2006 * | Outcomes / Audit | 2 | Cardiothoracic | Intra Op | UK | 24 | 217 |
| Hickey et al. 2015 * | Outcomes / Audit | 2 | Cardiothoracic | Pre/Intra/Post Op | Canada | 500 | 428 |
Denotes Multi-Institutional Study
Denotes Research Funding
There were 6 different error definitions and 5 study methods. Themes spanning across multiple studies included: systems-focused approaches, correlation between errors and increased complexity, and the relationship between error and adverse events.
3.1. Definitions and Methodology
There were large variations in both error definition and study methods (Table 2). Only three articles defined error broadly using a definition proposed by either Lucian Leape (n = 2) or James Reason (n = 1). One article used a taxonomy to define error. All other articles specifically defined error as negative appendectomy (n = 3), events during medication use (n = 3), or retained foreign body (n = 2).
Table 2:
Error definitions and study methods used in each article.
| Error Definition | |
|---|---|
| Negative appendectomy (n = 3) |
Smink et al. 2004
Kutasy et al. 2010 Bachur et al. 2012 |
| Events During Medication Use (n = 3) | King et al. 2003 Engum et al. 2008 Kaushal et al. 2008 |
| Retained Foreign Body (n = 2) |
Shah et al. 2009
Camp et al. 2010 |
| Based on Lucian Leape (n = 2) |
Proctor et al. 2003
Hickey et al. 2015 |
| Based on James Reason (n = 1) | Tang et al. 2004 |
| List/Taxonomy of Types of Error (n = 1) | Catchpole et al. 2006 |
| Error Methodology | |
| Database Review (n = 5) |
Smink et al. 2004
Engum et al. 2008 Shah et al. 2009 Camp et al. 2010 Bachur et al. 2012 |
| Medical Record Review (n = 4) | King et al. 2003 Kaushal et al. 2008 Engum et al. 2008 Kutasy et al. 2010 |
| Direct Observer (n = 3) |
Proctor et al. 2003
Catchpole et al. 2006 Hickey et al. 2015 |
| Video Review (n = 2) |
Tang et al. 2004
Catchpole et al. 2006 |
| Technical Scoring System (n = 1) | Tang et al. 2004 |
Regarding research methods, the vast majority of articles utilized either a database review (n = 5) or medical record review (n = 4). Other study methods included direct observation (n = 3), video review (n = 2), or a technical scoring system (n =1). Three articles used more than one study method; all other articles examined error only using a single method.
3.2. System-Focus vs. Human Factors
Four articles explored the interplay between systems and individuals. Catchpole et al. 2006 and Hickey et al. 2015 used a “threat and error” model from the 6-σ aviation industry. This system-based approach proposes that an accumulation of predisposed threats leads to error. Similarly, Tang et al. 2004 observed human factors regarding technical errors and discussed system aspects that could minimize individual error. For example, poor instrument design – a system error – contributed to many of the individual surgeons’ technical errors involving specific holding forceps. The interplay between systems and individuals was further highlighted by Smink et al. 2004. This retrospective database review showed that higher hospital volume (system) is associated with a lower risk of misdiagnosis of pediatric appendicitis (individual).
3.3. Complexity and Errors
Four articles in the present study suggest that increased patient complexity is associated with more errors. Catchpole et al. 2006 and Hickey et al. 2015 describe how a sequence of multiple minor errors can propagate a major error. The authors also discuss that the “threat” of an error is increased in more complex patients or during high clinical workloads. Kaushal et al. 2008 found more errors on intensive care units and less error on general surgical units, given that patients in intensive care unit settings are generally more complex than those on the general units. Individual patients’ risks and comorbidities also contribute to their overall complexity. Kutasy et al. 2010 noted that pediatric patients living with obesity more often had negative appendectomies, speaking to the increased diagnostic complexity in this patient population.
3.4. Errors vs Adverse Events
Six articles discussed the relationship between errors and adverse events. Engum et al. 2008 found that only 5% of errors resulted in adverse events. On the other hand, Proctor et al. 2003 found that 47% of adverse events were attributable directly to error. Proctor et al. 2003 also found that if a patient experienced 5 or more errors, all had an adverse event.
Due to the relationship between error and adverse events, Kaushal et al. 2008 proposed a pharmacist intervention to reduce medication errors. Ultimately, the intervention also decreased the number of adverse events in pediatric intensive care units – from 29 per 1000 patient days to 6 per 1000 patient days. However, reducing error does not always influence the frequency of adverse events. King et al. 2003 found that introduction of a computerized prescriber order entry system decreased the number of errors by 40%, but the number of adverse events did not significantly change. Regardless, the authors point out that most errors have the potential to cause harm. Lastly, Shah et al. 2008 and Camp et al. 2010 queried national databases to study retained foreign bodies – a specific type of adverse event.
4. Discussion:
Research findings can be summarized by recognizing varied error definitions and study methods, employing systems-focused approaches, noting a correlation between errors and increased complexity, and acknowledging the relationship between error and adverse events. These findings lead to the discovery of multiple gaps in existing literature. Discussed further below, these gaps include the lack of standardized error definitions, varied sensitivities of available study methods, means to decrease error, considerations for errors in pediatric patients in particular, and cost analyses.
With a total of only 12 final articles included in this study, there were 6 different definitions of error and 5 study methods. Lucian Leape defined error as “an unintended act (either of omission or commission) or one that does not achieve its intended outcome”19; James Reason defined error as “either a failure of a planned action to be completed as intended (i.e., an error of execution), or the use of a wrong plan to achieve an aim (i.e., an error of planning)”20. Drawing from a broad base of literature in other surgical fields, many more definitions of error and study methods have been explored (Marsh et al., in submission). In part due to inconsistent definitions and variety of research methods, the true epidemiology of medical error is unknown21. The first step to determining the prevalence of error is to establish universal definitions. As an individual example of the importance of clearly defining error, Kutsay et al. 2010 investigated negative appendectomies in the pediatric population. Ultrasonography was performed only when clinical findings were equivocal in patients with suspected appendicitis. This points to differences in diagnosing based on imaging selection, but whether this is truly an error in care delivery remains in question. Until types of error are clearly defined, this question will remain up for debate.
Another topic of debate is the role of systems versus human factors in patient care. There has been a shift in the culture of healthcare – removing blame from individuals and instead placing it on systemic flaws. While redirecting emphasis to the system avoids impugning individuals as negligent, systems are comprised of individuals. Errors in communication remain the most common type of error22, reinforced in the present study by results from Proctor et al. 2003 and Catchpole et al. 2006. Thus, human factors are an important element to consider as a part of the system. For instance, Smink et al. 2004 studied the effect of hospital volume on pediatric appendectomies. Due to database limitations, the analysis did not control for volume of procedure per surgeon. It is conceivable that individual surgeons with higher case volume are less likely to make misdiagnoses, but also that being in a system with more efficient processes of care lead to the appropriate imaging (Bachur et al. 2012) and referrals, thus ultimately the correct diagnosis. Various system improvements have been proposed to minimize individual error. For example, Engum et al. 2008 suggests that medication errors specifically could be decreased with computerized prescriber order entry, providing accessible dosage information, and restructuring teams to include clinical pharmacists. However, this study also suggests further education of involved team members as more of an individual contribution to the system. With the increased overall emphasis on system errors, the importance of individual contribution to error and individual expertise should not be disregarded.
Similarly, individual complexity contributes to the risk of error. Increased complexity not only refers to each individual patient, but also the type of error committed. For example, technical errors such as studied by Tang et al. 2004 are possibly more easily enumerated than errors in judgement. Areas with increased complexity may offer a larger opportunity for untapped error measurement, and ultimately more prospect to decrease the total number of errors.
To decrease the number of adverse events, multiple system changes have been implemented, such as the World Health Organization’s Surgical Safety Checklist and the Joint Commission’s Universal Protocol. However, it is important to differentiate between errors and adverse events. Adverse events result in harm to the patient23. Adverse events are defined by Lucian Leape as “an unintended injury that was caused by medical management and that resulted in measurable disability”24. Errors are more common but may or may not cause harm, thus do not always lead to an adverse event. However, error can be associated with adverse events. Prior studies have suggested that more than half of adverse events are due to medical errors24,25. An extreme version of an adverse event is a “never event,” defined by the Agency for Healthcare Research and Quality as surgery on the wrong body part, surgery on the wrong patient, performing the wrong procedure, presence of a retained foreign object, or death in an American Society of Anesthesiologists Class I patient26. The databases used in the studies by Shah et al. 2008 and Camp et al. 2010 for retained foreign bodies did not delineate the need for reoperation, what items were retained, or what events led to the retained item. These factors are important to explore to further investigate the relationship between errors, adverse events and never events.
Most existing research on medical errors has been retrospective in nature. There are multiple benefits to prospective data collection, namely capturing more error. Prior literature reports widely varied incidence of error largely depending on definition and study method. For example, the Institute for Healthcare Improvement found that errors occur to slightly over 40% of Americans from survey data27. However, by using a direct observer to capture error prospectively, Proctor et al. 2003 found errors in the care of 67% of patients with an average of 2.5 errors per patient. Overall dramatic variations in error rates were appreciated in existing literature and further highlighted amongst the final 12 articles in this study. For instance, Catchpole et al. 2006 reported 217 errors in 24 patients, whereas King et al. 2003 reported 804 errors in 36,103 patients (Table 1). The seemingly higher rate of error in certain studies is likely due to the increased sensitivity of particular researchers’ study methods, suggesting the true prevalence of medical error may be higher than initially suspected. Learning about this variation helps clinicians understand how to examine errors in a more informed way. In order to grasp the true extent of medical error, it will be necessary to also establish sensitivities of study methods.
Once definitions and methods are more clearly delineated, a taxonomy of error can be outlined. In this study, the articles mainly studied medication errors, technical errors, error in diagnosis and system errors. System errors encompass many other subtypes of error including equipment, team structure, communication, documentation, and delays. The two papers using the “threat and error model” did also address judgement errors. Catchpole et al. 2006 included “decision-related surgical error” in the taxonomy of error definition, and Hickey et al. 2015 found the second most frequent errors to be those in judgement. These are perhaps the most difficult errors to measure and should be an area of future research. Catchpole et al. 2006 and Hickey et al. 2015 drew on comparisons to the airline industry – a corollary also made by other researchers28,29. Aviation has achieved the gold standard 6-σ safety level or beyond30. Realizing that humans are the least reliable metric in a cockpit has allowed the industry to set systems in place that account for human fallibility. The most obvious difference between aviation and healthcare is the involvement of human patients as opposed to machines. While this adds to the complexity of healthcare, there is much to be learned from the success of other industries such as the airline industry.
Another important consideration in the present study is the patient population. With multiple non-pediatric physicians and surgeons caring for infants and children, there is added team complexity thus possibility for error. However, it is unknown whether more errors occur when non-pediatric surgeons, physicians, and other team members care for pediatric patients compared to pediatric-specific team members. Also, characteristics unique to pediatric patients can contribute to possible error. For example, pediatric patients are at increased susceptibility for medication errors due to the need to adjust medication dosages to patient weight, changes in pharmacokinetic parameters, age-related patient communication challenges, among other reasons31. Errors also drive-up healthcare costs. There was minimal focus on cost in our final collection of articles with the exception of Shah et al. 2009, and to a lesser extent Camp et al. 2010. This is an area that requires further research.
There were three main limitations to consider in this study. Unlike adult intensive care units, often medical and surgical patients are in the same neonatal or pediatric intensive care units. Thus, some studies included both medical and surgical pediatric patients (King et al. 2003, Kaushal et al. 2008). The definition of pediatric patients occasionally differed per paper. For example, Shah et al. 2009 included patients until the age of 20 while most studies defined the pediatric population as those less than 18 years of age. Lastly, the only articles included were in English.
4.1. Conclusions
In summary, there are important considerations to make for pediatric patients in particular. It is vital to establish universal definitions of error including a taxonomy, and to use the most sensitive study methods. In order to minimize error and improve safety, medicine can also further explore lessons previously learned from other industries.
Supplementary Material
Acknowledgements:
Xizhao Chen BS, Stephany Vittitow BA, Karen Knight MSLS, Elaine Attridge MLS
Footnotes
Declarations of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Published online 2000. [PubMed] [Google Scholar]
- 2.Dzau VJ, Shine KI. Two Decades Since To Err Is Human: Progress, but Still a “Chasm.” JAMA. 2020;324(24):2489–2490. doi: 10.1001/jama.2020.23151 [DOI] [PubMed] [Google Scholar]
- 3.Anderson O, Davis R, Hanna GB, Vincent CA. Surgical adverse events: a systematic review. Am J Surg. 2013;206(2):253–262. doi: 10.1016/j.amjsurg.2012.11.009 [DOI] [PubMed] [Google Scholar]
- 4.Hempel S, Maggard-Gibbons M, Nguyen DK, et al. Wrong-Site Surgery, Retained Surgical Items, and Surgical Fires : A Systematic Review of Surgical Never Events. JAMA Surg. 2015;150(8):796–805. doi: 10.1001/jamasurg.2015.0301 [DOI] [PubMed] [Google Scholar]
- 5.Treadwell JR, Lucas S, Tsou AY. Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf. 2014;23(4):299–318. doi: 10.1136/bmjqs-2012-001797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothschild JM, Keohane CA, Cook EF, et al. A controlled trial of smart infusion pumps to improve medication safety in critically ill patients. Crit Care Med. 2005;33(3):533–540. doi: 10.1097/01.ccm.0000155912.73313.cd [DOI] [PubMed] [Google Scholar]
- 7.Hale AR, Coombes ID, Stokes J, et al. Perioperative medication management: expanding the role of the preadmission clinic pharmacist in a single centre, randomised controlled trial of collaborative prescribing. BMJ Open. 2013;3(7). doi: 10.1136/bmjopen-2013-003027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weerakkody RA, Cheshire NJ, Riga C, et al. Surgical technology and operating-room safety failures: a systematic review of quantitative studies. BMJ Qual Saf. 2013;22(9):710–718. doi: 10.1136/bmjqs-2012-001778 [DOI] [PubMed] [Google Scholar]
- 9.Taber DJ, Spivey JR, Tsurutis VM, et al. Clinical and economic outcomes associated with medication errors in kidney transplantation. Clin J Am Soc Nephrol CJASN. 2014;9(5):960–966. doi: 10.2215/CJN.09300913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Unal AE, Bayar S, Arat M, Ilhan O. Malpositioning of Hickman catheters, left versus right sided attempts. Transfus Apher Sci Off J World Apher Assoc Off J Eur Soc Haemapheresis. 2003;28(1):9–12. doi: 10.1016/S1473-0502(02)00094-0 [DOI] [PubMed] [Google Scholar]
- 11.Wood KB, Devine J, Fischer D, Dettori JR, Janssen M. Vascular injury in elective anterior lumbosacral surgery. Spine. 2010;35(9 Suppl):S66–75. doi: 10.1097/BRS.0b013e3181d83411 [DOI] [PubMed] [Google Scholar]
- 12.Rassweiler MC, Mamoulakis C, Kenngott HG, Rassweiler J, de la Rosette J, Laguna MP. Classification and detection of errors in minimally invasive surgery. J Endourol. 2011;25(11):1713–1721. doi: 10.1089/end.2011.0068 [DOI] [PubMed] [Google Scholar]
- 13.Shin M-H, Hur J-W, Ryu K-S, Park C-K. Prospective Comparison Study Between the Fluoroscopy-guided and Navigation Coupled With O-arm-guided Pedicle Screw Placement in the Thoracic and Lumbosacral Spines. J Spinal Disord Tech. 2015;28(6):E347–351. doi: 10.1097/BSD.0b013e31829047a7 [DOI] [PubMed] [Google Scholar]
- 14.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32. [Google Scholar]
- 15.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci IS. 2010;5:69. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48. doi: 10.1186/1471-2288-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howick J, Phillips B, Ball C, et al. Oxford Centre for Evidence-Based Medicine: Levels of Evidence. Centre for Evidence-Based Medicine. Published March2009. Accessed October 1, 2020. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 [Google Scholar]
- 19.Leape LL. Error in medicine. JAMA. 1994;272(23):1851–1857. [PubMed] [Google Scholar]
- 20.Reason JT. Human error. Camb MA Camb Univ Press. Published online 1990. [Google Scholar]
- 21.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Published online 2000. [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality. AHRQ’s Patient Safety Initiative: Building Foundations, Reducing Risk. Published online December 2003. http://archive.ahrq.gov/research/findings/final-reports/pscongrpt/psini2.htm [Google Scholar]
- 23.World Health Organization, WHO Patient Safety. The Conceptual Framework for the International Classification for Patient Safety (ICPS). Published online 2010. https://www.who.int/patientsafety/taxonomy/icps_full_report.pdf [Google Scholar]
- 24.Leape LL, Brennan TA, Laird N, et al. The Nature of Adverse Events in Hospitalized Patients: Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384. doi: 10.1056/NEJM199102073240605 [DOI] [PubMed] [Google Scholar]
- 25.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324(6):370–376. doi: 10.1056/NEJM199102073240604 [DOI] [PubMed] [Google Scholar]
- 26.Agency for Healthcare Research and Quality. Never Events. Patient Safety Primer. Published September 7, 2019. Accessed October 1, 2020. https://psnet.ahrq.gov/primer/never-events [Google Scholar]
- 27.NORC at the University of Chicago ILLI. Americans’ Experiences with Medical Errors and Views on Patient Safety. Published online 2017. http://www.ihi.org/about/news/Documents/IHI_NPSF_NORC_Patient_Safety_Survey_2017_Final_Report.pdf [Google Scholar]
- 28.El-Shafy IA, Delgado J, Akerman M, Bullaro F, Christopherson NAM, Prince JM. Closed-Loop Communication Improves Task Completion in Pediatric Trauma Resuscitation. J Surg Educ. 2018;75(1):58–64. doi: 10.1016/j.jsurg.2017.06.025 [DOI] [PubMed] [Google Scholar]
- 29.Gerstle CR. Parallels in safety between aviation and healthcare. J Pediatr Surg. 2018;53(5):875–878. doi: 10.1016/j.jpedsurg.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 30.Panagopoulos I, Atkin C, Sikora I. Lean Six-Sigma in Aviation Safety: An implementation guide for measuring aviation system’s safety performance. J Saf Stud. 2016;2(2):30. doi: 10.5296/jss.v2i2.10438 [DOI] [Google Scholar]
- 31.Poole RL, Carleton BC. Medication errors: neonates, infants and children are the most vulnerable! J Pediatr Pharmacol Ther JPPT Off J PPAG. 2008;13(2):65–67. doi: 10.5863/1551-6776-13.2.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.