Abstract
Most iliac artery aneurysms occur in association with aortic aneurysms. Isolated aneurysms of the iliac arteries are uncommon, and those of the external iliac arteries are even more rare. In the present report, we have presented the case of a bilateral external iliac artery aneurysm in a young man.
Keywords: Aneurysms, External iliac artery, Solitary iliac artery aneurysms
Aneurysms of the external iliac artery (EIA) are rare, with few case series reported.1, 2, 3, 4, 5 Some studies of autopsies showed that <1% of cases of iliac aneurysms correspond with external iliac aneurysm. Others have reported no findings of this aneurysm in series of cases analyzed for more than one decade.1, 2, 3,6 In the present report, we have described the case of a young man who had presented with pain in the left hip region. During the investigation, he was found to have aneurysms of the external iliac arteries, with a bilateral presentation, with the left one of large proportions. The patient provided written informed consent for the report of his case and imaging studies.
Case report
A young male patient, aged 31 years, had undergone outpatient magnetic resonance imaging of the left hip to investigate pain in this region that had spread to the left lower limb, especially during physical exercise. He was referred to the hospital emergency service because of the finding of a large left EIA aneurysm (EIAA). The patient had no comorbidities, was not chronically taking any regular medication, was healthy, and had regular physical activity. He also denied any recent or previous trauma.
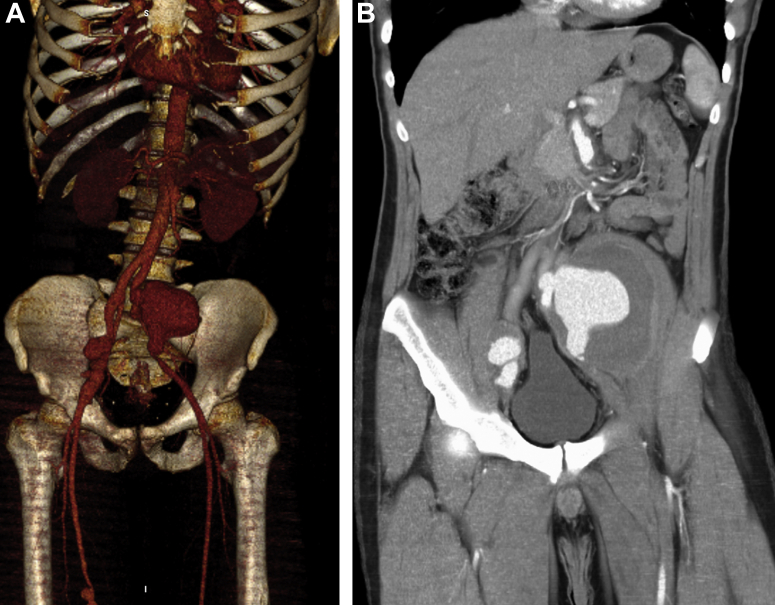
During the investigation, computed tomography angiography was performed, which showed a fusiform aneurysm of the right EIA measuring 3.5 cm in diameter, a fusiform aneurysm of the left EIA measuring 11 cm, a fusiform aneurysm of the superior mesenteric artery measuring 2.3 cm, and an aneurysm of the right common femoral artery (CFA) in its proximal portion measuring 1.5 cm in diameter (Fig). Also, a saccular aneurysm of the right and left superficial femoral arteries was found, at 1.5 cm and 1.2 cm in diameter, respectively. No other aneurysms were found. The case was discussed with the patient and his family, including the need for treatment using conventional open surgery.
Fig.
A, Three-dimensional reconstruction of computed tomography angiogram demonstrating bilateral external iliac artery (EIA) aneurysms (EIAAs), superior mesenteric artery aneurysm, right common femoral artery aneurysm, and femoral artery aneurysm. B, Coronal section computed tomography angiogram of the abdomen and pelvis showing large left and right external iliac artery aneurysms.
The decision for conventional surgery instead of endovascular treatment was determined by the morphology of the aneurysms in the EIA, which were large and tortuous. Thus, the use of a bifurcated stent-graft to preserve the internal iliac arteries was not feasible because the patient was a young man. In addition, the risk of some form of erectile dysfunction and claudication was considered. Open surgery was also chosen because of the compressive symptoms caused by the dimensions of the aneurysms.
Conventional surgical repair was performed using transperitoneal access, with an 8-mm polytetrafluoroethylene prosthesis on the right and reconstruction of the right EIA with an end-to-end anastomosis. The proximal anastomosis was close to the iliac bifurcation and the distal anastomosis to the right CFA, in its proximal portion. Thus, the proximal anastomosis corrected both the aneurysm of the EIA, which was degenerating beyond the inguinal ligament, and the aneurysm of the CFA. On the left, the giant aneurysm was repaired with a 10-mm polytetrafluoroethylene bypass on the left EIA using an end-to-end anastomosis. The aneurysm was tightly adherent to the left ureter, which required resection and reconstruction with the insertion of a double-J catheter. Fragments of the aneurysm wall and its thrombus were sent for analysis, and the bacterial and fungal culture results were negative. The blood and urine culture results were also negative.
The anatomicopathologic analysis revealed the presence of atherosclerotic degeneration of the wall. The patient underwent investigation for rheumatologic diseases, such as connective tissue disorders, also with negative results. He had no family history of aneurysms or rheumatologic disease.
The patient experienced good progress after surgery and was discharged from the hospital after 9 days. He had no postoperative complications but had remained in the hospital for monitoring of his renal function and the presence of hematuria. He was followed up on an outpatient basis by the urologist, who removed the double-J catheter after 30 days. Follow-up computed tomography angiography showed patent bypasses and good contrast flow through the ureters. He was able to return to physical activity without compressive pain complaints.
Because of the magnitude of the surgery, we had decided not to repair the other aneurysms at the same procedure. During follow-up, the need for the repair of the other aneurysms was discussed and scheduled. These were planned to be performed conventionally with a vein bypass. However, the patient was no longer able to be followed up because of problems with his health insurance. Thus, the repair was not performed until the current presentation.
Discussion
Isolated aneurysms of the iliac arteries are rare and estimated to represent <2% of intra-abdominal aneurysms. In contrast, aneurysms of the EIA have been reported to have an even lower incidence.1, 2, 3, 4, 5, 6, 7, 8 In 1921, Lucke and Rea1 reported a study of 12,000 autopsies performed over a period of 40 years, in which only one iliac artery aneurysm was found and was located in the internal iliac artery.1 Garland,3 in 1932, in his review of 167 autopsies to study the pathology of aneurysms, reported no aneurysms of the EIA, demonstrating the rarity of this type of aneurysm. Since then, other studies reported over the years have confirmed the rarity of EIAA.4,5,8, 9, 10 Brunkwall et al,6 in 1989, reported a study in which they had reviewed 26,251 autopsy records from the pathology department of Malmo General Hospital. They found 1267 aneurysms of the aortoiliac system, 170 combined aortic and iliac aneurysms, and 7 solitary aneurysms of the iliac system, only 1 of which was from the EIA. They estimated that solitary aneurysms of the iliac arteries represented 0.03% in the general population.6 The symptoms of iliac artery aneurysms, owing to their location inside the pelvic cavity, have a variety of presentations. They can be asymptomatic and diagnosed incidentally or can lead to the suspicion of other pathologies, such as appendicitis, limb pain, low back pain, and urinary tract pathologies. However, they can also rupture, with the patient presenting with hemorrhagic shock.2,6,10 Atherosclerosis has been the etiology most reported in previous studies. However, other etiologies have been reported for aneurysms of the iliac arteries, such as collagen diseases, vasculitis, infections (eg, mycotic and syphilitic), and trauma.2, 3, 4,6,8, 9, 10 Owing to the rarity of EIAAs, few cases have been reported, none with a bilateral presentation. In 1952, Priddle11 reported the case of a pregnant patient who had presented with abdominal pain, left lower limb pain, and transvaginal bleeding. A ruptured EIAA was diagnosed intraoperatively and required a ligature of the common iliac artery.11 In 1986, Crivello et al12 reported the case of a male patient with an EIAA secondary to cystic medial necrosis. In 2019, van de Luijtgaarden and Bhrem13 presented the case of a 65-year-old male patient in whom the EIAA had mimicked May-Thurner syndrome with left lower limb edema. Also in 2019, Hussain and Aziz14 reported the case of a 7-cm diameter EIAA in a 55-year-old male patient. The EIAA was diagnosed incidentally when the patient was in the preoperative setting for mitral valve repair.14 In the present report, we have described the case of a young man, age 31 years. His compressive symptoms were revealed to have been caused by bilateral EIAAs. Investigation for the etiology revealed only the finding of atherosclerosis in the anatomicopathologic analysis. Regardless of the advances in diagnostic imaging techniques, no increase has been found in the incidence of EIAA. Until the presentation of our case, a search of PubMed found only four reported cases of EIAA, none of which had a bilateral presentation.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Lucke B., Rea M.H. Studies on aneurysm: I. General statistical data on aneurysm. JAMA. 1921;77:935–940. [Google Scholar]
- 2.Richardson J.W., Greenfield L.J. Natural history and management of iliac aneurysms. J Vasc Surg. 1988;8:165–171. [PubMed] [Google Scholar]
- 3.Garland H.G. The pathology of aneurysm: a review of 167 autopsies. J Pathol Bacteriol. 1932;35:335–350. [Google Scholar]
- 4.Levi N., Schroeder T.V. Isolated iliac artery aneurysms. Eur J Vasc Endovasc Surg. 1998;16:342–344. doi: 10.1016/s1078-5884(98)80054-3. [DOI] [PubMed] [Google Scholar]
- 5.Sandhu R.S., Pipinos I.I. Isolated iliac artery aneurysms. Semin Vasc Surg. 2005;18:209–215. doi: 10.1053/j.semvascsurg.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Brunkwall J., Hauksson H., Bengtsson H., Bergqvist D., Takolander R., Bergentz S.-E. Solitary aneurysms of the iliac arterial system: an estimate of their frequency of occurrence. J Vasc Surg. 1989;10:381–384. doi: 10.1067/mva.1989.13733. [DOI] [PubMed] [Google Scholar]
- 7.Lowry S.F., Kraft R.O. Isolated aneurysms of the iliac artery. Arch Surg. 1978;113:1289–1293. doi: 10.1001/archsurg.1978.01370230079009. [DOI] [PubMed] [Google Scholar]
- 8.Weimann S., Tauscher T., Flora G. Isolated iliac artery aneurysms. Ann Vasc Surg. 1990;4:297–301. doi: 10.1007/BF02009461. [DOI] [PubMed] [Google Scholar]
- 9.Nachbur B.H., Inderbitzi R.G.C., Bär W. Isolated iliac aneurysms. Eur J Vasc Surg. 1991;5:375–381. doi: 10.1016/s0950-821x(05)80169-0. [DOI] [PubMed] [Google Scholar]
- 10.Markowitz A.M., Normlan J.C. Aneurysms of the iliac artery. Ann Surg. 1961;154:777–787. [PMC free article] [PubMed] [Google Scholar]
- 11.Priddle H.D. Rupture of an aneurysm of the left external iliac artery during pregnancy. Am J Obstet Gynecol. 1952;63:461–463. doi: 10.1016/s0002-9378(15)32849-0. [DOI] [PubMed] [Google Scholar]
- 12.Crivello M.S., Porter D.H., Kim U., Critchlow J.F., Scoutt L. Isolated external iliac artery aneurysm secondary to cystic medial necrosis. Cardiovasc Intervent Radiol. 1986;9:139–141. doi: 10.1007/BF02577923. [DOI] [PubMed] [Google Scholar]
- 13.van de Luijtgaarden K.M., Brehm V. External iliac artery aneurysm causing severe venous obstruction. Eur J Vasc Endovasc Surg. 2019;57:739. doi: 10.1016/j.ejvs.2018.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Hussain A.S., Aziz A. Giant external iliac artery aneurysm. Ann Vasc Surg. 2019;58:386.e1–386.e3. doi: 10.1016/j.avsg.2018.11.012. [DOI] [PubMed] [Google Scholar]