Abstract
Sodium-glucose cotransporter-2 (SGLT2) inhibitors have emerged as powerful drugs that can be used to treat heart failure (HF) patients, both with preserved and reduced ejection fraction and in the presence or absence of type 2 diabetes. While the mechanisms underlying the salutary effects of SGLT2 inhibitors have not been fully elucidated, there is clear evidence for a beneficial metabolic effect of these drugs. In this review, we discuss the effects of SGLT2 inhibitors on cardiac energy provision secondary to ketone bodies, pathological ventricular remodeling, and inflammation in patients with HF. While the specific contribution of ketone bodies to the pleiotropic cardiovascular benefits of SGLT2 inhibitors requires further clarification, ketone bodies themselves may also be used as a therapy for HF.
Keywords: Sodium-glucose transporter 2 inhibitors, Ketone bodies, Heart failure, Inflammation, Ventricular remodeling
INTRODUCTION
Heart failure (HF) is a devastating condition that affects 40 million people worldwide. The prevalence of HF is reaching epidemic proportions, at least partially explained by the global burden of cardiovascular risk factors and population aging.1,2,3,4,5 In the past decades, advances in medical and device-based therapy have considerably improved outcomes for HF patients.6 Nevertheless, the mortality rates continue to be very high.7 For instance, a recent meta-analysis demonstrated that the 10-year survival rate of HF is only 34.9%, irrespective of the cause of HF.8
Pharmacotherapy remains the cornerstone of HF treatment, and several powerful new therapeutic opportunities have recently emerged,9 such as angiotensin-neprilysin receptor inhibitors (ARNi),10 sodium-glucose cotransporter-2 (SGLT2) inhibitors, omecamtiv mecarbil (INN),11 and vericiguat.12 Of these, SGLT2 inhibitors have arguably provided the most impressive and consistent benefits across the HF spectrum, coupled with an exceptional safety profile.13 This feature is all the more remarkable because SGLT2 inhibitors were initially designed as antidiabetic drugs, and recent antidiabetic drugs have paradoxically increased the incidence of cardiovascular events.14,15
Despite taking the HF world by storm, the mechanism responsible for the beneficial effects on HF outcomes is not fully understood and is often debated. Multiple mechanisms have been proposed,16,17,18 including metabolic, diuretic, and pleiotropic off-target effects.19,20 The current review will discuss a prevailing theory in which SGLT2 inhibitors provide the failing heart with an additional energy source, secondary to an increase in circulating ketone bodies.16,21,22
SGLT2 INHIBITORS
The first SGLT inhibitor was isolated from the bark of apple trees, evoking the aphorism “an apple a day keeps the doctor away”.23,24 Nevertheless, the connection between the benefit of SGLT2 inhibitors and HF is a serendipitous story.23,24 SGLT2 inhibitors were designed as antidiabetic drugs because they block glucose reabsorption in the proximal renal tubules, resulting in renal excretion of glucose; promoting glycosuria, they cause a mild insulin-independent reduction in serum glucose levels.25
Phlorizin, the first-discovered unselective SGLT1/SGLT2 inhibitor, was discovered in 1835 and was used to treat malaria, nephritis, and sarcoma. It was also noted that phlorizin promoted glucosuria and decreased plasma glucose levels.26,27 However, high doses were required to achieve glucosuria, often offset by severe diarrhea.28 More recently, the stability, specificity, and selectivity of SGLT2 inhibitors have been considerably improved, resulting in modern SGLT2 inhibitors with favorable safety characteristics such as dapagliflozin,29 canagliflozin,30 ertugliflozin,31 sotaglifozin,32 and empagliflozin.33 The main differences lie in their selectivity. For example, while canagliflozin is 250-fold more selective for SGLT2 than SGLT1, empagliflozin is the most selective, exceeding 2,500-fold.33,34
These compounds are all registered antidiabetic agents that were approved by the United States Food and Drug Administration (FDA) to manage type 2 diabetes mellitus (T2DM) in 2008 and by the European Medicines Agency (EMA) in 2012.28,35
CARDIOVASCULAR EFFECTS OF SGLT2 INHIBITORS
Following the discovery that dipeptidyl peptidase-4 increases ischemic cardiovascular risk,14 the monitoring of HF outcomes is currently mandatory in the USA during the clinical development of new antidiabetic therapies. Surprisingly, the safety analysis of the EMPA-REG OUTCOME trial published in 2015 demonstrated that empagliflozin resulted in a significant reduction in HF hospitalizations.36 Furthermore, a similar reduction in HF hospitalizations in patients with T2DM was observed with canagliflozin30 and dapagliflozin in the DECLARE-TIMI 58 trial,37 suggesting a class effect.35
A possible beneficial effect of these drugs in patients with HF was quickly hypothesized. Subsequently, this benefit in cardiovascular events was confirmed in HF patients with or without diabetes through clinical trials, such as DAPA-HF,38,39 EMPEROR-Reduced,40 EMPEROR-Preserved,41 and SOLOIST-WHF.32 More recently, systematic reviews with meta-analyses revealed that the beneficial effects of SGLT2 inhibitors in HF are comparable in patients with and without diabetes (hazard ratio [HR], 0.77; 95% confidence interval [CI], 0.71–0.83 and HR, 0.75; 95% CI, 0.65–0.87, respectively).42
Within a decade since the first clinical trial in diabetes, SGLT2 inhibitors are now recommended as the first-line therapy for patients with HF with reduced ejection fraction (HFrEF).6 Furthermore, SGLT2 inhibitors have been shown to reduce HF hospitalization and mortality in patients with HF with preserved ejection fraction (HFpEF).41
KETOGENESIS
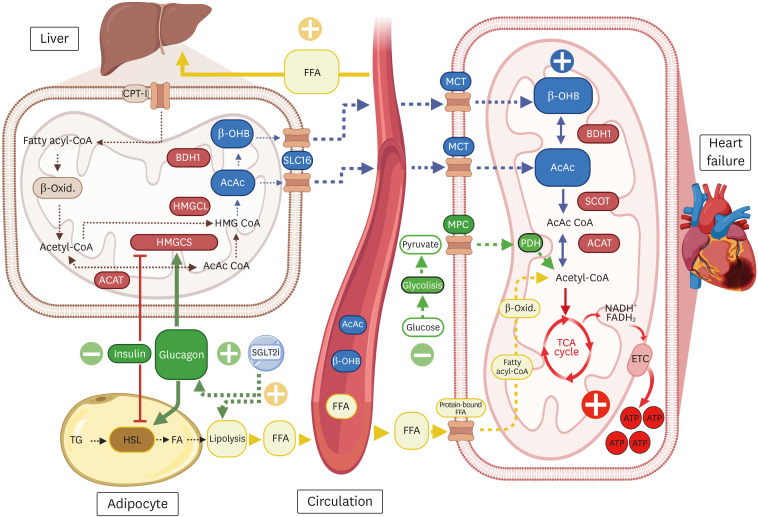
Ketogenesis is a metabolic pathway that generates ketone bodies, predominantly in the liver.43 First, free fatty acids (FFA) are converted to acetyl-coenzyme A (CoA) via mitochondrial β-oxidation. Acetyl-CoA is condensed with acetoacetyl-CoA via 3-methylglutaryl-CoA synthase 2 (HMGCS2) to generate 3-hydroxy 3-methylglutaryl-CoA (HMGC), and later converted by HMGC lyase to acetoacetate (AcAc). AcAc is then reduced by D-b-hydroxybutyrate dehydrogenase (BDH1) to generate 3-hydroxybutyrate (β-OHB), which is released into the circulation by the solute carrier 16A family on hepatocytes.44,45,46,47 β-OHB consequently enters the myocyte mitochondria via monocarboxylic acid transporter 1/2 (MCT1/2)46,47 and is converted back to AcAc by BDH1,48 subsequently transformed into acetoacetyl-CoA by succinyl-CoA, 3-ketoacid-CoA transferase/3-oxoacid CoA-transferase 1 (SCOT/OXCT1), and finally by conversion of mitochondrial acetoacetyl-CoA thiolase into two acetyl-CoA molecules that enter the tricarboxylic acid (TCA) cycle to produce ATP (Fig. 1).49
Fig. 1. Energy production through SGLT2 inhibitors and ketone bodies.
By reducing plasma glucose levels due to increased insulin sensitivity and enhanced gluconeogenesis, the mobilization of deposits of FFA to the liver increases secondary to HSL stimulation. In the liver, FFA are oxidized, generating acetyl-CoA. Two acetyl-CoA derived from FFA are used to produce acetoacetyl-CoA by a thiolase reaction; another acetyl-CoA is condensed into acetoacetyl-CoA by HMGCS2 (this synthase is inhibited by insulin and stimulated by glucagon). After HMGC, it is lysed by HMGCL, generating AcAc, which is oxidized by BDH1 to generate β-OHB. The latter two substances are probably released into circulation through SCL16. Myocytes take up ketone bodies through MCT. β-OHB is converted to AcAc again to be metabolized to acetoacetyl-CoA by SCOT; subsequently, through ACAT, acetyl-CoA is generated to enter the TCA cycle and produce ATP. The image was created with BioRender.com.
ACAT, acetoacetyl-CoA thiolase; AcAc, acetoacetate; ATP, adenosine triphosphate; BDH1, β-hydroxybutyrate dehydrogenase-1; CPT-I, carnitine palmitoyltransferase 1; ECT, electron transport chain; FA, fatty acid; FFA, free fatty acids; HMGCS2, 3-methylglutaryl-CoA synthase 2; HMGC, 3-hydroxy 3-methylglutaryl-CoA; HMGCL, 3-hydroxy 3-methylglutaryl-CoA lyase; HSL, hormone-sensitive lipase; MCT, monocarboxylate transporter; MPC, mitochondrial pyruvate carrier; PDH, pyruvate dehydrogenase; SCL16, solute carrier 16A family members; SGLT2i, sodium-glucose cotransporter-2 Inhibitors; SCOT, succinyl-CoA: 3-ketoacid coenzyme A transferase; TCA, tricarboxylic acid; TG, triglyceride; β-OHB, β-hydroxybutyrate; β-Oxid, β-oxidation.
REGULATION OF KETOGENESIS
Ketone bodies are considered evolutionarily conserved fuels for cellular metabolism designed to provide energy during periods of nutritional stress, such as starvation.49,50 Ketone bodies are mainly generated in the liver,48,51 with minor if any production of ketone bodies in the kidney and the retinal pigment epithelium.49,52,53,54 Ketogenesis is sensitive to multiple hormonal stimuli released during physiological and pathological stress conditions, the most important of which is insulin. In the presence of insulin,49,55 lipolysis is reduced, and the ketogenetic flux in the liver is diminished.56 Conversely, catecholamines (norepinephrine and epinephrine) stimulate lipolysis and, subsequently, ketogenesis.57 Natriuretic peptides (NPs) also stimulate lipolysis.58,59,60,61 Type B natriuretic peptide (BNP), a central peptide in the diagnosis and treatment of HF, has been shown to correlate with circulating total ketone body levels.62 This suggests that BNP is secreted from the heart under stress to promote lipolysis and ketogenesis and provide an endogenous fuel surge during hemodynamic stress.58
Atrial natriuretic peptide (ANP) activates hormone-sensitive lipase (HSL) in adipocytes; as a result, it increases lipolysis and mobilizes FFA from adipose tissue deposits to the liver.59,63 ANP is now increasingly recognized as a metabolic hormone that controls lipid metabolism and energy expenditure.61 However, whether its lipolytic effects also translate into a ketogenic effect has not been well described.
The myocardium is the largest consumer of ketone bodies per unit mass44,64,65 and follows a pattern of circadian oscillations.66 In overnight-fasted adults, total ketone body concentrations are approximately 0.1–0.4 mM64 and tend to increase 1–8 mM during prolonged fasting, extreme physical activity, and insulin deprivation.65,66,67,68,69 Ketosis is defined as a β-OHB concentration above 0.5 mM.18,51 Chu et al.70 recently proposed that the ideal therapeutic β-OHB concentration is 1–3 mM, which may be achieved with treatment with SGLT2 inhibitors. However, the available clinical evidence suggests that the ketogenic effects of SGLT2 inhibitors are less pronounced.71
THE PHYSIOLOGICAL ROLE OF KETONE BODIES IN THE HEART
The heart requires tremendous amounts of ATP, for which it primarily depends on the oxidation of fatty acids (60%–90%), followed by glucose at 10%–30%. Finally, ketone bodies contribute up to 5% of total ATP under normal conditions.20,72,73 The most abundant systemic ketone body is β-OHB. The amount of cardiac ketone body oxidation is strongly correlated with its circulating concentrations, and a dramatic spare capacity for ketone body oxidation exists.48,72 Of note, when concentrations reach 2.0 mM in ex vivo perfused hearts, ketone bodies become the primary source of fuel.74
Ketone bodies in HF
In HF, ketone body concentrations are increased in the circulation of patients with acute and chronic HF, both with reduced and preserved ejection fraction75 and also in animal models.72,76,77 Furthermore, it has been postulated that the increase in ketone body production reflects an autonomous response to cardiac stress in HF that is mediated by NPs and other neurohormones.58
A myocardial energy deficit has been well described in patients with HF, and it is attributed to a progressive diminution of FFA and glucose oxidation, the “energy-starved heart” theory.78 ATP production in advanced HF is reduced by approximately 30%–40%,79 associated with losses of high-energy phosphates and creatine kinase activity that reduce the delivery of ATP to the myofibrils.80,81 In this context, the HF-induced increase in ketone body levels is considered to be adaptive for several reasons82,83,84,85: 1) ketone body oxidation does not influence the oxidation rates of fatty acids (FA) or glucose; thus, ketone bodies provide an additional source fuel72,84,86,87; 2) because the failing heart is considered to be oxygen-deprived and ketone bodies are more oxygen-efficient than FA, multiple authors have referred to ketones as super-fuels, although their oxygen efficiency is lower than glucose48; and 3) there is a linear relationship between circulating ketone body concentrations and extraction by the heart muscle,20,22,85,88 suggesting that there is an impressive spare capacity for ketone body oxidation that can be used to refuel the failing heart.20
The increase in ketone body oxidation is accompanied by a parallel increase in the cardiac expression of the ketolytic enzymes BDH1 and SCOT.48,49 Furthermore, in models with cardio-specific deletion of BDH1 and SCOT, the severity of HF increases.76,89 In contrast, transgenic animal models with BDH1 overexpression and increased afterload revealed increased ketone oxidation, decreased oxidative stress, and consequent protection against adverse cardiac remodeling.77
Mechanism of ketogenesis by SGLT2 inhibitors
The mechanism by which SGLT2 inhibitors increase ketone body concentrations is not entirely understood.25,87 By decreasing plasma glucose levels90 secondary to increased insulin sensitivity in muscle tissue and endothelium,91,92 glucagon levels increase (thereby decreasing the insulin/glucagon ratio), mobilizing fat deposits towards the liver through the stimulation of HSL.93,94 In the liver, FFA are oxidized to acetyl-CoA to generate energy.35,95,96 However, when gluconeogenesis increases and glucose levels are low, acetyl-CoA is redirected from the TCA cycle to produce ketone bodies (AcAc or β-OHB).95
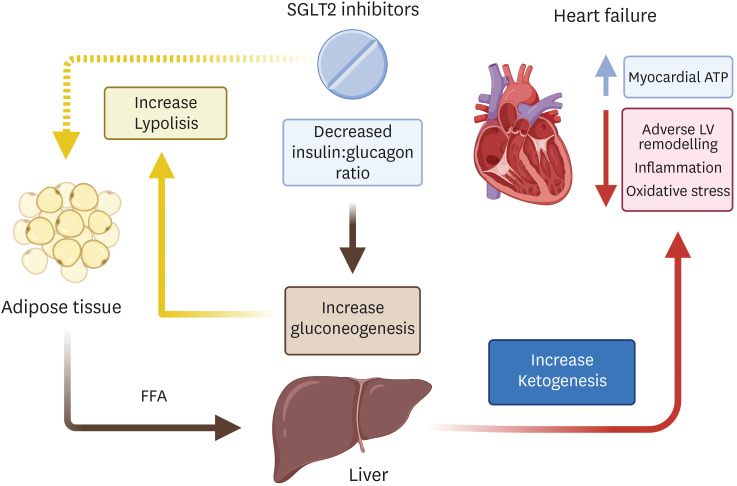
This shift in fuel consumption from glucose to fat oxidation87,97 leads to a decreased insulin-to-glucagon ratio, which enhances gluconeogenesis,90,95 promotes lipolysis,25,98,99,100,101 and facilitates ketogenesis (Fig. 2).
Fig. 2. Mechanism of ketogenesis by SGLT2 inhibitors.
SGLT2 inhibitors increase lipolysis, gluconeogenesis, and ketogenesis by decreasing the insulin-to-glucagon ratio and increasing myocardial ATP content, providing extra fuel to a starved and falling heart. This image was created with BioRender.com.
ATP, adenosine triphosphate; FFA, free fatty acids; LV, left ventricular; SGLT2, sodium-glucose cotransporter-2.
Ketone body levels with SGLT2 administration
Since improvements in cardiac energetic efficiency have been attributed to ketone bodies, they have been called a “super-fuel”48 and “thrifty substrate”.22 Thus, it is attractive to hypothesize that the increased bioavailability of ketones and the use of ketone bodies by the myocardium observed during SGLT2 inhibitor therapy102 could explain the cardiovascular benefits observed in HFrEF and HFpEF in clinical trials (Table 1). However, it should be noted that experimental and clinical evidence comparing the ketogenic effects of different SGLT2 inhibitors currently remains sparse.
Table 1. Relationship of the use of SGLT2 inhibitors and ketone bodies in pre-clinical and clinical studies.
| Reference | SGLT2 inhibitor | Model | HF | Diabetes | Ketone body measured | Outcome |
|---|---|---|---|---|---|---|
| Al Jobori et al. 90 | EMPA | Human | No | T2DM and non-diabetic | β-OHB (µmol/L) | Significant increase in glucagon, FFA and β-OHB in T2DM vs. non-diabetic |
| Polidori et al. 103 | CANA | Human | No | T2DM | β-OHB and acetoacetate (µmol/L) | Increases in ketone bodies that were greater than other metabolic measures in patients with T2DM |
| Ferrannini et al. 87 | EMPA | Human | No | T2DM and non-diabetic | β-OHB (µmol/L) | Lower insulin to glucagon ratio favours ketogenesis. T2DM patients doubled fasting β-OHB levels |
| Daniele et al. 97 | DAPA | Human | No | T2DM | β-OHB and acetoacetate (µmol/L) | DAPA caused a shift from glucose to lipid oxidation and increased plasma ketone bodies concentration |
| Inagaki et al. 104 | CANA | Human | No | T2DM | Total ketone body (μmol/L) | Canagliflozin is tolerated by patients irrespective of their BMI, and total ketone body ≥ 1,000 μmol/L tented to be highest in patients with BMI ≤ 22 kg/m2 |
| Oldgren et al. 105 | DAPA | Human | No | T2DM | β-OHB (µmol/L) | No differences in plasma levels of β-OHB between DAPA vs the placebo group. DAPA reduced heart work but limited effects on myocardial function |
| Yabe et al. 106 | LUSEO | Human | No | T2DM | Ketone bodies (μmol/L) | Ketone bodies were significantly higher in the low carbohydrate and high glycaemic index diet |
| Verma et al. 107 | EMPA | C57BL/6J and db/db mice | No | Mouse surrogates for diabetes (db/db mice) | Total ketone body (μmol/L) | EMPA treatment is associated with an increase in ATP production but did not increase cardiac efficiency |
| Yurista et al. 102 | EMPA | Sprague-Dawley rats | Yes (MI) | Non-diabetic | Total ketone body (μmol/L) | EMPA increases circulating levels of total ketone body, increase ATP production and improves LVEF and cardiac remodelling |
| Santos-Gallego et al. 21 | EMPA | Yorkshire pigs | Yes (MI) | Non-diabetic | Total ketone bodies myocardial uptake (ng/g/min) | EMPA switches myocardial fuel to ketone bodies, FFA and BCAA. It also ameliorates adverse cardiac remodelling and improves LV systolic function |
| Moellmann et al. 108 | EMPA | Male db/db mice | Yes (DD) | Mouse surrogates for diabetes (db/db mice) | β-OHB and acetoacetate (µmol/L) | EMPA improves diastolic function regardless of changes in cardiac ketone body metabolism |
| Connelly et al. 109 | EMPA | Sprague-Dawley rats | Yes (DD) | Non-diabetic | β-OHB (µmol/d) | β-OHB does not differ in EMPA compared to the control group but improves LV mass and improves diastolic dysfunction |
ATP, Adenosine triphosphate; BCAA, branched-chain amino acids; BMI, body mass index; CANA, canagliflozin; DAPA, dapagliflozin; DD, diastolic dysfunction; EMPA, empagliflozin; FFA, free fatty acids; HF, heart failure; LUSEO, luseogliflozin; LV, left ventricle; LVEF, left ventricle ejection fraction; MI, myocardial infarction; SGLT2, sodium/glucose cotransporter-2; T2DM, type 2 diabetes mellitus; β-OHB, β-hydroxybutyrate.
In an animal HF model, Yurista et al.102 demonstrated an increase in β-OHB levels, associated with a significant increase in the expression of BDH1 and SCOT. Santos-Gallego et al.21 also showed increased levels of total ketone bodies in a non-diabetic HF animal model treated with empagliflozin. Moreover, using a non-selective SGLT1/SGLT2 inhibitor, it has been demonstrated that there is an increase in tubular reabsorption of ketone bodies, which contributes to the sustained increment in circulating ketone body levels.110,111,112
The possible mechanism behind the increase in circulating ketone body levels is that treatment with SGLT2 inhibitors produce a metabolic state that resembles the accelerated starvation response (a quicker shift from glucose to FFA oxidation).113 As a consequence of a reduction in glucose oxidation, the mobilization of FA from adipocytes increases and, consequently, the levels of β-OHB and acetoacetate rise significantly.25,95 With long-term SGLT2 inhibitor treatment, ketone body levels double; for β-OHB, the median percent increase is 78% compared to baseline,103 suggesting downstream effects of SGLT2 inhibitors on hepatic metabolism.114
In patients with T2DM, Ferrannini et al.87 Identified an increase in fasting β-OHB of up to 0.56 mmol/L 4 weeks after starting treatment with empagliflozin. Furthermore, Al Jobori et al.90 demonstrated a significant increase in ketone body concentrations and a strong correlation between plasma FFA levels and plasma ketone concentrations in patients with T2DM. Moreover, it has been observed that in patients with a low-carbohydrate diet combined with SGLT2 inhibitors, the increase in ketone bodies is more pronounced than in those consuming high-carbohydrate diets.106 It should be noted that the association between SGLT2-induced ketonemia and the salutary effects observed are descriptive in nature. Future studies—for instance research employing cardiomyocyte-specific knockdown of the BDH1 receptor—are required to define the exact contribution of ketones to the salutary effects of SGLT2 inhibitors.
Ketone bodies as a metabolic biomarker in heart failure
The increase of ketone body levels in HF suggests that they could serve as a prognostic metabolic biomarker. Moreover, a strong correlation has been found between the concentration of ketone bodies and that of BNP.62 Many methods are used to detect elevated ketone body levels, such as blood, urine, and exhaled acetone concentrations in the breath of HF patients.115,116,117,118,119,120
Yokokawa et al.119 found elevated exhaled acetone concentrations in patients with acute HF and observed a decrease in concentrations after treatment and clinical improvement. Furthermore, exhaled acetone concentrations have shown a good correlation with hemodynamic severity (pulmonary capillary wedge pressure ≥18 mmHg) in non-ischemic HF.120 A similar observation is a higher exhaled acetone concentration in stage C of HF than in early stages.121
Other methods have also found a correlation between ketone bodies and HF. For example, in animal models with HF due to cardiotoxicity, using positron emission tomography of the myocardium, [11C]-acetoacetate has been proposed as a possible early marker of damage.122 Moreover, elevated levels of β-OHB in patients with acute HF have been associated with increased mortality using nuclear magnetic resonance spectroscopy, suggesting its prognostic value.123,124
POTENTIAL BENEFITS SECONDARY TO THE ELEVATION OF KETONE BODIES BY SGLT2 INHIBITORS
Increased cardiac energetics
In HF, roadblocks in cardiac substrate metabolism result in impediments in the cardiac capacity to oxidize glucose and FA,20,113 so that the falling heart begins to rely more on ketone bodies and other substrates.22,125,126 Indeed, ketone bodies can account for up to 20% of cardiac metabolism in HF.72 β-OHB has been debated as a “thrifty substrate” because the heart takes it up freely, and it is oxidized in preference to FFA. In addition, Ferrannini et al.22 hypothesized that β-OHB improves work efficiency at the mitochondrial level.
It has been postulated that ketone body oxidation is an additional fuel source72,127 that is energy-efficient22 and has a very high extraction by the heart.20,38,40 Moreover, patients without T2DM with HFrEF who received a continuous infusion of β-OHB showed increases in cardiac output, left ventricular ejection fraction (LVEF), and myocardial oxygen consumption, without altering the myocardial external energy efficiency.16 Furthermore, animal models of myocardial infarction treated with empagliflozin or a ketone ester diet increased circulating ketone body levels and improved left ventricular function.21,102,128 Notwithstanding, different studies have not shown an improvement in cardiac efficiency.20,129
Increasing ketone body levels could be a valuable strategy for treating metabolic dysfunction in HF, and it is reasonable to assume that the low ketonemia level induced by SGLT2 inhibitors19,103,106,107 could improve myocardial energetics and contractile function (Fig. 2). Recently, the EMPA-TROPISM trial demonstrated improvement in left ventricular systolic function in patients with HFrEF without T2DM who received empagliflozin.101 Nevertheless, more evidence is required to determine the degree of the contribution of ketone bodies to energy metabolism and cardiac contractility.
Reversing cardiac remodeling
Adverse cardiac remodeling manifests as changes in sphericity, enlargement, and decreased left ventricular function after cardiac injury.101,130,131 In addition, inflammation, fibrosis, type I collagen levels, and cardiomyocyte cell death are involved in this process19,130,132 and can occur in HFrEF and HFpEF, worsening the prognosis.133 However, it has been shown that reversing cardiac remodeling can reduce mortality and the risk of cardiovascular events.130,134,135 Moreover, Kramer et al.136 have shown a proportional relationship between the effects of drugs or devices on short-term ventricular remodeling and long-term mortality.
Clinical trials such as DAPA-HF,39 EMPEROR-Reduced,40 and EMPA-TROPISM101 have repeatedly shown that SGLT2 inhibitors reverse and improve adverse cardiac remodeling in patients with HFrEF and HFpEF,41,129,137,138 which could explain the observed cardiovascular benefits.38,139 However, since SGLT2 receptors are not expressed in the heart,140 the effect of SGLT2 inhibitors on left ventricular mass is likely indirect and mediated by hemodynamic, anti-inflammatory, and metabolic effects.19,35,129
Various hypotheses have been proposed. The diuretic and natriuretic hypotheses suggest that the sustained reduction in intravascular volume leads to a reduction in preload with consequent improvement in left ventricular systolic and diastolic function.141 This finding was also seen in the EMPA-TROPISM trial, which proved a significant reduction in end-systolic and diastolic volumes and a significant increase in LVEF compared to placebo (6% vs. −0.1%). Furthermore, this hypothesis was also supported by the findings of Mullens et al.,142 who demonstrated a significant decrease in mean pulmonary artery pressure after the initiation of SGLT2 inhibitors.
Another hypothesis suggests that ketone bodies may mitigate pathological remodeling. β-OHB has previously been shown to inhibit class I histone deacetylases, which can inhibit pro-hypertrophic transcription in HF.143,144,145 In addition, overexpression of key enzymes in ketone body oxidation, such as BDH1, protects against cardiac remodeling in models with ischemia or increased afterload.77 Moreover, in the SCOT knockout models, greater pathological remodeling is evidenced,89 suggesting some benefits of ketone bodies in cardiac remodeling. Thus, it is plausible to assume that the increase in levels of ketone bodies following SGLT2 inhibitors can ameliorate pathological remodeling. However, the mechanism is still unknown and requires further elucidation.
Attenuation of the inflammatory profile
Inflammation is central to HF syndrome, and the levels of several circulating inflammatory biomarkers correlate with the prognosis and severity of HF with a reduced or preserved ejection fraction.146,147,148 In particular, the NOD-, LRR-, and pyrin domain-containing protein 3 (NLRP3) inflammasome has recently been recognized as contributing to inflammation in the myocardium of patients with chronic HF and has recently emerged as a new promising target in HF.149,150
In patients with T2DM,151 SGLT2 inhibitors attenuate the activation of the NLRP3 inflammasome and the secretion of interleukin-1β through an increase in β-OHB levels and decreases in insulin and glucose levels, which could improve cardiovascular outcomes.152,153,154 In addition, by decreasing glucose levels, SGLT2 inhibitors minimize the inflammatory response of macrophages.155,156
In HFpEF animal models, it was shown that the increase in β-OHB levels secondary to the use of empagliflozin attenuated the formation of the NLPR3 inflammasome, fibrosis, and mitochondrial dysfunction. As a mechanism, the authors proposed that mitochondrial protein acetylation was diminished due to the decrease in the acetyl-CoA pool through activation of citrate synthase and suppression of fatty acid uptake.157 Thus, this finding suggests that the SGLT2 inhibitor-mediated increase in β-OHB levels may serve as a therapeutic target to mitigate mitochondrial hyperacetylation and inflammation involved in the pathogenesis of HFpEF. Of note, in the EMPEROR-Preserved trial, a significant risk reduction was described with empagliflozin for the combination of cardiovascular death or hospitalization for HF in patients with HFpEF.41
CONCLUSION
SGLT2 inhibitor therapy improves cardiac function and outcomes in patients with HF with or without T2DM, through multiple pleiotropic effects including increased ketone body levels. The increase in ketone body levels appears to reflect an adaptive process that optimizes cardiac energy metabolism and could explain the improvement in overall cardiac function in patients treated with SGLT2 inhibitors.
Moreover, the reduction of adverse cardiac remodeling and fibrosis associated with ketone bodies could improve ventricular diastolic function and may also translate into benefits for patients with HFpEF. The exact contribution of ketone bodies to the cardiovascular benefits of SGLT2 inhibitors is not entirely clear and requires further clarification. Nevertheless, this mechanism of ketone bodies suggests that ketone bodies themselves could represent a new therapeutic option for HF.
Footnotes
Funding: None.
Conflict of Interest: The authors have no conflicts of interest to declare.
- Conceptualization: Saucedo-Orozco H, Westenbrink BD.
- Investigation: Saucedo-Orozco H.
- Methodology: Saucedo-Orozco H, Voorrips SN, Westenbrink BD.
- Supervision: Yurista SR, de Boer RA, Westenbrink BD.
- Writing - original draft: Saucedo-Orozco H.
- Writing - review & editing: Voorrips SN, Yurista SR, de Boer RA, Westenbrink BD.
References
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 3.Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020;22:1342–1356. doi: 10.1002/ejhf.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–ee492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 5.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 6.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. Corrigendum to: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42:4901. doi: 10.1093/eurheartj/ehab670. [DOI] [PubMed] [Google Scholar]
- 7.Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, Kizer JR, et al. Temporal trends in the incidence of and mortality associated with heart failure with preserved and reduced ejection fraction. JACC Heart Fail. 2018;6:678–685. doi: 10.1016/j.jchf.2018.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones NR, Roalfe AK, Adoki I, Hobbs FD, Taylor CJ. Survival of patients with chronic heart failure in the community: a systematic review and meta-analysis. Eur J Heart Fail. 2019;21:1306–1325. doi: 10.1002/ejhf.1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Straw S, McGinlay M, Witte KK. Four pillars of heart failure: contemporary pharmacological therapy for heart failure with reduced ejection fraction. Open Heart. 2021;8:e001585. doi: 10.1136/openhrt-2021-001585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Dual angiotensin receptor and neprilysin inhibition as an alternative to angiotensin-converting enzyme inhibition in patients with chronic systolic heart failure: rationale for and design of the Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure trial (PARADIGM-HF) Eur J Heart Fail. 2013;15:1062–1073. doi: 10.1093/eurjhf/hft052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teerlink JR, Diaz R, Felker GM, McMurray JJV, Metra M, Solomon SD, et al. Cardiac myosin activation with omecamtiv mecarbil in systolic heart failure. N Engl J Med. 2021;384:105–116. doi: 10.1056/NEJMoa2025797. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382:1883–1893. doi: 10.1056/NEJMoa1915928. [DOI] [PubMed] [Google Scholar]
- 13.Writing Committee. Maddox TM, Januzzi JL, Jr, Allen LA, Breathett K, Butler J, et al. 2021 update to the 2017 ACC Expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77:772–810. doi: 10.1016/j.jacc.2020.11.022. [DOI] [PubMed] [Google Scholar]
- 14.Bourg CA, Phillips BB. Rosiglitazone, myocardial ischemic risk, and recent regulatory actions. Ann Pharmacother. 2012;46:282–289. doi: 10.1345/aph.1Q400. [DOI] [PubMed] [Google Scholar]
- 15.Home PD, Pocock SJ, Beck-Nielsen H, Gomis R, Hanefeld M, Jones NP, et al. Rosiglitazone evaluated for cardiovascular outcomes--an interim analysis. N Engl J Med. 2007;357:28–38. doi: 10.1056/NEJMoa073394. [DOI] [PubMed] [Google Scholar]
- 16.Nielsen R, Møller N, Gormsen LC, Tolbod LP, Hansson NH, Sorensen J, et al. Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation. 2019;139:2129–2141. doi: 10.1161/CIRCULATIONAHA.118.036459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gormsen LC, Svart M, Thomsen HH, Søndergaard E, Vendelbo MH, Christensen N, et al. Ketone body infusion with 3-hydroxybutyrate reduces myocardial glucose uptake and increases blood flow in humans: a positron emission tomography study. J Am Heart Assoc. 2017;6:6. doi: 10.1161/JAHA.116.005066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yurista SR, Chong CR, Badimon JJ, Kelly DP, de Boer RA, Westenbrink BD. Therapeutic potential of ketone bodies for patients with cardiovascular disease: JACC focus seminar. J Am Coll Cardiol. 2021;77:1660–1669. doi: 10.1016/j.jacc.2020.12.065. [DOI] [PubMed] [Google Scholar]
- 19.Lopaschuk GD, Verma S. Mechanisms of cardiovascular benefits of sodium glucose co-transporter 2 (SGLT2) inhibitors: a state-of-the-art review. JACC Basic Transl Sci. 2020;5:632–644. doi: 10.1016/j.jacbts.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Honka H, Solis-Herrera C, Triplitt C, Norton L, Butler J, DeFronzo RA. Therapeutic manipulation of myocardial metabolism: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77:2022–2039. doi: 10.1016/S0735-1097(21)03378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, Ishikawa K, Watanabe S, Picatoste B, et al. Empagliflozin Ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J Am Coll Cardiol. 2019;73:1931–1944. doi: 10.1016/j.jacc.2019.01.056. [DOI] [PubMed] [Google Scholar]
- 22.Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME trial: a “Thrifty Substrate” hypothesis. Diabetes Care. 2016;39:1108–1114. doi: 10.2337/dc16-0330. [DOI] [PubMed] [Google Scholar]
- 23.Davis MA, Bynum JP, Sirovich BE. Association between apple consumption and physician visits: appealing the conventional wisdom that an apple a day keeps the doctor away. JAMA Intern Med. 2015;175:777–783. doi: 10.1001/jamainternmed.2014.5466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White JR., Jr Apple trees to sodium glucose co-transporter inhibitors: a review of SGLT2 inhibition. Clin Diabetes. 2010;28:5–10. [Google Scholar]
- 25.Ferrannini E, Muscelli E, Frascerra S, Baldi S, Mari A, Heise T, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124:499–508. doi: 10.1172/JCI72227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chasis H, Jolliffe N, Smith HW. The action of phlorizin on the excretion of glucose, xylose, sucrose, creatinine and urea by man. J Clin Invest. 1933;12:1083–1090. doi: 10.1172/JCI100559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petersen C. Analyse des phloridzins. Ann Acad Sci Fr. 1835;15:178. [Google Scholar]
- 28.Zelniker TA, Braunwald E. Mechanisms of Cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:422–434. doi: 10.1016/j.jacc.2019.11.031. [DOI] [PubMed] [Google Scholar]
- 29.Meng W, Ellsworth BA, Nirschl AA, McCann PJ, Patel M, Girotra RN, et al. Discovery of dapagliflozin: a potent, selective renal sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes. J Med Chem. 2008;51:1145–1149. doi: 10.1021/jm701272q. [DOI] [PubMed] [Google Scholar]
- 30.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–657. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
- 31.Miao Z, Nucci G, Amin N, Sharma R, Mascitti V, Tugnait M, et al. Pharmacokinetics, metabolism, and excretion of the antidiabetic agent ertugliflozin (PF-04971729) in healthy male subjects. Drug Metab Dispos. 2013;41:445–456. doi: 10.1124/dmd.112.049551. [DOI] [PubMed] [Google Scholar]
- 32.Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021;384:117–128. doi: 10.1056/NEJMoa2030183. [DOI] [PubMed] [Google Scholar]
- 33.Scheen AJ. Pharmacokinetic and pharmacodynamic profile of empagliflozin, a sodium glucose co-transporter 2 inhibitor. Clin Pharmacokinet. 2014;53:213–225. doi: 10.1007/s40262-013-0126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grempler R, Thomas L, Eckhardt M, Himmelsbach F, Sauer A, Sharp DE, et al. Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors. Diabetes Obes Metab. 2012;14:83–90. doi: 10.1111/j.1463-1326.2011.01517.x. [DOI] [PubMed] [Google Scholar]
- 35.Cowie MR, Fisher M. SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycaemic control. Nat Rev Cardiol. 2020;17:761–772. doi: 10.1038/s41569-020-0406-8. [DOI] [PubMed] [Google Scholar]
- 36.Tikkanen I, Narko K, Zeller C, Green A, Salsali A, Broedl UC, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care. 2015;38:420–428. doi: 10.2337/dc14-1096. [DOI] [PubMed] [Google Scholar]
- 37.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–357. doi: 10.1056/NEJMoa1812389. [DOI] [PubMed] [Google Scholar]
- 38.McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008. doi: 10.1056/NEJMoa1911303. [DOI] [PubMed] [Google Scholar]
- 39.McMurray JJV, DeMets DL, Inzucchi SE, Køber L, Kosiborod MN, Langkilde AM, et al. A trial to evaluate the effect of the sodium-glucose co-transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA-HF) Eur J Heart Fail. 2019;21:665–675. doi: 10.1002/ejhf.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–1424. doi: 10.1056/NEJMoa2022190. [DOI] [PubMed] [Google Scholar]
- 41.Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–1461. doi: 10.1056/NEJMoa2107038. [DOI] [PubMed] [Google Scholar]
- 42.Lu Y, Li F, Fan Y, Yang Y, Chen M, Xi J. Effect of SGLT-2 inhibitors on cardiovascular outcomes in heart failure patients: a meta-analysis of randomized controlled trials. Eur J Intern Med. 2021;87:20–28. doi: 10.1016/j.ejim.2021.03.020. [DOI] [PubMed] [Google Scholar]
- 43.Dhillon KK, Gupta S. Biochemistry, ketogenesis. StatPearls. Treasure Island (FL): StatPearls; 2021. [Google Scholar]
- 44.Cotter DG, d’Avignon DA, Wentz AE, Weber ML, Crawford PA. Obligate role for ketone body oxidation in neonatal metabolic homeostasis. J Biol Chem. 2011;286:6902–6910. doi: 10.1074/jbc.M110.192369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hugo SE, Cruz-Garcia L, Karanth S, Anderson RM, Stainier DY, Schlegel A. A monocarboxylate transporter required for hepatocyte secretion of ketone bodies during fasting. Genes Dev. 2012;26:282–293. doi: 10.1101/gad.180968.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Halestrap AP. The monocarboxylate transporter family--structure and functional characterization. IUBMB Life. 2012;64:1–9. doi: 10.1002/iub.573. [DOI] [PubMed] [Google Scholar]
- 47.Halestrap AP, Wilson MC. The monocarboxylate transporter family--role and regulation. IUBMB Life. 2012;64:109–119. doi: 10.1002/iub.572. [DOI] [PubMed] [Google Scholar]
- 48.Karwi QG, Biswas D, Pulinilkunnil T, Lopaschuk GD. Myocardial ketones metabolism in heart failure. J Card Fail. 2020;26:998–1005. doi: 10.1016/j.cardfail.2020.04.005. [DOI] [PubMed] [Google Scholar]
- 49.Puchalska P, Crawford PA. Multi-dimensional roles of ketone bodies in fuel metabolism, signaling, and therapeutics. Cell Metab. 2017;25:262–284. doi: 10.1016/j.cmet.2016.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mitchell GA, Kassovska-Bratinova S, Boukaftane Y, Robert MF, Wang SP, Ashmarina L, et al. Medical aspects of ketone body metabolism. Clin Invest Med. 1995;18:193–216. [PubMed] [Google Scholar]
- 51.Volek JS. The art and science of low carbohydrate performance: a revolutionary program to extend your physical and mental performance envelope. Miami (FL): Beyond Obesity LLC; 2012. [Google Scholar]
- 52.Adijanto J, Du J, Moffat C, Seifert EL, Hurle JB, Philp NJ. The retinal pigment epithelium utilizes fatty acids for ketogenesis. J Biol Chem. 2014;289:20570–20582. doi: 10.1074/jbc.M114.565457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tran MT, Zsengeller ZK, Berg AH, Khankin EV, Bhasin MK, Kim W, et al. PGC1α drives NAD biosynthesis linking oxidative metabolism to renal protection. Nature. 2016;531:528–532. doi: 10.1038/nature17184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Puisac B, Ramos M, Arnedo M, Menao S, Gil-Rodríguez MC, Teresa-Rodrigo ME, et al. Characterization of splice variants of the genes encoding human mitochondrial HMG-CoA lyase and HMG-CoA synthase, the main enzymes of the ketogenesis pathway. Mol Biol Rep. 2012;39:4777–4785. doi: 10.1007/s11033-011-1270-8. [DOI] [PubMed] [Google Scholar]
- 55.McGarry JD, Foster DW. Hormonal control of ketogenesis. Biochemical considerations. Arch Intern Med. 1977;137:495–501. [PubMed] [Google Scholar]
- 56.Hegardt FG. Mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase: a control enzyme in ketogenesis. Biochem J. 1999;338:569–582. [PMC free article] [PubMed] [Google Scholar]
- 57.Keller U, Lustenberger M, Müller-Brand J, Gerber PP, Stauffacher W. Human ketone body production and utilization studied using tracer techniques: regulation by free fatty acids, insulin, catecholamines, and thyroid hormones. Diabetes Metab Rev. 1989;5:285–298. doi: 10.1002/dmr.5610050306. [DOI] [PubMed] [Google Scholar]
- 58.Yurista SR, Nguyen CT, Rosenzweig A, de Boer RA, Westenbrink BD. Ketone bodies for the failing heart: fuels that can fix the engine? Trends Endocrinol Metab. 2021;32:814–826. doi: 10.1016/j.tem.2021.07.006. [DOI] [PubMed] [Google Scholar]
- 59.Birkenfeld AL, Boschmann M, Moro C, Adams F, Heusser K, Franke G, et al. Lipid mobilization with physiological atrial natriuretic peptide concentrations in humans. J Clin Endocrinol Metab. 2005;90:3622–3628. doi: 10.1210/jc.2004-1953. [DOI] [PubMed] [Google Scholar]
- 60.Birkenfeld AL, Budziarek P, Boschmann M, Moro C, Adams F, Franke G, et al. Atrial natriuretic peptide induces postprandial lipid oxidation in humans. Diabetes. 2008;57:3199–3204. doi: 10.2337/db08-0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sengenes C, Moro C, Galitzky J, Berlan M, Lafontan M. Natriuretic peptides: a new lipolytic pathway in human fat cells. Med Sci (Paris) 2005;21:29–33. [PubMed] [Google Scholar]
- 62.Kashiwagi Y, Nagoshi T, Inoue Y, Tanaka Y, Takahashi H, Oi Y, et al. Close linkage between blood total ketone body levels and B-type natriuretic peptide levels in patients with cardiovascular disorders. Sci Rep. 2021;11:6498. doi: 10.1038/s41598-021-86126-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sengenes C, Bouloumie A, Hauner H, Berlan M, Busse R, Lafontan M, et al. Involvement of a cGMP-dependent pathway in the natriuretic peptide-mediated hormone-sensitive lipase phosphorylation in human adipocytes. J Biol Chem. 2003;278:48617–48626. doi: 10.1074/jbc.M303713200. [DOI] [PubMed] [Google Scholar]
- 64.Balasse EO, Féry F. Ketone body production and disposal: effects of fasting, diabetes, and exercise. Diabetes Metab Rev. 1989;5:247–270. doi: 10.1002/dmr.5610050304. [DOI] [PubMed] [Google Scholar]
- 65.Cahill GF., Jr Fuel metabolism in starvation. Annu Rev Nutr. 2006;26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258. [DOI] [PubMed] [Google Scholar]
- 66.Wildenhoff KE, Johansen JP, Karstoft H, Yde H, Sorensen NS. Diurnal variations in the concentrations of blood acetoacetate and 3-hydroxybutyrate. The ketone body peak around midnight and its relationship to free fatty acids, glycerol, insulin, growth hormone and glucose in serum and plasma. Acta Med Scand. 1974;195:25–28. [PubMed] [Google Scholar]
- 67.Johnson RH, Walton JL. The effect of exercise upon acetoacetate metabolism in athletes and non-athletes. Q J Exp Physiol Cogn Med Sci. 1972;57:73–79. doi: 10.1113/expphysiol.1972.sp002139. [DOI] [PubMed] [Google Scholar]
- 68.Robinson AM, Williamson DH. Physiological roles of ketone bodies as substrates and signals in mammalian tissues. Physiol Rev. 1980;60:143–187. doi: 10.1152/physrev.1980.60.1.143. [DOI] [PubMed] [Google Scholar]
- 69.Cotter DG, Schugar RC, Crawford PA. Ketone body metabolism and cardiovascular disease. Am J Physiol Heart Circ Physiol. 2013;304:H1060–H1076. doi: 10.1152/ajpheart.00646.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chu Y, Zhang C, Xie M. Beta-hydroxybutyrate, friend or foe for stressed hearts. Front Aging. 2021;2:681513. doi: 10.3389/fragi.2021.681513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pietschner R, Kolwelter J, Bosch A, Striepe K, Jung S, Kannenkeril D, et al. Effect of empagliflozin on ketone bodies in patients with stable chronic heart failure. Cardiovasc Diabetol. 2021;20:219. doi: 10.1186/s12933-021-01410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ho KL, Zhang L, Wagg C, Al Batran R, Gopal K, Levasseur J, et al. Increased ketone body oxidation provides additional energy for the failing heart without improving cardiac efficiency. Cardiovasc Res. 2019;115:1606–1616. doi: 10.1093/cvr/cvz045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murashige D, Jang C, Neinast M, Edwards JJ, Cowan A, Hyman MC, et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science. 2020;370:364–368. doi: 10.1126/science.abc8861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ho KL, Karwi QG, Wagg C, Zhang L, Vo K, Altamimi T, et al. Ketones can become the major fuel source for the heart but do not increase cardiac efficiency. Cardiovasc Res. 2021;117:1178–1187. doi: 10.1093/cvr/cvaa143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Voros G, Ector J, Garweg C, Droogne W, Van Cleemput J, Peersman N, et al. Increased cardiac uptake of ketone bodies and free fatty acids in human heart failure and hypertrophic left ventricular remodeling. Circ Heart Fail. 2018;11:e004953. doi: 10.1161/CIRCHEARTFAILURE.118.004953. [DOI] [PubMed] [Google Scholar]
- 76.Horton JL, Davidson MT, Kurishima C, Vega RB, Powers JC, Matsuura TR, et al. The failing heart utilizes 3-hydroxybutyrate as a metabolic stress defense. JCI Insight. 2019;4:e124079. doi: 10.1172/jci.insight.124079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Uchihashi M, Hoshino A, Okawa Y, Ariyoshi M, Kaimoto S, Tateishi S, et al. Cardiac-specific Bdh1 overexpression ameliorates oxidative stress and cardiac remodeling in pressure overload-induced heart failure. Circ Heart Fail. 2017;10:e004417. doi: 10.1161/CIRCHEARTFAILURE.117.004417. [DOI] [PubMed] [Google Scholar]
- 78.Ingwall JS, Weiss RG. Is the failing heart energy starved? On using chemical energy to support cardiac function. Circ Res. 2004;95:135–145. doi: 10.1161/01.RES.0000137170.41939.d9. [DOI] [PubMed] [Google Scholar]
- 79.Neubauer S. The failing heart--an engine out of fuel. N Engl J Med. 2007;356:1140–1151. doi: 10.1056/NEJMra063052. [DOI] [PubMed] [Google Scholar]
- 80.Weiss RG, Gerstenblith G, Bottomley PA. ATP flux through creatine kinase in the normal, stressed, and failing human heart. Proc Natl Acad Sci U S A. 2005;102:808–813. doi: 10.1073/pnas.0408962102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ye Y, Gong G, Ochiai K, Liu J, Zhang J. High-energy phosphate metabolism and creatine kinase in failing hearts: a new porcine model. Circulation. 2001;103:1570–1576. doi: 10.1161/01.cir.103.11.1570. [DOI] [PubMed] [Google Scholar]
- 82.Abdul Kadir A, Clarke K, Evans RD. Cardiac ketone body metabolism. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165739. doi: 10.1016/j.bbadis.2020.165739. [DOI] [PubMed] [Google Scholar]
- 83.Lopaschuk GD, Karwi QG, Ho KL, Pherwani S, Ketema EB. Ketone metabolism in the failing heart. Biochim Biophys Acta Mol Cell Biol Lipids. 2020;1865:158813. doi: 10.1016/j.bbalip.2020.158813. [DOI] [PubMed] [Google Scholar]
- 84.Bedi KC, Jr, Snyder NW, Brandimarto J, Aziz M, Mesaros C, Worth AJ, et al. Evidence for intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation. 2016;133:706–716. doi: 10.1161/CIRCULATIONAHA.115.017545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huynh K. Heart failure: ketone bodies as fuel in heart failure. Nat Rev Cardiol. 2016;13:122–123. doi: 10.1038/nrcardio.2016.22. [DOI] [PubMed] [Google Scholar]
- 86.Aubert G, Martin OJ, Horton JL, Lai L, Vega RB, Leone TC, et al. The failing heart relies on ketone bodies as a fuel. Circulation. 2016;133:698–705. doi: 10.1161/CIRCULATIONAHA.115.017355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferrannini E, Baldi S, Frascerra S, Astiarraga B, Heise T, Bizzotto R, et al. Shift to fatty substrate utilization in response to sodium-glucose cotransporter 2 inhibition in subjects without diabetes and patients with type 2 diabetes. Diabetes. 2016;65:1190–1195. doi: 10.2337/db15-1356. [DOI] [PubMed] [Google Scholar]
- 88.Sato K, Kashiwaya Y, Keon CA, Tsuchiya N, King MT, Radda GK, et al. Insulin, ketone bodies, and mitochondrial energy transduction. FASEB J. 1995;9:651–658. doi: 10.1096/fasebj.9.8.7768357. [DOI] [PubMed] [Google Scholar]
- 89.Schugar RC, Moll AR, André d’Avignon D, Weinheimer CJ, Kovacs A, Crawford PA. Cardiomyocyte-specific deficiency of ketone body metabolism promotes accelerated pathological remodeling. Mol Metab. 2014;3:754–769. doi: 10.1016/j.molmet.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Al Jobori H, Daniele G, Adams J, Cersosimo E, Triplitt C, DeFronzo RA, et al. Determinants of the increase in ketone concentration during SGLT2 inhibition in NGT, IFG and T2DM patients. Diabetes Obes Metab. 2017;19:809–813. doi: 10.1111/dom.12881. [DOI] [PubMed] [Google Scholar]
- 91.Cherney DZ, Perkins BA, Soleymanlou N, Har R, Fagan N, Johansen OE, et al. The effect of empagliflozin on arterial stiffness and heart rate variability in subjects with uncomplicated type 1 diabetes mellitus. Cardiovasc Diabetol. 2014;13:28. doi: 10.1186/1475-2840-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Merovci A, Solis-Herrera C, Daniele G, Eldor R, Fiorentino TV, Tripathy D, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124:509–514. doi: 10.1172/JCI70704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Akram M. A focused review of the role of ketone bodies in health and disease. J Med Food. 2013;16:965–967. doi: 10.1089/jmf.2012.2592. [DOI] [PubMed] [Google Scholar]
- 94.Laffel L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev. 1999;15:412–426. doi: 10.1002/(sici)1520-7560(199911/12)15:6<412::aid-dmrr72>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 95.Qiu H, Novikov A, Vallon V. Ketosis and diabetic ketoacidosis in response to SGLT2 inhibitors: basic mechanisms and therapeutic perspectives. Diabetes Metab Res Rev. 2017;33:e2886. doi: 10.1002/dmrr.2886. [DOI] [PubMed] [Google Scholar]
- 96.McGarry JD, Foster DW. Regulation of hepatic fatty acid oxidation and ketone body production. Annu Rev Biochem. 1980;49:395–420. doi: 10.1146/annurev.bi.49.070180.002143. [DOI] [PubMed] [Google Scholar]
- 97.Daniele G, Xiong J, Solis-Herrera C, Merovci A, Eldor R, Tripathy D, et al. Dapagliflozin enhances fat oxidation and ketone production in patients with type 2 diabetes. Diabetes Care. 2016;39:2036–2041. doi: 10.2337/dc15-2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yokono M, Takasu T, Hayashizaki Y, Mitsuoka K, Kihara R, Muramatsu Y, et al. SGLT2 selective inhibitor ipragliflozin reduces body fat mass by increasing fatty acid oxidation in high-fat diet-induced obese rats. Eur J Pharmacol. 2014;727:66–74. doi: 10.1016/j.ejphar.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 99.Suzuki M, Takeda M, Kito A, Fukazawa M, Yata T, Yamamoto M, et al. Tofogliflozin, a sodium/glucose cotransporter 2 inhibitor, attenuates body weight gain and fat accumulation in diabetic and obese animal models. Nutr Diabetes. 2014;4:e125. doi: 10.1038/nutd.2014.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Requena-Ibáñez JA, Santos-Gallego CG, Rodriguez-Cordero A, Vargas-Delgado AP, Mancini D, Sartori S, et al. Mechanistic insights of empagliflozin in nondiabetic patients with HFrEF: from the EMPA-TROPISM study. JACC Heart Fail. 2021;9:578–589. doi: 10.1016/j.jchf.2021.04.014. [DOI] [PubMed] [Google Scholar]
- 101.Santos-Gallego CG, Vargas-Delgado AP, Requena-Ibanez JA, Garcia-Ropero A, Mancini D, Pinney S, et al. Randomized trial of empagliflozin in nondiabetic patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2021;77:243–255. doi: 10.1016/j.jacc.2020.11.008. [DOI] [PubMed] [Google Scholar]
- 102.Yurista SR, Silljé HH, Oberdorf-Maass SU, Schouten EM, Pavez Giani MG, Hillebrands JL, et al. Sodium-glucose co-transporter 2 inhibition with empagliflozin improves cardiac function in non-diabetic rats with left ventricular dysfunction after myocardial infarction. Eur J Heart Fail. 2019;21:862–873. doi: 10.1002/ejhf.1473. [DOI] [PubMed] [Google Scholar]
- 103.Polidori D, Iijima H, Goda M, Maruyama N, Inagaki N, Crawford PA. Intra- and inter-subject variability for increases in serum ketone bodies in patients with type 2 diabetes treated with the sodium glucose co-transporter 2 inhibitor canagliflozin. Diabetes Obes Metab. 2018;20:1321–1326. doi: 10.1111/dom.13224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Inagaki N, Goda M, Yokota S, Maruyama N, Iijima H. Safety and efficacy of canagliflozin in Japanese patients with type 2 diabetes mellitus: post hoc subgroup analyses according to body mass index in a 52-week open-label study. Expert Opin Pharmacother. 2015;16:1577–1591. doi: 10.1517/14656566.2015.1055250. [DOI] [PubMed] [Google Scholar]
- 105.Oldgren J, Laurila S, Åkerblom A, Latva-Rasku A, Rebelos E, Isackson H, et al. Effects of 6 weeks of treatment with dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, on myocardial function and metabolism in patients with type 2 diabetes: A randomized, placebo-controlled, exploratory study. Diabetes Obes Metab. 2021;23:1505–1517. doi: 10.1111/dom.14363. [DOI] [PubMed] [Google Scholar]
- 106.Yabe D, Iwasaki M, Kuwata H, Haraguchi T, Hamamoto Y, Kurose T, et al. Sodium-glucose co-transporter-2 inhibitor use and dietary carbohydrate intake in Japanese individuals with type 2 diabetes: a randomized, open-label, 3-arm parallel comparative, exploratory study. Diabetes Obes Metab. 2017;19:739–743. doi: 10.1111/dom.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Verma S, Rawat S, Ho KL, Wagg CS, Zhang L, Teoh H, et al. Empagliflozin increases cardiac energy production in diabetes: novel translational insights into the heart failure benefits of SGLT2 inhibitors. JACC Basic Transl Sci. 2018;3:575–587. doi: 10.1016/j.jacbts.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Moellmann J, Klinkhammer BM, Droste P, Kappel B, Haj-Yehia E, Maxeiner S, et al. Empagliflozin improves left ventricular diastolic function of db/db mice. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165807. doi: 10.1016/j.bbadis.2020.165807. [DOI] [PubMed] [Google Scholar]
- 109.Connelly KA, Zhang Y, Visram A, Advani A, Batchu SN, Desjardins JF, et al. Empagliflozin improves diastolic function in a nondiabetic rodent model of heart failure with preserved ejection fraction. JACC Basic Transl Sci. 2019;4:27–37. doi: 10.1016/j.jacbts.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cohen JJ, Berglund F, Lotspeich WD. Renal tubular reabsorption of acetoacetate, inorganic sulfate and inorganic phosphate in the dog as affected by glucose and phlorizin. Am J Physiol. 1956;184:91–96. doi: 10.1152/ajplegacy.1955.184.1.91. [DOI] [PubMed] [Google Scholar]
- 111.Taylor SI, Blau JE, Rother KI. SGLT2 inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab. 2015;100:2849–2852. doi: 10.1210/jc.2015-1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kashiwagi A, Araki S, Maegawa H. Sodium-glucose cotransporter 2 inhibitors represent a paradigm shift in the prevention of heart failure in type 2 diabetes patients. J Diabetes Investig. 2021;12:6–20. doi: 10.1111/jdi.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ekanayake P, Hupfeld C, Mudaliar S. Sodium-glucose cotransporter type 2 (SGLT-2) inhibitors and ketogenesis: the good and the bad. Curr Diab Rep. 2020;20:74. doi: 10.1007/s11892-020-01359-z. [DOI] [PubMed] [Google Scholar]
- 114.Selvaraj S, Kelly DP, Margulies KB. Implications of altered ketone metabolism and therapeutic ketosis in heart failure. Circulation. 2020;141:1800–1812. doi: 10.1161/CIRCULATIONAHA.119.045033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Brooke J, Stiell M, Ojo O. Evaluation of the accuracy of capillary hydroxybutyrate measurement compared with other measurements in the diagnosis of diabetic ketoacidosis: a systematic review. Int J Environ Res Public Health. 2016;13:837. doi: 10.3390/ijerph13090837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Klocker AA, Phelan H, Twigg SM, Craig ME. Blood β-hydroxybutyrate vs. urine acetoacetate testing for the prevention and management of ketoacidosis in type 1 diabetes: a systematic review. Diabet Med. 2013;30:818–824. doi: 10.1111/dme.12136. [DOI] [PubMed] [Google Scholar]
- 117.Guerci B, Tubiana-Rufi N, Bauduceau B, Bresson R, Cuperlier A, Delcroix C, et al. Advantages to using capillary blood beta-hydroxybutyrate determination for the detection and treatment of diabetic ketosis. Diabetes Metab. 2005;31:401–406. doi: 10.1016/s1262-3636(07)70211-2. [DOI] [PubMed] [Google Scholar]
- 118.Misra S, Oliver NS. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis. Diabet Med. 2015;32:14–23. doi: 10.1111/dme.12604. [DOI] [PubMed] [Google Scholar]
- 119.Yokokawa T, Sato T, Suzuki S, Oikawa M, Yoshihisa A, Kobayashi A, et al. Change of exhaled acetone concentration levels in patients with acute decompensated heart failure. Int Heart J. 2018;59:808–812. doi: 10.1536/ihj.17-482. [DOI] [PubMed] [Google Scholar]
- 120.Yokokawa T, Sugano Y, Shimouchi A, Shibata A, Jinno N, Nagai T, et al. Exhaled acetone concentration is related to hemodynamic severity in patients with non-ischemic chronic heart failure. Circ J. 2016;80:1178–1186. doi: 10.1253/circj.CJ-16-0011. [DOI] [PubMed] [Google Scholar]
- 121.Yokokawa T, Sato T, Suzuki S, Oikawa M, Yoshihisa A, Kobayashi A, et al. Elevated exhaled acetone concentration in stage C heart failure patients with diabetes mellitus. BMC Cardiovasc Disord. 2017;17:280. doi: 10.1186/s12872-017-0713-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Croteau E, Tremblay S, Gascon S, Dumulon-Perreault V, Labbé SM, Rousseau JA, et al. [11C]-Acetoacetate PET imaging: a potential early marker for cardiac heart failure. Nucl Med Biol. 2014;41:863–870. doi: 10.1016/j.nucmedbio.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 123.Stryeck S, Gastrager M, Degoricija V, Trbušić M, Potočnjak I, Radulović B, et al. Serum concentrations of citrate, tyrosine, 2- and 3-hydroxybutyrate are associated with increased 3-month mortality in acute heart failure patients. Sci Rep. 2019;9:6743. doi: 10.1038/s41598-019-42937-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Du Z, Shen A, Huang Y, Su L, Lai W, Wang P, et al. 1H-NMR-based metabolic analysis of human serum reveals novel markers of myocardial energy expenditure in heart failure patients. PLoS One. 2014;9:e88102. doi: 10.1371/journal.pone.0088102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease. Physiol Rev. 2010;90:207–258. doi: 10.1152/physrev.00015.2009. [DOI] [PubMed] [Google Scholar]
- 126.Mudaliar S, Alloju S, Henry RR. Can a Shift in fuel energetics explain the beneficial cardiorenal outcomes in the EMPA-REG OUTCOME study? A unifying hypothesis. Diabetes Care. 2016;39:1115–1122. doi: 10.2337/dc16-0542. [DOI] [PubMed] [Google Scholar]
- 127.Lopaschuk GD, Verma S. Empagliflozin’s fuel hypothesis: not so soon. Cell Metab. 2016;24:200–202. doi: 10.1016/j.cmet.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 128.Yurista SR, Matsuura TR, Silljé HH, Nijholt KT, McDaid KS, Shewale SV, et al. Ketone ester treatment improves cardiac function and reduces pathologic remodeling in preclinical models of heart failure. Circ Heart Fail. 2021;14:e007684. doi: 10.1161/CIRCHEARTFAILURE.120.007684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Verma S, Garg A, Yan AT, Gupta AK, Al-Omran M, Sabongui A, et al. Effect of empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: an important clue to the EMPA-REG OUTCOME trial? Diabetes Care. 2016;39:e212–e213. doi: 10.2337/dc16-1312. [DOI] [PubMed] [Google Scholar]
- 130.Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000;35:569–582. doi: 10.1016/s0735-1097(99)00630-0. [DOI] [PubMed] [Google Scholar]
- 131.Burchfield JS, Xie M, Hill JA. Pathological ventricular remodeling: mechanisms: part 1 of 2. Circulation. 2013;128:388–400. doi: 10.1161/CIRCULATIONAHA.113.001878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bertero E, Maack C. Metabolic remodelling in heart failure. Nat Rev Cardiol. 2018;15:457–470. doi: 10.1038/s41569-018-0044-6. [DOI] [PubMed] [Google Scholar]
- 133.Braunwald E. Heart failure. JACC Heart Fail. 2013;1:1–20. doi: 10.1016/j.jchf.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 134.Konstam MA, Kramer DG, Patel AR, Maron MS, Udelson JE. Left ventricular remodeling in heart failure: current concepts in clinical significance and assessment. JACC Cardiovasc Imaging. 2011;4:98–108. doi: 10.1016/j.jcmg.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 135.Kim GH, Uriel N, Burkhoff D. Reverse remodelling and myocardial recovery in heart failure. Nat Rev Cardiol. 2018;15:83–96. doi: 10.1038/nrcardio.2017.139. [DOI] [PubMed] [Google Scholar]
- 136.Kramer DG, Trikalinos TA, Kent DM, Antonopoulos GV, Konstam MA, Udelson JE. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction: a meta-analytic approach. J Am Coll Cardiol. 2010;56:392–406. doi: 10.1016/j.jacc.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Cohen ND, Gutman SJ, Briganti EM, Taylor AJ. Effects of empagliflozin treatment on cardiac function and structure in patients with type 2 diabetes: a cardiac magnetic resonance study. Intern Med J. 2019;49:1006–1010. doi: 10.1111/imj.14260. [DOI] [PubMed] [Google Scholar]
- 138.Lan NSR, Fegan PG, Yeap BB, Dwivedi G. The effects of sodium-glucose cotransporter 2 inhibitors on left ventricular function: current evidence and future directions. ESC Heart Fail. 2019;6:927–935. doi: 10.1002/ehf2.12505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 140.Di Franco A, Cantini G, Tani A, Coppini R, Zecchi-Orlandini S, Raimondi L, et al. Sodium-dependent glucose transporters (SGLT) in human ischemic heart: a new potential pharmacological target. Int J Cardiol. 2017;243:86–90. doi: 10.1016/j.ijcard.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 141.Sattar N, McLaren J, Kristensen SL, Preiss D, McMurray JJ. SGLT2 Inhibition and cardiovascular events: why did EMPA-REG Outcomes surprise and what were the likely mechanisms? Diabetologia. 2016;59:1333–1339. doi: 10.1007/s00125-016-3956-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Mullens W, Martens P, Forouzan O, Dauw J, Vercammen J, Luwel E, et al. Effects of dapagliflozin on congestion assessed by remote pulmonary artery pressure monitoring. ESC Heart Fail. 2020;7:2071–2073. doi: 10.1002/ehf2.12850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Xie M, Hill JA. HDAC-dependent ventricular remodeling. Trends Cardiovasc Med. 2013;23:229–235. doi: 10.1016/j.tcm.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kong Y, Tannous P, Lu G, Berenji K, Rothermel BA, Olson EN, et al. Suppression of class I and II histone deacetylases blunts pressure-overload cardiac hypertrophy. Circulation. 2006;113:2579–2588. doi: 10.1161/CIRCULATIONAHA.106.625467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shimazu T, Hirschey MD, Newman J, He W, Shirakawa K, Le Moan N, et al. Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013;339:211–214. doi: 10.1126/science.1227166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Briasoulis A, Androulakis E, Christophides T, Tousoulis D. The role of inflammation and cell death in the pathogenesis, progression and treatment of heart failure. Heart Fail Rev. 2016;21:169–176. doi: 10.1007/s10741-016-9533-z. [DOI] [PubMed] [Google Scholar]
- 147.Mehta JL, Pothineni NV. Inflammation in heart failure: the holy grail? Hypertension. 2016;68:27–29. doi: 10.1161/HYPERTENSIONAHA.116.07307. [DOI] [PubMed] [Google Scholar]
- 148.Dick SA, Epelman S. Chronic heart failure and inflammation: what do we really know? Circ Res. 2016;119:159–176. doi: 10.1161/CIRCRESAHA.116.308030. [DOI] [PubMed] [Google Scholar]
- 149.Butts B, Gary RA, Dunbar SB, Butler J. The importance of NLRP3 inflammasome in heart failure. J Card Fail. 2015;21:586–593. doi: 10.1016/j.cardfail.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477–489. doi: 10.1038/s41577-019-0165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Iannantuoni F, M de Marañon A, Diaz-Morales N, Falcon R, Bañuls C, Abad-Jimenez Z, et al. The SGLT2 inhibitor empagliflozin ameliorates the inflammatory profile in type 2 diabetic patients and promotes an antioxidant response in leukocytes. J Clin Med. 2019;8:1814. doi: 10.3390/jcm8111814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kim SR, Lee SG, Kim SH, Kim JH, Choi E, Cho W, et al. SGLT2 inhibition modulates NLRP3 inflammasome activity via ketones and insulin in diabetes with cardiovascular disease. Nat Commun. 2020;11:2127. doi: 10.1038/s41467-020-15983-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357–1361. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Grebe A, Hoss F, Latz E. NLRP3 inflammasome and the IL-1 pathway in atherosclerosis. Circ Res. 2018;122:1722–1740. doi: 10.1161/CIRCRESAHA.118.311362. [DOI] [PubMed] [Google Scholar]
- 155.Staels B. Cardiovascular protection by sodium glucose cotransporter 2 inhibitors: potential mechanisms. Am J Med. 2017;130:S30–S39. doi: 10.1016/j.amjmed.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 156.Grubić Rotkvić P, Cigrovski Berković M, Bulj N, Rotkvić L. Minireview: are SGLT2 inhibitors heart savers in diabetes? Heart Fail Rev. 2020;25:899–905. doi: 10.1007/s10741-019-09849-3. [DOI] [PubMed] [Google Scholar]
- 157.Deng Y, Xie M, Li Q, Xu X, Ou W, Zhang Y, et al. Targeting mitochondria-inflammation circuit by β-hydroxybutyrate mitigates HFpEF. Circ Res. 2021;128:232–245. doi: 10.1161/CIRCRESAHA.120.317933. [DOI] [PubMed] [Google Scholar]