Abstract
Proviral human immunodeficiency virus type 1 (HIV-1) DNA could be a useful marker for exploring viral reservoirs and monitoring antiretroviral treatment, particularly when HIV-1 RNA is undetectable in plasma. A new technique was developed to quantify proviral HIV-1 using a TaqMan real-time PCR assay. One copy of proviral HIV-1 DNA could be detected with 100% sensitivity for five copies and the assay had a range of 6 log10. Reproducibility was evaluated in intra- and interassays using independent extractions of the 8E5 cell line harboring the HIV-1 proviral genome (coefficients of variation [CV], 13 and 27%, respectively) and peripheral blood mononuclear cells (PBMC) from a patient with a mean proviral load of 26 copies per 106 PBMC (CV, 46 and 56%, respectively). The median PBMC proviral load of 21 patients, measured in a cross-sectional study, was determined to be 215 copies per 106 PBMC (range, <10 to 8,381). In a longitudinal study, the proviral load of 15 out of 16 patients with primary infection fell significantly during 1 year of antiretroviral therapy (P = 0.004). In the remaining patient, proviral HIV-1 DNA was detectable but not quantifiable due to a point mutation at the 5′ end of the TaqMan probe. No correlation was observed between proviral load and levels of CD4+ cells or HIV-1 RNA in plasma. TaqMan PCR is sensitive and adaptable to a large series of samples. The full interest of monitoring proviral HIV-1 DNA can now be ascertained by its application to the routine monitoring of patients.
Measuring human immunodeficiency virus type 1 (HIV-1) RNA in plasma has enabled the pathophysiology of the infection to be studied, and this parameter, which directly reflects viral replication, is the main prognostic factor for the evolution of the disease (29). Standardization of commercial tests has allowed this measurement to be used for routine monitoring of the initiation of antiretroviral treatments and the follow-up of their efficacy. These tests are currently used to assess efficacy of combination therapy in clinical trials (19, 20). Highly active antiretroviral therapy (HAART) that includes combinations of nucleoside and nonnucleoside inhibitors of reverse transcriptase (RT) and/or antiprotease drugs leads to dramatic reductions in HIV-1 RNA in plasma to below detectable levels, currently 50 copies per ml.
However, it is now well established that despite a powerful, long-term inhibition of viral production in the majority of patients under HAART, proviral HIV-1 DNA persists in peripheral blood mononuclear cells (PBMC) and lymphoid tissue (8, 15, 37, 38). This reservoir, which establishes rapidly during the primary infection phase, is one of the major obstacles to the total eradication of the virus, even if treatment is initiated at an early stage (32). Antiretroviral treatment also decreases proviral HIV-1 DNA, but the rate of decline is generally lower than that of plasma HIV-1 RNA, and detectable proviral HIV-1 DNA persists even after prolonged treatment (3, 12, 36).
Therefore, it is important to be able to quantify proviral HIV-1 DNA and to study its dynamics, particularly when HAART has led to plasma HIV-1 RNA levels dropping below detection limits. Proviral HIV-1 DNA quantification would thus be useful for monitoring individual patients, and it could also be a helpful marker when HIV-1 RNA becomes undetectable in order to compare the efficacies of different treatments in cohort studies.
Several techniques for measuring proviral HIV-1 DNA have been described (2, 23). However, these tests are difficult to carry out and lack standardization, and at present none have been commercialized, illustrating the difficulty of quantifying this marker. To be of use in clinical protocols and routine measurements, a test should be validated; have a defined sensitivity and specificity, a wide dynamic range, and good intra- and interassay reproducibility; and be easy to perform.
Our aim was therefore to develop a method for quantifying proviral HIV-1 DNA using real-time PCR that would be sensitive and reproducible and have a high throughput. Proviral HIV-1 DNA could be measured not only in PBMC but also in lymphoid tissue biopsy specimens. The application of this technique to the monitoring of patients with primary HIV-1 infection has confirmed that HAART decreases the proviral load but has also shown that a detectable viral reservoir persists in the majority of patients.
MATERIALS AND METHODS
Patients.
Twenty-one consenting, HIV-1-seropositive adults were enrolled in a cross-sectional study over a 10-day consultation period in the Infectious Diseases Unit of the Rothschild Hospital, Paris, France. Blood samples were collected for CD4+ and CD8+ lymphocyte counts and measurements of HIV-1 RNA in plasma and proviral HIV-1 DNA. Sixteen consenting adult patients with symptomatic primary HIV-1 infection were also included in a longitudinal study. The treatment began, on average, 15 days from the onset of symptoms, with a three-drug combination of stavudine (D4T), lamivudine (3TC), and indinavir (IDV) for nine patients and zidovudine, 3TC and didanosine for seven patients. Virological and immunological parameters were monitored at day 0 (D0), and at month 1 (M1), M2, M3, M6, M9, and M12 during therapy. Evaluation included a CD4+ and CD8+ lymphocyte count and measurements of HIV-1 RNA in plasma and quantitative cellular viremia at each follow-up. In addition, proviral HIV-1 DNA was quantified at D0, M1, M6, and M12 for nine patients and at D0 and M12 for the remaining seven patients. The characteristics of the latter seven patients are described in part elsewhere (17).
Lymphoid tissue biopsy specimens were taken from two consenting patients. A rectal biopsy specimen was taken from a 33-year-old homosexual man who had been HIV-1 seropositive for 14 months (classed following the guidelines of the Centers for Disease Control and Prevention [CDC] as clinical stage CDC A) and was being treated with D4T, IDV and 3TC. A ganglion biopsy specimen was taken from a 37-year-old woman who had been HIV-1 seropositive for 5 years (clinical stage, CDC C) and was not receiving treatment.
Quantification of plasma HIV-1 RNA.
A quantitative RT-PCR assay (Amplicor HIV1 Monitor version 1.5; Roche Diagnostics Systems, Meylan, France) was performed on samples from primary-infected patients with a lower detection limit of either 200 or 50 copies per ml. For the other clinical samples, plasma HIV-1 RNA levels were determined by the branched-DNA signal amplification method (Quantiplex HIV-RNA 2.0; Chiron, Cergy Pontoise, France), following the manufacturer's procedure, with a lower detection limit of 500 copies per ml.
Quantitative cellular viremia.
Quantitative PBMC cultures were performed as previously described by Rouzioux et al. (34). The titers were calculated by using the Poisson distribution (Poisson Pilote software; Agence Nationale de Recherche sur le SIDA) and expressed as the number of infectious units (IU) per 106 PBMC. The cutoff value was 0.1 IU per 106 PBMC.
Preparation of biological samples and standard curves.
Blood samples were collected into EDTA and, after separation on a Ficoll-Hypaque gradient, pellets corresponding to 5 × 106 PBMC were prepared and stored at −80°C before use. After lysis by proteinase K, DNA was extracted by a classic phenol-chloroform procedure followed by ethanol precipitation and stored at −20°C. Biopsy material was finely chopped before being treated with collagenase (2 U/ml) for 18 h at 37°C. After filtration over a Becton cell strainer (Becton Dickinson, Le Pont de Claix, France), mononuclear cells were separated on a Ficoll gradient and then treated as for the blood samples. The T lymphoblastoid cell line 8E5 (ATCC 8993), which contains a single proviral genome of HIV-LAV per cell, was used as a control for the quantification, with cells being treated in parallel as described above.
A double standard plasmid, pcHIV-Alb, was constructed by cloning one copy of each PCR region from intron 12 of the human albumin gene and the HIV-1 pol gene obtained from the LAV-BRU strain. The concentration of this plasmid standard was determined by spectrometry at 260 nm. Single-stock solutions of serial dilutions from 106 to 102 copies were prepared and stored in siliconized tubes at −20°C. The final dilution (10 copies) was prepared immediately before use.
Measurement of the proviral HIV-1 DNA by TaqMan real-time PCR.
The principle of TaqMan real-time PCR is based on the cleavage of an internal probe by the 5′-3′ exonuclease activity of the Taq polymerase during amplification. This probe contains fluorescent reporter and quencher dyes at its 5′ and 3′ ends, respectively. At the start of the reaction there is no fluorescence due to the proximity of the quencher and reporter dyes. However, during each cycle of the extension phase one molecule of reporter dye is released for each target molecule amplified. A passive reference dye provides an internal reference for normalization of the reporter fluorescence (ΔRn). The threshold cycle (Ct) value is the number of cycles before the fluorescence emitted passes a fixed limit. The log10 of the number of targets initially present is proportional to Ct and can be measured using a standard curve.
PCR primers and the TaqMan probe for HIV-1 DNA quantification were selected using the Oligo (version 4; National Biosciences, Plymouth, Minn.) and Primer Express (PE Applied Biosystems, Courtabœuf, France) software programs and checked by a BLAST search of GenBank (1). The forward primer, P1 (5′-TGGCATGGGTACCAGCACA-3′), and the reverse primer, P2 (5′-CTGGCTACTATTTCTTTTGCTA-3′), were chosen to amplify a 199-bp fragment in a region of low variability of the B subtype HIV-1 pol gene, determined from data bank sequences and previously used by Yerly et al. (39). The internal HIV-1 TaqMan probe (5′-TTTATCTACTTGTTCATTTCCTCCAATTCCTT-3′) was designed following the general rules outlined by the manufacturer. The primers, Alb-S (5′-GCTGTCATCTCTTGTGGGCTGT-3′) and Alb-AS (5′-AAACTCATGGGAGCTGCTGGTT-3′), and the Alb TaqMan probe (5′-CCTGTCATGCCCACACAAATCTCTCC-3′) were used to quantify the human albumin gene (26). The TaqMan probes carried a 5′ reporter dye, 6-carboxy fluorescein (FAM), and a 3′ quencher dye, 6-carboxy tetramethyl rhodamine, and were synthesized by Genset Oligos (Paris, France).
The 50-μl PCR mixture for HIV-1 or albumin DNA amplification consisted of 1/20 of the DNA extract; high-performance liquid chromatography-purified primers P1 and P2 or Alb-S and Alb-AS (200 nM concentration of each); 100 nM HIV-1 or Alb TaqMan probe; dATP, dCTP, and dGTP, each at a concentration of 200 nM; 400 nM dUTP; 5 mM MgCl2; 0.5 U of uracil N-glycosylase; 1.25 U of AmpliTaq Gold polymerase; and 1× PCR buffer (TaqMan PCR Core Reagent Kit; PE Applied Biosystems).
For both HIV-1 and albumin DNA amplification, 1 cycle at 50°C for 2 min and 1 cycle at 95°C for 10 min were followed by a two-step PCR procedure consisting of 15 s at 95°C and 1 min at 60°C for HIV-1, or at 65°C for albumin, for 45 cycles. Amplification, data acquisition, and analysis were performed using the ABI Prism 7700 Sequence Detector System (PE Applied Biosystems).
All standard dilutions, controls, and samples from patients were run in duplicate, and the average value of the copy number was used to quantify both HIV-1 and albumin DNA. Standard curves for HIV-1 and albumin were accepted when the slopes were between −3.74 and −3.32 (corresponding to PCR efficiencies of between 85 and 100%) and the coefficients of correlation (r2) were >0.990.
Albumin DNA was quantified in order to determine the input level of cellular DNA in the sample and was used as an endogenous reference to normalize variations due to differences in the PBMC count or DNA extraction. The normalized value of the HIV-1 proviral load was calculated as HIV-1 copy number/albumin copy number × 2 × 106 and expressed as the number of HIV-1 copies per 106 PBMC. The 8E5 cell line was used as a positive control for each run, and acceptable results were considered to be 0.7 to 1.3 HIV-1 copies per cell.
The measurements of the HIV-1 proviral load in the biological samples were validated if the coefficients of variation (CV) were <20% for albumin with a minimum of 9,000 cells analyzed, <30% for >10 copies of HIV-1, and <50% for <10 copies of HIV-1. If these criteria were not met, the measurements were repeated until satisfactory. HIV-1 proviral loads ranging from 1 to 9 copies per 106 PBMC were expressed as <10 copies per 106 PBMC. Exact values were used for calculations.
Reverse transcriptase sequencing for subtyping.
Blood specimens were collected in EDTA and free virus was obtained by ultracentrifugation. RNA was extracted with a High Pure RNA Isolation Kit (Boehringer, Mannheim, Germany) and reverse transcribed. Two RT gene fragments (RT1, codons 6 to 152; RT2, codons 157 to 252) were amplified by nested PCR as described elsewhere (25). PCR products were directly sequenced on both strands, using an ABI Prism 377 automatic sequencer and an ABI Prism Dye Primer Sequencing Kit (PE Applied Biosystems). The subtype of most viral isolates was determined by using the BLAST-based HIV-1 subtyping tool program on the NCBI website (http://www.ncbi.nlm.nih.gov:80/retroviruses/subtype/makepage.cgi?page=sub&type=0). Isolates yielding ambiguous results were reanalyzed against a background of reference sequences (24), with the Phylogenetic Analysis using Parsimony (PAUP∗) software (version 4.0d64 [in progress]; D. Swofford). Assignment to a given subtype was based on neighbor-joining and maximum-parsimony inferences, confirmed by 100 bootstrap replicates each.
Sequencing of HIV-1 sequence amplified by TaqMan PCR.
Two nested PCR techniques were used to sequence the region amplified by real-time PCR in DNA extracts from primary-infected patients at D0. To obtain the whole target sequence, a 323-bp fragment was obtained by PCR nested with the external primers A′ (5′-CAGACTCACAATATGCA-3′) and B′ (5′-ACTTGTCCATGCATGGCTTC-3′) and the internal primers C1 (5′-GCATTAGGAGCTTTCAAGC-3′) and C2 (5′-GCTTCTCCTTTAAGCTTACA-3′). In addition a 199-bp fragment that did not contain the target sequence of the primers used in TaqMan PCR was obtained with the external C1 and C2 and internal P1 and P2 primers. PCR products were directly sequenced on both strands, using an ABI Prism 377 automatic sequencer and an ABI Prism Dye Terminator Sequencing kit (PE Applied Biosystems).
Statistical analysis.
Correlations between virological and immunological factors were analyzed using the Wilcoxon (rank sum), Kruskall-Wallis (mean rank), or Spearman (rank correlation) nonparametric tests, as appropriate. The decrease in the proviral load between D0 and M12 was analyzed using the Wilcoxon matched-pairs signed-rank test.
Nucleotide sequence accession numbers.
All nucleotide sequences shown in Fig. 1 are available in the GenBank database, under accession numbers AF277299 to AF277314.
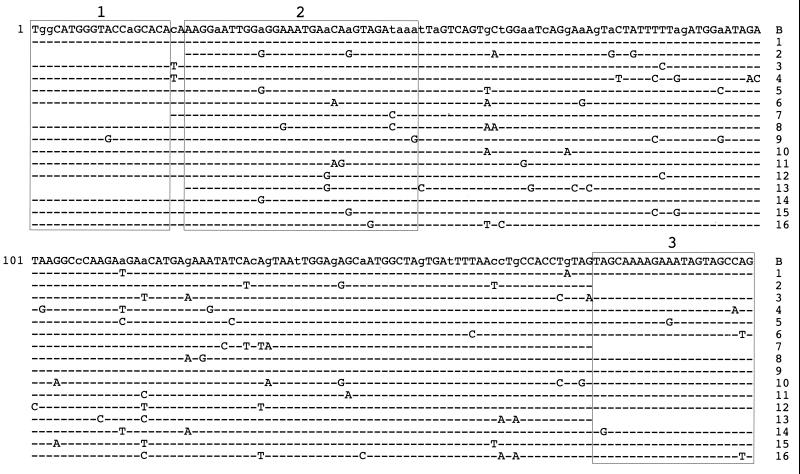
FIG. 1.
Sequence of the region amplified for HIV-1 quantification. In the B subtype consensus region from the Los Alamos data bank, the lowercase letters indicate the variable positions identified. Boxes 1, 2, and 3 correspond, respectively, to the target sequences of the forward primer P1, the probe, and the reverse primer P2 used for HIV-1 quantification. The target region was sequenced as described in Materials and Methods, and for each patient only the mutations relative to the consensus sequence are indicated. For patients 2, 7, and 13, the sequences were not obtained for the primer target regions.
RESULTS
Standard curve and dynamic range of the TaqMan PCR.
The main objective was to obtain a standard curve that would be easy to prepare, highly reproducible, and stable with time, to monitor the evolution of the proviral load. We therefore chose to use serial dilutions of the standard plasmid pcHIV-Alb that contained one copy of the HIV-1 subtype B target sequence and one copy of the albumin target sequence. Distilled water, with or without a constant amount of murine DNA, was tested as a dilution medium, and no major differences were observed (Table 1). Standard dilutions in distilled water alone were therefore used for subsequent experiments.
TABLE 1.
Comparison of standard curves obtained using either water alone or water plus murine DNAa
| Dilution medium and target | Mean Ct at the indicated target copy no.b:
|
ΔRn from plateauc | Sloped | PCR efficiencye (%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| 106 | 105 | 104 | 103 | 102 | 101 | ||||
| Water alone | |||||||||
| HIV-1 | 17.4 | 21.1 | 24.4 | 28.3 | 31.8 | 35.2 | 1.3 | −3.57 | 90 |
| Albumin | 17.4 | 21.6 | 25.0 | 28.7 | 32.3 | 35.7 | 1.9 | −3.60 | 89 |
| Water + murine DNA | |||||||||
| HIV-1 | 18.4 | 21.9 | 25.9 | 29.2 | 32.8 | 35.6 | 1.1 | −3.51 | 92 |
| Albumin | 18.3 | 22.0 | 26.0 | 29.7 | 33.5 | 36.8 | 1.8 | −3.73 | 85 |
The amplification parameters for HIV-1 and albumin quantification were obtained with dilutions ranging from 106 to 101 copies of the double plasmid standard, and experiments were carried out in either water alone or water containing 1 μg of murine DNA from the BALB/3T3 cell line.
Average Ct values measured in duplicate for each point of the calibration curve.
Average values of normalized fluorescence intensity (ΔRn) taken from the plateau of all the amplification curves.
Slopes of the calibration curves.
Percent amplification efficiency, calculated as (10(−1/slope) − 1) × 100.
The dynamic range of the assay encompassed at least 6 orders of magnitude, with a strong linear relationship (r2 > 0.995) between the Ct values and the log10 of the input number of copies (data not shown). The Ct values obtained for HIV-1 or albumin quantification were identical or almost identical for the same plasmid copy number, showing that both quantitative PCR assays have comparable efficiencies (Table 1).
Sensitivity and intra- and interassay reproducibility.
Using the same primer pair as above and a classical PCR method with detection by an ethidium bromide-stained agarose gel, it was possible to detect 10 copies of plasmid HIV-1 DNA (data not shown). With real-time PCR however, one copy could be inconsistently detected and five copies were always detected.
The intra-assay reproducibility was first evaluated using 8 replicates of the different points of the calibration curve used to quantify HIV-1. The coefficients of variation (CV) were 32% for the most dilute solution (10 copies) and ≤18% for 102 to 107 copies.
Intra- and interassay reproducibility was also analyzed using independent extractions of 8E5 cells and a single blood sample taken from a patient infected with HIV-1 subtype B (Table 2). These experiments were carried out to take into account variations in sample pretreatment and also to validate normalization of the results using data from the amplification of the albumin gene. Large variations in the HIV-1 copy number were observed in inter- and intra-assay reproducibility analyses. This variability was reduced for proviral HIV-1 DNA after normalization of the results. In addition, the normalized data showed that the 8E5 cells contained an average of one copy of proviral HIV-1 DNA per cell, as expected. Therefore, in each subsequent TaqMan assay an 8E5 control was introduced, with the limit for an acceptable result being taken as 0.7 to 1.3 copies of proviral HIV-1 DNA per cell.
TABLE 2.
Real-time PCR intra- and interassaysa
| Target | Mean no. of copies ± SD (CV [%]) with:
|
|||
|---|---|---|---|---|
| PBMC
|
8E5 cells
|
|||
| Intra-assay (nc = 12) | Interassay (n = 10) | Intra-assay (n = 12) | Interassay (n = 18) | |
| HIV-1 | 1.48 ± 0.97 (66) | 1.30 ± 1.25 (96) | 13,617 ± 5,393 (40) | 25,217 ± 14,582 (58) |
| Albumin | 87,090 ± 29,346 (34) | 93,402 ± 52,016 (56) | 27,788 ± 12,166 (44) | 49,998 ± 23,948 (48) |
| Proviral HIV-1 DNAb | 32 ± 15 (46) | 26 ± 15 (56) | 1,007,046 ± 130,490 (13) | 1,001,377 ± 265,646 (27) |
The reproducibility of the quantitative PCR was tested using independent extractions of 8E5 cells and PBMC from an HIV-1 infected patient, either in the same TaqMan assay (intra-assay) or in separate assays (interassay).
Each proviral HIV-1 DNA result in intra- or interassay was calculated from each individual pair of HIV-1 and albumin measurements by the equation described in Materials and Methods.
n, number of extractions.
Specificity and HIV-1 subtypes amplified.
The primers and the probe were chosen to quantify HIV-1 group M subtype B, the most frequent subtype found in the European population, representing 80 to 85% of the strains isolated in France. However, a BLAST search of GenBank indicated that the primers might also amplify subtypes A, C, and D. In addition, the sequence alignments available in the Los Alamos bank also indicated that the TaqMan assay might detect subtype A and especially subtype D but that a large number of mutations would theoretically prevent the amplification of group O. The capacity of our assay to detect the different HIV types was therefore tested, using one strain for each type (data not shown). The results showed that, as expected, subtypes A, C, and D could be amplified as well as E, F, G, and H. However, HIV group O and HIV-2 were not amplified. The specificity of the assay against human T-cell leukemia virus was also tested using an extract of the lymphoblastic T-cell line, MT2. The results were negative, with a Ct of >45 cycles (data not shown).
Cross-sectional study of proviral HIV-1 DNA.
The TaqMan method was used to measure the HIV-1 proviral load of 21 patients who had been seropositive for a median of 7 years (range, 5 months to 13 years). All the patients had a detectable proviral load with an average of 773 ± 1,794 copies per 106 PBMC and a median of 215 (range, <10 to 8,381) (Table 3). In parallel measurements no correlation was found between the peripheral proviral load and the plasma HIV-1 RNA or the CD4+ or CD8+ cell levels (Spearman tests). The plasma HIV-1 RNA and CD4+ levels were also found to be independent parameters in this study (Spearman test). In addition, the proviral load was not correlated with the CDC clinical stages (Kruskall-Wallis test) or with the type of antiretroviral treatment (with or without antiprotease drugs [Wilcoxon test]).
TABLE 3.
Results from patients in the cross-sectional study
| Patient no. | Proviral HIV-1 DNA (copies/106 PBMC) | Plasma HIV-1 RNA (copies/ml) | No. of cells/mm3
|
CDC stage | Antiretroviral treatmentc | |
|---|---|---|---|---|---|---|
| CD4+ | CD8+ | |||||
| 1 | 8,381 | 194,100 | 335 | 1,927 | B | AZT + 3TC + IDV |
| 2 | 1,456 | 4,960 | 518 | 840 | A | AZT + 3TC |
| 3a | 1,389 | 11,450 | 217 | 591 | B | D4T + 3TC + NVP + NFV |
| 4 | 909 | 17,560 | 441 | 1,053 | B | D4T + 3TC |
| 5 | 783 | 2,570 | 405 | 1,098 | B | D4T + 3TC |
| 6 | 681 | <500 | 472 | 835 | B | D4T + 3TC + IDV |
| 7 | 421 | <500 | 215 | 806 | B | AZT + DDI |
| 8 | 417 | <500 | 157 | 297 | C | AZT + 3TC + IDV |
| 9 | 355 | <500 | 522 | 2,026 | A | AZT + DDI |
| 10 | 217 | <500 | 322 | 306 | B | AZT + 3TC + NFV |
| 11a | 215 | 52,150 | 198 | 1,346 | B | D4T + RTV + SQV |
| 12 | 185 | 4,420 | 456 | 1,253 | B | Untreated |
| 13 | 176 | 5,640 | 642 | 770 | A | Untreated |
| 14 | 154 | <500 | 170 | 911 | B | D4T + 3TC + IDV |
| 15 | 128 | 16,900 | 584 | 749 | A | AZT + 3TC + IDV |
| 16 | 88 | <500 | 621 | 714 | A | D4T + 3TC + NFV |
| 17 | 86 | 41,870 | 134 | 1,181 | C | D4T + 3TC + IDV |
| 18a | 72 | <500 | 553 | 1,317 | C | D4T + 3TC + IDV |
| 19a | 63 | 8,230 | 157 | 594 | B | AZT + 3TC |
| 20a | 49 | <500 | 174 | 1,243 | B | AZT + 3TC + IDV |
| 21b | <10 | 205,360 | 8 | 334 | C | D4T + NVP + NFV |
| Mean ± SD | 773 ± 1,794 | 27,022 ± 59,103 | 348 ± 189 | 961 ± 465 | ||
| Median | 215 | 4,420 | 335 | 840 | ||
B subtype.
A subtype.
Abbreviations: AZT, zidovudine; ddI, didanosine; NVP, nevirapine; NFV, nelfinavir; SQV, saquinavir.
Evolution of proviral HIV-1 DNA after primary infection under antiretroviral treatment.
The possibility of conducting a longitudinal study of the HIV-1 proviral load during antiretroviral therapy was also investigated. Sixteen patients infected with HIV-1 subtype B were included on average 15 days after the appearance of the clinical signs of primary infection and were monitored for 1 year under antiretroviral treatment from D0 (Table 4). Proviral HIV-1 DNA quantification was performed on samples from all patients using an annealing temperature of 60°C for the real-time PCR, as described in Materials and Methods. Patient 9 had proviral loads that were either undetectable or ≤10 copies per 106 PBMC throughout the study period. The median values for the proviral load for the remaining 15 patients were 466 copies per 106 PBMC (range, 42 to 9,182) at D0, 211 (range, 0 to 369) at M1 to M4, 97 (range, <10 to 175) at M6, and 38 (range, 0 to 358) at M12 to M15. The corresponding mean values ± standard deviations were 1,122 ± 2,267, 188 ± 1,151, 89 ± 74, and 67 ± 102 copies per 106 PBMC, respectively.
TABLE 4.
Follow-up of the patients with primary HIV-1 infection
| Patient no.a | Follow-up | Proviral HIV-1 DNA (copies/106 PBMC) at:
|
QCVc (IU/106 PBMC) | Plasma HIV-1 RNA (copies/ml) | No. of cells/mm3
|
||
|---|---|---|---|---|---|---|---|
| 60°C | 65°Cb | CD4+ | CD8+ | ||||
| 1 | D0 | 1,342 | 1,025 | 32.9 | >750,000 | 621 | 1,454 |
| M1 | 362 | 449 | <0.1 | 1,208 | 620 | 456 | |
| M6 | 146 | 116 | <0.1 | 72 | 501 | 571 | |
| M12 | 44 | 25 | <0.1 | <50 | 645 | 685 | |
| 2 | D0 | 923 | 0 | 166.3 | >750,000 | 813 | 745 |
| M1 | 212 | 0 | <0.1 | NDd | 859 | 756 | |
| M6 | 48 | 0 | <0.1 | <50 | 704 | 558 | |
| M12 | 21 | 0 | <0.1 | <50 | 887 | 684 | |
| 3 | D0 | 676 | 331 | 2.9 | 57,161 | 417 | 1,124 |
| M1 | 288 | 355 | 3.1 | 324 | 463 | 748 | |
| M6 | 147 | 91 | <0.1 | <50 | 658 | 559 | |
| M12 | 0 | <10 | <0.1 | <50 | 650 | 619 | |
| 4 | D0 | 436 | 105 | 24.2 | 52,674 | 438 | 1,826 |
| M1 | 369 | 27 | 0.6 | 940 | 659 | 1,070 | |
| M6 | 175 | 9 | <0.1 | <50 | 828 | 1,118 | |
| M12 | 72 | 10 | <0.1 | <50 | 758 | 778 | |
| 5 | D0 | 266 | <10 | ND | 128,100 | 663 | 743 |
| M4 | 0 | <10 | <0.1 | ND | 831 | 648 | |
| M6 | 20 | <10 | <0.1 | 105 | 985 | 788 | |
| M12 | <10 | 0 | <0.1 | <50 | 1,216 | 998 | |
| 6 | D0 | 259 | 0 | 32.9 | 404,906 | 258 | 1,632 |
| M1 | 210 | 0 | 2.1 | 11,251 | 604 | 1,203 | |
| M6 | 159 | 0 | <0.1 | <50 | 711 | 979 | |
| M12 | 38 | 0 | <0.1 | <50 | 760 | 925 | |
| 7 | D0 | 155 | <10 | 16.2 | 181,988 | 502 | 441 |
| M1 | 32 | <10 | 0.3 | 3,552 | 740 | 332 | |
| M6 | 12 | <10 | <0.1 | <50 | 738 | 258 | |
| M12 | <10 | 19 | <0.1 | <50 | 1,003 | 404 | |
| 8 | D0 | 105 | 26 | ND | 46,029 | ND | ND |
| M1 | 30 | <10 | <0.1 | 284 | 485 | 798 | |
| M6 | <10 | <10 | <0.1 | <50 | 546 | 693 | |
| M12 | 0 | <10 | <0.1 | <50 | 637 | 986 | |
| 9 | D0 | 10 | <10 | 2.5 | 89,049 | 367 | 454 |
| M3 | 0 | <10 | <0.1 | <50 | 177 | 130 | |
| M6 | <10 | <10 | <0.1 | <50 | 582 | 466 | |
| M15 | 0 | <10 | <0.1 | <50 | 590 | 407 | |
| 10 | D0 | 9,182 | ND | 35.0 | >750,000 | 261 | 1,783 |
| M12 | 53 | ND | <0.1 | <50 | 508 | 381 | |
| 11 | D0 | 1,168 | ND | 32.9 | 57,480 | 543 | 625 |
| M12 | 358 | ND | <0.1 | 178 | 746 | 723 | |
| 12 | D0 | 963 | ND | 24.2 | 100,740 | 306 | 1,193 |
| M12 | 245 | ND | <0.1 | <50 | 454 | 861 | |
| 13 | D0 | 707 | ND | 9.1 | 139,120 | 534 | 1,595 |
| M12 | 108 | ND | <0.1 | 75 | 661 | 610 | |
| 14 | D0 | 466 | ND | 17.0 | 178,000 | 238 | 938 |
| M12 | 10 | ND | <0.1 | <50 | 188 | 776 | |
| 15 | D0 | 143 | ND | 24.2 | 254,400 | 600 | 3,186 |
| M12 | 38 | ND | <0.1 | <200 | 1,113 | 1,089 | |
| 16 | D0 | 42 | ND | 24.0 | 28,960 | 270 | 450 |
| M12 | 16 | ND | <0.1 | <50 | 505 | 355 | |
Patients 1 to 9 were treated with lamivudine, stavudine and indinavir and patients 10 to 16 were treated with zidovudine, lamivudine and didanosine and monitored as described in Materials and Methods.
For patients 1 to 9, proviral HIV-1 DNA was also quantified with a PCR annealing temperature of 65°C, instead of 60°C.
QCV, quantitative cellular viremia.
ND, not determined.
A global analysis of the results from these 15 patients did not find any correlation between the HIV-1 proviral load and quantitative cellular viremia or plasma HIV-1 RNA or CD4+ and CD8+ levels (Spearman tests). Nevertheless, proviral HIV-1 DNA levels decreased significantly for these 15 patients (P = 0.004 [Wilcoxon matched-pairs signed-rank test]), and this overall reduction was observed in parallel with the reduction in HIV-1 RNA in plasma.
In contrast, given that the proviral load was always ≤10 copies per 106 PBMC for patient 9, the evolution of this marker with time could not be studied. To determine whether this was due to an amplification problem, the TaqMan PCR target region at D0 was sequenced for all 16 patients. Sequences were obtained either for the primers and probe target regions or for the probe region alone. The results were compared with the subtype B consensus sequence from the Los Alamos data bank shown in Fig. 1. In patient 9, one mutation was found in the target region of primer P1 and a second was found at the 5′ extremity of the probe. However, 12 other patients also had mutations in the probe and/or primer P2 regions. To evaluate the influence of these mutations on the quantification results, DNA extracts from the nine patients who were monitored at D0, M1, M6, and M12 were subjected to an annealing temperature of 65°C instead of the previously used 60°C (Table 4). As expected for patient 9, the proviral load was ≤10 copies per 106 PBMC at both temperatures. The results were similar at both temperatures for extracts from patients 1 and 3, where no mutations were found in either the probe or primer regions. In contrast, the presence of at least one mutation in the probe or primer P2 region led to an apparent decrease in proviral load when the annealing temperature was more stringent. In particular, patients 2 and 6 had undetectable levels from D0 onwards when an annealing temperature of 65°C was employed.
Proviral HIV-1 DNA of ganglion and rectal biopsy specimens.
The proviral load of ganglion and rectal biopsy specimens was measured to investigate the possibility of using the TaqMan technology to explore anatomical reservoirs of the virus. The ganglion biopsy specimen was taken before the start of antiretroviral therapy from a patient who was immunodepressed (173 CD4+ per mm3) and infected by HIV-1 subtype G. The proviral load of this sample was 2,091 copies per 106 mononuclear cells, while the corresponding plasma HIV-1 RNA of the patient was 697,400 copies per ml.
The rectal biopsy specimen was taken from a patient infected by HIV-1 subtype B. The patient was mildly immunodepressed (642 CD4+ per mm3); was receiving effective treatment with D4T, 3TC, and IDV; and had HIV-1 RNA that was undetectable in plasma (<500 copies per ml). The rectal biopsy specimen proviral load was 1,632 copies per 106 cells, while the blood proviral load was 920 copies per 106 PBMC.
DISCUSSION
TaqMan real-time PCR allows simultaneous amplification and quantification, thereby eliminating the need for further manipulation of PCR products. This limits the risk of contamination, and a large number of samples can be processed rapidly. When applied to the quantification of proviral HIV-1 DNA, this technique has a wide dynamic range of 6 orders of magnitude, with a strong linear correlation between the threshold cycles and the log10 of the number of initial copies. This compares favorably with other methods described in the literature, often based on competitive PCR, whose range is generally limited to 3 to 4 log10 (5, 10, 18). In addition, the use of a double plasmid as standard showed that the amplification efficiency was comparable for HIV-1 and albumin, permitting the normalization of the proviral load for 106 cells. Normalizing the results minimizes the influence of variations in the steps preceding quantification that are essentially linked to the yield of the DNA extraction step. Better reproducibility was obtained after normalization in both intra- and interassays, in comparison with the quantification of HIV-1 alone, and normalized results confirmed that the 8E5 cell line contains an average of 1 copy of integrated HIV-1 per cell.
Intra- and interassay variability were, respectively, 46 and 56% for a patient with a proviral load of only 26 copies per 106 PBMC. It is difficult to compare these results to those obtained with other in-house techniques previously used to quantify proviral HIV-1 DNA, and to date no commercial technique is available. However, for low levels of HIV-1 RNA measured in plasma by commercial techniques, the assay CV has been shown to be as high as 35% (30, 35; F. Huysse, personal communication). Therefore the TaqMan technique could enable patients to be monitored over a course of treatment as sequential samples taken from a patient can be analyzed with confidence in separate TaqMan runs.
Although the technique was developed to quantify HIV-1 subtype B, the major subtype found in France, it also amplified strain subtypes A, C, D, E, F, G, and H. In addition, subtyping of 25 patients showed that 23 had subtype B, while 1 patient had subtype A and the remaining patient had subtype G. The capacity of the assay to amplify non-B subtypes will have to be confirmed with a larger number of samples, as well as the validity and reproducibility of the quantification. Indeed, the method is based on measuring a kinetic parameter, and mutations could lead to erroneous results. Thus, the proviral loads calculated for the various subtypes cannot be directly compared, but the follow-up of a non-B subtype patient could be feasible.
All the patients in the cross-sectional study had detectable proviral HIV-1 DNA that ranged from <10 to 8,381 copies per 106 PBMC, in agreement with the results reported by Escaich et al. (13), although Izopet et al. found higher values (23). Nevertheless, it is difficult to compare the results of these studies, as the quantitative techniques used were very different and the groups studied were not homogeneous. In our study, no correlation was found between the proviral load and other immunovirological markers. In the primary infection study, one of the patients (patient 9) had a proviral load that was ≤10 copies per 106 PBMC throughout the study. Sequencing the TaqMan PCR target region of the specimen from this patient showed a mutation in the primer P1 target region and, more importantly, a second mutation that would prevent hybridization of the 5′ end of the TaqMan probe. It seems likely that with the latter mutation there would be no cleavage by the 5′-3′ exonuclease activity of the Taq polymerase and therefore no liberation of the fluorescent reporter, making quantification impossible. The absence of this mutation in the other patients is in agreement with this hypothesis. On the other hand, sequencing the target regions of the other patients indicated the frequent existence of at least one mutation in the probe and/or the primer target sequences. Increasing the temperature to 65°C showed that the proviral load is underestimated if mutations are present, probably due to incomplete hybridization. However, these mutations did not prevent quantification at an annealing temperature of 60°C.
As in the cross-sectional study, no correlation was found in the primary infection group between proviral load and either plasma HIV-1 RNA or CD4+ CD8+ levels. In contrast, for 15 patients a decrease in the proviral load was observed between D0 and M12, in parallel with a decrease in the number of international units in culture (for 13 patients) and in HIV-1 RNA in plasma. Several groups have demonstrated a rapid fall in HIV-1 RNA in plasma due to HAART during the primary infection phase (40), as well as a decrease in cellular viremia (4). In the present work, the number of international units measured in culture was smaller than the proviral load. This is to be expected, as the proviral load measurement by real-time PCR includes both integrated and nonintegrated virus, whether or not it is replication competent.
The reservoir of circulating latent virus, constituted essentially by resting CD4+ lymphocytes, is low (6) and formed as early as 10 days after the first clinical signs of primary infection (7). Therefore, in our patients with primary infection, the proviral load measurements at D0 already include the latent reservoir. Nevertheless, this probably only represents a minor fraction of the total, compared to proviral HIV-1 DNA of activated circulating cells, with which there is intensive viral replication in the primary infection phase (9, 11). The significant decrease in the proviral load observed between D0 and M12 is, therefore, certainly not solely due to a reduction in the latent reservoir but is essentially linked to a progressive decrease in the number of activated, virus-replicating CD4+ cells. Ibanez et al. reported a significant decrease in proviral HIV-1 DNA 48 weeks after the initiation of HAART in 10 drug-naive patients (22). They also found that integrated proviral HIV-1 DNA in latent cells did not decrease in a parallel manner. Our method does not differentiate between nonintegrated and integrated proviral HIV-1 DNA. Thus, the data obtained at M12 reflect viral reservoirs of latent cells or cells with a low level of viral replication, as an ongoing, low level of replication could be found even when HIV-1 RNA was undetectable in plasma (14, 31).
At M12, quantitative cellular viremia gave negative results for all the patients tested, while for 13 of these patients proviral HIV-1 DNA could still be detected. The TaqMan technique is therefore more sensitive than quantitative cellular viremia for exploring the proviral load. The persistence of proviral HIV-1 DNA, as previously reported (27, 28), could indicate that there is a risk of a rapid rebound of viral replication if therapy is discontinued, as shown by several studies (16, 17, 21, 33).
In this study proviral HIV-1 DNA has been quantified in only two lymphoid tissue biopsy specimens. These preliminary results suggest that TaqMan PCR could also be used to measure the proviral load in the lymphoid compartment. However, further longitudinal studies including a large number of patients are needed to assess the usefulness and the clinical significance of this marker.
As TaqMan real-time PCR enables the rapid and easy processing of a large number of samples, the HIV-1 proviral load can be used as a routine tool for the longitudinal monitoring of patients. This marker is particularly interesting when HIV-1 RNA is no longer detectable in plasma, allowing the degree of residual replication and latent viral reservoirs under antiretroviral treatment to be assessed.
ACKNOWLEDGMENTS
This work was supported by the UPRES EA 2391 (Unité Pour La Recherche et l'Enseignement Scientifique) and in part by grants from ARVIH (Association de Recherche sur le VIH) and Glaxo Wellcome.
We thank S. Yerly and L. Perrin for helpful discussion about the primer's design and P. Mariot for technical assistance.
REFERENCES
- 1.Altschul S F, Madden T L, Schaffer A A, Zhang J, Zhang Z, Miller W, Lipman D J. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aoki S, Yarchoan R, Thomas R V, Pluda J M, Marczyk K, Broder S, Mitsuya H. Quantitative analysis of HIV-1 proviral DNA in peripheral blood mononuclear cells from patients with AIDS or ARC: decrease of proviral DNA content following treatment with 2′,3′-dideoxyinosine (ddI) AIDS Res Hum Retrovir. 1990;6:1331–1339. doi: 10.1089/aid.1990.6.1331. [DOI] [PubMed] [Google Scholar]
- 3.Bruisten S M, Reiss P, Loeliger A E, van Swieten P, Schuurman R, Boucher C A, Weverling G J, Huisman J G. Cellular proviral HIV type 1 DNA load persists after long-term RT-inhibitor therapy in HIV type 1 infected persons. AIDS Res Hum Retrovir. 1998;14:1053–1058. doi: 10.1089/aid.1998.14.1053. [DOI] [PubMed] [Google Scholar]
- 4.Brun-Vezinet F, Boucher C, Loveday C, Descamps D, Fauveau V, Izopet J, Jeffries D, Kaye S, Krzyanowski C, Nunn A, Schuurman R, Seigneurin J M, Tamalet C, Tedder R, Weber J, Weverling G J. HIV-1 viral load, phenotype, and resistance in a subset of drug-naive participants from the Delta trial. The National Virology Groups. Delta Virology Working Group and Coordinating Committee. Lancet. 1997;350:983–990. doi: 10.1016/s0140-6736(97)03380-1. [DOI] [PubMed] [Google Scholar]
- 5.Christopherson C, Kidane Y, Conway B, Krowka J, Sheppard H, Kwok S. PCR-based assay to quantify human immunodeficiency virus type 1 DNA in peripheral blood mononuclear cells. J Clin Microbiol. 2000;38:630–634. doi: 10.1128/jcm.38.2.630-634.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chun T W, Carruth L, Finzi D, Shen X, DiGiuseppe J A, Taylor H, Hermankova M, Chadwick K, Margolick J, Quinn T C, Kuo Y H, Brookmeyer R, Zeiger M A, Barditch-Crovo P, Siliciano R F. Quantification of latent tissue reservoirs and total body viral load in HIV-1 infection. Nature. 1997;387:183–188. doi: 10.1038/387183a0. [DOI] [PubMed] [Google Scholar]
- 7.Chun T W, Engel D, Berrey M M, Shea T, Corey L, Fauci A S. Early establishment of a pool of latently infected, resting CD4(+) T cells during primary HIV-1 infection. Proc Natl Acad Sci USA. 1998;95:8869–8873. doi: 10.1073/pnas.95.15.8869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chun T W, Stuyver L, Mizell S B, Ehler L A, Mican J A, Baseler M, Lloyd A L, Nowak M A, Fauci A S. Presence of an inducible HIV-1 latent reservoir during highly active antiretroviral therapy. Proc Natl Acad Sci USA. 1997;94:13193–13197. doi: 10.1073/pnas.94.24.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark S J, Saag M S, Decker W D, Campbell-Hill S, Roberson J L, Veldkamp P J, Kappes J C, Hahn B H, Shaw G M. High titers of cytopathic virus in plasma of patients with symptomatic primary HIV-1 infection. N Engl J Med. 1991;324:954–960. doi: 10.1056/NEJM199104043241404. [DOI] [PubMed] [Google Scholar]
- 10.Comandini U V, Sonnerborg A, Vahlne A, Yun Z. Quantification of HIV-1 proviral DNA from peripheral blood mononuclear cells using a high throughput four-competitor competitive PCR. J Virol Methods. 1997;69:171–180. doi: 10.1016/s0166-0934(97)00153-5. [DOI] [PubMed] [Google Scholar]
- 11.Daar E S, Moudgil T, Meyer R D, Ho D D. Transient high levels of viremia in patients with primary human immunodeficiency virus type 1 infection. N Engl J Med. 1991;324:961–964. doi: 10.1056/NEJM199104043241405. [DOI] [PubMed] [Google Scholar]
- 12.Dickover R E, Donovan R M, Goldstein E, Cohen S H, Bolton V, Huth R G, Liu G Z, Carlson J R. Decreases in unintegrated HIV DNA are associated with antiretroviral therapy in AIDS patients. J Acquir Immune Defic Syndr. 1992;5:31–36. [PubMed] [Google Scholar]
- 13.Escaich S, Ritter J, Rougier P, Lepot D, Lamelin J P, Sepetjan M, Trepo C. Relevance of the quantitative detection of HIV proviral sequences in PBMC of infected individuals. AIDS Res Hum Retrovir. 1992;8:1833–1837. doi: 10.1089/aid.1992.8.1833. [DOI] [PubMed] [Google Scholar]
- 14.Finzi D, Blankson J, Siliciano J D, Margolick J B, Chadwick K, Pierson T, Smith K, Lisziewicz J, Lori F, Flexner C, Quinn T C, Chaisson R E, Rosenberg E, Walker B, Gange S, Gallant J, Siliciano R F. Latent infection of CD4+ T cells provides a mechanism for lifelong persistence of HIV-1, even in patients on effective combination therapy. Nat Med. 1999;5:512–517. doi: 10.1038/8394. [DOI] [PubMed] [Google Scholar]
- 15.Finzi D, Hermankova M, Pierson T, Carruth L M, Buck C, Chaisson R E, Quinn T C, Chadwick K, Margolick J, Brookmeyer R, Gallant J, Markowitz M, Ho D D, Richman D D, Siliciano R F. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science. 1997;278:1295–1300. doi: 10.1126/science.278.5341.1295. [DOI] [PubMed] [Google Scholar]
- 16.Garcia F, Plana M, Vidal C, Cruceta A, O'Brien W A, Pantaleo G, Pumarola T, Gallart T, Miro J M, Gatell J M. Dynamics of viral load rebound and immunological changes after stopping effective antiretroviral therapy. AIDS. 1999;13:F79–F86. doi: 10.1097/00002030-199907300-00002. [DOI] [PubMed] [Google Scholar]
- 17.Girard P M, Schneider V, Dehee A, Mariot P, Jacomet C, Delphin N, Damond F, Carcelain G, Autran B, Saimot A G, Nicolas J C, Rozenbaum W. Treatment interruption after one year of triple nucleoside analog therapy for primary HIV infection. AIDS. 2001;15:275–287. doi: 10.1097/00002030-200101260-00020. [DOI] [PubMed] [Google Scholar]
- 18.Gratzl S, Moroni C, Hirsch H H. Quantification of HIV-1 viral RNA and proviral DNA by isotopic competitive PCR. J Virol Methods. 1997;66:269–282. doi: 10.1016/s0166-0934(97)00064-5. [DOI] [PubMed] [Google Scholar]
- 19.Gulick R M, Mellors J W, Havlir D, Eron J J, Gonzalez C, McMahon D, Richman D D, Valentine F T, Jonas L, Meibohm A, Emini E A, Chodakewitz J A. Treatment with indinavir, zidovudine, and lamivudine in adults with human immunodeficiency virus infection and prior antiretroviral therapy. N Engl J Med. 1997;337:734–739. doi: 10.1056/NEJM199709113371102. [DOI] [PubMed] [Google Scholar]
- 20.Hammer S M, Squires K E, Hughes M D, Grimes J M, Demeter L M, Currier J S, Eron J J, Jr, Feinberg J E, Balfour H H, Jr, Deyton L R, Chodakewitz J A, Fischl M A. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med. 1997;337:725–733. doi: 10.1056/NEJM199709113371101. [DOI] [PubMed] [Google Scholar]
- 21.Harrigan P R, Whaley M, Montaner J S. Rate of HIV-1 RNA rebound upon stopping antiretroviral therapy. AIDS. 1999;13:F59–F62. doi: 10.1097/00002030-199905280-00001. [DOI] [PubMed] [Google Scholar]
- 22.Ibanez A, Puig T, Elias J, Clotet B, Ruiz L, Martinez M A. Quantification of integrated and total HIV-1 DNA after long-term highly active antiretroviral therapy in HIV-1-infected patients. AIDS. 1999;13:1045–1049. doi: 10.1097/00002030-199906180-00007. [DOI] [PubMed] [Google Scholar]
- 23.Izopet J, Tamalet C, Pasquier C, Sandres K, Marchou B, Massip P, Puel J. Quantification of HIV-1 proviral DNA by a standardized colorimetric PCR-based assay. J Med Virol. 1998;54:54–59. doi: 10.1002/(sici)1096-9071(199801)54:1<54::aid-jmv8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 24.Korber B, Hahn B, Foley B, Mellors J W, Leitner T, Myers G, McCutchan F, Kuiken C, Bradac J. HIV sequence compendium 1997. Theoretical Biology and Biophysics Group T10. Los Alamos, N.Mex: Los Alamos National Laboratory; 1997. [Google Scholar]
- 25.Larder B A, Boucher C A B. PCR detection of human immunodeficiency virus drug resistance mutations. In: Persing D H, editor. Diagnostic molecular microbiology: principles and applications. Vol. 1. Washington, D.C.: American Society for Microbiology; 1993. pp. 527–533. [Google Scholar]
- 26.Laurendeau I, Bahuau M, Vodovar N, Larramendy C, Olivi M, Bieche I, Vidaud M, Vidaud D. TaqMan PCR-based gene dosage assay for predictive testing in individuals from a cancer family with INK4 locus haploinsufficiency. Clin Chem. 1999;45:982–986. [PubMed] [Google Scholar]
- 27.Lillo F B, Ciuffreda D, Veglia F, Capiluppi B, Mastrorilli E, Vergani B, Tambussi G, Lazzarin A. Viral load and burden modification following early antiretroviral therapy of primary HIV-1 infection. AIDS. 1999;13:791–796. doi: 10.1097/00002030-199905070-00007. [DOI] [PubMed] [Google Scholar]
- 28.Markowitz M, Vesanen M, Tenner-Racz K, Cao Y, Binley J M, Talal A, Hurley A, Ji X, Chaudhry M R, Yaman M, Frankel S, Heath-Chiozzi M, Leonard J M, Moore J P, Racz P, Nixon D F, Ho D D. The effect of commencing combination antiretroviral therapy soon after human immunodeficiency virus type 1 infection on viral replication and antiviral immune responses. J Infect Dis. 1999;179:527–537. doi: 10.1086/314628. [DOI] [PubMed] [Google Scholar]
- 29.Mellors J W, Rinaldo C R, Jr, Gupta P, White R M, Todd J A, Kingsley L A. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science. 1996;272:1167–1170. doi: 10.1126/science.272.5265.1167. [DOI] [PubMed] [Google Scholar]
- 30.Murphy D G, Gonin P, Fauvel M. Reproducibility and performance of the second-generation branched-DNA assay in routine quantification of human immunodeficiency virus type 1 RNA in plasma. J Clin Microbiol. 1999;37:812–814. doi: 10.1128/jcm.37.3.812-814.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Natarajan V, Bosche M, Metcalf J A, Ward D J, Lane H C, Kovacs J A. HIV-1 replication in patients with undetectable plasma virus receiving HAART. Lancet. 1999;353:119–120. doi: 10.1016/s0140-6736(05)76156-0. [DOI] [PubMed] [Google Scholar]
- 32.Perelson A S, Neumann A U, Markowitz M, Leonard J M, Ho D D. HIV-1 dynamics in vivo: virion clearance rate, infected cell life-span, and viral generation time. Science. 1996;271:1582–1586. doi: 10.1126/science.271.5255.1582. [DOI] [PubMed] [Google Scholar]
- 33.Poggi C, Profizi N, Djediouane A, Chollet L, Hittinger G, Lafeuillade A. Long-term evaluation of triple nucleoside therapy administered from primary HIV-1 infection. AIDS. 1999;13:1213–1220. doi: 10.1097/00002030-199907090-00010. [DOI] [PubMed] [Google Scholar]
- 34.Rouzioux C, Puel J, Agut H, Brun-Vezinet F, Ferchal F, Tamalet C, Descamps P, Fleury H. Comparative assessment of quantitative HIV viraemia assays. AIDS. 1992;6:373–377. doi: 10.1097/00002030-199204000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Sun R, Ku J, Jayakar H, Kuo J C, Brambilla D, Herman S, Rosenstraus M, Spadoro J. Ultrasensitive reverse transcription-PCR assay for quantitation of human immunodeficiency virus type 1 RNA in plasma. J Clin Microbiol. 1998;36:2964–2969. doi: 10.1128/jcm.36.10.2964-2969.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tamalet C, Lafeuillade A, Fantini J, Poggi C, Yahi N. Quantification of HIV-1 viral load in lymphoid and blood cells: assessment during four-drug combination therapy. AIDS. 1997;11:895–901. doi: 10.1097/00002030-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Wong J K, Gunthard H F, Havlir D V, Zhang Z Q, Haase A T, Ignacio C C, Kwok S, Emini E, Richman D D. Reduction of HIV-1 in blood and lymph nodes following potent antiretroviral therapy and the virologic correlates of treatment failure. Proc Natl Acad Sci USA. 1997;94:12574–12579. doi: 10.1073/pnas.94.23.12574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong J K, Hezareh M, Gunthard H F, Havlir D V, Ignacio C C, Spina C A, Richman D D. Recovery of replication-competent HIV despite prolonged suppression of plasma viremia. Science. 1997;278:1291–1295. doi: 10.1126/science.278.5341.1291. [DOI] [PubMed] [Google Scholar]
- 39.Yerly S, Chamot E, Hirschel B, Perrin L H. Quantitation of human immunodeficiency virus provirus and circulating virus: relationship with immunologic parameters. J Infect Dis. 1992;166:269–276. doi: 10.1093/infdis/166.2.269. [DOI] [PubMed] [Google Scholar]
- 40.Zaunders J J, Cunningham P H, Kelleher A D, Kaufmann G R, Jaramillo A B, Wright R, Smith D, Grey P, Vizzard J, Carr A, Cooper D A. Potent antiretroviral therapy of primary human immunodeficiency virus type 1 (HIV-1) infection: partial normalization of T lymphocyte subsets and limited reduction of HIV-1 DNA despite clearance of plasma viremia. J Infect Dis. 1999;180:320–329. doi: 10.1086/314880. [DOI] [PubMed] [Google Scholar]