Abstract
Objective:
To compare the treatment time, outcome, and anchorage loss among orthodontic patients treated by self-ligating brackets (SLBs) and conventional brackets (CBs).
Materials and Methods:
A retrospective cohort study compared 34 patients (SLB group) treated by SmartClip brackets (3M Unitek, Monrovia, Calif) to 35 patients (CB group) treated by conventional preadjusted Victory series brackets (3M Unitek) and ligated by stainless steel wire ligatures. Pretreatment (T1) and posttreatment (T2) lateral cephalograms were traced and analyzed using Pancherz sagittal-occlusion analysis to obtain skeletal and dental changes in the maxilla and the mandible. The dental cast models were assessed by the Peer Assessment Rating (PAR) Index for the treatment outcomes.
Results:
The mean treatment time for SLBs (19.19 months) did not show a statistically significant difference from 21.25 months of CBs; the treatment time and pretreatment PAR scores were strongly correlated. There was no difference in anchorage loss between the SLB and CB groups. There were significant dental and skeletal changes among adolescent orthodontic patients regardless of the bracket used. The lingual inclination of the mandibular incisors in the CB group was 3.62° more than in the SLB group (P < .01).
Conclusions:
The treatment time and anchorage loss are not influenced by the type of bracket used. There are significant dental and skeletal changes among adolescent orthodontic patients regardless of the bracket used. There is significantly greater lingual inclination of mandibular incisors in the CB group than in the SLB group.
Keywords: Self-ligating brackets, Anchorage loss
INTRODUCTION
Self-ligating brackets (SLBs) have several supposed advantages over conventional brackets (CBs) and are recently popular in orthodontic clinics worldwide. Of American orthodontists, 33% reported that more than 70% of their patients were treated using SLBs.1 Passive and active self-ligating appliances with different ligating mechanisms have been introduced, presumably to allow for efficient sliding mechanics by reducing the force required for tooth movement owing to friction reduction and absence of binding of ligatures on the archwire.2
The reported advantages of SLBs over CBs include greater patient comfort during treatment, fewer visits to orthodontists, overall shorter treatment time, improved anchorage stability, less need for extractions, and better outcomes in term of occlusal and facial esthetics.3 Some reported advantages, however, are lacking evidence due to conflicting findings. Whereas some in vitro and retrospective clinical studies reported significant advantages of self-ligating over conventional-ligating brackets,4–6 the prospective clinical studies found no significant differences especially on treatment time and number of visits required for orthodontic treatment.7,8
Extraction of some teeth is indicated to resolve space deficit in conditions with severe crowding and anterior teeth protrusion. Anchorage control is of paramount importance to achieve the treatment goal in extraction cases. There are four anchorage situations defined by the ratio of incisor retraction to molar protraction in the anteroposterior dimension. These include minimum, moderate, maximum, and absolute anchorage.9
The superiority of SLBs over CBs in some aspects is uncertain. Since Victory series and SmartClip brackets have the same tip and torque values, we therefore investigated their effectiveness and efficiency for possible differences between the two bracket systems based on their ligation styles.
Our study aimed at comparing the treatment time, outcome, and anchorage loss among orthodontic patients treated by SLB SmartClip and CB Victory series brackets.
MATERIALS AND METHODS
Ethical approval for the study was obtained from the Jilin University Scientific Committee. We compared groups of patients randomly selected from a pool of completed cases treated by the same investigator at the orthodontic clinic of the Jilin University College of Dentistry between 2007 and 2011. The patients were treated under the same protocol adopted by the institution with the following archwire sequence: nickel titanium 0.012-inch, 0.014-inch, 0.016-inch, 0.018 × 0.025-inch, 0.019 × 0.025-inch, and stainless steel (SS) 0.019 × 0.025-inch in brackets with 0.022 × 0.028-inch slot.
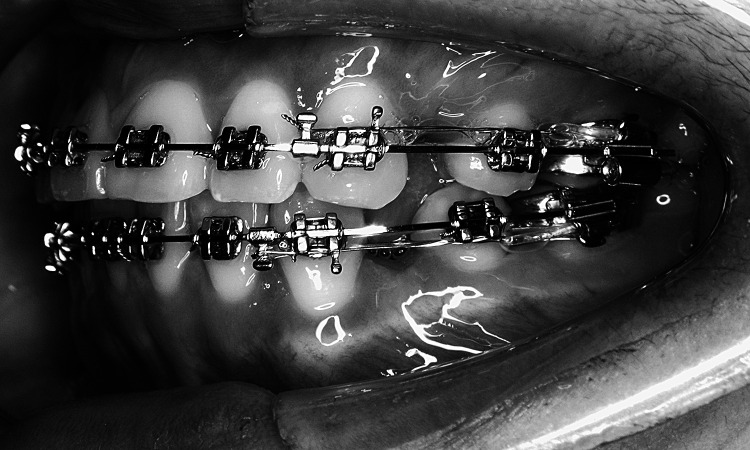
The first group (SLB) consisted of 34 patients treated by SmartClip (3M Unitek, Monrovia, Calif) brackets. The second group (CB) consisted of 35 patients treated by conventional preadjusted Victory series brackets (3M Unitek) tightly ligated with SS 0.020-inch ligatures. During space closure, an elastic chain with SS 0.025-inch ligature wire was tied on the first molar hook to the anterior arch hook placed between the canine and lateral incisor and used for en masse traction of anterior teeth in both the SLB and CB groups (Figure 1). The elastic chains were changed on a monthly appointment basis.
Figure 1. .
Illustration of the force delivery method used during en masse space closure.
The study used patients' case notes to extract demographic information, treatment duration, appointments, and clinical information for inclusion and exclusion criteria. Pretreatment and posttreatment lateral cephalograms and dental cast models were examined for treatment outcome variables.
The requirements for inclusion in this study were patients needing extraction of four first premolars, without transverse discrepancies, use of conventional first molar anchorage, and no previous history of orthodontic or orthognathic surgery.
We excluded cases based on lack of data required for our research, use of additional anchorage reinforcement (mini-implant, head gear, transpalatal arch, lingual arch, intermaxillary elastics, pendulum, twin block, and Nance and any removable appliances during active treatment), missing three or more appointments, and unclear pretreatment or posttreatment lateral cephalograms.
Pretreatment (T1) and posttreatment (T2) lateral cephalograms were traced on acetate paper by the same investigator, and all complete cephalogram tracings were proofread by a second researcher; the two researchers discussed the location of landmarks in cases of uncertainty. Cases with unclear radiographs were excluded. Skeletal changes as well as dental changes in the maxilla and the mandible were obtained using the Pancherz sagittal-occlusion analysis (Figure 2).10 The incisor positions were also investigated by measuring the angle between the maxillary plane and the upper incisors long axis (Ui/Max plane angle), and the angle between the mandibular plane and the lower incisors long axis (Li/Mn plane angle). The cephalogram variables measured were: Ui/Max plane angle (degree), Li/Mn plane angle (degree), maxillary central incisor (Ui-Y) (mm), mandibular central incisor (Li-Y) (mm), maxillary permanent molar (Um-Y) (mm), mandibular permanent molar (Lm-Y) (mm), maxillary base (A-Y) (mm), and mandibular base (Pg-Y) (mm). Measurements were made by hand to the nearest 0.5 mm or 0.5°. Images of bilateral structures were bisected. Changes in the various measuring points were calculated as the difference between the T1 and T2 position.
Figure 2. .
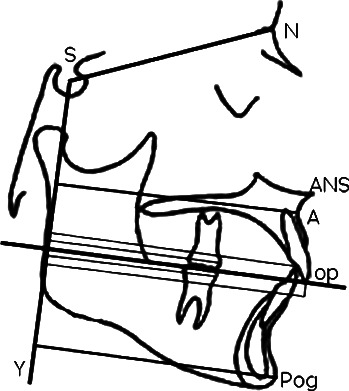
Schematic diagram of linear variables used in Pancherz sagittal cephalogram analysis.
We used the Peer Assessment Rating (PAR) Index to measure the treatment outcome on dental cast models. All measurements were done by the same investigator who was blinded both to bracket type and patient names. Both pretreatment and posttreatment weighted PAR scores were calculated according to the British weightings system, and the overall improvement in PAR score as percentage reduction was computed.
Descriptive and analytical statistical analyses were performed with SPSS for Windows, version 13.0 software (SPSS Inc, Chicago, Ill). The data showed a normal distribution tendency; hence, we applied parametric statistical analysis, with the level of statistical significance set at P < .05. By paired samples t-test, we tested for significant differences between the mean scores of cephalograms variables and PAR scores before and after treatment. The independent sample Student's t-test was used to detect significant differences between mean scores of SLB and CB on treatment duration, percentage PAR score reduction, and cephalogram variable changes.
We randomly selected cephalograms and dental cast models for error study to test the examiner's accuracy and consistency in evaluating the study models and radiographs. Thirty-five cephalograms as well as 30 dental cast models were measured twice at the interval of 5 days to obtain two sets of data. The paired samples t-test showed no significant mean differences between the two series of records, with a method error of less than 0.5 mm and 1.0°.11
RESULTS
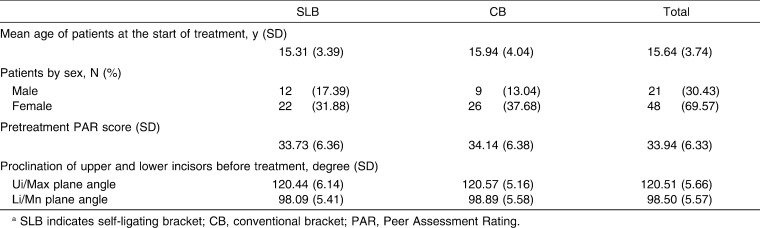
The study included 69 completed cases with mean age of 15.64 ± 3.74 years at the start of treatment. There were no significant group differences by sex, age, pretreatment PAR score, and proclination of incisors. Only 4.8% and 4.0% of participants in the SLB and CB groups, respectively, had skeletal Class II (2-5 mm Wits appraisal of jaw disharmony) occlusion. Severe occlusal discrepancies were not included due to additional orthodontic appliances used sometimes in the course of their treatment. Table 1 shows the sample demographic distribution.
Table 1. .
Demographics of the Sample Groups at the Start of Treatmenta
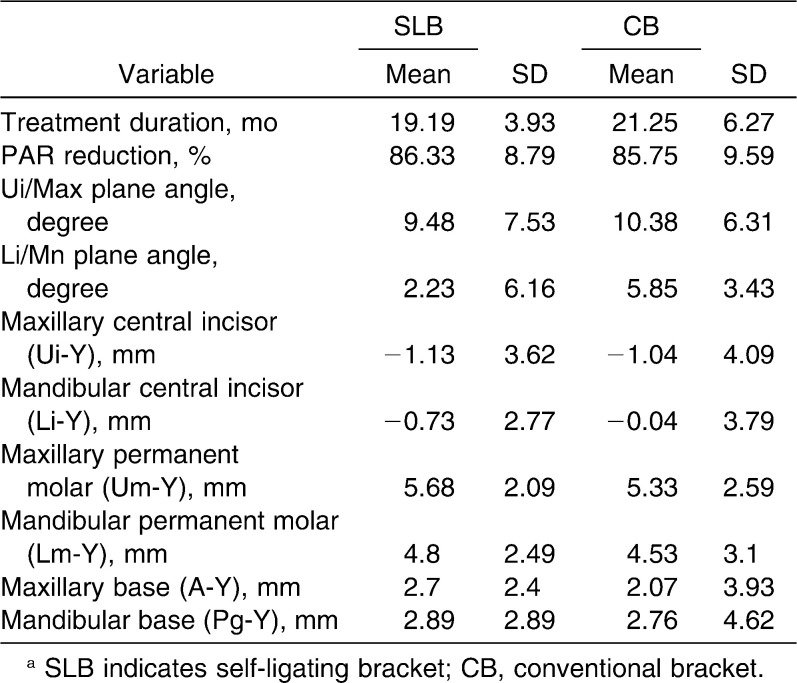
On comparison of the positions of cephalogram points before and after treatment in both the SLB and CB groups, there were significant differences between the T1 and T2 measurements in the SLB group for the positions of the maxillary base, the maxillary central incisor, the maxillary molar, and the mandibular molar, all at P < .001. In the CB group, there were significant differences between the T1 and T2 measurements for the positions of the mandibular base (P < .001), the maxillary molar (P < .001), the mandibular molar (P < .001), and the mandibular central incisor (P = 0.008). The difference in PAR score before and after treatment was not affected by the bracket type used; however, there was strong correlation between the treatment duration and pretreatment PAR score, r = 0.87, P < .001.
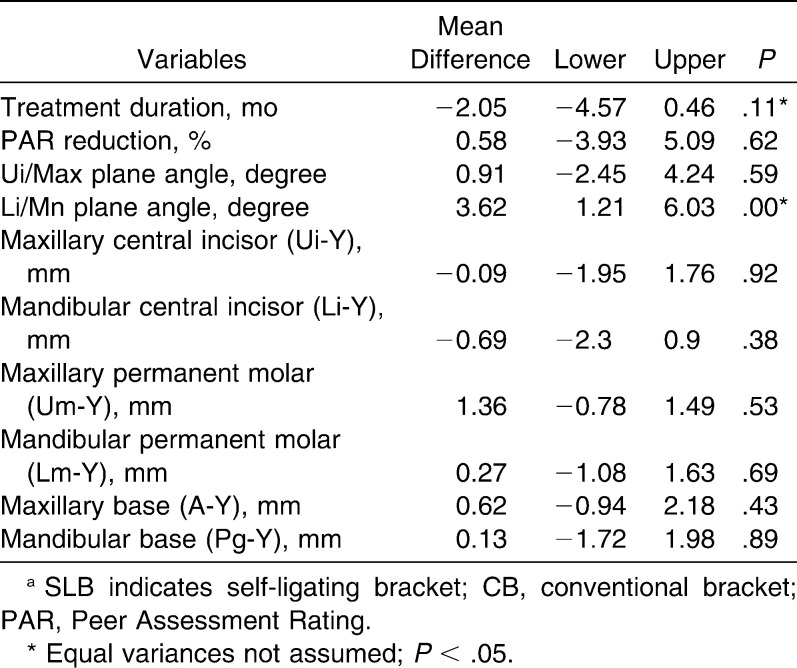
The arithmetic mean and standard deviation for treatment duration percentage PAR reduction and cephalogram variable changes were calculated (Table 2). The independent sample t-test for treatment duration, reduction in PAR score, and cephalogram variable changes are shown in Table 3.
Table 2. .
The Mean and Standard Deviation for Treatment Duration, Peer Assessment Rating (PAR) Reduction, and Cephalometric Variable Changes After Treatmenta
Table 3. .
Differences in Treatment Changes Between SLB and CB Groups (34 SLB and 35 CB Patients), Independent Samples t-testa
DISCUSSION
Very low friction with self-ligating brackets has been demonstrated clearly and quantified in work by various authors.12,13 It is assumed, therefore, that low friction in vitro, is associated with more rapid space closure and reduced treatment time in vivo. The results of this study demonstrate that the time required to complete orthodontic treatment is not significantly different between the passive SmartClip brackets and the conventional Victory series brackets tied with stainless steel ligatures (Table 3).
Although some previous studies have reported up to 6 months of treatment time reduction by SLBs,5,6 our finding is in keeping with other studies that found no differences in treatment time between the two bracket systems.7,14 The differences in average treatment durations may be due to different criteria for ending active treatment and type of patients enrolled in the studies. Our study found 2.06 months of treatment time reduction by self-ligating brackets; this difference, however, is not statistically significant. Although the mean PAR reduction is not affected by the bracket type in this study (Table 3), there is strong positive correlation between treatment time and pretreatment PAR score. The higher the pretreatment PAR score, the longer the time required for completing orthodontic treatment. The findings are consistent with the randomized clinical trial by DiBiase et al.,7 and other authors who reported the degree of tooth displacement rather than bracket type to be the most significant factor influencing alignment rate.14,15
Anchorage conservation is among the said advantages of self-ligating over conventional brackets.6,16 Friction reduction during sliding mechanics is supposed to reduce the force needed to move teeth during orthodontic treatment, which in turn lowers the reciprocal force on anchor tooth or unit. This phenomenon is expected to improve anchorage and favor physiologic tooth movement, which may produce more stable treatment outcome.16
Although there was significant mesial movement of first molars in both self-ligating and conventional brackets in our study, the loss of anchorage between the two groups was not significantly different (Table 3). The results in this retrospective study may be affected by unrecorded additional arch wire bending and interarch elastics use during treatment. However, we went through all dental record details to exclude all possible factors that could cause bias this study, as mentioned in our methodology. Mezomo et al.17 in a clinical study reported no anchorage differences between self-ligating and conventional brackets. They, however, reported lower average loss of anchorage since the anchor was against canine retraction as opposed to en masse traction in our study. Other studies have reported one third of the mesial movement of posterior teeth onto the first premolar extraction.18,19
The loss of anchorage in this research is higher in the maxilla than mandible for both SLB and CB groups; this may be explained by the well-known fact of the maxilla having lower bone density than the mandible.20,21 Clinicians should expect more anchorage loss in the maxilla than in the mandible; hence, relatively more effort is required to enforce anchorage in the maxilla than in the mandible during orthodontic treatment.
We assessed changes in the cephalometric variables before and after treatment irrespective of the bracket type. We noted mesial displacement for the skeletal landmark points A and Pg. The changes were not significantly different between bracket types, but the skeletal changes are not a surprise due to growth potential among adolescent patients making up the sample mean age of 15.64 years. It is also consistent with the observation by Urias and Mustafa.22 These skeletal changes were taken into account by employing the Pancherz cephalogram analysis, which allows for detection of tooth movement within the jaw despite skeletal growth changes.10
The proclination of the lower incisors, measured by the change in angle between the mandibular plane and the lower incisors long axis, showed significant difference between the two bracket systems. There was more lingual inclination in the CB group by an average of 5.85° angle reduction compared to 2.23° in the SLB group. We also noted 0.9° greater reduction of the angle between the upper incisors and the maxillary plane in the CB group, which was not significantly different.
Although our findings may be influenced by the multiple factors determining torque expression in the clinical situation like the interbracket distance23 and vertical positioning of the brackets on the tooth,24,25 the observation may be attributed to difference in archwire-slot interaction of the two bracket systems; the stainless steel wire ligature keeps the arch wire tighter in the slot than the passive SmartClip SLB. An active ligating mechanism seems to reduce the amount of archwire play in the bracket slot.26 The −6° torque MBT Versatile+ appliance prescription for lower incisors rotates the tooth on the long axis moving the crown in the lingual direction. More lingual inclination in the CB group may be the result of better torque expression in this group than in the SLB group. This may be one of the reasons for the observation.
Since there are manufacturer-reported reported differences in the 0.022-inch slot size,27 the manufacturing slot size dimension difference between the CBs and SLBs may be another possible explanation for the difference in torque expression observed in the study.
The results of this study are not in agreement with an investigation that examined maxillary central incisor inclination with conventional and Damon brackets and reported no significant torque difference on incisors among patients treated by the two types of appliances.28 This observation is probably due to the difference in torque values between CBs with Roth prescription and the Damon SLBs compared to the brackets with MBT prescription used in our research.
Because one person treated all patients with the same standards of bracket positioning and treatment protocols and the strict inclusion criteria, we are optimistic that our study is reliable. The findings are consistent with Morina et al.29 and Fleming et al.30 Self-ligating brackets are reported to present reduced torquing moments compared with conventional brackets in experimental studies; however, this is difficult to confirm in clinic due to multiple factors in play.
Both the SLBs and CBs used in this study have MBT Versatile+ Appliance prescription (ie, −6° torque, 0° tip, and 1.5 mm in/out for all mandibular incisors). Our findings highlight the possibility of reaching different torque based on the bracket ligation system despite having the same torque and tip prescription.
CONCLUSIONS
The treatment time, percentage PAR reduction, and anchorage loss are not influenced by the type of bracket.
There are significant dental and skeletal changes among adolescent orthodontic patients regardless of the bracket used.
There is more lingual inclination of mandibular incisors in the CB group than in the SLB group.
REFERENCES
- 1.Prettyman C, Best AM, Lindauer SJ, Tufekci E. Self-ligating vs conventional brackets as perceived by orthodontists. Angle Orthod. 2012 Mar 12 doi: 10.2319/101311-640.1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harradine NW. Self-ligating brackets: where are we now. J Orthod. 2003;30:262–273. doi: 10.1093/ortho/30.3.262. [DOI] [PubMed] [Google Scholar]
- 3.Loh KW. Rapid tooth movement with a low-force, low-friction bracket system. J Clin Orthod. 2007;41:451–457. [PubMed] [Google Scholar]
- 4.Damon DH. The Damon low friction bracket: a biologically compatible straight-wire system. J Clin Orthod. 1998;32:670–680. [PubMed] [Google Scholar]
- 5.Eberting JJ, Straja SR, Tuncay OC. Treatment time, outcome, and patient satisfaction comparisons of Damon and conventional brackets. Clin Orthod Res. 2001;4:228–234. doi: 10.1034/j.1600-0544.2001.40407.x. [DOI] [PubMed] [Google Scholar]
- 6.Harradine NW. Self-ligating brackets and treatment efficiency. Clin Orthod Res. 2001;4:220–227. doi: 10.1034/j.1600-0544.2001.40406.x. [DOI] [PubMed] [Google Scholar]
- 7.DiBiase TA, Nasr HI, Scott P, Cobourned TM. Duration of treatment and occlusal outcome using Damon3 self-ligated and conventional orthodontic bracket systems in extraction patients: a prospective randomized clinical trial. Am J Orthod Dentofacial Orthop. 2011;139:e111–e116. doi: 10.1016/j.ajodo.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Ong E, McCallum H, Griffin PM, Ho C. Efficiency of self-ligating vs conventionally ligated brackets during initial alignment. Am J Orthod Dentofacial Orthop. 2010;138:138.e1–138.e7. doi: 10.1016/j.ajodo.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Baumgaertel S, Razavi RM, Hans GM. Mini-implant anchorage for the orthodontic practitioner. Am J Orthod Dentofacial Orthop. 2008;133:621–627. doi: 10.1016/j.ajodo.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod. 1982;82:104–113. doi: 10.1016/0002-9416(82)90489-4. [DOI] [PubMed] [Google Scholar]
- 11.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: Allen and Unwin; 1940. pp. 122–132. [Google Scholar]
- 12.Sims APT, Waters NE, Birnie DJ. A comparison of the forces required to produce tooth movement ex vivo through three types of preadjusted brackets when subjected to determined tip or torque values. Br J Orthod. 1994;21:367–373. doi: 10.1179/bjo.21.4.367. [DOI] [PubMed] [Google Scholar]
- 13.Berger JL. The influence of the SPEED bracket's self-ligating design on force levels in tooth movement: a comparative in vitro study. Am J Orthod Dentofacial Orthop. 1990;97:219–228. doi: 10.1016/S0889-5406(05)80055-1. [DOI] [PubMed] [Google Scholar]
- 14.Fleming PS, DiBiase AT, Lee RT. Randomized clinical trial of orthodontic treatment efficiency with self-ligating and conventional fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;137:738–742. doi: 10.1016/j.ajodo.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 15.Scott P, DiBiase AT, Sherriff M, Cobourne MT. Alignment efficiency of Damon3 self-ligating and conventional orthodontic bracket systems: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2008;134:470:e1–e8. doi: 10.1016/j.ajodo.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Pandis N, Polychronopoulou A, Eliades T. Self-ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. Am J Orthod Dentofacial Orthop. 2007;132:208–215. doi: 10.1016/j.ajodo.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 17.Mezomo M, Lima ES, Menezes LM, Weissheimer A, Allgayer S. Maxillary canine retraction with self-ligating and conventional brackets: a randomized clinical trial. Angle Orthod. 2011;81:292–297. doi: 10.2319/062510-348.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams R, Hosila FJ. The effect of different extraction sites upon incisor retraction. Am J Orthod. 1976;69:388–410. doi: 10.1016/0002-9416(76)90208-6. [DOI] [PubMed] [Google Scholar]
- 19.Creekmore TD. Where teeth should be positioned in the face and jaws and how to get them there. J Clin Orthod. 1997;31:586–608. [PubMed] [Google Scholar]
- 20.Park HS, Lee YJ, Jeong SH, Kwon TG. Density of the alveolar and basal bones of the maxilla and the mandible. Am J Orthod Dentofacial Orthop. 2008;133:30–37. doi: 10.1016/j.ajodo.2006.01.044. [DOI] [PubMed] [Google Scholar]
- 21.Seong JW, Kim KU, Swift QJ, Heo CY, Hodges SJ, Ko CC. Elastic properties and apparent density of human edentulous maxilla and mandible. Int J Oral Maxillofac Surg. 2009;38:1088–1093. doi: 10.1016/j.ijom.2009.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Urias D, Mustafa IAF. Anchorage control in bioprogressive vs straight-wire treatment. Angle Orthod. 2005;75:987–992. doi: 10.1043/0003-3219(2005)75[987:ACIBVS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Jarabak JR, Fizzel JA. Technique and Treatment With LightWire Edgewise Appliances Vol I and II 2nd ed. St Louis, Mo: Mosby; 1972. [Google Scholar]
- 24.Meyer M, Nelson G. Preadjusted edgewise appliances: theory and practice. Am J Orthod Dentofacial Orthop. 1987;73:485–498. doi: 10.1016/0002-9416(78)90239-7. [DOI] [PubMed] [Google Scholar]
- 25.Miethke RR. Third order tooth movements with straight wire appliances. Influence of vestibular tooth crown morphology in the vertical plane. J Orofac Orthop. 1997;58:186–197. doi: 10.1007/BF02679959. [DOI] [PubMed] [Google Scholar]
- 26.Badawi MH, Toogood WR, Carey RPJ, Heo G, Majore WP. Torque expression of self-ligating brackets. Am J Orthod Dentofacial Orthop. 2008;133:721–728. doi: 10.1016/j.ajodo.2006.01.051. [DOI] [PubMed] [Google Scholar]
- 27.Cash AC, Good SA, Curtis RV, McDonald F. An evaluation of slot size in orthodontic brackets—are standards as expected. Angle Orthod. 2004;74:450–453. doi: 10.1043/0003-3219(2004)074<0450:AEOSSI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Pandis N, Strigou S, Eliades T. Maxillary incisor torque with conventional and self-ligating brackets: a prospective clinical trial. Orthod Craniofac Res. 2006;9:193–198. doi: 10.1111/j.1601-6343.2006.00375.x. [DOI] [PubMed] [Google Scholar]
- 29.Morina E, Eliades T, Pandis N, Jäger A, Bourauel C. Torque expression of self-ligating brackets compared with conventional metallic, ceramic, and plastic brackets. Eur J Orthod. 2008;30:233–238. doi: 10.1093/ejo/cjn005. [DOI] [PubMed] [Google Scholar]
- 30.Fleming SP, DiBiase TA, Sarri G, Leed TR. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009;136:340–347. doi: 10.1016/j.ajodo.2007.08.030. [DOI] [PubMed] [Google Scholar]