Abstract
Objective:
To evaluate the dentoskeletal changes of Class II malocclusion treatment with the Twin Force Bite Corrector (TFBC).
Materials and Methods:
The sample comprised 86 lateral cephalograms obtained from 43 subjects with Class II division 1 malocclusion; the subjects were divided into two groups. The experimental group comprised 23 patients with a mean initial age of 12.11 years who were treated with the TFBC for a mean period of 2.19 years. The control group included 40 lateral cephalograms from 20 Class II nontreated patients, with an initial mean age of 12.55 years and a mean observation period of 2.19 years. The lateral cephalograms were evaluated before and after orthodontic treatment in group 1 and in the beginning and end of the observation period in group 2. t-Tests were used to compare the initial and final cephalometric characteristics of the groups as well as the amount of change.
Results:
The experimental group presented greater maxillary growth restriction and mandibular retrusion than the control group, as well as greater maxillomandibular relationship improvement and greater labial tipping of the mandibular incisors. The results also showed a greater decrease in overbite and overjet in the experimental group, and there were no statistically significant differences in the craniofacial growth pattern between groups.
Conclusions:
The TFBC promotes restriction of anterior maxillary displacement without significant changes in mandibular length and position and improvement of maxillomandibular relationship without changes in facial growth and significant buccal tipping of mandibular incisors. Class II correction with the TFBC occurred primarily as a result of dentoalveolar changes.
Keywords: Class II, Functional appliances
INTRODUCTION
Recently, the use of fixed, rather than removable, functional appliances has been advocated; the fixed appliance ensures that a constant anterior positioning of the mandible is maintained during the treatment period. Furthermore, evidence1,2 has indicated that use of a one-phase protocol in the permanent dentition is more efficient than use of a two-phase protocol since similar occlusal results are achieved in a shorter treatment time.
Accordingly, several intermaxillary fixed appliances have been developed and applied for Class II malocclusion treatment, mainly in the permanent dentition. These appliances promote mandibular protrusion with reciprocal distal forces in the maxillary arch.3–5 Among these appliances, the Twin Force Bite Corrector (TFBC; Ortho Organizers Inc, Carlsbad, Calif) is a hybrid fixed functional appliance that has a plunger system combined with active push coils that deliver a constant force of approximately 210 g.6,7
Consider that several successful reports of nonextraction Class II treatment are described in the orthodontic literature3,6,8 using either fixed/removable and intra- or extraoral appliances to promote mandibular protrusion. Currently, a few studies6,7 have been conducted to assess the dentoskeletal changes of the TFBC appliance, but none of these studies have evaluated the treatment effects of the TFBC appliance compared to a control sample. Therefore, the objective of this prospective study was to evaluate the dentoskeletal changes resulting from Class II malocclusion treatment with the TFBC compared to changes within an untreated Class II control sample.
MATERIALS AND METHODS
Ethical approval was obtained from the Ethics Research Committee of the Bauru Dental School, University of São Paulo, Brazil, before the study was conducted. A power analysis was performed to determine the required sample size. According to the power analysis at α = .05 significance level and 80% power (based on 1.6-mm standard deviation and 2.0-mm detectable group difference), the minimum sample size needed for each group was 19. The patients were selected to begin orthodontic treatment based on the following criteria: all patients should present with at least a bilateral half–Class II molar relationship, with a minimum of 4 mm of overjet (OVJ), absence of agenesis or loss of permanent teeth up to the first molars, absence of supernumerary teeth, convex facial profile, mandibular arch with minimal (4 mm) or no crowding, and without having undergone any previous orthodontic treatment.
Of the 30 initially selected patients, five patients dropped out of treatment (dropout rate of 16.6%), and two patients were excluded from the sample in order to match the experimental and control groups with regard to initial age and gender distribution. Consequently, the experimental group comprised 23 patients. Patients for the experimental group were collected from two different centers and were treated by two different operators. No extractions were performed in any patient; patients were treated until Class I molar and canine relationships and a satisfactory OVJ were obtained. The control group was selected from a longitudinal growth study sample from the files of the orthodontic department at Bauru Dental School, University of São Paulo, Brazil, with the following characteristics: subjects with Class II division 1 malocclusion, with absence of agenesis or loss of permanent teeth, absence of supernumerary teeth, who had not undergone any previous orthodontic treatment.
The total sample comprised 86 lateral cephalograms (corresponding to initial [T1] and final [T2] cephalograms) obtained from 43 subjects who were divided into two groups. The experimental group (group 1) was composed of 46 lateral cephalograms from 23 patients (10 males, 13 females) with Class II division 1 malocclusion treated with the TFBC associated with fixed appliances, with a mean initial age of 12.11 years (range, 9.66–14.58 years). The total treatment time was 2.19 years (range, 0.58–3.91 years), with a mean period of utilization of the appliance TFBC of 0.24 years (range, 0.08–0.33 years). The mean final patient age was 14.29 years (range, 11.33–16.50 years).
The control group (group 2) was composed of 40 lateral cephalograms from 20 nontreated Class II division 1 subjects (10 males, 10 females) with an initial mean age of 12.55 years (range, 11.21–13.90 years) and a mean final age of 14.73 years (range, 12.32–19.11 years). The mean observation period was 2.19 years (range, 0.56–6.58 years). Furthermore, according to cervical vertebrae maturation (CVM), both groups were between stage 2 and stage 4 at T1.
Clinical Materials
The TFBC has two plunger/telescopic tube assemblies applied bilaterally, with a total length of 16 mm, with the nickel-titanium coil spring delivering a total protraction force of nearly 210 g (Figure 1).6,7 The appliance is attached to the arch by ball-and-socket joint fasteners, which allow free lateral mandibular movements. The plungers' compression reduces the appliance length in 15 mm, and at full compression the TFBC delivers the force that carries the mandible into an anterior edge-to-edge occlusion. Like other fixed intermaxillary appliances, it is used full time because it is not subject to patient compliance.9
Figure 1. .
Intrabuccal photographs of a patient with a Twin Force Bite Corrector.
Before delivering the TFBC, the orthodontic mechanics included fixed Roth preadjusted braces with 0.022 × 0.028–inch slots and archwires that were progressively increased until 0.019 × 0.025–inch stainless-steel wires could be used in both arches. In order to counteract the buccal flaring of the maxillary molars with the use of the TFBC appliance, a transpalatal arch was placed, and both archwires ends were cinched back 90° against the distal side of the molar tubes. The mandibular molars, premolars, and canines were connected with 0.010-inch metal ligature before the rectangular archwire placement, and premolars, canines, and incisors were individually tied to the archwire with metal ligatures. Elastic chain was used in the mandibular arch to prevent incisor flaring.
After the Class II correction with the TFBC, Class II intermaxillary elastics were used as an active retainer for an additional 3 months.6
Cephalometric Records
Two lateral cephalograms from each patient were analyzed at the initial (T1) and final (T2) examinations. Given the long time span between the two intragroup and intergroup stages, the lateral head films were obtained with several x-ray machines, and different magnification factors of the images were produced—ranging between 6% and 9.8%. After the magnification factors were calculated, the cephalometric program corrected the magnification for enlargement.
The cephalometric tracings and landmark identification were performed on acetate paper by a single investigator and were then digitized with a Numonics AccuGrid XNT (model A30TLF digitizer, Numonics, Montgomeryville, Pa). The skeletal measurements and dental relationships performed are illustrated in Figures 2 and 3. These data were stored on a computer and analyzed with Dentofacial Planner 7.02 (Dentofacial Planner Software, Toronto, Ontario, Canada).
Figure 2. .
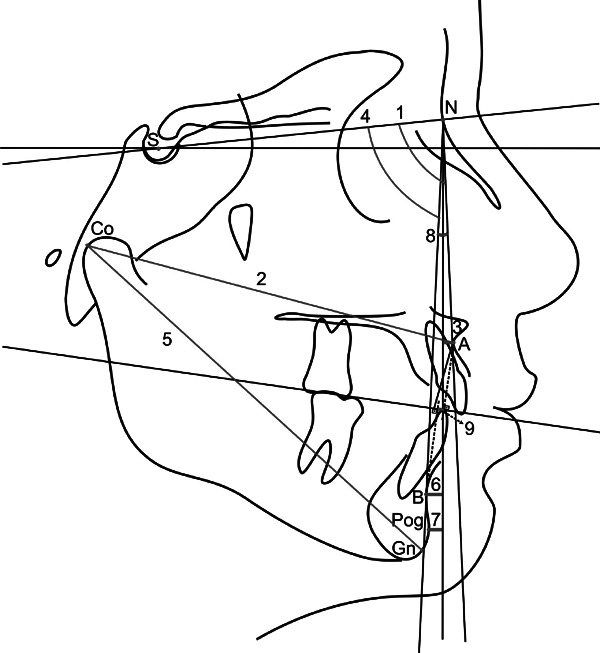
Skeletal measurements. (1) SNA. (2) Co-A. (3) A-N pFHc: Distance between the A point to a perpendicular line to SN7, through the N point. (4) SNB. (5) Co-Gn. (6) B-N pFHc: Distance between the B point to a perpendicular line to SN7, through the N point. (7) P-N pFHc: Distance between the P point to a perpendicular line to SN7, through the N point. (8) ANB. (9) Wits.
Figure 3. .
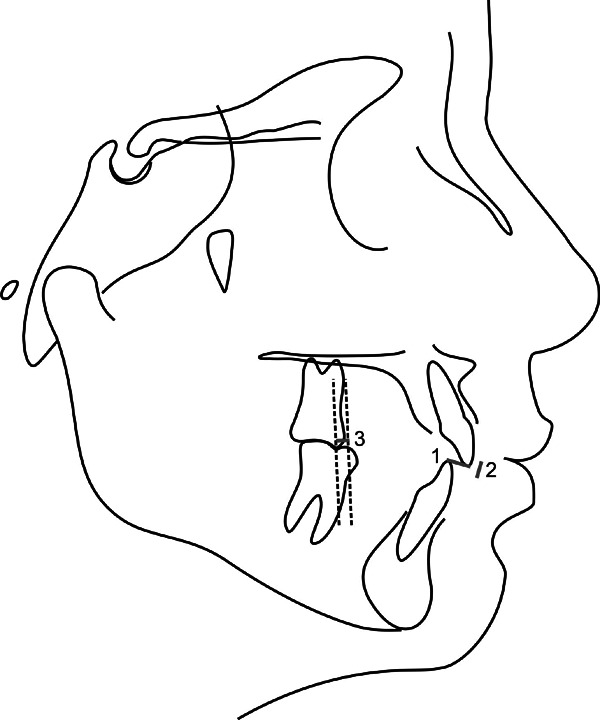
Dental relationships: (1) Overjet (OVJ): Distance between the incisal edge of mandibular incisor to the incisal edge of maxillary incisor, parallel to functional occlusal plane. (2) Overbite (OVB): Distance between the incisal edge of mandibular incisor to the incisal edge of maxillary incisor, perpendicular to occlusal plane. (3) Molar relationship: Distance between the mesial surface of first mandibular molar to the mesial surface of the first maxillary molar parallel to occlusal plane.
In the experimental group, the treatment evaluation was calculated by subtracting the final from the initial values (T2 − T1). In the control group, the evaluation comprised the difference between the final and initial measurements.
Error of the Study
The reliability of the measurements was assessed by randomly selecting 15 lateral cephalograms from the two study groups; these were traced and digitized by the same examiner a second time a month after the first evaluation. Systematic errors were evaluated with paired t-tests at P < .05, and casual errors were calculated according to Dahlberg's formula (Se2 = Σd2/2n), in which Se2 is the error variance and d is the difference between two determinations of the same variable.10
Statistical Analysis
Compatibility of the groups with regard to the distributions of gender was evaluated with chi-square tests. t-Tests were used to compare the ages of patients in the groups at T1 and T2 and during the observation period. Means and standard deviations for each cephalometric variable were calculated to enable characterization of both groups. In order to apply the t-test, a normal distribution was verified with the Kolmogorov-Smirnov test. Results of this test demonstrated that all cephalometric variables presented a normal distribution (for initial and final values, as well as for the changes). Therefore, t-tests were also used to compare the initial and final cephalometric characteristics and the stages' differences of the groups (T2-T1).
The results were regarded as significant at P < .05. All of the analyses were performed with Statistica Software (Statistica for Windows 6.0, Statsoft, Tulsa, Okla).
RESULTS
The systematic errors were significant for five of 25 measurements (Mx1.PP, Mx1-PP, Mx6-PP, Mx6-PTV, and Md1-MP), and the casual errors ranged from 0.10 (OVJ) to 1.12 (NS.GoGn).
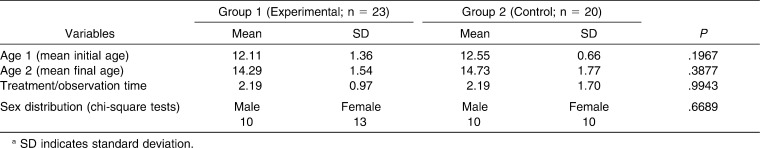
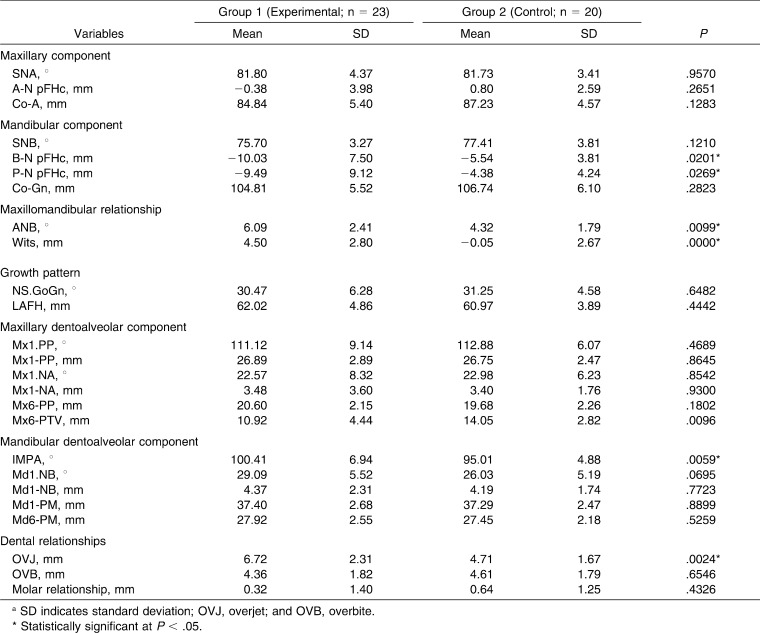
The groups were compatible with regard to initial and final ages, observation period, gender distribution (Table 1), overbite (OVB), molar relationship, and in most of the cephalometric variables, except for B-NpFHc, P-NpFHc, ANB, Wits, IMPA, and OVJ, which presented greater values in the experimental group (Table 2). They were also not compatible with regard to Mx6-PTV, which was greater in the control group (Table 2).
Table 1. .
Results of the Intergroup Compatibility Tests (t- and Chi-Square Tests)a
Table 2. .
Comparison of the Cephalometric Variables at the Initial Stage (T1) (Independent t-Test)a
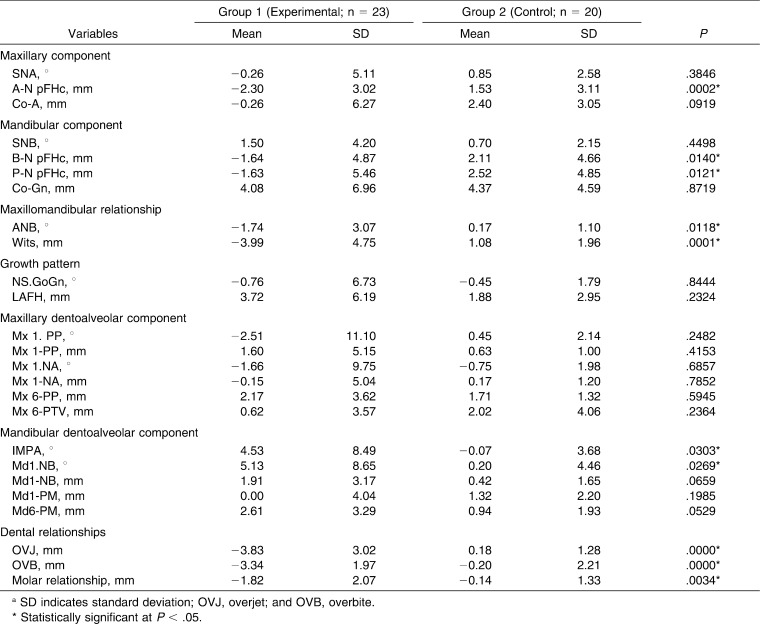
During treatment, group 1 had significantly greater maxillary forward displacement restriction (A-NpFHc), greater mandibular retrusion (B-N pFHc and P-N pFHc), and greater maxillomandibular correction (ANB and Wits) than did the control group. This group also presented greater mandibular incisor labial tipping (IMPA and Md1.NB) and greater OVJ, OVB, and molar relation correction than did the control group (Table 3).
Table 3. .
Intergroup Comparison of Changes (Final Stage [T2] − Initial Stage [T1]) (Independent t-Test)a
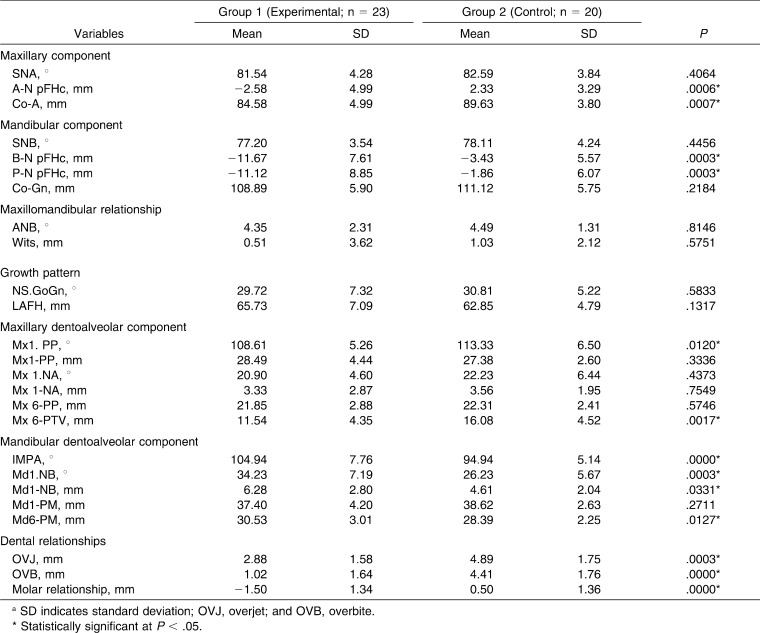
In the final stage, group 1 showed less maxillary forward displacement and length (A-N pFHc and Co-A), greater mandibular retrusion (B-N pFHc and P-N pFHc), greater maxillary palatal tipping (Mx1.PP), more distal maxillary molar position (Mx6-PTV), greater mandibular incisor labial tipping and protrusion (IMPA, Md1.NB and Md1-NB), and greater mandibular molar vertical development (6-MP). This group also presented greater correction of OVJ, OVB, and molar relationship (Table 4).
Table 4. .
Comparison of Cephalometric Variables at the Final Stage (T2) (Independent t-Test)a
DISCUSSION
Although both groups were similar with regard to age, observation time, and gender distribution, no effort was made to match the groups with regard to the initial cephalometric characteristics (ie, only seven variables among 25 showed statistically significant differences between them). It can be assumed that the groups were reasonably matched (Tables 1 and 2). Moreover, on assessing skeletal maturity at T1 according to the CVM, both groups were at a similar stage (CVM 2 to 4). At T1, the experimental group had statistically greater mandibular retrusion (B-NpFHc, P-NpFHc), worse maxillomandibular relationship (ANB, Wits), greater distal position of the maxillary molar (Mx6-PTV), and mandibular incisor labial tipping (IMPA) and greater OVJ than the control group (Table 2). This indicates that Class II malocclusion was more severe in the experimental group than in the control group. This is likely related to ethical aspects concerning Class II control groups, since a severe Class II malocclusion would require a high-priority orthodontic intervention.11–13
During treatment, in the experimental group there was greater anterior displacement restriction of the maxilla than in the control group, since the TFBC promotes a distal force to the maxilla and the maxillary teeth (Table 3). This effect is often observed with the use of fixed functional appliances, and it is reported to be a “headgear effect,”14–16 which helps to correct the Class II relationship. At T2, the maxilla also presented with a small length and retrusion (Table 4).
In addition, in the experimental group, the mandibular retrusion was greater than in the control group before and after treatment (B-N pFHc and P-N pFHc). As TFBC is an appliance that promotes mandibular protrusion, it could be expected that we would note better mandibular position in the experimental group than in the control group. The mandibular protrusion was not greater, most likely because of the clockwise rotation (Figure 4) of the mandible that was responsible for an increase of 3.72 mm in LAFH.7,17,18 Moreover, the TFBC was used for a short period of time of 0.24 years, with predominantly dentoalveolar changes, rather than skeletal effects. In relation to mandibular component, the SNB angle increased 1.50° and the mandibular length (Co-Gn) increased 4.08 mm (Figure 4), although these variables were not statistically significant when compared to the control group changes (Table 3). According to the CVM analysis used in this prospective study, most of the patients started treatment just before or during the pubertal growth spurt, and mandibular length increased. The changes that the TFBC promoted in maxillary and mandibular components improved significantly the maxillomandibular relationship (Table 3), in accordance with the findings of other studies.3,19,20 At T2 (Table 4), these significant differences in maxillomandibular relationship were not present, since the maxillomandibular relationship was more accentuated in the experimental group (Table 2) in T1. This likely occurred because the experimental group presented more accentuated Class II characteristics at T1 and presented more Class II correction with treatment, resulting in non–statistically significant differences between groups at T2.
Figure 4. .
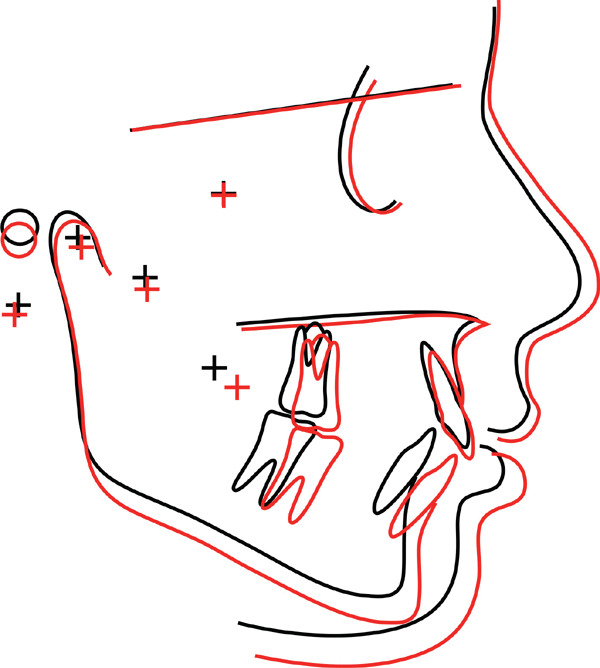
Superimposition of initial (black) and final (red) mean tracings of the experimental group.
The treatment did not promote a significant difference between groups in the mandibular rotation (Table 3), and although there has not been a significant difference in changes of the variables related to the maxillary dentoalveolar component, the experimental group showed a greater palatal tip of maxillary incisors than did the control group (Mx1.PP), likely related to the “headgear effect” observed in this group.
In the experimental group, there was a greater labial tip of the mandibular incisors, which is a common fixed–functional appliance effect (Figure 4).14–16 At T2, the maxilla presented a small length and retrusion in the experimental group; in addition, the mandibular retrusion was greater than in the control group before and after treatment (B-N pFHc and P-N pFHc) (Table 4). In the experimental group, the first mandibular molar showed a tendency to protrusion and vertical development (6-MP). This mandibular anterior movement of the buccal segments and dental compensation, associated with maxillary anterior restriction, helps to correct the maxillomandibular discrepancy of Class II malocclusion. This way, while in the experimental group, the molar Class II relationship, the increased OVJ, and the OVB were corrected (Figure 4), but in the control group these discrepancies were maintained. The major effect of this mandibular protrusion appliance used for a small period of time, then, is mainly a dentoalveolar one.21
Clinical Considerations
The TFBC is a flexible appliance that presents several advantages since it is quite agreeable to the patient, as it allows free lateral mandibular movements, practicability, and easy installation. It also delivers an intermittent force by the nickel-titanium coil spring in the cylindrical system. No appliance damage was observed in this study, as was observed in others,3,18 likely because of the appliance's superior robustness and the proper fastening of the archwires. Moreover, even though this study did not aim to directly evaluate the effects on the temporomandibular joint (TMJ), it should be highlighted that no patients in this sample related any clinically observable adverse effects on the TMJ, according to the literature about mandibular protrusion appliances.22
It is important to consider that additional studies should be conducted to evaluate those effects in different treatment stages, the long-term stability of the results, and the effects of this protocol in adult patients.
CONCLUSIONS
The appliance promotes restriction of anterior maxillary displacement without significant changes in mandibular length and position and improvement of maxillomandibular relationship without changes in facial growth and significant buccal tipping of mandibular incisors.
Class II correction with the TFBC occurred mainly as a result of dentoalveolar changes.
REFERENCES
- 1.Dolce C, McGorray SP, Brazeau L, King GJ, Wheeler TT. Timing of Class II treatment: skeletal changes comparing 1-phase and 2-phase treatment. Am J Orthod Dentofacial Orthop. 2007;132:481–489. doi: 10.1016/j.ajodo.2005.08.046. [DOI] [PubMed] [Google Scholar]
- 2.Cançado RH, Pinzan A, Janson G, et al. Occlusal outcomes and efficiency of 1- and 2-phase protocols in the treatment of Class II division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008;133:245–253. doi: 10.1016/j.ajodo.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 3.Pancherz H. Treatment of Class II malocclusions by jumping the bite with the Herbst appliance. A cephalometric investigation. Am J Orthod. 1979;76:423–442. doi: 10.1016/0002-9416(79)90227-6. [DOI] [PubMed] [Google Scholar]
- 4.Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 5.Moro A, Janson G, de Freitas MR, et al. Class II correction with the Cantilever Bite Jumper. Angle Orthod. 2009;79:221–229. doi: 10.2319/121807-591.1. [DOI] [PubMed] [Google Scholar]
- 6.Rothenberg J, Campbell ES, Nanda R. Class II correction with the Twin Force Bite Corrector. J Clin Orthod. 2004;38:232–240. [PubMed] [Google Scholar]
- 7.Uribe F, Rothenberg J, Nanda R. The Twin Force Bite Corrector in the correction of Class II malocclusion in adolescent patients. In: Papadopoulos M, editor. Orthodontic Treatment of the Class II Noncompliant Patient Current Principles and Techniques. Philadelphia, Pa: Mosby Elsevier; 2006. pp. 181–202. [Google Scholar]
- 8.DeVincenzo J. The Eureka Spring: a new interarch force delivery system. J Clin Orthod. 1997;31:454–467. [PubMed] [Google Scholar]
- 9.Nanda R, Dandajena T, Nanda R. Biomechanic strategies for nonextraction Class II malocclusions. In: Nanda R, editor. Biomechanics and Esthetic Strategies in Clinical Orthodontics. St Louis, Mo: Elsevier Saunders; 2005. pp. 177–193. [Google Scholar]
- 10.Dahlberg G. Statistical Methods for Medical and Biological Students. New York, NY: Interscience; 1940. [Google Scholar]
- 11.Dermaut LR, van den Eynde F, de Pauw G. Skeletal and dento-alveolar changes as a result of headgear activator therapy related to different vertical growth patterns. Eur J Orthod. 1992;14:140–146. doi: 10.1093/ejo/14.2.140. [DOI] [PubMed] [Google Scholar]
- 12.Wieslander L. Long-term effect of treatment with the headgear-Herbst appliance in the early mixed dentition. Stability or relapse. Am J Orthod Dentofacial Orthop. 1993;104:319–329. doi: 10.1016/S0889-5406(05)81328-9. [DOI] [PubMed] [Google Scholar]
- 13.Janson G, Caffer Dde C, Henriques JF, de Freitas MR, Neves LS. Stability of Class II, division 1 treatment with the headgear-activator combination followed by the edgewise appliance. Angle Orthod. 2004;74:594–604. doi: 10.1043/0003-3219(2004)074<0594:SOCIDT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Valant JR, Sinclair PM. Treatment effects of the Herbst appliance. Am J Orthod Dentofacial Orthop. 1989;95:138–147. doi: 10.1016/0889-5406(89)90392-2. [DOI] [PubMed] [Google Scholar]
- 15.Pancherz H, Anehus-Pancherz M. The headgear effect of the Herbst appliance: a cephalometric long-term study. Am J Orthod Dentofacial Orthop. 1993;103:510–520. doi: 10.1016/0889-5406(93)70090-B. [DOI] [PubMed] [Google Scholar]
- 16.Croft RS, Buschang PH, English JD, Meyer R. A cephalometric and tomographic evaluation of Herbst treatment in the mixed dentition. Am J Orthod Dentofacial Orthop. 1999;116:435–443. doi: 10.1016/s0889-5406(99)70230-1. [DOI] [PubMed] [Google Scholar]
- 17.Cope JB, Buschang PH, Cope DD, Parker J, Blackwood HO., III Quantitative evaluation of craniofacial changes with Jasper Jumper therapy. Angle Orthod. 1994;64:113–122. doi: 10.1043/0003-3219(1994)064<0113:QEOCCW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Papadopoulos M. Orthodontic Treatment of the Class II Noncompliant Patient—Current Principles and Techniques. London, UK: Elsevier; 2006. pp. 181–202. [Google Scholar]
- 19.Clements RM, Jr, Jacobson A. The MARS appliance. Report of a case. Am J Orthod. 1982;82:445–455. doi: 10.1016/0002-9416(82)90311-6. [DOI] [PubMed] [Google Scholar]
- 20.Nanda R. Biomechanics and Esthetic Strategies in Clinical Orthodontics. St Louis, Mo: Elsevier Saunders; 2005. pp. 188–192. [Google Scholar]
- 21.Drage KJ, Hunt NP. Overjet relapse following functional appliance therapy. Br J Orthod. 1990;17:205–213. doi: 10.1179/bjo.17.3.205. [DOI] [PubMed] [Google Scholar]
- 22.Ruf S, Pancherz H. Temporomandibular joint growth adaptation in Herbst treatment: a prospective magnetic resonance imaging and cephalometric roentgenographic study. Eur J Orthod. 1998;20:375–388. doi: 10.1093/ejo/20.4.375. [DOI] [PubMed] [Google Scholar]