Abstract
Objective:
To compare the diagnostic accuracy between cone-beam computed tomography (CBCT) and periapical radiography for detecting simulated external apical root resorption (EARR) in vitro.
Materials and Methods:
The study sample consisted of 160 single-rooted premolar teeth for simulating EARR of varying degrees according to four setups: no (intact teeth), mild (cavity of 1.0 mm in diameter and depth on root surface), moderate (0.4 mm, 0.8 mm, 1.2 mm, and 1.6 mm root shortening), and severe (2.4 mm, 2.8 mm, 3.2 mm, and 3.6 mm root shortening). Two groups of radiographic images were obtained via CBCT and periapical radiography. The absence or presence and the severity for all resorption lesions were evaluated blindly by two calibrated observers.
Results:
With the CBCT method, the rates of correct classification of no, mild, moderate, and severe EARR were 96.3%, 98.8%, 41.3%, and 87.5%, respectively; with the periapical radiography method, the rates were 82.5%, 41.3%, 68.8%, and 92.5%, respectively. Highly significant differences were found between the two imaging methods for detection of mild (P < .001), moderate (P < .001), and all EARR (P < .001). For detection of all EARR, the sensitivity and specificity values were 75.8% and 96.3% for CBCT, compared with 67.5% and 82.5% for periapical radiography.
Conclusion:
CBCT is a reliable diagnostic tool to detect simulated EARR, whereas periapical radiography underestimates it. However, if a periapical radiograph is already available to the diagnosis of EARR, CBCT should be used with extreme caution to avoid additional radiation exposure.
Keywords: Cone-beam computed tomography, Apical root resorption, Periapical radiography
INTRODUCTION
External apical root resorption (EARR) is a common complication in orthodontic treatment. In one study, it was found that 94% of patients investigated had one or more roots with root shortening >1 mm, and 6.6% had one or more teeth where root resorption exceeded 4 mm at the end of orthodontic treatment. Monthly root shortening was greater after 6-month control than before.1 In a separate study, clinically significant resorption was found for 74% of the centrals and 82% of the laterals, and apical root resorption was thought to be correlated with treatment duration and premolar extraction.2 The process of root resorption in the permanent teeth is usually pathological, resulting in loss of dentin, cementum, or bone.3 The diagnostic efficiency of EARR is an essential aspect to the definition of the adequate therapeutic approach and eventually to success in treatment. The clinical diagnosis of EARR mainly depends on routine radiographic techniques, such as periapical and panoramic radiography. However, there are many limitations to the image acquisition of EARR using conventional radiography, since the three-dimensional (3D) structure is displayed on a two-dimensional (2D) image.
Quantitative evaluation of resorption using radiographs has proven to be highly inaccurate because of magnification errors and their inability to be readily repeated and reproduced.4 What's more, periapical radiographs cannot detect external root resorption during the first month of orthodontic treatment.5 Assessing EARR generally requires a 3D technique, such as computed tomography (CT). However, the expense and exposure to ionizing radiation of CT is much higher than that of conventional 2D radiography. In addition, because it is too difficult for most dentists to interpret the CT image, trained radiologists are always required, which therefore restricts its use. Even now, there is still no gold standard for the EARR detection.
There is a great need for a more accurate and economical diagnostic method for detecting EARR. As a new radiographic method in dentomaxillofacial radiology, cone-beam computed tomography (CBCT) has a lot of superiority. Its imaging is characterized by extraordinary accuracy, rapid scan time, reduced radiation dose, and unmatched 3D image reconstruction capabilities.
In orthodontics, CBCT imaging has been applied to impacted teeth,6 assessment of bone volume,7 cleft patients,8 and root resorption.9–12 But the data are still scarce even now, with regard to its application in detecting EARR. One prospective study showed that all patients and up to 91% of all teeth investigated showed some degree of root shortening and CBCT technique can provide valid and accurate information about EARR.1 However, the diagnostic superiority of CBCT over periapical radiography has not yet been established for detecting orthodontically induced EARR.
The aim of imaging in dentistry is to promote diagnostic accuracy and reduce exposure of patients to x-rays. With this in mind, the purpose of this research was to compare the efficacy of CBCT and periapical radiography in detecting simulated EARR in vitro. The experimental variables were lesion size and imaging technique.
MATERIALS AND METHODS
Subjects
One hundred sixty single-rooted premolar teeth extracted for orthodontic treatment, without abnormalities, defects, or root fractures were used. All the teeth were submitted to a disinfection process in 2% glutaraldehyde for approximately 2 hours and then hydrated in water.13 For each root of the 160 teeth, there were four simulation possibilities: mild, moderate, or severe defect or no defect. Therefore, for each simulation possibility, 40 teeth were randomly selected. The College of Stomatology, Chongqing Medical University, Chongqing, PR China, approved this research project.
Simulation and Model Making
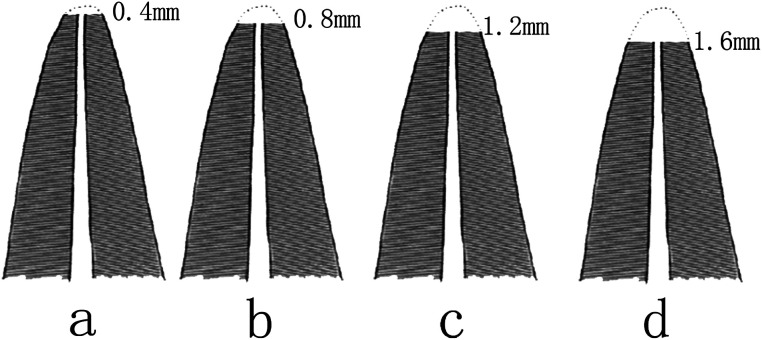
To simulate mild EARR, all crowns of the selected 40 teeth were placed in plaster bases. A cavity of 1.0 mm in diameter and depth was drilled in the apical root third of each tooth with a 1-mm-diameter round bur to its full depth and the assistance of magnifier.12 The cavity types were distributed to ensure an equal number in the buccolingual and proximal root surfaces. To simulate moderate EARR, the selected 40 teeth, divided into four groups of 10 specimens each, were also placed in plaster bases. The apical root portions of 0.4 mm, 0.8 mm, 1.2 mm, and 1.6 mm were ground off with a fissure bur for the four groups of teeth (Figure 1). Similarly, to simulate severe EARR, the apical root portions of 2.4 mm, 2.8 mm, 3.2 mm, and 3.6 mm were ground off for the other four groups of teeth. All defects were made by the same investigator, and the defect sizes were verified by another investigator also using magnified vision.
Figure 1. .
Procedure to simulate moderate external apical root resorption: apical root portions of 0.4 mm, 0.8 mm, 1.2 mm, and 1.6 mm were ground off, respectively.
The 160 teeth, randomly divided into 40 groups of four specimens each after simulation, were fixed in 40 standard mandibular model boxes for making standard models. To obtain a radiographic aspect equivalent to the soft tissue (periodontal space) and alveolar trabecular bone (dental alveolus), simulating an in vivo situation, the radicular portion of each tooth was covered uniformly with a layer of utility wax, approximately 0.3-mm thick, and surrounded by plaster mixed with ground rice in an equal ratio by volume. The presence of the wax layer reduced the artifacts around the root surface in the image.13,14 The excess part of each standard model was removed after the plaster was dry, leaving only the mandibular body (Figure 2).
Figure 2. .

Completed model.
Radiographic Examination
The CBCT images were obtained with the KAVO 3D EXAM (KaVo Sybron, Germany and United States) at 120 kV, 18.54 mA, and an exposure time of 8.9 seconds and were reconstructed with a high-resolution (0.3 mm3) voxel size (80-mm field of view). Periapical images were acquired with the KODAK 2100 (Kodak, Rochester, NY) at 60 kV, 7 mA, and an exposure time of 0.1 seconds. All images were stored in the database. All exposures were performed by the same operator.
Assessment of Root Resorption
Calibration consisted of identification of the existence of EARR in a group of images that did not belong to the study sample for each imaging method. Two postgraduate orthodontic residents assessed blindly and separately the presence or absence and the severity of simulated EARR in the CBCT and the periapical images using the modified score system of Levander and Malmgren15: grade 0, no root resorption; grade 1, mild resorption—root with normal length and only irregular contour; grade 2, moderate resorption—small area of root loss with apex having almost straight contour; grade 3, severe resorption—loss of almost one-third of root length (Figure 3). CBCT images were analyzed by using the i-CAT View software (Imaging Sciences International Inc, Hatfield, PA, USA). Figure 4 shows varying degrees of simulated EARR displayed on the periapical radiography and the CBCT, respectively. All images were viewed on a 15-inch flat-panel screen without time limitation. The gray scale and the magnification were allowed to be adjusted by the observers. If disagreement occurred between the two observers, the second evaluation was adopted 20 days later, the consensus of which was used for final evaluation. A substantial kappa value of 0.74 was found for the agreement between the two examiners with CBCT, whereas a moderate value of 0.57 was found with periapical radiography.
Figure 3. .
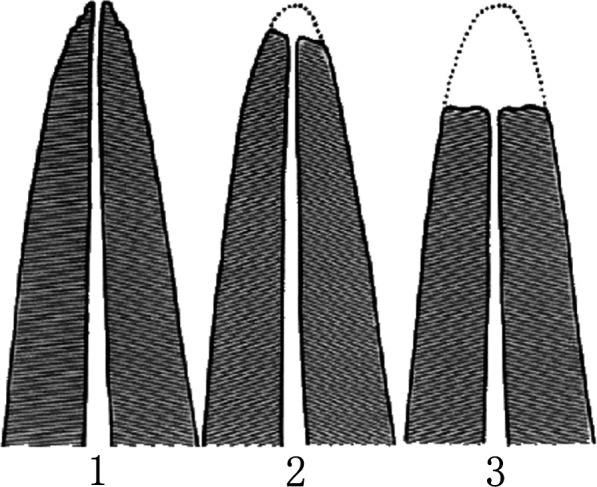
Index for quantitative evaluation of external apical root resorption reported by Levander and Malmgren15: 1, mild resorption—root with normal length and only irregular contour; 2, moderate resorption—small area of root loss with apex having almost straight contour, amounting to less than 2 mm; 3, severe resorption—loss of almost one-third of original root length.
Figure 4. .
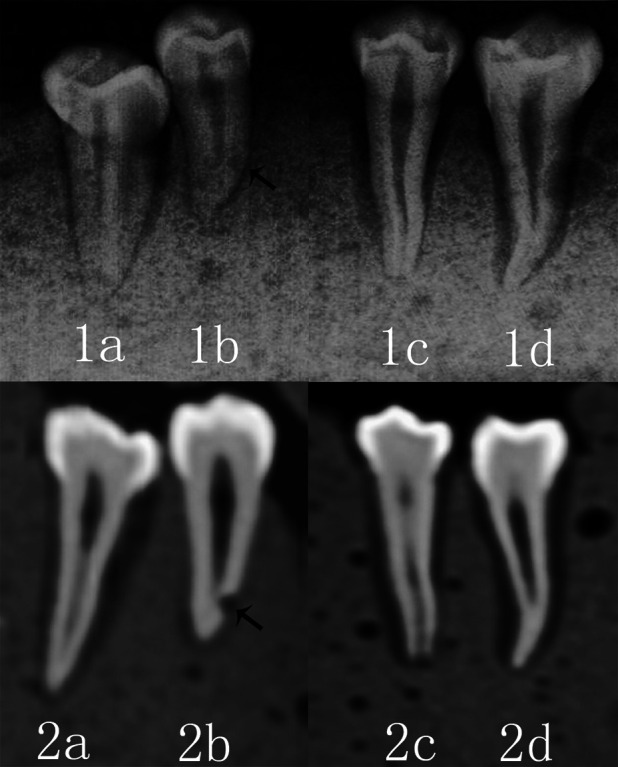
Root sections showing the presence of simulated external apical root resorption on the apical third visualized with the two imaging methods. With the periapical radiography: moderate (1a), mild (1b), severe (1c), no (1d); with the cone-beam computed tomography: moderate (2a), mild (2b), severe (2c), no (2d).
Statistical Analyses
For statistical analysis, the rates of correct classifications of each degree of EARR were compared between the two imaging methods using the McNemar test. All P values were regarded significant if less than .05. SAS 9.1 (SAS Institute, Cary, NC) was used for all analyses.
RESULTS
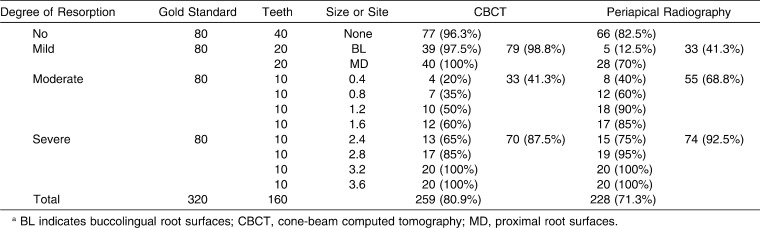
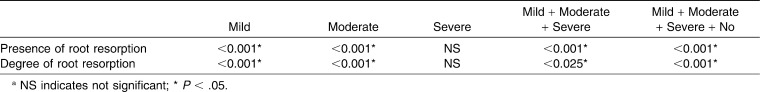
The rates of correct classification of mild EARR with CBCT and periapical radiography were 98.8% and 41.3%, respectively (Table 1), and a significant difference was found between the two imaging methods (P < .001; Table 2). As far as the periapical radiography method is concerned, the correct classification rates of mild resorption on buccolingual and proximal surfaces were found to be 12.5% and 70%, respectively (Table 1).
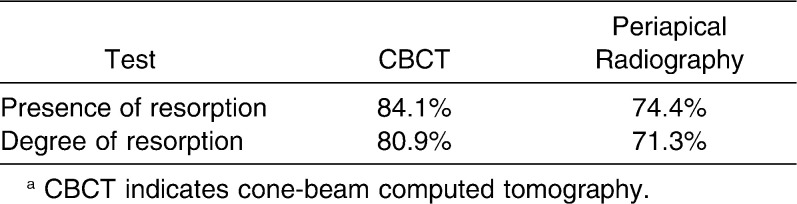
Table 1. .
The Percentages of Correct Classifications of No, Mild, Moderate, and Severe Resorptions Performed by Two Observers When Compared With the Gold Standard for the Two Imaging Methodsa
Table 2. .
McNemar Test Results for Cone-Beam Computed Tomography Versus Periapical Radiography (Comparison of the Correct Classification Rates of Mild, Moderate, Severe, and All Resorptions)a
For correct classification of severe EARR, no significant difference was found between the two imaging methods (Table 2). However, for correct classification of moderate EARR, 68.8% of the lesions were correctly classified for periapical radiography, compared with 41.3% for CBCT (Table 1), and a significant difference was found between the two imaging methods (P < .001; Table 2).
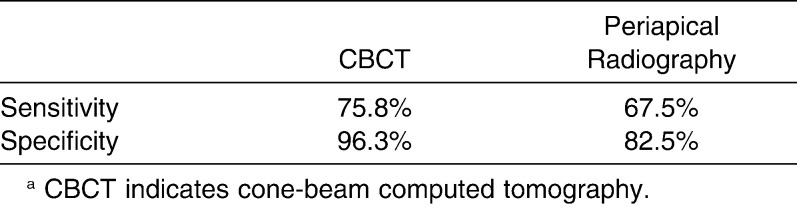
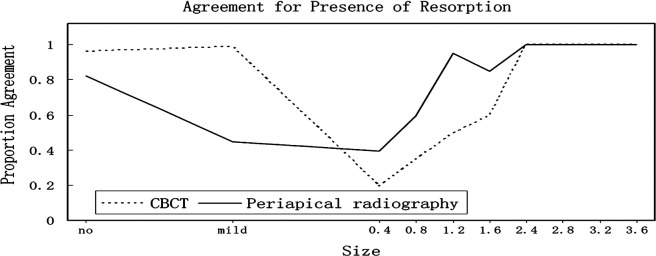
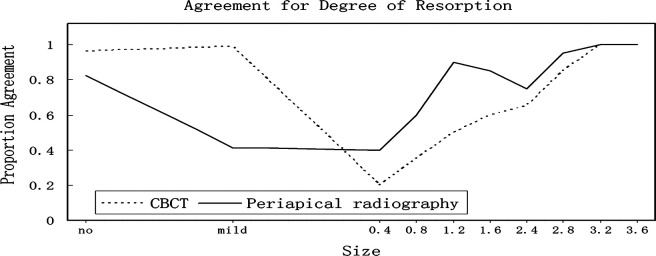
For detection of all EARR, the sensitivity values were 75.8% for CBCT and 67.5% for periapical radiography, and the specificity values were 96.3% for CBCT and 82.5% for periapical radiography (Table 3). The rates of correct classification of all EARR with CBCT and periapical radiography were 80.9% and 71.3%, respectively (Table 4), and a highly significant difference was also found between the two imaging methods (P < .001; Table 2). The rates for correctly evaluating the absence or presence and the severity of EARR for each defect size are shown in Figures 5 and 6.
Table 3. .
The Sensitivity and Specificity Values for Detection of All Resorptions by Using the Two Imaging Methodsa
Table 4. .
The Percentages of Correct Detection of All Resorptions by Using the Two Imaging Methodsa
Figure 5. .
The rates for correctly evaluating the absence and presence of external apical root resorption for each defect size.
Figure 6. .
The rates for correctly evaluating the severity of external apical root resorption for each defect size.
DISCUSSION
Radiography is the most important tool for the diagnosis of EARR. No single two-dimensional imaging technique has been readily available to provide an accurate, easily interpreted representation of EARR and associated structure. This study was designed to compare the efficacy of CBCT and periapical radiography in detecting simulated EARR of varying degrees in premolars. Periapical radiography was chosen because it is usually used for the diagnosis or planning in orthodontic treatment.
A cavity of 1.0 mm in diameter and depth was adopted to simulate mild EARR, considering that conventional radiography cannot detect lesions smaller than 0.30 mm in depth and 0.60 mm in diameter.16,17 Moreover, CBCT was found to be a sensitive method in the evaluation of simulated external root resorption. A 0.3-mm voxel appeared to be the best protocol.18 Therefore, we used a CBCT unit with a high-resolution (0.3 mm3) voxel size. Periapical radiography can be obtained from different angles to ensure that some more information would be acquired.19 However, a single periapical image was used in this study because it might be more practical in the clinic.
CBCT provides 3D volume image data of the craniofacial complex about 10 seconds, eliminating superimposition of anatomic structures, which could provide convenience for clinicians. The diagnostic capacity of CBCT scans to detect simulated external root resorption has been reported by Liedke.20 Cavities of 0.6, 1.2, or 1.8 mm in diameter and 0.3, 0.6, or 0.9 mm in depth were drilled on the buccal root surfaces, and CBCT showed excellent specificity and high sensitivity in detecting these lesions. In the present study, the rates of correct classification of mild EARR with CBCT and periapical radiography were 98.8% and 41.3%, respectively, and a significant difference was found between the two imaging methods (P < .001). These results imply that CBCT imaging was superior to periapical radiography for detecting simulated mild EARR. Durack et al.11 investigated the accuracy of periapical radiography and CBCT for the detection of simulated resorption cavities. Their findings verified the shortcomings of periapical radiography and showed that these were overcome by CBCT. Some other studies also indicated that the CBCT method is more sensitive than periapical radiography in detecting simulated external root resorption cavities.10,12 For the moment, it is obvious that CBCT imaging can provide reliable data on simulated mild EARR, whereas periapical radiography underestimates it.
In the present study, the determination of severe EARR was not significantly different when using CBCT and periapical radiography. The reason might be it was very easy to detect severe resorption for the two imaging methods. However, for detecting moderate EARR, none of the detection rates of the two imaging methods was high, as most observers scored moderate defects as no. What's more, periapical radiography's performances were much better than that of CBCT imaging (P < .001). The rate of correct classification of moderate EARR was 68.8% for periapical radiography compared with 41.3% for CBCT. In contrast, Sherrard et al.21 inferred that CBCT scans are at least as accurate and reliable as periapical radiographs for root-length and tooth-length determinations. However, because of methodological differences, it is difficult to make direct comparisons with the current study. Another in vitro study implied that periapical radiography seems to be a very blunt instrument for detecting lingual root shortening resorption.22 Other in vivo studies further confirmed that slanted apical root resorption could be evaluated only on tomographic images and was found in up to 15% of palatal root surfaces investigated.1 In this study, the simulation of root shortening contained no slanted apical root resorption, and most moderate root shortening was more easily detectable on periapical radiography than the CBCT method as it could offer an overall view of the apical lesion. For the moment, we tentatively put forward that CBCT could not replace periapical radiography, which remains the primary imaging modality for detecting orthodontically induced EARR. However, in some complex cases, the 3D imaging might be more proper than conventional radiography.
Periapical radiography is commonly used for detecting apical root resorption, but it has been reported to underestimate resorption lesion compared with micro CT.23 In this study, CBCT showed higher sensitivity than periapical radiography. The sensitivity values were 75.8% for CBCT and 67.5% for periapical radiography. For correct classification of all EARR, the rates of CBCT and periapical radiography were 80.9% and 71.3%, respectively, and CBCT imaging performed significantly better than periapical radiography (P < .001). Furthermore, an in vitro study showed that buccal or lingual resorption is less detectable in 2D radiographs.22 This agrees with our results: the correct classification rate of mild resorptions was 70% on proximal compared with 12.5% on buccolingual surfaces for periapical radiography. In addition, during orthodontic treatment, angulations of the teeth usually change; thus, the severity of EARR could not be evaluated accurately with periapical radiography. These data might justify that the routine diagnostic tool for detecting EARR should be CBCT rather than periapical radiography. In orthodontic practices, CBCT could be used to evaluate the severity of EARR to provide enough reference for modification or continuation of orthodontic treatment. However, some authors have reported that the radiation dose from large-volume CBCT scanners is between 50 µSv and 1024 µSv, compared with 1–8 µSv from periapical radiography.24 CBCT delivers a much higher radiation dose to the patient than periapical radiography does, so if a periapical radiograph is already available to the diagnosis of EARR, the choice of CBCT should be used with extreme caution to avoid additional radiation exposure.
These results suggest that CBCT is a reliable diagnostic tool to detect simulated EARR. However, it must be noted that this experimental study carried out ideal imaging geometry, without associated motion, which is scarcely ever achieved in clinic. It is also true that the methods used in the present study produced lesions with regular edges. These lesions are not real replicas of EARR, which might have raised the diagnostic ability of CBCT and periapical radiography. Therefore, considering that quantitative analysis for EARR similar to this research might be unrealistic in vivo, studies in the future should seek methods for creating irregular and standardized lesions.
CONCLUSIONS
CBCT is a reliable diagnostic tool to detect simulated EARR, whereas periapical radiography underestimates it.
If a periapical radiograph is already available to the diagnosis of EARR, CBCT should be used with extreme caution to avoid additional radiation exposure.
Acknowledgments
This work was supported by the General Program of National Natural Science Foundation for Young Scholars of China (81000463) and the Chongqing Health Bureau (2011-2-192).
REFERENCES
- 1.Lund H, Grondahl K, Hansen K, Grondahl HG. Apical root resorption during orthodontic treatment. Angle Orthod. 2012;82:480–487. doi: 10.2319/061311-390.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohandesan H, Ravanmehr H, Valaei N. A radiographic analysis of external apical root resorption of maxillary incisors during active orthodontic treatment. Eur J Orthod. 2007;29:134–139. doi: 10.1093/ejo/cjl090. [DOI] [PubMed] [Google Scholar]
- 3.Armas JM, Savarrio L, Brocklebank LM. External apical root resorption: two case reports. Int Endod J. 2008;41:997–1004. doi: 10.1111/j.1365-2591.2008.01419.x. [DOI] [PubMed] [Google Scholar]
- 4.Chan EK, Darendeliler MA. Exploring the third dimension in root resorption. Orthod Craniofac Res. 2004;7:64–70. doi: 10.1111/j.1601-6343.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- 5.Levander E, Malmgren O. Long-term follow-up of maxillary incisors with severe apical root resorption. Eur J Orthod. 2000;22:85–92. doi: 10.1093/ejo/22.1.85. [DOI] [PubMed] [Google Scholar]
- 6.Oberoi S, Knueppel S. Three-dimensional assessment of impacted canines and root resorption using cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:260–267. doi: 10.1016/j.tripleo.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 7.Gracco A, Lombardo L, Mancuso G, Gravina V, Siciliani G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod. 2009;79:692–702. doi: 10.2319/081908-437.1. [DOI] [PubMed] [Google Scholar]
- 8.Wortche R, Hassfeld S, Lux CJ, et al. Clinical application of cone beam digital volume tomography in children with cleft lip and palate. Dentomaxillofac Radiol. 2006;35:88–94. doi: 10.1259/dmfr/27536604. [DOI] [PubMed] [Google Scholar]
- 9.Alqerban A, Jacobs R, Souza PC, Willems G. In-vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am J Orthod Dentofacial Orthop. 2009;136 doi: 10.1016/j.ajodo.2009.03.036. [DOI] [PubMed] [Google Scholar]
- 10.D'Addazio PS, Campos CN, Ozcan M, Teixeira HG, Passoni RM, Carvalho AC. A comparative study between cone-beam computed tomography and periapical radiographs in the diagnosis of simulated endodontic complications. Int Endod J. 2011;44:218–224. doi: 10.1111/j.1365-2591.2010.01802.x. [DOI] [PubMed] [Google Scholar]
- 11.Durack C, Patel S, Davies J, Wilson R, Mannocci F. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J. 2011;44:136–147. doi: 10.1111/j.1365-2591.2010.01819.x. [DOI] [PubMed] [Google Scholar]
- 12.Kamburoglu K, Kursun S, Yuksel S, Oztas B. Observer ability to detect ex vivo simulated internal or external cervical root resorption. J Endod. 2011;37:168–175. doi: 10.1016/j.joen.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Neves FS, Vasconcelos TV, Vaz SL, Freitas DQ, Haiter-Neto F. Evaluation of reconstructed images with different voxel sizes of acquisition in the diagnosis of simulated external root resorption using cone beam computed tomography. Int Endod J. 2012;45:234–239. doi: 10.1111/j.1365-2591.2011.01966.x. [DOI] [PubMed] [Google Scholar]
- 14.Ozer SY. Detection of vertical root fractures by using cone beam computed tomography with variable voxel sizes in an in vitro model. J Endod. 2011;37:75–79. doi: 10.1016/j.joen.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 15.Levander E, Malmgren O. Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors. Eur J Orthod. 1988;10:30–38. doi: 10.1093/ejo/10.1.30. [DOI] [PubMed] [Google Scholar]
- 16.Andreasen FM, Sewerin I, Mandel U, Andreasen JO. Radiographic assessment of simulated root resorption cavities. Endod Dent Traumatol. 1987;3:21–27. doi: 10.1111/j.1600-9657.1987.tb00167.x. [DOI] [PubMed] [Google Scholar]
- 17.Westphalen VP, Gomes DMI, Westphalen FH, Martins WD, Souza PH. Conventional and digital radiographic methods in the detection of simulated external root resorptions: a comparative study. Dentomaxillofac Radiol. 2004;33:233–235. doi: 10.1259/dmfr/65487937. [DOI] [PubMed] [Google Scholar]
- 18.Liedke GS, Da SH, Da SH, Dutra V, de Figueiredo JA. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod. 2009;35:233–235. doi: 10.1016/j.joen.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Brynolf I. Roentgenologic periapical diagnosis. II. One, two or more roentgenograms. Sven Tandlak Tidskr. 1970;63:345–350. [PubMed] [Google Scholar]
- 20.Da SH, Silveira HE, Liedke GS, Lermen CA, Dos SR, de Figueiredo JA. Diagnostic ability of computed tomography to evaluate external root resorption in vitro. Dentomaxillofac Radiol. 2007;36:393–396. doi: 10.1259/dmfr/13347073. [DOI] [PubMed] [Google Scholar]
- 21.Sherrard JF, Rossouw PE, Benson BW, Carrillo R, Buschang PH. Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am J Orthod Dentofacial Orthop. 2010;137:S100–S108. doi: 10.1016/j.ajodo.2009.03.040. [DOI] [PubMed] [Google Scholar]
- 22.Follin ME, Lindvall AM. Detection of lingual root resorptions in the intraoral radiographs: an experimental study. Swed Dent J. 2005;29:35–42. [PubMed] [Google Scholar]
- 23.Dudic A, Giannopoulou C, Martinez M, Montet X, Kiliaridis S. Diagnostic accuracy of digitized periapical radiographs validated against micro-computed tomography scanning in evaluating orthodontically induced apical root resorption. Eur J Oral Sci. 2008;116:467–472. doi: 10.1111/j.1600-0722.2008.00559.x. [DOI] [PubMed] [Google Scholar]
- 24.Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol. 2009;82:35–40. doi: 10.1259/bjr/31419627. [DOI] [PubMed] [Google Scholar]