Abstract
Objective:
To compare posttreatment and postretention occlusal changes with the physiologic occlusal changes caused by natural development of untreated subjects.
Materials and Methods:
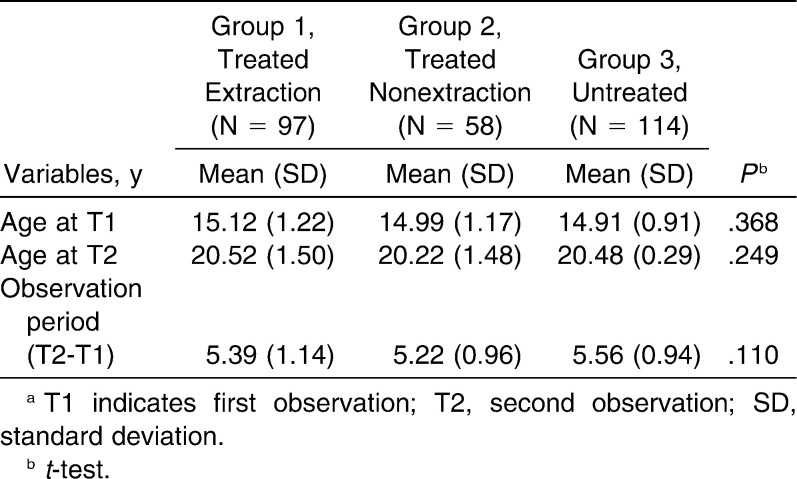
The sample was divided into three groups. Group 1 comprised 97 subjects treated with four premolar extractions at a mean pretreatment (T0) age of 13.03 years, a mean posttreatment (T1, first observation) age of 15.12 years, and a mean postretention (T2, second observation) age of 20.52 years. The mean observation period (T2-T1) was 5.39 years. Group 2 comprised 58 subjects treated nonextraction at a mean pretreatment age of 12.83 years, a mean posttreatment age of 14.99 years, a mean postretention age of 20.22 years, and a mean observation period of 5.22 years. Group 3 comprised 114 untreated subjects at a mean age at T1 of 14.91 years and at T2 of 20.48 years. The mean observation period was 5.56 years. Dental casts were evaluated using the Peer Assessment Rating (PAR) index and the Little irregularity index in maxillary and mandibular arches. Changes in PAR and Little indexes were compared among the three groups by analysis of variance and Tukey tests.
Results:
Intergroup comparison showed that at T1 and T2 the treated groups presented smaller PAR and Little indexes than the untreated group. In the observation period, the treated groups showed greater increase in PAR and Little maxillary indexes than the untreated group. The extraction group showed a greater increase of the Little mandibular index than the untreated group.
Conclusions:
The treated groups showed more changes according to PAR and Little maxillary indexes than the untreated group. The posttreatment change of the mandibular anterior crowding of the treated extraction group was greater than the mandibular crowding caused by physiologic changes in the untreated group.
Keywords: Stability, Relapse, Crowding
INTRODUCTION
Orthodontists and researchers are aware that changes occur after orthodontic treatment, and the most studied is the relapse of mandibular anterior crowding. However, late mandibular incisor crowding can occur regardless of whether a person receives orthodontic treatment. The natural aging process causes some changes that are similar to those that occur after orthodontic treatment and removal of retainers.1–3
Some studies have demonstrated the changes over time with natural development.3–5 Sinclair and Little1 compared the natural development in an untreated normal group with four premolar extraction groups and found that mandibular crowding relapse was greater than the late mandibular crowding presented in the untreated group. However, the authors studied only normal occlusion cases, and the treated and untreated samples were not compatible regarding ages and observation period.
Driscoll-Gilliland et al.6 compared skeletal and dental changes in treated patients with an untreated group to evaluate the relationship between skeletal changes and mandibular incisor crowding. Changes were annualized because the observation periods did not match between groups. There were no differences in the changes in irregularity between the groups.
The above mentioned studies showed controversial results. Sinclair and Little1 found that relapse in the treated group was greater than late mandibular crowding in the untreated group. Driscoll-Gilliland et al.6 found no difference in mandibular irregularity changes between the treated and untreated group. Therefore, we still do not know if the amount of posttreatment and natural development change is comparable or not.
In order to clarify this issue, the present study aimed to compare posttreatment and postretention occlusal changes with the physiologic occlusal changes of untreated subjects, using the Peer Assessment Rating (PAR) index and the Little irregularity index in the maxillary and mandibular arches.
MATERIALS AND METHODS
This research was approved by the Ethics Committee of the University of São Paulo. The sample comprised the retrospective records of 269 subjects obtained from the files of two institutions.
The sample was divided into three groups. Groups 1 and 2 were obtained from the Department of Orthodontics at Bauru Dental School, Bauru, São Paulo, Brazil. Subjects were treated with fixed appliances and chosen according to the following criteria:
Class I or II malocclusion present at the beginning of orthodontic treatment;
Treatment protocol with extraction of the four first premolars (Group1) or nonextraction (Group 2);
Age at the end of orthodontic treatment between 13 and 16 years;
All permanent teeth erupted up to the first molars, at pretreatment stage;
Absence of tooth agenesis and anomalies;
Maxillary removable (Hawley), worn for 1 year, and mandibular fixed canine to canine retainers worn for 1 to 2 years posttreatment, and no retention at the time of followup record;
Dental casts from pretreatment, posttreatment, and postretention available at the time of the study; and
At the end of treatment, all patients presented a Class I molar relationship.
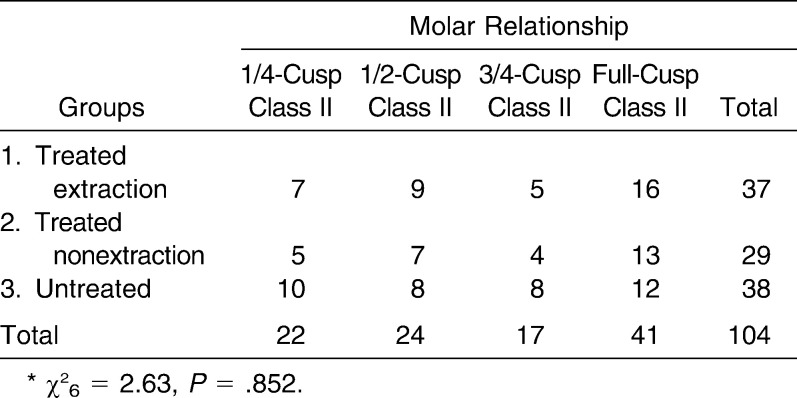
Group 1 comprised 97 subjects (44 male, 53 female) treated with extraction of four first premolars; 60 subjects presented Class I and 37 presented Class II malocclusion (seven 1/4-cusp Class II, nine half-cusp Class II, five 3/4-cusp Class II, and 16 full-cusp Class II).7,8 The mean age at pretreatment (T0) was 13.03 years (SD = 1.09), at posttreatment (T1) 15.12 years (SD = 1.22), and at postretention (T2, second observation stage) 20.52 years (SD = 1.50). The mean treatment time was 2.09 years (SD = 0.58), and the mean observation period was 5.39 years (SD = 1.14).
Group 2 comprised 58 subjects (24 male, 34 female) treated nonextraction; 29 subjects presented Class I and 29 presented Class II malocclusion (five 1/4-cusp Class II, seven half-cusp Class II, four 3/4-cusp Class II, and 13 full-cusp Class II).7,8 The mean age at pretreatment (T0) was 12.83 years (SD = 1.11), at posttreatment (T1) 14.99 years (SD = 1.17), and at postretention (T2) 20.22 years (SD = 1.48). The mean treatment time was 2.16 years (SD = 0.71), and the mean observation period was 5.22 years (SD = 0.96).
Group 3 was obtained from the Burlington Growth Centre, University of Toronto, Ontario, Canada. Subjects of this group were chosen according to the following criteria:
Class I or II malocclusion. Normal occlusions were excluded;
No orthodontic treatment;
All permanent teeth erupted up to the first molars, at the first observation stage;
Absence of tooth agenesis and anomalies; and
At least two dental casts at ages 14 to 16 and 19 to 21, available at the time of the study.
This group comprised 114 subjects (59 male, 55 female), 76 presenting Class I and 38 presenting Class II malocclusions (ten 1/4-cusp Class II, eight half-cusp Class II, eight 3/4-cusp Class II, and 12 full-cusp Class II).7,8
The mean age at the first observation stage was 14.91 years (SD = 0.92), and the mean age at the second observation stage was 20.48 years (SD = 0.29). The mean observation period was 5.5 years (SD = 0.94).
Stages were defined as follows: T1, end of treatment (posttreatment) in Groups 1 and 2 and first observation in Group 3; T2, postretention stage in Groups 1 and 2 and second observation in Group 3. Intergroup comparisons of PAR and Little indexes were performed at T1 and T2, and intergroup change comparisons from T1 to T2 (T2-T1) were also conducted.
To check whether the severity of the mandibular irregularity influenced its amount of increase in the untreated group, it was divided into two subgroups according to the severity of mandibular crowding at T1. Subgroup A included subjects with a Little mandibular index less than 4 mm, and subgroup B included subjects with an index of 4 mm or more.
Pretreatment (T0), posttreatment (T1), and postretention (T2) dental casts were used for Groups 1 and 2, and observation stages 1 (T1) and 2 (T2) for Group 3. All dental cast measurements were performed with a 0.01-mm precision digital caliper (Mitutoyo America, Aurora, Ill) by one calibrated examiner. The assessed variables were: PAR index, described by Richmond et al.9 and scored with the American weight,10 and Little irregularity index11 for maxillary and mandibular teeth.
The PAR index is an occlusal index designed and validated as an instrument to measure how much a patient deviates from normal occlusion.9 This index was designed to measure the outcome of treatment by comparing the severity of the initial malocclusion with the result, as seen on pretreatment and posttreatment dental casts.9 A posttreatment PAR score of 5 or less is considered an excellent outcome,12 and a posttreatment PAR score above 10 indicates residual malocclusion.13 The PAR index has been widely used for evaluating the effects of treatment in a variety of circumstances,14–16 even in untreated cases.4,5
The Little irregularity index11 is the summed displacement of the five anatomic contact points of mandibular anterior teeth. The caliper should be parallel to the occlusal plane.
The degree of change from the first to the second observation (T2-T1) was assessed by the index changes (PAR and Little Mx and Md).
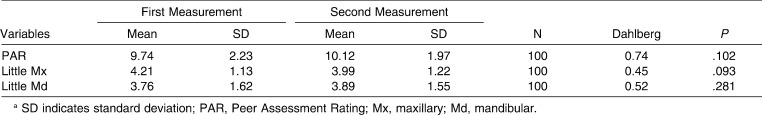
Error Study
One month after the original exam, 100 pairs of dental casts were randomly selected and remeasured by the same examiner. The casual error was calculated according to Dahlberg's17 formula (S2 = Σd2/2n) and the systematic error with dependent t-tests18 for P < .05.
Statistical Analysis
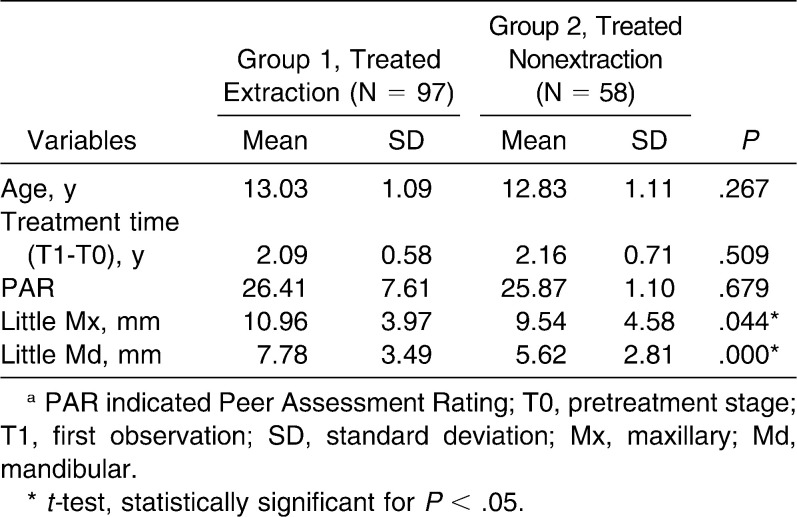
To check the compatibility of groups 1 and 2 for the age at pretreatment (T0), treatment time (T1-T0), and the PAR and Little indexes at T0, t-tests were used.
To check group compatibility, chi-square tests were used to compare sex distribution, type of malocclusion, and severity of the Class II molar relationship; one-way analysis of variance and Tukey tests were used to compare the ages and the observation period.
Intergroup comparison of the PAR and Little indexes was performed by one-way analysis of variance and Tukey tests. Comparison of subgroups A and B was performed by t-tests.
Intragroup comparisons of the unweighted components of the PAR index between the first and second observations for treated and untreated groups were performed by Wilcoxon tests.
Results were considered statistically significant for P < .05. All statistical analyses were performed on Statistica software (Statistica for Windows 6.0; Statsoft, Tulsa, Okla).
RESULTS
No systematic errors were detected, and the casual errors were within acceptable levels (between 0.45 for the Little Mx and 0.74 for the PAR; Table 1).
Table 1. .
Casual and Systematic Errors Between the First and Second Measurementsa
Groups 1 and 2 were compatible regarding pretreatment age, treatment time, and PAR at T0. Little maxillary and mandibular indexes were significantly greater in the extraction group (Table 2).
Table 2. .
Comparison of Age and PAR and Little Indexes at T0 for Groups 1 and 2a
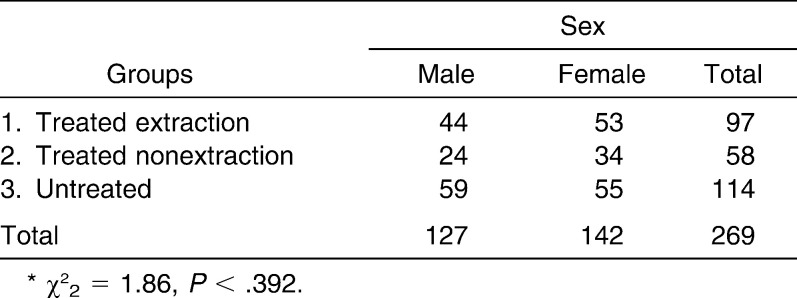
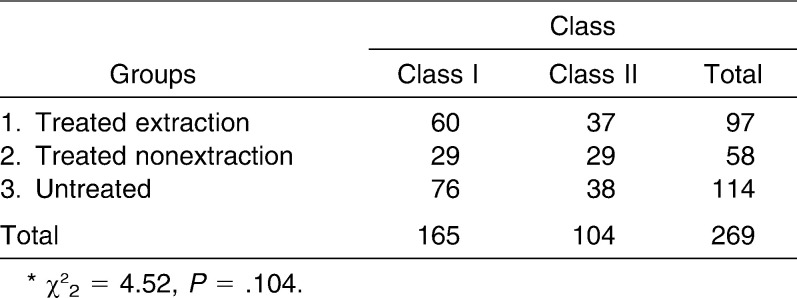
Groups were compatible regarding sex distribution (Table 3), type of malocclusion (Table 4), severity of the Class II molar relationship (Table 5), and age at first and second observation stages and observation period (Table 6).
Table 3. .
Comparison of Sex Distribution Among the Groups*
Table 4. .
Comparison of Type of Malocclusion Among the Groups*
Tables 5. .
Comparison of the Severity of the Class II Molar Relationship Among the Groups*
Table 6. .
Intergroup Comparison of Ages at T1 and T2 and Observation Perioda
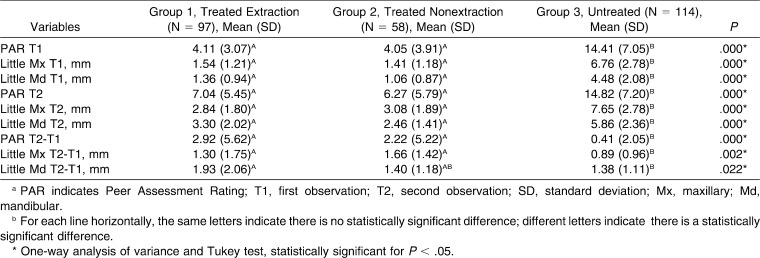
Intergroup comparison results showed that, at T1 and T2, both treated groups presented smaller PAR and Little indexes than the untreated group (Table 7). In the observation period, the treated groups showed a greater increase in PAR and Little maxillary indexes than the untreated group. The treated extraction group showed a greater increase of the Little mandibular index than the untreated group (Table 7).
Table 7. .
Results of Intergroup Comparison of the PAR and Little Indexes at T1 and T2 and Observation Period (T2-T1)ab
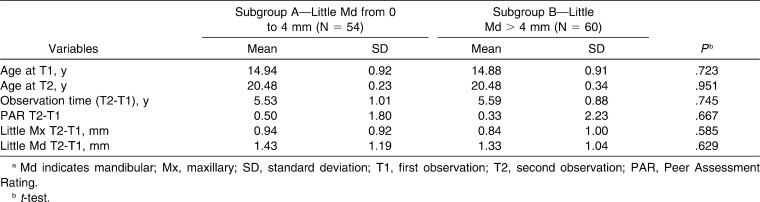
There was no difference in ages, observation period, and PAR and Little index changes (T2-1) when subgroups A and B were compared (Table 8).
Table 8. .
Results of Comparison of Subgroups A and B, Divided by the Severity of Mandibular Crowding at the First Observation Stagea
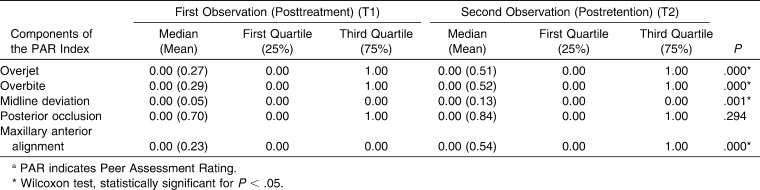
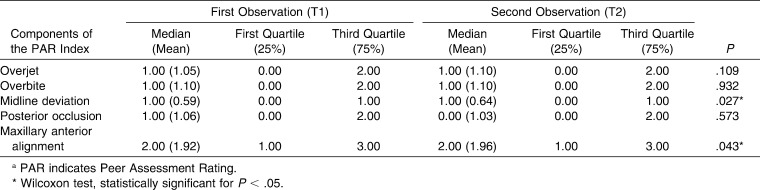
For the treated groups, the overjet, overbite, midline deviation, and maxillary anterior alignment components significantly increased from posttreatment to postretention stage (Table 9). For the untreated group, only the midline deviation and the maxillary anterior component significantly increased (Table 10).
Table 9. .
Intragroup Comparison of the Components of the PAR Index Between First and Second Observations for Groups 1 and 2 (Treated, N = 155)a
Table 10. .
Intragroup Comparison of the Components of the PAR Index Between First and Second Observations for Group 2 (Untreated, N = 114)a
DISCUSSION
Sample and Groups Compatibility
The sample includes a great number of subjects divided into three groups, two treated and one untreated. This way, it is certainly not a totally homogeneous sample, because patients of the treated groups presented, as expected, a better occlusal condition (PAR and Little indexes) at posttreatment (T1) than the untreated group presented at the first observation stage (T1; Table 7). This difference was already reported in other studies comparing treated and untreated groups,1,6 because the treated group is expected to have a better occlusal condition than untreated patients.
However, the groups presented similar sex distribution (Table 3), type of malocclusion (Table 4), severity of the Class II molar relationship (Table 5), and ages and length of observation period (Table 6).
The sample selection criteria and compatibility of the groups seemed to be appropriately used for the comparison of posttreatment and postretention changes with those of the natural development.
Regarding the treated groups, all cases had similar retention protocol to ensure the stability of the results.19–21 Extraction and nonextraction protocols seem to have no influence on postretention stability2; however, we evaluated these cases in groups separately. Extraction- and nonextraction-treated groups were compatible regarding age at pretreatment, treatment time, and PAR at T0. As expected, the extraction group showed greater Little maxillary and mandibular indexes than the nonextraction group (Table 2).
Methodology
The best evaluation of occlusion changes is performed on dental casts. Despite not allowing clinic and radiographic evaluation, the dental cast gathers the largest amount of information related to orthodontic diagnosis and treatment.23
Currently the occlusal indexes constitute an important research method.5 Therefore, the PAR index was used for occlusal evaluation and the Little index was used for the detailed evaluation of maxillary and mandibular irregularity.
Intergroup and Intragroup Comparison
As expected, at T1, the treated groups presented a better occlusal condition, showing smaller PAR and Little indexes than the untreated group (Table 7). At T2, the treated groups also presented smaller PAR and Little indexes when compared to the untreated group (Table 7). This was expected because the treated groups received orthodontic treatment to correct the malocclusion and the untreated group did not.
In the observation period, the treated groups showed greater increases in PAR and Little maxillary indexes than the untreated group (Table 7).
Our result corroborates the findings of Al Yami et al.,5 in which the evaluation of an untreated sample found that the PAR score was not affected by physiological growth between 12 and 22 years of age, irrespective of the Angle classification or the treatment need. Sixty three percent of the cases showed no improvement of the PAR index or became worse. The present study found an increase of only 0.41 in the PAR index between the first and second observation stages in the untreated group.
The treated extraction and nonextraction groups showed a similar change (relapse) of 2.92 and 2.22 for the PAR index, respectively, which is in agreement with the relapse found by Freitas et al.24 (2.87 measured by the PAR index) and is less than the 4.00 points in the PAR relapse found by Woods et al.25
Based on the present study results, the postretention relapse of the treated groups according to the PAR index was significantly greater than the physiological changes due to normal development in the untreated group. This is also true for maxillary anterior crowding.
In the observation period, the change in the Little mandibular index was greater in the treated extraction group than in the untreated group (Table 7).
Our results corroborate the findings of Sinclair and Little1 that compared the natural development in an untreated normal occlusion group with a treated extraction group and found that mandibular crowding relapse was greater than the late mandibular crowding presented in the untreated group.
Richardson26 found that 50 untreated subjects who were longitudinally followed from 13 to 18 years showed an average increase in mandibular crowding of 2.36 mm, which is greater than the 1.38 mm of the present study. Maybe the difference in the ages can explain this difference.
Eslambolchi et al.3 found that from 13 to 19 years, the mandibular crowding of untreated subjects increased 1.57 mm, similar to the present study that demonstrated that from 15 to 20 years the mandibular irregularity increased 1.38 mm.
Driscoll-Gilliland et al.6 found that there were no difference in the changes in irregularity of mandibular teeth between a treated extraction and an untreated group. Our results showed similar changes in the mandibular index between the nonextraction and untreated groups, but significantly different changes among the extraction and the untreated groups. Maybe the greater pretreatment mandibular irregularity of the extraction group can explain these findings, since the severity of initial mandibular crowding can influence the amount of relapse.27,28
One concern was whether the severity of the mandibular irregularity would influence the amount of crowding increase in the untreated group. To address this concern, the untreated group was divided into two subgroups according to the severity of the mandibular crowding at T1.
The results showed that the changes of PAR and Little maxillary and mandibular indexes were similar in both groups (Table 7). It indicates that the amount of mandibular anterior crowding does not influence the changes due to natural development of untreated subjects. Untreated subjects with less or more mandibular crowding showed similar increase in crowding from 15 to 20 years.
For the whole treated group, overjet, overbite, midline deviation, and maxillary anterior alignment components increased significantly from the posttreatment to postretention stages, ie, showed a significant postretention relapse (Table 8). Only the posterior occlusion did not show significant relapse (Table 8). The posterior occlusion was previously shown to be stable in the long term.19
For the untreated group, only midline deviation and maxillary anterior alignment increased significantly (Table 9). Overjet, overbite, and posterior occlusion did not significantly change from T1 to T2. Maxillary anterior crowding is known to increase with age,5 and therefore midline deviation should increase consequent to displacement of the maxillary incisors.
The present study proved that the mandibular incisor crowding occurs as a relapse of orthodontic treatment and also as part of the normal developmental process, despite the fact that it is greater in treated extraction cases, but it is similar to treated nonextraction cases. This corroborates somewhat the statement of Thilander2 that late changes occurring during the postretention period generally cannot be distinguished from normal aging processes.
The present results underline the importance of studies showing that untreated dentitions change with time. Education of orthodontic patients about retention protocols and late developmental crowding is imperative.3 The development of mandibular incisor crowding appears to be a continuous process throughout life, but more evidence is needed to understand why these changes occur.3
CONCLUSIONS
The treated groups showed more changes according to PAR and Little maxillary indexes than the untreated group in the observation period.
The posttreatment change of the mandibular anterior crowding of the treated extraction group was greater than the mandibular crowding caused by physiologic changes in the untreated group.
REFERENCES
- 1.Sinclair P. M, Little R. M. Maturation of untreated normal occlusions. Am J Orthod. 1983;83:114–123. doi: 10.1016/s0002-9416(83)90296-8. [DOI] [PubMed] [Google Scholar]
- 2.Thilander B. Orthodontic relapse versus natural development. Am J Orthod Dentofacial Orthop. 2000;117:562–563. doi: 10.1016/s0889-5406(00)70200-9. [DOI] [PubMed] [Google Scholar]
- 3.Eslambolchi S, Woodside D. G, Rossouw P. E. A descriptive study of mandibular incisor alignment in untreated subjects. Am J Orthod Dentofacial Orthop. 2008;133:343–353. doi: 10.1016/j.ajodo.2006.04.038. [DOI] [PubMed] [Google Scholar]
- 4.Afsharpanah A, Feghali R, Hans M. G, Nelson S. Assessment of orthodontically untreated adolescents using the PAR index [abstract 2767] J Dent Res. 1996;75:363. [Google Scholar]
- 5.Al Yami E. A, Kuijpers-Jagtman A. M, van't Hof M. A. Assessment of biological changes in a nonorthodontic sample using the PAR index. Am J Orthod Dentofacial Orthop. 1998;114:224–228. doi: 10.1053/od.1998.v114.a85827. [DOI] [PubMed] [Google Scholar]
- 6.Driscoll-Gilliland J, Buschang P. H, Behrents R. G. An evaluation of growth and stability in untreated and treated subjects. Am J Orthod Dentofacial Orthop. 2001;120:588–597. doi: 10.1067/mod.2001.118778. [DOI] [PubMed] [Google Scholar]
- 7.Wheeler T. T, McGorray S. P, Dolce C, Taylor M. G, King G. J. Effectiveness of early treatment of Class II malocclusion. Am J Orthod Dentofacial Orthop. 2002;121:9–17. doi: 10.1067/mod.2002.120159. [DOI] [PubMed] [Google Scholar]
- 8.Andrews L. F. The Straight Wire Appliance Syllabus of Philosophy and Techniques 2nd ed. San Diego, Calif: Larry F. Andrews Foundation of Orthodontic Education and Research; 1975. [Google Scholar]
- 9.Richmond S, Shaw W. C, O'Brien K. D, et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 10.DeGuzman L, Bahiraei D, Vig K. W, Vig P. S, Weyant R. J, O'Brien K. The validation of the Peer Assessment Rating index for malocclusion severity and treatment difficulty. Am J Orthod Dentofacial Orthop. 1995;107:172–176. doi: 10.1016/s0889-5406(95)70133-8. [DOI] [PubMed] [Google Scholar]
- 11.Little R. M. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 12.Burden D. J, McGuinness N, Stevenson M, McNamara T. Predictors of outcome among patients with class II division 1 malocclusion treated with fixed appliances in the permanent dentition. Am J Orthod Dentofacial Orthop. 1999;116:452–459. doi: 10.1016/s0889-5406(99)70232-5. [DOI] [PubMed] [Google Scholar]
- 13.Richmond S, Shaw W. C, Stephens C. D, Webb W. G, Roberts C. T, Andrews M. Orthodontics in the general dental service of England and Wales: a critical assessment of standards. Br Dent J. 1993;174:315–329. doi: 10.1038/sj.bdj.4808166. [DOI] [PubMed] [Google Scholar]
- 14.Otuyemi O. D, Jones S. P. Long-term evaluation of treated class II division 1 malocclusions utilizing the PAR index. Br J Orthod. 1995;22:171–178. doi: 10.1179/bjo.22.2.171. [DOI] [PubMed] [Google Scholar]
- 15.Birkeland K, Furevik J, Boe O. E, Wisth P. J. Evaluation of treatment and posttreatment changes by the PAR Index. Eur J Orthod. 1997;19:279–288. doi: 10.1093/ejo/19.3.279. [DOI] [PubMed] [Google Scholar]
- 16.Dyken R. A, Sadowsky P. L, Hurst D. Orthodontic outcomes assessment using the peer assessment rating index. Angle Orthod. 2001;71:164–169. doi: 10.1043/0003-3219(2001)071<0164:OOAUTP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Dahlberg G. Statistical Methods for Medical and Biological Students. New York, NY: Interscience Publications; 1940. [Google Scholar]
- 18.Houston W. J. B. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 19.Al Yami E. A, Kuijpers-Jagtman A. M, van't Hof M. A. Stability of orthodontic treatment outcome: follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999;115:300–304. doi: 10.1016/s0889-5406(99)70333-1. [DOI] [PubMed] [Google Scholar]
- 20.Little R. M, Wallen T. R, Riedel R. A. Stability and relapse of mandibular anterior alignment—first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:349–365. doi: 10.1016/0002-9416(81)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Shah A. A. Postretention changes in mandibular crowding: a review of the literature. Am J Orthod Dentofacial Orthop. 2003;124:298–308. doi: 10.1016/s0889-5406(03)00447-5. [DOI] [PubMed] [Google Scholar]
- 22.Rossouw P. E, Preston C. B, Lombard C. A longitudinal evaluation of extraction versus nonextraction treatment with special reference to the posttreatment irregularity of the lower incisors. Semin Orthod. 1999;5:160–170. doi: 10.1016/s1073-8746(99)80007-3. [DOI] [PubMed] [Google Scholar]
- 23.Han U. K, Vig K. W, Weintraub J. A, Vig P. S, Kowalski C. J. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofacial Orthop. 1991;100:212–219. doi: 10.1016/0889-5406(91)70058-5. [DOI] [PubMed] [Google Scholar]
- 24.Freitas K. M, Janson G, Freitas M. R, Pinzan A, Henriques J. F, Pinzan-Vercelino C. R. Influence of the quality of the finished occlusion on postretention occlusal relapse. Am J Orthod Dentofacial Orthop. 2007;132:428e9–428e14. doi: 10.1016/j.ajodo.2007.02.051. [DOI] [PubMed] [Google Scholar]
- 25.Woods M, Lee D, Crawford E. Finishing occlusion, degree of stability and the PAR index. Aust Orthod J. 2000;16:9–15. [PubMed] [Google Scholar]
- 26.Richardson M. E. Late lower arch crowding: the role of the transverse dimension. Am J Orthod Dentofacial Orthop. 1995;107:613–617. doi: 10.1016/s0889-5406(95)70104-4. [DOI] [PubMed] [Google Scholar]
- 27.Artun J, Garol J. D, Little R. M. Long-term stability of mandibular incisors following successful treatment of Class II, Division 1, malocclusions. Angle Orthod. 1996;66:229–238. doi: 10.1043/0003-3219(1996)066<0229:LTSOMI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Kahl-Nieke B, Fischbach H, Schwarze C. W. Treatment and postretention changes in dental arch width dimensions—a long-term evaluation of influencing cofactors. Am J Orthod Dentofacial Orthop. 1996;109:368–378. doi: 10.1016/s0889-5406(96)70118-x. [DOI] [PubMed] [Google Scholar]