Abstract
Background:
Yoga has been extensively used as an alternative or complementary therapy in psychiatric disorders depending on the type and severity of the disorders. However, data related to perspective on yoga services and the benefits and adverse effects attributed to yoga by patients with major psychiatric disorders is lacking.
Aim:
The aim of the study was to assess feedback of the patients who attended yoga sessions at a Yoga center in a tertiary neuropsychiatric hospital.
Materials and Methods:
This was a cross-sectional retrospective study using a specific questionnaire to get feedback from patients referred to the NIMHANS Integrated Center for Yoga, at the end of their yoga training.
Results:
Two hundred and one patients’ data were included in this retrospective study. Most of the patients were referred by the doctors. The yoga module for schizophrenia was most commonly utilized, followed by depression. On an average, patients attended 13 sessions. Most of them practiced yoga for 1–2 weeks and had missed less than 2 sessions. The great majority of the patients reported that practicing yoga helped them. Spearman correlation analysis revealed positive associations between improvement attributed to yoga and variables affecting quality of yoga services at the center, including the quality of yoga sessions attended. Overall health and sleep improvement also positively correlated with improvement attributed to yoga. A minority of patients reported adverse effects, although these did not lead to discontinuation.
Conclusion:
In this retrospective study of patients referred to a Yoga center in a tertiary psychiatric facility, the majority of patients with major mental disorders were able to practice yoga under supervision and reported significant improvement in symptoms with minimal adverse effects.
Keywords: Feedback, psychiatric disorders, retrospective study, yoga, yoga practice
INTRODUCTION
Complementary and Alternative Medicine (CAM) or “complementary health approaches” are a group of diverse medical and health-care practices/products that are outside of conventional modern medicine. The National Center for Complementary and Integrative Health classifies most complementary health approaches into two subgroups, namely natural products and mind and body practices. Yoga is one of the practices classified under mind and body practices.[1]
CAM therapies are termed as Alternative when used in place of conventional treatments and Complementary when used together with conventional treatments. Integrative medicine combines mainstream medical therapies and CAM therapies in a coordinated way.
Yoga is a group of physical, mental, and spiritual practices or disciplines which had its origin in ancient India. It is known worldwide for its general benefits such as increase in muscle strength, flexibility, and improvement in mood/ability to handle stress.[2,3] Recently, it has been shown to be effective in psychiatric disorders as an add-on treatment or even sole therapy in some cases. Studies have demonstrated its efficacy in reducing depressive/anxiety symptoms and negative symptoms of schizophrenia.[4,5,6] It has also been found useful in improving social cognition in schizophrenia patients[7] and cognitive functions, sleep and quality of life (QOL) in the elderly.[8,9] In addition to patients, yoga has been found useful in reducing perceived burden and improving QOL of caregivers attending to patients with major mental disorders.[10] Yoga can be used as an Alternative or Complementary therapy or as a part of an integrated approach depending on the type/severity of disorder. For example, as a monotherapy in mild depressive episode, it becomes an alternative approach; as an add-on in schizophrenia, it becomes complementary, and in anxiety disorders, it becomes a part of an integrated approach along with pharmacotherapy and behavioral therapy.
Although there are benefits from yoga as an add-on in psychiatric disorders, its utilization as clinical service by the patients, especially in hospital settings, appears to be suboptimal. Data related to utilization of yoga services and the benefits/adverse effects in major psychiatric disorders in a tertiary care setup is lacking. The NIMHANS Integrated Center for Yoga (NICY), located in a tertiary care psychiatric hospital in South India, has been offering yoga clinical services to patients for the past 13 years, and is one of the few such centers dedicated to patients with major mental disorders. Patients referred to the NICY are initially screened by a psychiatrist and then seen by a yoga physician. After an initial orientation session, the patient is then allocated to a group session of yoga where a trained yoga therapist teaches a generic module of yoga designed for specific groups of disorders such as schizophrenia,[11] depression,[12] obsessive-compulsive disorder,[13] mild cognitive impairment,[14] caregivers of schizophrenia,[15] and Parkinson's disease.[16] In this manuscript, we present the data related to the feedback given by the patients who attended yoga sessions at NICY.
MATERIALS AND METHODS
Sample and setting
It was a cross-sectional retrospective study done using a questionnaire, conducted at the NICY. Patients (both inpatients and outpatients) with neuropsychiatric disorders, referred to the NICY from September 2017 to August 2019 for yoga therapy formed the sample. A total of 3290 patients were referred to Yoga center during this period. Among these, patients who had finished more than 2 weeks of yoga training or attended more than 10 sessions of yoga were given the feedback form. These criteria were considered to cover an adequate period for the yoga to be learned and produce effects. 201 patients meeting the above criteria consented and filled the feedback form. About 30 patients who met the criteria could not be given the form since they did not give consent to fill the form or were discharged without the yoga therapists knowledge, or did not turn up for the sessions. Available data from all the filled feedback forms were analyzed.
The sample consisted of patients with neuropsychiatric disorders with the majority being psychiatric disorders. Specific diagnosis was schizophrenia/psychotic illness, bipolar affective disorders, major depressive disorder, anxiety disorders, ADHD, autism, seizure disorder, Parkinson's disease. Data of consenting patients who had the capacity to answer the questionnaire at the time of discharge or completion of yoga sessions at the center were included in this retrospective study. A written informed consent was taken from the parents/guardians (in case patient could not give consent), and assent was taken from subjects below 18 years of age at the time of starting the yoga sessions for willingness to practice yoga and at the end of the training for taking their feedback.
Ethical approval for analysis of retrospective data was obtained from the Humans Ethics committee for Research in AYUSH and Integrative Medicine, National Institute of Mental Health and Neurosciences with the reference no: NIMHANS/HECAIM/2nd/Meeting/2020–2021.
Questionnaire development
The contents of the questionnaire were arrived at by a consensus among the investigators. It was developed in the year 2017. It included details of demographics, mode of referral, past history of yoga practice, yoga module practiced, yoga sessions in the center (number of sessions attended/missed), benefits/side effects of yoga, and their view regarding continuation of yoga sessions at home. A visual analog scale (VAS) was used to assess improvement in symptoms, patients’ attribution of improvement to yoga practice (0 being no improvement and 10 being complete improvement) and to rate the facilities available at the Yoga center (0 being worst, 10 being best). It was a self-administered questionnaire. The options given to the patient for each question were generated based on the clinical experience of the authors who were following up psychiatric patients receiving yoga therapy in the Yoga center for the past 5–8 years. The option of “others” was added for patients in case what they had to express was unavailable in the given options.
Data collection
Data of the consecutive patients referred to the NICY were screened, and consenting patients data were included in this retrospective study. The questionnaire was given to them at the end of their yoga training. Data of 201 patients were included in this retrospective study.
Analysis
IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. (Armonk, NY: IBM Corp.) was used for analysis. Descriptive statistics and Spearman correlation were used.
RESULTS
A total of 201 (N) subjects with age range between 16 and 79 years (M-33.4, SD-13.5) completed the retrospective study. The sample consisted of 55.7% (112) males and 44.3% (89) females. It was observed that 77% (154) of the subjects were referred to yoga therapy by the treating doctor as shown in Figure 1.
Figure 1.
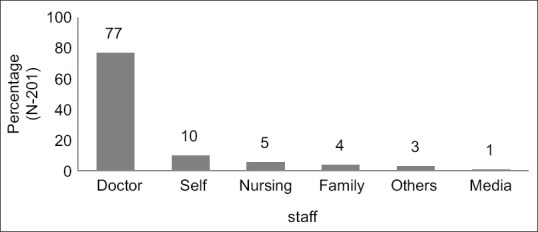
Mode of patients referral to the Yoga center. Each bar represents the source of referral. Value is expressed in percentage at the top of the bar
Yoga session details
Among the modules, the most commonly prescribed yoga module was the module for schizophrenia (38%), followed by yoga module for depression (20%) [Figure 2]. Individual yoga sessions lasted for 1 h, with usually one session per day. 38% (76) of the patients attended yoga sessions for a duration of 1–2 weeks [Figure 3]. The number of sessions attended by the patients ranged between 2 and 62 (M-13, SD-10.5). It was observed that 51% (103) of them had missed 2 or less than 2 sessions, 19% (39) had missed 2–5 sessions, 11% (22) had missed more than 6 sessions, and in 18% (37), the data were missing. The reasons given for missing the session was that they were feeling sleepy (n-26, 13%), had increased pain and stiffness (n-10, 5%), fatigue (n-8, 4%), other reasons (n-106, 53%), with missing values of 25% (51).
Figure 2.

Generic Yoga modules prescribed to the patients. Each bar represents the name of the generic yoga modules used for a particular psychiatric disorder. Value is expressed in percentage at the top of the bar
Figure 3.

Duration of yoga practice by the patients during their practice at the Yoga center. Each bar represents duration of the practice in weeks. Value is expressed in percentage at the top of the bar
Yoga practice
Benefits of yoga
The great majority of the patients (n-194, 96.5%) reported that practicing yoga helped them [Figure 4]. They reported that yoga practice helped them by improving their general fitness (n-44, 23%), disorder-specific symptoms like depressive/anxiety symptoms (n-27, 14%), emotional stability (n-29, 15%), spirituality (n-6, 3%), and other ways (n-3, 1.5%). This data had 43% (92) missing values.
Figure 4.

Yoga practice details. Bars in individual groups represent benefits, adverse/side effects of yoga practice along with their opinion about continuing it at home and past history of yoga practice. Value is expressed in percentage at the top of the bar
Adverse effects of yoga
93% (186) of them reported that there were no adverse effects during the yoga practice [Figure 4]. 7.5% (15) patients reported some adverse effects in the form of pain (n-4), minor injury (n-3), worsening of symptoms (n-2), emotional instability (2), and others (n-4).
Previous history of yoga practice
It was observed that a significant proportion of patients (108, 54%) had practiced some yoga in the past 1 year [Figure 4]. 22% (44) of them had practiced 4–20 sessions, 20% (39) of them had practiced for less than 4 sessions, 13% (26) of them had practiced for more than 20 sessions, and this data had 46% (92) missing values.
Willingness to practice at home after training
89% (178) of them reported that there would be no difficulty in continuing yoga practice at home [Figure 4]. 11% (23) of them anticipated difficulty in continuing yoga at home with reasons such as not being able to remember the yoga module, nonavailability of yoga therapist, laziness to practice, and feeling that there was no need to practice once they feel better.
Correlation analysis
Results of the Spearman correlation indicated that there was a significant positive association between percentage of improvement specifically attributed to yoga practice and the variables such as facilities at yoga center, yoga module practiced, yoga center staff, yoga therapists and doctors in the Yoga center, overall health/sleep after yoga, and the patients recommending yoga to their family or friends. All these variables were measured on VAS. These associations were of weak-moderate strength (rs[195] =0.205–0.487, P < 0.01). Details are shown in Table 1.
Table 1.
Correlations among variables
| Variables | Percentage of improvement specifically attributed Yoga practice |
|---|---|
| Quality of Yoga center facilities | |
| Correlation coefficient | 0.301** |
| Significant (two-tailed) | 0.001 |
| n | 195 |
| Quality of the Yoga module practiced | |
| Correlation coefficient | 0.324** |
| Significant (two-tailed) | 0.001 |
| n | 195 |
| Quality rating of Yoga center staff | |
| Correlation coefficient | 0.250** |
| Significant (two-tailed) | 0.001 |
| n | 195 |
| Quality of yoga therapist | |
| Correlation coefficient | 0.234** |
| Significant (two-tailed) | 0.001 |
| n | 195 |
| Quality of doctors in Yoga center | |
| Correlation coefficient | 0.205** |
| Significant (two-tailed) | 0.004 |
| n | 195 |
| Improvement in overall health after Yoga | |
| Correlation coefficient | 0.487** |
| Significant (two-tailed) | 0.001 |
| n | 195 |
| Improvement in sleep after yoga | |
| Correlation coefficient | 0.269** |
| Significant (two-tailed) | 0.001 |
| n | 191 |
| Possibility of recommending yoga to family/friend | |
| Correlation coefficient | 0.211** |
| Significant (two-tailed) | 0.003 |
| n | 195 |
**P<0.01
DISCUSSION
This article aims to provide details on the feedback of patients referred to an in-house Yoga center at a tertiary care psychiatric hospital, which is a rarity in such institutions. We observed that most patients were referred to the Yoga center by the doctors, followed by self-referrals. Higher referral from doctors is likely to be due to the presence of a dedicated Yoga center in the same hospital. Second, since the hospital is primarily a modern medicine hospital, the patients may also not be aware of the availability of the yoga services in the hospital till the doctor informed them. This indicates that awareness about the availability and possible benefits of yoga in psychiatric disorders needs to be increased among the patients/caregivers and more such centers need to be established within hospitals.
Since this study was conducted in a tertiary neuropsychiatric hospital and the majority of the subjects were inpatients, it seems logical that the yoga module for schizophrenia was most commonly used followed by the yoga module for depression. On an average, patients attended 13 sessions. Most of them practiced yoga for 1–2 weeks and had missed less than 2 sessions. This shows that psychiatrically ill patients also can learn and practice yoga and adhere to yoga practice.
Most of the patients reported that yoga helped them in improving their general fitness, emotional stability, overall health, and sleep. This is similar to previous studies.[2,3,17] Some of them reported disorder-specific benefits like improvement in depressive/anxiety symptoms, which correspond to the known benefits of yoga.[18,19] In spite of being on other modes of treatment, some of them considered yoga as one of the important reasons for their improvement. Most of them did not suffer from any adverse effects of yoga, the minority who did experience had mild adverse effects which did not lead to discontinuation of yoga practice or significant morbidity. This indicates that Yoga may be beneficial and safe in psychiatrically ill patients.
The majority of patients reported that they did not anticipate any difficulty in practicing at home after discharge, although a minority anticipated difficulties due to various factors including lack of trained therapists near their residence. This has been recognized as one of the major barriers to utilization of yoga among patients with mental disorders.[20] Half of the patients had past experience of yoga practice. This indicates that yoga therapy can be considered as a feasible add-on therapy in psychiatric disorders but more thought needs to be given to increase availability of trained therapists in the community or providing continued supervision through other means such as virtual tele yoga sessions.
Spearman correlation revealed positive associations between improvement attributed to yoga and the arrangements available in the yoga center like facilities, yoga module, doctors, therapists, and staff. This suggests that improvement due to yoga is linked to better facilities at the yoga center. From this, it can be concluded that the environment and service providers are important for the benefits of yoga therapy to be achieved in such populations.
Overall health and sleep improvement also positively correlated with improvement due to yoga. Yoga is well known to improve physical and psychological health. Although yoga was an add-on treatment for most patients, they appreciated the specific benefits of yoga, separating it from benefits from the other modes of treatments they were receiving. This suggests that yoga has additional benefits than treatment as usual. The finding that recommendation of yoga to others positively correlated to improvement due to yoga in the patients further suggests that these patients did perceive real benefits from the practice which made them confident to suggest yoga to their family and friends.
Limitations of the study
Since it was a retrospective study in a selected population attending a yoga center in a tertiary hospital, the results, associations, and conclusions drawn may not be generalizable to other populations. Given the nature of the study, there is likely to be responder bias and memory bias.
CONCLUSION
In this retrospective study of patients referred to a Yoga center in a tertiary psychiatric facility, the majority of patients with major mental disorders were able to practice yoga under supervision and reported significant improvement in symptoms with minimal incidence of adverse effects. Most patients also endorsed yoga as a significant contributing factor in the improvement and were willing to continue practice at home, although some anticipated difficulties due to the lack of such facilities close to their home. These findings should encourage the provision of more such units in psychiatric hospitals and also spur innovative models for providing continued yoga supervision to such patients in the community.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank the doctors in the NICY for evaluating the patients before the recruitment, Yoga Therapists at the NICY for training the patients in Yoga practice, and Dr. Mariamma Philip, Additional Professor, Biostatistics, NIMHANS for the help in data analysis. We acknowledge the Central Council for Research in Yoga and Naturopathy (CCRYN), New Delhi for funding a Collaborative Research Centre for Yoga at NIMHANS.
REFERENCES
- 1.Wong SS, Nahin RL. National Center for Complementary and Alternative Medicine perspectives for complementary and alternative medicine research in cardiovascular diseases. Cardiol Rev. 2003;11:94–8. doi: 10.1097/01.CRD.0000053452.60754.C5. [DOI] [PubMed] [Google Scholar]
- 2.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ross A, Thomas S. The health benefits of yoga and exercise: A review of comparison studies. J Altern Complement Med. 2010;16:3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- 4.Naveen GH, Thirthalli J, Rao MG, Varambally S, Christopher R, Gangadhar BN. Positive therapeutic and neurotropic effects of yoga in depression: A comparative study. Indian J Psychiatry. 2013;55:S400–4. doi: 10.4103/0019-5545.116313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia – A randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 6.Cramer H, Lauche R, Anheyer D, Pilkington K, de Manincor M, Dobos G, et al. Yoga for anxiety: A systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2018;35:830–43. doi: 10.1002/da.22762. [DOI] [PubMed] [Google Scholar]
- 7.Jayaram N, Varambally S, Behere RV, Venkatasubramanian G, Arasappa R, Christopher R, et al. Effect of yoga therapy on plasma oxytocin and facial emotion recognition deficits in patients of schizophrenia. Indian J Psychiatry. 2013;55:S409–13. doi: 10.4103/0019-5545.116318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hariprasad VR, Varambally S, Shivakumar V, Kalmady SV, Venkatasubramanian G, Gangadhar BN. Yoga increases the volume of the hippocampus in elderly subjects. Indian J Psychiatry. 2013;55:S394–6. doi: 10.4103/0019-5545.116309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hariprasad VR, Sivakumar PT, Koparde V, Varambally S, Thirthalli J, Varghese M, et al. Effects of yoga intervention on sleep and quality-of-life in elderly: A randomized controlled trial. Indian J Psychiatry. 2013;55:S364–8. doi: 10.4103/0019-5545.116310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varambally S, Vidyendaran S, Sajjanar M, Thirthalli J, Hamza A, Nagendra HR, et al. Yoga-based intervention for caregivers of outpatients with psychosis: A randomized controlled pilot study. Asian J Psychiatr. 2013;6:141–5. doi: 10.1016/j.ajp.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 11.Govindaraj R, Varambally S, Sharma M, Gangadhar BN. Designing and validation of a yoga-based intervention for schizophrenia. Int Rev Psychiatry. 2016;28:323–6. doi: 10.3109/09540261.2016.1151404. [DOI] [PubMed] [Google Scholar]
- 12.Naveen GH, Rao MG, Vishal V, Thirthalli J, Varambally S, Gangadhar BN. Development and feasibility of yoga therapy module for out-patients with depression in India. Indian J Psychiatry. 2013;55:S350–6. doi: 10.4103/0019-5545.116305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhat S, Varambally S, Karmani S, Govindaraj R, Gangadhar BN. Designing and validation of a yoga-based intervention for obsessive compulsive disorder. Int Rev Psychiatry. 2016;28:327–33. doi: 10.3109/09540261.2016.1170001. [DOI] [PubMed] [Google Scholar]
- 14.Hariprasad VR, Varambally S, Varambally PT, Thirthalli J, Basavaraddi IV, Gangadhar BN. Designing, validation and feasibility of a yoga-based intervention for elderly. Indian J Psychiatry. 2013;55:S344–9. doi: 10.4103/0019-5545.116302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jagannathan A, Hamza A, Thirthalli J, Nagendra H, Nagarathna R, Gangadhar BN. Development and feasibility of need-based yoga program for family caregivers of in-patients with schizophrenia in India. Int J Yoga. 2012;5:42–7. doi: 10.4103/0973-6131.91711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kakde N, Metri KG, Varambally S, Nagaratna R, Nagendra HR. Development and validation of a yoga module for Parkinson disease. J Complement Integr Med. 2017;14:20150112. doi: 10.1515/jcim-2015-0112. [DOI] [PubMed] [Google Scholar]
- 17.Diamond L. The benefits of yoga in improving health. Prim Health Care. 2012;22:16–9. [Google Scholar]
- 18.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 19.Li AW, Goldsmith CA. The effects of yoga on anxiety and stress. Altern Med Rev. 2012;17:21–35. [PubMed] [Google Scholar]
- 20.Baspure S, Jagannathan A, Kumar S, Varambally S, Thirthalli J, Venkatasubramanain G, et al. Barriers to yoga therapy as an add-on treatment for schizophrenia in India. Int J Yoga. 2012;5:70–3. doi: 10.4103/0973-6131.91718. [DOI] [PMC free article] [PubMed] [Google Scholar]


