Abstract
This systematic review and meta-analysis aimed to provide a summary of the existing evidence on the prevalence of depression among cancer patients worldwide to assist health policymakers in adopting appropriate measures to prevent and control depression in these patients. EMBASE, Google Scholar, Scopus, PubMed, and Web of Science databases were searched for original studies published in English from January 2000 to July 2019. The studies were screened on the basis of quality and relevance criteria. The statistical analyses were conducted in the R software. Out of 182,521 cancer patients examined in 183 studies, 49,280 (~27%) had depression (95% confidence interval [CI] = 24%–30%). The highest prevalence of depression was among patients with colorectal cancer with 32% (95% CI = 20%–47%). Among countries, Pakistan with 43% (95% CI = 26%–64%), and among continents, Africa with 36% (95% CI = 29%–43%) had the highest prevalence of reported depression in cancer patients. Adjusting for sample size, the prevalence of depression among female cancer patients, 31% (95% CI = 26%–36%), was higher than men, 26% (95% CI = 21%–31%). The prevalence of depression among cancer patients is increasing by an average of 0.6% per year. The findings show higher prevalence of depression among cancer patients in underdeveloped and developing countries compared to the developed nations and the global average.
Keywords: Cancer, depression, global, meta-analysis, review
INTRODUCTION
Depression is the most common mental illness that can substantially affect the quality of personal and social life, resulting in a major public health problem. According to the World Health Organization (WHO), approximately 264 million people worldwide suffer from depression.[1] Depression can cause a wide range of disabilities and increase the overall burden of the disease as well as the cost of treatments.[2] Thus, to save the resources of the healthcare system, it is better to adopt some measures to prevent depression than to deal with its consequences.[3,4,5,6]
While the main causes of depression are family, social, and economic problems, physical illnesses can also cause mental symptoms such as anxiety and depression. Studies have shown that depression is more prevalent among patients with chronic diseases and fatal diseases such as cancer than in healthy populations.[7] Patients with cancer are more likely to experience physical and psychological stress than patients with nonneoplastic diseases, even those with a worse prognosis.[8] Prolonged psychological stress can cause anxiety and depression, explaining why they are common problems among cancer patients. Further, depression is often associated with other syndromes and symptoms such as anxiety disorders (e.g., posttraumatic stress disorder, panic disorder, and generalized anxiety disorder) and pain.[9,10,11,12]
Psychological conditions such as depression can greatly affect the progression of the disease.[13] Many cancer patients as well as physicians believe that the patient's mental state can affect the outcome of treatment.[14] Cancer patients with depression have a higher mortality prevalence than nondepressed patients, which highlights the importance of preventing and treating depression in these patients.[15,16,17,18]
Literature suggested that psychological interventions could effectively improve physical and mental health of cancer patients.[19] However, before psychotherapy or use of antidepressant medication, it is suggested to initially evaluate the prevalence of depression among cancer patients and identify influencing factors which potentially contribute to mental disorders.[20] Consequently, effective psychological supportive interventions could be established for these patients to effectively respond to their emotional and mental needs. Thus, the first important step is to evaluate the overall prevalence of depression in populations suffering from cancer and then develop relevant treatment strategies based on the findings.
There have been several studies on the prevalence of depression in cancer patients. In a 2013 cross-sectional study conducted in the United States, 34% of the 34,123 patients with cervical cancer were diagnosed to be depressed.[21] In another cross-sectional study, which was conducted in Korea in 2017, only 3% of the 30,000 patients with various types of cancer were diagnosed as depressed with ICD-10.[22] Reviewing similar studies reveals that the overall prevalence of depression in cancer patients ranges between 0% and 58%.[23] Lack of a definite prevalence might be due to different definitions given for depression; the use of diverse tools to assess depression; patients’ diversity in terms of cancer type; and disease severity.[24]
Despite the multitude of studies carried out on this topic, there are still a number of gaps in the existing literature. To the best of our knowledge, up to now, there has not been a meta-analysis to assess the prevalence of depression and the impact of various factors among cancer patients worldwide, with a view to adopt appropriate measures to prevent and control depression in these patients, thereby reducing treatment costs and saving resources of healthcare systems.[25,26] Researchers can benefit from a prevalence systematic review and meta-analysis of the findings reported from various aspects to further investigate the issue of depression in cancer patients.
METHODS
Registration
The study was registered in PROSPERO, which is an international database established and maintained by the University of York for prospectively registered systematic reviews in relation to health and social care. The registration sheet can be accessed from the following link:
https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID = 171363.
Search process
EMBASE, Scopus, PubMed, and Web of Science databases were searched for original articles published in English from January 2000 to July 2019 with the following keywords: “Neoplasia,” “Neoplasias,” “Neoplasm,” “Tumors,” “Tumor” “Cancer,” “Cancers,” “Malignancy,” and “Malignancies” (Main MeSH terms for Depression, available at https://www.ncbi.nlm.nih.gov/mesh/68003863), and also “Depressions,” “Depression,” “Depressive Symptoms,” and “Emotional Depression” (Main MeSH terms for Neoplasms, available at https://www.ncbi.nlm.nih.gov/mesh/68009369). The initial search revealed 2865 articles. Other sources such as Google Scholar were also searched, and 34 articles were retrieved. The studies conducted before 2000 were excluded to limit the time span to the past 20 years. The software EndNote was used to detect and remove duplicates. At the end of this phase, the number of articles included in the study was 1260.
Study selection
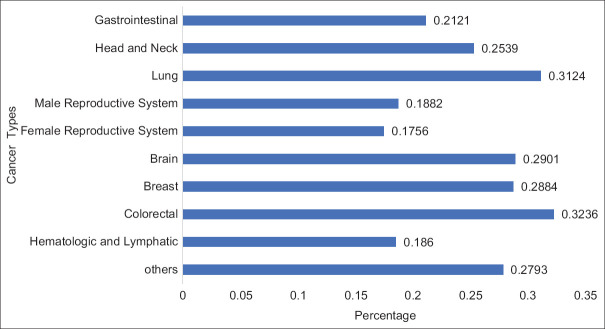
Titles and abstracts of the articles were reviewed by two reviewers working independently to screen the articles according to the inclusion and exclusion criteria explained below. In this screening, 286 articles were included for full-text review. After the full-text review, 183 of the articles were deemed to be eligible for inclusion in meta-analysis [Figure 1].
Figure 1.
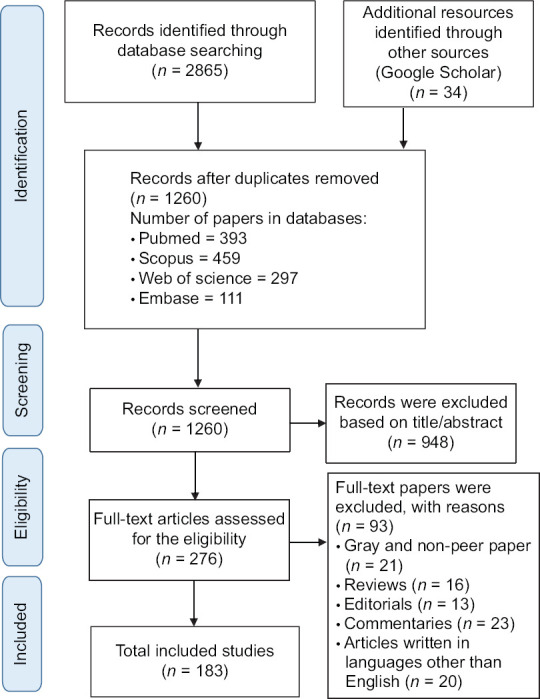
Flow diagram of the review process (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)
The inclusion criteria were as follows:
Published between January 2000 and April 2020
Published in English language
Having an observational study with a descriptive, prospective, cross-sectional, case study, or cohort research design
Providing a quantitative (numerical) report of the prevalence of depression in cancer patients and other types of data from which a report could be directly extracted.
The exclusion criteria were as follows:
Lacking a full text being a review, brief report, letter to the editor, expert opinion, editorial, book, a chapter of a book, commentary, case–control, case study, case series, thesis, or randomized controlled trial
Assessing therapies or drugs or their effects, follow-ups, and clinical decision-making as the main subject
Having invalid figures or tables.
Quality assessment of articles
The Newcastle–Ottawa Scale (NOS) was used to assess the quality of the articles. This quality assessment was carried out by two evaluators working independently to avoid bias. In cases where the two evaluators could not agree on the assessment of the quality of an article, the issue was discussed in the presence of a third evaluator until reaching a consensus. In the NOS-based quality assessment, the evaluator assesses the study in terms of eight criteria in three categories and awards a point for each category. The sum of these points, which range from 0 to 9, is an indicator of the risk of bias in the study. The assessment categories are as follows: (1) selection of study groups, for which 0–4 points can be awarded, (2) comparability of the groups, for which 0–2 points can be awarded, and (3) determination of exposure or outcomes, for which 0–3 points can be awarded. An article is said to be of good quality if it earns 3 or 4 points in the first category, 1 or 2 points in the second category, and 2 or 3 points in the third category. It is said to be of fair quality if it earns 2 points in the first category, 1 or 2 points in the second category, and 2 or 3 points in the third category, while it is said to be of poor quality if it earns 0 or 1 points in the first category, 0 points in the second category, and 0 or 1 points in the third category.[21]
Data extraction process
For organized data extraction from the articles, a data extraction form was designed by the researchers, with the following fields: authors’ name, publication date, study quality, place of study, type of cancers, prevalence of depression among cancer patients, the gender of depressed patients and nondepressed patients, and the type of depression.
Statistical analysis
The random-effects model (DerSimonian and Laird) was used to compute the means; the forest plot of the results at the 95% confidence interval (CI) was also drawn. The heterogeneity test (I2) and meta-regression analysis were carried out for sample size and publication date. A sensitivity analysis was performed to confirm the stability of the findings. The subgroup analysis was conducted by breaking down the data based on the type of cancer, the quality of the study, type of study, type of questionnaire, gender, date of publication, place of study, and sample size. The cumulative meta-analysis was performed with the sample size and date of publication, taken into account. The publication bias was measured by using Egger's test. The analyses were carried out in the R software.
RESULTS
The findings of the study are reported on the basis of Preferred Reporting Items for Systematic Reviews and Meta-Analyses.[22] The number of cancer patients in the 183 selected studies was 182,521, among whom, 49,280 patients, or about 27%, had depression (95% CI = 24%–30%) [Figure 2].
Figure 2.
Meta regression based on type of cancer
Meta-regression by type of cancer
Analyzing the data based on the type of cancer, we found out that depression was the most prevalent among patients with colorectal cancer with 32% (95% CI = 20%–47%), followed by patients with lung cancer with 31% (95% CI = 21%–43%). The lowest prevalence of depression was among female patients with cancers of the reproductive system with 17% (95% CI = 6%–38%) [Figure 2].
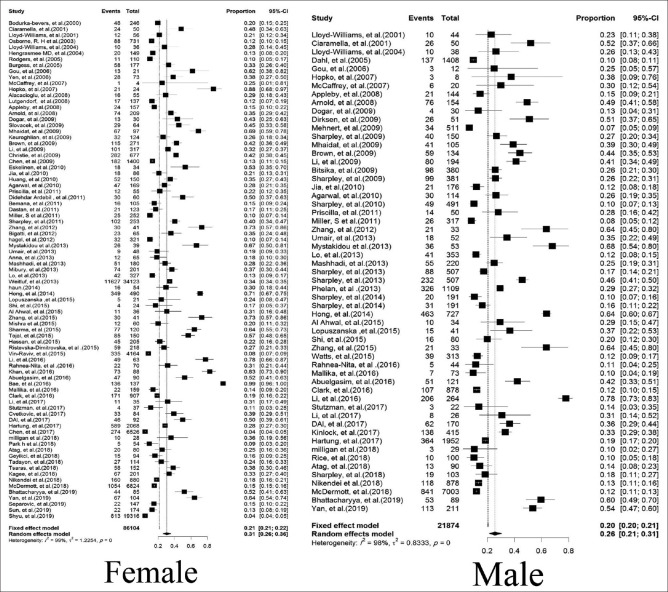
Meta-regression by gender
The results of meta-regression analysis by gender showed that depression was more prevalent among female cancer patients with 31% (95% CI = 26%–36%) than male cancer patients with 26% (95% CI = 21%–31%) [Figure 3].
Figure 3.
The forest plot of meta-regression based on gender
Meta-regression by World Health Organization regions
After breaking down the reports based on the WHO regions, it was found that depression was the most prevalent among cancer patients in the AFRO region with 35% (95% CI = 29%–43%), followed by the EMRO region with 34% (95% CI = 23%–46%), and the SEARO region with 34% (95% CI = 23%–46%). The lowest prevalence of depression among cancer patients was in the EURO and PAHO regions with 25% (95% CI = 20%–31%) [Table 1].
Table 1.
Meta-regression based on World Health Organization regions and continents
| Areas | Prevalence of depression | Lower | Upper | I-square (%) | P |
|---|---|---|---|---|---|
| WHO regions | |||||
| AFRO | 0.3582 | 0.2949 | 0.4268 | 99.40 | <0.001 |
| EMRO | 0.3426 | 0.2398 | 0.4628 | 99.10 | <0.001 |
| EURO | 0.2534 | 0.2018 | 0.3129 | 98.40 | <0.001 |
| PAHO | 0.2522 | 0.2029 | 0.3088 | 95.90 | <0.001 |
| SEARO | 0.341 | 0.238 | 0.4615 | 95.70 | <0.001 |
| WPRO | 0.2659 | 0.2116 | 0.3283 | 98.00 | <0.001 |
| Continents | |||||
| Europe | 0.2548 | 0.2015 | 0.3167 | 98.50 | <0.001 |
| Asia | 0.3077 | 0.256 | 0.3647 | 98.80 | <0.001 |
| America | 0.2522 | 0.2029 | 0.3088 | 99.40 | <0.001 |
| Australia | 0.1997 | 0.1424 | 0.2728 | 96.30 | <0.001 |
| Africa | 0.3582 | 0.2949 | 0.4268 | 98.00 | <0.001 |
WHO – World Health Organization; EMRO – Eastern Mediterranean; WPRO – Regional Office for the Western Pacific; SEARO – Regional Office for South-East Asia; AFRO – World Health Organization Regional Office for Africa; PAHO – Pan American Health Organization; EURO – European Region
Meta-regression by continents
The analysis carried out after analyzing the data by continent showed that depression is most prevalent among cancer patients in Africa with 36% (95% CI = 29%–43%) and least prevalent among cancer patients in Europe and North America with 25% (95% CI = 20%–31%) [Table 1].
Meta-regression by countries
After analyzing the data based on country, the results showed that depression was most prevalent among cancer patients in Pakistan with 43% (95% CI = 26%–64%) and then Italy with 39% (95% CI = 25%–57%). The lowest prevalence of depression among cancer patients was in Taiwan with 13% (95% CI = 4%–36%), and Germany with 14% (95% CI = 10%–19%) [Table 2].
Table 2.
Meta-regression based on Countries
| Sub group | Number studies | Prevalence | 95% CI (lower–upper) | I-square (%) |
|---|---|---|---|---|
| Countries | ||||
| Greece | 9 | 0.2664 | 0.1265-0.4765 | 96.70 |
| Japan | 4 | 0.1688 | 0.1045-0.2612 | 98.00 |
| Pakistan | 6 | 0.4397 | 0.2565-0.6409 | 95.10 |
| Canada | 6 | 0.2462 | 0.1474-0.3816 | 95.20 |
| USA | 40 | 0.2556 | 0.1994-0.3213 | 99.50 |
| United Kingdom | 11 | 0.158 | 0.0992-0.2421 | 97.40 |
| China | 14 | 0.3822 | 0.2739-0.5035 | 98.50 |
| Taiwan | 4 | 0.1356 | 0.0424-0.3574 | 99.60 |
| Korea | 5 | 0.3433 | 0.117-0.6735 | 99.50 |
| Australia | 12 | 0.1997 | 0.1424-0.2728 | 96.30 |
| India | 7 | 0.3682 | 0.2328-0.5281 | 96.20 |
| Iran | 7 | 0.2705 | 0.1718-0.3986 | 93.70 |
| Germany | 9 | 0.1417 | 0.104-0.1903 | 95.90 |
| Italy | 6 | 0.3981 | 0.246-0.5728 | 94.80 |
| Turkey | 7 | 0.3315 | 0.1792-0.5297 | 95.50 |
| Other | 36 | 0.3037 | 0.2411-0.3746 | 97.10 |
CI – Confidence interval
Meta-regression by year of publication
The results of meta-regression analysis by year of publication showed that the mean of prevalence reported in the articles published in each year was on average 0.6% higher than the corresponding figure in the previous year (slope = 0.006, z-value = 0.37, P = 0.70). Table 3 shows the 20-year trend of the prevalence of depression among cancer patients in 5-year intervals.
Table 3.
The 20-year trend of depression in cancer patients
| Sub group | Prevalence | 95% CI (lower–upper) | I-square |
|---|---|---|---|
| Year | |||
| 2015-2020 | 70 | 0.2561-0.3088 | 1.1845 |
| 2010-2014 | 55 | 0.3007-0.3585 | 0.9441 |
| 2005-2009 | 42 | 0.2953-0.3656 | 1.0478 |
| 2000-2004 | 16 | 0.1651-0.2367 | 0.7898 |
CI – Confidence interval
Meta-regression by type of questionnaires
The instruments used in the selected studies were as follows: PHQ-2, GDS, CES-D, BDI-II, HADS, SDS, HAM-D, DASS-21, and ICD-10. According to the results of meta-regression analysis, the prevalence of depression in cancer patients based on the type of questionnaires was 27% (95% CI = 24%–30%). Among these questionnaires, the highest depression prevalence was related to DASS-21 with 44% (95% CI = 27%–63%) and the lowest was related to ICD-10.9 with 10% (95% CI = 4%–23%) [Table 4].
Table 4.
Meta-regression based on questionnaires
| Type of questionnaires | Prevalence of depression | Lower | Upper | I-square (%) | P |
|---|---|---|---|---|---|
| PHQ-2 | 0.2456 | 0.1725 | 0.3371 | 98.60 | <0.001 |
| GDS | 0.3735 | 0.2403 | 0.5292 | 97.30 | <0.001 |
| CES-D | 0.3101 | 0.2422 | 0.3872 | 98.00 | <0.001 |
| BDI-II | 0.2893 | 0.213 | 0.3798 | 94.90 | <0.001 |
| HADS | 0.2413 | 0.1899 | 0.3014 | 98.90 | <0.001 |
| SDS | 0.3072 | 0.2314 | 0.3951 | 98.70 | <0.001 |
| HAM-D | 0.3695 | 0.3056 | 0.4382 | 96.50 | <0.001 |
| DASS-21 | 0.446 | 0.2725 | 0.6338 | 70.60 | <0.001 |
| ICD-10,9 | 0.1092 | 0.0456 | 0.2393 | 95.80 | <0.001 |
| Other | 0.2645 | 0.1839 | 0.3646 | 99.90 | <0.001 |
| Total | 0.2736 | 0.2458 | 0.3047 | 96.40 | <0.001 |
PHQ-9 – Patient Health Questionnaire-9; BDI-II – Beck depression inventoryor-II; CESD – Center for Epidemiologic Studies Depression Scale; GDS – Geriatric Depression Scale; DASS-21 – Depression, Anxiety, and Stress Scale-21; HAMD – Hamilton Depression Scale; HADS – Hospital anxiety and depression; SDS – Self-Rating Depression Scale; ICD – International Classification of Diseases
Publication bias
As shown in Figure 4, the results of Egger's regression test shows no insignificant publication bias in the studies included in the analysis (t-value = 1.18, df = 181, P = 0.23) [Figure 4].
Figure 4.
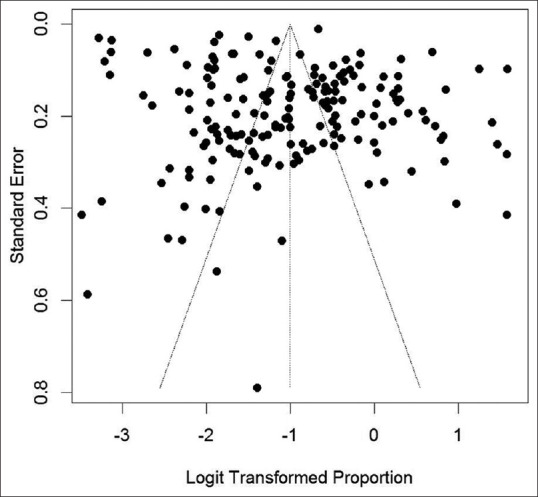
The funnel plot of publication bias
DISCUSSION
To the best of our knowledge, up to now, there has not been a meta-analysis to assess the prevalence of depression and the impact of various factors among cancer patients worldwide with a view to adopt appropriate measures to prevent and control depression in these patients, thereby reducing treatment costs and saving resources of healthcare systems. According to the results of this meta-analysis, the prevalence of depression among cancer patients was estimated at 27% (95% CI = 24%–30%). In a meta-analysis by Krebber et al., the prevalence was reported to be 14% (95% CI = 11%–16%), which is much lower than our estimate.[27] In a similar study, Mitchell et al. reported the prevalence of depression prevalence among patients who referred to nonpalliative care settings to be 16.3% (95% CI = 13%–20%), as estimated by face-to-face interviews with cancer patients according to the DSM-IV criteria.[28] Furthermore, in a systematic review conducted by Walker et al., the prevalence of depression in outpatients and inpatients was 5%–16% and 4%–14%, respectively; while the mentioned prevalence among mixed patients (both outpatients and inpatients) was estimated at 4%–11%. They also found that patients who referred to palliative care settings had the highest prevalence of depression (7%–49%).[29] Studies of the prevalence of depression in cancer patients referred for psychiatric consultation are one source of information about depression in cancer patients. Five studies which concentrated on cancer patients referred to psychiatric clinics reported the prevalence of major depression ranging from 9% to 58%.[30,31,32,33,34] Reviewing the existing literature reveals that although a considerable number of studies have been conducted in the area of depression among cancer patients, the prevalence of depression in different subgroups of patients is still ambiguous. To resolve the issue, we have done subgroup analysis to examine the prevalence of depression based on gender, type of cancer, WHO regions, continents, countries, and depression assessment instrument.
Analysis of the data by year of publication showed that the prevalence of depression among cancer patients has a growing trend, which is consistent with the report of Krebber et al.[27] The increasing prevalence might be due to the remarkable advancement of communication technologies, which has indeed affected public awareness of the disease, as well as making people sensitive to its potentially devastating consequences. In addition, the development of objective assessment criteria such as PHQ-2, GDS, CES-D, BDI-II, HADS, SDS, HAM-D, DASS-21, and ICD-10 helped discover and classify psychiatric disorders among cancer patients.[27] Regardless the cause of the issue, our findings can help clinicians, policymakers, and health authorities take immediate actions to prevent the increasing prevalence of depression among these patients.
Our findings also showed that depression is more prevalent among cancer patients in underdeveloped countries. For example, in a 2016 study of 695 cancer patients in Vietnam, the prevalence of depression was 58%,[35] and in a 2015 study of 77 cancer patients in Nepal, this prevalence was about 65%.[36] However, the prevalence reported in developed countries including Japan, Denmark, and the United Kingdom is lower than 10%.[37,38,39,40] These prevalence are also much lower than the mean prevalence obtained in the present study. We assume that the better quality of the healthcare system, the way the patients are treated, the treatment environment, and the effectiveness of the care services provided in developed countries might explain the low prevalence of depression among cancer patients in these countries. In a study conducted in Scotland, the prevalence of depression was shown to be higher in lower socioeconomic groups compared to the advantaged population.[41] Anxiety was also unevenly disseminated in cancer patients so that it suffered the least privileged population strata more significantly.[41] To effectively organize supportive psychiatric interventions in low- and middle-income countries, such differences should be addressed by health policymakers.
Our findings also revealed that depression is more prevalent among female cancer patients than males. Similarly, a study conducted among 4020 cancer patients in Germany reported much higher prevalence of depression among women compared to men.[42] These findings are also in line with another research conducted among 1217 Chinese people who affirmed higher prevalence among females.[43] In some cancer types, depression prevalence was approximately two to threefold greater in female patients.[44] In a review of 49 studies by Massie, no significant gender differences were reported in 23 articles; while four studies acknowledged an increased depression prevalence in female patients.[23] For example in a research by Lloyd et al., higher depression prevalence was reported for female patients with lymphoma;[45] or in a study by Pettingale et al. among patients with breast cancer, women were found to be more depressed than men.[46] However, it should be noted that a large number of studies in this area were done among female subjects or measured the prevalence of depression among patients with breast cancer, which consequently led to significantly higher depression prevalence in women rather than men. To prevent the bias, we analyzed men and women separately to obtain prevalence based on sample size; yet, the results still revealed higher prevalence of depression for women compared to the opposite gender.
Meta-regression analysis based on cancer type revealed that depression was the most prevalent among patients with colorectal cancer, followed by patients with lung cancer. However, the lowest prevalence of depression was among female patients with cancers of the reproductive system. In a meta-analysis by Krebber et al., the prevalence of depression was reported to be highest in patients with digestive tract cancer and those suffering from hematological malignancies.[27] Several studies affirmed the findings and mentioned patients with pancreatic, pulmonary, and breast cancer in the first category of patients with depression and other psychiatric disorders.[44,45,46,47,48,49] Lung cancer patients were also reported to have the highest incidence prevalence of depression in a Korean study. Among five cancer types reviewed in a study by Walker et al., the depression prevalence was highest in patients with lung cancer, followed by those affected by malignancies in women's reproductive system and breast cancer.[29] The high prevalence of depression in patients with colorectal and lung cancer can be due to the high mortality prevalence of these cancer types and consequent physical disabilities that put patients in troublesome condition.
Depression prevalence differed significantly based the depression diagnostic instrument applied so that the highest depression prevalence was related to DASS-21 and the lowest was reported for patients who were assessed by ICD-10.9. Similar studies confirmed this finding and mentioned higher depression prevalence in patients who filled out self-report questionnaires compared with those assessed by diagnostic tools. Such differences might be due to the fact that diagnostic clinical interviews based on the ICD use strict criteria for clinical depression, which makes them more suitable for identifying a depressive disorder.[27] Therefore, studies that applied self-report instruments might overestimate the prevalence of depression in cancer patients.
Limitations
There was a high level of heterogeneity in the results, because the selected articles included a large number of cross-sectional studies, some of which had used convenience sampling while others had used cluster sampling methods. Therefore, people interested in using the findings should take necessary precautions to account for these limitations. In addition, in the present study, we did not consider the diversities between depression prevalence of patients who are in different phases of treatment. Third, type of treatment and the relative side effects are among factors which were not mentioned in subgroup analyses due to lack of data in included studies. Forth, we merged the results of studies conducting among both patients attending outpatient clinics as well as inpatients who received palliative care in hospitals which might increase the heterogeneity of findings. Finally, grey literature and unpublished manuscripts were not included in our review.
CONCLUSION
In this systematic review and meta-analysis, studies of the past 20 years were examined to determine the global prevalence of depression in patients with different types of cancer. This is the first study to offer a comprehensive analysis of the prevalence of depression, with its different aspects, in cancer patients worldwide. The findings show higher prevalence of depression among cancer patients living in underdeveloped and developing countries than those in developed countries and the global average. This and the fact that the prevalence of depression in cancer patients seems to be on the rise should alarm the health policymakers, especially in underdeveloped and developing countries. This is indeed important because, if left unchecked, depression in cancer patients can lead to indifference toward treatment, poor commitment to lifelong therapies, and social rejection and its consequences, which will impose extra burdens on patients and their families as well as the healthcare system. The findings of this study can assist health policymakers in developing and implementing better care programs with necessary antidepression measures for cancer patients to limit the adverse effects of this issue on the affected people and the healthcare system.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rezaei S, Ahmadi S, Rahmati J, Hosseinifard H, Dehnad A, Aryankhesal A, et al. Global prevalence of depression in HIV/AIDS: A systematic review and meta-analysis. BMJ Support Palliat Care. 2019;9:404–12. doi: 10.1136/bmjspcare-2019-001952. [DOI] [PubMed] [Google Scholar]
- 2.Aryankhesal A, Ghashghaee A, Sardari E, Mahmoudi S, Alihosseini S, Dehnad A, et al. Prevalence of depression in patients with cancer in Iran: A systematic review and meta-analysis. BMJ Support Palliat Care 2019. doi: 10.1136/bmjspcare-2018-001724. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 3.Khue PM, Thom VT, Minh DQ, Quang LM, Hoa NL. Depression and anxiety as key factors associated with quality of life among lung cancer patients in Hai Phong, Vietnam. Front Psychiatry. 2019;10:352. doi: 10.3389/fpsyt.2019.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin CY, Cheng AS, Imani V, Saffari M, Ohayon MM, Pakpour AH. Advanced psychometric testing on a clinical screening tool to evaluate insomnia: Sleep condition indicator in patients with advanced cancer. Sleep Biol Rhythms. 2020;18:343–49. [Google Scholar]
- 5.Isfahani P, Arefy M, Shamsaii M. Prevalence of severe depression in iranian women with breast cancer: A meta-analysis. Depress Res Treat. 2020;2020:5871402. doi: 10.1155/2020/5871402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kouhestani M, Gharaei HA, Fararouei M, Hosienpour Ghahremanloo H, Ghaiasvand R. Global and regional geographical prevalence of depression in gastric cancer: A systematic review and meta-analysis. BMJ Support Palliat Care. 2020 doi: 10.1136/bmjspcare-2019-002050. [DOI] [PubMed] [Google Scholar]
- 7.Gan GG, Ng DL, Leong YC, Bee PC, Chin EF, Abdul Halim H, et al. Anxiety and depression in patients with haematological neoplasms in Malaysia. Med J Malaysia. 2019;74:191–7. [PubMed] [Google Scholar]
- 8.Sahadevan S, Namboodiri V. Depression in caregivers of patients with breast cancer: A cross-sectional study from a cancer research center in South India. Indian J Psychiatry. 2019;61:277–82. doi: 10.4103/psychiatry.IndianJPsychiatry_46_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritti-Dias RM, Cucato GG, de Matos LD, Cendoroglo MS, Nasri F, Wolosker N, et al. Depression and cancer were independently associated with quality of life in Brazilian older people. Australas J Ageing. 2019;38:E7–11. doi: 10.1111/ajag.12581. [DOI] [PubMed] [Google Scholar]
- 10.Abuelgasim KA, Ahmed GY, Alqahtani JA, Alayed AM, Alaskar AS, Malik MA. Depression and anxiety in patients with haematological malignancies, prevalence, and associated factors. Saudi Med J. 2016;37:877–81. doi: 10.15537/smj.2016.8.14597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bae H, Park H. Sexual function, depression, and quality of life in patients with cervical cancer. Support Care Cancer. 2016;24:1277–83. doi: 10.1007/s00520-015-2918-z. [DOI] [PubMed] [Google Scholar]
- 12.Cvetković J, Nenadović M. Depression in breast cancer patients. Psychiatry Res. 2016;240:343–7. doi: 10.1016/j.psychres.2016.04.048. [DOI] [PubMed] [Google Scholar]
- 13.Sudarisan SS, Abraham B, George C. Prevalence, correlates of depression, and its impact on quality of life of cancer patients attending a palliative care setting in South India. Psychooncology. 2019;28:1308–13. doi: 10.1002/pon.5083. [DOI] [PubMed] [Google Scholar]
- 14.Chang HA, Barreto N, Davtyan A, Beier E, Cangin MA, Salman J, et al. Depression predicts longitudinal declines in social support among women with newly diagnosed breast cancer. Psychooncology. 2019;28:635–42. doi: 10.1002/pon.5003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Villoria E, Lara L. Assessment of the hospital anxiety and depression scale for cancer patients. Rev Med Chil. 2018;146:300–7. doi: 10.4067/s0034-98872018000300300. [DOI] [PubMed] [Google Scholar]
- 16.Milligan F, Martinez F, Aal SH, Ahmed SA, Joby B, Matalam JS, et al. Assessing anxiety and depression in cancer patients. Br J Nurs. 2018;27:S18–23. doi: 10.12968/bjon.2018.27.10.S18. [DOI] [PubMed] [Google Scholar]
- 17.Morin RT, Midlarsky E. Depressive symptoms and cognitive functioning among older adults with cancer. Aging Ment Health. 2018;22:1465–70. doi: 10.1080/13607863.2017.1363868. [DOI] [PubMed] [Google Scholar]
- 18.Muneer H, Altaf F, Anwar W. Depression in cancer patients of Punjab. Pak J Med Health Sci. 2018;12:523–5. [Google Scholar]
- 19.Tamagawa R, Garland S, Vaska M, Carlson LE. Who benefits from psychosocial interventions in oncology? A systematic review of psychological moderators of treatment outcome. J Behav Med. 2012;35:658–73. doi: 10.1007/s10865-012-9398-0. [DOI] [PubMed] [Google Scholar]
- 20.Niedzwiedz CL, Knifton L, Robb KA, Katikireddi SV, Smith DJ. Depression and anxiety among people living with and beyond cancer: A growing clinical and research priority. BMC Cancer. 2019;19:943. doi: 10.1186/s12885-019-6181-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weitlauf JC, Jones S, Xu X, Finney JW, Moos RH, Sawaya GF, et al. Receipt of cervical cancer screening in female veterans: Impact of posttraumatic stress disorder and depression. Womens Health Issues. 2013;23:e153–9. doi: 10.1016/j.whi.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park B, Youn S, Yi KK, Lee SY, Lee JS, Chung S. The prevalence of depression among patients with the top ten most common cancers in South Korea. Psychiatry Investig. 2017;14:618–25. doi: 10.4306/pi.2017.14.5.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;32:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 24.Vodermaier A, Linden W, Siu C. Screening for emotional distress in cancer patients: A systematic review of assessment instruments. J Natl Cancer Inst. 2009;101:1464–88. doi: 10.1093/jnci/djp336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hotopf M, Chidgey J, Addington-Hall J, Ly KL. Depression in advanced disease: A systematic review Part 1. Prevalence and case finding. Palliat Med. 2002;16:81–97. doi: 10.1191/02169216302pm507oa. [DOI] [PubMed] [Google Scholar]
- 26.Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: A review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30:112–26. doi: 10.1016/j.genhosppsych.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 27.Krebber AM, Buffart LM, Kleijn G, Riepma IC, de Bree R, Leemans CR, et al. Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psychooncology. 2014;23:121–30. doi: 10.1002/pon.3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–74. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 29.Walker J, Hansen CH, Martin P, Symeonides S, Ramessur R, Murray G, et al. Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: A cross-sectional analysis of routinely collected clinical data. Lancet Psychiatry. 2014;1:343–50. doi: 10.1016/S2215-0366(14)70313-X. [DOI] [PubMed] [Google Scholar]
- 30.Hinton JM. The psychiatry of terminal illness in adults and children. Proc R Soc Med. 1972;65:1035–40. [PMC free article] [PubMed] [Google Scholar]
- 31.Levine PM, Silberfarb PM, Lipowski ZJ. Mental disorders in cancer patients. Cancer. 1978;42:1385–91. doi: 10.1002/1097-0142(197809)42:3<1385::aid-cncr2820420349>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 32.Massie MJ, Gorzynski JG, Mastrovito R, Theis D, Holland JC. Proceedings of the AARC and the American Society of Clinical Oncology. The diagnosis of depression in hospitalized patients with cancer. Proc Am Soc Clin Oncol. 1979;20:432. [Google Scholar]
- 33.Massie MJ, Holland JC. Consultation and liaison issues in cancer care. Psychiatr Med. 1987;5:343–59. [PubMed] [Google Scholar]
- 34.Razavi D, Delvaux N, Farvacques C, Robaye E. Screening for adjustment disorders and major depressive disorders in cancer in-patients. Br J Psychiatry. 1990;156:79–83. doi: 10.1192/bjp.156.1.79. [DOI] [PubMed] [Google Scholar]
- 35.Yen NT, Weiss B, Trung LT. Caseness prevalences and risk factors for depression among Vietnamese cancer patients. Asian J Psychiatry. 2016;23:95–8. doi: 10.1016/j.ajp.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharma A, Zhang JP. Depression and its predictors among breast cancer patients in Nepal. ASEAN J Psychiatr. 2015;16:106–15. [Google Scholar]
- 37.Grov EK, Dahl AA, Moum T, Fosså SD. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol. 2005;16:1185–91. doi: 10.1093/annonc/mdi210. [DOI] [PubMed] [Google Scholar]
- 38.Hadi N, Asadollahi R, Talei AR. Anxiety, depression and anger in breast cancer patients compared with the general population in Shiraz, Southern Iran. Iran Red Crescent Med J. 2009;11:312–7. [Google Scholar]
- 39.Haun MW, Sklenarova H, Villalobos M, Thomas M, Brechtel A, Löwe B, et al. Depression, anxiety and disease-related distress in couples affected by advanced lung cancer. Lung cancer (Amsterdam, Netherlands) 2014;86:274–80. doi: 10.1016/j.lungcan.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 40.Hartung TJ, Brähler E, Faller H, Härter M, Hinz A, Johansen C, et al. The risk of being depressed is significantly higher in cancer patients than in the general population: Prevalence and severity of depressive symptoms across major cancer types. Eur J Cancer. 2017;72:46–53. doi: 10.1016/j.ejca.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 41.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multi-morbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 42.Hengrasmee P, Padungsutt P, Boriboonhirunsarn D. Depression among gynecologic cancer patients at Siriraj Hospital: Prevalence and associated factors. J Med Assoc Thai. 2004;87(Suppl 3):S74–9. [PubMed] [Google Scholar]
- 43.Hong JS, Tian J. Prevalence of anxiety and depression and their risk factors in Chinese cancer patients. Support Care Cancer. 2014;22:453–9. doi: 10.1007/s00520-013-1997-y. [DOI] [PubMed] [Google Scholar]
- 44.Smith HR. Depression in cancer patients: Pathogenesis, implications and treatment (Review) Oncol Lett. 2015;9:1509–14. doi: 10.3892/ol.2015.2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lloyd GG, Parker AC, Ludlam CA, McGuire RJ. Emotional impact of diagnosis and early treatment of lymphomas. J Psychosom Res. 1984;28:157–62. doi: 10.1016/0022-3999(84)90009-6. [DOI] [PubMed] [Google Scholar]
- 46.Pettingale KW, Burgess C, Greer S. Psychological response to cancer diagnosis – I. Correlations with prognostic variables. J Psychosom Res. 1988;32:255–61. doi: 10.1016/0022-3999(88)90066-9. [DOI] [PubMed] [Google Scholar]
- 47.Park B, Youn S, Yi KY, Lee S, Lee JS, Chung S. The prevalence of depression among patients with the top ten most common cancers in South Korea. Psychiatry Investig. 2017;14:618–25. doi: 10.4306/pi.2017.14.5.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carlson LE, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L, et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90:2297–304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]