Abstract
In a defined geographic area in rural India (1,60,000 population), osteoporosis detection and calcium and vitamin D supplementation program was instituted. Of the eligible 15,386 subjects, 5,992 (38%) participated in the program; 2,882 (48%) had osteopenia and osteoporosis; supervised calcium and vitamin D supplementation was instituted; 2,113 (73.3% of those identified) completed 2 years of supplementation. The mean duration of the follow-up was 5 years (range 2–8 years). On follow-up, three groups emerged; those who were regular, those who were irregular, and those who did not take supplements. In those who were regular with calcium and vitamin D supplementation, we found a significant reduction in fractures (RR 0.27, 95% CI 0.09–0.81) compared with those who did not take supplements. There was no significant difference in falls between the three groups. Mortality was significantly lower (RR 0.53, 95% CI 0.31–0.91) in those who were regular with calcium and vitamin D supplements compared to those who did not take supplements. While the reduction in fractures was probably due to calcium and vitamin D supplementation, the reduction in mortality was probably because those who took regular supplements accessed healthcare services more readily for other comorbidities as part of their follow-up program.
Keywords: Calcium and vitamin D supplementation, fractures, osteoporosis, rural health
INTRODUCTION
Osteoporosis, a silent disease, a common problem in postmenopausal women 5 years or more after menopause and in men over age 60, occurs at a younger age in Indians than in the West.[1,2] In systematic studies in cluster samples, the prevalence of osteoporosis, in a semiurban and rural population in southern India, was 50% for women and 30% for men.[1,2,3] A similarly high prevalence has been reported from other parts of the country.[4,5,6] Mithal et al.,[7] in their Asian Pacific regional audit, highlighted the costs and burden of osteoporosis in India. Thulkar and Singh, in an overview of research studies on osteoporosis in India,[8] point out the lack of community-level reporting on the treatment and outcomes.
In compliant subjects, calcium and vitamin D supplements have the potential to reduce fractures by about 18–25% in vulnerable subjects, if both nutrients are supplemented and if vitamin D intake is more than 700 IU per day.[9,10,11,12] The high prevalence of calcium and vitamin D deficiency in Indian postmenopausal women and older men,[1,2] their importance as risk factors in Indian women with hip fracture,[13] the high mortality reported after hip fracture in Indian women,[13] and the apparent protective efficacy of calcium and vitamin D in preventing osteoporotic fractures[9,10,11,12] point to an urgent need to implement calcium and vitamin D supplementation programs in Indian postmenopausal women and older Indian men. We describe a simple community-level model for addressing this need and report the relevant long-term follow-up outcomes on the subjects in our supplementation program in this manuscript.
METHODS
Structure of the organization
The 50-year-old charitable non-governmental organization (NGO), located in a rural/semiurban area in southern India, is involved with primary health care in a defined geographic area, with a population of 1,60,000 in 35,000 families in 315 hamlets and villages around the hospital. Addressing non-communicable diseases (NCD) is the thrust area. The NGO and the secondary-level hospital started functioning in 2010 in an integrated manner. The area covered is divided into seven regions for administrative convenience. The basic care providers at the community level are family care volunteers (FCVs, 1 for approximately 50 households) drawn from each hamlet, and two to four multipurpose health workers (MPWs) for each area; each in charge of approximately 500 households.
Awareness programs
The community-level osteoporosis program was popularized through awareness programs conducted by our health workers and school children, utilizing small skits and street plays before commencement. These skits and street plays were devised by school teachers under the guidance of a team of doctors in the hospital. The content of these awareness programs was reviewed in a demonstration to an audience of doctors and nurses, suitably modified for accuracy of facts presented; the language was simplified for easy understanding and then taken to the community. The program was initiated and conducted in the secondary-level hospital and field-level follow-up was through FCVs and MPWs.
Subjects studied
The community-dwelling ambulatory adults—women above age 50, postmenopausal for 5 years, and men above age 55 were the intended target population for the program.
Study commencement and closing dates
The osteoporosis screening program followed by calcium and vitamin D supplementation for those identified to have osteoporosis was initiated on 01-04-2012. As it takes at least 12 months time for calcium and vitamin D supplements to have an impact on fractures,[11] only those subjects who have completed at least 2 years of follow-up by 31-03-2020 are included for analysis in this manuscript. By 01-06-2020, all the data from the patients who completed at least 2 years of supplementation up to 31-03-2020 had been collected for analysis.
Evaluation of subjects at baseline
The eligible subjects attended the hospital in batches of 10–15 per day (free transportation was provided). Each subject, at the first visit, had a clinical evaluation including height, weight, body mass index (BMI), blood pressure; details of comorbidities such as diabetes hypertension, and heart disease were documented. Each subject underwent a dual-energy X-ray absorptiometry (DEXA) scan of the lumbar spine and hip.
Dual-Energy X-Ray Absorptiometry
DEXA scans were performed free of cost, using the Hologic DEXA scanner (QDR 4500 Model: ASY-00409, Hologic Inc, 35 Crosby Drive, Bedford, MA 01730, USA), using the Asian database from Hologic for defining osteopenia (T-score − 1.5 to − 2.5) and osteoporosis (T-score < −2.5). Calibration of the scanner was performed daily using the lumbar spine and hip phantoms. The coefficient of variation (CV) for measurement was <1% throughout the study period. The subjects with T-score <−3, at higher risk for osteoporotic fracture, were considered to have osteoporosis severe enough to warrant bisphosphonate therapy.
Interventions
Calcium and Vitamin D supplementation: The subjects with osteoporosis and osteopenia were counseled about calcium and vitamin D supplementation and fall prevention. They were advised to take a single tablet of calcium carbonate (500 mg elemental calcium) with 250 units of vitamin D3 daily. To ensure the adequacy of and compliance with vitamin D supplementation, we offered 6,00,000 IU of intramuscular vitamin D3 annually to each patient (the average daily dose of vitamin D works out to approximately 2,000 IU). Each participant was given a card with the date of vitamin D injection (the information was also captured in their medical record), and was advised against any other calcium or vitamin D supplement.
Bisphosphonate: The subjects with osteoporosis (T-score <−3 at either site, n = 177), severe enough to warrant bisphosphonate therapy, were advised three annual injections of IV zoledronic acid after correcting calcium and vitamin D deficiency (148 have had the first dose, others had contra-indications or declined zoledronic acid).
Subjects who were excluded
Subjects (n = 592, M: 162, F: 430), who had not completed 2 years of calcium and vitamin D supplementation were excluded from the analysis. For the present study, which focuses only on calcium and vitamin D supplementation, the subjects (n = 177, M: 77, F: 100) who required bisphosphonates were also excluded from the final analysis.
Follow-up at the field level: All the subjects were followed-up at the community level by our FCVs and MPWs. At the field level, the health workers visited these subjects once in 2-3 months to assess and reinforce compliance. The participants were encouraged to seek medical help from the hospital for any health-related problems. Compliance with calcium and vitamin D supplementation was assessed by tablet count by our FCVs. The patients were categorized as (1) Group 1: taking regular supplements (>75% of the time), (2) Group 2: irregular supplements (30–74% of the time), and (3) Group 3: no supplements (<30% of the time). Information was collected prospectively about the falls, fractures, and mortality. The site of the fracture, as informed by the subjects who sustained a fracture, was noted. Information on falls, fractures, and mortality in all the participants was updated monthly as part of our ongoing community-level information reporting and at the Program Evaluation and Monitoring Committee (PEMC) meetings conducted once in 3 months. The cause of death was ascertained by a verbal autopsy.
The subjects with normal bone density at screening were advised annual follow-up at the hospital and to access health care when needed but were not visited by our health workers on a regular basis. However, information on mortality for this group of subjects, collected as part of our overall community project, is available to us.
Quality of life assessment
The International Osteoporosis Federation Quality of Life (QOL) questionnaire,[14] modified for the sociocultural context, was used to assess QOL in a subset of 120 subjects on regular supplements (group 1) and 120 subjects not on supplements (group 3). The accuracy of the questionnaire was confirmed by back-translation of the local language version to English. The maximum possible score was 169. The field staff, trained by one of the investigators (P), administered the questionnaire to the participants in the QOL study at the field level.
IRB approval
Approval from the Institutional Review Board was obtained for the QOL study (which required the collection of personal information from the subjects) and each subject gave written informed consent. The supplementation program is in line with the current management practices of osteoporosis and the collection of data for outcomes was part of our routine program implementation and monitoring in the community.
Sample size calculation
A 20% difference in the QOL scores was considered to be a clinically meaningful difference. In order to detect this difference with an alpha of 0.05 and power of 80%, the sample size required for the QOL study was 110 in each arm. We included 120 subjects in each arm for this sub-study.
Statistical methods
Statistical calculations were performed using Statistical software for Social Sciences[15] accessed online on 9-5-2020 (https://www.socscistatistics.com/) Chi-square was used to compare the proportions and the Student's t-test was used to compare the continuous variables which are normally distributed. The relative risk and 95% confidence intervals were also calculated.
The protocol
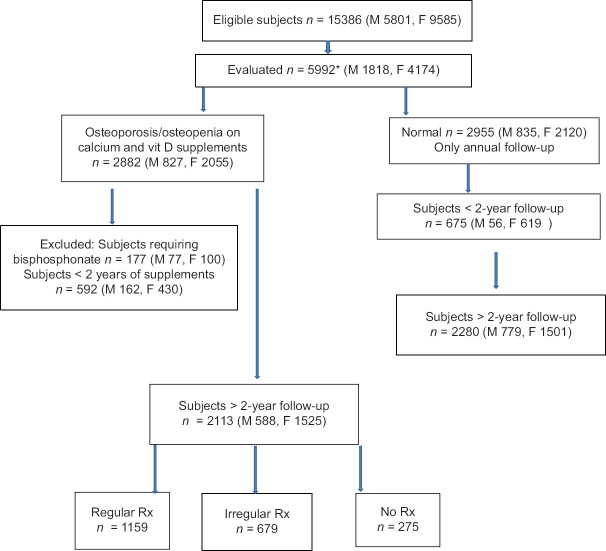
The protocol for evaluation and supplementation is presented in the form of a Consort diagram [Figure 1].
Figure 1.
Consort diagram of the study. *155 subjects moved out of study area after the initial evaluation. Available subjects 5992-155 = 5837
RESULTS
The subjects fell into three groups (a) those who were regular with supplements, (b) those who were irregular with supplements, and (c) those who did not take supplements. They were followed-up for a mean duration of 5 years (range 2–8 years). The information on falls, fractures, and deaths was prospectively collected and documented in the three groups through our network of community-level FCVs and MPWs.
The details of the eligible numbers, proportion evaluated, those excluded from the analysis, those lost to follow-up—are all provided in Figure 1. Briefly, a total of 5,837 subjects (37.9%) out of the 15,386 eligible subjects enrolled in the program up to 31-03-2020. Overall, women outnumbered men [Table 1]. Of those enrolled, there were 2,882 (48.1%) subjects with osteoporosis or osteopenia who were started on calcium and vitamin D supplementation; 177 subjects who required bisphosphonate therapy and 592 who had not completed 2 years of supplementation by 31-03-2020 were excluded.
Table 1.
Demographic details
| Population | No. (%) | Males (%) | Females (%) | Mean age (SD) | M:F ratio |
|---|---|---|---|---|---|
| Total eligible M >55, F >50, 5 years after menopause | 15386 | 5801 (37.7) | 9585 (62.3) | 69.49 (7.34) | 1:1.65 |
| Evaluated | 5992# (38.94) | 1818 (30.3) | 4174 (69.7) | 58.15 (6.38) | 1:1.29 |
| Normal | 2955 | 835 | 2120 | 58.53 (6.67) | |
| Osteoporosis+osteopenia in those evaluated | 2882 (48.10) | 827 (28.7) | 2055 (71.3) | 1:2.49 | |
| T-score < −3 | 177@ | 77 | 100 | ||
| < 2 years in study | 592@ | 162 | 430 | ||
| >2 years in study | |||||
| Osteoporosis and osteopenia (BMI) | 2113* (24±3.2) | 588 (27.8) | 1525 (72.2) | 1:2.59 | |
| Normal BMD N (BMI)* | 2280 * (27±2.6) | 779 (34.2) | 1501 (65.8) |
*The subjects with normal initial DEXA scans had significantly higher BMI (P<0.02) than those with osteoporosis or osteopenia. @These subjects from the group with osteoporosis or osteopenia were excluded from the analysis. #155 subjects moved out of the study area within 6 months of baseline evaluation.
Of the 2,882 subjects in the calcium and vitamin D supplementation group, 2,113 (73.32%) have completed >2 years of D supplementation. Of the 2,955 subjects with normal baseline DEXA scans, 2,280 subjects (77.1%) have been followed-up for more than 2 years. There was no significant difference in age or sex ratio between those who had osteoporosis or osteopenia and those with normal DEXA scans [Table 1].
The demographic profile of those who completed more than 2 years of supplementation is presented in Table 2. A significantly greater proportion of women were regular with the supplements (P = 0.025) but there was no difference between the three groups in terms of age. Comorbidities such as diabetes (11,10.5, and 11.4%), hypertension (12, 11.4, and 11.7%), and known heart disease (4, 3.8, and 4.1%) were similar between the three groups of subjects. Of those in the calcium and vitamin D supplementation study, the proportion of the subjects with osteopenia (68.4, 70.2, and 69.6%) did not differ between the three groups.
Table 2.
Baseline characteristics: subjects >2 years on calcium and vitamin D
| Normal baseline BMD | Osteoporosis, Osteopenia | No treatment | Total | Significance | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Regular | Irregular | |||||
| Male | 638 | 297 | 214 | 77 | 588 | |
| Female | 1642 | 862 | 465 | 198 | 1525 | |
| Total no. | 2280 | 1159 | 679 | 275 | 2113 | |
| Age (M+SD) | 57.8 (6.02) | 57.78 (6.11) | 57.67 (5.94) | 58.25 (5.89) | NS | |
| M: F ratio | 1:2.59 | 1:2.90* | 1:2.17 | 1:2.57 | *P=0.025 | |
NS: Not significant. Mean age in the different groups did not differ. *In the regular treatment group, a significantly greater proportion were women
Those with normal BMD at baseline had a higher BMI (27+2.6, m ± SD) than those who had abnormal BMD (24 ± 3.2, P < 0.02) Table 1.
The details of the fractures, falls, and mortality in the subjects with osteoporosis or osteopenia are presented in Table 3. The subjects in the regular supplementation group had significantly fewer fractures (Chi-square 8.4, P = 0.015, RR 0.27, 95% CI 0.09 – 0.81) than in those not on supplements. However, there was no significant difference in the falls between the three groups. It is of interest that the majority of fractures in our subjects occurred in the wrists and forearms [Table 4]. Only two femoral fractures occurred, both in the no supplement group and one of them succumbed a month after the fracture.
Table 3.
Fractures, falls, and mortality in the three groups
| Group | Fracture (%) | No fracture | Chi-square (P) | Relative risk (95% CI) |
|---|---|---|---|---|
| Regular Rx | 7 (0.6) * | *8.41 (0.015) | 0.27 (0.09-0.81) | |
| Irregular Rx | 13 (1.91) | 669 | ||
| No Rx | 6 (2.18) | 266 | ||
|
| ||||
| Group | Falls (%) | No Falls | ||
|
| ||||
| Regular Rx | 53 (4.57) ** | 1106 | **NS | 0.69 (0.41-1.16) |
| Irregular Rx | 32 (4.69) | 650 | ||
| No Rx | 18 (6.61) | 254 | ||
|
| ||||
| Group | Dead (%) | Alive | ||
|
| ||||
| Regular Rx | 41 (3.53%) *** | 1118 | ***5.29 (0.02) | 0.53 (0.31-0.91) |
| Irregular Rx | 30 (4.40%) | 652 | ||
| No Rx* | 18 (6.61%) | 254 | ||
*Fractures were significantly few in those on regular supplements. **NS No significant difference in falls between the three groups. ***Mortality was significantly lower in the regular supplement group.
Table 4.
Site of fracture in the three groups
| Fracture site | Regular treatment | Irregular treatment | No treatment |
|---|---|---|---|
| Wrist | 4 | 5 | 2 |
| Forearm | 0 | 2 | 1 |
| Ankle | 1 | 2 | 0 |
| Tibia | 2 | 4 | 1 |
| Femur | 0 | 0 | 2 |
Those subjects on regular calcium and vitamin D supplements had significantly lower mortality than those in group 3 (Table 3, Chi-square 5.3, P = 0.02, RR 0.52, 95% CI 0.31–0.91). The cause of death did not differ significantly in the three groups (data not shown).
The QOL score of 90.6 (±18.9, mean ± SD) in the regular supplement group did not differ significantly from that observed in the no supplement group, 90.20 (±15.3, mean ± SD).
On follow-up, subjects in the calcium and vitamin D supplementation group had significantly lower mortality [Table 5] than those with normal baseline BMD (Chi-square 10.8, P = 0.001, RR 0.65, 95% CI 0.50–0.84). This was a surprise.
Table 5.
Mortality comparison between those on regular follow-up in the calcium and vitamin D supplementation program and those who had normal baseline DEXA (not on regular follow-up)
| Dead | Alive | Chi-square (P) | Relative risk (95% CI) | |
|---|---|---|---|---|
| Abnormal BMD group | 89 (4.21%) | 2024 | ||
| Normal BMD group | 147 (6.45%) | 2133 | 10.78 (P=0.001) | 0.65 (0.50-0.84) |
DISCUSSION
While many Indian studies have reported on the prevalence and risk factors for osteoporosis and related fractures,[1,2,3,4,5,6] ours is the first large-scale Indian study to report a reduced number of fractures and reduced mortality with community-level calcium and vitamin D supplementation. The widespread poor dietary calcium intake and vitamin D deficiency reported from different regions of India[16] underscores the need for such supplementation. In fact, postmenopausal women in India, who tend to have very poor sun exposure and poor dietary calcium intake,[13] resemble institutionalized Western counterparts with calcium and vitamin D deficiency. The significant decrease in fractures and all-cause mortality noted by us attest to the benefits of this program. The fracture benefits accrue only if the subjects are >75% compliant with calcium and vitamin D supplements, a fact commented on in the earlier studies.[17] (This was the basis for our defining the regular treatment group.) The value of additional calcium and vitamin D supplements in preventing fractures is evident even in postmenopausal women on estrogen therapy with or without progesterone.[18]
There is a confusing body of literature about the benefits of calcium and vitamin D supplementation for postmenopausal women and older men because the dose, frequency, route of administration of vitamin D, and the age at commencement of the supplements have varied in different studies and the skeletal benefits depend on a number of these variables.[9,10] While some studies used vitamin D alone, most used calcium and vitamin D together. Vitamin D supplementation alone is inadequate and additional calcium is required to prevent fractures.[10,11] We used a standard supplement—500 mg of elemental calcium as a single tablet once daily, a dose similar to those used in most studies (500–1000 mg of elemental calcium per day). While these supplements are likely to be beneficial in the subjects deficient in these nutrients, a meta-analysis from the West where vitamin D fortification of food is prevalent and where dietary calcium intake is adequate, finds no benefit from additional supplements.[19,20]
In general, there is agreement that a daily dose of vitamin D of 600–800 units is required to decrease fracture rates.[10] In subjects whose baseline vitamin D levels are >20/mL, additional vitamin D to increase the levels to 30 ng/mL is not beneficial.[21] In fact, doses in excess of 4,000 IU per day may actually cause a reduction in the volumetric bone density at distal radius and tibia and are better avoided.[22]
Hip fracture prevention with calcium and vitamin D is evident only in the supplement-naive subjects who were more than 75% compliant in the large Women's Health Initiative study[17,18]—an observation that is corroborated by meta-analysis.[10] In our program, group 1 subjects with >75% compliance with calcium and vitamin D supplements were the ones in whom we observed significant fracture prevention.
None of our subjects were on calcium or vitamin D supplements earlier and judging by the reported high prevalence of calcium and vitamin D deficiency in India,[16] were probably deficient in both nutrients. We administered vitamin D3 as a single parenteral dose of 6,00,000 units once a year (total daily vitamin D dose ~2,000 IU including the 250 units present in the calcium supplement), because this was the most practical way to ensure compliance. There is no consensus on the amount of vitamin D supplement required nor the route of administration. The previous studies[13,23] attest to the advantages of this approach, as such doses were better able to sustain normal (>20 ng/mL) serum levels of 25(OH) vitamin D. A comparison of three different protocols of vitamin D administration in vitamin D-deficient Indian women[24] concluded that the most effective regimen was the one that employed a high parenteral dose at the beginning followed by oral doses. In the WHI (Womens’ Health Initiative) study, the majority of subjects were already on calcium and vitamin D supplements and additional supplements did not protect against fractures.[25]
Whether high annual doses of vitamin D are associated with frequent falls in the recipients is controversial. While one controlled clinical trial in subjects aged 70 or above, with annual high-dose vitamin D[26] reported increased falls and fractures, a meta-analysis of vitamin D supplementation and falls in the elderly[27] (mean age 76), showed a significant decrease in the falls particularly in vitamin D-deficient subjects, when calcium was coadministered with vitamin D. Our subjects on regular supplements were much younger with a mean age of 58; we observe no difference in the falls but a significant reduction in fractures.
In our subjects, the commonest fractures noted were wrist and forearm fractures, fractures of the femur were rare (only two femur fractures in group 3 subjects, not on regular supplements). This preponderance of wrist and forearm fractures in our program is probably due to our subjects stalling their fall by an outstretched hand. A previous study on high-dose annual vitamin D supplements showed a preferential reduction in the upper extremity fractures.[12]
We did not study incident vertebral fractures but the cross-sectional Delhi vertebral fracture study[28] (DEVOS) identified vertebral fractures in a substantial proportion of Indian men and women in the vulnerable age group. The average daily elemental calcium dose of 500 mg and vitamin D dose of 2,000 IU in our subjects would be sufficient for preventing vertebral fractures also.
The association between calcium and vitamin D supplementation and cardiovascular events or cancer in postmenopausal women and elderly men is controversial.[29] In the WHI study, even though the overall results showed no increase in the cardiovascular events, a post hoc subgroup analysis showed a small but significant risk of increased cardiovascular events, but mortality was similar in the two arms.[30,31,32] The sum of evidence suggests that supplements of 500 mg of elemental calcium and up to 2,000 IU vitamin D per day is cardiovascular and cancer[33] neutral. For subjects aged >75, with pre-existing, age-related increased cardiovascular risk, cardiovascular risk assessment by risk scores such as QRISK (Cardiovascular risk assessment score) score may be prudent before instituting community-level supplementation program.
In our program, there was a not only a significant decrease in fractures but also a significant decrease in mortality in those who took regular calcium and vitamin D supplements, compared to those who did not take supplements.
While the decrease in fractures can be attributed to the supplements, the mortality reduction is probably multifactorial; frequent visits by our health workers facilitated easy access to health care for other comorbid conditions and this probably contributed to a reduced mortality. Our community-level model can complement other efforts to prevent fractures such as the Fracture Liaison Service initiated in Mumbai and Chandigarh.[34]
The overall lower mortality in the subjects with osteoporosis/osteopenia in our program, compared to those with normal baseline BMD was probably due to the systematic follow-up efforts at the community level, overall better health awareness, and better health care utilization for all comorbid conditions by the subjects in our supplementation program.
In conclusion, a simple community-level osteoporosis screening and calcium -vitamin D supplementation program in rural India prevented fractures without increasing falls. The poor participation (38%) of the eligible population underscores the need for more community osteoporosis awareness programs.
The lack of the difference in the QOL scores between those on regular supplements and those who were not on supplements highlights the silent nature of osteoporosis—a major reason why people are reluctant to participate and are irregular with supplements. The subjects need to be educated that even in the absence of symptomatic improvement, they will benefit in terms of reduced fractures.
Ours is an observational study, not a prospective randomized-controlled clinical trial (it may be unethical to perform a placebo-controlled study on this topic). We describe long-term favorable outcomes of a calcium and vitamin D supplementation program in subjects with osteopenia and osteoporosis in the community setting. The strength of our study are the large numbers, hard clinical outcomes that were counted, and the completeness, regularity, and long duration of follow-up.
Calcium and vitamin D supplementation is inexpensive and compliance with vitamin D is ensured when it is given as an annual IM (Intramuscular) injection. Such a program is easy to implement and replicable in similar low-resource rural and semiurban settings. If cost constraints preclude the use of DEXA scans, the fracture risk assessment score (FRAX) without DEXA can be used to identify the subjects with high fracture risk for supplementation.
Our observation that subjects in a health promotion program, such as our osteoporosis program, frequently visited by health care workers who enable easy access to health education and health care, have a significant survival benefit [Table 5], has major implications for public health programs in rural India.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Supported by Thirumalai Charity Trust.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
FCVs and MPWs of TCT for field work.
Dr J Richard PhD, Consultant, Biostatistics and Research Methods, Former Professor and Head, Department of Biostatistics, Christian Medical College, Vellore for statistical assistance.
Dr. Mathangi for help with evaluating and counseling patients.
Mrs Bhooma Parthasarathy, Director, Thirumalai Charity Trust for support and encouragement.
Presented as part of an oration in TRENDO 2020.
REFERENCES
- 1.Paul TV, Thomas N, Seshadri MS, Oommen R, Jose A, Mahendri NV. Prevalence of osteoporosis in ambulatory postmenopausal women from a semiurban region in Southern India: Relationship to calcium nutrition and vitamin D status. Endocr Pract. 2008;14:665–71. doi: 10.4158/EP.14.6.665. [DOI] [PubMed] [Google Scholar]
- 2.Shetty S, Kapoor N, Naik D, Asha HS, Prabu S, Thomas N, et al. Osteoporosis in healthy South Indian males and the influence of life style factors and vitamin D status on bone mineral density. J Osteoporosis. 2014 doi: 10.1155/2014/723238. doi: 10.1155/2014/723238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binu AJ, Cherian KE, Kapoor N, Jebasingh FK, Asha HS, Paul TV. Bone health after fifth decade in rural ambulatory South Indian postmenopausal women. Indian J Community Med. 2019;44:205–8. doi: 10.4103/ijcm.IJCM_161_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kadam NS, Chiplonkar SA, Khadilkar AV, Khadilkar VV. Prevalence of osteoporosis in apparently healthy adults above 40 years of age in Pune City, India. Indian J Endocrinol Metab. 2018;22:67–73. doi: 10.4103/ijem.IJEM_438_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaushal N, Vohora D, Jalali RK, Jha S. Prevalence of osteoporosis and osteopenia in an apparently healthy Indian population-A cross-sectional retrospective study. Osteoporos Sarcopenia. 2018;4:53–60. doi: 10.1016/j.afos.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khadilkar AV, Mandlik RM. Epidemiology and treatment of osteoporosis in women: An Indian perspective. Int J Womens Health. 2015;7:841–50. doi: 10.2147/IJWH.S54623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mithal A, Bansal B, Kyer CS, Ebeling P. The Asia-Pacific regional audit-epidemiology, costs, and burden of osteoporosis in India 2013: A report of International Osteoporosis Foundation. Indian J Endocrinol Metab. 2014;18:449–54. doi: 10.4103/2230-8210.137485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thulkar J, Singh S. Overview of research studies on osteoporosis in menopausal women since the last decade. J Midlife Health. 2015;6:104–7. doi: 10.4103/0976-7800.165589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: A meta-analysis of randomized controlled trials. JAMA. 2005;293:2257–64. doi: 10.1001/jama.293.18.2257. [DOI] [PubMed] [Google Scholar]
- 10.Boonen S, Lips P, Bouillon R, Bischoff-Ferrari HA, Vanderschueren D, Haentjens P. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: Evidence from a comparative metaanalysis of randomized controlled trials. J Clin Endocrinol Metab. 2007;92:1415–23. doi: 10.1210/jc.2006-1404. [DOI] [PubMed] [Google Scholar]
- 11.The DIPART (vitamin D Individual Patient Analysis of Randomized Trials) Group. Patient level pooled analysis of 68 500 patients from seven major vitamin D fracture trials in US and Europe. BMJ. 2010;340:b5463. doi: 10.1136/bmj.b5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heikinheimo RJ, Inkovaara JA, Harju EJ, Haavisto MV, Kaarela RH, Kataja JM, et al. Annual injection of vitamin D and fractures of aged bones. Calcif Tissue Int. 1992;51:105–10. doi: 10.1007/BF00298497. [DOI] [PubMed] [Google Scholar]
- 13.Paul TV, Selvan SA, Asha HS, Thomas N, Venkatesh K, Oommen AT, et al. Hypovitaminosis D and other risk factors of femoral neck fracture in South Indian postmenopausal women: A pilot study. J Clin Diagn Res. 2015;9:OC19–22. doi: 10.7860/JCDR/2015/9444.6131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Osteoporosis Federation (IOF) Quality of Health questionnaire. [Last acessed on 2015 Mar 12].15]. Available from: https://www. osteoporosis.foundation/sites/iofbonehealth/files/2020.01/IOF.Qualeffo41.questionnaire.England.pdf . Available from: https://www.socscistatistics. com/. [Last accessed on 2020 May 9]
- 15.Harinarayan CV, Joshi SR. vitamin D status in India – Its implications and remedial measures – A review. J Assoc Physicians India. 2009;57:40–8. [PubMed] [Google Scholar]
- 16.Prentice RL, Pettinger MB, Jackson RD, Wactawski-Wende J, LaCroix AZ, Anderson GL, et al. Health risks and benefits from calcium and vitamin D supplementation: Women's Health Initiative clinical trial and cohort study. Osteoporos Int. 2013;24:567–80. doi: 10.1007/s00198-012-2224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robbins JA, Aragaki A, Crandall CJ, Manson JE, Carbone L, Jackson R, et al. Women's health initiative clinical trials: Interaction of calcium plus vitamin D and hormone therapy. Menopause. 2014;21:116–23. doi: 10.1097/GME.0b013e3182963901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: A systematic review, meta. analysis, and trial sequential analysis, Lancet Diabetes Endocrinol. 2018;6:847–58. doi: 10.1016/S2213-8587(18)30265-1. [DOI] [PubMed] [Google Scholar]
- 19.Kahwati LC, Weber RP, Pan H, Gourlay M, LeBlanc E, Coker-Schwimmer M, et al. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: Evidence report and systematic review for the US preventive services task force. JAMA. 2018;319:1600–12. doi: 10.1001/jama.2017.21640. [DOI] [PubMed] [Google Scholar]
- 20.Hansen KE, Johnson RE, Chambers KR, Johnson MG, Lemon CC, Thuy Vo TN, et al. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: Evidence report and systematic review for the US preventive services task force. JAMA. 2018;319:1600–12. doi: 10.1001/jama.2017.21640. [DOI] [PubMed] [Google Scholar]
- 21.Burt LA, Billington EO, Marianne RS, Raymond DA, Hanley DA, Boyd SK. Effect of high-dose vitamin D supplementation on volumetric bone density and bone strength: A randomized clinical trial. JAMA. 2019;322:736–45. doi: 10.1001/jama.2019.11889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kearns MD, Alvarez JA, Tangpricha V. Large, single-dose, oral vitamin D supplementation in adult populations: A systematic review. Endocr Pract. 2014;20:341–51. doi: 10.4158/EP13265.RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harinarayan CV, Srinivasa PM, Thennarasu K, Leena A. Vitamin D supplementation therapy – comparison of efficacy of three different protocols. J Clin Sci Res. 2015;4:273–80. [Google Scholar]
- 24.Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669–83. doi: 10.1056/NEJMoa055218. [DOI] [PubMed] [Google Scholar]
- 25.Sanders KM, Stuart AL, Bapp SC, Williamson EJ, Simpson JA, Kotowicz MA, et al. Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial. JAMA. 2010;303:1815–22. doi: 10.1001/jama.2010.594. [DOI] [PubMed] [Google Scholar]
- 26.Murad MH, Elamin KB, Abu Elnour NO, Elamin MB, Alkatib AA, Fatourechi MM, et al. The effect of vitamin D on falls: A systematic review and meta-analysis. J Clin Endocrinol Metabo. 2011;96:2997–3006. doi: 10.1210/jc.2011-1193. [DOI] [PubMed] [Google Scholar]
- 27.Marwaha RK, Tandon N, Gupta Y, Bhadra K, Narang A, Mani K, et al. The prevalence of and risk factors for radiographic vertebral fractures in older Indian women and men: Delhi Vertebral Osteoporosis Study (DeVOS) Arch osteoporosis. 2012;7:201–7. doi: 10.1007/s11657-012-0098-8. [DOI] [PubMed] [Google Scholar]
- 28.Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: Reanalysis of the Women's Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040. doi: 10.1136/bmj.d2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hsia J, Heiss G, Ren H, Allison M, Dolan NC, Greenland P, et al. Calcium/Vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846–54. doi: 10.1161/CIRCULATIONAHA.106.673491. [DOI] [PubMed] [Google Scholar]
- 30.LaCroix AZ, Kotchen J, Anderson G, Brzyski R, Cauley JA, Cummings SR, et al. Calcium plus vitamin D supplementation and mortality in postmenopausal women: The women's health initiative calcium–vitamin D randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2009;64A:559–67. doi: 10.1093/gerona/glp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung M, Lee J, Terasawa T, Lau J, Trikalinos TA. Calcium plus vitamin D supplementation and mortality in postmenopausal women: The women's health initiative calcium–vitamin D randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2009;64A:559–67. doi: 10.1093/gerona/glp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manson JAE, Cook NR, Lee I-M, Christen W, Bassuk SS, Mora S, et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med. 2019;380:33–44. doi: 10.1056/NEJMoa1809944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chadha M, Shingare A, Prasanth A, Chauhan P, Nishit F, Shah NF. Fracture liaison service: Prevention by coordination. Indian J Endocrinol Metab. 2018;22:719–21. doi: 10.4103/ijem.IJEM_606_18. [DOI] [PMC free article] [PubMed] [Google Scholar]