Abstract
Aim
Previous studies have shown that children of caregivers with low oral health literacy (OHL) had more untreated caries than children of caregivers with adequate OHL. However, there is a paucity of information on this relationship among children and youth with special health care needs (CYSHCN). Accordingly, this study aims to assess the association between the caregivers’ OHL and the oral health status of CYSHCN.
Methods
This cross-sectional study was conducted in four schools dedicated for CYSHCN. A 48-item questionnaire gathered information about the demographic and socioeconomic factors, the child/adolescent’s medical condition, dental characteristics, caregiver self-efficacy and the child’s dental attitude. The Comprehensive Measure of Oral Health Knowledge (CMOHK) questionnaire was used to assess the caregivers’ OHL. The Löe & Silness gingival index (GI) and the Silness & Löe plaque index (PI) were used to assess gingival health and plaque levels, respectively. Directed acyclic graphs (DAGs) were utilized for the selection of the appropriate set of confounding variables for regression analysis. The mean score differences and 95% confidence intervals (CI) were estimated to quantify the associations of the various covariates with oral health outcome variables.
Results
This study included 214 child/caregiver dyads. Most participants were physically disabled (56.1%) followed by children with hearing difficulty (9.8%) and congenital anomalies/syndromes (7.9%). The mean PI and GI of the children was 1.26±0.52 and 1.30±0.47, respectively. The median CMOHK score was 12 and the respondents were dichotomized based on the median value. Low caregiver oral health conceptual knowledge was significantly associated with higher PI scores (β [95% CI] = -0.26 [-0.41, -0.13]; p<0.001. Older participants (12-21-year-olds) had significantly higher plaque scores compared with younger participants (6-12-year-olds) (β [95% CI] = 0.33 [0.18, 0.51]; p<0.001). Participants who brushed their teeth twice or more daily had significantly lower (β [95% CI] = -0.15 [-0.43, -0.01]; p = 0.046). Conceptual knowledge score was not significantly associated with GI.
Conclusion
This study found lower caregiver OHL levels to be associated with higher plaque scores for their child.
Introduction
Oral health literacy (OHL) is “the degree to which individuals have the capacity to obtain, process, and understand basic oral health information and services needed to make appropriate health decisions” [1]. In the last two decades, OHL has increasingly gained the attention of oral health practitioners, researchers, and policy makers due to its proven impact on oral health outcomes [2]. The initial studies on OHL primarily focused on work recognition (Rapid Estimate of Adult Literacy in Dentistry -REALD [3]) or the reading comprehension (Test of Functional Health Literacy in Adults -TOFHLA [4]) skills of the respondents. However, these measures ignore the fact that individuals get information from a variety of sources, including written materials, audio-visual media, interpersonal interaction within the healthcare system, to name a few. The Institute of Medicine [5] in its landmark publication, Health Literacy: A Prescription to End Confusion, identified conceptual knowledge as one of the constructs of health literacy. Conceptual knowledge focuses assessing the general oral health knowledge, as well as specific knowledge of oral disease prevention and management. Macek et al. [6] presented a conceptual framework for the pathway between health literacy and oral health. According to this framework, oral health literacy encompasses four unique constructs: 1) word recognition, 2) reading comprehension, 3) conceptual knowledge, and 4) communication skills. The authors reported that conceptual knowledge provides a more suitable means of assessing how well an individual might understand, appraise and apply health information, as compared with assessing an individual’s reading comprehension or word recognition skills. The authors developed an instrument to measure the oral health conceptual knowledge, called the Comprehensive Measure of Oral Health Knowledge (CMOHK) [6]. Researchers have encouraged the use of conceptual knowledge instrument for studies pertaining to beliefs and self-efficacy in oral health [7].
In healthy individuals, poor OHL has been associated with poor oral health status, deleterious oral health behaviors, poor patient compliance and poor utilization of health care services [2, 8–19]. Recently, Zhou et al. [20] reported that parents with poor OHL had less compliance with oral health education and follow-up appointments for their preschool children with special health care needs (SHCN).
The American Academy of Pediatric Dentistry (AAPD) defines SHCN as “any physical, developmental, mental, sensory, behavioral, cognitive, or emotional impairment or limiting condition that requires medical management, health care intervention, and/or use of specialized services or programs” [21]. Among this population, oral diseases can have a direct and debilitating effect on the general health and quality of life of the individuals [21, 22]. Previous reports among children and youth with SHCN (CYSHCN) revealed that this population has significantly poorer oral hygiene, higher caries incidence and unmet restorative needs and severe periodontal disease compared with other children [13, 23–25]. CYSHCN might be at an increased risk for the development of oral diseases due to their compromised motor, sensory and intellectual abilities [26]. Maintaining good oral hygiene for CYSHCN is a challenge as they tend to have poor control of lips or tongue, inadequate motor capacity and poor cognitive abilities to understand the importance of oral health [27–29]. A recent study using data from the 2016–2018 National Survey of Children’s Health (NSCH) in the United States, reported that CYSHCN have poorer oral health compared with non-CYSHCN despite receiving more preventive oral health services [30]. CYSHCN rely more on their parents or caregivers to support their daily living activities [31]. Therefore, it may be assumed that the caregiver’s health literacy, attitude and expectations about oral health and oral hygiene practices would have a greater influence the oral health of CYSHCN than for others [32].
Though the body of dental literature linking OHL to oral health status continues to grow, far less is known about the influence of OHL on oral health status of CYSHCN. The present study is based on the null hypothesis that caregivers’ OHL is not associated with the oral health status of CYSHCN. Accordingly, this study aims to assess the association between the caregivers’ OHL and the oral health status of CYSHCN.
Materials and methods
Study setting and sampling procedure
This study was conducted between October 2019 and December 2020. Kuwait is divided into six different administrative areas (Governorates). A list of all the schools dedicated to CYSHCN across the six Governorates in Kuwait were compiled from the Public Authority for Disability Affairs (PADA). The sampling frame comprised of 40 schools dedicated to CYSHCN in Kuwait (14 schools in Hawalli Governorate, 10 schools in Farwaniya Governorate, five schools in Ahmadi Governorate, 4 schools each in Al-Asimah and Jahra Governorates and three schools in Mubarak Al-Kabir Governorate). Nursery schools catering to children less than 6 years were excluded. A two-stage cluster sampling technique was used for the selection of sample. For the first stage, four schools were randomly selected from sampling frame, representing 10% of all schools dedicated to CYSHCN in Kuwait. In the second stage, the selected schools were contacted for information on the class strength. Based on the reported class strength, it was decided to randomly select four to five classes from each school between grades 1 to 12 to match with the a priori sample size estimates. All the students in the selected classes were invited to participate in the study. The following selection criteria were employed for the inclusion of subjects: (1) CYSHCN as defined by AAPD [21]; (2) 6–21 years old; and (3) enrolled in the selected SHCN school. Students (1) who received professional dental prophylaxis within the previous three months; (2) undergoing fixed orthodontic treatment; (3) with severe debilitating medical condition; (4) who were taking medications are known to induce gingival changes; and (5) for whom an oral examination could not be performed, were excluded from this study. The questionnaires as well as the consent forms were sent to the caregivers of the selected students. For non-respondents, a second reminder was sent two weeks later.
Power analysis
A power assessment for linear regression was based on using plaque/gingival scores as the continuous outcome variable and dichotomized health literacy scores as predictor variable. Sample size calculation was performed by G*Power 3.1.9.7 [33]. Assuming a moderate effect size of 0.13 [34] for a model with six predictor variables, it was estimated that with the inclusion of at least 112 subjects, the study will achieve 80% power with a 0.05 two-sided significance level. The final required sample size was fixed at 200 subjects to account for the design effect of cluster sampling. Assuming a conservative 50% response rate, it was decided to invite 100 students from each of the four selected schools to participate in the study.
Data collection
The study team visited the schools and distributed the questionnaire with the informed consent forms to the students in the selected classrooms. Caregivers were contacted and the study objectives were explained. Those caregivers who agreed to participate in the study were asked to sign the informed consent form and complete the questionnaire. The 48-item questionnaire gathered information about the demographic and socioeconomic factors (age, gender, marital status, monthly income, educational level, area of residence and their relationship to the child), the child’s medical condition (diagnosis of the child’s condition, the caregiver perception of its severity and number of hospitalizations in the preceding year) and the child’s dental characteristics (last dental visit, treatment received in the previous visit and frequency of brushing).
Caregivers were asked to answer 5 self-efficacy items that were adopted from the Dental Self-Efficacy Scales by Syrjälä et al. [35] and Self-Efficacy Scale described by Kakudate et al. [36]. A 4-point Likert-type scale was used to record the responses, which ranged from ‘well prepared (+ +)’, ‘moderately prepared (+)’, ‘a little prepared (-)’ and ‘not at all prepared (- -)’. A dichotomous variable was created for each question by merging the affirmative responses (+ +/+) and non-affirmative responses (- -/-). Affirmative responses were scored of 1 and non-affirmative responses were scored 0. The five items of self-efficacy were summed up to get the total score (Range 0 to 5). The child’s dental attitude during examination was assessed using the Frankl Behavior Scale [37]. Dental attitude was dichotomized into positive (definitely positive and positive) and negative (definitely negative and negative) categories.
The main independent variable was the caregivers’ OHL. The Comprehensive Measure of Oral Health Knowledge (CMOHK) questionnaire was used to assess the caregivers’ OHL [6]. CMOHK questionnaire consists of 23 questions: 10 questions assessing the respondents’ basic knowledge, six questions assessing knowledge about dental caries prevention and management, five questions assessing knowledge about periodontal disease prevention and management, and two questions assessing oral cancer prevention and management. A previously validated Arabic version of CMOHK (CMOHK–A) questionnaire was used in this study [15]. The correct response for each CMOHK item was given a score of 1 and wrong answer was scored 0. We computed a cumulative score ranging from 0 (least conceptual knowledge level) to 23 (highest conceptual knowledge level) and estimated Cronbach-α as a measure of internal consistency and reliability. Subjects were then dichotomized into those with adequate (> the median score) and low (≤ the median score) conceptual knowledge levels [9, 15].
Clinical examination
The children were examined at the dental clinics of the SOHP by two trained and calibrated dentists. Prior to the study, the examiners were calibrated for accuracy and repeatability using the Löe & Silness gingival index (GI) [38] and Silness & Löe plaque index (PI) [39]. GI and PI were assessed on all teeth present in the mouth and the total score were computed by adding up all the scores by tooth and then dividing them by the number of teeth. Total individual scores ranged from 0 (healthy) to 3 (disease). Training and calibration of the examiners were conducted by two experienced specialists (JKB and MAQ) at the Faculty of Dentistry, Kuwait University. The inter- and intra-examiner reliability was assessed using Kappa statistics and the values obtained was >80% for both GI and PI, indicating excellent reliability. A mouth mirror and a standardized periodontal probe (CP11; Hu-Friedy, Chicago, IL, USA) were used for the examination.
Directed Acyclic Graphs (DAGs)
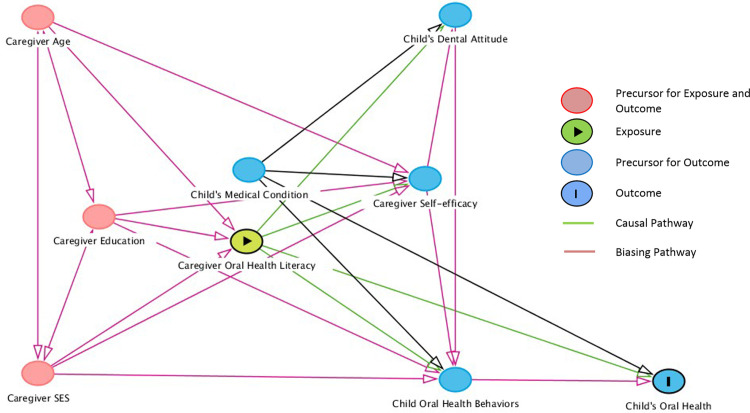
The selection of appropriate set of confounding variables were made utilizing directed acyclic graphs (DAGs). Based on causal diagram theory, DAGs are considered sets of arrows that characterize causal associations between exposures and outcomes and also specify relationships among other variables that influence the exposure or outcome [40]. The nodes on the DAGs represent the variables and the arrows represent the paths. The front door paths have arrowheads pointing from exposure to the outcome representing the presence of causal effects. Backdoor paths are noncausal biasing paths between exposure and outcome. Backdoor paths may confound a direct effect between exposure and outcome when left open [41]. In Fig 1, the socio-demographics and the child’s medical condition were considered as a priori confounders for the association between caregivers’ OHL levels and the child’s oral health. The caregivers’ self-efficacy, the child’s dental attitude and the child’s oral health behaviors (dental utilization and frequency of brushing) were considered as effect mediators in the association between the caregiver’s OHL and their child’s oral health.
Fig 1. Directed acyclic graphs (DAG) showing the associations between exposure (oral health literacy) and outcome (oral health) specifying the relationships among the covariates.
Data management and analysis
Normality assumption for GI, PI and OHL was tested using the Kolmogorov-Smirnov (K-S) test and the Shapiro-Wilk test [42]. The multivariable regression model for the outcome variables GI and PI were built using the backwards procedure for variable selection with a p<0.1 criterion. Covariates were included in the model if they improved the maximum adjusted R square estimate of the effect of literacy on the outcome variables (GI and PI). The models were adjusted for selected socio-demographic variables, medical condition, oral health behaviors, dental attitude, self-efficacy and OHL. Pairwise correlations did not exceed 80% and both mean and individual variance inflation factors approximated 1, indicating no signs of serious multicollinearity. The DAGitty (http://www.dagitty.net/) online tool was used to check the postulated DAGs for consistency and validity of the minimum adjustment sets. Chi-square and Fisher’s exact tests was used to test the significance of associations in cross tables. Means between groups were assessed using Student’s t-test or ANOVA. The mean score differences between the reference group and each variable’s response level, the 95% confidence intervals (CI) and the covariates significance levels under the multivariable models are presented. The level of significance was set to p<0.05. All bivariate and multivariable analyses were carried out using SPSS 27.0 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp.).
Ethical aspects
The Ethics Committee of Kuwait University at the Health Science Center (HSC) approved this study (VDR/EC/3329; Dated: June 3, 2018). Permission to conduct the study in the selected schools was obtained from the Ministry of Health, the Ministry of Education and from the concerned authorities at the selected schools. This study is reported in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement [43].
Results
A total of 485 children, aged 6–21 years, were identified by the study team as potentially eligible for the study and consent forms along with the questionnaire were sent to their caregivers. Among these, 237 children returned the signed informed consent form and the completed questionnaires.
Case-wise deletion method was adopted for handling missing data in CMOHK. This resulted in deletion of 23 responses. Finally, data from 214 students were analysed.
Cronbach α for CMOHK was 0.83. The mean PI and GI of the children was 1.26±0.52 and 1.30±0.47, respectively. The median CMOHK score was 12 (interquartile range: 8–14) and the respondents were dichotomized based on the median value. Table 1 shows the results of the bivariate analysis of the distribution of the study sample in relation to the two oral health literacy groups: There were almost 40% of caregivers in the age group of 30-40-year-old age group and 40-50-year-old age group. A significantly (p = 0.033) higher percentage of female caregivers had adequate OHL levels (53.1%) as compared with male caregivers’ (37.3%). None of the other child/caregiver characteristics were significantly different between the two groups.
Table 1. Bivariate comparison for the demographics, medical conditions, dental characteristics between caregivers with low and adequate levels of oral health literacy.
| Variables | All Subjects | Low OHL | Adequate OHL | |
|---|---|---|---|---|
| N (%) | (< = 12) N (%) | (>12) N (%) | p-value* | |
| Total | 214 (100.0) | 111 (51.9) | 103 (48.1) | |
| Caregiver Characteristics | ||||
| Age in years | 42.68±8.02 | 43.3±8.78 | 42.01±7.10 | 0.242 |
| Less than 30 | 9 (4.2) | 6 (66.7) | 3 (33.3) | |
| 31–40 | 87 (40.7) | 42 (48.3) | 45 (51.7) | 0.351 |
| 41–50 | 85 (39.7) | 42 (49.4) | 43 (50.6) | |
| Greater than 51 | 33 (15.4) | 21 (63.6) | 12 (36.4) | |
| Relationship with the child | ||||
| Mother | 147 (68.7) | 69 (46.9) | 78 (53.1) | 0.033 |
| Father | 67 (31.3) | 42 (62.7) | 25 (37.3) | |
| Marital Status | ||||
| Married | 188 (87.9) | 94 (50.3) | 94 (50.0) | |
| Divorced/Widow | 26 (12.1) | 17 (65.4) | 9 (34.6) | 0.15 |
| Monthly Household Income (USD) | ||||
| Less than 1650 | 21 (9.8) | 9 (42.9) | 12 (57.1) | |
| 1650 to 3300 | 44 (20.6) | 22 (50.0) | 22 (50.0) | 0.684 |
| 3301 to 6600 | 89 (41.6) | 50 (56.2) | 39 (43.8) | |
| More than 6600 | 60 (28.0) | 30 (50.0) | 30 (50.0) | |
| Educational Level | ||||
| Less than high school | 83 (38.8) | 47 (56.6) | 36 (43.4) | |
| High School | 40 (18.7) | 15 (37.6) | 25 (62.5) | 0.075 |
| Bachelor | 70 (32.7) | 41 (58.6) | 29 (41.4) | |
| Master and above | 21 (9.8) | 8 (38.1) | 13 (61.9) | |
| Participant’s Demographics | ||||
| Age in years | 12.90±3.40 | 13.17±3.6 | 12.6±3.16 | 0.22 |
| 6–12 | 99 (46.3) | 49 (49.5) | 50 (50.5) | 0.306 |
| 13–21 | 115 (53.7) | 62 (53.9) | 53 (46.1) | |
| Gender | ||||
| Female | 51 (23.8) | 23 (45.1) | 28 (54.9) | 0.267 |
| Male | 163 (76.2) | 88 (54.0) | 75 (46.0) | |
| Participant’s Medical Condition | ||||
| ADHD/Intellectual Disability | 9 (4.2) | 5 (55.6) | 4 (44.4) | |
| Learning Disability | 3 (1.4) | 2 (66.7) | 1 (33.3) | |
| Muscular Dystrophy | 14 (6.5) | 4 (28.6) | 10 (71.4) | |
| Asthma | 15 (7.0) | 6 (40.0) | 9 (60.0) | |
| Autism / Cerebral Palsy | 11 (5.1) | 5 (45.5) | 6 (54.6) | |
| Hearing Difficulty | 21 (9.8) | 10 (47.6) | 11 (52.4) | |
| Physical Disability | 120 (56.1) | 71 (59.2) | 49 (40.8) | |
| Congenital Anomalies/Downs Syndrome | 17 (7.9) | 7 (41.2) | 10 (58.8) | |
| Metabolic Disorders | 4 (1.9) | 1 (25.0) | 3 (75.0) | |
| Caregivers perception of the severity of medical condition # | ||||
| Mild | 35 (18.8) | 14 (40.0) | 21 (60.0) | 0.402 |
| Moderate | 48 (25.8) | 26 (54.2) | 22 (45.8) | |
| Severe | 103 (55.4) | 53 (51.5) | 50 (48.5) | |
| Participant’s hospitalization history in the preceding year # | ||||
| None | 162 (85.7) | 81 (50.0) | 81 (50.0) | 0.679 |
| One or more times | 27 (14.3) | 15 (55.6) | 12 (44.4) | |
| Participant’s Dental Characteristics | ||||
| Last Dental Visit | ||||
| Within the last 6 months | 103 (48.1) | 53 (51.5) | 50 (48.1) | 0.494 |
| Between 6 months– 1 year | 63 (29.4) | 36 (57.1) | 27 (42.9) | |
| More than a year back | 48 (22.4) | 22 (45.8) | 26 (54.2) | |
| Reason for the previous dental visit | ||||
| Routine check-up | 80 (37.4) | 43 (53.8) | 37 (46.3) | 0.422 |
| Extraction | 32 (15.0) | 17 (53.1) | 15 (46.9) | |
| Restoration | 43 (20.1) | 24 (55.8) | 19 (44.2) | |
| Prophylaxis | 47 (22.0) | 24 (51.1) | 23 (48.9) | |
| Root canal treatment | 12 (5.6) | 3 (25.0) | 9 (75.0) | |
| Frequency of toothbrushing | ||||
| Less than twice daily | 90 (42.1) | 48 (53.3) | 42 (46.7) | 0.41 |
| Twice daily or more | 124 (57.9) | 63 (50.8) | 61 (49.2) | |
| Participant’s Dental Attitude # | ||||
| Positive | 126 (62.1) | 68 (54.0) | 58 (46.0) | 0.318 |
| Negative | 77 (37.9) | 36 (46.8) | 41 (53.2) | |
*Pearson Chi-square statistics.
# Missing values present.
OHL–Oral health literacy.
Most of the caregivers were married (87.9%) and about 40% had a monthly household income within the range of 3,300 to 6,600 US dollars. A high percentage of caregivers had less than high school education (38.8%) and about a third of the respondents had a bachelor’s degree. The mean age (SD) of the children was 12.9 (3.40) years and about three-fourths were boys (76.2%). They were categorized into two age groups: 6-12-year-olds (46.3%) and 13-21-year-olds (53.7%). Most of the children were physically disabled (56.1%) followed by children with hearing difficulty (9.8%) and congenital anomalies/syndromes (7.9%). More than half of the caregivers perceived the child’s medical condition to be ‘severe’, and about 14% of the children had been hospitalized due to their medical condition in the preceding year. About half of the children had a dental visit within the previous six months and about 40% of the visits were for routine dental check-up. Most of the children brushed twice or more daily (57.9%) and had a positive dental attitude (62.1%).
Table 2 presents the self-efficacy of caregivers with low OHL and adequate OHL. A significantly higher percentage of caregivers with adequate OHL levels reported being confident of getting their child the necessary medical attention (p = 0.048) and obtaining the necessary information to care for their child (p = 0.001) as compared with those with low OHL. The caregivers with adequate OHL had a significantly (p = 0.019) higher mean self-efficacy score compared with those with low OHL (2.22±1.02 and 1.87±1.01, respectively).
Table 2. Association between caregivers’ oral health literacy and self-efficacy.
| Variables | All Subjects | Low OHL | Adequate OHL | |
|---|---|---|---|---|
| N (%) | (< = 12) N (%) | (>12) N (%) | p-value* | |
| How confident are you that you can… | ||||
| 1. …get your child the required medical care | ||||
| Very confident | 90 (45.0) | 40 (44.4) | 50 (55.6) | 0.048 |
| Not confident | 110 (55.0) | 63 (57.3) | 47 (42.7) | |
| 2. …get your child the required dental care | ||||
| Very confident | 165 (80.1) | 83 (50.3) | 82 (49.7) | 0.313 |
| Not confident | 41 (19.9) | 23 (56.1) | 18 (43.9) | |
| 3. …control the child’s daily sugar intake | ||||
| Very confident | 57 (27.1) | 27 (47.4) | 30 (52.6) | 0.316 |
| Not confident | 153 (72.9) | 80 (52.3) | 73 (47.7) | |
| 4. …obtain the necessary health information to take care of your child | ||||
| Very confident | 44 (20.8) | 13 (29.5) | 31 (70.5) | 0.001 |
| Not confident | 168 (79.2) | 96 (57.1) | 72 (42.9) | |
| 5. …choose the right health care provider to meet your child’s healthcare needs | ||||
| Very confident | 47 (22.1) | 24 (51.1) | 23 (48.9) | 0.530 |
| Not confident | 166 (77.9) | 86 (51.8) | 80 (48.2) | |
| Self-efficacy (Mean±SD) | 2.05±1.03 | 1.87±1.01 | 2.22±1.02 | 0.019 |
*Pearson Chi-square statistics.
OHL–Oral health literacy.
The association between the various covariates and the outcome variable is represented as DAGs (Fig 1).
After adjusting for the other covariates in the multivariable linear regression model, the caregiver’s OHL was significantly associated with PI scores (β [95% CI] = -0.26 [-0.41, -0.13]; p<0.001) (Table 3). As compared with families with less than 1650 USD monthly income, children belonging to families with higher incomes had significantly lower PI scores (p<0.05). Older participants (12-21-year-olds) had significantly higher plaque scores compared with younger participants (6-12-year-olds) (β [95% CI] = 0.33 [0.18, 0.51]; p<0.001). Participants who brushed their teeth twice or more daily had significantly lower (β [95% CI] = -0.15 [-0.43, -0.01]; p = 0.046). The adjusted R square value for the model for PI was 20%. After adjusting the model for covariates, OHL was not significantly associated with GI (Table 4). As compared with younger participants, older participants had significantly higher GI scores (β [95% CI] = 0.30 [0.13, 0.43]; p<0.001). There was no significant association between the other covariates and GI. The variables in the model explained about 13% of the variance in the GI scores.
Table 3. Multivariable linear regression analysis for the association of plaque index with the various caregiver/child level factors.
| Variables | Unadjusted | Adjusted | |||
|---|---|---|---|---|---|
| Mean±SD* | 95% Confidence Interval | Standardized Coefficients Beta | 95% Confidence Interval | p-value | |
| PLAQUE INDEX | |||||
| Oral health literacy | |||||
| Low | 1.40±0.48 | Ref | Ref. | Ref. | |
| Adequate | 1.10±0.52 | -0.43, -0.16 ‡ | -0.26 | -0.41, -0.13 ‡ | <0.001 ‡ |
| Monthly Household Income (USD) | |||||
| Less than 1650 | 1.32±0.52 | Ref | Ref | Ref. | |
| 1650 to 3300 | 1.25±0.50 | -0.34, 0.20 | -0.23 | -0.58, -0.03 † | 0.03 † |
| 3301 to 6600 | 1.25±0.50 | -0.32, 0.18 | -0.28 | -0.55, -0.05 † | 0.029 † |
| More than 6600 | 1.26±0.56 | -0.32, 0.20 | -0.27 | -0.58, -0.06 † | 0.015 † |
| Participant’s age in years | |||||
| 6–12 | 1.11±0.51 | Ref | Ref | Ref | |
| 12–21 | 1.39±0.49 | 0.14, 0.41 ‡ | 0.33 | 0.18, 0.51 ‡ | <0.001 ‡ |
| Frequency of daily brushing | |||||
| Less than twice | 1.31±0.47 | Ref | Ref | Ref | |
| Twice or more | 1.19±0.48 | -0.33, 0.10 | -0.15 | -0.43, -0.01 † | 0.046 † |
| Age of Caregiver | |||||
| Less than 30 | 1.32±0.48 | -0.54, 0.22 | 0.02 | -0.38, 0.45 | 0.862 |
| 30–40 | 1.13±0.53 | -0.56, -0.15 † | -0.19 | -0.43, 0.03 | 0.092‡ |
| 40–50 | 1.30±0.50 | -0.40, 0.02 | -0.11 | -0.34, 0.10 | 0.291 |
| Greater than 50 | 1.49±0.47 | Ref | Ref | Ref | |
| Self-efficacy Score | 1.30±0.46 | -0.04, 0.11 | 0.08 | -0.04, 0.12 | 0.308 |
Adjusted R2 for Plaque Index = 0.20.
*Independent sample t-test or ANOVA.
† Statistically significant at the 5% level;
‡Statistically significant at the 1% level.
Table 4. Multivariable linear regression analysis for the association of gingival index with the various caregiver/child level factors.
| Variables | Unadjusted | Adjusted | |||
|---|---|---|---|---|---|
| Mean±SD* | 95% Confidence Interval | Standardized Coefficients Beta | 95% Confidence Interval | p-value | |
| GINGIVAL INDEX | |||||
| Oral health literacy | |||||
| Low | 1.34±0.48 | Ref | Ref | Ref | |
| Adequate | 1.26±0.46 | -0.21, 0.05 | -0.08 | -0.21, 0.06 | 0.283 |
| Participant’s age in years | |||||
| 6–12 | 1.15±0.50 | Ref | Ref | Ref | |
| 12–21 | 1.44±0.40 | 0.16, 0.41 ‡ | 0.30 | 0.13, 0.43 ‡ | <0.001 ‡ |
| History of Hospitalization in the last one year | |||||
| None | 1.31±0.47 | Ref | Ref | Ref | |
| Yes | 1.19±0.48 | 0.26, -0.31 | -0.14 | -0.38, 0.01 | 0.068‡ |
| Frequency of brushing | |||||
| Less than twice daily | 1.31±0.44 | Ref | Ref | Ref | |
| Twice daily or more | 1.30±0.49 | -0.14, 0.11 | -0.07 | -0.20, 0.07 | 0.336 |
| Monthly Household Income (USD) | |||||
| Less than 1650 | 1.32±0.36 | Ref | Ref | Ref | |
| 1650 to 3300 | 1.35±0.45 | -0.22, 0.28 | -0.09 | -0.36, 0.07 | 0.420 |
| 3301 to 6600 | 1.26±0.48 | -0.28, 0.17 | -0.14 | -0.37, 0.10 | 0.263 |
| More than 6600 | 1.34±0.50 | -0.21, 0.26 | -0.09 | -0.34, 0.15 | 0.449 |
| Age of Caregiver | |||||
| Less than 30 | 1.25±0.54 | -0.64, 0.04 | -0.06 | -0.55, 0.25 | 0.470 |
| 30–40 | 1.22±0.47 | -0.52, -0.15 † | -0.17 | -0.39, 0.06 | 0.141 |
| 40–50 | 1.30±0.48 | -0.44, -0.07 † | -0.15 | -0.36, 0.07 | 0.182 |
| Greater than 50 | 1.55±0.35 | Ref | Ref | Ref | |
Adjusted R2 for Gingival Index = 0.13.
*Independent sample t-test or ANOVA.
† Statistically significant at the 5% level; `
‡Statistically significant at the 1% level.
Discussion
This study is the first to our knowledge to report on the relationship between caregivers’ oral health conceptual knowledge, sociodemographic characteristics, personality traits and the oral health status of CYSHCN. The results of this study suggest that caregiver characteristics like low oral health conceptual knowledge and low socioeconomic status; and, child level characteristics like older-age-group and lower frequency of brushing are strongly associated with higher plaque scores. In addition, older age group subjects (>12 years) had more gingival inflammation compared with younger children.
CMOHK was found to be a valid and reliable measure of OHL to detect statistical associations with clinical measures of periodontal health including plaque scores [44]. The Arabic translated version of CMOHK (CMOHK-A) has been previously validated in a similar population [15]. The CMOHK was found to be better suited for differentiating health literacy levels at the lower end of the scale than REALD or TOFHLA [6]. Previous research [7] have shown that conceptual knowledge was significantly related to dental beliefs, attitudes and self-efficacy, thereby confirming the suitability of using CMOHK as an OHL measure in this study. In the original study, Macek et al. [6] categorized the respondents CMOHK scores into three categories: scores from 0 to 11 represented ‘poor’, scores from 12–14 represented ‘fair’, and scores from 15–23 represented ‘good’ OHL levels. However, to date there are no norms established to indicate a score for ‘adequate’ OHL. As in a previous investigation [15], the median score was used to categorize the respondents into ‘low’ and ‘adequate’ conceptual knowledge level groups. In this study, children of caregivers with higher levels of oral health conceptual knowledge had lower plaque scores. Oral health conceptual knowledge directly results from interacting with dentists/dental hygienists and individuals with higher levels of oral health conceptual knowledge might be more likely to visit a dentist/dental hygienist because they might be more aware of the importance of oral health.
Previous research has shown that CMOHK is associated with the respondents confidence in filling out forms [7]. Since CMOHK was able to assess the functional skill set of the caregivers, it provides additional evidence of its applicability as a valid measure of OHL [7]. The health seeking behavior is influenced by a number of factors, including the individual’s perception about the symptoms, perceived disrespect, and ability to understand the health care system [45]. Since OHL plays a central role in one’s ability to recognize oral health information and act upon it, it may affect the caregivers’ perception of their children’s oral status, as well as their healthcare seeking behavior.
Studies comparing individuals with disabilities to similarly aged individuals with normal development have shown poorer oral hygiene and increased periodontal disease within the disability group [46]. CYSHCN may have poorer oral health due to their underlying medical condition which puts them at higher risk and/or due to caregiver level factors like not being able to recognize a need. CYSHCN have chronic dependence on caregivers for their oral as well as general health. The caregiver’s knowledge and attitude towards the child’s oral health plays a vital role in ensuring that the child receives timely and routine dental care.
This study reports lower caregiver conceptual knowledge to be consistently and independently associated with higher plaque scores for their child. Similar findings were reported in the study by Vann et al. [12], though their study was conducted in a low-income community using a different OHL instrument (REALD). Bridges et al. [13] also reported caregiver oral health literacy to be associated with their child’s oral health even after adjusting for the effect of various potential confounders. Baskaradoss et al. [15] found that children of caregivers with poor OHL levels had more untreated caries than children of caregivers with adequate OHL. These findings suggest that oral health literacy is a fundamental dimension that confers oral health impacts above and beyond education and socio-demographic characteristics.
Almost half of the children in this study had a dental visit within the previous six-months and in more than half of the visits, only routine dental check-up or dental prophylaxis was performed. This is an indication of the raised awareness about the importance of preventive dental visits. Pediatric and public health programs have always promoted preventive dental care as the “cornerstone of optimal oral health promotion” [47]. Preventive dental care is also cost-effective and routine preventive and restorative services can reduce the need for more expensive emergency or inpatient treatment of dental problems.
Recognizing the benefits of focusing on of early prevention of dental diseases, the Ministry of Health, Kuwait, have implemented one of the largest SOHP in the world. SOHP is a comprehensive school-based oral health program with educational, preventive and treatment components serving the oral health needs of more than 300,000 school children between the age group of 6–16 years [22]. Schools for CYSHCN have been included to this program and most of these schools have dental clinics within their campuses. These initiatives help in raising the awareness among the caregivers on the importance of good oral health.
Lee et al. [48] found self-efficacy to act as a mediator or modifier for the relationship between OHL and oral health status. Studies by Jonsson et al. [49] showed that approaches targeting factors regarding the self-efficacy can improve oral hygiene behavior. This relationship was explored in this study. The general self-efficacy questionnaire [50] is popularly used in dental researches. However, previous research has shown that this instrument does not show significant correlation with oral hygiene indices [51]. It has been suggested that it may not be possible to predict better oral hygiene from a high general self-efficacy. Instead, it is important to measure task specific self-efficacy [52]. Therefore, task specific self-efficacy questions matching our study objectives were developed for this research. In this study, caregivers with low conceptual knowledge scores had significantly lower self-efficacy scores compared with those with adequate conceptual knowledge scores. Though the association between self-efficacy scores and plaque scores were not statistically significant, it was added to the final models as it improved the predictive value of the final model.
In this study older age group subjects had significantly more plaque and gingival inflammation compared to younger age group subjects. It was indistinguishable whether the difference in oral health between younger and older age group subjects were due to the child level (e.g., child’s chronic illness or oral health behaviors) or more related to the caregiver level factors. It could be that the caregivers give more attention to the oral hygiene practices of younger children as compared to older children. This could also be due to the higher focus given by the SOHP on the oral health of younger children with regards to placement of dental sealants in this group. Our analysis did not differentiate preventive services from other dental treatments and therefore was not included in the final model.
The results of this study suggest children who brushed twice or more daily have lower levels of plaque. However, the frequency of brushing was not associated with the caregiver’s conceptual knowledge levels. This is in contrast to the results of Vann et al. [12], which reported lower caregiver literacy to be strongly associated with no daily tooth brushing. There are several factors that may explain the difference in the study findings between the two studies. Vann et al. [12] included only infants (less than 5-years-old) in their study, whereas, the current did not include this age group. The dependence on the caregiver for oral hygiene is much more higher for infants than for any other age groups. Additionally, the difference in the data collection method employed by the two studies could also have contributed to the contrasting results. Data collection for the study by Vann et al. [12] was performed by trained examiners using an interview schedule as compared with the current study, which used self-administered questionnaires.
The present results should be considered in light of the study’s limitations. Firstly, the cross-sectional design of the study limits the potential to make any causal inferences with regard to the pathways that may link caregiver conceptual knowledge levels with the child’s oral health. Secondly, this study used a non-probability sampling technique for selection of study participants, thus limiting the generalizability of the results. Thirdly, as with all the investigations examining health literacy, it is acknowledged that low caregiver conceptual knowledge levels may be a threat to the study’s validity because of the caregiver’s difficulty in reading and comprehending survey questions. The caregiver’s with low levels of conceptual knowledge are likely to have difficulty completing the questionnaire or giving informed consent to participate in this study. It was not feasible to assess if the caregiver characteristics differed between those who agreed to participate in the study and those who did not. Finally, influence of culture might have shaped the caregivers’ perspectives, negotiating these opinions culturally was not within the scope of this study.
To conclude, this study found lower caregiver OHL levels to be associated with higher plaque scores for their child. The results of this study could help in planning awareness campaigns to improve the oral health knowledge and attitude of the caregiver. Integrating literacy-based approaches to existing initiatives for caregivers may help to improve the oral hygiene of CYSHCN.
Supporting information
(SAV)
Acknowledgments
The authors thank all the children and their caregiver’s who participated in this study. We thank Dr. Sahar Behzadi, Dr. Fatemah AlWaheeb, Dr. Sultan Hanna. Ms. Khitam AlShorbaji. Ms Anila Moneesh, Ms. Rosy Veena Syriac, Ms. Safeera Kovapurath and Mr. Vimal Lukose for assisting in data collection.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
JKB received a grant for this study. The study was supported by the Research Sector of Kuwait University (Grant Number: DD 01/18). Webpage of funding agency: http://www.ovpr.ku.edu.kw/index.php/en/ The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Institute of Medicine. Health literacy: a prescription to end confusion. National Academies Press Washington, DC; 2004. [PubMed] [Google Scholar]
- 2.Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health. 2018;18(1):172. Epub 2018/10/26. doi: 10.1186/s12903-018-0640-1 ; PubMed Central PMCID: PMC6201552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30—a brief communication. J Public Health Dent. 2007;67(2):94–8. Epub 2007/06/15. doi: 10.1111/j.1752-7325.2007.00021.x . [DOI] [PubMed] [Google Scholar]
- 4.Gong DA, Lee JY, Rozier RG, Pahel BT, Richman JA, Vann WF Jr,. Development and testing of the Test of Functional Health Literacy in Dentistry (TOFHLiD). J Public Health Dent. 2007;67(2):105–12. Epub 2007/06/15. doi: 10.1111/j.1752-7325.2007.00023.x . [DOI] [PubMed] [Google Scholar]
- 5.Kindig DA, Panzer AM, Nielsen-Bohlman L. Health literacy: a prescription to end confusion. 2004. [PubMed] [Google Scholar]
- 6.Macek MD, Haynes D, Wells W, Bauer-Leffler S, Cotten PA, Parker RM. Measuring conceptual health knowledge in the context of oral health literacy: preliminary results. J Public Health Dent. 2010;70(3):197–204. doi: 10.1111/j.1752-7325.2010.00165.x ; PubMed Central PMCID: PMC3612930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macek MD, Atchison KA, Chen H, Wells W, Haynes D, Parker RM, et al. Oral health conceptual knowledge and its relationships with oral health outcomes: Findings from a Multi-site Health Literacy Study. Community Dent Oral Epidemiol. 2017;45(4):323–9. doi: 10.1111/cdoe.12294 ; PubMed Central PMCID: PMC5498245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blizniuk A, Ueno M, Zaitsu T, Kawaguchi Y. Association of oral health literacy with oral health behaviour and oral health status in Belarus. Community Dent Health. 2015;32(3):148–52. . [PubMed] [Google Scholar]
- 9.Baskaradoss JK. The association between oral health literacy and missed dental appointments. J Am Dent Assoc. 2016;147(11):867–74. doi: 10.1016/j.adaj.2016.05.011 . [DOI] [PubMed] [Google Scholar]
- 10.Kranz AM, Pahel BT, Rozier RG. Oral literacy demand of preventive dental visits in a pediatric medical office: a pilot study. Pediatr Dent 2013;35(2):E68–74. Epub 2013/05/03. . [PubMed] [Google Scholar]
- 11.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Medical Care. 2002;40(5):395–404. Epub 2002/04/19. doi: 10.1097/00005650-200205000-00005 . [DOI] [PubMed] [Google Scholar]
- 12.Vann WF Jr., Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. 2010;89(12):1395–400. doi: 10.1177/0022034510379601 ; PubMed Central PMCID: PMC3123718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bridges SM, Parthasarathy DS, Wong HM, Yiu CK, Au TK, McGrath CP. The relationship between caregiver functional oral health literacy and child oral health status. Patient Educ Couns. 2014;94(3):411–6. doi: 10.1016/j.pec.2013.10.018 . [DOI] [PubMed] [Google Scholar]
- 14.Divaris K, Lee JY, Baker AD, Vann WF Jr,. Caregivers’ oral health literacy and their young children’s oral health-related quality-of-life. Acta Odontol Scand. 2012;70(5):390–7. doi: 10.3109/00016357.2011.629627 ; PubMed Central PMCID: PMC3305855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baskaradoss JK, AlThunayan MF, Alessa JA, Alobaidy SS, Alwakeel RS, Alshubaiki AH, et al. Relationship between Caregivers’ Oral Health Literacy and their Child’s Caries Experience. Community Dent Health. 2019;36(2):111–7. Epub 2019/04/26. doi: 10.1922/CDH_4444Baskaradoss07 . [DOI] [PubMed] [Google Scholar]
- 16.Miller E, Lee JY, DeWalt DA, Vann WF Jr,. Impact of caregiver literacy on children’s oral health outcomes. Pediatrics. 2010;126(1):107–14. Epub 2010/06/16. doi: 10.1542/peds.2009-2887 ; PubMed Central PMCID: PMC2896459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parker EJ, Jamieson LM. Associations between indigenous Australian oral health literacy and self-reported oral health outcomes. BMC Oral Health. 2010;10:3. Epub 2010/03/30. doi: 10.1186/1472-6831-10-3 ; PubMed Central PMCID: PMC2859391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sistani MMN, Virtanen J, Yazdani R, Murtomaa H. Association of oral health behavior and the use of dental services with oral health literacy among adults in Tehran, Iran. Eur J Dent. 2017;11(2):162–7. Epub 2017/07/22. doi: 10.4103/ejd.ejd_332_16 ; PubMed Central PMCID: PMC5502558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wehmeyer MM, Corwin CL, Guthmiller JM, Lee JY. The impact of oral health literacy on periodontal health status. J Public Health Dent. 2014;74(1):80–7. Epub 2012/11/06. doi: 10.1111/j.1752-7325.2012.00375.x ; PubMed Central PMCID: PMC3800213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou N, Wong HM, McGrath CP. Parental Compliance towards Oral Health Education among Preschoolers with Special Healthcare Needs. Int J Environ Res Public Health. 2021;18(14). Epub 2021/07/25. doi: 10.3390/ijerph18147323 ; PubMed Central PMCID: PMC8307991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Academy of Pediatric Dentistry. Definition of special health care needs. The Reference Manual of Pediatric Dentistry. Chicago, Ill. 2020:19. [Google Scholar]
- 22.Shyama M, Al-Mutawa SA, Honkala S, Sugathan T, Honkala E. Oral hygiene and periodontal conditions in special needs children and young adults in Kuwait. J Disabil Oral Health. 2000;1:13–9. [Google Scholar]
- 23.Lewis C, Robertson AS, Phelps S. Unmet dental care needs among children with special health care needs: implications for the medical home. Pediatrics. 2005;116(3):e426–e31. doi: 10.1542/peds.2005-0390 [DOI] [PubMed] [Google Scholar]
- 24.Newacheck PW, Hughes DC, Hung Y-Y, Wong S, Stoddard JJ. The Unmet Health Needs of America9s Children. Pediatrics. 2000;105(Supplement 3):989–97. [PubMed] [Google Scholar]
- 25.Newacheck PW, McManus M, Fox HB, Hung Y-Y, Halfon N. Access to health care for children with special health care needs. Pediatrics. 2000;105(4):760–6. doi: 10.1542/peds.105.4.760 [DOI] [PubMed] [Google Scholar]
- 26.Bertness J, Holt KA. Oral Health Services for Children and Adolescents with Special Health Care Needs: A Resource Guide: National Maternal and Child Oral Health Resource Center; 2011. [Google Scholar]
- 27.Al-Allaq T, DeBord TK, Liu H, Wang Y, Messadi DV. Oral health status of individuals with cerebral palsy at a nationally recognized rehabilitation center. Spec Care Dentist. 2015;35(1):15–21. Epub 2014/04/09. doi: 10.1111/scd.12071 . [DOI] [PubMed] [Google Scholar]
- 28.Du RY, Yiu CKY, King NM. Oral Health Behaviours of Preschool Children with Autism Spectrum Disorders and Their Barriers to Dental Care. J Autism Dev Disord. 2019;49(2):453–9. Epub 2018/08/24. doi: 10.1007/s10803-018-3708-5 . [DOI] [PubMed] [Google Scholar]
- 29.Kim K, Kang JY, Jang DH. Relationship Between Mobility and Self-Care Activity in Children With Cerebral Palsy. Ann Rehabil Med. 2017;41(2):266–72. Epub 2017/05/16. doi: 10.5535/arm.2017.41.2.266 ; PubMed Central PMCID: PMC5426278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lebrun-Harris LA, Canto MT, Vodicka P, Mann MY, Kinsman SB. Oral Health Among Children and Youth With Special Health Care Needs. Pediatrics. 2021;148(2). Epub 2021/07/23. doi: 10.1542/peds.2020-025700 . [DOI] [PubMed] [Google Scholar]
- 31.Chinn D. Review of Interventions to Enhance the Health Communication of People With Intellectual Disabilities: A Communicative Health Literacy Perspective. J Appl Res Intellect Disabil. 2017;30(2):345–59. Epub 2016/02/19. doi: 10.1111/jar.12246 . [DOI] [PubMed] [Google Scholar]
- 32.Ferguson FS, Cinotti D. Home oral health practice: the foundation for desensitization and dental care for special needs. Dent Clin North Am. 2009;53(2):375–87, xi. Epub 2009/03/10. doi: 10.1016/j.cden.2008.12.009 . [DOI] [PubMed] [Google Scholar]
- 33.Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. doi: 10.3758/bf03193146 [DOI] [PubMed] [Google Scholar]
- 34.Cohen J. Statisticalpower analysis for the behavioral sciences (2nd ed.). New York: Academic. 1988. [Google Scholar]
- 35.Syrjälä AMH, Kneckt MC, Knuuttila ML. Dental self-efficacy as a determinant to oral health behaviour, oral hygiene and HbA1c level among diabetic patients. J Clin Periodontol. 1999;26(9):616–21. doi: 10.1034/j.1600-051x.1999.260909.x [DOI] [PubMed] [Google Scholar]
- 36.Kakudate N, Morita M, Yamazaki S, Fukuhara S, Sugai M, Nagayama M, et al. Association between self-efficacy and loss to follow-up in long-term periodontal treatment. J Clin Periodontol. 2010;37(3):276–82. doi: 10.1111/j.1600-051X.2009.01529.x [DOI] [PubMed] [Google Scholar]
- 37.Frankl S, Shiere F, H. F. Should the parent remain with the child in the dental operatory? J Dent Child. 1962;29:150–63. [Google Scholar]
- 38.Löe H, Silness J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand. 1963;21(6):533–51. doi: 10.3109/00016356309011240 [DOI] [PubMed] [Google Scholar]
- 39.Silness J, Löe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22(1):121–35. [DOI] [PubMed] [Google Scholar]
- 40.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. Epub 1999/01/15. . [PubMed] [Google Scholar]
- 41.Birungi N, Fadnes LT, Kasangaki A, Nankabirwa V, Okullo I, Lie SA, et al. Assessing causal effects of early life-course factors on early childhood caries in 5-year-old Ugandan children using directed acyclic graphs (DAGs): A prospective cohort study. Community Dent Oral Epidemiol. 2017;45(6):512–21. Epub 2017/06/21. doi: 10.1111/cdoe.12314 . [DOI] [PubMed] [Google Scholar]
- 42.Öztuna D, Elhan AH, Tüccar E. Investigation of four different normality tests in terms of type 1 error rate and power under different distributions. Turk J Med Sci. 2006;36(3):171–6. [Google Scholar]
- 43.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. doi: 10.1016/j.ijsu.2014.07.013 . [DOI] [PubMed] [Google Scholar]
- 44.Holtzman JS, Atchison KA, Macek MD, Markovic D. Oral Health Literacy and Measures of Periodontal Disease. J Periodontol. 2017;88(1):78–88. Epub 2016/08/16. doi: 10.1902/jop.2016.160203 ; PubMed Central PMCID: PMC5557021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lacy NL, Paulman A, Reuter MD, Lovejoy B. Why we don’t come: patient perceptions on no-shows. Ann Fam Med. 2004;2(6):541–5. doi: 10.1370/afm.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pilebro C, Backman B. Teaching oral hygiene to children with autism. Int J Paediatr Dent. 2005;15(1):1–9. Epub 2005/01/25. doi: 10.1111/j.1365-263X.2005.00589.x . [DOI] [PubMed] [Google Scholar]
- 47.Lewis CW, Johnston BD, Linsenmeyar KA, Williams A, Mouradian W. Preventive dental care for children in the United States: a national perspective. Pediatrics. 2007;119(3):e544–53. Epub 2007/03/03. doi: 10.1542/peds.2006-1958 . [DOI] [PubMed] [Google Scholar]
- 48.Lee JY, Divaris K, Baker AD, Rozier RG, Vann WF Jr,. The relationship of oral health literacy and self-efficacy with oral health status and dental neglect. Am J Public Health. 2012;102(5):923–9. doi: 10.2105/AJPH.2011.300291 ; PubMed Central PMCID: PMC3267012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jonsson B, Ohrn K, Lindberg P, Oscarson N. Evaluation of an individually tailored oral health educational programme on periodontal health. J Clin Periodontol. 2010;37(10):912–9. Epub 2010/06/22. doi: 10.1111/j.1600-051X.2010.01590.x . [DOI] [PubMed] [Google Scholar]
- 50.Schwarzer R, Jerusalem M. Generalized self-efficacy scale. Measures in health psychology: A user’s portfolio Causal and control beliefs. 1995;1(1):35–7. [Google Scholar]
- 51.Woelber JP, Bienas H, Fabry G, Silbernagel W, Giesler M, Tennert C, et al. Oral hygiene-related self-efficacy as a predictor of oral hygiene behaviour: a prospective cohort study. J Clin Periodontol. 2015;42(2):142–9. Epub 2014/12/05. doi: 10.1111/jcpe.12348 . [DOI] [PubMed] [Google Scholar]
- 52.Kakudate N, Morita M, Yamazaki S, Fukuhara S, Sugai M, Nagayama M, et al. Association between self-efficacy and loss to follow-up in long-term periodontal treatment. J Clin Periodontol. 2010;37(3):276–82. Epub 2010/01/22. doi: 10.1111/j.1600-051X.2009.01529.x . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.