ABSTRACT
Styloidogenic jugular venous compression syndrome has been recently described as a new cause of idiopathic intracranial hypertension. We present a 69-year-old patient, without other relevant medical history, presenting with 3 years of positional headache associated with decreased vision when reading and while turning her head to the right or left. She also reported pulsatile low-frequency tinnitus. Papilloedema was noted on the physical examination and, on imaging, an enlarged styloid process that induced jugular vein compression. The patient underwent styloidectomy with resolution of her symptoms and normalisation of her visual fields.
KEYWORDS: Papilloedema, styloid process, eagle syndrome, jugular venous compression, intracranial hypertension
Introduction
Papilloedema is a key feature in intracranial hypertension, especially in idiopathic intracranial hypertension (IIH).1 IIH is characterised as a primary cause of intracranial hypertension, thus making it a diagnosis of exclusion, in which space occupying lesions, venous thrombosis and other anatomical problems should be ruled out.1 Since 2012, a new form of secondary intracranial hypertension has been described, in which an enlarged styloid process induces immediate jugular vein compression, decrease in venous outflow, and a secondary increase in intracranial pressure.2
Eagle’s syndrome (ES), due to an enlarged styloid process, was first described in 1937 by Dr. W.W. Eagle in Duke University.3 The underlying anatomical abnormality found in Eagle Syndrome is the elongation and calcification of the styloid process, either unilaterally or bilaterally.4 It can manifest in one of three ways: 1) the classic presentation; 2) associated with carotid compression; and 3) associated with an IIH-like syndrome.4 The classic presentation consists of neck pain, dysphagia, foreign body sensation, otalgia, pain with yawning, or pain on turning of the head.2,4,5 The second clinical presentation is associated with carotid artery compression, transient ischaemic attacks, Horner’s syndrome, and stroke.2,4–6 It has been estimated that 4–7.3% of the population has an elongated styloid process, defined as 30 mm or longer.4,7
In 2012, a third syndromic presentation associated with an enlarged styloid process was defined.8 The elongated styloid process can compress the jugular vein in certain head positions, causing an intermittent decrease in the venous outflow. This leads to a jugular pressure gradient dependent on the position of the head.9 When the gradient is maintained, the venous stasis may lead to thrombosis or increased intracranial pressure without thrombosis.2,10,11 This ultimately manifests with an IIH-like clinical picture with headaches, pulsatile tinnitus, transient visual obscurations, and visual field defects.2,10–12 Thirty-two cases of the third manifestation of Eagle’s syndrome have been reported in the literature; however, to date, only one has been reported with optic disc swelling, and no report has described the swelling in detail nor the ophthalmic results after treatment of the condition.12 Medical treatment has been attempted in cases with thrombosis,13 but most cases need a surgical approach to decompress the jugular vein.2,8,10–12,14 We present a case of styloidogenic jugular venous compression syndrome causing papilloedema and a review of the current literature. We adhered to the CARE recommendations for this report.15 The patient gave written consent for the publication.
Case report
An otherwise healthy 69-year-old female presented with 3 years of intermittent holocranial headache, that worsened when she turned her head to the right or to the left and down when she read. She also stated that her right hemiface became swollen if she read for prolonged periods. For the last 6 months prior to her initial neuro-ophthalmology visit, she also experienced a low frequency, pulse-synchronous tinnitus.
Physical examination demonstrated normal weight (BMI 24.0), normal neurological examination, and visual acuity of 20/20 in both eyes. Fundus examination demonstrated Frisén grade 1 papilloedema in both eyes with engorged vein vasculature. Both the vascular engorgement and optic disc oedema increased after half a minute of left head turn (Figure 1). Optical coherence tomography (OCT) of the optic nerves demonstrated mild elevation of the optic nerves and oedema of the retinal nerve fibre layers (RNFL) at 111 μm and 114 μm in the right and left eyes, respectively. 30–2 Humphrey visual field examination demonstrated an enlarged blind spot in both eyes.
Figure 1.
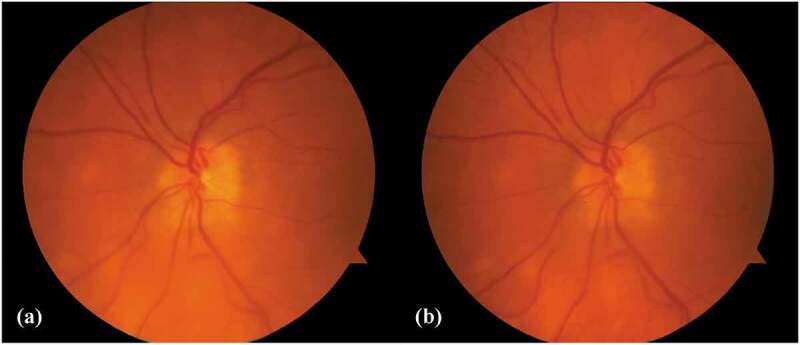
Colour photograph of the left optic nerve prior to surgery. (A) Demonstrates a normal, flat optic nerve when the patient is in the neutral head position. (B) Picture of the same nerve after 10 minutes of right head turn. The temporal portion of the optic nerve is elevated, with nerve fibre oedema. There is also detention of the vasculature, when compared with (A).
Brain magnetic resonance imaging (MRI) with and without contrast demonstrated a partially empty sella turcica and kinking of the optic nerve sheaths. The MRI also demonstrated that the right styloid process was enlarged at 35 mm, while the left process was 28 mm. There was a focal narrowing between the styloid process and the lateral tubercle of C1, bilaterally. The styloid process-lateral C1 tubercle distance was 3.8 mm on both sides. Magnetic resonance venography showed a dominant right transverse sinus (a normal anatomic variant), and patent dural venous sinuses, without dural venous sinus stenosis. The patient underwent dynamic catheter cerebral angiography and venography to confirm the diagnosis by measuring the pressure gradient across the narrowed segment of the dominant jugular vein. The pressure gradient averaged 4.4 mmHg and it increased to 5.4 mmHg with left lateral rotation of the head (Figure 2). Given that the right transverse sinus was dominant, there were no significant changes with contralateral head rotation. The patient underwent right-sided styloidectomy. Intraoperatively, approximately 20 mm of the styloid was removed (Figure 3). Three months after surgery her vision was 20/20 in both eyes, she denied visual symptoms with head turn or while reading and the tinnitus had subsided. She still had occasional pulsatile headaches. The headaches were less frequent and less severe. OCT demonstrated normalisation of her optic nerves, with RNFL measurements at 99 um and 101 μm, respectively. There was also resolution of the enlarged blind spots and resolution of the retinal vasculature engorgement.
Figure 2.
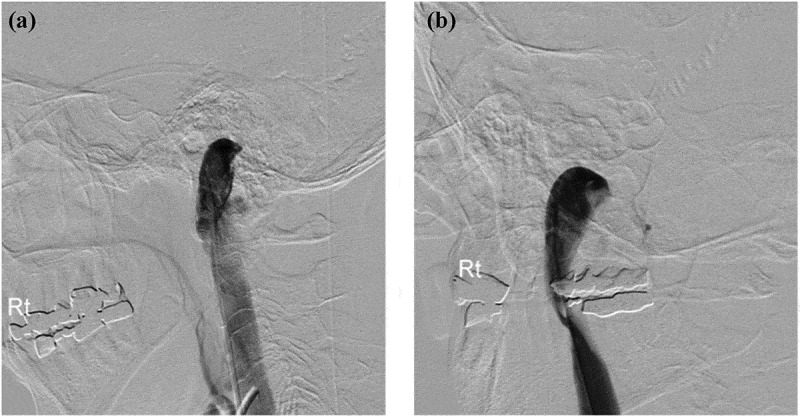
Catheter venography of the right jugular vein, lateral projection.
(A) In neutral position. (B) After left head rotation. The stenosis at the C1 level becomes more pronounced.
Figure 3.
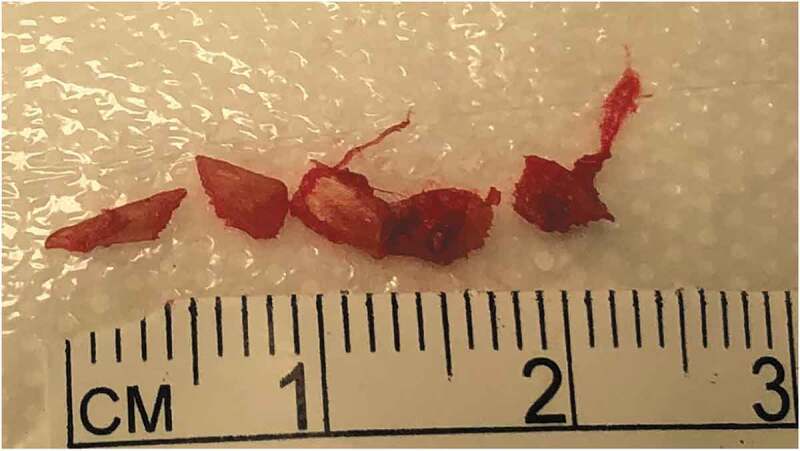
Picture of the intraoperative styloid process resection demonstrating 20 mm of bone removal.
Discussion
We present a case of secondary intracranial hypertension due to styloidogenic jugular venous compression, with positional headache, intermittent face oedema, pulsatile tinnitus, and papilloedema, that all resolved after styloidectomy. Careful interpretation of the MRI of the brain and MR venography are important starting points in the evaluation of styloidogenic jugular venous compression. These studies are needed to exclude the presence of transverse venous sinus stenosis (a far more common cause of IIH) and to evaluate for jugular venous compression between the styloid process and the lateral tubercle of C1. A computed tomography study of the temporal bones can also be useful in measuring the styloid process-lateral C1 tubercle distance, which has been reported to be shorter in this subset of patients, and averages 2.9 mm, compared with 9.9 mm in asymptomatic controls.2 A dynamic MR venogram can demonstrate any stenosis when the head is rotated or extended prior to proceeding with the catheter angiography. Dynamic catheter angiography/venography is the gold standard diagnostic study, as it can demonstrate the presence of a significant gradient across the jugular stenosis, which increased with head rotation.2 The present case provides better documentation in agreement with previous reports that suggest that styloidectomy is the treatment of choice as most of the patients had improvement or resolution of their symptoms after surgery (16/17). Anticoagulation seems to be least likely method of therapy with 2 out of 5 patients having improvement or resolutions reported (see Table 1).
Table 1.
Summary of literature reports of patients with idiopathic intracranial hypertension-like symptoms and findings due to styloidogenic jugular venous compression
| Patient no. | Authors | Gender | Age in years |
BMI (kg/m2) | Symptoms | Positional symptoms |
Side | Length of styloid process in mm |
Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Dashti et al. 20128 | NR | NR | NR | NR | NR | NR | NR | Styloidectomy | Resolved |
| 2 | Dashti et al. 20128 | NR | NR | NR | NR | NR | NR | NR | Styloidectomy | Resolved |
| 3 to 14 | Higgins et al. 201614 | NR | NR | NR | NR | NR | NR | NR | Styloidectomy | Improved or resolved |
| 15 | Zhao et al. 20192 | M | 23 | 23.0 | Headache | Yes | R | 42 | Styloidectomy | Improved |
| 16 | Zhao et al. 20192 | F | 30 | 22.3 | Blurry Vision | Yes | R | 20 | Styloidectomy | Resolved |
| 17 | Zhao et al. 20192 | M | 59 | 29.9 | Blurry vision | Yes | R | 17 | Styloidectomy | Improved |
| 18 | Zhao et al. 20192 | F | 44 | 23.4 | Headache | Yes | R | 11 | Styloidectomy | Improved |
| 19 | Zhao et al. 20192 | M | 51 | 42.9 | Blurry Vision | NR | L | 15 | Styloidectomy | resolved |
| 20 | Zhao et al. 20192 | M | 38 | 26.3 | Blurry Vision | Yes | R | 20 | Styloidectomy | No change |
| 21 | Zhao et al. 20192 | M | 32 | 23.5 | Headache | Yes | R | 20 | Styloidectomy | Improved |
| 22 | Zhao et al. 20192 | F | 21 | 26.7 | Blurry Vision | Yes | L | 24 | Styloidectomy | Improved; recurred in 6 months |
| 23 | Zhao et al. 20192 | M | 21 | 24.0 | Headache | NR | L | NR | Styloidectomy | Improved |
| 24 | Zhao et al. 20192 | M | 39 | NR | Headache | NR | R | 15 | Jugular stent | Resolved |
| 25 | Zhao et al. 20192 | M | 15 | NR | Headache; left transverse sinus thrombosis | NR | L | NR | Anticoagulation | Improved |
| 26 | Li et al. 201911 | F | 65 | NR | Headache, tinnitus, blurry vision | No | Bilateral | NR | Anticoagulation | No change |
| 27 | Li et al. 201911 | M | 58 | NR | Headache | No | Bilateral | NR | Anticoagulation | No change |
| 28 | Li et al. 201911 | F | 61 | NR | Insomnia | NR | Bilateral | NR | Anticoagulation | Improved |
| 29 | Li et al. 201911 | M | 60 | NR | Tinnitus | Yes | L | NR | Jugular stent | Improved, recurred in 20 days |
| 30 | Li et al. 201911 | M | 49 | NR | Intermittent dizziness | No | Bilateral | NR | Styloidectomy | Resolved |
| 31 | Pokeerbux et al. 202010 | M | 19 | NR | Facial oedema and headache | Yes | L | 35 | Anticoagulation | NR |
| 32 | Mooney et al. 202012 | M | 12 | NR | Headache, nausea, vomiting | Yes | Bilateral | NR | Right Styloidectomy | Resolved |
| 33 | Current patient | F | 69 | 24.0 | Headache, tinnitus, blurry vision, face oedema | Yes | R | 35 | Styloidectomy | Resolved |
BMI = Body mass index
F = Female
L = Left
M = Male
NR = Not reported
R = Right
This case represents the 33rd reported case since 2012 of patients with IIH-like symptoms and findings due to styloidogenic jugular venous compression (Table 1).2,10−12,8,10−12,14 Our patient had a dominant right venous system and developed compression on the right side. She had more extensive symptomatology and documentation of retinal and vascular changes. Neuro-ophthalmological follow-up demonstrated visual field changes compatible with the diagnosis, which recovered completely after surgery, without needing acetazolamide or other conventional IIH therapy. The patient is also the first in which resolution of the papilloedema has been noticed after styloidectomy. Her right-side dominance may explain the reason for her recovery with unilateral surgery. Our patient had persistent pulsatile headaches after surgery, which is common (up to 60%) in IIH patients, unrelated to persistent intracranial hypertension.16
Conclusion
Understanding this new pathophysiology of secondary intracranial hypertension due to styloidogenic jugular compression, in patients with positional symptoms, can improve neuro-ophthalmological treatment and outcome in cases of jugular venous compression.
Funding Statement
This work was partially supported by the Pan-American Ophthalmological Foundation (PAOO) and the Retina Research Foundation (RRF) (2019 Gillingham Grant). The funding bodies did not have any role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Declaration of interest statement
The authors report no conflicts of interest.
References
- 1.Friedman DI, Liu GT, Digre KB.. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81(13):1159–1165. doi: 10.1212/WNL.0b013e3182a55f17. [DOI] [PubMed] [Google Scholar]
- 2.Zhao X, Cavallo C, Hlubek RJ, et al. Styloidogenic jugular venous compression syndrome: clinical features and case series. Oper Neurosurg. 2019;17(6):554–561. doi: 10.1093/ons/opz012. [DOI] [PubMed] [Google Scholar]
- 3.Eagle WW. Elongated styloid processes: report of two cases. Arch Otolaryngol. 1937;25(5):584–587. doi: 10.1001/archotol.1937.00650010656008. [DOI] [Google Scholar]
- 4.Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: A comprehensive review. Clin Neurol Neurosurg. 2017;159(April):34–38. doi: 10.1016/j.clineuro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 5.Costantinides F, Vidoni G, Bodin C, Di Lenarda R. Eagle’s syndrome: signs and symptoms. CRANIO®. 2013;31(1):56–60. doi: 10.1179/crn.2013.008. [DOI] [PubMed] [Google Scholar]
- 6.Chuang WC, Short JH, McKinney AM, Anker L, Knoll B, McKinney ZJ. Reversible left hemispheric ischemia secondary to carotid compression in Eagle syndrome: surgical and CT angiographic correlation. AJNR Am J Neuroradiol. 2007;28:143–145. [PMC free article] [PubMed] [Google Scholar]
- 7.Kaufman SM, Elzay RP, Irish EF. Styloid process variation: radiologic and clinical study. Arch Otolaryngol. 1970;91(5):460–463. doi: 10.1001/archotol.1970.00770040654013. [DOI] [PubMed] [Google Scholar]
- 8.Dashti SR, Nakaji P, Hu YC, et al. Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report. Neurosurgery. 2012;70(3):783. doi: 10.1227/NEU.0b013e3182333859. [DOI] [PubMed] [Google Scholar]
- 9.Lehrman JN, Narayanan M, Cavallo C. et al. Evaluation of abnormal styloid anatomy as a cause of internal jugular vein compression using a 3D-printed model: a laboratory investigation. J Clin Neurosci Off J Neurosurg Soc Australas. 2020;72:386–391. doi: 10.1016/j.jocn.2019.11.048. [DOI] [PubMed] [Google Scholar]
- 10.Pokeerbux MR, Delmaire C, Morell-dubois S, Demondion X, Lambert M. Styloidogenic compression of the internal jugular vein, a new venous entrapment syndrome? Vasc Med (United Kingdom). 2020;25(4):378–380. doi: 10.1177/1358863X20902842. [DOI] [PubMed] [Google Scholar]
- 11.Li M, Sun Y, Chan CC, Fan C, Ji X, Meng R. Internal jugular vein stenosis associated with elongated styloid process: five case reports and literature review. BMC Neurol. 2019;19(1):1–8. doi: 10.1186/s12883-019-1344-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mooney J, Lepard J, Akbari SHA, Johnston JM. Styloidogenic jugular venous compression syndrome: a case report and review of the literature. Child’s Nerv Syst. 2020;36:3135–3139. doi: 10.1007/s00381-020-04622-6. [DOI] [PubMed] [Google Scholar]
- 13.Zhang FL, Zhou HW, Guo ZN, Yang Y. Eagle syndrome as a cause of cerebral venous sinus thrombosis. Can J Neurol Sci. 2019;46(3):344–345. doi: 10.1017/cjn.2019.17. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JN, Garnett MR, Pickard JD, Axon PR. An evaluation of styloidectomy as an adjunct or alternative to jugular stenting in idiopathic intracranial hypertension and disturbances of cranial venous outflow. J Neurol Surgery, Part B Skull Base. 2017;78(2):158–163. doi: 10.1055/s-0036-1594238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riley DS, Barber MS, Kienle GS. et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218–235. doi: 10.1016/j.jclinepi.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 16.Friedman DI, Quiros PA, Subramanian PS, et al. Headache in idiopathic intracranial hypertension: findings from the idiopathic intracranial hypertension treatment trial. Headache. 2017;57(8):1195–1205. doi: 10.1111/head.13153. [DOI] [PMC free article] [PubMed] [Google Scholar]


