Abstract
Objectives
The predictive accuracy and clinical role of the focused assessment with sonography for trauma (FAST) exam in pediatric blunt abdominal trauma are uncertain. This study investigates the performance of the emergency department (ED) FAST exam to predict early surgical intervention and subsequent free fluid (FF) in pediatric trauma patients.
Methods
Pediatric level 1 trauma patients ages 0 to 15 years with blunt torso trauma at a single trauma center were retrospectively reviewed. After stratification by initial hemodynamic (HD) instability, the association of a positive FAST with (1) early surgical intervention, defined as operative management (laparotomy or open pericardial window) or angiography within 4 hours of ED arrival and (2) presence of FF during early surgical intervention was determined.
Results
Among 508 salvageable pediatric trauma patients with an interpreted FAST exam, 35 (6.9%) had HD instability and 98 (19.3%) were FAST positive. A total of 42 of 508 (8.3%) patients required early surgical intervention, and the sensitivity and specificity of FAST predicting early surgical intervention were 59.5% and 84.3%, respectively. The specificity and positive predictive value of FF during early surgical intervention in FAST‐positive HD unstable patients increased from 50% and 90.9% at 4 hours after ED arrival to 100% and 100% at 2 hours after ED arrival, respectively.
Conclusions
In this large series of injured children, a positive FAST exam improves the ability to predict the need for early surgical intervention, and accuracy is greater for FF in HD unstable patients 2 hours after arrival to the ED.
Keywords: abdominal/gastrointestinal, angiography, blunt injury, FAST exam, focused assessment with sonography for trauma, hypotension, laparotomy, pediatric emergency medicine, pediatric resuscitation, pediatric trauma, pediatrics, pericardiostomy, traumatic brain injury, therapeutic embolization, ultrasound
1. INTRODUCTION
1.1. Background
Pediatric trauma is the leading cause of death for children in the United States. 1 , 2 Blunt trauma accounts for most pediatric trauma, with intraabdominal injury (IAI) found in approximately 6% of pediatric blunt trauma patients. 3 The role of the focused assessment with sonography for trauma (FAST) exam in pediatric patients with blunt abdominal trauma has been considered for over 2 decades. Prior pediatric studies have examined the accuracy of the abdominal FAST exam compared to abdominal computerized tomography (CT) scan 4 , 5 , 6 and utility of the FAST exam in directing the use of CT imaging 7 , 8 in order to avoid radiation. However, these studies have shown that the FAST exam has poor sensitivity in detecting pediatric intraabdominal injuries. 4 , 5 , 6 , 7 , 9 In 2017, a randomized control trial of 925 children showed no significant difference in length of emergency department stay, number of CT scans performed, or missed intraabdominal injury when an abdominal FAST exam was performed on hemodynamically (HD) stable children with blunt abdominal trauma. 10 A 2019 retrospective study with quality assessment of FAST exam in a cloud‐based video storage system compared to the gold standard of CT scan showed a "concerning FAST exam" had a sensitivity of 61.5% and a specificity of 99% in detecting IAI that required operative intervention or admission to the hospital trauma service. 11 The lack of sonographic free fluid (FF) despite IAI in children leads to poor sensitivity but improved specificity of FAST in detecting IAI. However, rather than ruling out the need for CT imaging, the pediatric FAST can be meaningful in determining operative management in consultation with a surgeon, particularly in cases of HD instability refractory to transfusion. 12
1.2. Importance
Few studies have examined the FAST exam as a predictor of the need for early surgical intervention. 13 , 14 , 15 , 16 , 17 Also, few studies have examined how the diagnostic accuracy of FAST might vary with HD instability in a large series of pediatric patients. The latter consideration is particularly important because early ultrasound results on arrival to the ED may potentially be used to accelerate care in unstable patients.
1.3. Goals of this investigation
In this study we sought to determine the ability of early FAST ultrasound to identify injured children in need of early surgical intervention. Our hypothesis was that a positive FAST exam in hemodynamically unstable children leads to early surgical intervention. The primary outcome is the accuracy of the FAST exam in predicting early surgical intervention. The secondary outcomes are the accuracy of the FAST exam in predicting subsequent gross FF in patients who received early surgical intervention at both 2 and 4 hours after arrival to the ED.
2. METHODS
2.1. Study design and setting
We conducted a retrospective study of pediatric level 1 blunt trauma activations. This study was approved by the University of Texas Health Science Center at Houston Institutional Review Board. The study occurred at Memorial Hermann‐Texas Medical Center, a level 1 trauma center for both pediatric and adult patients in Houston, Texas. The pediatric ED is staffed by board‐certified pediatric emergency physicians and provides care for 18,000 pediatric patients annually, including approximately 225 pediatric trauma activations. Care for pediatric trauma patients is provided jointly by pediatric emergency physicians and trauma surgeons.
2.2. Selection of participants
The study population included children age 0 to 15 years with blunt abdominal trauma who were classified as a level 1 trauma activation receiving care from March 1, 2012 to June 30, 2018. We excluded patients with penetrating trauma. This time interval was chosen based on availability of data in the electronic medical record (EMR) to perform this analysis. Per local practice preference, trauma patients over 15 years are managed per adult trauma guidelines in the adult trauma center.
2.3. Measures—FAST ultrasonography
All eligible children underwent a "FAST" ultrasonography exam per standard pediatric trauma care practices. Attending pediatric emergency physician interpretation of the FAST exam was recorded in the trauma registry. We combined data from the institution's trauma registry with data manually abstracted from the EMR. The data included the FAST exam outcome, method of arrival, ED records, consultative reports, death summaries, CT scan results, CT angiography (CTA) results, operative report, and interventional radiology (IR) report.
2.4. Outcomes
The FAST exam interpretation documented in the trauma registry was used. For this study, we classified indeterminate exams as positive.
Outcome measures were early surgical intervention, FF, embolization, non‐survivable traumatic brain injury (TBI) and mortality. A patient was considered to have a non‐survivable TBI if neurosurgical consultation deemed the patient moribund and no neurosurgical intervention was performed.
We classified patients as hemodynamically unstable if they were hypotensive at triage, based upon systolic blood pressures below the age‐specific fifth percentile according to the American Heart Association Pediatric Advanced Life Support Guidelines. 18
Early surgical intervention is defined as operative management (laparotomy or open pericardial window) or angiography within 4 hours of ED arrival. The time interval of 4 hours was chosen a priori with the rationale that as the time interval increases more factors exist that influence the decision for early surgical intervention, yet with a shorter time window, fewer patients have early surgical intervention. Cases of early surgical intervention were reviewed to determine if gross FF was present.
Two ultrasound fellowship‐trained emergency medicine attending physicians (Richard Gordon and Sara K. Miller) independently performed blinded reviews of operative reports for each patient. In instances where the reviewers disagreed regarding classification, a third reviewer, an attending pediatric surgeon (Myron Allukian), reviewed the case to determine a final classification. The case was considered positive for FF if the operative report indicated gross FF was present upon entry into the peritoneum or pericardial space. A CTA was considered a true positive if a blush was present on angiography necessitating an embolization performed by IR.
2.5. Data analysis
We compared demographics, clinical characteristics, interventions, and outcomes including age, sex, race, mechanism of injury, injury severity score (ISS), 19 ED length of stay, transfusion of blood products in 24 hours, and death between FAST‐positive and FAST‐negative cases. We compared ordinal variables with the Wilcoxon rank‐sum test, categorical variables with Pearson's chi‐square, and continuous variables with Student's t test. We determined inter‐agreement between blinded reviewer classification of FF using kappa statistics.
We assessed FAST accuracy for prediction of early surgical intervention and for the presence of gross FF, calculating sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), negative likelihood ratio, positive likelihood ratio, and area under the receiver operating characteristics curve. We carried out a sensitivity analysis reclassifying indeterminate FAST exams as negative exams.
We did not carry out power calculations for sample size as we sought to use all available clinical data. Data were collected and managed using REDCap electronic data capture tools. We analyzed the data using Stata IC/15 for Windows, StataCorp LLC, College Station, Texas, USA.
The Bottom Line.
In a retrospective study of 508 pediatric level 1 trauma patients ages 0 to 15 years with blunt trauma presenting to a single trauma center, the sensitivity and specificity of focused assessment with sonography for trauma (FAST) in predicting early surgical intervention were 59.5% and 84.3%, respectively. These results suggest that a positive FAST improves the ability to predict the need for early surgical intervention in injured children.
3. RESULTS
3.1. Characteristics of study participants
A FAST exam was documented in 564 of 667 (84%) patients and an interpretation was present for 560 of 564 (99.3%); the baseline characteristics of these are summarized in Table 1. There were 107 pediatric blunt abdominal trauma patients who did not have a FAST exam both performed and interpretation documented and therefore were excluded from this analysis. The median age of FAST‐positive patients was 10 years whereas median age of FAST‐negative patients was 8 years. Notably, the FAST‐positive patients had a significantly higher ISS, ED length of stay, transfusion of blood products in 24 hours, and deaths compared to FAST‐negative patients. In total, 42 out of 560 (7.5%) patients had early surgical intervention, of whom 14 of 42 (33.3%) were HD unstable and 28 of 42 (66.7%) were HD stable (Figure 1). Fifty‐two patients had unsuccessful cardiopulmonary resuscitation on arrival or had a non‐survivable TBI and were considered unsalvageable. Time to early surgical intervention in this study was dichotomized at a 4‐hour threshold; however, 17 of 42 (40.5%) of our patients had early surgical intervention within 1 hour. By 2 hours after arrival to the ED, 31 of 42 (73.8%) patients had early surgical intervention. Ultimately, early surgical intervention was required in 42 of 508 (8.3%) salvageable patients with an interpreted FAST exam. Among pediatric blunt abdominal trauma patients without a FAST exam performed, there was 1 patient (1.0%) of 103 who had early surgical intervention. Four patients had a FAST exam that was documented but not interpreted.
TABLE 1.
Baseline characteristics of pediatric level 1 blunt trauma patients from 2012 to 2018, stratified by FAST results
| FAST positive (N=129) | FAST negative (N=431) | P value | |
|---|---|---|---|
| Demographics | |||
| Age, median (IQR) a | 10 (5‐13) | 8 (4‐13) | 0.15 |
| Sex b | 0.99 | ||
| Male, N (%) | 80 (62.0) | 267 (62.0) | |
| Female, N (%) | 49 (38.0) | 164 (38.0) | |
| Race/ethnicity b | 0.49 | ||
| White/non‐Hispanic, N (%) | 43 (33.3) | 145 (33.6) | |
| Hispanic, N (%) | 41 (31.8) | 111 (25.8) | |
| Black, N (%) | 30 (23.3) | 104 (24.1) | |
| Asian, N (%) | 4 (3.1) | 9 (2.1) | |
| Other, N (%) | 10 (7.8) | 56 (13.0) | |
| Missing, N (%) | 1 (0.8) | 6 (1.4) | |
| Clinical characteristics | |||
| Mechanism of injury b | |||
| Motor vehicle collision, N (%) | 69 (53.1) | 201 (45.7) | 0.17 |
| All‐terrain vehicle, N (%) | 11 (8.5) | 39 (8.9) | 0.86 |
| Pedestrian hit by vehicle, N (%) | 26 (20.0) | 66 (15.0) | 0.19 |
| Bicycle hit by vehicle, N (%) | 6 (4.6) | 13 (3.0) | 0.37 |
| Fall, N (%) | 9 (6.9) | 64 (14.5) | 0.02 |
| Other, N (%) | 9 (6.9) | 57 (13.0) | 0.053 |
| Injury severity score, mean (SD) c | 31.6 (16.7) | 19.3 (13.1) | <.001 |
| HD stability b | <.001 | ||
| Stable, N (%) | 93 (72.1) | 403 (93.5) | |
| Unstable, N (%) | 36 (27.9) | 28 (6.5) | |
| Interventions | |||
| Transfused blood products < 24 hours from arrival b | <.001 | ||
| Yes, N (%) | 71 (55.0) | 124 (28.8) | |
| No, N (%) | 58 (45.0) | 307 (71.2) | |
| CT chest b | 0.009 | ||
| Abnormal, N (%) | 68 (52.7) | 196 (45.5) | |
| Normal, N (%) | 13 (10.1) | 87 (20.2) | |
| Not performed, N (%) | 48 (37.2) | 148 (34.3) | |
| CT abdomen/pelvis b | <.001 | ||
| Abnormal, N (%) | 74 (57.4) | 105 (24.4) | |
| Normal, N (%) | 24 (18.6) | 249 (57.8) | |
| Not performed, N (%) | 31 (24.0) | 77 (17.9) | |
| Emergent angiogram performed, N (%) b | 3 (2.3) | 2 (0.5) | 0.049 |
| Emergent embolization performed, N (%) b | 3 (2.3) | 0 | 0.002 |
| Exploratory laparotomy performed, N (%) b | 24 (18.6) | 15 (3.5) | <0.001 |
| Outcomes | |||
| ED length of stay, mins (SD) c | 112 (89) | 153 (107) | <.001 |
| Hospital length of stay, days (SD) c | 8.6 (9.9) | 7.0 (7.6) | 0.051 |
| Hospital discharge b | <.001 | ||
| Dead, N (%) | 44 (34.1) | 41 (9.5) | |
| Alive, N (%) | 85 (65.9) | 390 (90.5) |
Abbreviations: CT, computed tomography; ED, emergency department; FAST, focused assessment with sonography for trauma; HD, hemodynamic; IQR, interquartile range; N, number; SD, standard deviation.
Differences assessed by the Mann‐Whitney test.
Differences assessed by the chi‐square test.
Differences assessed Student's t test.
FIGURE 1.
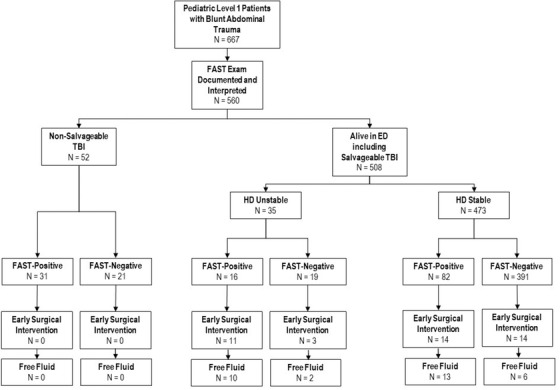
Outcomes of patients in the study
Abbreviations: ED, emergency department; FAST, focused assessment with sonography for trauma; HD, hemodynamic; TBI, traumatic brain injury
3.2. Main results
The performance of the FAST exam was compared to the need for early surgical intervention among the entire cohort. Of 508 salvageable, living patients, 473 of 508 (93.1%) were HD stable and 35 of 508 (6.9%) were HD unstable. Among both unstable and stable salvageable trauma patients, FAST was positive in 98 of 508 (19.3%), and early surgical intervention was required in 25 of 98 (25.5%) (sensitivity 59.5%, specificity 84.3%) (Table 2). Among HD stable patients, FAST was positive in 82 of 473 (17.3%), and early surgical intervention was required in 14 of 82 (17.1%) (sensitivity 50.0%, specificity 84.7%) whereas in HD unstable patients, FAST was positive in 16 of 35 (45.7%), and early surgical intervention was required in 11 of 16 (68.8%) (sensitivity 78.6%, specificity 76.2%). Of the 5 other FAST‐positive unstable patients who did not have early surgical intervention, 3 ultimately had operative intervention for intraabdominal injuries later in their course of care, 1 was managed non‐operatively after hypotension responded to blood transfusion, and 1 had a grade IV liver laceration managed without operative intervention, as HD instability was attributed to TBI (Table 3). Overall 68.8% (11 of 16) of FAST‐positive, unstable patients underwent early surgical intervention versus 15.8% (3 of 19) of FAST‐negative unstable patients (P = 0.001). Three of the 16 FAST‐negative unstable patients without early surgical intervention required intervention outside the 4‐hour window.
TABLE 2.
Performance of the FAST exam for early surgical intervention relative to triage HD status for entire cohort
| N | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | LR+ | LR‐ | AUC | |
| Time to ESI ≤ 4 hours | 508 | 59.5 (43.3–74.4) | 84.3 (80.7–87.5) | 25.5 (19.8–32.2) | 95.9 (94.1–97.1) | 3.8 | 0.5 | 0.72 |
| HD unstable | 35 | 78.6 (49.2–95.3) | 76.2 (52.8–91.8) | 68.8 (41.3–89.0) | 84.2 (60.4–96.6) | 3.3 | 0.3 | 0.77 |
| HD stable | 473 | 50.0 (30.6–69.4) | 84.7 (81.0–87.9) | 17.1 (9.7–27.0) | 96.4 (94.1–98.0) | 3.3 | 0.6 | 0.67 |
Abbreviations: AUC, area under the receiver operating characteristics curve; CI, confidence interval; ESI, early surgical intervention; FAST, focused assessment with sonography for trauma; HD, hemodynamic; LR, likelihood ratio; N, number; NPV, negative predictive value; PPV, positive predictive value.
TABLE 3.
Course of FAST‐positive hemodynamically unstable salvageable patients without early surgical intervention
| Case | Age (years) | Sex | Triage SBP | Mechanism | ISS | Blood transfusion in < 24 hours | CT performed | Clinical course |
|---|---|---|---|---|---|---|---|---|
| 1 | 15 | M | 81 | MVC with ejection | 29 | No | Yes | Grade IV liver laceration; hypotension attributed to TBI; managed medically in the PICU for 6 days and discharged home |
| 2 | 14 | M | 70 | ATV struck by 18‐wheeler truck | 43 | Yes | Yes | Grade V liver laceration and extensive hemoperitoneum on abdomen/pelvis CT; femur fracture and pulseless, open tibia and fibula fracture; fracture reduction in the ED and admitted to PICU; taken to OR on hospital day 3 for laparotomy due to abdominal compartment syndrome, bile leak, and liver laceration; patient discharged home on hospital day 19 |
| 3 | 11 | M | 88 | MVC | 5 | No | Yes | Transferred with outside hospital abdomen/pelvis CT showing small fluid in pericolic gutters without evidence of solid organ injury; SBP stabilized in the ED; admitted 2 days, for serial abdominal exams and doing well; discharged home. Returned to ED a week later with abdominal pain; had small bowel resection and ileostomy |
| 4 | 13 | F | 75 | MVC | 30 | Yes | Yes | Hypotension responded to fluids in the ED, so abdomen/pelvis CT done and showed complex liver laceration; blood pressures stabilized; admitted to PICU and discharged home on hospital day 8 |
| 5 | 2 | F | 61 | Pedestrian struck by vehicle | 45 | Yes | Yes | Grade V liver and grade I splenic lacerations with large hemoperitoneum on abdomen/pelvis CT; required blood products in PICU and taken for exploratory laparotomy on hospital day 15 for liver laceration with bile leak; admitted a total of 43 days, then discharged home |
Abbreviations: ATV, all‐terrain vehicle; CT, computed tomography; ED, emergency department; FAST, focused assessment with sonography for trauma; ISS, injury severity score; MVC, motor vehicle collision; OR, operating room; PICU, pediatric intensive care unit; SBP, systolic blood pressure; TBI, traumatic brain injury.
3.3. Secondary results and sensitivity analyses
The accuracy of the FAST exam was also determined by the presence of FF in the 42 patients who received early surgical intervention and upon adjudicated review the sensitivity and specificity of a positive FAST for FF during early surgical intervention was 74.2% and 81.8%, respectively (Table 4). FF was present in 6 of 14 (42.9%) HD stable, FAST‐negative patients versus 13 of 14 (92.9%) HD stable, FAST‐positive patients and 10 of 11 (90.9%) HD unstable, FAST‐positive patients. FF was present in 2 of 3 (66.7%) FAST‐negative unstable patients. The sensitivity and specificity of a positive FAST for FF in HD unstable patients who required early surgical intervention were 83.3% and 50%, respectively. The reviewers performed the adjudication with a high rate of agreement 95.2% (Cohen's kappa [Κ] statistic = 0.88) when assessing for FF.
TABLE 4.
Performance of the FAST exam for FF during early surgical intervention relative to triage HD status
| N | Sensitivity (95% CI) | Specificity (95% CI%) | PPV (95% CI) | NPV (95% CI) | LR+ | LR‐ | AUC | |
| Time to ESI ≤ 4 hours | 42 | 74.2 (55.4–88.1) | 81.8 (48.2–97.7) | 92.0 (74.0–99.0) | 52.9 (27.8–77.0) | 4.1 | 0.3 | 0.8 |
| HD unstable | 14 | 83.3 (51.6–97.9) | 50.0 (1.3–98.7) | 90.9 (58.7–99.8) | 33.3 (0.8–90.6) | 1.7 | 0.3 | 0.7 |
| HD stable | 28 | 68.4 (43.4–87.4) | 88.9 (51.8–99.7) | 92.9 (66.1–99.8) | 57.1 (28.9–82.3) | 6.2 | 0.4 | 0.8 |
| Time to ESI ≤ 2 hours | 31 | 70.8 (48.9–87.4) | 85.7 (42.1–99.6) | 94.4 (72.7–99.9) | 46.2 (19.2–74.9) | 5.0 | 0.3 | 0.8 |
| HD unstable | 11 | 80.0 (44.4–97.5) | 100 (2.5–100) | 100 (63.1–100) | 33.3 (0.8–90.6) | NA | 0.2 | 0.9 |
| HD stable | 20 | 64.3 (35.1–87.2) | 83.3 (35.9–99.6) | 90 (55.5–99.7) | 50 (18.7–81.3) | 3.9 | 0.4 | 0.7 |
Abbreviations: AUC, area under the receiver operating characteristics curve; CI, confidence interval; ESI, early surgical intervention; FAST, focused assessment with sonography for trauma; FF, free fluid; HD, hemodynamic; LR, likelihood ratio; N, number; NA, not applicable; NPV, negative predictive value; PPV, positive predictive value.
The PPV of a positive FAST exam in predicting FF in HD unstable patients and all patients with early surgical intervention was 90.9% and 92%, respectively. Although sample size was limited in FAST‐negative patients who underwent early surgical intervention, the NPV of a negative FAST in predicting FF in HD unstable and all patients was 33.3% and 52.9%, respectively. The specificity and PPV of FF in FAST‐positive HD unstable patients increases from 50% and 90.9% at 4 hours after ED arrival to 100% and 100% at 2 hours after ED arrival, respectively (Table 4). On sensitivity analysis, reclassification of 18 indeterminate cases as FAST‐negative resulted in similar classification accuracy (Table 5).
TABLE 5.
Sensitivity analysis. Performance of the FAST exam for early surgical intervention relative to triage HD status for entire cohort
| N | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | LR+ | LR‐ | AUC | |
|---|---|---|---|---|---|---|---|---|
| Time to ESI ≤ 4 hours | 508 | 54.8 (38.7–70.2) | 87.3 (84.0–90.2) | 28.0 (18.7–39.1) | 95.5 (93.1–97.3) | 4.3 | 0.5 | 0.71 |
| HD unstable | 35 | 78.6 (49.2–95.3) | 76.2 (52.8–91.8) | 68.8 (41.3–89.0) | 84.2 (60.4–96.6) | 3.3 | 0.3 | 0.77 |
| HD stable | 473 | 42.9 (24.5–62.8) | 87.9 (84.5–90.8) | 18.2 (9.8–29.6) | 96.1 (93.7–97.7) | 3.5 | 0.7 | 0.65 |
Note: Indeterminate cases (N = 18) reclassified as negative FAST exam.
Abbreviations: AUC, area under the receiver operating characteristics curve; CI, confidence interval; ESI, early surgical intervention, FAST, focused assessment with sonography for trauma; HD, hemodynamic; LR, likelihood ratio; N, number; NPV, negative predictive value; PPV, positive predictive value.
4. LIMITATIONS
Limitations of our study include its retrospective nature, and therefore it is subject to misclassification bias. Images themselves were infrequently archived and therefore unable to be evaluated for accuracy. Indeterminate FAST exams were considered positive; however, overall there were few indeterminate studies and the 2 patients with an indeterminate FAST who had early surgical exploration and were initially HD stable and became HD unstable had FF on exploration making a FAST‐positive scan plausible. Notably, sensitivity analysis with indeterminates classified as negative yielded a similar performance of the FAST exam. A single FAST result was recorded in the trauma registry and used for this study and the registry does not account for repeat FAST exams as serial exams are not reliably documented in the EMR. Furthermore, the EMR used for this study did not reliably include the location of sonographic FF in FAST positive subjects. Literature suggests that whereas adults are most likely to have FF accumulate in the right upper quadrant, specifically the caudal edge of the liver, 20 serious IAI in pediatric patients may follow a different pattern. Recently published data in children show fluid is more likely to accumulate in the pelvis in FAST‐positive children. 11 , 21 Without this additional descriptive data or archived images for qualitative review, we are unable to evaluate for an association with sonographic FF location that could affect the accuracy of the FAST exam.
For our study, we used triage systolic blood pressure as a marker of HD instability. These pressure parameters were used given the clinical relevance in daily practice. The typical practice in level 1 patients is to perform the FAST exam alongside the primary survey while obtaining triage vital signs; however, patients often may become hypotensive within minutes after the triage vital signs were performed. Given that children are more likely than adults to quickly progress to HD instability despite a previously normotensive blood pressure, identifying patients who became hypotensive before surgical exploration and assessing the HD instability in relation to repeated FAST exams would be informative. Advocating for FAST and re‐FAST protocols with assessments, including emphasis on repeat physical exam to determine decision‐making for the clinical course is supported by the 2020 retrospective study published by Bahrami‐Motlagh et al, which found a sensitivity and specificity of 87% and 77% respectively when using a FAST, re‐FAST, and tenderness protocol. 22 A prospective study is needed to better assess HD instability in relation to the timing of the initial FAST exam as well as how repeat FAST exams can be used to predict early surgical exploration in patients who become hypotensive during the ED stay. Furthermore, a prospective study would allow FAST images themselves to be reviewed for accuracy.
5. DISCUSSION
In this study, we evaluated the ability of FAST to identify pediatric blunt trauma patients needing early surgical intervention. We found that although FAST demonstrated some accuracy in predicting early surgical intervention, sensitivity was the highest for patients presenting with HD instability. Additionally, early surgical intervention had improved accuracy for predicting FF during early surgical intervention, particularly in unstable patients at 2 hours after arrival to the ED.
Our findings are in contrast to the findings by Scaife and colleagues. 7 In their prospective trial with surgeons trained to perform the FAST exam, they rarely had a true positive FAST exam and concluded that the exam did not influence management. In their study, only 1 hypotensive patient had operative intervention as a result of a positive FAST exam with hemoperitoneum before an abdominal CT was performed whereas 11 FAST‐positive, HD unstable patients in our study required early surgical intervention and over half of these had surgical intervention without a prior CT scan. Our data support that patients who are FAST positive have higher ISS and are more likely to be HD unstable. Although all level 1 blunt trauma activations at our institution are to receive FAST exams on arrival to the ED, the rates of early surgical intervention differed among level 1 traumas with the FAST exam (7.5%, 42 of 560) compared to those without the FAST exam (1.0%, 1 of 103). These data suggest that there may be other criteria, such as vital signs, exam findings, trauma type (ie, apparent isolated trauma), which create a bias to perform the FAST exam. Nonetheless, our results suggest that a positive FAST exam does affect clinical decision‐making in pediatric blunt trauma patients.
Another recent, prospective, multicenter study at 14 level 1 pediatric trauma centers found the opposite, that the FAST exam in pediatric patients had low sensitivity for detecting IAI and did not affect clinical decision‐making. 23 However, the majority of the patients in the study were level 2 trauma patients, and the patients who underwent emergent intervention had normal blood pressure for age, and therefore HD unstable patients were not evaluated. 23 Another retrospective study had only 2 hypotensive patients but did find that ultrasound proved to be effective in 97% (34 of 35) of patients in establishing a diagnosis and leading to appropriate surgical decision‐making. 24 In a prospective study of the FAST exam from 2001, Holmes et al 15 reported the sensitivity of the FAST exam was 100% in HD unstable pediatric patients in predicting intraabdominal fluid. All 7 FAST‐positive HD unstable patients had laparotomy and 6 of 6 FAST‐negative HD unstable patients were observed. However, this study has some limitations. First, only 13 patients had HD instability; second, pericardiotomy and angiography were not included as exploration; and lastly, radiology department sonographers conducted the FAST exam, not physicians already at the bedside caring for patients in the ED. 15 Using radiology‐trained sonographers as some studies have is not practical in most EDs with critically ill patients because radiology‐trained sonographers are not otherwise immediately available or involved in the care of the patient to intervene.
Our study included more HD unstable patients than prior pediatric studies with our overall sensitivity and specificity of the FAST exam in predicting FF during early surgical intervention at 4 hours from arrival to the ED similar to a multicenter retrospective study published in 2019 by Rowell et al, which showed that a FAST‐positive exam had a sensitivity and specificity of 62% and 83% respectively for a therapeutic laparotomy among 317 hypotensive adults taken for an abdominal operation with a definitive procedure within 6 hours. 17 However, compared to Rowell et al, our study shows improved sensitivity and specificity of 80% and 100% respectively of a positive FAST for FF during early surgical intervention among 11 salvageable unstable children at 2 hours from arrival to the ED.
We demonstrate findings consistent with Riera et al as hemodynamically unstable patients had a higher incidence of both positive FAST or "concerning FAST" exams and abnormal abdomen/pelvis CT imaging. 11 In our study the FAST exam did not perform as well in ruling out FF in HD unstable patients, as shown by the lower NPV compared to the PPV, although the calculation of the NPV was limited by the relatively low number of unstable patients with negative FAST who underwent early surgical intervention. This may reflect the known limitations of ultrasound in detecting retroperitoneal hemorrhage that could result in a HD unstable patient. Notably, among only 3 of the HD unstable patients with negative FAST exams who did not undergo early surgical intervention required intra‐abdominal intervention outside the 4‐hour window. Collectively, these data would suggest that a positive FAST in a HD unstable patient adds value in predicting which patients should undergo early surgical intervention versus those patients who may benefit from conservative management.
We propose that there is clinical relevance in a positive FAST exam in pediatric patients with blunt abdominal trauma, particularly in hemodynamically unstable patients in predicting not only who will require early surgical intervention but also for whom FF will be present. Therefore, the FAST exam should continue to be taught and used in clinical practice. Future research should focus on prospective evaluation of HD unstable patients with both serial FAST exams and serial evaluation of HD status in relation to early surgical intervention. Qualitative assessment of FAST exams, including location of sonographic FF, probe type, and quantity of fluid, should be recorded for analysis in future studies.
In conclusion, our longitudinal retrospective study demonstrates that a positive FAST exam enhances the ability to predict both early surgical intervention and FF in pediatric patients with blunt abdominal trauma, particularly FF at 2 hours after arrival to the ED in those who are HD unstable.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Megan K. Long, Marylou Cardenas‐Turanzas, Henry E. Wang, Irma T. Ugalde, Myron Allukian, Hannah E. Smith designed the study. Megan K. Long, Mohammed K. Vohra, Pablo D. Vega Parra, Sara K. Miller, Richard Gordon, Myron Allukian and Hannah E. Smith acquired the data. Megan K. Long, Henry E. Wang, Pablo D. Vega Parra, Sara K. Miller, Richard Gordon, Myron Allukian, Hannah E. Smith analyzed and interpreted the data. Megan K. Long and Hannah E. Smith drafted the manuscript. Megan K. Long, Henry E. Wang, Austin Bonnette, Emily Ayub, Marylou Cardenas‐Turanzas, Richard Gordon, Irma T. Ugalde, Hannah E. Smith revised the manuscript. Henry E. Wang, Austin Bonnette, Marylou Cardenas‐Turanzas provided statistical expertise. Henry E. Wang provided administrative support. Hannah E. Smith supervised the study.
ACKNOWLEDGMENTS
None.
Biography
Megan Long, MD, is an Assistant Professor of Pediatric Emergency Medicine at The University of Texas Health Science Center at Houston McGovern Medical School in Houston, Texas, USA.

Long MK, Vohra MK, Bonnette A, et al. Focused assessment with sonography for trauma in predicting early surgical intervention in hemodynamically unstable children with blunt abdominal trauma. JACEP Open. 2022;3:e12650. 10.1002/emp2.12650
Henry Wang is now affiliated with the Department of Emergency Medicine, The Ohio State University, Columbus, OH, USA.
Supervising Editor: Chadd Kraus, DO, DrPH.
Prior Presentations: Pediatric Academic Societies. Virtual Meeting. April 2021.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. Neglect CoCAa , Committee on Injury Vo, and Poison Prevention, Pediatrics CoC. American Academy of Pediatrics. Policy statement—child fatality review. Pediatrics. 2010;126(3):592‐596. [DOI] [PubMed] [Google Scholar]
- 2. (CDC) CfDCaP . Vital signs: unintentional injury deaths among persons aged 0‐19 years—United States, 2000‐2009. MMWR Morb Mortal Wkly Rep. 2012;61:270‐276. [PubMed] [Google Scholar]
- 3. Holmes JF, Lillis K, Monroe D, et al. Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013;62(2):107‐116.e102. [DOI] [PubMed] [Google Scholar]
- 4. Coley BD, Mutabagani KH, Martin LC, et al. Focused abdominal sonography for trauma (FAST) in children with blunt abdominal trauma. J Trauma. 2000;48(5):902‐906. [DOI] [PubMed] [Google Scholar]
- 5. Emery KH, McAneney CM, Racadio JM, Johnson ND, Evora DK, Garcia VF. Absent peritoneal fluid on screening trauma ultrasonography in children: a prospective comparison with computed tomography. J Pediatr Surg. 2001;36(4):565‐569. [DOI] [PubMed] [Google Scholar]
- 6. Mutabagani KH, Coley BD, Zumberge N, et al. Preliminary experience with focused abdominal sonography for trauma (FAST) in children: is it useful?. J Pediatr Surg. 1999;34(1):48‐52. [DOI] [PubMed] [Google Scholar]
- 7. Scaife ER, Rollins MD, Barnhart DC, et al. The role of focused abdominal sonography for trauma (FAST) in pediatric trauma evaluation. J Pediatr Surg. 2013;48(6):1377‐1383. [DOI] [PubMed] [Google Scholar]
- 8. Menaker J, Blumberg S, Wisner DH, et al. Use of the focused assessment with sonography for trauma (FAST) examination and its impact on abdominal computed tomography use in hemodynamically stable children with blunt torso trauma. J Trauma Acute Care Surg. 2014;77(3):427‐432. [DOI] [PubMed] [Google Scholar]
- 9. Taylor GA, Sivit CJ. Posttraumatic peritoneal fluid: is it a reliable indicator of intraabdominal injury in children?. J Pediatr Surg. 1995;30(12):1644‐1648. [DOI] [PubMed] [Google Scholar]
- 10. Holmes JF, Kelley KM, Wootton‐Gorges SL, et al. Effect of abdominal ultrasound on clinical care, outcomes, and resource use among children with blunt torso trauma: a randomized clinical trial. JAMA. 2017;317(22):2290‐2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Riera A, Hayward H, Silva CT, Chen L. Reevaluation of FAST sensitivity in pediatric blunt abdominal trauma patients: should we redefine the qualitative threshold for significant hemoperitoneum?. Pediatr Emerg Care. 2019. [DOI] [PubMed] [Google Scholar]
- 12. Guttman J, Nelson BP. Diagnostic point‐of‐care ultrasound: assessment techniques for the pediatric trauma patient. Pediatr Emerg Med Pract. 2019;16(Suppl):1‐50. [PubMed] [Google Scholar]
- 13. Patel JC, Tepas JJ. The efficacy of focused abdominal sonography for trauma (FAST) as a screening tool in the assessment of injured children. J Pediatr Surg. 1999;34(1):44‐47. [DOI] [PubMed] [Google Scholar]
- 14. Fox JC, Boysen M, Gharahbaghian L, et al. Test characteristics of focused assessment of sonography for trauma for clinically significant abdominal free fluid in pediatric blunt abdominal trauma. Acad Emerg Med. 2011;18(5):477‐482. [DOI] [PubMed] [Google Scholar]
- 15. Holmes JF, Brant WE, Bond WF, Sokolove PE, Kuppermann N. Emergency department ultrasonography in the evaluation of hypotensive and normotensive children with blunt abdominal trauma. J Pediatr Surg. 2001;36(7):968‐973. [DOI] [PubMed] [Google Scholar]
- 16. Dammers D, El Moumni M, Hoogland II, Veeger N, Ter Avest E. Should we perform a FAST exam in haemodynamically stable patients presenting after blunt abdominal injury: a retrospective cohort study. Scand J Trauma Resusc Emerg Med. 2017;25(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rowell SE, Barbosa RR, Holcomb JB, Fox EE, Barton CA, Schreiber MA. The focused assessment with sonography in trauma (FAST) in hypotensive injured patients frequently fails to identify the need for laparotomy: a multi‐institutional pragmatic study. Trauma Surg Acute Care Open. 2019;4(1):e000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: pediatric advanced life support: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S876‐908. [DOI] [PubMed] [Google Scholar]
- 19. Brown JB, Gestring ML, Leeper CM, et al. The value of the injury severity score in pediatric trauma: time for a new definition of severe injury?. J Trauma Acute Care Surg. 2017;82(6):995‐1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lobo V, Hunter‐Behrend M, Cullnan E, et al. Caudal edge of the liver in the right upper quadrant (RUQ) view is the most sensitive area for free fluid on the FAST exam. West J Emerg Med. 2017;18(2):270‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brenkert TE, Adams C, Vieira RL, Rempell RG. Peritoneal fluid localization on FAST examination in the pediatric trauma patient. Am J Emerg Med. 2017;35(10):1497‐1499. [DOI] [PubMed] [Google Scholar]
- 22. Bahrami‐Motlagh H, Hajijoo F, Mirghorbani M, SalevatiPour B, Haghighimorad M. Test characteristics of focused assessment with sonography for trauma (FAST), repeated FAST, and clinical exam in prediction of intra‐abdominal injury in children with blunt trauma. Pediatr Surg Int. 2020;36(10):1227‐1234. [DOI] [PubMed] [Google Scholar]
- 23. Calder BW, Vogel AM, Zhang J, et al. Focused assessment with sonography for trauma in children after blunt abdominal trauma: a multi‐institutional analysis. J Trauma Acute Care Surg. 2017;83(2):218‐224. [DOI] [PubMed] [Google Scholar]
- 24. Retzlaff T, Hirsch W, Till H, Rolle U. Is sonography reliable for the diagnosis of pediatric blunt abdominal trauma?. J Pediatr Surg. 2010;45(5):912‐915. [DOI] [PubMed] [Google Scholar]


