Abstract
Background
The balance between supply and demand for primary health care (PHC) services is one of the main challenges to the health system in Brazil. In this context, the application of planning methods could benefit the decision-making process for human resources organizations. Hence, the objective of this study was to assess the staffing needs for registered nurses (RNs) and licensed practical nurses (LPNs) at PHC services using the WISN method.
Methods
The Workload Indicators of Staffing Need (WISN) methodology was applied at 13 Primary Care Units (PCU) located in the city of São Paulo, Brazil. It included 87 RNs and 174 LPNs, and used data from 2017 to 2019.
Results
The WISN results found that RNs were under high workload pressure at 10 PCUs (77%) in 2017 and 2018, with a decrease to 8 PCUs (61%) in 2019. For LPNs, high workload pressure increased from 2 PCUs (15%) in 2017 to 13 PCUs (100%) in 2018, with a decrease to 11 (85%) in 2019.
Conclusion
The assessment of staffing needs for RNs and LPNs at the PCUs included in the study identified a consistent deficit in the number of professionals, and high workload pressure in most services throughout the study period.
Keywords: Primary health care, Human Resources in Health, Nursing, Health services
Background
Balancing the supply of healthcare professionals against the growing demand of patients is one of the biggest challenges for primary health care (PHC) systems around the world. In this context, the use of workforce planning methods could contribute to the analyses and decision-making process to allocate the right number of professionals in the right place, at the right time, in order to meet the health needs of specific populations.
Health workforce planning is understood as a strategic function and a continuous and iterative process, with investigations and analyses of the quantity and quality of workers, supported by data that reflect both planned and unplanned changes at the various determining levels of supply and demand [1, 2].
Some human resource planning methods, such as the Workload Indicators of Staffing Need (WISN) [3], have been used in different regions of the world, in PHC, hospital, and outpatient services for decision-making and planning at local, regional, and national levels [4]. Studies conducted in urgency and emergency services demonstrated that the WISN tool is simple and easy to use, can measure direct and indirect nursing activities and translate the workload. In addition, it can be used to expand the role of the nursing staff and define strategies to increase the efficiency of units [5].
In Brazil, PHC managers make their staffing decisions based on two criteria: following guiding policies, such as the National Policy for Primary Care (PNAB, acronym in Portuguese) [6], and on professional experience and/or judgment. The end result is a fragile planning for staffing needs, and little optimization of financial resources.
The PNAB establishes the composition of PHC teams, which are composed of a registered nurse (RN), a physician, two licensed practical nurses (LPNs), and a varied number of community health workers (CHW), that are organized geographically covering populations of 2000 to 3500 individuals each, with no overlap or gap between coverage areas. Oral health teams, composed of a dental surgeon and an oral health technician, endemic diseases control agents, and a manager can also be added to PCUs to work alongside PHC teams [6].
The PNAB criteria for staffing PCUs is mainly based on the size of the population covered, and do not consider varying workloads produced by different population profiles, nor different regional and local characteristics that should guide the structuring of services and the organization of work processes [7].
The Brazilian Federal Council of Nursing, through Resolution no. 543 of 2017, [8] has established staffing parameters for different nursing categories and healthcare settings based on the application of the adapted WISN method, as well as the definition of direct care for health service activities, and indirect care for support activities and additional activities [8].
In spite of published resolutions and policies, PHC continues to suffer from a growing gap between the demand for services and the number of professionals available [9]. This situation is fueling a growing debate on the need to expand the scope of practice of PHC nurses to increase universal access to health and improve quality of care [10]. To reach these goals it would be important to combine the efforts of changing the scope of nursing practice and of implementing evidence-based nursing staffing methodologies for PHC.
Hence, the objective of this study was to assess the staffing needs for RNs and LPNs at PHC services using the WISN method.
Methods
Scope and setting
The WISN methodology was applied to two large districts of the city of São Paulo, Brazil, covered by 87 PHC teams distributed across 13 PCUs serving approximately 270 000 individuals. Management of these services is done through a public–private partnership between the Municipal Health Department and the Instituto Israelita de Responsabilidade Social Albert Einstein.
The study included data from 87 RNs and 174 LPNs that were working at the 13 PCUs included in the study between 2017 and 2019.
WISN calculation
The available working time (AWT) was obtained through institutional data provided by the human resources system. The absences on working days related to vacation, sick leave and other leave (including provided trainings) were considered, as well as national and local holidays and long weekends. All nursing professionals were hired to work 8 h per day, 5 days per week.
The time in minutes was converted into hours, and the workload components were defined as proposed by Bonfim et al. [11] This study defined parameters for average times and activities using a work sampling technique, and included 32 613 non-participatory observations of activities performed by nurses working as part of PHC teams in five Brazilian regions. As a result, it made it possible to estimate time patterns for activities that are usually registered in administrative databases, as well as for activities that are not, facilitating the use of human resource planning equations in Brazil [11].
Health Service Activities were considered to be direct care activities, that is, those performed by all nursing professionals in the presence of patients, and that were recorded on a productivity sheet. Support activities and additional activities were considered to be indirect care activities, that is, activities that would benefit patients, but would not require their presence, and usually were not recorded on a productivity sheet. Productivity data were extracted from an administrative PHC database. Vaccination activities were assigned to LPNs, since these tasks are performed by them most of the time, and it was not possible to link individual activity to an individual professional.
For educational groups activities, the number of meetings conducted and not the number of patients attending, was considered. For appointments, home visits, outpatient procedures, monitoring of vital signs, administration of medications, venipuncture, and unscheduled care, the number of services delivered was considered.
For support activities and additional activities, the percentage of work time defined by Bonfim et al. [11] was used.
Data analysis
The available working time (AWT) was calculated according to the WISN manual [3]. To calculate the necessary number of professionals to conduct needed health services, activities were considered to be direct care activities (), and the following equations were used:
i (i = 1, 2, …, n) = workload component, = annual workload, = standard workload (hours), the calculation of indirect care (), which included support activities and additional activities components, used the percentage of participation of nursing professionals, obtained by adding up the percentages of participation of each category, as proposed by Bonfim et al. [11]
The quantity Q for the nursing category being evaluated was calculated by the equation:
The difference between current and required staffing levels can identify under- or overstaffing, while the WISN ratio can evaluate the level of daily work pressure among employees. A WISN ratio greater than 1 indicates a surplus of employees, and a ratio smaller than 1 indicates a shortage of employees. Whenever the ratio is smaller than 1, it indicates that working pressure is high [3].
Ethics approval
The research project was approved by the Research Ethics Committee (protocol CAAE: 23388819.9.0000.0071) according to Resolution 466/12 of the Brazilian National Health Council.
Results
The found AWTs ranged from 1402.48, for RNs in PCU M, to 1804.48, for LPNs in PCU H. There was an increase in other leaves of absence in 2019 because of trainings offered by the organization (Table 1).
Table 1.
Available working time (AWT) of registered nurses and licensed practical nurses in 2017, 2018 and 2019
| Unit | Professional category | Absent days due to holidays in the year | Working days in vacations | Days on leave | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | ||
| PCU A | RN | 17 | 13.5 | 15.5 | 14 | 25 | 17 | 6.6 | 8 | 2.6 |
| LPN | 17 | 13.5 | 15.5 | 15.2 | 23.7 | 13.1 | 7.4 | 14.4 | 6.3 | |
| PCU B | RN | 17 | 13.5 | 15.5 | 10.6 | 17.6 | 16.2 | 2 | 5.2 | 3 |
| LPN | 17 | 13.5 | 15.5 | 18.7 | 33 | 18.8 | 2.4 | 3.6 | 6.3 | |
| PCU C | RN | 17 | 13.5 | 15.5 | 13.1 | 23.8 | 9.4 | 3.9 | 5.8 | 1 |
| LPN | 17 | 13.5 | 15.5 | 18 | 42.6 | 13.4 | 4.4 | 2.3 | 5.1 | |
| PCU D | RN | 17 | 13.5 | 15.5 | 15.3 | 24.2 | 16.3 | 1 | 0 | 2.8 |
| LPN | 17 | 13.5 | 15.5 | 15.3 | 31.3 | 15.8 | 2.1 | 4.2 | 0.9 | |
| PCU E | RN | 17 | 13.5 | 15.5 | 20.9 | 36.7 | 28.6 | 3.6 | 1.5 | 0.6 |
| LPN | 17 | 13.5 | 15.5 | 19.9 | 30.2 | 24 | 2.9 | 5.4 | 1.4 | |
| PCU F | RN | 17 | 13.5 | 15.5 | 12.8 | 29.1 | 12.5 | 4.2 | 4.5 | 2.6 |
| LPN | 17 | 13.5 | 15.5 | 16.8 | 29.9 | 13.2 | 3.9 | 5.5 | 4.4 | |
| PCU G | RN | 17 | 13.5 | 15.5 | 11.2 | 29.2 | 14.4 | 7.4 | 0.4 | 6.6 |
| LPN | 17 | 13.5 | 15.5 | 23.3 | 32.3 | 22 | 2.5 | 4.8 | 17 | |
| PCU H | RN | 17 | 13.5 | 15.5 | 20.8 | 22 | 18.5 | 6.2 | 7.3 | 12.3 |
| LPN | 17 | 13.5 | 15.5 | 18.5 | 31.1 | 12.3 | 3 | 4 | 1.1 | |
| PCU I | RN | 17 | 13.5 | 15.5 | 11.8 | 28.1 | 19.2 | 2.2 | 5.5 | 3.7 |
| LPN | 17 | 13.5 | 15.5 | 17.1 | 26.5 | 10.5 | 2.4 | 4.2 | 9.3 | |
| PCU J | RN | 17 | 13.5 | 15.5 | 17.4 | 21.5 | 15.7 | 4 | 0.6 | 1.3 |
| LPN | 17 | 13.5 | 15.5 | 14.6 | 22.9 | 14.9 | 4.9 | 3.8 | 5.6 | |
| PCU L | RN | 17 | 13.5 | 15.5 | 16.8 | 34 | 15.3 | 4.5 | 5 | 4.2 |
| LPN | 17 | 13.5 | 15.5 | 15.4 | 28.3 | 12.3 | 3.7 | 3.1 | 4.4 | |
| PCU M | RN | 17 | 13.5 | 15.5 | 16.7 | 30.2 | 23.4 | 2.7 | 2.5 | 40.4 |
| LPN | 17 | 13.5 | 15.5 | 15.3 | 22.9 | 35.4 | 2.9 | 2.2 | 3.6 | |
| PCU N | RN | 17 | 13.5 | 15.5 | 10.6 | 18.5 | 14.1 | 3.6 | 0 | 0 |
| LPN | 17 | 13.5 | 15.5 | 20.3 | 26.9 | 11.4 | 1.1 | 5.6 | 5.7 | |
| Unit | Professional category | Absent days due to other leaves in the year | Working hours/day | AWT | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | ||
| PCU A | RN | 6 | 4.5 | 9.2 | 8 | 8 | 8 | 1732 | 1672 | 1726 |
| LPN | 3.6 | 2.7 | 8.2 | 8 | 8 | 8 | 1734 | 1646 | 1735 | |
| PCU B | RN | 4.4 | 8.2 | 22 | 8 | 8 | 8 | 1808 | 1724 | 1626 |
| LPN | 5.1 | 7.1 | 10.1 | 8 | 8 | 8 | 1735 | 1622 | 1675 | |
| PCU C | RN | 4.8 | 6.3 | 15.8 | 8 | 8 | 8 | 1770 | 1685 | 1746 |
| LPN | 5.3 | 5.7 | 7.1 | 8 | 8 | 8 | 1723 | 1567 | 1752 | |
| PCU D | RN | 4.5 | 8.2 | 17 | 8 | 8 | 8 | 1778 | 1713 | 1668 |
| LPN | 6.1 | 8.3 | 7.4 | 8 | 8 | 8 | 1756 | 1622 | 1764 | |
| PCU E | RN | 8.1 | 6 | 21.3 | 8 | 8 | 8 | 1684 | 1618 | 1553 |
| LPN | 6.6 | 6.7 | 28 | 8 | 8 | 8 | 1709 | 1634 | 1528 | |
| PCU F | RN | 5.9 | 5.7 | 17.4 | 8 | 8 | 8 | 1761 | 1658 | 1696 |
| LPN | 4.8 | 4.6 | 8.8 | 8 | 8 | 8 | 1740 | 1652 | 1745 | |
| PCU G | RN | 5.6 | 6.2 | 14 | 8 | 8 | 8 | 1751 | 1686 | 1676 |
| LPN | 4.7 | 7.4 | 10.5 | 8 | 8 | 8 | 1700 | 1616 | 1560 | |
| PCU H | RN | 5.1 | 6.3 | 9.1 | 8 | 8 | 8 | 1687 | 1687 | 1637 |
| LPN | 5.9 | 4.8 | 5.6 | 8 | 8 | 8 | 1725 | 1653 | 1804 | |
| PCU I | RN | 6.9 | 5.2 | 22.8 | 8 | 8 | 8 | 1777 | 1662 | 1591 |
| LPN | 5.1 | 5.1 | 11.7 | 8 | 8 | 8 | 1747 | 1686 | 1705 | |
| PCU J | RN | 3 | 14.2 | 12.8 | 8 | 8 | 8 | 1749 | 1682 | 1718 |
| LPN | 3.5 | 6.4 | 15.8 | 8 | 8 | 8 | 1760 | 1707 | 1665 | |
| PCU L | RN | 7.9 | 7.4 | 19.5 | 8 | 8 | 8 | 1710 | 1601 | 1644 |
| LPN | 5.6 | 7.8 | 9 | 8 | 8 | 8 | 1747 | 1658 | 1751 | |
| PCU M | RN | 5.4 | 2.9 | 5.4 | 8 | 8 | 8 | 1745 | 1687 | 1402 |
| LPN | 3.6 | 5.5 | 9.6 | 8 | 8 | 8 | 1769 | 1727 | 1567 | |
| PCU N | RN | 7 | 13.7 | 10.2 | 8 | 8 | 8 | 1775 | 1714 | 1761 |
| LPN | 4.2 | 12.9 | 17.5 | 8 | 8 | 8 | 1739 | 1609 | 1679 | |
RN, registered nurses; LPN, licensed practical nurses. Number of weeks in the year = 52. Number of working days in the week = 5
The activity with the greatest workload volume for RNs was appointments, with 207 008 in 2017; 205 365 in 2018; and 184 725 in 2019. For LPNs, there was an important increase in the vaccination activity jumping from 80 143 in 2017 to 256 194 in 2018, and 224 436 in 2019 (Table 2).
Table 2.
Annual workload of registered nurses and licensed practical nurses in 2017, 2018 and 2019
| Unit | Professional category | Consultation | Outpatient procedures | Home visit | Support to exams | Promotion of education actions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | ||
| PCU A | RN | 10864 | 11250 | 10368 | – | – | 2 | 943 | 874 | 864 | 1 | – | – | 324 | 169 | 147 |
| LPN | – | – | – | 1229 | 850 | 1185 | 7498 | 5643 | 5915 | 180 | 321 | 375 | 196 | 33 | – | |
| PCU B | RN | 14235 | 11352 | 11617 | – | 16 | 31 | 639 | 526 | 336 | – | 371 | 807 | 1323 | 771 | 189 |
| LPN | – | – | – | 591 | 1049 | 1159 | 7911 | 7183 | 5522 | 689 | 1201 | 1023 | 89 | 8 | 1 | |
| PCU C | RN | 18337 | 18886 | 16889 | – | 4 | 72 | 2425 | 2275 | 2301 | 43 | 117 | 150 | 200 | 28 | 375 |
| LPN | – | – | – | 2601 | 3279 | 3102 | 11974 | 11598 | 11710 | 963 | 2365 | 1399 | – | 1 | – | |
| PCU D | RN | 7508 | 11227 | 9006 | – | – | – | 482 | 366 | 141 | 6 | 23 | 496 | 81 | 6 | – |
| LPN | – | – | – | 1031 | 914 | 1719 | 2976 | 2678 | 3310 | 650 | 579 | 370 | 9 | 3 | – | |
| PCU E | RN | 17781 | 17677 | 19498 | – | – | 7 | 2728 | 2401 | 2036 | 280 | 433 | 1268 | 217 | 127 | 151 |
| LPN | – | – | – | 1285 | 1539 | 1588 | 11023 | 9294 | 4663 | 1538 | 1390 | 630 | 254 | 125 | 78 | |
| PCU F | RN | 27814 | 23323 | 21585 | – | 1 | 19 | 2522 | 2176 | 1744 | 346 | 559 | 125 | 333 | 227 | 180 |
| LPN | – | – | – | 3532 | 2416 | 1901 | 15431 | 13744 | 9215 | 756 | 1245 | 561 | 15 | – | – | |
| PCU G | RN | 17398 | 19687 | 14050 | – | 16 | 4 | 859 | 942 | 761 | – | 186 | 888 | 13 | 25 | 36 |
| LPN | - | - | - | 1316 | 1752 | 2169 | 7304 | 7270 | 5165 | 928 | 1813 | 1515 | 57 | 52 | 7 | |
| PCU H | RN | 14902 | 14245 | 10718 | 176 | 59 | 70 | 1880 | 1040 | 1370 | 125 | 562 | 1933 | 112 | 115 | 190 |
| LPN | – | – | – | 2265 | 2007 | 2434 | 8006 | 6012 | 6329 | 834 | 1487 | 471 | – | – | – | |
| PCU I | RN | 19268 | 16013 | 13144 | 1 | – | 16 | 1371 | 986 | 1694 | 319 | 372 | 1489 | 64 | 23 | 3 |
| LPN | – | – | – | 1171 | 1321 | 1512 | 8718 | 5766 | 2858 | 195 | 419 | 355 | – | – | – | |
| PCU J | RN | 11493 | 12630 | 13068 | – | – | 3 | 217 | 456 | 1558 | 2 | 303 | 1336 | 44 | 53 | 280 |
| LPN | – | – | – | 481 | 621 | 1094 | 7206 | 8106 | 9250 | 571 | 339 | 725 | 59 | 26 | – | |
| PCU L | RN | 19195 | 20869 | 17284 | – | – | 1 | 1723 | 1189 | 2692 | – | 126 | 32 | 38 | 175 | 6 |
| LPN | – | – | – | 2027 | 1996 | 2175 | 15454 | 13613 | 10572 | 793 | 665 | 757 | 1 | – | – | |
| PCU M | RN | 13862 | 14629 | 14276 | 18 | 12 | 26 | 2354 | 2304 | 2240 | 134 | 197 | 1545 | 167 | 61 | 58 |
| LPN | – | – | – | 2028 | 1178 | 1699 | 11115 | 11205 | 11085 | 209 | 198 | 427 | 133 | 75 | 1 | |
| PCU N | RN | 14351 | 13577 | 13222 | – | 3 | 57 | 1120 | 1262 | 1296 | 157 | 303 | 701 | 230 | 8 | 31 |
| LPN | 620 | 726 | 661 | 7795 | 7647 | 7329 | 332 | 609 | 692 | 171 | 60 | 13 | ||||
| Unit | Professional category | Administration of medications | Control of immunization and vaccination | Vital signs, weight and height measurements | Venopuncture: venous blood sample | Care delivered to spontaneous demand | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | 2017 | 2018 | 2019 | ||
| PCU A | RN | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| LPN | 3203 | 2774 | 2930 | 3377 | 12265 | 12686 | 4325 | 2973 | 3605 | 7526 | 6474 | 6855 | – | – | – | |
| PCU B | RN | – | – | – | – | – | – | – | – | – | – | 1 | 8 | 3 | 486 | 8 |
| LPN | 1852 | 2815 | 2916 | 4224 | 13613 | 15056 | 11935 | 7676 | 6412 | 4638 | 4014 | 3592 | – | – | – | |
| PCU C | RN | – | – | 3 | – | – | – | – | – | 1 | 60 | – | – | 105 | 328 | 34 |
| LPN | 4924 | 7436 | 6552 | 4642 | 26453 | 19266 | 6047 | 6364 | 4455 | 9992 | 8473 | 7204 | – | – | – | |
| PCU D | RN | – | – | – | – | – | – | – | – | – | – | – | – | 5485 | 21 | 9 |
| LPN | 6086 | 13934 | 14656 | 4232 | 10209 | 12258 | 6498 | 5914 | 4089 | 5101 | 4117 | 4208 | – | – | – | |
| PCU E | RN | 1 | 1 | – | – | – | – | – | – | – | – | – | 1 | 8 | 16 | 7 |
| LPN | 12119 | 13554 | 15597 | 6806 | 18212 | 14339 | 8289 | 5517 | 5278 | 6490 | 5557 | 5668 | – | – | – | |
| PCU F | RN | – | – | – | – | – | – | – | 24 | 2 | – | – | 1 | 276 | 6 | – |
| LPN | 10854 | 8123 | 7578 | 6257 | 25959 | 20668 | 11631 | 8987 | 5558 | 10347 | 9226 | 9386 | – | – | – | |
| PCU G | RN | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 101 |
| LPN | 4377 | 5246 | 6067 | 4627 | 16058 | 15154 | 6496 | 5598 | 6390 | 4981 | 5949 | 6667 | – | – | – | |
| PCU H | RN | – | – | – | – | – | – | – | – | – | 469 | 45 | 4 | 635 | 387 | 175 |
| LPN | 2532 | 3734 | 4030 | 4867 | 16104 | 15580 | 5378 | 4491 | 3326 | 7277 | 7946 | 4836 | – | – | – | |
| PCU I | RN | – | – | – | – | – | – | – | – | – | – | – | – | 138 | 100 | 30 |
| LPN | 3335 | 3782 | 4466 | 5333 | 17515 | 16133 | 4273 | 3657 | 3227 | 4672 | 5394 | 5069 | – | – | – | |
| PCU J | RN | – | – | – | – | – | – | – | – | – | – | – | – | 2829 | 1433 | 75 |
| LPN | 2022 | 3896 | 4434 | 4629 | 16098 | 16920 | 5050 | 3853 | 5006 | 3230 | 4923 | 5991 | – | – | – | |
| PCU L | RN | 12 | – | – | – | – | 39 | 5 | 1 | 5 | – | – | – | – | – | |
| LPN | 5254 | 4468 | 5539 | 5850 | 30192 | 29919 | 12417 | 8368 | 5882 | 9536 | 7260 | 8109 | – | – | – | |
| PCU M | RN | – | – | – | – | – | – | – | – | 1 | – | – | – | 38 | – | 1 |
| LPN | 3431 | 1009 | 3028 | 6570 | 16183 | 11950 | 10684 | 6758 | 6588 | 7093 | 5202 | 5443 | – | – | 3 | |
| PCU N | RN | – | – | – | – | – | – | – | – | 238 | – | – | – | – | – | 103 |
| LPN | 2279 | 2775 | 3395 | 18729 | 37333 | 24507 | 2961 | 4077 | 3919 | 5575 | 4337 | 4901 | – | – | – | |
RN, registered nurses; LPN, licensed practical nurses
The percentage of support and additional activities for RNs and LPNs was 37.4% and 24.7%, respectively (Table 3).
Table 3.
Support activities and Additional activities of registered nurses and licensed practical nurses in 2017, 2018 and 2019, proposed by Bonfim et al. [11]
| Activities [11] | Registered nurse (%) | Licensed ractical nurse (%) |
|---|---|---|
| Education actions for healthcare workers | 2.1 | 1.4 |
| Infection control | 0.1 | 1.4 |
| Control of supplies | 0.5 | 3.6 |
| Organization of working process | 3.7 | 1 |
| Documentation | 12.4 | 9.3 |
| Mapping and territorialization | 0.1 | 0 |
| Referral and Contra-referral | 0.3 | 0.3 |
| Administrative meeting | 5.9 | 1.4 |
| Meeting to assess professional care | 1.9 | 1 |
| Supervision of works at the unit | 0.4 | 0 |
| Sharing information on health care | 6.2 | 3 |
| Interpretation of laboratory data | 0.2 | 0 |
| Health surveillance | 1.3 | 0.4 |
| Support to students | 1 | 0.3 |
| Development of administrative process/routine | 0.3 | 0.1 |
| Orientations on health system | 1 | 1.5 |
| Sums | 37.4 | 24.7 |
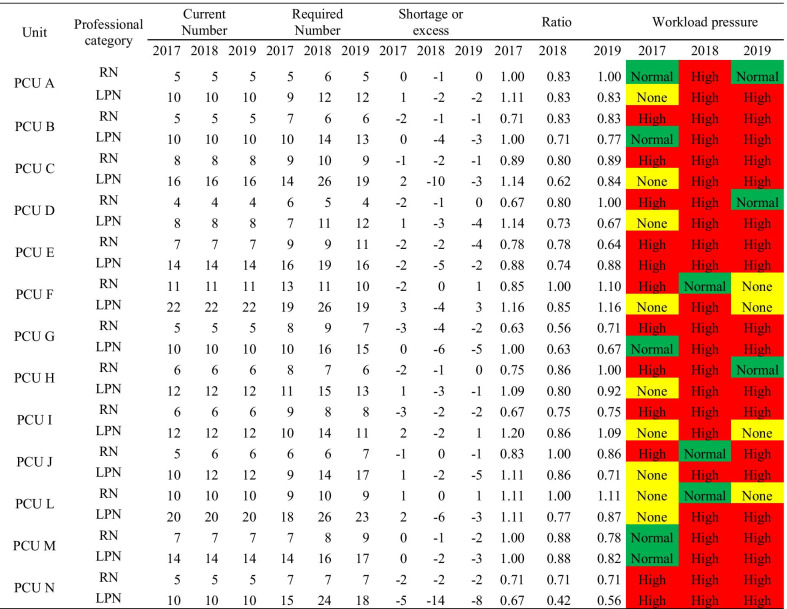
The WISN calculations found that in 2017 RNs were under a high workload pressure at 10 PCUs (77%), with a similar pattern in 2018, and with a decrease to 8 PCUs (61%) in 2019. For LPNs, a high workload pressure was found at 2 PCUs (15%) in 2017, however it increased to 13 PCUs (100%) in 2018, and remained high at 11 of them (85%) in 2019 (Table 4).
Table 4.
Total required staff based on WISN
RN, registered nurses; LPN, licensed practical nurses
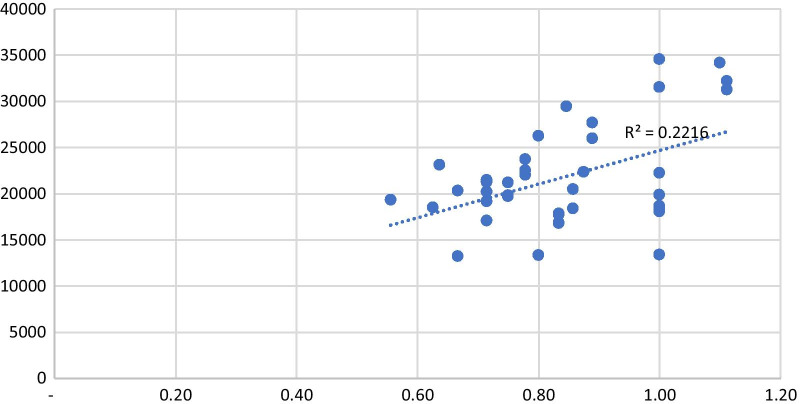
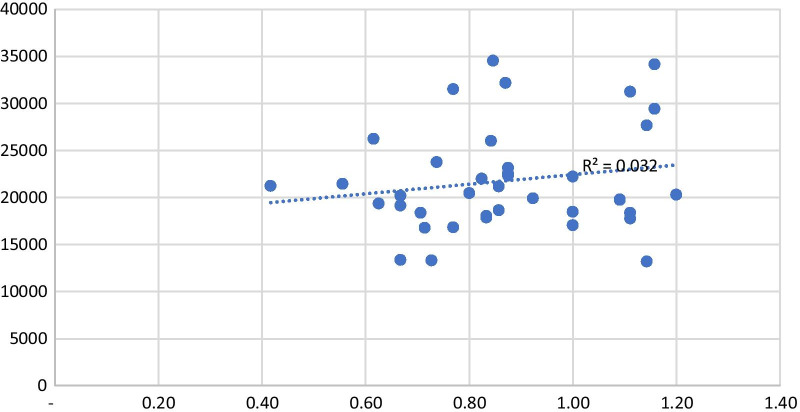
There was no statistically significant correlation between workload pressure for RNs and LPNs and the number of people registered per PCU (Figs. 1 and 2).
Fig. 1.
Comparing the registered nurse ratio and number of people registered in each PCU in 2017, 2018 and 2019
Fig. 2.
Comparing the licensed practical nurse ratio and number of people registered in each PCU in 2017, 2018 and 2019
Discussion
2020, the International Year of the Nurse and the Midwife, elevated the worldwide recognition of the work performed by nurses and their demands for better working conditions, education, and professional development [12]. In line with this recognition is the fact that nursing plays a critical role in the successful implementation of PHC, which is recognized as the basis of an effective and responsive health system—key to universal coverage [13]. However, the results of this study show how RNs and LPNs working in PHC have been suffering from increasing workload pressure, and the need for better planning and implementation of staffing policies for PHC.
The study identified PCUs with high work pressure and a shortage of nursing professionals needed to meet the actual demand seen during the 3 years of analysis. This is a challenge that PHC must resolve in order to guarantee access and to be able to meet the population’s health needs [14]. The shortage of professionals and its impact should be reported and discussed with PHC teams, so that they can manage high work pressure in the best way possible, balancing access and to promote continuity of care [15]. This scenario of imbalance is known to impact access, generating longer waiting times, which in turn could result in higher mortality rates and other adverse outcomes [16].
In this study, we found no significant association between the number of registered patients and workload pressure. This could be explained not only by the size of PHC teams, but also by additional aspects, such as how frequently patients demand care from PCUs and their teams, which impacts the annual workload and consequently the required number of professionals based on the WISN method. Perhaps more elements, like detailed patient characteristics, are necessary to understand the demand for PHC.
The size of patient panels and the number of PHC teams per service also play an important role, and have been discussed in the literature, including its association with user satisfaction [17]. Ideally, patient panel size should be adjusted to balance the number of professionals on a team and the expected workload. Family physicians have been questioned about the number of patients that could be under their care [15] and the “ideal” patient panel size per physician [18] and advanced methods like machine-learning algorithms have even been tested to answer this question [19]. However, there is little evidence about the “ideal” patient panel size for nursing professionals working as part of a PHC team, such as those established in Brazil and there are investigation gaps about how nursing staff imbalance impact the quality of care in PHC scenario.
Additionally, the distribution of activities among the different professionals that compose the family health team, in spite of presenting common competencies described in the PNAB [6], shows that the actions with the largest impact on the nursing team’s workload, such as vaccination and consultations/appointments, are exclusive to the nurses. However, indirect care activities, such as documentation and administrative meetings related to organizing the work process, are common among team members [20], and can be distributed in such a way that the nurse can dedicate the larger part of their workload to caring for patients.
A study conducted in 2011 [21] that applied the WISN method at a single PCU in São Paulo, Brazil, found that the workload and the number of professionals available was balanced, with a ratio of 0.8 for RNs and 1.0 for LPNs. This study found very different results, and is probably more representative of the real situation, since it included 13 PCUs evaluated for a period of 3 years.
Another study that evaluated workloads of nursing professionals working in PHC teams in Brazil found an association between excessive demand, problems in the physical structure of the units, and gaps in the healthcare network to increased workloads among these professionals, which affected the quality of care and impacted the effectiveness of PHC [22].
The required number of professionals is influenced by a number of variables, including available working time, absences, leave, an adequate information system, the epidemiological background, and the structure of organizational processes at PCUs. These factors were recently put to the test in Brazil during the outbreaks of measles and yellow fever in 2018 and 2019. Nursing professionals working on PHC teams had to organize and implement vaccination strategies in an expedited manner in addition to their routine work [23, 24].
The study presents an increase in work pressure among LPNs between 2017 and 2019, especially in 2019, likely because LPNs started to allocate more of their time to organizing vaccination campaigns and performing household visits to vaccinate, activities that are not accounted for in their productivity evaluation. Moreover, the vaccination calendar has been expanded, and currently includes 19 vaccines for more than 20 diseases [25], with the introduction of new vaccines against the SARS-CoV-2 expected to put even more pressure on PCUs to deliver them in a timely fashion.
As described previously, in Brazil LPNs play a major part in the national immunization program and in preventive actions [26]. The number of nursing professionals can impact the health system’s response to public emergencies, such as vaccination campaigns for both scheduled and pandemic situations, like with COVID-19. This reinforces the importance of applying the WISN method to the planning and implementation of public policies.
Thus, to understand the current deficit of LPNs it would be relevant to plan staffing needs in the face of a probable high demand for vaccination campaigns, and for future analysis that could take into account seasonal variations and target coverage rates that can be used to plan, improve allocation, and when necessary, increase the number of professionals during strategic periods. Historical patterns that characterize an increase in demand or a reduction in AWT can be analyzed to determine strategic periods. This is why it is important for the WISN method to be applied dynamically and relevantly with periods of rapid and assertive actions throughout the year.
As in other parts of the world, an aging population and the shift of the disease burden from infectious to noncommunicable diseases are important factors impacting the demand for PHC services and the volume of RNs’ scheduled and unscheduled appointments in Brazil [27]. An observational study conducted in Brazil found that RNs working as part of a PHC team spent 11.6% of their working time with appointments [11], which matches the high volume found for the PCUs included in this study.
In addition, the reduction in activities over the years, probably associated with time spent on unscheduled appointments, is a notable finding. This could be explained by the implementation of advanced access scheduling at the PCUs included in the study, which began [14] in 2017, with RNs’ unscheduled appointments accounting for up to 70% of their agenda.
The evaluation of staffing needs could also work as an ongoing education and quality improvement strategy, since annual analyses provide an opportunity to reflect on the practice and organization of nursing professionals. A study that evaluated the implementation of the WISN method to two PHC teams in the state of São Paulo found that it promoted a change in the team’s attitude towards the correct recording of data in information systems, and prompted a reorganization of the territory covered by each team [28].
Thus, staff planning with the WISN method allows for an important reflection, considering that not all of the problems at the PCUs are related to the amount of professionals, just as the amount of professionals is not a solution to all of the problems. Analyzing the data that make up the calculation makes it possible to recognize the obstacles in organizing work, distributing activities among team members, the amount of activities performed annually, the amount of absences for health leave and/or other types of leave that historically contribute to understanding the pressure on the team’s workload due to dynamic patient demand.
In this way, staff planning at PHCs is a strategic process, balancing demand and supply through the analysis of the availability staff and their work process, and through a systematic planning method that aims for continual improvement in the process of ongoing education and implementation of public policy.
Studies using the WISN contribute prominently to the discussion on staff planning at PHCs as a tool for public policy that facilitates management decisions and thus allows for the strengthening of universal health coverage, considering the key role that professionals like RNs and LPNs play in the results and increase of health access.
One of the main limitations of this study is the fact that it only included data recorded for patients that accessed the PCUs during the study period. PHC in Brazil is organized geographically, with the assignment of catchment areas to PCUs and PHC teams, with no overlap or gaps between them. Although PCUs are responsible for the entire population living in their catchment area, some proportion of these individuals never or rarely access services, and are not represented in productivity-based analyses, such as those conducted in this study. Therefore, the study results reflect nursing staffing needs based on the population that accessed services, and not on the entire covered population, an additional challenge that needs to be addressed in future studies.
Conclusion
This study found that RNs and LPNs, working as part of PHC teams in Brazil, experienced high workload pressures, which could be associated with the epidemiological background, the structure of organizational processes, and the flexibility of policies determining the composition and number of professionals on PHC teams.
The PCUs should work as the first point of contact with the health system, while ensuring equitable access and quality of care. The appropriate staffing of PHC teams represents a key activity in order to be successful in that mission, and the WISN method could be a useful tool to support this process.
Acknowledgements
Not applicable.
About this supplement
This article has been published as part of Human Resources for Health Volume 19, Supplement 1 2021: Countries' experiences on implementing WISN methodology for health workforce planning and estimation. The full contents of the supplement are available at https://human-resources-health.biomedcentral.com/articles/supplements/volume-19-supplement-1.
Abbreviations
- PHC
Primary health care
- WISN
Workload Indicators of Staffing Need
- FHS
Family Health Strategy
- PNAB
National Policy for Primary Care (PNAB, acronym in Portuguese)
- RN
Registered nurse
- LPNs
Licensed practical nurses
- AWT
Available working time
- PCU
Primary Care Unit
Authors' contributions
DB: conceptualization, investigation, project administration, interpretation of data, writing—original draft preparation, and writing—review and editing. ACCNM: formal analysis, writing—original draft preparation, and writing—review and editing. TR: conceptualization, interpretation of data and writing—review and editing. DCP: conceptualization, project administration and writing—review and editing. All authors read and approved the final manuscript.
Funding
This article is part of the project “Panel Size for Primary Health Care Teams” (2020/11695-3) that received funding from the Ministry of Health, Brazilian National Council for Scientific and Technological Development (CNPq), The São Paulo Research Foundation (FAPESP) and Secretariat of Health to the São Paulo Government (SES-SP).
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The research project was approved by the Research Ethics Committee of the Hospital Israelita Albert Einstein (protocol CAAE: 23388819.9.0000.0071) according to Resolution 466/12 of the Brazilian National Health Council.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tomblin Murphy G, MacKenzie A, Alder R, Birch S, Kephart G, O'Brien-Pallas L. An applied simulation model for estimating the supply of and requirements for registered nurses based on population health needs. Policy Polit Nurs Pract. 2009;10(4):240–251. doi: 10.1177/1527154409358777. [DOI] [PubMed] [Google Scholar]
- 2.Hongoro C, McPake B. How to bridge the gap in human resources for health. Lancet. 2004;364(9443):1451–1456. doi: 10.1016/S0140-6736(04)17229-2. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. WISN: Workload Indicators of Staffing Need. User’s manual. Geneva: WHO; 2010. http://www.who.int/hrh/resources/wisn_user_manual/en/. Accessed 20 Jun 2021.
- 4.Doosty F, Maleki MR, Yarmohammadian MH. An investigation on workload indicator of staffing need: a scoping review. J Educ Health Promotion. 2019;8:22. doi: 10.4103/jehp.jehp_220_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wundavalli L, Kumar P, Dutta S. Workload Indicators of Staffing Need as a tool to determine nurse staffing for a high volume academic Emergency Department: an observational study. Int Emerg Nurs. 2019;46:100780. doi: 10.1016/j.ienj.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Gomes CBS, Gutiérrez AC, Soranz D. National Primary Care Policy 2017: analysis of teams composition and national coverage of Family Health. Cien Saude Colet. 2020;25(4):1327–1338. doi: 10.1590/1413-81232020254.31512019. [DOI] [PubMed] [Google Scholar]
- 7.Bousquat A, et al. Structural typology of Brazilian primary healthcare units: the 5 Rs. Cad. Saúde Pública. 2017, 33(8), e00037316. Epub Aug 21 2017. ISSN 1678–4464. 10.1590/0102-311X00037316 [DOI] [PubMed]
- 8.Brasil. Resolução COFEN 543/2017. Updated and establishes parameters for dimensioning the Staff of Nursing Professionals in the services/sites where nursing activities are performed. Brasília; 2017. http://www.cofen.gov.br/resolucao-cofen-5432017_51440.html. Accessed 29 Jun 2021.
- 9.Bodenheimer T, Bauer L. Rethinking the primary care workforce—an expanded role for nurses. N Engl J Med. 2016;375(11):1015–1017. doi: 10.1056/NEJMp1606869. [DOI] [PubMed] [Google Scholar]
- 10.Miranda Neto MV, Rewa T, Leonello VM, Oliveira MAC. Advanced practice nursing: a possibility for Primary Health Care? Rev Bras Enferm. 2018;71(Suppl. 1):716–721. doi: 10.1590/0034-7167-2017-0672. [DOI] [PubMed] [Google Scholar]
- 11.Bonfim D, Fugulin FM, Laus AM, Peduzzi M, Gaidzinski RR. Time standards of nursing in the Family Health Strategy: an observational study. Rev Esc Enferm USP. 2016 doi: 10.1590/S0080-623420160000100016. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Year of the Nurse and the Midwife 2020 (cited Jan 20 2020). https://www.who.int/campaigns/year-of-the-nurse-and-the-midwife-2020. Accessed 13 Jun 2021.
- 13.Pan American Health Organization. Expanding the Roles of Nurses in Primary Health Care. Washington, D.C.: OPAS; 2018. https://iris.paho.org/handle/10665.2/34960. Accessed 13 Jun 2021.
- 14.Assis M, Jesus W. Access to health services: approaches, concepts, policies and analysis model. Ciência Saúde Coletiva. 2012;17(11):2865–2875. doi: 10.1590/S1413-81232012001100002. [DOI] [PubMed] [Google Scholar]
- 15.Murray M, Davies M, Boushon B (2007). Panel size: how many patients can one doctor manage? Family Pract Manag. 14(4), 44–51. https://www.aafp.org/fpm/2007/0400/p44.html. Accessed 29 Jun 2021. [PubMed]
- 16.Stefos T, Burgess JF, Jr, Mayo-Smith MF, Frisbee KL, Harvey HB, Lehner L, Lo S, Moran E. The effect of physician panel size on health care outcomes. Health Serv Manage Res. 2011;24(2):96–105. doi: 10.1258/hsmr.2011.011001. [DOI] [PubMed] [Google Scholar]
- 17.Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract. 2010;11:61. doi: 10.1186/1471-2296-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raffoul M, Moore M, Kamerow D, Bazemore A. A primary care panel size of 2500 is neither accurate nor reasonable. J Am Board Fam Med. 2016;29(4):496–499. doi: 10.3122/jabfm.2016.04.150317. [DOI] [PubMed] [Google Scholar]
- 19.Rajkomar A, Yim JW, Grumbach K, Parekh A. Weighting primary care patient panel size: a novel electronic health record-derived measure using machine learning. JMIR Med Inform. 2016;4(4):e29. doi: 10.2196/medinform.6530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonfim D, Pereira MJB, Pierantoni CR, Haddad AE, Gaidzinski RR. Tool to measure workload of health professionals in Primary Health Care: development and validation. Rev esc Enferm USP. 2015 doi: 10.1590/S0080-623420150000800004. [DOI] [PubMed] [Google Scholar]
- 21.Bonfim D, Laus AM, Leal AE, Fugulin FMT, Gaidzinski RR. Application of the Workload Indicators of Staffing Need method to predict nursing human resources at a Family Health Service. Rev Lat Am Enfermagem. 2016;24:e2683. doi: 10.1590/1518-8345.1010.2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pires DEP, Machado RR, Soratto J, Scherer MA, Gonçalves ASR, Trindade LL. Nursing workloads in family health: implications for universal access. Rev Lat Am Enfermagem. 2016;24:e2682. doi: 10.1590/1518-8345.0992.2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Secretaria de Vigilância em Saúde. Measles situation in Brazil–2019. Epidemiol Report. 2019 (citado 2020 Nov 21); 36:1–8. http://portalarquivos2.saude.gov.br/images/pdf/2019/janeiro/28/Informe-Sarampo-n36-24jan19aed.pdf. Accessed 20 Jun 2021.
- 24.Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Epidemiological Bulletin: Epidemiological situation of yellow fever in monitoring. 2019/2020. Boletim Epidemiol. 2020 (cited 2020 Nov 21). http://www.rets.epsjv.fiocruz.br/sites/default/files/arquivos/biblioteca/boletim-epidemiologico-svs-01.pdf. Accessed 20 Jun 2021.
- 25.Domingues CMAS, Fantinato FFST, Duarte E, Garcia LP. Vacina Brasil Movement and immunization training and development strategies. Epidemiologia e Serviços de Saúde. 2019;28(2):e20190223. doi: 10.5123/s1679-49742019000200024. [DOI] [Google Scholar]
- 26.Lima AMV, Peduzzi M. Characterization of nursing actions in Primary Health Care for teamwork and collaborative practice. J Manag Prim Heal Care. 2017;8(3):32–33. doi: 10.14295/jmphc.v8i3.645. [DOI] [Google Scholar]
- 27.Pimentel TRS, et al. Description of demand in a Family Health Unit. Rev bras med fam comunidade. Florianópolis. 2011;6(20):175–181. doi: 10.5712/rbmfc6(20)95. [DOI] [Google Scholar]
- 28.Santos LC, Andrade J, Spiri WC. Dimensioning of nursing professionals: implications for the work process in the family health strategy. Escola Anna Nery. 2019;23(3):20180348. doi: 10.1590/2177-9465-ean-2018-0348. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.