Abstract
Although extensive efforts were made to improve maternal and child health, the magnitude of home child-birth is considerably high in Ethiopia. Therefore, this meta-analysis aimed to estimate the effect of lack of ANC visit and unwanted pregnancy on home child-birth among reproductive-age women in Ethiopia. International databases, including Cochrane Library, Google Scholar, PubMed, Global Health, HINARI, and CINAHL were searched systematically to identify studies reporting the prevalence of home child-birth and its association with lack of ANC visit and unwanted pregnancy among reproductive-age women in Ethiopia. STATA/SE version-14 was used to analyze the data and Der Simonian and Liard's method of random effect model was used to estimate the pooled effects. The heterogeneity between study and publication bias was assessed by using I-squared statistics and Egger's test respectively. A total of 19 studies with 25,228 study participants were included in this meta-analysis. The pooled prevalence of home child-birth among reproductive-age women in Ethiopia was 55.3%. Sever heterogeneity was exhibited among the included studies (I2 = 99.8, p = 0.000). The odds of home child-birth among mothers who have no ANC visit was 3.64 times higher compared to their counterparts [OR = 3.64, 95%, CI: (1.45, 9.13)]. There was significant heterogeneity among the included studies (I2 = 94%, p = 0.000). However, there was no statistical evidence of publication bias in the pooled effect of lack of ANC visit on home child-birth (P = 0.302). Women who experienced unwanted pregnancy were 3.02 times higher to give birth at home compared to women with a wanted pregnancy [OR = 3.02, 95%CI: (1.19, 7.67)]. Severe heterogeneity was exhibited (I2 = 93.1%, p = 0.000) but, there was no evidence of significant publication bias in the pooled effect of unwanted pregnancy on home child-birth (P = 0.832). The proportion of home child-birth among reproductive-age women in Ethiopia remains high. Lack of ANC visit and unwanted pregnancy had a significant effect on the practice of home child-birth. Strengthening behavioral change communication programs should be the primary focus area to improve institutional delivery service utilization among women with lack of ANC visit and unwanted pregnancy.
Subject terms: Health care, Risk factors
Introduction
Each year, an estimated 303,000 women die as a result of preventable pregnancy and childbirth complications worldwide1. Ninety-nine percent (99%) of the global maternal deaths occur in developing countries and Sub-Saharan African (SSA) countries alone shared 62% of all maternal deaths. Ethiopia is the fourth top ten countries in the world with the highest-burden of maternal mortality next to India, Nigeria, and the Democratic Republic Congo sharing 58% of all the global deaths1. The 2016 Ethiopia Demography and Health Survey (EDHS) report showed that the Maternal Mortality Ratio (MMR) in the country was 412/100,000 live births2.
More than two-thirds (73%) of maternal deaths occur during childbirth and within 24 h post-partum period due to direct obstetric causes such as hemorrhage, infection, obstructed labor, hypertension, and abortion3. Hypertensive disorders of pregnancy, hemorrhage, and sepsis alone accounted for more than 50% of all maternal mortality worldwide4.
One-third of births worldwide happen at home in the absence of SBA5. Studies have shown that home delivery ranged from 65% in Tanzania to 87.7% in Bangladesh6. The situation is worst in Africa in which more than 60% of women deliver at home without SBAs in contrary to less than 1% in developed nations7.
In Ethiopia, the prevalence of home delivery ranged from 19.1% in Shashemene town8 to 80% in Sherkole district of Benishangul Gumuz region9. According to the 2016 EDHS report, the prevalence of home delivery in the country was 73%, ranging from 3% in Addis Ababa to 85% in Afar region2.
In the last fifteen years, the Ethiopian government has established an inspiring framework for improving maternal and child health like training and deploying Health Officers with a master of Integrated Emergency Obstetrics and Surgery (IEOS) program, establishing Women Development Army (WDA), and creating pregnant women conferences to enable them to discuss issues related with pregnancy and delivery, constructing maternity waiting home at health facilities, availing traditional ambulances and increasing the number of modern ambulances for early referrals of emergency cases10. Regardless of these efforts, the rate of home delivery is considerably high in Ethiopia2.
Lack of ANC visits is the most fundamental and proximal factor responsible for the high rates of home delivery in developing countries like Ethiopia11–14. The World Health Organization (WHO) strongly emphasizes the need to have at least four ANC, in which the first visit should be started during the first trimester15. Although quality ANC strongly influences the use of skilled delivery care16–18, only 43% of women attended four or more ANC visits in Ethiopia19 which is far from the national target (increasing four or more ANC visits to 95% by the year 2020)20. Unwanted pregnancy is another major contributing factor affecting home childbirth21,22. A study showed that it increases the rate of home delivery by 40%23.
Reducing home delivery and increasing institutional delivery service utilization has a substantial contribution to the success of Sustainable Development Goal (SDG) 3 which aimed to reduce the global MMR below 70 per100, 000 live births by 203024, and the Ethiopian Health Sector Transformation Plan (HSTP) IV which aimed to decrease the national MMR to 199 per 100,000 live births by 202020.
Different studies were conducted to assess the practice of home child-birth in Ethiopia8,9,15,25–40. A systematic review and meta-analysis was also done41. However, the authors included those articles assessing institutional service utilization in their study which cannot indicate the exact figure of the prevalence of home delivery. They also included those studies assessing the intention of women towards the place of delivery that didn't clearly show the actual place of delivery. Moreover, they couldn't assess the effect of unwanted pregnancy on home delivery although it is the major factor that affects the rate of home child-birth in the Ethiopian context. Therefore, this study aimed to estimate the effect of lack of ANC visit and unwanted pregnancy on home child-birth among reproductive-age women in Ethiopia. The result of this meta-analysis will help to identify whether the absence of ANC follow-up and unwanted pregnancy affect home delivery practice in Ethiopia and to reduce unwanted pregnancy by improving family planning utilization and promote the importance of ANC visit through information communication education and behavioral change communication programs accordingly.
Materials and methods
Searching strategy
The current systematic review and meta-analysis was organized according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA-2009) guideline42 (see supplementary file 1). International databases including Cochrane Library, Google Scholar, PubMed, Global Health, HINARI, and CINAHL were searched systematically to estimate the pooled prevalence of home child-birth and its association with lack of ANC visit and unwanted pregnancy among reproductive-age women in Ethiopia. The searching was carried out from September 1 up to December 30, 2020, by two authors (YD and BK) independently, and research articles published from 2000 up to December 30, 2020, were included in the analysis.
All the relevant studies were identified by using the following search terms: "proportion", "magnitude", "prevalence", "incidence", "home delivery", "home birth", "home child-birth", "risk factors" , "predictors", "factors", "determinants", "associated factors", "women", " mothers", " Reproductive Age Women", " women of child bearing age", "Ethiopia" using Boolean operators "OR" or "AND" (see supplementary file 2). The protocol of this meta-analysis was not registered on the International Prospective Register of Systematic Reviews (PROSPERO).
Eligibility criteria
Inclusion criteria
Population: This systematic review and meta-analysis include studies conducted among women aged from15-49 years in Ethiopia.
Exposure: ANC unbooked women and women with an unwanted pregnancies.
Comparison: women who have ANC follow-up and women with a wanted pregnancy.
Outcome: Studies assessed home child-birth as a primary outcome.
Study design: all types of observational studies (Cross-sectional, case–control, and cohort) were included.
Country: studies conducted only in Ethiopia.
Study setting: all facility and community-based studies.
Time frame: studies published from the beginning of 2000 up to December 30, 2020.
Publication: both published and unpublished articles.
Language: studies written in the English language were included in this study.
Exclusion criteria
Those studies which are purely qualitative, the outcome of the interest not reported, and those with the absence of full text were excluded from this study after two email contacts of the corresponding author.
Outcome measurement
This systematic review and meta-analysis measure three main outcomes. The primary outcome of this study was the pooled prevalence of home child-birth which was calculated from each primary article by dividing the number of women delivered at home to the total sample size multiplied by 100.
The second outcome was the association between lack of ANC visit and home child-birth. In this study, using ANC was considered if women received at least one ANC visit and more during the period of pregnancy. The third outcome of this study was the association between unwanted pregnancy and home child-birth. Unwanted pregnancy was defined as a pregnancy that occurred when no more children were desired. For the second and the third outcomes, the association between predictor variables (lack of ANC visit and unwanted pregnancy) and home child birth was determined in the form of the log odds ratio.
Data extraction and quality assessment
After duplicate files were removed by endnote software, three reviewers (MY, NC, and MA) independently screened the leftover articles for inclusion. Then, based on their study design, the quality of the screened articles was assessed using Joana Brigg's Institute (JBI) critical appraisal checklist43. In this study, all of the included articles scored 50% and more, thus all are included in the review. A group of two authors (EA and BA) assessed the quality of each article independently and the disagreement or the difference in the results at the time of quality assessment was resolved by taking the mean score of the results of both reviewers.
All the relevant data were extracted by using a standardized data extraction sheet. The data extraction sheet includes the following variables; the name of the first author, region, year of study, publication year, study setting (whether it is institution or community based), study area, study design, the prevalence of home child-birth, sample size, response rate, the residence of the mother, number women delivered at home and frequencies of lack of ANC visit and unwanted pregnancy in the form of a two by two tables. Five reviewers (TB, ET, GB, WM, and AA) extract all the necessary data independently and the disagreement raised at the time of data extraction was resolved by consensus.
Data analysis
All the necessary data were extracted using Microsoft Excel and exported to STATA version-14 for analysis. DerSimonian and Liard's method of random effect model (p-value < 0.05) was used to calculate the pooled prevalence of home child-birth in Ethiopia44. Besides, pooled odds ratios with 95% confidence intervals was used to determine the association of home child-birth with lack of ANC visit and unwanted pregnancy.
The variation among the original articles was statistically estimated by using the I2 test. I2 tests > 75% was considered as severe heterogeneity and was subjected to subgroup and univariate Meta-regression analyses to identify the possible source of variations among the point estimates of the individual studies. Moreover, the funnel plot and egger's regression test at a p-value less than 0.05 was used to assess the presence of publication bias45.
Results
Study selection
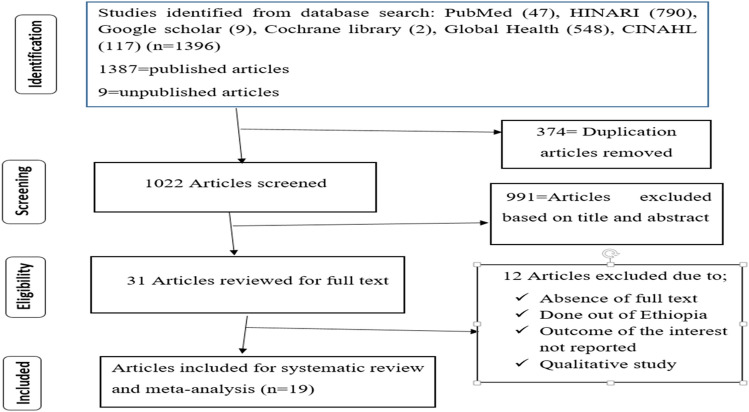
The review identified a total of 1,396 published and unpublished articles by searching international databases; Cochrane Library, Google Scholar, PubMed, Global Health, HINARI, and CINAHL. Then, 1,365 articles were removed due to duplication and as a result of their titles and abstracts. The rest 31 articles were critically assessed based on the eligibility criteria and finally, a total of 19 full-text articles were included in this meta-analysis (Fig. 1).
Figure 1.
PRISMA flow diagram describing the selection of studies for systematic review and meta-analysis.
Characteristics of the included studies
A total of nineteen studies8,9,15,25–40 with 25,228 study participants were included to estimate the pooled prevalence of home child-birth and its association with lack of ANC visit and unwanted pregnancy in Ethiopia. The sample size of the studies ranged from a minimum of 264 study participants from a study conducted in Abobo district, Gambella region33 to a maximum of 10,622 participants among a study conducted on 2016 EDHS data32. In this meta-analysis, seven regions from nine regions of the country were represented; six studies from SNNP25,26,35,36,39,40, four from Amhara28,30,31,34, three from Tigray29,37,38, one from Oromia8, one from Afar27, one from Benishangul Gumuz9 and one study from Gambella region33. However, there were no studies reported from Hareri, and Somali regions. Regarding the study design, twelve studies were cross-sectional8,9,15,25–27,30–32,34,35,40, five were case–control28,29,33,36,37 and the rest two were cohort studies38,39. (Table 1).
Table 1.
Descriptive summary of nineteen studies included in the meta-analysis of home child-birth and associated factors among pregnant women in Ethiopia, 2021.
| Authors | Publication year | Region | Study Area | Study design | Sample size | Response rate | No of women delivered at home | Prevalence (%) | Quality score (%) |
|---|---|---|---|---|---|---|---|---|---|
| Ibrahim S et al.25 | 2017 | SNNPR | Anlemo | Cross-sectional | 268 | 97.1 | 132 | 49.3 | 66.7 |
| Gistane Ayele et al.26 | 2015 | SNNPR | Arbaminch | Cross-sectional | 436 | 90.6 | 346 | 79.4 | 77.8 |
| Abdella M et al.27 | 2017 | Afar | Ayssaita | Cross-sectional | 317 | 99.7 | 225 | 71 | 77.8 |
| Abebe et al.28 | 2012 | Amhara | Bahirdar | Case–control | 324 | 91 | – | – | 66.7 |
| Berhe and Nigusie9 | 2020 | Benishangul Gumuz | Sherkole | Cross-sectional | 441 | 98 | 353 | 80 | 77.8 |
| Tololu A et al.29 | – | Tigray | Central zone | Case–control | 300 | 95 | – | – | 66.7 |
| Kasaye et al.30 | 2017 | Amhara | Debremarkos | Cross-sectional | 502 | 96.9 | 127 | 25.3 | 88.9 |
| Wodaynew et al.31 | 2018 | Amhara | Delanta | Cross-sectional | 557 | 96.7 | 196 | 35.2 | 88.9 |
| Chernet AG, et al.32 | 2019 | EDHS based | EDHS 2016 based | Cross-sectional | 10,622 | NR | 7137 | 67.2 | 88.9 |
| Yebyo H et al.15 | 2015 | EDHS based | EDHS 2011 based | Cross-sectional | 7908 | NR | 6980 | 88.3 | 88.9 |
| Mekonnen Y et al.34 | 2015 | Amhara | Gozamin | Cross-sectional | 497 | 100 | 374 | 75.3 | 88.9 |
| DenekeDelibo et al.35 | 2020 | SNNPR | Badawacho | Cross-sectional | 531 | 96.2 | 391 | 73.6 | 88.9 |
| Wondimu and Woldesemayat 36 | 2020 | SNNPR | Hamar district | Case–control | 292 | 94.5 | – | – | 66.7 |
| Tsegay et al.37 | 2017 | Tigray | Tanqua-Abergele | Case–control | 275 | 96.5 | – | – | 66.7 |
| Gultie et al.8 | 2016 | Oromia | Shashemene | Cross-sectional | 277 | 97.2 | 53 | 19.1 | 66.7 |
| Hinsermu Bayu et al.38 | 2015 | Tigray | Alamata, Mehoni, and Maichew | Cohort | 465 | 89 | 134 | 28.8 | 77.8 |
| Siyoum et al.39 | 2018 | SNNPR | Wolaita | Cohort | 505 | 91.2 | 68 | 13.5 | 77.8 |
| Kucho and Mekonnen40 | 2017 | SNNPR | Zala | Cross-sectional | 447 | 100 | 302 | 67.6 | 77.8 |
| Asmelash AberaMitiku et al.33 | 2020 | Gambella | Abobo District | Case–control | 264 | 100 | – | – | 66.7 |
SSNPR-Southern Nations, Nationalities, and Peoples Region.
Prevalence of home child-birth in Ethiopia
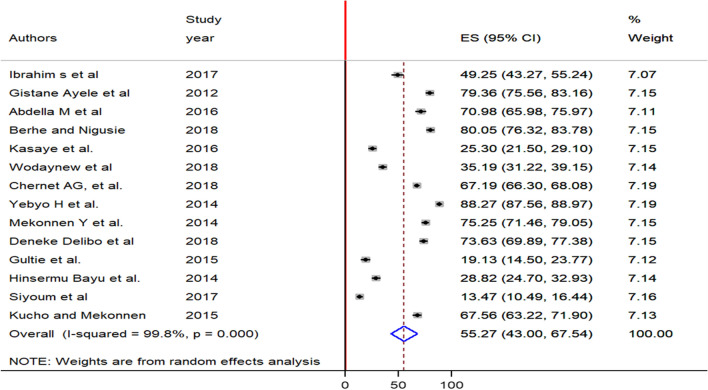
A meta-analysis of 14 studies showed that the pooled prevalence of home child-birth among reproductive-age women in Ethiopia was 55.3% (95% CI: 43, 67.5). As it was shown on the figure, DerSimonian and Laird random-effects meta-analysis model was used to estimate the pooled effect as a result of severe heterogeneity between the included studies(I2 = 99.8, p = 0.000) (Fig. 2).
Figure 2.
Forest plot of the pooled prevalence of home child-birth among reproductive-age women in Ethiopia, 2021.
Publication bias was graphically assessed by using the funnel plot and there was an asymmetrical distribution of the effect estimates showing the presence of publication bias (Fig. 3), the eggers test statistics also evidenced that the presence of significant publication bias (P = 0.040). Duval and Tweedie’s 'trim and fill' method was used to reduce and adjust the effect of publication bias46, and there was no significant variation in the newly estimated pooled prevalence as compared to the previous one.
Figure 3.
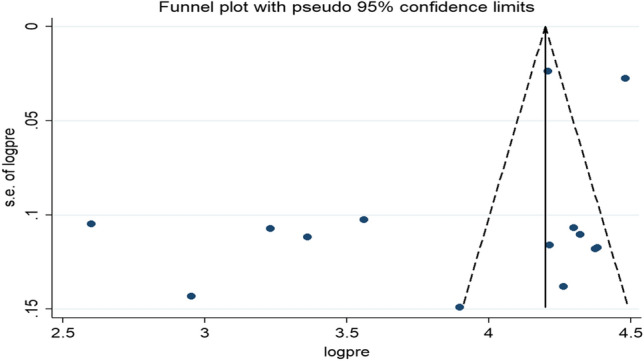
Funnel plot of the pooled prevalence of home child-birth among reproductive-age women in Ethiopia, 2021.
Subgroup analysis and meta-regression
Subgroup analysis was conducted by region, residence, study design and sample size to identify the variation across the individual studies. Even though heterogeneity has still existed in the subgroup analysis of all the aforementioned parameters, the prevalence of home child-birth was significantly higher among studies conducted in rural settings [67.6%, 95% CI: (52.6, 82.6)] as compared to studies conducted in an urban setting. Similarly, the prevalence of home child-birth was significantly different among cross-sectional [60.9, 95% CI: (50.2, 71.8)] and cohort studies [21.1, 95%CI: (6.03, 36.1)] (Table 2).
Table 2.
Subgroup prevalence of home child-birth among reproductive-age women in Ethiopia, 2021 (n = 14).
| Variables | Characteristics | Included studies | Estimate (95% CI) | I2 (%) |
|---|---|---|---|---|
| Region | Amhara | 3 | 45.2(14.9,75.5) | 99.5 |
| SNNPR | 5 | 56.6(28.4, 84.9) | 99.6 | |
| Others | 6 | 59.2(44, 74.3) | 99.8 | |
| Residence | Urban | 2 | 24 (14.5, 33.5) | 89.3 |
| Rural | 3 | 67.6 (52.6, 82.6) | 97.2 | |
| Rural and urban | 9 | 58.1( 43.4, 72.9) | 99.8 | |
| Sample size | < 500 | 8 | 58.8(42.3, 75.4) | 99.2 |
| ≥ 500 | 6 | 50.5(31.6, 69.5) | 99.9 | |
| Study design | Cross-sectional | 12 | 60.9 (50.2, 71.8) | 99.7 |
| Cohort | 2 | 21.1( 6.03, 36.1) | 97.1 |
SNNPR-Southern Nation Nationalities and Peoples Region; others- Benishangul Gumuz, Tigray, Afar, Oromia and EDHS based.
To identify the possible source of variation across the included studies, univariate meta-regression analysis was conducted using study-level characteristics (study year and sample size) as a cofactor, but none of them were found to be statistically significant (Table 3).
Table 3.
Univariate meta-regression analysis to determine factors related to the heterogeneity of the prevalence of home child-birth in Ethiopia, 2021.
| Variables | Coefficient | P value |
|---|---|---|
| Sample size | 0.0028425 | 0.225 |
| Study year | − 2.668666 | 0.492 |
Factors associated with home child-birth
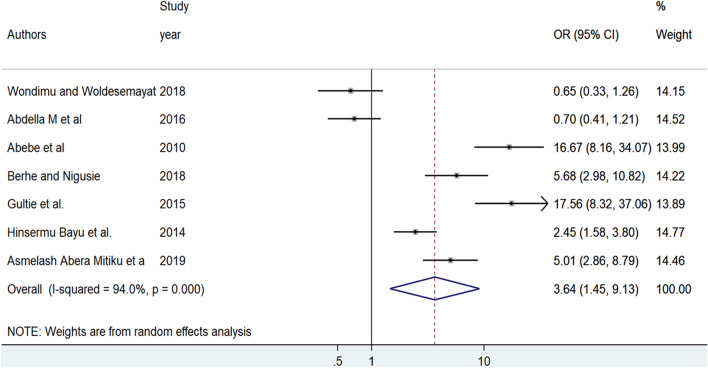
The effect of lack of ANC visit on home delivery was examined based on the results of seven studies8,9,27,28,33,36,38. The analysis revealed that women who have no ANC visit were 3.64 times more likely to deliver at home as compared to women who have ANC visit [OR = 3.64, 95%, CI: (1.45, 9.13)]. A random-effect meta-analysis model was employed to examine the association between lack of ANC visit and home delivery as a result of significant heterogeneity among the included studies (I2 = 94%, p = 0.000) (Fig. 4).
Figure 4.
Forest plot of the pooled odds ratio of lack of ANC visit among reproductive age in Ethiopia, 2021.
Publication bias was assessed using both funnel plots and Egger's tests. Although the funnel plot seems asymmetric (Fig. 5), the result of Egger's test witnessed that there was no statistical evidence of publication bias in the pooled effect of lack of ANC visit on home child-birth (P = 0.302).
Figure 5.
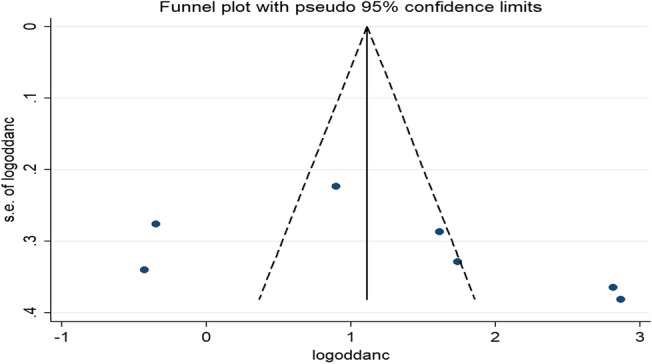
Funnel plot of the pooled odds ratio of lack of ANC visit among reproductive-age women in Ethiopia, 2021.
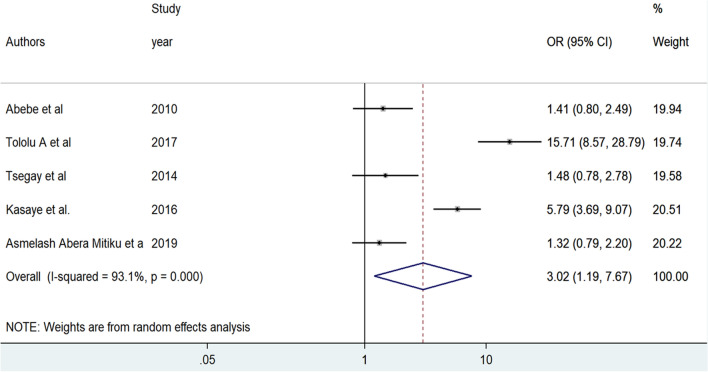
A total of five studies were included to identify the association between unwanted pregnancy and home delivery28–30,33,37. The random-effect meta-analysis revealed that women who experienced unwanted pregnancy were 3.02 times more likely to give birth at home as compared to women with wanted pregnancy [OR = 3.02, 95%CI: (1.19, 7.67)]. Sever heterogeneity was exhibited among the included articles (I2 = 93.1%, p = 0.000) (Fig. 6).
Figure 6.
Forest plot of the pooled odds ratio of unwanted pregnancy among reproductive-age women in Ethiopia, 2021.
There was no evidence of significant publication bias in the pooled effect of unwanted pregnancy on home delivery as it was indicated by Egger's tests (P = 0.832) despite the asymmetrical distribution of the effect estimates on the funnel plot (Fig. 7).
Figure 7.
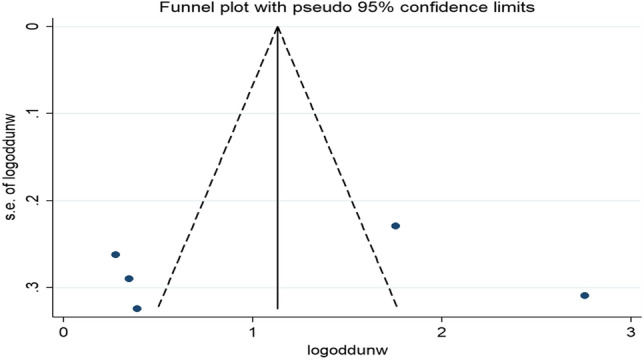
Funnel plot of the pooled odds ratio of unwanted pregnancy among reproductive-age women in Ethiopia, 2021.
Discussion
In this meta-analysis, the pooled prevalence of home child-birth among reproductive-age women in Ethiopia was 55.3% (95% CI: 43, 67.5). Lack of ANC visit and unwanted pregnancy had a statistically significant association with home delivery.
The pooled prevalence of home child-birth was in line with a recently published systematic review and meta-analysis study (66.7%)41. It is also in line with the 2019 mini Ethiopian Demographic and health survey report (50%)19 and another study conducted in Tanzania (65%)47. But, the finding was higher than studies conducted in Nepal(41.9%)48 and Burkina Faso (11%)49. The possible explanations for the variation could be due to the differences in the maternal socioeconomic and educational status, accesses to the health facility, quality of health service, media exposure, and health-seeking behavior. The result of subgroup analysis showed the pooled prevalence of home child-birth was significantly higher among studies conducted in rural settings as compared to studies conducted in an urban setting. The finding is similar to a systematic review and meta-analysis study conducted in sub-Saharan Africa50. It is because women living in rural areas face financial constraints, and lack transport access and decision-making power to receive skilled delivery care51. The finding of this meta-analysis indicates how much it is too far to achieve national and international goals to end maternal and infant mortality20,24. Thus, it urges the national government and other responsible individuals to invest their valuable effort to address the problem of home child-birth among women in all areas of the nation.
In this meta-analysis, the likelihood of home child-birth was higher among women who had no ANC visit compared to ANC-booked women. Consistent findings were also reported from studies conducted in Zambia, Malawi, and Kenya52–54. Studies evidenced that factors that predispose women not to use ANC also make them less likely to seek care during delivery55,56. ANC visit is the golden opportunity for pregnant women to discuss the place of delivery and to get information about the risks and complications encountered during pregnancy and delivery. A study conducted in Tanzania showed that women who are well informed about pregnancy complications during ANC visits are more likely to give birth in a health facility57. Failing to capitalize on ANC visits could be a significant missed opportunity to decrease maternal and neonatal mortality as a result of home delivery. Thus, clinicians need to promote the importance of ANC utilization to increase women's skilled delivery service utilization.
Unwanted pregnancy also had a positive association with home child-birth. It was in agreement with two studies conducted in Bangladesh58,59 and a study done in Zimbabwe60. A systematic review and meta-analysis conducted in low- and lower-middle-income countries showed that unwanted pregnancy was associated with a 25–39% reduction in the use of delivery care61. This could be because uncooperative and threatening behaviors from family members and sexual partners are common among women with an unwanted pregnancy and these might limit women’s decision-making power and financial support which might have a negative impact on accessing institutional delivery services61,62. In addition, mothers with unwanted pregnancies may not worried about the health of the baby and might give less value to the expected child so that they do not seek delivery care utilization.
As a limitation, this systematic review and meta-analysis may not be representative of articles published in languages other than English. In addition, most of the included articles were cross-sectional and had a small sample size and thus might affect the pooled effect. Moreover, this meta-analysis may not be representative of all regions of Ethiopia.
Conclusions
The proportion of home child-birth in Ethiopia was considerably high. The lack of ANC visit and unwanted pregnancy had a significant effect on home delivery. Increasing the access to family planning services and strengthening the Information, Education and Communication (IEC) program is vital to decrease unwanted pregnancy and improve maternal health service utilization particularly ANC follow-up to make a home delivery-free community.
Supplementary Information
Acknowledgements
The authors would like to thank all public health staff for their help when needed and Wollo University library for providing an available online database.
Abbreviations
- ANC
Antenatal care
- EDHS
Ethiopia demography and health survey
- HSTP
Health sector transformation plan
- IEC
Information, education and communication
- IESO
Integrated emergency obstetrics and surgery
- JBI
Joana Brigg's institute
- MMR
Maternal mortality ratio
- PRISMA
Preferred reporting items for systematic reviews and meta-analysis
- SBA
Skilled birth attendants
- SDG
Sustainable development goal
- SSA
Sub-Saharan African
- WDA
Women development army
Author's contributions
Y.D. involved in the conception of a research protocol, literature review, study design, data extraction, data analysis, and interpretation; B.K., M.Y., N.C. and M.A. involved in literature review and screening; T.B., E.T., G.B., W.M., A.A., E.A. and B.A. undertake data extraction and quality assessment; R.D. and B.K. involved in the drafting of the manuscript; G.B., A.A., and M.A. involved in reviewing the manuscript. All authors have read and approved the manuscript.
Data availability
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-05260-5.
References
- 1.Unfpa WHO. The World Bank, United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. Geneva: WHO; 2015. [Google Scholar]
- 2.Csace I. Ethiopia demographic and health survey 2016. Addis Ababa: CSA and ICF; 2016. [Google Scholar]
- 3.Abdella, A. Maternal mortality trend in Ethiopia. Ethiop. J. Health Dev. 2010;24(1).
- 4.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob. Health. 2014;2(6):e323–e333. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 5.Harvey SA, Ayabaca P, Bucagu M, Djibrina S, Edson WN, Gbangbade S, et al. Skilled birth attendant competence: an initial assessment in four countries, and implications for the Safe Motherhood movement. Int. J. Gynecol. Obstet. 2004;87(2):203–210. doi: 10.1016/j.ijgo.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Rockers PC, Wilson ML, Mbaruku G, Kruk ME. Source of antenatal care influences facility delivery in rural Tanzania: a population-based study. Matern. Child Health J. 2009;13(6):879–885. doi: 10.1007/s10995-008-0412-7. [DOI] [PubMed] [Google Scholar]
- 7.Kumbani L, Bjune G, Chirwa E, Odland JØ. Why some women fail to give birth at health facilities: a qualitative study of women’s perceptions of perinatal care from rural Southern Malawi. Reprod. Health. 2013;10(1):1–12. doi: 10.1186/1742-4755-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gultie T, Wasihun B, Kondale M, Balcha B. Home delivery and associated factors among reproductive-age women in Shashemene town Ethiopia. J. Women's Health Care. 2016;5(300):2167–2420. [Google Scholar]
- 9.Berhe R, Nigusie A. Magnitude of home delivery and associated factors among child-bearing age mothers in Sherkole District, Benishangul Gumuz regional state-Western-Ethiopia. BMC Public Health. 2020;20:1–7. doi: 10.1186/s12889-020-08919-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Federal democratic republic of Ethiopia: Ministry of health. Addis Ababa, Ethiopia, 2006.
- 11.Wagle RR, Sabroe S, Nielsen BB. Socioeconomic and physical distance to the maternity hospital as predictors for the place of delivery: an observation study from Nepal. BMC Pregnancy Childbirth. 2004;4(1):1–10. doi: 10.1186/1471-2393-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abeje G, Azage M, Setegn T. Factors associated with Institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community-based cross-sectional study. Reprod. Health. 2014;11(1):1–7. doi: 10.1186/1742-4755-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14(1):1–13. doi: 10.1186/1471-2393-14-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop. J. Health Sci. 2014;24:93–104. doi: 10.4314/ejhs.v24i0.9s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yebyo H, Alemayehu M, Kahsay A. Why do women deliver at home? Multilevel modeling of Ethiopian National Demographic and Health Survey data. PLoS One. 2015;10(4):e0124718. doi: 10.1371/journal.pone.0124718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Celik Y, Hotchkiss DR. The socio-economic determinants of maternal health care utilization in Turkey. Soc. Sci. Med. 2000;50(12):1797–806. doi: 10.1016/S0277-9536(99)00418-9. [DOI] [PubMed] [Google Scholar]
- 17.Mayhew M, Hansen PM, Peters DH, Edward A, Singh LP, Dwivedi V, et al. Determinants of skilled birth attendant utilization in Afghanistan: a cross-sectional study. Am. J. Public Health. 2008;98(10):1849–56. doi: 10.2105/AJPH.2007.123471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DelBarco R. Monitoring birth preparedness and complication readiness. Tools and indicators for maternal and newborn health. Baltimore: Jhpiego; 2004. [Google Scholar]
- 19.CSA I. Ethiopia Mini Demographic and Health Survey 2019: key indicators report. Central statistics agency (CSA) [Ethiopia] and ICF. Addis Ababa: CSA and ICF. 2019.
- 20.Ministry of Health. Ethiopian Health Sector Transformation Plan. 2015/16–2019/20.
- 21.Teferra AS, Alemu FM, Woldeyohannes SM. Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia: A community-based cross-sectional study. BMC Pregnancy Childbirth. 2012;12(1):1–11. doi: 10.1186/1471-2393-12-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nigatu AM, Gelaye KA. Factors associated with the preference of institutional delivery after antenatal care attendance in Northwest Ethiopia. BMC Health Serv. Res. 2019;19(1):1–9. doi: 10.1186/s12913-019-4636-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magadi M, Diamond I, Rodrigues RN. The determinants of delivery care in Kenya. Soc. Biol. 2000;47(3–4):164–188. doi: 10.1080/19485565.2000.9989017. [DOI] [PubMed] [Google Scholar]
- 24.Assembly G. Sustainable development goals. SDGs Transform Our World. 2015;2030.
- 25.Ibrahim, S., Handiso, T., Jifar, M., Yoseph, E. Analyzing prevalence of home delivery and associated factors in Anlemo District, Southern Ethiopia. Int Ann Med. 2017;1(6).
- 26.Ayele G, Tilahune M, Merdikyos B, Animaw W, Taye W. Prevalence and associated factors of home delivery in Arbaminch Zuria district, southern Ethiopia: a community-based cross-sectional study. Science. 2015;3(1):6–9. [Google Scholar]
- 27.Abdella M, Abraha A, Gebre A, Reddy PS. The magnitude and associated factors for home delivery among women who gave birth in last 12 months in Ayssaita, Afar, Ethiopia-2016. A community-based cross-sectional study. Glob. J. Fertil. Res. 2017;2(1):030–9. [Google Scholar]
- 28.Abebe F, Berhane Y, Girma B. Factors associated with home delivery in Bahirdar, Ethiopia: a case-control study. BMC. Res. Notes. 2012;5(1):1–6. doi: 10.1186/1756-0500-5-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tololu, A.K., Massa, M.G., Kerie, M.W., Misgina, K.H., Alema, H.B., Weldu, M.G. Determinants of home delivery in the central zone of Tigrai, North Ethiopia: Evidence from case-control study. 2020.
- 30.Kasaye HK, Endale ZM, Gudayu TW, Desta MS. Home delivery among antenatal care booked women in their last pregnancy and associated factors: a community-based cross-sectional study in Debremarkos town, North West Ethiopia, January 2016. BMC Pregnancy Childbirth. 2017;17(1):1–12. doi: 10.1186/s12884-017-1409-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wodaynew T, Fekecha B, Abdisa B. Magnitude of home delivery and associated factors among antenatal care booked mothers in Delanta District, South Wollo Zone, North East Ethiopia: a cross-sectional study, March 2018. Int. J. Women's Health Wellness. 2018;4(2):1–11. [Google Scholar]
- 32.Chernet AG, Dumga KT, Cherie KT. Home delivery practices and associated factors in Ethiopia. J. Reprod. Infertility. 2019;20(2):102. [PMC free article] [PubMed] [Google Scholar]
- 33.Mitiku, A.A., Dimore, A.L., Mogas, S.B. Determinants of home delivery among mothers in Abobo District, Gambella Region, Ethiopia: A case-control study. Int. J. Reprod. Med. 2020. [DOI] [PMC free article] [PubMed]
- 34.Mekonnen Y, Ayichiluhm M, Dejenu G. Prevalence and determinants of home birth after antenatal care attendance in Gozamin District, Northwest Ethiopia. Health Sci. J. 2015;9(6):1. [Google Scholar]
- 35.Delibo, D., Damena, M., Gobena, T., Balcha, B. Status of home delivery and its associated factors among women who gave birth within the last 12 months in East Badawacho District, Hadiya Zone, Southern Ethiopia. BioMed Res. Int.. 2020;2020. [DOI] [PMC free article] [PubMed]
- 36.Wondimu MS, Woldesemayat EM. Determinants of home delivery among women in rural pastoralist community of Hamar District, Southern Ethiopia: A case-control study. Risk Manag. Healthcare Policy. 2020;13:2159. doi: 10.2147/RMHP.S268977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsegay R, Aregay A, Kidanu K, Alemayehu M, Yohannes G. Determinant factors of home delivery among women in Northern Ethiopia: a case-control study. BMC Public Health. 2017;17(1):1–8. doi: 10.1186/s12889-017-4159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bayu H, Fisseha G, Mulat A, Yitayih G, Wolday M. Missed opportunities for institutional delivery and associated factors among urban resident pregnant women in South Tigray Zone, Ethiopia: a community-based follow-up study. Glob. Health Action. 2015;8(1):28082. doi: 10.3402/gha.v8.28082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Siyoum M, Astatkie A, Mekonnen S, Bekele G, Taye K, Tenaw Z, et al. Homebirth and its determinants among antenatal care-booked women in public hospitals in Wolayta Zone, southern Ethiopia. PloS one. 2018;13(9):e0203609. doi: 10.1371/journal.pone.0203609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kucho B, Mekonnen N. Delivery at home and associated factors among women in childbearing age, who gave birth in the preceding two years in Zala Woreda, southern Ethiopia. J. Public Health Epidemiol. 2017;9(6):177–188. [Google Scholar]
- 41.Ayenew AA, Nigussie AA, Zewdu BF. Childbirth at home and associated factors in Ethiopia: a systematic review and meta-analysis. Arch. Public Health. 2021;79(1):1–8. doi: 10.1186/s13690-021-00569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moher D, Liberati AA, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., et al. Chapter 7: Systematic reviews of etiology and risk. Joanna Briggs Institute Reviewer's Manual The Joanna Briggs Institute. 2017;5.
- 44.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials. 2015;45:139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Duval S, Tweedie R. Trim and fill: a simple funnel–plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 47.Simfukwe M. Factors contributing to home delivery in Kongwa District, Dodoma-September 2008. Dar Es Salaam Med. Stud. J.. 2011;18(1):13–22. [Google Scholar]
- 48.Dhakal P, Shrestha M, Baral D, Pathak S. Factors affecting the place of delivery among mothers residing in Jhorahat VDC, Morang Nepal. Int. J. Commun. Based Nurs. Midwifery. 2018;6(1):2. [PMC free article] [PubMed] [Google Scholar]
- 49.De Allegri M, Tiendrebéogo J, Müller O, Yé M, Jahn A, Ridde V. Understanding home delivery in a context of user fee reduction: cross-sectional mixed methods study in rural Burkina Faso. BMC Pregnancy Childbirth. 2015;15(1):1–13. doi: 10.1186/s12884-015-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wong KL, Benova L, Campbell OM. A look back on how far to walk: systematic review and meta-analysis of physical access to skilled care for childbirth in sub-Saharan Africa. PloS one. 2017;12(9):e0184432. doi: 10.1371/journal.pone.0184432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chakrborty N, Islam MA, Chowdhurg RI, Bori W. Determinants of the use of maternal Health service in rural Bangladesh. Health Promot Int. 2005;18(4):327–337. doi: 10.1093/heapro/dag414. [DOI] [PubMed] [Google Scholar]
- 52.Scott NA, Henry EG, Kaiser JL, Mataka K, Rockers PC, Fong RM, et al. Factors affecting home delivery among women living in remote areas of rural Zambia: a cross-sectional, mixed-methods analysis. Int. J. Women's Health. 2018;10:589. doi: 10.2147/IJWH.S169067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palamuleni M. Determinants of non-institutional deliveries in Malawi. Malawi Med. J. 2011;23(4):104–108. [PMC free article] [PubMed] [Google Scholar]
- 54.Kitui J, Lewis S, Davey G. Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy Childbirth. 2013;13(1):1–10. doi: 10.1186/1471-2393-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nair, M., Ariana, P., Webster, P. What influences the decision to undergo institutional delivery by skilled birth attendants? A cohort study in rural Andhra Pradesh, India. 2012. [PubMed]
- 56.Stephenson R, Baschieri A, Clements S, Hennink M, Madise N. Contextual influences on modern contraceptive use in sub-Saharan Africa. Am. J. Public Health. 2007;97(7):1233–1240. doi: 10.2105/AJPH.2005.071522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, et al. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth. 2007;7(1):1–7. doi: 10.1186/1471-2393-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khan, M.N., Harris, M.L., Loxton, D. Does unintended pregnancy have an impact on skilled delivery care use in Bangladesh? A nationally representative cross-sectional study using Demography and Health Survey data. J. Biosoc. Sci. 2020:1–17. [DOI] [PubMed]
- 59.Rahman MM, Rahman MM, Tareque MI, Ferdos J, Jesmin SS. Maternal pregnancy intention and professional antenatal care utilization in Bangladesh: a nationwide population-based survey. PloS one. 2016;11(6):e0157760. doi: 10.1371/journal.pone.0157760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Muchabaiwa L, Mazambani D, Chigusiwa L, Bindu S, Mudavanhu V. Determinants of maternal healthcare utilization in Zimbabwe. Int. J. Econ. Sci. Appl. Res. 2012;5(2):145–162. [Google Scholar]
- 61.Khan MN, Harris ML, Shifti DM, Laar AS, Loxton D. Effects of unintended pregnancy on maternal healthcare services utilization in low-and lower-middle-income countries: systematic review and meta-analysis. Int. J. Public Health. 2019;64(5):743–754. doi: 10.1007/s00038-019-01238-9. [DOI] [PubMed] [Google Scholar]
- 62.Dahiru, T., Oche, O.M. Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr. Med. J. 2015;22(1). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.