Abstract
Although the etiology of obsessive–compulsive disorder (OCD) is largely unknown, it is accepted that OCD is a complex disorder. There is a known bi-directional interaction between the gut microbiome and brain activity. Several authors have reported associations between changes in gut microbiota and neuropsychiatric disorders, including depression or autism. Furthermore, a pediatric-onset neuropsychiatric OCD-related syndrome occurs after streptococcal infection, which might indicate that exposure to certain microbes could be involved in OCD susceptibility. However, only one study has investigated the microbiome of OCD patients to date. We performed 16S ribosomal RNA gene-based metagenomic sequencing to analyze the stool and oropharyngeal microbiome composition of 32 OCD cases and 32 age and gender matched controls. We estimated different α- and β-diversity measures and performed LEfSe and Wilcoxon tests to assess differences in bacterial distribution. OCD stool samples showed a trend towards lower bacterial α-diversity, as well as an increase of the relative abundance of Rikenellaceae, particularly of the genus Alistipes, and lower relative abundance of Prevotellaceae, and two genera within the Lachnospiraceae: Agathobacer and Coprococcus. However, we did not observe a different Bacteroidetes to Firmicutes ratio between OCD cases and controls. Analysis of the oropharyngeal microbiome composition showed a lower Fusobacteria to Actinobacteria ratio in OCD cases. In conclusion, we observed an imbalance in the gut and oropharyngeal microbiomes of OCD cases, including, in stool, an increase of bacteria from the Rikenellaceae family, associated with gut inflammation, and a decrease of bacteria from the Coprococcus genus, associated with DOPAC synthesis.
Subject terms: Obsessive compulsive disorder, Biomarkers
Introduction
Obsessive-compulsive disorder (OCD) is a neuropsychiatric disorder characterized by intrusive and unwanted thoughts (termed obsessions) and repetitive behaviors or mental acts (called compulsions) that are performed to partially relieve the anxiety or distress caused by the obsessions. The etiology of OCD is largely unknown, although it likely involves a combination of genetic, neurobiological and environmental factors or events. Genetic association studies, including genome-wide association analysis and a multispecies approach integrating evolutionary and regulatory information, have highlighted genes involved in dopamine, serotonin and glutamate signaling, synaptic connectivity and the cortico-striato-thalamo-cortical circuit (CSTC)1–5.
Several researchers have speculated that the microbiome might also play a role in the development of OCD6–8. In fact, a recent pilot study of the gut microbiome in OCD has observed some dysbiosis in OCD cases compared to controls9; a previous work observed a difference in gut microbial composition in deer mice presenting an obsessive behavior compared to the normal mice10; microbial treatments such as germ-free environment and probiotic treatments can modify OCD-like behavior in rodents11; and some OCD risk factors, such as stress, pregnancy or antibiotic use, are known to disrupt the gut microbiome6. Moreover, it is recognized that some children, after suffering a streptococcal infection, present with a sudden onset of tics, OCD and other behavioral symptoms, a condition known as pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections syndrome (PANS/PANDAS)12,13.
There is a well-known bi-directional interaction between the gut microbiota and brain activity14,15. Brain function can be affected by endocrine-, neurocrine- and inflammation-related signals from the gut microbiota, while psychological and physical stressors can affect the composition of the gut microbiome16,17. Differences in the composition of the gut microbiome have been associated to depression18, autistic disorder19–21, or schizophrenia22, among other psychiatric disorders (reviewed in Nikolova, et al.23). Moreover, two studies have found differences in gut bacterial distribution when OCD cases or PANS/PANDAS patients are compared to healthy age-matched individuals9,24. On the other hand, some studies have also shown an alteration of the oropharyngeal microbiome in patients with autism25,26 or schizophrenia27. However, so far, only one study has explored a potential link between gut microbiota and OCD, and the OCD oral microbiota has not been explored yet. Given that, in some cases, OCD-like symptoms develop after an acute streptococcal infection, we hypothesized that there could be differences between OCD cases and controls in the microbiome composition of the tonsils and back of the throat. Here, we explore the composition of fecal and oropharyngeal microbiota of OCD-patients before and after treatment and compare it to healthy matched controls.
Material and methods
Sample collection
Thirty-eight patients (20 females; mean age = 40.16 ± 14.12, see Table 1) with a diagnosis of OCD with at least one year of development were recruited from the OCD clinic at Bellvitge Hospital (Barcelona, Spain) from January 2016 to September 2017. Diagnoses were assigned by two psychiatrists with extensive clinical experience in OCD, following the DSM-IV criteria for OCD diagnosis28 and using the Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-I)29. A summary of the patients’ clinical data is provided in supplementary Table S1. Patients presenting psychoactive substance abuse/dependence (current or in the past six months), psychotic disorders, intellectual disability, severe organic or neurological pathology (excepting tic disorder), or autism spectrum disorder were excluded from the study. Other affective and anxiety disorders were not criteria for exclusion in cases where OCD was the main diagnosis.
Table 1.
Age and gender characteristics for the control and OCD sample cohorts.
| Group | Female | Male | Age | Diet | |||||
|---|---|---|---|---|---|---|---|---|---|
| Aver (SD; range) | Q6 | Q7 | Q11 | Q12 | Q17 | Q18 | |||
| OCD | 20 | 18 | 40.16 (14.12; 18–71) | 1.5 | 2.4 | 3.1 | 2.2 | 2.1 | 2.5 |
| Control | 18 | 15 | 36.00 (9.87; 23–59) | 2.15 | 2.4 | 3.6 | 2.1 | 2.1 | 2.5 |
Female/Male: number of female/male participants; Aver: average; SD: standard deviation; Diet: average value for group responses to questionnaire questions Q6 (alcohol); Q7 (yoghurt, kefir…); Q11 (vegetables); Q12 (beans); Q17 (red meat) and Q18 (white meat); values range from 1 (not in last 7 days) to 4 (daily). For more details, see questionnaire in supplementary table S3.
Thirty-three healthy controls (18 females; mean age = 36 ± 9.87) were recruited from the same sociodemographic environment and constituted a comparable sample in terms of age and gender (see Table 1 and supplementary Table S2 for a summary of clinical information on controls). Prior to inclusion, each control participant underwent the Structured Clinical Interview for DSM-IV non-patient version (SCID-NP)30 to exclude presence or history of any psychiatric disorder.
Written informed consent was obtained from all participants after a complete description of the study, which was performed in accordance with the Declaration of Helsinki (2013) and approved by Bellvitge Hospital’s ethical committee.
Stool samples from 28 OCD cases at two time-points (before (OCD T0) and after (OCD T3) three months of pharmacological treatment and cognitive behavioral therapy), 7 OCD cases at a single time-point (4 OCD T0 and 3 OCD T3), and 33 healthy subjects were collected in Stool Collection Tubes (Stratec Molecular) and delivered at room temperature following manufacturer’s guidelines. Samples were stored at − 20 °C until processed. DNA was extracted using the PSP Spin Stool DNA Basic Kit (Stratec Molecular).
Oropharyngeal swab samples, corresponding to the tonsils and the back of the throat, from 28 OCD cases at two time-points, 8 single timepoint OCD cases (4 OCD T0 and 4 OCD T3) and 32 healthy individuals were collected with the Catch-All sample collection swabs (Epicentre), conserved in PowerBead tubes (MO BIO Laboratories), frozen at − 20 °C and processed for DNA extraction with the PowerSoil DNA Isolation kit (MO BIO Laboratories). Details for the overlap between stool T0, stool T3, oropharyngeal T0 and oropharyngeal T3 samples are provided in Figure S1.
Sample sizes were deemed appropriate for this exploratory approach considering previous similar studies of microbiota involvement in other psychiatric disorders9,19,22,24,25,27, performed with similar sample sizes.
All participants were asked to provide dietary information through a questionnaire (supplementary tables S3 and S4). Severity of the obsessive and compulsive symptoms before and after treatment among the OCD patients was assessed through the clinician-administered version of the Yale-Brown Obsessive Compulsive Scale (Y-BOCS)31. A global measure as well as independent ones for both obsessions and compulsions were taken. Table 1 and supplementary Tables S1 and S2 summarize the main characteristics of the OCD and control cohorts.
Sequencing and data analysis
16S ribosomal RNA (rRNA) sequencing was performed by the UPF Genomics Core Facility following Illumina’s protocol with slight modifications. Briefly, in each sample, the variable V3-V4 region of the 16S rRNA gene was amplified for 35 cycles using the primers described in Klindworth et al.32 and Platinum High Fidelity Taq (Thermofisher) and purified, followed by 8 cycles of indexing PCR, and quantification. The indexed products were then pooled in an equimolar way in two final amplicon libraries (one for stool and one for tonsils), each containing 96 samples. Each library was sequenced in one 2 × 300 bp paired-end sequencing run on a MiSeq System.
The DADA2 R package (version 1.6.0)33 was employed to obtain counts of amplicon sequence variants (ASV), and sequence taxonomy was assigned using the SILVA database34. Resulting ASV counts, along with clinical data and diet information collected for each individual, were stored and analyzed using the Phyloseq package (version 1.22.3). Taxa that did not appear in at least 10% of samples were filtered out prior to analyses. 16S counts were normalized per sample, obtaining the relative abundance of each taxon within a sample, with all values ranging between 0 and 100.
We estimated different α- (within samples) and β-diversity (between samples) measures using the Phyloseq, picante and vegan R packages (see supplementary material for details). α-diversity indices included the Shannon and Simpson Diversity Index, Faith’s phylogenetic diversity, the observed species index, the Chao1 index and the ACE (Abundance-based Coverage Estimator) index. β-diversity measures included Unifrac distances, the Bray–Curtis dissimilarity, Jensen-Shannon diversity and Canberra indices. We performed a PERMANOVA test on β-diversity with 999 permutations considering even dependence of samples (paired OCD samples after and before treatment). Finally, we applied a Principal Coordinate Analysis (PCoA) to visualize the clustering of the samples.
Statistical analysis
Correlation between categorical variables (i.e. sample type, type of obsessions, etc.) and taxa abundances or other continuous variables was tested using the Kruskal–Wallis rank sum test, and correlation between two categorical variables was tested using Chi-squared tests. Statistical significance of α-diversity differences between groups was evaluated with Mann–Whitney U test when samples were independent, and with Wilcoxon rank-sum test when samples were paired. In all cases, we applied the Bonferroni correction to adjust the p values by the number of comparisons and provide only corrected p values. Correlation plots and boxplots were generated using ggplot2 (version 2.2.1) and association plots were generated using the assoc function from the R package vcd (version 1.4.4).
Linear discriminant analysis Effect Size (LEfSe) was performed using the Huttenhower lab’s tool implemented in Galaxy web35. For the statistical test we used an α value of 0.05 and a logarithmic LDA score threshold of 2.0.
Results
High-throughput sequencing analysis of bacterial 16S rRNA V3–V4 regions was conducted on fecal and oropharyngeal samples of the 32 OCD (two timepoints) and 33 control individuals (see Figure S1). In total, 8,653,960 high-quality reads (90,145.42 ± 15,356.44 reads/sample) were obtained from all 96 fecal samples, representing 196 operational taxonomic units (OTUs) when considering all samples, while each sample had, on average, 91.77 ± 17.51 OTUs. For the 96 oropharyngeal samples, 6,051,021 high-quality reads (63,031.47 ± 16,555 reads/sample) were obtained, representing 81 operational taxonomic units for all samples, with an average of 32.22 ± 9.29 OTUs/sample.
While statistical analyses revealed some differences between cases (at T0 and/or at T3) and controls, no statistically significant differences were identified when comparing OCD cases before and after treatment (T0 vs T3). On the other hand, we observed some association between some of the diet variables and taxa abundances, but there were no significant associations between the variables collected in the diet questionnaires and whether the individual belonged to the OCD or control group, which suggests that the taxa differences between OCD cases and controls may be influenced by the OCD phenotype, rather than by other variables.
OCD samples show a trend towards lower bacterial α- diversity in the gut
Analysis of the microbial composition of the gut showed that OCD T0 samples presented an overall lower level of all α-diversity indices compared to the control group, although no test reached statistical significance after adjusting for multiple testing (Bonferroni adjusted p value = 0.057) (Fig. 1A). These differences were reduced in the OCD T3 group, which was much closer to the control group (Bonferroni adjusted p value = 0.67) than the OCD T0 group (Bonferroni adjusted p value = 0.052). On the other hand, we did not observe a strong separation of sample groups based on the β-diversity measures (Figure S2), and there were no statistical differences between the Bacteroidetes to Firmicutes ratio when comparing OCD samples to controls (Wilcoxon rank-sum test Bonferroni adjusted p value = 0.0653; Fig. 2A). In all three groups, the 20 most abundant genera belonged to either the Bacteroidetes or Firmicutes Phyla, while at the family level there was also representation of Proteobacteria, Verrucomicrobia and Actinobacteria, albeit at very low abundances (Figure S3).
Figure 1.
Boxplots representing α-diversity indices: Observed, Chao1, ACE, Shannon, Simpson, Inverted Simpson, Fisher and PD. The plots represent the median, 25th, and 75th percentiles calculated for Controls (red), OCD T0 (green) and OCD T3 (blue) in stool samples (A) or oropharyngeal samples (B). The corresponding Bonferroni adjusted p values are reported below each index (OCD T0 vs controls and OCD T3 vs controls was calculated with Mann–Whitney U test; OCD T0 vs 0CD T3 with Wilcoxon rank-sum test).
Figure 2.
Notched boxplots representing the values of the ratio for the two most abundant taxa in each area: (A) Firmicutes to Bacteroidetes ratio in gut samples from Control, OCD T0 and OCD T3 subjects. (B) Fusobacteria to Actinobacteria ratio in Oropharyngeal samples from Control, OCD T0 and OCD T3 subjects. Bonferroni adjusted p value of Wilcoxon rank-sum test between Controls and OCD T0, and controls and OCD T3 are indicated.
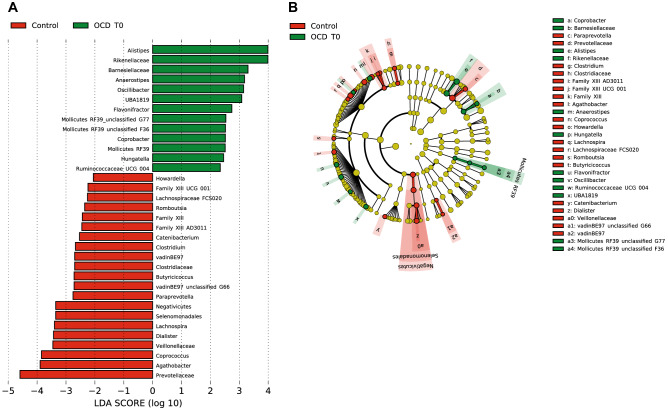
LEfSe results reveal an enrichment for Rikenellaceae and depletion of Prevotellaceae, and a shift from Coprococcus to Flavonifractor within the Clostridiales in the gut
LEfSe analysis revealed a significant increase of the relative abundance of Rikenellaceae, particularly of the Alistipes genus, and a decrease in the levels of Prevotellaceae, in OCD T0 stool samples compared to controls (Fig. 3). We also observed a different distribution of bacteria from the order Clostridiales, where OCD T0 samples presented a higher abundance of the genera Oscillibacter, Anaerostipes and Flavonifractor, and a depletion of Agathobacter, Coprococcus, Lachnospira, Howardella, Romboutsia, Butyricicoccus and Clostridium compared to controls. In addition, within these, depletion of Lachnospira pectinoschiza correlated with OCD severity on the obsessions subscale (YBOCS_OBS_0 vs Species Lachnospira pectinoschiza r = -0.420). Relative abundances in stool samples from cases and controls for these taxa are presented in Table S5. Most of these differences are also present when comparing OCD post-treatment samples versus controls (Figure S4).
Figure 3.
(A) Biomarkers associated with OCD and control groups discovered by LEfSe analysis (α value = 0.05, logarithmic LDA score threshold = 2.0) in stool samples. (B) Cladogram representing the phylogenetic relationship of biomarkers associated with OCD and control groups through the Linear discriminant Effect Size (LEfSe) analysis (α value = 0.05, logarithmic LDA score threshold = 2.0) in stool samples.
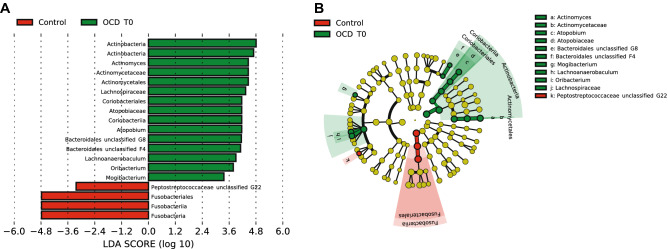
In the oropharyngeal microbiome, OCD samples show a lower Fusobacteria to Actinobacteria ratio
Again, in the analysis of the oropharyngeal microbiome, α-diversity indices did not show significant differences between the OCD and control groups (Fig. 1B). Similarly, we did not see any separation of sample groups based on most β-diversity measures (Figure S5). However, there was a significant difference in the ratio of Fusobacteria to Actinobacteria when comparing OCD samples (T0 and T3) to controls (Wilcoxon rank-sum test p value = 0.004; c, Fig. 2B), where OCD samples had lower ratios. Bacterial diversity in the oropharyngeal samples was lower than in the stool samples (Shannon diversity: Stool = 3.17 ± 0.46, oropharyngeal = 2.46 ± 0.45; Faiths PD: Stool = 23.18 ± 4.00, oropharyngeal = 15.25 ± 4.53). Among the 20 most abundant genera, the largest contribution belonged to the Actinobacteria and Fusobacteria phyla, although Epsilonbacteraeota (e.g. Campylobacter), Bacteroidetes, Firmicutes and Proteobacteria were also represented (Figure S6).
LEfSe analysis of the oropharyngeal microbiome data revealed an increase of species within the Actinobacteria and Coriobacteriia classes in the OCD samples: particularly, the genera Actinomyces and Atopobium represented a higher percentage of total bacteria in OCD T0 compared to control samples; there was also an increase of Lachnospiraceae and other Firmicutes. In contrast, control samples had a higher percentage of bacteria from the Fusobacteriia class (Fig. 4). Analysis of OCD T3 vs controls highlighted again the increase of the Actinobacteria and Coriobacteriia (Figure S7). Relative abundances in oropharyngeal samples from cases and controls for these taxa are presented in Table S6.
Figure 4.
(A) Biomarkers associated with OCD and control groups discovered by LEfSe analysis (α value = 0.05, logarithmic LDA score threshold = 2.0) in oropharyngeal samples. (B) Cladogram representing the phylogenetic relationship of biomarkers associated with OCD and control groups through the Linear discriminant Effect Size (LEfSe) analysis (α value = 0.05, logarithmic LDA score threshold = 2.0) in oropharyngeal samples.
We also performed a directed analysis of enrichment of Streptococcus in OCD samples versus controls, as this genus has been shown to be associated to the onset of PANDAS24. However, the top 15 most abundant species did not include bacteria form this genus in either OCD T0, OCD T3, or controls.
Discussion
We have performed an explorative comparative analysis of the gut (fecal) and oropharyngeal microbiome between OCD cases (before and after treatment) and age- and gender-matched healthy controls, via 16S rRNA amplicon sequencing.
While our analysis shows only a trend towards lower bacterial diversity in the gut of OCD patients which is not significant after correction for multiple testing, this result is consistent with the lower gut α-diversity in PANS/PANDAS patients reported by Quagliariello, et al.24, and in OCD by Turna, et al.9. Lower α-diversity has also been reported in subjects with attention deficit hyperactivity disorder36, and in some studies of ASD individuals37–39. While it is not consistently observed, and may be dependent on the cohort characteristics, including sample size, it should be noted that most of these studies, as ours, are exploratory analyses with small sample sizes.. However, a recent meta-analysis of microbiota in psychiatric disorders, taking into account most of these studies, reports a significant decrease in observed species in patients vs controls23. In addition, in the analysis of Quagliariello, et al.24 they also observed, in the younger subset of PANS/PANDAS patients (aged 4–8 years), a higher percentage of Bacteroidetes and lower level of Firmicutes, while we did not observe significant shifts in the Bacteroidetes to Firmicutes ratio. This discrepancy between our results and those of Quagliariello, et al.24 could be related to the age of our subjects, as all our patients are adults, while their study was performed on pediatric cases. However, we did not observe a correlation between age and any of the taxa ratios tested. Additional analyses on larger cohorts should clarify the observed trends.
The Wilcoxon and LEfSe tests performed here highlighted differences in OTU abundances in the gut. At the family level, we observed an increase of bacteria from the Rikenellaceae family, which had been reported as a biomarker of PANDAS24. In addition, an increase in abundance of Rikenellaceae has also been reported in ADHD40 and major depressive disorder (MDD)41. This bacterial family and, specifically, the Alistipes genus, is also positively associated with gut inflammation in human and mice studies42,43. Recently, a study linked neuroinflammation throughout the cortico-striatal-thalamo-cortilcal (CSTC) circuit to OCD44. Considering these observations, it is tempting to speculate a possible link between the neuroinflammation observed in OCD patients and the higher abundance of Alistipes and Rikenellaceae in these patients. Finally, OCD T0 samples showed lower levels of bacteria of the Prevotellaceae family, similarly to reports on ASD39.
LEfSe analysis also found specific members of the Firmicutes phylum with higher abundance in OCD T0 samples: Oscillibacter, Anaerostipes, and Flavonifractor, and a lower abundance of Coprococcus and Lachnospira; futhermore, abundance of Lachnospira pectinoschiza was also negatively correlated with severity, in line with the depletion in cases compared to controls. While several of these differences are maintained when comparing OCD post-treatment samples to the control group, the decrease in the genus Lachnospira is not. Furthermore, Valles-Colomer, et al.18 report a correlation of four mental well-being scores (measured by the RAND-36 health-related quality of life survey) with higher abundance of Coprococcus, and two of these (social functioning and emotional well-being) also correlate with a lower abundance of Flavonifractor genus in the gut microbiota. We observe precisely the opposite trend in our cohort of OCD patients, where OCD patients have lower abundance of Coprococcus and higher abundance of Flavonifractor. The relative abundance of Coprococcus in the aforementioned study was strongly associated with the microbial pathway for DOPAC (a dopamine metabolite) synthesis. Relevantly, dopaminergic transmission has been implicated in the neurobiology of OCD, as dopamine receptor agonists are effective as an augmentation therapy to selective serotonin reuptake inhibitors in reducing OC symptoms45, and OCD patients under deep brain stimulation show improvements associated with release of striatal dopamine46.
However, our results are not replicating the findings by Turna, et al.9. In their study, they observed a lower relative abundance of Oscillospira, Odoribacter and Anaerostipes. We do not see a significant difference for Oscillospira and Odoribacter, although a detailed look at the data show that, for Oscillospira, a similar trend is present, with lower abundance in OCD T0 samples compared to controls, and an increase in abundance in OCD T3 samples (supplementary table S5, figure S8). On the other hand, in the case of Anaerostipes we observe an increase of these bacteria as opposed to what was previously reported. These differences might be explained by chance, as both studies have a small, exploratory, sample size, or it could be related to dietary differences or to methodological differences in the analysis between both studies.
We also analyzed the oropharyngeal microbiome of OCD cases and controls. While the composition of the oral microbiome has received little attention in relation with psychiatric diseases, there are some studies that indicate possible changes in the oral microbiota of Parkinson’s disease or autistic disorder26,47,48. In addition, the bacterial composition of the oral cavity might be used to represent the composition of the upper gastrointestinal tract49. Furthermore, in this case we were particularly interested in the evaluation of the presence of Streptococcus pyogenes, as a potential biomarker of OCD, as it had been associated with PANDAS50, but we did not detect this species in our dataset. The available data of this cohort could not rule out whether a previous streptococcal infection might have triggered the disease and lead to the current difference in microbiome composition. We then analyzed bacterial diversity measures between cases and controls without observing an overall difference in α-diversity. We did observe a significantly higher Actinobacteria to Fusobacteria ratio in OCD T0 compared to controls, which is still present, but reduced, after treatment. This difference correlated with an increase in Actinomycetales and a decrease of Fusobacteriales observed in the LEfSe analysis. We then analyzed whether the Fusobacteria to Actinobacteria ratio could be used as a proxy for the increased abundance of Alistipes and Rikenellaceae in the gut microbiome, but we did not detect a significant correlation with either Alistipes or Rikenellaceae. The Fusobacteria/Actinobacteria ratio was, however, correlated with the presence of the Coprococcus genus or the Eggerthellaceae family (Figure S9).
Additionally, we explored changes in the microbiome after 3 months of treatment (pharmacological and cognitive behavioral therapy). While no statistically significant differences were observed between pre and post-treatment samples (OCD T0 vs OCD T3 Bonferroni adjusted p value = 0.052), the OCD T3 samples presented gut α-diversity values closer to the control samples than to the OCD T0 group. On the other hand, the top overrepresented and underrepresented taxa in the OCD T0 group identified by LEfSe analysis mostly persist in the OCD T3 dataset. It has been reported that SSRI treatment cause a decrease in abundance for certain taxa (reviewed in Weersma, et al.51), but these do not overlap with the ones identified by LEfSe and wilcoxon tests as potential biomarkers for OCD.
Finally, we considered the potential effect of dietary factors on microbiome composition by including questions related to food consumption for the last week at the time of sample collection in cases and controls. There were no significant differences between cases and controls in the responses to the questionnaire, indicating that while dietary factors have an effect on microbiome composition52, they are unlikely to explain the differences observed between patients and controls.
While our results support an imbalance in OCD cases, both in the gut and the oropharyngeal microbiome, it is not possible to establish a causal relationship, as the observed changes in the microbiome can be both a cause or a consequence of the disorder. It has been shown that the brain can modulate the gut microbiome by a top-down function of the gut-brain axis. For instance, the lower α-diversity observed in OCD cases could be a consequence of the anxiety provoked by obsessions. Since our study included only patients already diagnosed with OCD, it is not possible to discern between cause and effect.
Further studies involving animal models, larger sample sizes, longitudinal cohorts and eventually, interventional experiments, should help understand the contribution of intestinal and oral microbiota to obsessive–compulsive disorder. In this regard, a recent animal study points toward the existence of an underlying aetiological association between alterations in gut microbiota and development of obsessive–compulsive behavior10. Our analysis has some limitations: the study sample size is relatively small, although in line with other exploratory studies in autism or depression; on the other hand, gut microbiome composition has been analyzed through the bacterial composition of stool samples, which represents mostly the composition of the colon, while underestimating that of other regions of the gut such as the small intestine. Nevertheless, most studies on the gut microbiome use this same sample source, as it is more accessible and less invasive.
In summary, our results and those of others indicate that the gut microbiome might be playing a role in the pathogenesis of OCD, which might involve an increase in inflammation levels related to overabundance of bacteria in the Alistipes genus, or be related to a decrease in abundance of Prevotella and Coprococcus genera, the latter associated with the microbial DOPAC synthesis pathway. While awaiting confirmation on additional cohorts, these results open the door to further explorations into possible interventions directed to the modulation of both the microbiota in OCD patients or the mechanisms through which they exert their effect.
Supplementary Information
Acknowledgements
This project was supported by grants from the Spanish ministry of science and innovation (MICINN; SAF2013-49108-R); the Carlos III Health Institute (PI16/00950, PI18/00856, PI19/01184); FEDER funds (‘A way to build Europe’) and by the Agency of University and Research Funding Management of the Catalan Government (2014 SGR 1672 and 2017 SGR 738). We thank CERCA Programme / Generalitat de Catalunya for institutional support. LD was supported by a Severo Ochoa grant (SVP-2013-068066), MA was supported by the Secretariat for Universities and Research of the Ministry of Business and Knowledge of the Government of Catalonia Grant co-funded by the European Social Fund (ESF) “ESF, Investing in your future” (2017 FI_B 00327), DSC was supported by a grant from the MICINN (BES-2014-069814) and RR was supported by a fellowship from the Health Department of the Generalitat de Catalunya through the PERIS 2016-2020 program (SLT002/16/00310).
Author contributions
L.D., G.E., D.S.C., X.E., P.A., and R.R. participated in the design of the study and development of the protocol. L.D. M.A., E.R., and Sara B. recruited participants. E.R., Sara B., C.S., J.M.M and P.A. performed clinical evaluations, collected clinical data and, together with M.A. and L.D., analyzed clinical data. L.D., M.M and D.S.C performed experimental procedures. L.D., G.E., J.W., T.G., Susanna B, and R.R. participated in the NGS microbiome data analysis. All authors discussed data interpretation. L.D., J.W. and R.R. wrote the first draft of the manuscript. All authors contributed to the final manuscript and approved the final version.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Pino Alonso and Raquel Rabionet.
Contributor Information
Pino Alonso, Email: mpalonso@bellvitgehospital.cat.
Raquel Rabionet, Email: kelly.rabionet@ub.edu.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-05480-9.
References
- 1.Stewart SE, et al. Genome-wide association study of obsessive-compulsive disorder. Mol. Psychiatry. 2013;18:788–798. doi: 10.1038/mp.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mattheisen M, et al. Genome-wide association study in obsessive-compulsive disorder: Results from the OCGAS. Mol. Psychiatry. 2015;20:337–344. doi: 10.1038/mp.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noh HJ, et al. Integrating evolutionary and regulatory information with a multispecies approach implicates genes and pathways in obsessive-compulsive disorder. Nat. Commun. 2017;8:774. doi: 10.1038/s41467-017-00831-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Servaes S, Glorie D, Verhaeghe J, Stroobants S, Staelens S. Preclinical molecular imaging of glutamatergic and dopaminergic neuroreceptor kinetics in obsessive compulsive disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2017;77:90–98. doi: 10.1016/j.pnpbp.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 5.Gasso P, et al. Association between genetic variants related to glutamatergic, dopaminergic and neurodevelopment pathways and white matter microstructure in child and adolescent patients with obsessive-compulsive disorder. J. Affect. Disord. 2015;186:284–292. doi: 10.1016/j.jad.2015.07.035. [DOI] [PubMed] [Google Scholar]
- 6.Rees JC. Obsessive-compulsive disorder and gut microbiota dysregulation. Med. Hypotheses. 2014;82:163–166. doi: 10.1016/j.mehy.2013.11.026. [DOI] [PubMed] [Google Scholar]
- 7.Turna J, Grosman Kaplan K, Anglin R, Van Ameringen M. "What's bugging the gut in Ocd?" A review of the gut microbiome in obsessive-compulsive disorder. Depress Anxiety. 2016;33:171–178. doi: 10.1002/da.22454. [DOI] [PubMed] [Google Scholar]
- 8.Troyer EA, et al. Searching for host immune-microbiome mechanisms in obsessive-compulsive disorder: A narrative literature review and future directions. Neurosci. Biobehav. Rev. 2021;125:517–534. doi: 10.1016/j.neubiorev.2021.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turna J, et al. The gut microbiome and inflammation in Obsessive-Compulsive Disorder patients compared to age- and sex-matched controls: a pilot study. Acta Psychiatr. Scand. 2020 doi: 10.1111/acps.13175. [DOI] [PubMed] [Google Scholar]
- 10.Scheepers IM, et al. Natural compulsive-like behaviour in the deer mouse (Peromyscus maniculatus bairdii) is associated with altered gut microbiota composition. Eur. J. Neurosci. 2019 doi: 10.1111/ejn.14610. [DOI] [PubMed] [Google Scholar]
- 11.Bastiaanssen TFS, Cowan CSM, Claesson MJ, Dinan TG, Cryan JF. Making sense of … the microbiome in psychiatry. Int. J. Neuropsychopharmacol. 2019;22:37–52. doi: 10.1093/ijnp/pyy067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snider LA, Swedo SE. PANDAS: Current status and directions for research. Mol. Psychiatry. 2004;9:900–907. doi: 10.1038/sj.mp.4001542. [DOI] [PubMed] [Google Scholar]
- 13.Baj J, Sitarz E, Forma A, Wroblewska K, Karakula-Juchnowicz H. Alterations in the nervous system and gut microbiota after beta-hemolytic Streptococcus Group A infection-characteristics and diagnostic criteria of PANDAS recognition. Int. J. Mol. Sci. 2020;21:1476. doi: 10.3390/ijms21041476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K. Gut microbes and the brain: Paradigm shift in neuroscience. J. Neurosci. 2014;34:15490–15496. doi: 10.1523/JNEUROSCI.3299-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cryan JF, Dinan TG. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012;13:701. doi: 10.1038/nrn3346. [DOI] [PubMed] [Google Scholar]
- 16.Bailey MT, et al. Exposure to a social stressor alters the structure of the intestinal microbiota: Implications for stressor-induced immunomodulation. Brain Behav. Immun. 2011;25:397–407. doi: 10.1016/j.bbi.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Partrick KA, et al. Acute and repeated exposure to social stress reduces gut microbiota diversity in Syrian hamsters. Behav. Brain Res. 2018;345:39–48. doi: 10.1016/j.bbr.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valles-Colomer M, et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat. Microbiol. 2019 doi: 10.1038/s41564-018-0337-x. [DOI] [PubMed] [Google Scholar]
- 19.Tomova A, et al. Gastrointestinal microbiota in children with autism in Slovakia. Physiol. Behav. 2015;138:179–187. doi: 10.1016/j.physbeh.2014.10.033. [DOI] [PubMed] [Google Scholar]
- 20.Liu F, et al. Altered composition and function of intestinal microbiota in autism spectrum disorders: A systematic review. Transl. Psychiatry. 2019;9:43. doi: 10.1038/s41398-019-0389-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vuong HE, Hsiao EY. Emerging roles for the gut microbiome in autism spectrum disorder. Biol. Psychiatry. 2017;81:411–423. doi: 10.1016/j.biopsych.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwarz E, et al. Analysis of microbiota in first episode psychosis identifies preliminary associations with symptom severity and treatment response. Schizophr. Res. 2018;192:398–403. doi: 10.1016/j.schres.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 23.Nikolova VL, et al. Perturbations in gut microbiota composition in psychiatric disorders: A review and meta-analysis. JAMA Psychiat. 2021 doi: 10.1001/jamapsychiatry.2021.2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quagliariello A, et al. Gut microbiota profiling and gut-brain crosstalk in children affected by pediatric acute-onset neuropsychiatric syndrome and pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. Front. Microbiol. 2018;9:675. doi: 10.3389/fmicb.2018.00675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiao Y, et al. Alterations of oral microbiota distinguish children with autism spectrum disorders from healthy controls. Sci. Rep. 2018;8:1597. doi: 10.1038/s41598-018-19982-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hicks SD, et al. Oral microbiome activity in children with autism spectrum disorder. Autism Res. 2018;11:1286–1299. doi: 10.1002/aur.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castro-Nallar E, et al. Composition, taxonomy and functional diversity of the oropharynx microbiome in individuals with schizophrenia and controls. PeerJ. 2015;3:e1140. doi: 10.7717/peerj.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Association, A. P. DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Press; 1994. [Google Scholar]
- 29.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-CV) American Psychiatric Press; 1996. [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, Williams JBW. In New York: Biometrics Research. New York State Psychiatric Institute; 2002. [Google Scholar]
- 31.Goodman WK, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch. Gen. Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 32.Klindworth A, et al. Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res. 2013;41:e1. doi: 10.1093/nar/gks808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Callahan BJ, et al. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods. 2016;13:581–583. doi: 10.1038/nmeth.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yilmaz P, et al. The SILVA and "All-species Living Tree Project (LTP)" taxonomic frameworks. Nucleic Acids Res. 2014;42:D643–648. doi: 10.1093/nar/gkt1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Segata N, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prehn-Kristensen A, et al. Reduced microbiome alpha diversity in young patients with ADHD. PLoS ONE. 2018;13:e0200728. doi: 10.1371/journal.pone.0200728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kang DW, et al. Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PLoS ONE. 2013;8:e68322. doi: 10.1371/journal.pone.0068322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang DW, et al. Differences in fecal microbial metabolites and microbiota of children with autism spectrum disorders. Anaerobe. 2018;49:121–131. doi: 10.1016/j.anaerobe.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 39.Liu S, et al. Altered gut microbiota and short chain fatty acids in Chinese children with autism spectrum disorder. Sci. Rep. 2019;9:287. doi: 10.1038/s41598-018-36430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aarts E, et al. Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS ONE. 2017;12:e0183509. doi: 10.1371/journal.pone.0183509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jiang H, et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav. Immun. 2015;48:186–194. doi: 10.1016/j.bbi.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 42.Bassett SA, et al. Changes in composition of caecal microbiota associated with increased colon inflammation in interleukin-10 gene-deficient mice inoculated with Enterococcus species. Nutrients. 2015;7:1798–1816. doi: 10.3390/nu7031798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saulnier DM, et al. Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome. Gastroenterology. 2011;141:1782–1791. doi: 10.1053/j.gastro.2011.06.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Attwells S, et al. Inflammation in the neurocircuitry of obsessive-compulsive disorder. JAMA Psychiat. 2017;74:833–840. doi: 10.1001/jamapsychiatry.2017.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vulink NC, Denys D, Fluitman SB, Meinardi JC, Westenberg HG. Quetiapine augments the effect of citalopram in non-refractory obsessive-compulsive disorder: a randomized, double-blind, placebo-controlled study of 76 patients. J. Clin. Psychiatry. 2009;70:1001–1008. doi: 10.4088/JCP.08m04269. [DOI] [PubMed] [Google Scholar]
- 46.Figee M, et al. Deep brain stimulation induces striatal dopamine release in obsessive-compulsive disorder. Biol. Psychiatry. 2014;75:647–652. doi: 10.1016/j.biopsych.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 47.Clarke R, et al. Folate, vitamin B12, and serum total homocysteine levels in confirmed Alzheimer disease. Arch. Neurol. 1998;55:1449–1455. doi: 10.1001/archneur.55.11.1449. [DOI] [PubMed] [Google Scholar]
- 48.Mihaila D, et al. The oral microbiome of early stage Parkinson's disease and its relationship with functional measures of motor and non-motor function. PLoS ONE. 2019;14:e0218252. doi: 10.1371/journal.pone.0218252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsuda A, et al. Influence of proton-pump inhibitors on the luminal microbiota in the gastrointestinal tract. Clin. Transl. Gastroenterol. 2015;6:e89. doi: 10.1038/ctg.2015.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Orefici, G., Cardona, F., Cox, C. J. & Cunningham, M. W. in Streptococcus pyogenes: Basic Biology to Clinical Manifestations. (eds Ferretti J. J., Stevens D. L. & Fischetti V. A.). (University of Oklahoma Health Sciences Center, 2016). [PubMed]
- 51.Weersma RK, Zhernakova A, Fu J. Interaction between drugs and the gut microbiome. Gut. 2020;69:1510–1519. doi: 10.1136/gutjnl-2019-320204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.David LA, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.