To the Editor:
Vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic (VEXAS) syndrome was recently identified by genotype-driven approach [1]. This syndrome is characterised by the presence of somatic mutations affecting methionine-41 (p.Met41) in UBA1 gene. All the identified patients were adult males who had recurrent fevers, cytopenias, dysplastic bone marrow with vacuoles in myeloid and erythroid precursors, neutrophilic skin and lung tissue inflammation and often had treatment refractory and fatal disease course. The various phenotypes reported with VEXAS syndrome include relapsing polychondritis, giant cell arteritis, polyarteritis nodosa, Sweet’s syndrome, myelodysplastic syndrome and multiple myeloma.
We describe a case of VEXAS syndrome with systemic lupus erythematosus (SLE) phenotype, which has not been reported previously. A 70-years-old male presented in February 2020 with complaints of recurrent fevers, polyarthralgia, erythematous skin rash over the trunk, left leg venous thrombosis and weight loss for eight months duration. Investigations revealed macrocytic anaemia, leukopenia, neutropenia, raised erythrocyte sedimentation rate (99mm/hr) and C-reactive protein (33mg/L). He tested positive for anti-nuclear antibodies (ANA, 1:80 titres, fine speckled), anti-Scl-70 antibodies and low C3 (73 mg/dl) with normal C4 (23 mg/dl). Anti-ds-DNA, anti-Ro, anti-La, anti-phospholipid antibodies were negative. Bone marrow examination showed hypercellular marrow with borderline megakaryocytic dysplasia. He was diagnosed with late onset SLE with cytopenias and polyarthralgia and was started on oral glucocorticoids (GC, 0.5mg/kg/day) following which fever subsided and cytopenias and arthralgias improved. While on 5mg/day of prednisolone, he developed fever in August 2020 and had lung nodules. Fine needle aspiration from the nodules showed cryptococcal organisms. He was started on amphotericin B and fluconazole for pulmonary cryptococcosis, following which fever subsided. However, in hospital, he developed recurrence of fever and dry cough and he tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) by polymerase chain reaction (PCR) from naso-pharyngeal swab. He was managed with GC and heparin as per coronavirus disease 2019 (COVID-19) protocols and was discharged from hospital after 20 days. In October 2020, he again developed fever, breathlessness and altered mental status. He was found to have klebsiella pneumoniae associated urinary tract infection and was managed with intravenous antibiotics. He had respiratory failure for which he was put on mechanical ventilation and he again tested positive for SARS-CoV2 by PCR and was managed with intravenous dexamethasone and subsequently patient improved and was discharged from hospital.
Keeping in view the clinical picture of elderly male with recurrent fevers, neutropenia, skin lesions and treatment refractoriness, a possibility of VEXAS syndrome was considered. Previously performed bone marrow slides were reviewed which showed megakaryocytic dysplasia, toxic granules and vacuoles in myeloid precursors. The presence of VEXAS syndrome was confirmed by the detection of c.121 A>G, p.Met41Val mutation in the UBA1 gene. He was initiated on monthly intravenous immunoglobulin (IVIG, 1gm/kg/month) in December 2020. At his last visit, in March 2021, his haemoglobin increased and was not requiring any blood transfusion. Fever and leukopenia also resolved. Figure 1 shows the details of clinical course and treatment response. We report the first case of VEXAS syndrome in association with SLE, thus expanding the list of autoimmune diseases associated with VEXAS syndrome. While this patients meets both 2019 ACR/EULAR and SLICC classification criteria for SLE, whether this patient has true SLE or SLE like phenotype might become clearer on follow up.
Figure 1.
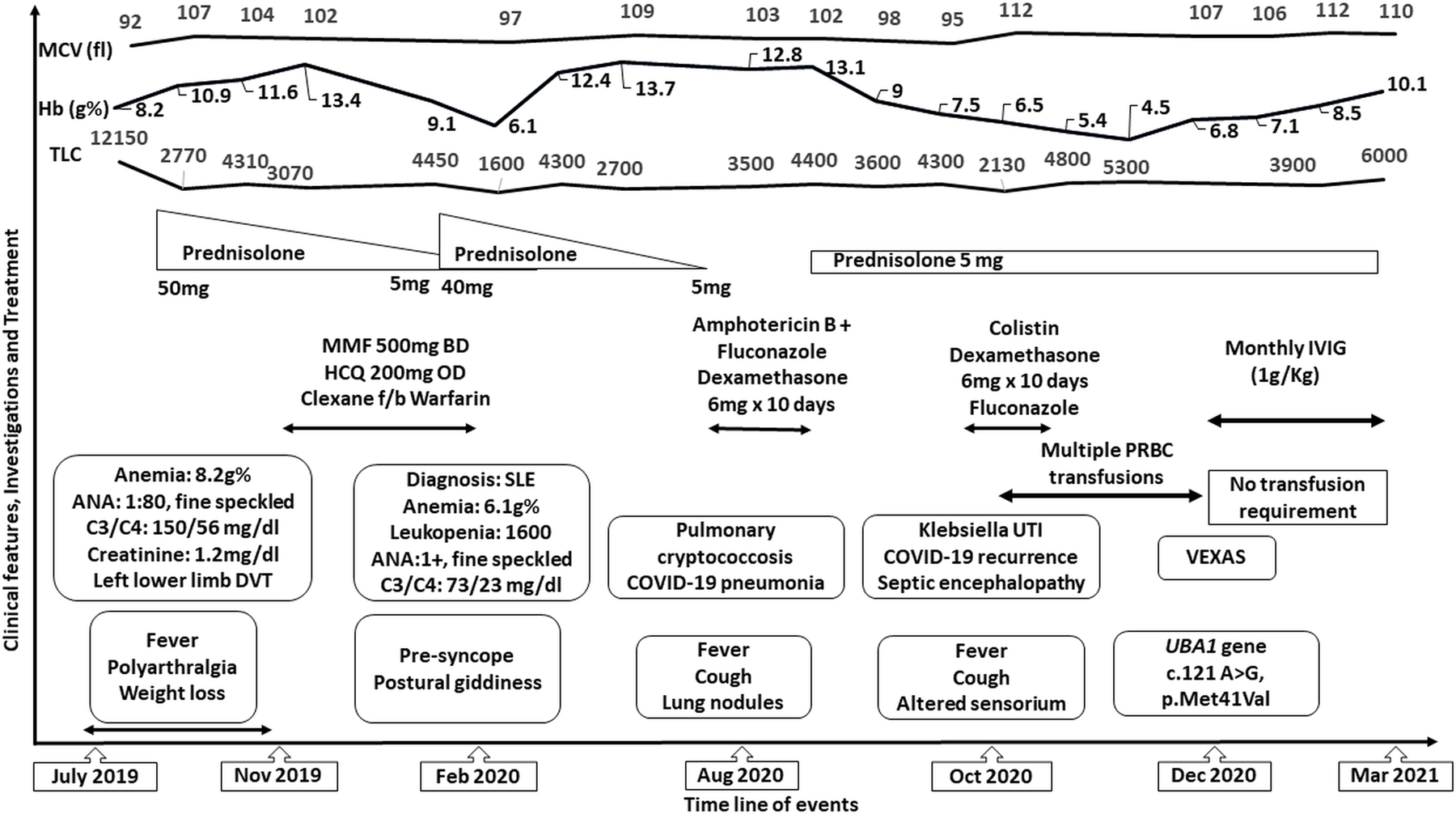
showing the clinical course and response to therapy. MCV- Mean corpuscular volume, Hb- haemoglobin, TLC- total leucocyte count, ANA- anti nuclear antibodies, DVT- deep venous thrombosis, SLE- systemic lupus erythematosus, MMF-Mycophenolate mofetil, HCQ- hydroxychloroquine, IVIG-intravenous immunoglobulin, UTI- urinary tract infection, VEXAS- Vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic Vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic (VEXAS) syndrome syndrome
Acknowledgments
Funding: None
Footnotes
Conflict of Interest: None
Disclosures: None
Consent for publication: Written informed consent was obtained from the patient for publication of this article and related clinical images
References:
- 1.Beck DB, Ferrada MA, Sikora KA, Ombrello AK, Collins JC, Pei W, et al. Somatic mutations in UBA1 and severe adut-onset autoinflammatory disease. N Engl J Med 2020; 383: 2628–38. [DOI] [PMC free article] [PubMed] [Google Scholar]


