Abstract
Background
Ethical conflict is a problem with negative consequences, which can compromise the quality and ethical standards of the nursing profession and it is a source of stress for health care practitioners’, especially for nurses.
Objectives
The main aim of this study was to analyze Spanish critical care nurses’ level of exposure to ethical conflict and its association with sociodemographic, occupational, and COVID-19–related variables. Research Design, Participants, and Research context: This was a quantitative cross-sectional descriptive study conducted among 117 nurses working in critical care units. Data collection tools were sociodemographic, occupational, and COVID-19–related questionnaires and previously validated Spanish version of Ethical Conflict in Nursing Questionnaire-Critical Care Version.
Ethical Considerations
We obtained permission from the Ethics Committee and participants' informed consent.
Findings
Data indicates a moderate level of exposure to ethical conflicts. The most frequent ethical conflicts were related to situations about "treatment and clinical procedures." The most intensity of ethical conflicts was related to situations about "treatment and clinical procedures" and "dynamics of the service and working environment." No statistical significance was identified between the socio-demographic variables and level of exposure to ethical conflicts. However, for critical care nurses working in ICU, nurses with perceived worked stress had a higher level of exposure to ethical conflicts. Likewise, critical care nurses whose family/friends were infected with COVID-19 had a higher level of exposure.
Conclusions
Critical care nurses experience a moderate level of exposure to ethical conflicts which is consistent with the results of previous studies. A deeper understanding of ethical conflicts in conflictive situations allows recognition of the situations that occur in everyday clinical practice, identification of the ethical conflicts, and facilitation of the nurses working in the challenging clinical situation.
Keywords: Ethics, conflict, critical care unit, nurse, COVID-19
Introduction
COVID-19 is the highly pathogenic human coronavirus disease to date and the rapid spreading of this contagious disease has posed the severest threat to global health in this century.1 Due to the severity of the disease and high morbidity and mortality rates, there might be necessary to ensure the hospitalization for patients who presents severe symptoms of the disease. Globally, for symptomatic patients with COVID-19 severe forms, Intensive Care Unit (ICU) admission must be considered as it has been described as necessary in almost 25% of hospitalized patients.2,3
The current pandemics is affecting health care systems all around the world in so many different aspects, which include limited resources, shortages of personal protective equipment, and lack of ICU beds number. There is a clear scarcity of resources capacity of health care systems and this lack of available responses to patient’s needs, could also generate ethical conflicts in nursing ICU clinical practice.
Background
In recent years, ethical issues appeared as a key component of healthcare for critically ill patients, who are vulnerable and reliant entirely on nurses employed in the critical care unit.4 Evidence shows that conflicts in the nursing sector continue to develop, due to both the increasing nature of treatment and the scientific and technical advances made in recent decades. Critical care units are, in this regard, a setting that is particularly prone to conflict.5
Concerning technical and medical advancements, the complexity of care situations and the lack of evidence-based approaches require nurses to focus continuously and objectively on how they can contribute to the well-being of their patients, which in turn demands high-level professional skills and ethical maturity. In everyday ethical dilemmas, ethical behavior appears to be most troublesome, resulting from circumstances involving contradictory principles or attitudes on what is the right or correct course of action.6
Ethical conflict
To better understand the content of this research, it is important to clarify the main concept on its basis. In a systematic analysis about ethical conflicts, a “moral (ethical) conflict” was defined as “a situation involving a clash of moral values within the practitioner, among practitioners, and/or between practitioners and patients, concerning what was the morally right action to take, or as a situation in which the duties and obligations of health professionals were unclear” (p. 362).7
Ethical conflict is a problem with negative consequences, which can compromise the quality and ethical standards of the nursing profession.8 In the literature we can find five ethical guiding principles: beneficence, non-maleficence, respect for autonomy, equity, and efficiency.9 According to those principles an ethical issue or an ethical conflict arises when at least one of those principles is not adequately considered or two or more of these principles are in conflict.10
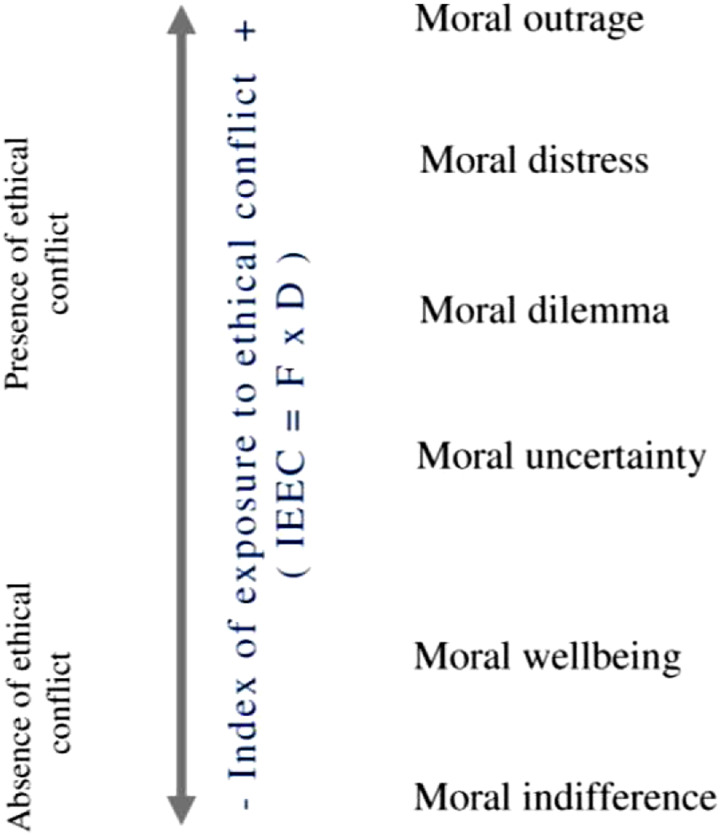
In the field of ethical conflict, the four forms or categories of ethical conflict identified are: moral uncertainty, moral dilemma, moral distress, and moral outrage.8 Nurses are also supposed to be mindful of the ethical aspects of nursing practice as the literature uses a variety of different terms to explain circumstances that are ethically questionable in one way or another. Some of these terms include ethical challenges, ethical dilemmas, ethical problems, ethical concerns, and ethical questions. Though these situations are described differently, their origin tends to include an individual facing circumstances in which beliefs, norms, or principles are either threatened or in dispute, and a decision about how to respond must be made.11 Over recent years, there has been a growing interest in exploring the ethical controversy of health professionals.
Ethical conflict is an obstacle to decision-making and is a concern arising from ethical obligations that nurses carefully take on.8 In fact, ethical conflict could also be seen as an opportunity to strengthen or otherwise improve/justify decision-making.
Nursing ethical conflicts
Conflict is often experienced by nurses when it comes to making decisions about health care and along with this sometimes, they are expected to carry out actions that they feel are morally wrong. Critical nurses experience complex situations involving multiple moral conflicts due to the nature of acutely ill patients.12 Ethical decision-making is considered a key requirement for professional excellence. It is defined as the ability to make decisions and is inter-related with the ethical competence and autonomy of the nurse.13 Besides, the concept of ethical conflict is a complex construct that includes not only the inability to carry out an ethical action due to the presence of obstacles (moral distress), but also other problems such as the lack of understanding of values and ethics (moral uncertainty), the difficulty in choosing two moral values (moral dilemma), and the feeling of failure to cope with the immoral act of others (moral outrage).14 Moral wellbeing relates to a positive condition in which moral thought and practice converge. Moral indifference defines the role of a person who does not show interest in or stand on an ethical issue.5
Ethical conflict exposure on nurses
Within the healthcare team, nurses also play a crucial role, keeping communication lines open and organizing all the clinical resources needed for patient care. The aim of nursing care is always to promote health and help the individual to cope with illness. Nurses are individuals with personal and professional values; they carry out their skills in institutions in conjunction with other professionals, all of whom have different values. In addition to this, they provide nursing care to patients who often have different religious, cultural, and moral values from their own.7 The dynamic complexity of the work climate, including lack of complete participation of nurses in the decision-making process, different conceptions about certain actions or procedures between doctors and nurses, or lack of time to provide high-quality critical care, and challenges in resolving bioethical problems often play a significant role in the prevalence of ethical conflict and can put nurses under ethical challenges.15,16
Intensive care unit nurses and ethical conflicts
Previous studies have focused on the analysis of ethical conflicts in nurses working in critical care units, as they are particularly exposed to the phenomenon and three main sources of conflict have been reported in these studies. First, there are decisions involving informed consent, confidentiality, and the protection of patient interests and wishes. Second, there is a conflict between the administration of certain treatments and the implementation of certain clinical procedures, with special attention to therapeutic futility and the limitations of life-sustaining treatment. Conflict situations were identified about nurses' perception of working in an atmosphere that looks like asking questions of a bioethical nature and their lack of participation in clinical decision-making.8 A qualitative study among 15 nurses was conducted in Portugal with the aims of recognizing the ethical issues perceived by intensive care nurses in their everyday practice and to understand why these situations were considered an ethical issue and what interventions/strategies have been or are expected to be developed to minimize them. The results of this study identified that end-of-life decisions, privacy, interaction, teamwork, and health-care access as rising ethical issues. However, the reasons behind this emerging issue are personal, team, and institutional aspects. In addition to this personal and team, resources are used for resolving these issues.17
Moral distress affects nursing procedures and, in some cases, patient outcomes and leads to several issues including impairment in physical and psychological well-being.18,19 A cross-sectional study was conducted in Italy among 406 nurses working in neonatal intensive care units (NICUs). The findings of this study reveal that nurses experience low-to-moderate levels of moral distress. However, the situations that obtain the highest scores for frequency, intensity, and level of moral distress related to the implementation of significant life-saving actions and involvement in the treatment of a child dependent on the ventilator.19
A descriptive cross-sectional study was conducted in Iran to determine the frequency, degree, level of exposure, and type of ethical conflict among 382 nurses working in the intensive care units. The results of this study suggest that the most frequent conflict reported was related to “using resources despite believing in its futility,” with the frequency of at least once a week or a month (68.6%). In addition to this, the most conflictive situation was a violation of privacy (76.9%). It also shows that the level of exposure to ethical conflict according to the theoretical model followed was the situation of “working with incompetent staff” and the most frequently observed type of conflict was moral dilemma.15
Moral outrage is unusually common among nurses who work in intensive care settings. Moral outrage arises when subsequent efforts by the nurse to operationalize a decision are disrupted by constraints. The outrage exacerbates when these restrictions not only obstruct actions but also compel a course of action that contradicts the moral values of the nurse.20 One study was conducted among 184 critical care nurses to obtain a transcultural Portuguese-language adaptation and validation of the Ethical Conflict Nursing Questionnaire–Critical Care Version (ECNQ-CCV) and to examine the level of exposure and characteristics of the Portuguese critical care nurses to ethical conflict. The results suggest that the frequency of occurrence of ethically conflictive situations, the following cases occurred at least once a month or week without addressing the degree of ethical conflict that might exist in professionals: Scenario: 2 “Having to administer treatments and/or carry out procedures without the critical patient, who is conscious, knowing their purpose and the risks involved,” with 62.5% and Scenario 3: “Caring for a patient who I believe should be on an ordinary hospital ward rather than in a critical care unit,” with 62%. The results also identify that moral outrage is the most encountered form of ethical conflict and moderate rates of conflict were exhibited.21 A major descriptive and correlational study was carried out in Spain among 203 nurses which identify that the index of exposure to ethical conflict (IEEC) was considered moderate. Situations involving analgesic medication (49.7%) and end-of-life care (48.7%) are a recurrent source of conflict. Moreover, forms of ethical conflict and moral systems typically ranged from a lower to a higher degree of exposure index to ethical conflict. The most frequently experienced ethical conflict by nursing professionals was moral outrage.8
There is also evidence that socio-demographic influences among patients admitted to critical care units have a significant impact on the role among patients in ethical decision-making. To address this issue an exploratory study was carried out in Kenya to determine the ethical dilemmas among 123 nurses working in Critical Care Units of the Kenyatta National Hospital in their daily practice and the socio-demographic factors influencing the experience. End-of-life decisions, patient care issues and human rights issues were identified as the emerging ethical issues. Level of knowledge of ethical issues, age and gender, were associated to influencing the way one perceives ethical dilemmas.4 Another major prospective and descriptive correlation study conducted in Barcelona, Spain, analyzed the level of exposure of nurses to ethical conflict and determine the relationship between this exposure, sociodemographic variables, and perceptions of the clinical environment. The exposure to the ethical conflict was moderate and the most often recorded ethical problems were a recognition that analgesia is ineffective and care administration with-out having engaged in the decision-making process. In addition to this, professionals who viewed their atmosphere as supporting in coping with ethical issues reported lower rates of these incidents.14
Experts accept that there are some circumstances related to patients and families, care, team interactions, and institutional features as well as ethical conflict outlets. The ethical issue of maintaining the safety of important patients and securing their rights and interests emerges from an informed consent policy about patients and their families. In respect to therapies, decisions on whether to administer them or not are related to restrictions on life-care and medical futility. Nonetheless, some data bring to our attention that it is a very conflictive and common situation in ICUs to test if analgesic medication is inadequate to control pain from the patient. In addition to this, it has been shown that certain contrasting circumstances emerge from professional-team-dynamics partnerships, from resource management or burnout.21
Until now, most of the research has been based on conditions that cause moral distress or moral dilemma in ICUs, due to the specific limitations of critical patients and the unique therapeutic option of ICUs. As the literature suggests, very few studies have been conducted among Spanish critical care nurses that examine the types of ethical conflict, and scarce studies speculating the positive perspective or the absence of ethical conflict as a moral state were conducted. This implicates that it is very essential to analyze how critical care nurses feel when they face a conflictive situation which eventually helps in clear recognition of the barrier that restricts the taking of action in ethical issues. The engagement of nurses in the decision-making process in critical care problems is a protective factor against the emergence of ethical issues within ICUs. Evaluating the level of ethical conflict makes it possible to gain a better insight into problematic situations in critical care units. The main research question was “What are the levels of exposure and characteristics of ethical conflict among Spanish critical care nurses?”
The objectives of this study were first, to examine Spanish critical care nurses’ level of exposure to ethical conflict during COVID-19 pandemics and its characteristics, to identify the most frequent type of conflict, and to analyze the association between sociodemographic, occupational data and COVID-19 situation, and self-experience with the level of exposure to ethical conflicts.
Methods
Design
A quantitative cross-sectional descriptive design was employed.
Time and setting
Data collection was conducted by researchers between July and October 2020. In this period, Spain was experiencing a hard period, which still corresponded to the first wave. Data were collected from a regional Central University Hospital, which is a hospital considered as a regional health reference in north of Spain and is dedicated to researching, teaching, caring, and providing health services for people. For this study, the specific setting was the critical care department formed by general ICU, Cardiac ICU, Pediatric ICU, and Neonatal ICU. Most of the nurses works in 8 h shift in a rotatory regimen.
Participants
The sample consists of 117 out of 165 nurses working in the critical care units, that is, ICU, Cardiac ICU, Pediatric ICU and Neonatal ICU of the public and university hospital in the north of Spain. Convenience sampling was done and only 144 were eligible. Therefore, research was conducted among 81.25% eligible nurses. The inclusion criteria were as follows: nurses working in critical care units and willingness to participate in the study. The exclusion criteria were nurses working in general wards.
Data Collection
Two self-administered instruments were used for data collection. The first instrument contained the sociodemographic, occupational, and COVID-19–related questionnaire, consists of items on nurses’ age, gender, marital status, level of education, working unit, type of contract, work shift, total professional years of experience, total years of professional experience in critical care units, COVID-19 infection(yes/no), having family or friends infected with COVID-19(yes/no), afraid of pandemic(yes/no), perceived ethical conflicts in pandemic (yes/no).
The second instrument used in this study was a Spanish validated version of Ethical Conflict in Nursing Questionnaire-Critical Care Version (ECNQ-CCV) developed by Falcó-Pegueroles et al.,5 which evaluates frequency, severity types, and level of exposure to ethical conflicts. The questionnaire contains 19 scenarios that are potentially conflictive from an ethical perspective (Supplementary table) which are categorized into three areas: interpersonal relationships with the patient and family (P&F); treatments and clinical procedures (T&CP) and finally, the dynamics of the service and the work environment (DS&WE). For each scenario, three questions are presented in terms of the frequency of ethical conflict the degree of perceived ethical conflict, and the type of the experienced ethical conflict.
By multiplying the frequency and intensity of ethical conflict variables, the variable ‘‘index of exposure to ethical conflicts’’ (IEEC) was generated which showed the level of exposure to ethical conflict. Therefore, the score range of the conflict level for each scenario would be from 0 to 25. A score of zero represents the frequency of zero (never) multiplied by the intensity 1 (not problematic) and a score of 25 shows the frequency of 5 (at least once a week) multiplied by the intensity 5 (very problematic). The total scores for the conflict level ranged from 0–475, higher scores represent a greater level of conflict. The ECNQ-CCV identifies four types of ethical conflicts including moral uncertainty, moral dilemma, moral distress, and moral outrage, while the type of conflict is stated as a percentage. Moral indifference and moral well-being indicate a lack of ethical conflict (see Figure 1).5 The value of Cronbach’s alpha coefficient for this tool is 0.882. (5 Low, moderate, and high exposure to ethical conflict were defined as <1 standard deviations (SD) below the mean, ±1 SD around the mean, and >1 SD above the mean, respectively.22
Figure 1.
Model for the analysis of ethical conflict (by Falcó-Pegueroles, Lluch-Canut, & Guàrdia-Olmos, 2013).
Procedure
After the Ethical Committee approval and the authorization of the Hospital Board, supervisors were informed about the aim of the study and their collaboration was asked. The questionaries were distributed on an envelope by the supervisor of each critical care unit to the nurses. After the completion of the instruments, participants leave it anonymously on a closed box and were later collected by the principal investigator.
Ethical considerations
Permission to carry out the research was obtained from the Ethical Committee for Clinical Research of the Principality of Asturias (CeimPA 2020.290). All the participants were informed about the objectives of the study and the voluntary nature of their participation. The questionnaires did not include names or other ways of personal identification of the participants to keep the protection of privacy and maintenance of confidentiality. Informed consent was obtained from each participant. Participants were not working under supervision of researchers. Regarding to that fact there is no conflict to declare.
Data analysis
The data were analyzed using the statistical software program SPSS version 21.0. Each survey was examined for completeness before entering the responses in the data set. Descriptive statistics were used to calculate the percentages and the total number of the nominal variables and means, standard deviations, and rank of the ordinal variables. Different tests were used: Kolmogorov-Smirnov test for the normality and T-test, ANOVA, and Chi-Square for comparing and examining the relationship of the independent variables. The value for accepting the statistical significance p< 0.05.
Results
The study included 144 nurses and out of the total returned questionnaires, 27 were excluded due to incompletion. Thus, 117 questionnaires were analyzed (response rate 81.25%). Most of the nurses 82.1% were female and 17.9% were male. The mean age of nurses was 37.62 years (SD 9.827). Age ranged from 24 to 64 years. Almost half of the nurses 50.40% were married or in living in a relationship and 52.1% had a master’s degree.
Most of the nurses 75.2% were working on rotational shifts (morning, afternoon, night). The mean of total professional years of work experience was 13.92 years, SD 9.727, range (1–43). Similarly, the mean of total professional years of work experience in critical care units was 9.92 years, SD 8.576, range (1–40). More than half 62.4% of the nurses find their work stressful.
Concerning the COVID-19 infection, only the minority of the sample nurses 4.3% had been infected with COVID-19, and less than half of the sample nurses 39.3% reported that their family and friends had been infected with COVID-19. Majority of the sample nurses 71% were afraid since the pandemic started. More than half 55.6% of the sample nurses perceived ethical conflicts in pandemic assessed by a “yes or no” dichotomic question.
Frequency and degree of ethical conflicts
Regarding the frequency of occurrence of ethical conflicts, the situation which occurred at least once a week was Scenario 17: “Administering treatments and/or carrying out procedures without, as a nurse, having been previously involved in the decision to do so” (n=36.30.8%). The situation which occurred at least once a month were Scenario 1: “Administering treatments and/or performing tests that I consider unnecessary because they serve merely to prolong a terminal, irreversible process” and Scenario 7 “Realizing that the analgesia and/or sedation being given to the patient is not effective enough and that the patient is suffering” (n=36, 30.8%). On the other hand, the situations that almost never occurred were Scenario 6: “Administering treatments and/or carrying out interventions without the patient’s family knowing the objectives, benefits, and risks involved (when the patient has consented to the family being informed)" (n=36.30.8%) and Scenario 18: “Failure to respect properly the privacy of the patient’s body when carrying out procedures and/or exploratory tests” (n=31.26.5%) (Table 1).
Table 1.
Frequencies with which ethically conflictive situations emerged.
| Scenario | Area | Never | Almost never | At least once a year | At least once every 6 months | At least once a month | At least once a week | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| S1 | T&CP | 13 | 11.1 | 7 | 6.0 | 18 | 15.4 | 29 | 24.8 | 36 | 30.8 | 14 | 12.0 |
| S2 | P&F | 29 | 24.8 | 20 | 17.1 | 10 | 8.5 | 18 | 15.4 | 22 | 8.8 | 18 | 15.4 |
| S3 | DS&WE | 21 | 17.9 | 16 | 13.7 | 9 | 7.7 | 20 | 17.1 | 42 | 35.9 | 9 | 7.7 |
| S4 | P&F | 30 | 25.6 | 29 | 24.8 | 19 | 16.2 | 24 | 20.5 | 14 | 12.0 | 1 | 0.9 |
| S5 | P&F | 51 | 43.6 | 30 | 25.6 | 9 | 7.7 | 13 | 11.1 | 12 | 10.3 | 2 | 1.7 |
| S6 | P&F | 43 | 36.8 | 36 | 30.8 | 10 | 8.5 | 13 | 11.1 | 11 | 9.4 | 4 | 3.4 |
| S7 | T&CP | 14 | 12.0 | 19 | 16.2 | 12 | 10.3 | 23 | 19.7 | 36 | 30.8 | 13 | 11.1 |
| S8 | DS&WE | 13 | 11.1 | 15 | 12.8 | 12 | 10.3 | 30 | 25.6 | 33 | 28.2 | 14 | 12.0 |
| S9 | DS&WE | 31 | 26.5 | 26 | 22.2 | 14 | 12.0 | 21 | 17.9 | 16 | 13.7 | 9 | 7.7 |
| S10 | P&F | 45 | 38.5 | 28 | 23.9 | 10 | 8.5 | 20 | 17.1 | 14 | 12.0 | - | - |
| S11 | T&CP | 27 | 23.1 | 19 | 16.2 | 16 | 13.7 | 28 | 23.9 | 25 | 21.4 | 2 | 1.7 |
| S12 | DS&WE | 18 | 15.4 | 21 | 17.9 | 14 | 12.0 | 24 | 20.5 | 32 | 27.4 | 8 | 6.8 |
| S13 | DS&WE | 45 | 38.5 | 24 | 20.5 | 12 | 10.3 | 19 | 16.2 | 15 | 12.8 | 2 | 1.7 |
| S14 | T&CP | 51 | 43.6 | 24 | 20.5 | 13 | 11.1 | 21 | 17.9 | 6 | 5.1 | 2 | 1.7 |
| S15 | DS&WE | 57 | 48.7 | 24 | 20.5 | 10 | 8.5 | 11 | 9.4 | 7 | 6.0 | 8 | 6.8 |
| S16 | P&F | 44 | 37.6 | 18 | 15.4 | 6 | 5.1 | 11 | 9.4 | 17 | 14.5 | 21 | 17.9 |
| S17 | T&CP | 25 | 21.4 | 14 | 12.0 | 10 | 8.5 | 10 | 8.5 | 22 | 18.8 | 36 | 30.8 |
| S18 | P&F | 30 | 25.6 | 31 | 26.5 | 8 | 6.8 | 11 | 9.4 | 18 | 15.4 | 19 | 16.2 |
| S19 | DS&WE | 42 | 35.9 | 24 | 20.5 | 8 | 6.8 | 14 | 12.0 | 14 | 12.0 | 15 | 12.8 |
Abbreviations: S = Situations, T&CP = Treatment and Clinical Procedures, P&F: Patient and family interpersonal relationships, DS&WE: Dynamics of the Service and Working Environment, n = number of respondents, N= Total number of respondents in each situation.
As far as the degree of the ethical conflict is concerned, Scenario 12: “Working with a nurse or nursing assistant who I consider to be professionally incompetent” (n=43.43.4%) and Scenario 7: “Realizing that the analgesia and/or sedation being given to the patient is not effective enough and that the patient is suffering” (n=41.39.8%) were the very problematic situations. However, the less problematic situations were Scenario 3: “Caring for a patient who I believe should be on an ordinary hospital ward rather than in a critical care unit” (n=44.45.8%) and Scenario 2: “Having to administer treatments and/or carry out procedures without the critical patient, who is conscious, knowing their purpose and the risks involved” (n=33.37.5%) (Table 2).
Table 2.
Degree of ethical conflict.
| Scenario | Area | Not problematic | Little problematic | Somewhat problematic | Moderately problematic | Very problematic | N | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |||
| S1 | T&CP | 1 | 1 | 23 | 22.1 | 39 | 37.5 | 33 | 31.7 | 8 | 7.7 | 104 |
| S2 | P&F | 6 | 6.8 | 33 | 37.5 | 26 | 29.5 | 15 | 17.0 | 8 | 9.1 | 88 |
| S3 | DS&WE | 13 | 13.5 | 44 | 45.8 | 18 | 18.8 | 19 | 19.8 | 2 | 2.1 | 96 |
| S4 | P&F | 2 | 2.3 | 18 | 20.5 | 26 | 29.5 | 27 | 30.7 | 15 | 17.0 | 88 |
| S5 | P&F | 5 | 7.6 | 8 | 12.1 | 17 | 25.8 | 22 | 33.3 | 14 | 21.2 | 66 |
| S6 | P&F | 11 | 14.9 | 20 | 27.0 | 18 | 24.3 | 15 | 20.3 | 10 | 13.5 | 74 |
| S7 | T&CP | 5 | 4.9 | 7 | 6.8 | 17 | 16.5 | 33 | 32.0 | 41 | 39.8 | 103 |
| S8 | DS&WE | 10 | 9.6 | 17 | 16.3 | 21 | 20.2 | 44 | 42.3 | 12 | 11.5 | 104 |
| S9 | DS&WE | 1 | 1.2 | 9 | 10.5 | 20 | 23.3 | 26 | 30.2 | 30 | 34.9 | 86 |
| S10 | P&F | 1 | 1.4 | 6 | 8.3 | 12 | 16.7 | 22 | 30.6 | 31 | 43.1 | 72 |
| S11 | T&CP | 4 | 4.4 | 6 | 6.7 | 16 | 17.8 | 36 | 40.0 | 28 | 31.1 | 90 |
| S12 | DS&WE | 1 | 1.0 | 11 | 11.1 | 16 | 16.2 | 28 | 28.3 | 43 | 43.4 | 99 |
| S13 | DS&WE | 1 | 1.4 | 12 | 16.7 | 14 | 19.4 | 22 | 30.6 | 23 | 31.9 | 72 |
| S14 | T&CP | 1 | 1.5 | 15 | 22.7 | 20 | 30.3 | 14 | 21.2 | 16 | 24.2 | 66 |
| S15 | DS&WE | 4 | 6.7 | 17 | 28.3 | 12 | 20.0 | 18 | 30.0 | 9 | 15.0 | 60 |
| S16 | P&F | 5 | 6.8 | 14 | 19.2 | 15 | 20.5 | 19 | 26.0 | 20 | 27.4 | 73 |
| S17 | T&CP | 11 | 12.0 | 23 | 25.0 | 27 | 29.3 | 21 | 22.8 | 10 | 10.9 | 92 |
| S18 | P&F | 3 | 3.4 | 17 | 19.5 | 23 | 26.4 | 21 | 24.1 | 23 | 26.4 | 87 |
| S19 | DS&WE | 5 | 6.7 | 15 | 20.0 | 18 | 24.0 | 21 | 28.0 | 16 | 21.3 | 75 |
Abbreviations: S = Situations, T&CP = Treatment and Clinical Procedures, P&F: Patient and family interpersonal relationships, DS&WE: Dynamics of the Service and Working Environment, n=number of respondents, N=total number of respondents in each situation.
Types of conflict and moral states
Moral outrage was the type of ethical conflict most frequently selected by sample nurses in 10 of 19 scenarios. Following this were moral dilemma and moral uncertainty, selected in three situations each. Moral distress and moral indifference were the types of ethical conflict least selected by nurses (Table 3).
Table 3.
Index of exposure to ethical conflicts and types of ethical conflicts.
| Scenario | IEEC | Moral indifference | Moral well-being | Moral uncertainty | Moral dilemma | Moral distress | Moral outrage | N | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ±SD | n | % | n | % | n | % | n | % | n | % | n | % | ||
| S1 | 9.75 ± 6.094 | 3 | 2.9 | 5 | 4.8 | 17 | 16.3 | 25 | 24.0 | 23 | 22.1 | 31 | 29.8 | 104 |
| S2 | 6.569 ± 5.826 | 8 | 9.1 | 18 | 20.5 | 26 | 29.5 | 14 | 15.9 | 5 | 5.7 | 17 | 19.3 | 88 |
| S3 | 6.71 ± 5.438 | 29 | 30.2 | 17 | 17.7 | 16 | 16.7 | 16 | 16.7 | 4 | 4.2 | 14 | 14.6 | 96 |
| S4 | 5.99 ± 5.705 | 3 | 3.4 | 9 | 10.2 | 9 | 10.2 | 27 | 30.7 | 19 | 21.6 | 21 | 23.9 | 88 |
| S5 | 4.42 ± 5.677 | 4 | 6.1 | 10 | 15.2 | 9 | 13.6 | 17 | 25.8 | 10 | 15.2 | 16 | 24.2 | 66 |
| S6 | 3.99 ± 5.107 | 18 | 24.3 | 9 | 12.2 | 10 | 13.5 | 12 | 16.2 | 16 | 21.6 | 9 | 12.2 | 74 |
| S7 | 11.38 ± 7.811 | 2 | 1.9 | 11 | 10.7 | 6 | 5.8 | 13 | 12.6 | 28 | 27.2 | 43 | 41.7 | 103 |
| S8 | 9.59 ± 6.623 | 6 | 5.8 | 16 | 15.4 | 13 | 12.5 | 21 | 20.2 | 24 | 23.1 | 24 | 23.1 | 104 |
| S9 | 7.94 ± 7.661 | 6 | 7.0 | 3 | 3.5 | 11 | 12.8 | 10 | 11.6 | 18 | 20.9 | 38 | 44.2 | 86 |
| S10 | 5.90 ± 6.613 | 1 | 1.4 | 7 | 9.7 | 6 | 8.3 | 13 | 18.1 | 19 | 26.4 | 26 | 36.1 | 76 |
| S11 | 8.32 ± 6.728 | 3 | 3.3 | 5 | 5.6 | 9 | 10.0 | 14 | 15.6 | 28 | 31.1 | 31 | 34.4 | 90 |
| S12 | 10.50 ± 7.833 | 5 | 5.1 | 9 | 9.1 | 8 | 8.1 | 10 | 10.1 | 28 | 28.3 | 39 | 39.4 | 99 |
| S13 | 5.85 ± 6.636 | 3 | 4.2 | 7 | 9.7 | 11 | 15.3 | 13 | 18.1 | 25 | 34.7 | 13 | 18.1 | 72 |
| S14 | 4.66 ± 5.996 | 12 | 18.2 | 4 | 6.1 | 13 | 19.7 | 11 | 16.7 | 8 | 12.1 | 18 | 27.3 | 66 |
| S15 | 4.34 ± 6.315 | 10 | 16.7 | 6 | 10.0 | 7 | 11.7 | 16 | 26.7 | 12 | 20.0 | 9 | 15.0 | 60 |
| S16 | 7.19 ± 8.148 | 5 | 6.8 | 10 | 13.7 | 17 | 23.3 | 13 | 17.8 | 15 | 20.5 | 13 | 17.8 | 73 |
| S17 | 8.83 ± 8.832 | 18 | 19.6 | 12 | 13.0 | 20 | 21.7 | 15 | 16.3 | 15 | 16.3 | 12 | 13.0 | 92 |
| S18 | 7.85 ± 7.915 | 5 | 5.7 | 14 | 16.1 | 18 | 20.7 | 14 | 16.1 | 17 | 19.5 | 19 | 21.8 | 87 |
| S19 | 6.74 ± 7.938 | 4 | 5.3 | 9 | 12.0 | 15 | 20.0 | 15 | 20.0 | 11 | 14.7 | 21 | 28.0 | 75 |
Abbreviations: S = Situations, n=number of respondents, N=total number of respondents in each situation, SD: Standard Deviation, IEEC = Index of Exposure to Ethical Conflicts.
Index of exposure to ethical conflict
Exposure to ethical conflict resulted from the product of the frequency and the degree of ethical conflict, named as index of exposure to ethical conflict (IEEC). At the descriptive level, central tendency measures showed a mean of 136.50, standard deviation (SD) of 85.706, and the range of 0–358. Low exposure to an ethical conflict was up to 76.50, moderate was 76.51–197.99, and the high was 198 and above. So, this proves that the critical care nurses had a moderate level of exposure to ethical conflict.
The relative frequencies of the low and high level of exposure to an ethical conflict were 24.8% both in the same line, while the relative frequency of moderate level of exposure to the ethical conflict was 50.4%.
Data analysis shows that Scenario 7: “Realizing that the analgesia and/or sedation being given to the patient is not effective enough and that the patient is suffering” (Mean=11.38, SD=7.811) and Scenario 12: “Working with a nurse or nursing assistant who I consider to be professionally incompetent” (Mean=10.50, SD =7.833) were the most conflictive situation (Table 4).
Table 4.
Associated variables with level of exposure to ethical conflict.
| Variables | Categories | N (%) | p* |
|---|---|---|---|
| Unit of work | ICU | 62 (53) | p<0.001 |
| CCU | 28 (23.9) | ||
| NICU | 20 (17.1) | ||
| PICU | 7 (6) | ||
| Perceived work stress | Yes | 73 (62.4) | p<0.001 |
| No | 44 (37.6) | ||
| Having family/friends with COVID-19 infection | Yes | 46 (39.3) | p<0.05 |
| No | 71 (60.7) |
*Chi-square tests.
Relationship between level of exposure to ethical conflicts and socio-demographic, occupational, and COVID-19 variables.
All the socio-demographic variables such as age, gender, marital status, and level of education were not statistically significant in association with the level of exposure to ethical conflicts (p>0.05).
The occupational variables such as type of contract, work shift, total years of professional work experience, and total years of professional work experience in critical care units are statistically insignificant. At p<0.001, the statistically significant variables were unit of work and perceived work stress, related to a higher level of exposure to ethical conflicts. Nurses working in ICU had a higher level of exposure than nurses working in CCU, NICU, and PICU. Likewise, critical care nurses with perceived work stress had a higher level of exposure to ethical conflict (Table 4).
Variables such as COVID-19 infection, afraid of the pandemic, and perceived ethical conflicts in a pandemic are statistically insignificant. However, at p<0.05, the only significant variable was having family/friends with COVID-19 infection. Critical care nurses whose family/friends were infected with COVID-19 had a higher level of exposure to ethical conflicts (Table 4).
Discussion
The main aim of this research was to explore critical care nurses' level of exposure to ethical conflicts. The finding of this study showed a moderate level of exposure to ethical conflicts and this result is consistent with five earlier studies.8,14,15,21,23 In fact, the rate of critical care nurses who are exposed to moderate levels of exposure to ethical conflicts in this research is lower than in previous studies. A study conducted in Iran found that 58.3% of the critical care nurses are exposed to moderate levels of exposure to ethical conflicts.23
These results might reflect a high engagement of ICU nurses in the decision-making process, previously described as a protective factor against the emergence of ethical. Perhaps higher levels were expected to be found considering the pandemic situation. However, we believe that the fact that this study was carried out during the critical phase of the first wave of the pandemic in the country may somehow be helpful to understand the results. The high demand for care and the scarcity of resources may have left nurses insufficient time to dedicate themselves to identifying and discussing sources of ethical conflicts in their work contexts, especially in the ICU. In addition, given the absence of family members in these contexts during the pandemic, it may have generated the delegation of these types of questions to the background, to the detriment of practical and objective questions that were constantly being asked to health professionals, especially nurses.
In this study, the highest level of exposure to ethical conflicts in critical care units was related to the ineffectiveness of analgesic pain control treatment in critical patients. This result is similar to two studies conducted in Portugal and Barcelona, which reports the highest level of exposure in the same scenario with mean scores of 13.217 and 14.43.5,21 In contrast to this, studies conducted in Iranian critical care nurses identify that working with professionally incompetent medical staff and working with nurses or nursing assistants who are professionally incompetent generated a higher level of exposure to ethical conflict.15,23
This study also mentions that one of the potentially conflictive situations in which the family did not know the aims or risks entailed in the treatment administered to a patient-generated the lowest level of conflict and this result corroborates with another Spanish study.8
The next aim of the research was to identify the types of ethical conflicts. According to this objective, “Moral Outrage” was the type of ethical conflict most frequently experienced by the professionals, in line with the previous study conducted in Barcelona.8 However, these results differ from studies conducted in Iranian nurses, in which “Moral dilemma” was the most frequently experienced type of ethical conflict.15,23
In line with what was described in the literature,4,14 we assumed as a hypothesis that sociodemographic variables could have some influence or be related to ethical decision-making processes. However, the findings of our study add support to this statement that socio-demographic variables are not related to exposure to ethical conflicts. This finding is in the same line with the results of a study conducted in the USA which mentions that sociodemographic variables cannot assume the level of moral distress.18 Conversely, one of the studies revealed that marital status and level of education of critical care nurses were associated with a high level of exposure to ethical conflicts.23 Likewise, previous studies about moral distress have shown correlations between age and gender with the high level of moral distress.19,24
Regarding to the occupational variables, type of contract, work shift, total professional experience no association was detected with exposure to ethical conflicts. However, variables as “unit of work” and “perceived work stress” were found to be related to the exposure to ethical conflicts. In simpler words, nurses working in ICU had higher exposure to ethical conflict than nurses working in other critical care units. Also, nurses with perceived work stress had more exposure to ethical conflict. It seems that high exposure to ethical conflicts also creates high perceived work stress. Previous studies in ICU shown that conflicts are strongly associated with burnout syndrome in nurses.25 In the same line, neonatal and pediatric ICU had a low level of exposure to ethical conflict.24 Another finding of this study indicates that perceived work stress leads to higher exposure to ethical conflicts which is in the same line with the results of the study conducted among Portuguese nurses.21 In contrast to this, one of the studies implies that neither demographic nor work-related variables can predict moral distress.18
Concerning the COVID-19 variables, to date, exposure to the ethical conflict has not been compared in the related literature. However, having friends/family infected with COVID-19 showed significant relation to exposure to ethical conflicts in our study. Nurses being infected with COVID-19, being afraid of the pandemic, and perceived ethical conflict in pandemic were not related to exposure to ethical conflict. It´s important to highlight that “Administering treatments and/or carrying out procedure without, as a nurse, having been previously involved in the decision to do so” arise with the highest frequency in our study. We believe these data have a strict relationship with COVID-19 pandemic. In the COVID-19 pandemic, one of the general measures adopted by many health systems was the total limitation or restriction to visitors or relatives to reduce the transmission of the virus.26 This limitation was also found in the Spanish health system.
The work overload associated with the need for immediate decision-making that occurred in the context of critical care has, in many cases, removed nurses from this prior decision-making process, often discussed with the family in previous situations. However, one of the studies conducted among Chinese nurses to determine ethical challenges while caring for COVID-19 patients reported that nurses faced ethical challenges on numerous facades in caring for COVID-19 patients.27
Study limitations
Although the present study provides interesting clinical data, it has some limitations.
The first limitation concerns sample selection. The data was collected from critical care units of a hospital in Asturias in a very short period. Even though the response rate was 81.25%; considered sufficient, it cannot be considered nationwide representative. Therefore, it can only be applied to the mention units and comparable settings. To address this limitation, further research with a larger sample and a variety of critical care and emergency settings of different countries or larger areas of Spain is recommended.
Nursing implications
Overall, this study contributes to the evaluation of exposure to ethically problematic situations and types of ethical conflicts encountered by critical care nurses. Furthermore, the findings of these results provide a deeper understanding of ethical conflicts in such conflictive situations such as implications on recognizing the situations that occur in everyday clinical practice, identifying the ethical conflicts, and facilitating the nurses working in the challenging clinical situation. Mainly, the results inform the development of interventions that aim to proactively and broadly favor low level of ethical conflicts in the critical care unit, and allows more professional adherence to the ethical standards, thereby improving the delivery of care.
Future research
This study highlights that more research regarding exposure to ethical conflicts and COVID-19 is needed. It would be interesting to nursing field to know the main differences between ICU ethical conflicts before and after the COVID-19 pandemics and to describe the nursing professional gaps on the ability and skills to cope with the found differences. Another investigation line could be to determine which variables could predict a higher exposure to ethical conflicts in nursing from ICU awards. Another investigation line could be to determine which variables could predict a higher exposure to ethical conflicts in nursing from ICU awards.
Conclusion
Globally, comparing to studies before the pandemic, not higher levels of exposure to ethical conflicts were identified in ICU nurses despite data were collected during COVID-19 outbreak. Intensive Care Unit nurses revealed moderate level of exposure to ethical conflicts, which indicates a clear emphasis on the deeper examination of the complex phenomenon of ethical conflict in the clinical setting. The most conflictive situations identified were related to the ineffectiveness of analgesics and working with the potentially incompetent nurse or nursing assistant. There seems to be an association between ICU nurses’ level of exposure and unit of work, perceived work stress, and having family/friends with COVID-19 infection. Moral outrage is identified as the most experienced type of ethical conflict on this population.
Supplemental Material
Supplemental Material, sj-pdf-1-nej-10.1177_09697330211066574 for Ethical conflict among critical care nurses during the COVID-19 pandemic by Anjita Khanal, Sara Franco-Correia and Maria-Pilar Mosteiro-Diaz in Nursing Ethics
Acknowledgments
The authors like to express thanks to all critical care nurses who participated in the study.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Anjita Khanalhttps://orcid.org/0000-0003-0007-1645
Sara Franco-Correia https://orcid.org/0000-0001-5341-5419
Maria-Pilar Mosteiro-Diaz https://orcid.org/0000-0002-3375-9334
References
- 1.WHO . WHO COVID-19 Explorer, 2021, https://worldhealthorg.shinyapps.io/covid/(accessed 17 May 2021). [Google Scholar]
- 2.Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. LancetResp Med 2020; 8(5): 506–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quigley AL, Stone H, Nguyen PY, et al. Estimating the burden of COVID-19 on the Australian healthcare workers and health system during the first six months of the pandemic.IJNS 2021; 114: 103811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ndunge Mutinda J, Wagoro M. Sociodemographic factors influencing the experience of ethical dilemmas among nurses in critical care unit of Kenyatta National Hospital. Am J Nurs Sci 2017; 6(2): 113–124. [Google Scholar]
- 5.Falcó-Pegueroles A, Lluch-Canut T, Guàrdia-Olmos J. Development process and initial validation of the ethical conflict in nursing questionnaire-critical care version. BMC Med Ethics 2013; 14: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dierckx de Casterlé B, Izumi S, Godfrey NS, et al. Nurses’ responses to ethical dilemmas in nursing practice: meta-analysis. J Adv Nurs 2008; 63(6): 540–549. [DOI] [PubMed] [Google Scholar]
- 7.Redman BK, Fry ST. Nurses’ ethical conflicts: what is really known about them? Nurs Ethics 2000; 7(4): 360–366. [DOI] [PubMed] [Google Scholar]
- 8.Falcó-Pegueroles A, Lluch-Canut T, Roldan-Merino J, et al. Ethical conflict in critical care nursing: correlation between exposure and types. Nurs Ethics 2015; 22(5): 594–607. [DOI] [PubMed] [Google Scholar]
- 9.Marckmann G, Schmidt H, Sofaer N, et al. Putting public health ethics into practice: a systematic framework.Front PublicHealth 2015; 3: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klingler C, Silva DS, Schuermann C, et al. Ethical issues in public health surveillance: a systematic qualitative review. BMC Public Health 2017; 17(1): 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zolkefli Y. Negotiated ethical responsibility: bruneian nurses’ ethical concerns in nursing practice. Nurs Ethics 2019; 26(7–8): 1992–2005. [DOI] [PubMed] [Google Scholar]
- 12.Gutierrez KM. Critical care nurses’ perceptions of and responses to moral distress. Dimens Crit Care Nurs 2005; 24(5): 299–341. [DOI] [PubMed] [Google Scholar]
- 13.Cerit B, Dinç L. Ethical decision-making and professional behavior among nurses: a correlational stud. Nurs Ethics 2013; 20(2): 200–212. [DOI] [PubMed] [Google Scholar]
- 14.Falcó-Pegueroles A, Lluch-Canut MT, Martínez-Estalella G, et al. Levels of exposure to ethical conflict in the ICU: correlation between sociodemographic variables and the clinical environment. Intensive Crit Care Nurs 2016; 33: 12–20. [DOI] [PubMed] [Google Scholar]
- 15.Pishgooie AH, Barkhordari-Sharifabad M, Atashzadeh-Shoorideh F, et al. Ethical conflict among nurses working in the intensive care units.Nurs Ethics 2019; 26(7–8): 2225–2238. [DOI] [PubMed] [Google Scholar]
- 16.Peter E, Liaschenko J. Moral distress reexamined: a feminist interpretation of nurses’ identities, relationships, and responsibilites. J Bioeth Inq 2013; 10(3): 337–345. [DOI] [PubMed] [Google Scholar]
- 17.Fernandes MI, Moreira IM. Ethical issues experienced by intensive care unit nurses in everyday practice. Nurs Ethics 2013; 20(1): 72–82. [DOI] [PubMed] [Google Scholar]
- 18.Corley MC, Elswick RK, Gorman M, et al. Development and evaluation of a moral distress scale. J Adv Nurs 2001; 33(2): 250–256. [DOI] [PubMed] [Google Scholar]
- 19.Sannino P, Giannì ML, Carini M, et al. Moral distress in the pediatric intensive care unit: an Italian study. Front Pediat 2019; 7: 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pike AW. Moral outrage and moral discourse in nurse-physician collaboration.J Prof Nurs 1991; 7(6): 351–362. [DOI] [PubMed] [Google Scholar]
- 21.Lluch-Canut T, Sequeira C, Falcó-Pegueroles A, et al. Ethical conflicts and their characteristics among critical care nurses. Nurs Ethics 2020; 27(2): 537–553. [DOI] [PubMed] [Google Scholar]
- 22.Bond L, Kearns A, Mason P, et al. Exploring the relationships between housing, neighbourhoods and mental wellbeing for residents of deprived areas.BMC Public Health 2012; 12: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saberi Z, Shahriari M, Yazdannik AR.The relationship between ethical conflict and nurses’ personal and organisational characteristics.Nurs Ethics 2019; 26(7–8): 2427–2437. [DOI] [PubMed] [Google Scholar]
- 24.Sporrong SK, Höglund AT, Arnetz B. Measuring moral distress in pharmacy and clinical practice. Nurs Ethics 2006; 13(4): 416–427. [DOI] [PubMed] [Google Scholar]
- 25.Poncet MC, Toullic P, Papazian L, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med 2007; 175(7): 698–704. [DOI] [PubMed] [Google Scholar]
- 26.Karanikola MNK, Albarran JW, Drigo E, et al. Moral distress, autonomy and nurse-physician collaboration among intensive care unit nurses in Italy. J Nurs Manag 2014; 22(4): 472–484. [DOI] [PubMed] [Google Scholar]
- 27.Jia Y, Chen O, Xiao Z, et al. Nurses’ ethical challenges caring for people with COVID-19: a qualitative study. Nurs Ethics 2021; 28(1): 33–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-nej-10.1177_09697330211066574 for Ethical conflict among critical care nurses during the COVID-19 pandemic by Anjita Khanal, Sara Franco-Correia and Maria-Pilar Mosteiro-Diaz in Nursing Ethics