Abstract
We used a structured interview to explore approaches to comprehensive hemophilia and arthropathy care among 24 healthcare professionals (HCPs) from multidisciplinary teams (MDTs) in Canada and the UK. Represented MDTs typically comprise a hematologist, nurse, physiotherapist, and sometimes an orthopedic surgeon; pediatric (and some adult) MDTs also include a social worker/psychologist. HCPs emphasized the centrality of a team approach, facilitated through MDT meetings and involvement of all MDT members in patient care. In both countries, nurses and physiotherapists play critical, multifaceted roles. Respondents agreed that MDTs are crucial for successful transitioning, which can be facilitated by close collaboration between pediatric and adult MDTs, even when they are not co-located. Physiotherapists are instrumental in providing non-pharmacological pain relief. Hematologists or physiotherapists typically make orthopedic referrals, with the nurse, physiotherapist and hematologist working together in patient preparation for (and follow-up after) surgery. MDT best practices include a non-hierarchical team approach, ensuring that all MDT members know all patients, and regular MDT meetings. Together, these real-life insights from the MDT perspective emphasize the value of the MDT approach in comprehensive hemophilia care.
Keywords: hemophilia A, comprehensive healthcare, joint diseases, patient care team, surveys, questionnaires
Introduction
Recurrent joint bleeds in hemophilia inevitably lead to hemophilic arthropathy, 1 the treatment and prevention of which are best achieved through the integrated delivery of comprehensive care in a hemophilia treatment center (HTC) by a multidisciplinary team (MDT). The World Federation of Hemophilia (WFH) guidelines recommend that MDTs include a hematologist, nurse, physiotherapist, and a psychosocial expert (social worker or psychologist). 2 MDT structure and function are similar in countries like Canada and the UK; they provide specialist care in the different aspects of hemophilia, maintain patient records, educate stakeholders, undertake research, and participate in national registries in both countries.3,4
However, healthcare systems in these countries differ in certain respects. In Canada, healthcare is primarily funded and administered by each province and territory, paid for through taxation and public funds, and available to all Canadians at no out-of-pocket expense. 5 The National Health Service in the UK is a government-funded, centralized healthcare service paid for mostly through taxation and available to all UK residents. It is free to patients at the point of delivery, though there are slight differences in what is fully government-funded between the different UK countries.6,7 Differences in healthcare systems mean there could be significant differences in the function of MDTs between Canada and the UK. An analysis of contemporary practices within and between the 2 countries can provide a cross-sectional description of how care is delivered and potentially offer opportunities for stakeholders in these and other healthcare systems to examine areas of similar or divergent practice, highlighting challenges faced by teams in developing MDT care.
Hence, a survey was conducted among members of MDTs in HTCs from Canada and the UK, with a 3-fold aim: to investigate MDT practices across early and late arthropathy, including specialty-specific and team-based practices; to highlight approaches to comprehensive hemophilia care; and to identify system-wide and specialty-specific barriers to successful MDT care.
Materials and Methods
Participants and Survey Development
Healthcare professionals (HCPs) within MDTs were interviewed using a structured, qualitative survey developed by a contract research organization (CRO) in collaboration with the authors (Supplemental materials). The survey was developed using an existing Survey Monkey® survey, case study material, and probing questions. Consent was assumed when participants confirmed acceptance of an email invitation and agreed to proceed with the survey. Each HCP was asked to respond to each question based on his/her recall and opinion. All data were anonymized, kept password-protected and confidential by the CRO, and treated in accordance with data protection laws and ethical research guidelines. Data were analyzed using descriptive statistics.
Survey Content
General questions covering the role of MDTs in managing patients with hemophilia were presented to all HCPs; questions covering specific individual roles in managing hemophilic arthropathy were posed based on specialty (Supplemental materials). These included: HCP role and responsibility; years of experience; patient age; clinical services; processes/practices in place for communication; policies/practices that were thought effective and policies/practices that should be different; and common challenges in the management of hemophilic arthropathy.
Managing Hemophilic Arthropathy
HCPs were asked how their MDT would treat 2 case studies detailing early and late hemophilic arthropathy (Supplemental materials): an 8-year-old male receiving prophylaxis for severe hemophilia B who developed an acute traumatic ankle bleed, and a sedentary 56-year-old male with severe hemophilia A and chronic knee arthropathy, receiving on-demand therapy.
Results and Discussion
Participants
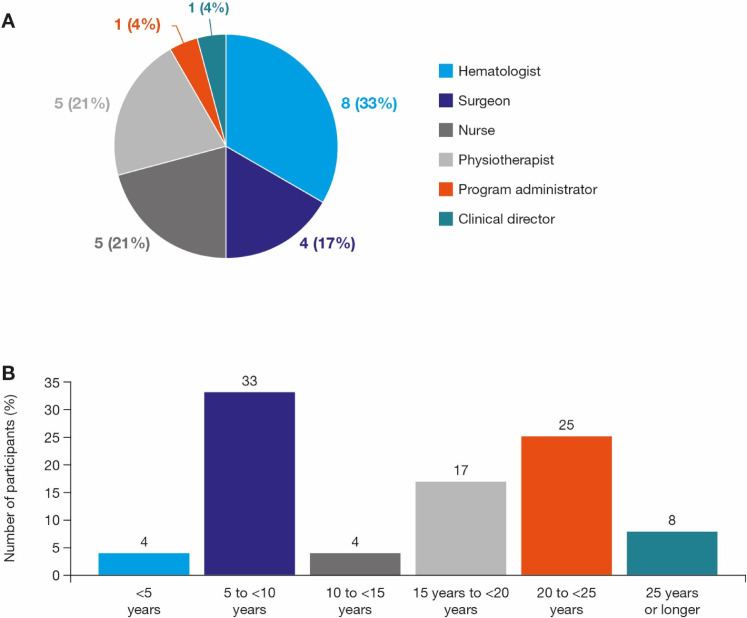
Between September and November 2019, the CRO conducted structured, ∼1-h interviews. In total, 24 participants from 11 HTCs completed interviews; a further 34 HCPs declined to participate. Most participating HCPs were hematologists (33%), nurses (21%), and physiotherapists (21%) (Figure 1a), and a plurality (33%) had 5–<10 years’ experience in their specialty (Figure 1b). The 11 HTCs from which participating HCPs were selected treat from 60 to 1500 patients with hemophilia; several of these HTCs are regional, with a wide catchment area. Most HCPs in our survey treat children/adolescents or adolescents/adults only, with 7 HCPs from 2 HTCs in Canada treating patients throughout their lifetime.
Figure 1.
A. Healthcare professionals in the MDT survey study by specialty. B. Healthcare professional years of experience in specialty.*
*Years of experience was not obtained from two HCPs.
MDT, multidisciplinary team.
Structure and Function of MDTs
Responses from survey participants showed that MDTs typically comprise 1 or more hematologists, nurses, and physiotherapists. All pediatric, and some adult, MDTs include a social worker or psychologist; 1 HCP's MDT also included a laboratory specialist. These responses show that MDT composition is generally in accordance with WFH guidelines. 2 Some HCPs reported their MDT also included a dedicated orthopedic surgeon, while others at least had access to an orthopedic surgeon, and to other specialties, as needed.
A key finding of the survey was that nurses and physiotherapists play crucial and multifaceted roles in patient care and coordinating the MDT. Additionally, HCPs consistently emphasized the centrality of a team approach by ascribing considerable importance to clear, regular communication within the MDT and by highlighting the involvement of all MDT members on clinic days.
It should be noted here that the range of activities or types of care (such as modifying a treatment plan or prescribing a medication) that a given category of HCP, such as the hemophilia nurse, can autonomously perform varies by country and jurisdiction, and is usually governed by the health laws of that jurisdiction. In Canada, this jurisdiction is provided at the provincial level. Hemophilia clinics have often been at the forefront of delegating certain medical acts to nurses, but this is usually under the legal responsibility of the physician. A similar arrangement is present in UK. The survey did not specifically ask which activities or aspects of care could or could not be provided by the nurse within each MDT, and the nurse's roles in different teams may have evolved since the survey was conducted.
Regarding internal MDT communication, most HCPs confirmed MDT meetings occur regularly, usually weekly; some HCPs also attend other meetings, such as those focusing on clinical development, laboratory issues or research. Meetings involving orthopedic surgeons tend to happen separately, less frequently and are typically associated with musculoskeletal clinics; one orthopedic surgeon reported holding bi-annual meetings with orthopedic surgical colleagues. HCPs from several disciplines also emphasized the importance of informal, ad hoc communication either as an adjunct to scheduled team meetings or as a key mode of communication replacing formal team meetings. These HCPs indicated that such informal communication is greatly facilitated by all team members being located in the same space within the building.
HCPs consistently reported that the whole MDT is always involved in clinic days, further highlighting the centrality of the team approach in patient care. Clinic days operate according to a highly structured workflow that defines each individual clinic. HCPs reported many similarities in specific details of clinic days, but there were also variations. For instance, the nurse is often, though not always, the first team member to see the patient; psychologists and/or social workers tend to play a more prominent role in pediatric clinics. HTCs are open 5 days a week for virtual or face-to-face assessment/treatment and review. An HTC-affiliated physician is always available to medical colleagues for night/weekend consultations. Most HTCs have a once-weekly clinic day, though larger HTCs may have 2 clinic days each week. All patients have a comprehensive, annual, in-clinic visit, with additional visits scheduled based on clinical need. Two HCPs (1 physiotherapist, 1 orthopedic surgeon) also noted that separate musculoskeletal clinics are held approximately monthly or quarterly; the quarterly musculoskeletal clinics double up as annual or semi-annual visits. These findings show that the MDTs represented by the survey respondents are following WFH guidelines for hemophilia care, which stipulate that patients should be seen by all core MDT members at least annually (semi-annually for children) for a complete hematological, musculoskeletal, and quality-of-life assessment, 2 although the survey showed that formal psychosocial assessment seems to be less consistent in adult practice compared to pediatric care.
Clinical Arthropathy Care
The survey addressed six key aspects of patient care and arthropathy management: transitional care, orthopedic surgery, pain management, technology and new therapies, research and keeping up to date.
Transitional care
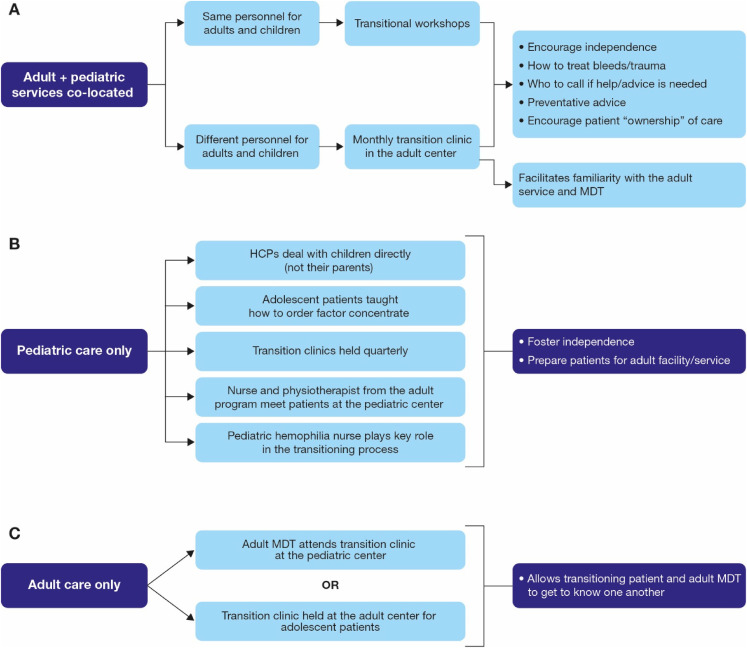
Sometimes, where pediatric and adult care services are in the same center, HCPs provide care to patients throughout their lifetime; in these cases, HCPs indicated that graduating from pediatric to adult care is an element of ongoing, lifelong “continuous” care where patients are treated and managed by many of the same personnel. This allows for easier, more natural transitioning. Transitional workshops in these clinics encourage patients to become more independent in terms of managing their care and liaising with the MDT (Figure 2a). Co-location of pediatric and adult care eases transition even when the services are overseen by different personnel, simply because the two services exist on the same campus. HCPs in our survey indicated that, in these circumstances, transition workshops not only help patients take ownership of their treatment, but also familiarizes them with the adult service and the MDT members they will interact with after the transition to adult care (Figure 2a).
Figure 2.
Characteristics of representative transitioning processes when adult and pediatric services are co-located (A) and when pediatric (B) and adult (C) services are in separate facilities.
HCP, healthcare professional; MDT, multidisciplinary team.
HCPs who only treat children or adults emphasized the importance of dedicated transitional care programs where transitioning patients spend time in the adult clinic or staff from an adult clinic spend time in the pediatric clinic. Again, the goal of these transitional care programs is to foster independence, prepare patients for adult care, allow patients and HCPs to get to know each other and develop confidence in the new team (Figures 2b, 2c). Logistically, the process is less straightforward, but several HCPs noted close collaboration between pediatric and adult MDTs can still successfully support the transitioning process. This survey confirmed the pivotal role of hemophilia nurses and physiotherapists in transitional care.
A multidisciplinary approach is key to successful transitioning 8 and, accordingly, HCPs in our survey consistently recognized the importance of transitional care; most clinics represented by the respondents have dedicated transition services handling patient transitioning sensitively using structured protocols. Supporting patient independence and personal responsibility for care were the primary aims of transition and key outcome indicators of success, including adherence, self-efficacy skills (eg self-infusion and ordering factor independently), and a good understanding of all aspects of hemophilia. 9 Furthermore, as one HCP emphasized, transition can be an emotional process for patients and their families: patients have often known their care providers all their lives, so leaving the pediatric service can be like leaving home. Data are lacking on the optimal model of transition but the key principle ie ensuring a smooth transfer to adult services is highly likely to enhance lifelong hemophilia care. 10 This survey suggests the feasibility of a smooth transfer is considerably enhanced when pediatric and adult services are co-located in the same center.
Orthopedic surgery
Respondents highlighted similar approaches in terms of the MDT members typically responsible for each aspect of surgical management. Referrals to formal orthopedic review were usually from hematologists and physiotherapists. If the HTC had integrated hematology and orthopedics, a specific MDT member was not responsible for referrals. In other instances, physiotherapists suggest referrals to hematologist or orthopedic surgeon, and preparing the patient for surgery, which included assessment of arthropathy, patient education, development of action plan, and patient follow-up. Nurses were also responsible for patient preparation and follow-up, working with the hematologist to administer perioperative hemostasis treatment. The orthopedic surgeon usually saw patients ≥1 times during follow-up. Although an MDT coordinator has been recommended for elective surgery in patients with hemophilia, 11 several respondents stated the physiotherapist is usually very involved in patient assessment and follow-up.
Pain management
Several HCPs indicated that physiotherapists are instrumental in providing non-pharmacological pain relief (for example, rehabilitation, bracing, use of ice). Pharmacological approaches identified by most HCPs included nonsteroidal anti-inflammatory drugs and opioids, although opioid use was “minimal” in most cases. Several respondents also said that despite pain being typically managed by the MDT, sometimes referral to a pain clinic is necessary.
Technology
Technology use in hemophilia care is evolving. Most participants reported their patients use electronic diaries, apps, and/or electronic national databases to record bleed and treatment information. Participants highlighted the following positive impact on care: apps showing pharmacokinetic data/estimating factor levels (thus serving as a treatment reminder) can educate patients about the potential effects of certain physical activities on joint health; for acute bleeds, initial treatment can be prescribed using video conferencing and email, with face-to-face consultations if the bleed does not resolve; two HCPs emphasized the usefulness of remote care for acute bleeds. Technology use can be more efficient, allowing early review of emergencies and treatment initiation, reducing the need for extensive travel by MDT personnel and has the potential to address current gaps in service.
New therapies, research, and keeping up-to-date
Most HCPs reported a research program at their HTC; however, not all had dedicated research funding. Research often overlaps with clinical care, and nurses were commonly identified as being heavily involved in research and performing a “bridging” role between research and the clinic. HCPs reported a variety of avenues for learning and keeping up to date with developments in the field, including international meetings, interaction and collaboration with colleagues, inter-clinic and MDT meetings, teaching, and training programs. Although the training of new MDT members was not specifically covered by the survey, it is worth noting here that the training of new HCPs in their duties is typically provided by more senior HCPs of the same category within each HTC. In Canada, there are also annual workshops organized by the Hemophilia Society for new team members from across the country to receive training and interact with peers. In the UK, training is organised by nursing and medical professional bodies and in-house.
Among survey participants, there was overall optimism about the newer therapies, and several HCPs indicated the potential for improved outcomes.
Managing Hemophilic Arthropathy: Case Studies
Pediatric case study: early arthropathy
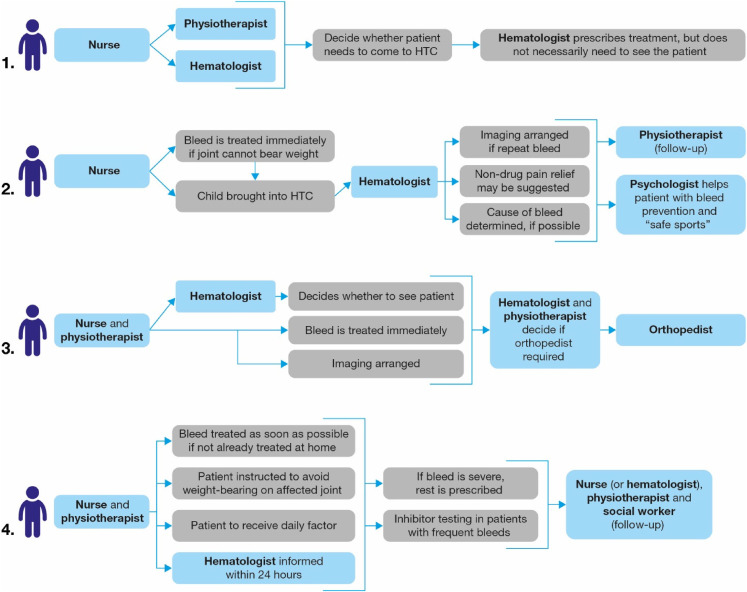
Acute bleeding in an 8-year-old patient with early arthropathy: HCPs providing pediatric care highlighted four approaches to managing this case (Figure 3). All respondents agreed the nurse, physiotherapist, and hematologist would typically be the MDT's key members; in many cases the nurse would normally be the patient's first point of contact (approach 1 and 2), often in conjunction with the physiotherapist (approach 3 and 4). Beyond this, there were other broad similarities in managing the case (Figure 3). For example, commonly, hematologists are kept informed about patients with acute bleeds, and consulted as necessary, but do not need to see the patient unless the bleed is significant or severe: often, treatment can be administered/assessed by other MDT members. As physiotherapy is crucial for the management of hemarthrosis and maintenance of function in patients with hemophilia,12,13 guidelines recommend a physiotherapist becomes involved in patient care as soon as a joint bleed is reported.12,13 Accordingly, most HCPs indicated that their MDT physiotherapist is usually instrumental in managing acute bleeds; however, one HCP noted that physiotherapy might need to be delayed if the bleed or injury is severe. MDT members highlighted as being involved in follow-up were the nurse (or hematologist), physiotherapist and perhaps a social worker/psychologist.
Figure 3.
Approaches to management of an acute bleed in a child with early arthropathy (pediatric case study).*
*All approaches are based on survey responses that provided sufficient specific detail when asked about the management of acute bleeds in a child with early arthropathy.
HTC, hemophilia treatment center.
Some HCPs reported they would perform imaging (typically ultrasound) at presentation for such a young patient with arthropathy, but one HCP suggested physical examination is adequate, and another noted imaging would only be arranged if a repeat bleed occurred. Imaging may be used during assessment or follow-up. One HCP reported they would consider multiple factors (eg, pharmacokinetic studies, trough levels, phenotype) if the MDT concluded a change in the patient's treatment was necessary.
Adult case study: late arthropathy
Total knee replacement was recommended for a 56-year-old patient with hemophilia and chronic arthropathy: all HCPs providing care for adults agreed this surgery would be necessary and a routine part of the management plan for such a patient. However, as one HCP highlighted, patients can sometimes take a long time to agree to recommended surgery, therefore, comprehensive counselling including a psychologist can help these patients understand the value of receiving a joint replacement and address their concerns.
Most HCPs agreed the whole MDT would be involved in the patient's care, but with some variations regarding team member roles. For instance, for one HCP, the whole MDT would manage perioperative bleeding and follow-up treatment (except pain relief, which would be prescribed by surgeons); several other HCPs reported their treatment protocol for perioperative hemostasis would be managed by the hematologist. The same HCP also reported the physiotherapist would have a more prominent role than other MDT members in assessing the patient, preparing recommendations for the orthopedist and overseeing post-surgical care. Another HCP indicated the nurse would be the patient's direct point-of-contact, liaising with the orthopedist; however, where a dedicated orthopedist is not available, the hematologist, nurse and physiotherapist would jointly manage the patient (an orthopedist would be sought if necessary, depending on the affected joint). Suggestions for less invasive options included physiotherapy, an injection to reduce inflammation and radioactive synovectomy for pain relief prior to total knee replacement. Physiotherapists and nurses play significant roles in follow-up (occurring weekly or bi-weekly) and long-term prophylaxis would be encouraged.
HCPs consistently emphasized the importance of preparing patients for surgery (“prehabilitation”) and ensuring thorough surgical aftercare. Physiotherapists were reported to play a prominent role in prehabilitation and aftercare; nurses were also crucial. Two key challenges to follow-up care were identified: first, if patients do not live locally, post-operative management and rehabilitation can be difficult and may necessitate coordination with local care services/resources. Second, as more older patients with hemophilia and co-morbidities (eg, cardiovascular disease) are encountered, medical and post-surgical needs become more complex. Thus, treatment strategies need to evolve, so the general management of such individuals may benefit from a more collaborative approach involving HCPs from other specialties.
Challenges in Improving Care
Many HCPs identified a lack of financial resources and personnel as a key barrier to optimal hemophilia care. For example, total full-time equivalents within specific disciplines, such as physiotherapy, psychology/social work, and nursing were limited. Therefore, resources need to be maximized and staff upskilled to optimize care and meet the challenges of inadequate funding.14,15 Several HCPs emphasized the need for more physiotherapy time and cited a lack of patient adherence as a major issue hindering the provision of best care, particularly for adolescents and young adults.
When asked about challenges specific to the management of arthropathy, HCPs again identified lack of funding and resources, and lack of patient engagement as key barriers. Another key challenge is accurate detection of early disease and subtle joint changes between different regimens/treatments, which requires sensitive tools such as MRI; however, MRI images lack a reliable and valid correlation with clinical joint status in real time. 15 Notwithstanding, ultrasound is becoming a first-line tool for the point of care of joint status, although the images may have limited value compared to MRI.15,16 Overall, respondents noted there are still issues in managing hemophilic arthropathy; patient engagement in chronic disorders is challenging and newer ways of improving engagement is warranted.
Best Practices and Policies
When asked to identify what they considered to be the most helpful practices and policies employed by their centers, HCPs provided a variety of responses broadly categorized as relating to the MDT, patient management, technology and orthopedics. These responses are summarized in Table 1.
Table 1.
Best Practices and Policies From the Perspective of Individual HCPs.
| Area | Highlighted best practice or policy |
|---|---|
| MDT |
|
| Patient management |
|
| Technology |
|
| Orthopedics |
|
MDT, multidisciplinary team; MSK, musculoskeletal.
Suggested Changes in Clinical Practices and Policies
Respondents provided several suggestions for potential improvements to clinical practices and policies. These included more opportunities for learning on the job, more involvement in research and attending conferences, and the development of more policies with a fuller understanding of hemophilia treatment practices. Additional suggestions included: streamlining assessment tools; creating a formal registry; improving network services and record keeping; and establishing online care plans to improve ease of access, for patients and clinicians, and ensure smoother care (eg, improving out-of-hours patient safety).
Conclusion
This study provides real-life insights into the management of hemophilic arthropathy from various members of MDTs in Canada and the UK. Unlike a formal, external accreditation-type evaluation, our perspective is from within the MDTs. Based on these perspectives, best practices in comprehensive hemophilia care were shown to be similar between Canadian and UK HTCs, despite significant differences in healthcare structure, and both countries faced similar challenges in providing care due to resource constraints. Further, HCP responses indicate that different MDTs in different centers share broadly similar functioning, with each team working well and efficiently within its particular setting. However, these settings also give rise to variations in practice: the functioning of MDTs evolves not only according to their contexts, but also according to the unique contributions of the different individuals comprising the MDT. Thus, each MDT exhibits a uniqueness stemming from its distinct circumstances and members. Additionally, even though the majority of survey respondents were “core” members of the MDT (hematologists, nurses and physiotherapists), it is important to emphasize that all MDT members—including those who also have administrative duties, such as the clinical director and program administrator—are directly involved in patient care.
To our knowledge, best practices between two countries and between specialties have not been compared in the context of an MDT approach to managing hemophilic arthropathy; therefore, this study contributes a unique perspective. Limitations of this study include the small number of clinics and specialists, and the non-random nature of the sample. Future studies including a larger number of HTCs from a wider variety of countries, and perhaps including patient interviews, are warranted. Further, the survey was conducted in two countries (Canada and the UK) where individual specialties such as hemophilia nurses and physiotherapists have long-standing, established and recognized roles within the MDT and are therefore instrumental in shaping its organization and functioning. However, this is not the case for hemophilia care in many countries worldwide, and so the MDT practices described in this study may not be applicable to (or possible in) those regions.
In light of the critical and indispensable roles of nurses, physiotherapists, and social workers/psychologists in the daily functioning of efficient MDTs, this study suggests ways these professionals can be most effective. Importantly, this study also helps all HCPs involved in hemophilia management to better understand the critical role and value of the MDT approach in providing optimal patient care. Involvement in an MDT provides a stimulating work environment, and the MDT model of care is now applied in many fields of medicine. However, care teams face various pressures, and this survey encourages all hemophilia MDT members to evaluate their practice to ensure that they remain committed to true interdisciplinarity in their work.
Supplemental Material
Supplemental material, sj-docx-1-cath-10.1177_10760296211070002 for Multidisciplinary Team Care of Patients with Hemophilic Arthropathy: A Qualitative Assessment of Contemporary Practice in the UK and Canada by Jean St-Louis, Pratima Chowdary, Gerry Dolan, Dawn Goodyear, Karen Strike, Debra Pollard and Jerry Teitel in Clinical and Applied Thrombosis/Hemostasis
Acknowledgments
Medical writing support was provided by Bill Kadish and Jo Fetterman (Parexel International) and funded by Novo Nordisk A/S.
Footnotes
Disclosures: All participants signed a consulting agreement and were paid an honorarium for their time; survey participants who are authors received a stipend only for the time responding to the survey.
JSL has served as a consultant for Novo Nordisk, Octapharma, Roche, Sanofi, and Takeda; and receives research funding from Sanofi and Takeda. PC has served on advisory boards for Bayer, Biogen Idec, Chugai, CSL Behring, Freeline, Novo Nordisk, Pfizer, Roche, Sanofi, SOBI, Spark, and Takeda; and has received research funding from Bayer, CSL Behring, Freeline, Novo Nordisk, Pfizer, and SOBI. GD has received grants from Pfizer and honoraria for advice/speaker bureau from Bayer, Biomarin, CSL Behring, Freeline, Novo Nordisk, Roche, Spark Therapeutics, and Takeda. DG has received consulting fees from CSL Behring, Novo Nordisk, Roche, Sanofi, and Takeda. KS has received honoraria and consulting fees from Bayer, Biogen, Novo Nordisk, Octapharma, Pfizer, Roche, and Shire. DP has received honoraria/speaker and consultancy fees from BioMarin, CSL Behring, Novo Nordisk, Roche-Chugai, Sobi, Takeda, and UniQure. JT has received fees as a symposium speaker and advisory board member for Novo Nordisk.
Authors’ Contributions: J. St-Louis, P. Chowdary, G. Dolan, D. Goodyear, K. Strike, D. Pollard, and J. Teitel were the principal investigators who developed the survey and analyzed the data. All authors had full access to data and contributed to drafting of manuscript and approved the final version of the manuscript.
Ethics and Patient Consent: Our institution does not require ethical approval for reporting individual cases or case series. Informed consent for patient information to be published in this article was not obtained because patients were not included in this study. Consent was assumed when participants of the survey confirmed acceptance of an email invitation and agreed to proceed with the survey. All participants signed a consulting agreement and were paid an honorarium for their time.
Data Availability: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Jean St-Louis has served as a consultant for Novo Nordisk, Octapharma, Roche, Sanofi, and Takeda; and receives research funding from Sanofi and Takeda. All relevant disclosures in respect to the authors are listed in the manuscript.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Novo Nordisk A/S
ORCID iD: Jean St-Louis https://orcid.org/0000-0003-1183-533X
Supplemental Material: Supplemental material for this article is available online.
References
- 1.van Vulpen LFD, Holstein K, Martinoli C. Joint disease in haemophilia: pathophysiology, pain and imaging. Haemophilia. 2018;24(Suppl 6):44-49. [DOI] [PubMed] [Google Scholar]
- 2.Srivastava A, Santagostino E, Dougall A, et al. WFH Guidelines for the management of hemophilia, 3rd edition. Haemophilia. 2020. [DOI] [PubMed] [Google Scholar]
- 3.NHS Commissioning Board. NHS Standard Contract for Haemophilia (All Ages). https://www.england.nhs.uk/wp-content/uploads/2013/06/b05-haemophilia.pdf. Accessed April 23, 2020.
- 4.Canadian Hemophilia Standards Group. Canadian Comprehensive Care Standards for Inherited Bleeding Disorders. https://www.hemophilia.ca/wp-content/uploads/2020/06/Canadian-Integrated-and-Comprehensive-Care-Standards-for-Inherited-Bleeding.pdf. Accessed March 10, 2020.
- 5.Martin D, Miller AP, Quesnel-Vallee A, et al. Canada's universal health-care system: achieving its potential. Lancet. 2018;391(10131):1718-1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peckham S. Accountability in the UK healthcare system: an overview. Healthc Policy. 2014;10(Spec issue):154-162. [PMC free article] [PubMed] [Google Scholar]
- 7.Full Fact. What is the NHS? https://fullfact.org/health/what-is-the-nhs/. Accessed April 23, 2020.
- 8.Brand B, Dunn S, Kulkarni R. Challenges in the management of haemophilia on transition from adolescence to adulthood. Eur J Haematol. 2015;95(Suppl 81):30-35. [DOI] [PubMed] [Google Scholar]
- 9.Sun HL, Breakey VR, Straatman L, et al. Outcomes indicators and processes in transitional care in adolescents with haemophilia: a delphi survey of Canadian haemophilia care providers. Haemophilia. 2019;25(2):296-305. [DOI] [PubMed] [Google Scholar]
- 10.Breakey VR, Blanchette VS, Bolton-Maggs PH. Towards comprehensive care in transition for young people with haemophilia. Haemophilia. 2010;16(6):848-857. [DOI] [PubMed] [Google Scholar]
- 11.Escobar MA, Brewer A, Caviglia H, et al. Recommendations on multidisciplinary management of elective surgery in people with haemophilia. Haemophilia. 2018;24(5):693-702. [DOI] [PubMed] [Google Scholar]
- 12.Stephensen D, Bladen M, McLaughlin P. Recent advances in musculoskeletal physiotherapy for haemophilia. Ther Adv Hematol. 2018;9(8):227-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanley J, McKernan A, Creagh MD, et al. Guidelines for the management of acute joint bleeds and chronic synovitis in haemophilia: a United Kingdom haemophilia centre Doctors’ organisation (UKHCDO) guideline. Haemophilia. 2017;23(4):511-520. [DOI] [PubMed] [Google Scholar]
- 14.Stoffman J, Andersson NG, Branchford B, et al. Common themes and challenges in hemophilia care: a multinational perspective. Hematology. 2019;24(1):39-48. [DOI] [PubMed] [Google Scholar]
- 15.Lambert T, Auerswald G, Benson G, et al. Joint disease, the hallmark of haemophilia: what issues and challenges remain despite the development of effective therapies? Thromb Res. 2014;133(6):967-971. [DOI] [PubMed] [Google Scholar]
- 16.Kidder W, Nguyen S, Larios J, et al. Point-of-care musculoskeletal ultrasound is critical for the diagnosis of hemarthroses, inflammation and soft tissue abnormalities in adult patients with painful haemophilic arthropathy. Haemophilia. 2015;21(4):530-537. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cath-10.1177_10760296211070002 for Multidisciplinary Team Care of Patients with Hemophilic Arthropathy: A Qualitative Assessment of Contemporary Practice in the UK and Canada by Jean St-Louis, Pratima Chowdary, Gerry Dolan, Dawn Goodyear, Karen Strike, Debra Pollard and Jerry Teitel in Clinical and Applied Thrombosis/Hemostasis