Abstract
Abstract
Background
The rapid spread of the coronavirus disease 2019 (COVID-19) has created considerable strain on the physical and mental health of healthcare workers around the world. The effects have been acute for physician trainees—a unique group functioning simultaneously as learners and care providers with limited autonomy.
Objective
To investigate the longitudinal effects of physician trainee exposure to patients being tested for COVID-19 on stress, anxiety, depression, and burnout using three surveys conducted during the early phase of the pandemic.
Design
Longitudinal survey study.
Participants
All physician trainees (N = 1375) at an academic medical center.
Main Measure
Assess the relationship between repeated exposure to patients being tested for COVID-19 and stress, anxiety, depression, and burnout.
Key Results
Three hundred eighty-nine trainees completed the baseline survey (28.3%). Of these, 191 and 136 completed the ensuing surveys. Mean stress, anxiety, and burnout decreased by 21% (95% confidence interval (CI): − 28 to − 12%; P < 0.001), 25% (95% CI: − 36 to − 11%; P < 0.001), and 13% (95% CI: − 18 to − 7%; P < 0.001), respectively, per survey. However, for each survey time point, there was mean increase in stress, anxiety, and burnout per additional exposure: stress [24% (95% CI: + 12 to + 38%; P < 0.001)], anxiety [22% (95% CI: + 2 to + 46%; P = 0.026)], and burnout [18% (95% CI: + 10 to + 28%; P < 0.001)]. For depression, the association between exposure was strongest for the third survey, where mean depression scores increased by 33% per additional exposure (95% CI: + 18 to + 50%; P < 0.001).
Conclusions
Training programs should adapt to address the detrimental effects of the “pileup” of distress associated with persistent exposure through adaptive programs that allow flexibility for time off and recovery.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-07350-y.
KEY WORDS: physician trainees, mental health, depression, anxiety, stress, burnout, longitudinal effects
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has dramatically affected the well-being of healthcare workers increasing their occupational burden and mental well-being.1–4 With the protracted effects of the pandemic still lingering, the long-term psychological distress among frontline healthcare workers is a serious concern. These concerns are exacerbated among physician trainees who are at the frontline of patient care, performing the dual responsibilities of learners and patient care providers, albeit with limited autonomy.5–8
Recent research has highlighted considerable distress among physician trainees.9–11 These studies have evaluated specific trainee groups with cross-sectional surveys, and found evidence for a variety of pandemic-related effects on trainees including increased stress and burnout,10,12 concerns regarding safety, implications of their decisions on family,13 challenges of child care, financial challenges,10 and lost educational opportunities10 and its effect on their job prospects.5,14 Studies have described the impact of the pandemic on physician trainees in general surgery,15 ophthalmology,16 otolaryngology,14 cardiothoracic surgery,5 pediatric anesthesia,7 general anesthesia,8 and pediatrics.6
During a 3-month time period at the beginning of the pandemic, we evaluated the longitudinal and cumulative effects of trainee exposure to COVID-19 patients on their stress, anxiety, depression, and burnout outcomes. Such a longitudinal approach can help in elucidating the effects of persistent exposure and devising strategies for mitigating its proximal and longer-term effects.
METHOD
Participants
All physician trainees (residents and clinical fellows; hereafter, “trainees”) (N = 1375) at Washington University School of Medicine, Barnes Jewish Hospital, and St Louis Children’s Hospital were invited via email to complete a series of three voluntary, web-based surveys. Consenting participants provided a unique keyword to longitudinally track their participation. Participants entered the same keyword for each survey, which consisted of the first three letters of their mother’s maiden name, three letters of their city of birth, and their 2-digit birth day. Surveys were sent on April 10, 2020; May 13, 2020; and June 19, 2020, respectively, with a reminder after a week. Participants completing all three surveys were offered to be part of a $50 raffle.
The first survey was sent (April 10, 2020) during the early phase of the pandemic. During this period, there was a shortage of personal protective equipment and suspension of most elective procedures, and the region was under a partial lockdown. By the time of the second survey (May 13, 2020), the number of cases had stabilized, with patient care services being partially transitioned to telemedicine and elective procedures still being suspended. By the third survey (June 19, 2020), the number of tests had markedly increased; however, routine and telemedicine services had restarted along with elective procedures.
Prior to completing the survey, all participants read an “information sheet” with details regarding the survey; by completing the survey, participants provided consent to participate. This study was approved by the institutional review board of Washington University (IRB#202004021).
Surveys
Survey questions included socio-demographic characteristics including race, sex, marital status, occupation of the spouse or partner, training program, clinical role (resident, fellow), and current year in the program. There were questions related to perceived stressors including childcare and home schooling, care of elderly relatives, educational concerns regarding missed opportunities, and financial stressors. These questions followed the format “Currently, how stressed are you about…,” with response choices on a 5-point scale ranging from “not at all” to “extremely” stressed. There were also additional questions related to work-life and work-family balance from the National Institute of Occupational Health and Safety (NIOSH)17 survey.
In addition, the following four mental health and well-being measures were based on validated survey instruments: depression, anxiety, stress, and burnout. Depression, anxiety, and stress were measured using the DASS-21 (Depression Anxiety Stress Scale, short-form),18 a 21-item scale previously used among the general adult population19,20 and among trainees.21DASS-21 has been validated against the Beck Depression Inventory, the Beck Anxiety Inventory, and the State-Trait Anxiety Inventory Trait.22
Burnout was measured using the Stanford Professional Fulfillment Index (PFI). PFI is a 16-item survey combining burnout—based on workload exhaustion and interpersonal disengagement (depersonalization)—and professional fulfillment.(23) The burnout component of the PFI has been shown to be correlated with the Maslach Burnout Inventory (MBI) and the professional fulfillment with “quality of life.”23,24 PFI also has an advantage as the questions are aligned toward capturing recent burnout (i.e., “in the past 2 weeks”).
Exposure
The primary exposure variable was the response to the question in each of the three surveys: “in your current clinical role are you caring for patients currently being tested for COVID-19?” with a response choice of “Yes/No.”
Outcomes
Four outcomes were considered: depression, anxiety, stress, and burnout.
Statistical Analysis
The primary focus was to assess the relationship between repeated exposure and mental health and well-being outcomes. To ensure that we captured individuals actively engaged in care starting at the beginning of the pandemic, only those individuals responding to the first survey were included in this analysis. All participants were then categorized into zero–, single–, and multiple (2 or 3)–exposure groups.
Race was categorized as Caucasian or non-Caucasian, sex was categorized as female or not female, and marital status was categorized as married or not married. Depression, anxiety, and stress were categorized as normal and not normal using the following cutoffs, based on previously published literature20: depression (0–9 normal, 310 not normal), anxiety (0–7 normal, 38 not normal), and stress (0–14 normal, 315 not normal). The average item score for workload and depersonalization scales was calculated; scores ≥ 1.33 were considered as “burned out.”23
To adjust for repeated measurements on individuals in this cohort, all data were analyzed using a generalized estimating equation (GEE) approach assuming a negative binomial distribution (stress, anxiety, depression) or a normal distribution (burnout) with log-link functions. All analyses assumed a compound symmetry correlation structure. All models included reported exposure to patients and survey number (surveys 1, 2, and 3 in April, May, and June). The exposure variable corresponded to the cumulative number of survey responses where a participant reported being exposed to patients being tested for COVID-19 and, thus, varied over time for some individuals, ranging from a minimum of zero to a maximum of three.
For the stress, anxiety, and burnout outcomes, exposure and survey number were treated as ordered explanatory variables in the statistical models. The relationship between depression and exposure was more variable over time; as such, for this outcome, survey number was treated as a categorical variable, whereas exposure was treated as an ordered variable.
Baseline covariates that were found in a prior study10 (based on survey 1) to be associated with exposure to patients being tested for COVID-19 (gender [female or not female], race [Caucasian or non-Caucasian], years in program, marital status [married or not married], and clinical role [fellow or resident]) were considered for inclusion in multivariable models. For all outcomes, a survey number by exposure interaction was tested and retained if the P value was < 0.10. A backward elimination model-selection approach was used to select a final model retaining exposure and survey number variables in all models, and only those baseline covariates that had evidence of an association (P < 0.10) were retained in the final multivariable model. Results are reported as model-adjusted slopes, percentage change in means, or means. All analyses were conducted using SAS, 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Cohort Characteristics
Three hundred eighty-nine (28.3% response) individuals responded to the baseline survey. Of those completing the baseline survey, 191 responded to survey 2 and 136 responded to survey 3. 181 (47%) responded to only the baseline survey, 89 (23%) responded to two of the three surveys, and 119 (31%) responded to all surveys. During the course of the study, the percentage of participants that were never exposed declined from 44% during survey 1 to 17% during survey 3, whereas those that reported exposure in one or more surveys increased from 56% during survey 1 to 83% by the final survey (see Table 1).
Table 1.
Summary of the Number of Participants Reporting Exposure to COVID-19 Testing for All Surveys
| Survey # | Cumulative reported exposures | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | Total | |
| 1 | 172 (44%) | 217 (56%) | NA | NA | 389 |
| 2 | 48 (25%) | 56 (29%) | 87 (46%) | NA | 191 |
| 3 | 23 (17%) | 25 (18%) | 34 (25%) | 54 (40 %) | 136 |
Stress and Anxiety
Results from the negative binomial regression model indicated that the mean stress scores exhibited significant variation both by survey number and by the number of reported exposures.
The model-adjusted slope for survey number indicated that there was a mean stress decrease of 21% (95% confidence interval (CI): − 28 to − 12%; P < 0.001) per survey. In contrast to the negative association between survey number and stress, the cumulative number of reported exposures within a survey indicated a mean increase of 24% (95% CI: + 12 to + 38%; P < 0.001) for each additional exposure. In other words, the group with the highest number of reported exposures during each survey had elevated stress levels (see Fig. 1). Alternatively, those reporting no exposure had the highest stress level during survey 1 (adjusted mean = 8.9), with their mean stress levels declining by over 3 points by the third survey (adjusted mean = 5.6). The interaction between survey and reported exposures was not significant (P = 0.223) indicating that the association between test exposure and stress did not markedly vary over time.
Figure 1.
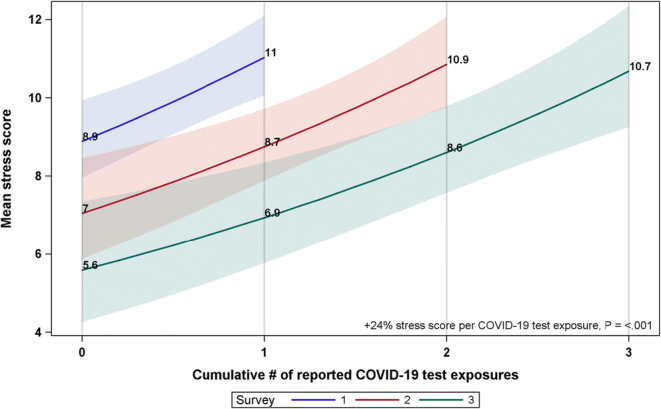
Mean stress score estimates and 95% CIs from negative binomial GEE regression for # of reported exposures to COVID-19 testing stratified by survey number. Estimates are based on parameter estimates for survey number and exposures, adjusted for covariates.
Anxiety scores showed similar patterns. The model-adjusted slope for survey number declined by 25% (95% CI: − 36 to − 11%; P < 0.001) per survey. The cumulative number of reported exposures within a survey indicated a mean increase in anxiety of 22% per additional exposure (95% CI: + 2 to + 46%; P = 0.026) in each of the surveys (see Fig. 2). As with stress, there was not a significant interaction for anxiety score (P = 0.294) suggesting that the association between exposure and anxiety did not change over time.
Figure 2.
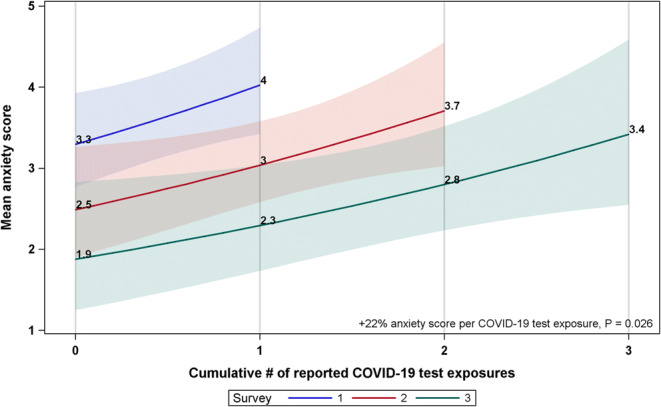
Mean anxiety score estimates and 95% CIs from negative binomial GEE regression for # of reported exposures to COVID-19 testing stratified by survey number. Estimates are based on parameter estimates for survey number and exposures, adjusted for covariates.
Burnout
Mean burnout estimates declined by about 13% per additional survey (95% CI: − 18 to − 7%; P < 0.001). The cumulative number of reported exposures within a survey indicated a mean increase in burnout of 18% per additional exposure (95% CI: + 10 to + 28%; P < 0.001). Within each survey, the highest exposure levels were at or exceeded the 1.33 threshold score for burnout; however, the burnout levels were below the threshold, for all other exposure levels except the highest exposure level (see Fig. 3). As with stress and anxiety, there was not strong evidence for an interaction between survey number and exposure (P = 0.12).
Figure 3.
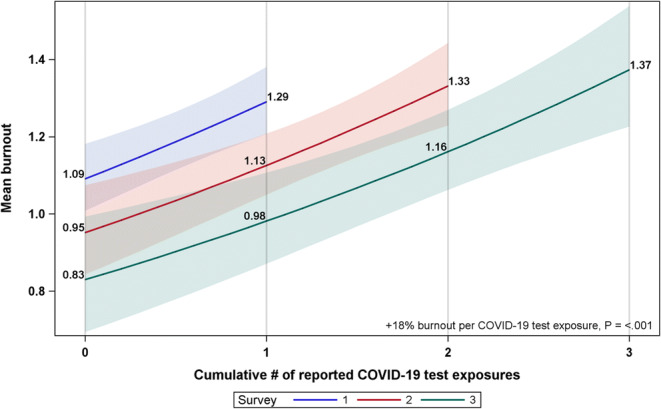
Mean burnout estimates and 95% CIs from negative binomial GEE regression for # of reported exposures to COVID-19 testing stratified by survey number. Estimates are based on parameter estimates for survey number and exposures, adjusted for covariates.
Depression
Depression scores also exhibited evidence of marked differences between the exposure groups. Depression was the only outcome where the exposure by survey interaction effect had a P value less than 0.10 (P = 0.058 in the final multivariable model) the effect of which is illustrated by plots of the model predictions for each survey indicating a small difference between exposure groups during the first survey which increases in magnitude for later surveys (see Fig. 4).
Figure 4.
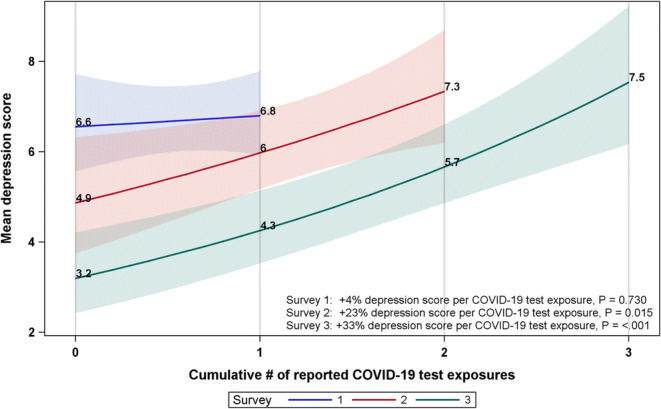
Mean depression score estimates and 95% CIs from negative binomial GEE regression for # of reported exposures to COVID-19 testing stratified by survey number. Estimates are based on parameter estimates for survey number and exposures, adjusted for covariates.
During the first survey, there was no evidence of a significant difference between the exposure groups (mean increase of 4% [95% CI: − 16 to 28%]; P = 0.73); during the second survey, there was a significant association (P = 0.015) indicating that there was a 23% (95% CI: 4 to 45%) increase in the mean depression score per additional reported exposure; the association between exposure and depression was strongest in the third survey where the depression score increased by 33% per additional exposure (95% CI: + 18 to + 50%; P ≤ 0.001).
Although there was variability in the amount of decline over time, all exposure groups exhibited some evidence of decline over the course of the study with a decline of 51% (P < 0.001) between the first and third survey for the zero-exposure group, a decline of 37% (P < 0.001) for the 1-exposure group between surveys 1 and 3, and a 23% (P = 0.003) decline for the 2-exposure group between surveys 2 and 3.
DISCUSSION
Trainees reported the highest levels of stress, anxiety, depression, and burnout during the early phase of the pandemic (March–April 2020), with a marginal decrease across all considered outcomes over time. At each survey time point, the group reporting the highest level of exposure had the worst outcome (stress, anxiety, depression, burnout) compared to groups having fewer exposures. Such a pattern emphasizes the impact of persistent stressors related to exposure on the distress experienced by trainees. In contrast, trainees who were not exposed at all had significant improvements across all considered outcomes over time, further highlighting the detrimental effects for those who were likely at the forefront of pandemic care.
To the best of our knowledge, there are very few studies investigating the longitudinal effects of the pandemic on the mental health and well-being of physicians or trainees in the USA. One longitudinal study, based on surveys among trainees in Singapore, found lower perceived stress and stigma at a second survey time point compared to the first.25 Other longitudinal studies have been with nurses in China26 and in New York27 and found individual differences as predictors for changes in longitudinal stress.
Our findings highlight the considerable immediate, and the potential extended, effects of persistent exposure to COVID-19 patients on the well-being of trainees. Although further research is needed to ascertain the long-term effects of such exposure, our study highlights the distress experienced by trainees. Prior psychological research has shown that daily or repeated stressors produce negative stress responses,28 leading to poor emotional, physical, and clinical outcomes.29,30 For example, persistent exposure to daily stressors is associated with higher negative affectivity,31 leading to greater depression symptoms or major depressive disorder at 2 months32,33 and at 1 year after such episodes.34
More concerningly, such persistent stressors and associated higher affectivity can lead to a recovery paradox35 and “pileup” effects.30 This is because the presence of persistent stressors leads to greater exhaustion,35,36 and consequently a higher need for recovery.37,38 However, greater job-related stressors affect the ability to disassociate from work,39 resulting in poorer recovery activities such as exercise, sleep, and self-care.40,41 This contradictory situation—arising from the greater need for recovery along with low resources and propensity for recovery—is referred to as the recovery paradox.30,35
The case of burnout further demonstrates the considerable downstream effects of the vicious cycle associated with the recovery paradox. Prior research has shown that for people that are chronically burned out, there is an increased perception of greater daily job demands leading to increased exhaustion,42 thereby affecting their ability to recover from burnout. First, the lack of recovery—including lack of appropriate sleep and physical activity42,43—contributes to such a “loss cycle,” where those that are burned out and persistently exposed to stressors are unable to recover. Second, chronic burnout also depletes their ability to utilize available job-related and social support resources44,45 to cope with their challenges, potentially preventing them from “gain cycles” where they can utilize employee-based or other resources to recover. This secondary prevention of gain cycles further exacerbates the challenges faced by those that are persistently burned out, further contributing to a potentially debilitating cycle of burnout.46
With respect to frontline healthcare workers, the contributors to stressors include understaffing for COVID-19 care, increased work responsibilities and hours, increased COVID-19 hospitalizations, lack of available personal protective equipment, fears of getting sick, changing protocols for clinical practice, and moral dilemmas regarding care decisions.47–49 In addition, the short-term distress, arising from persistent exposure, can also potentially impact their clinical decision-making, leading to potential errors50,51 and conflicts in the workplace.35
There are several areas that might be addressed by individual training programs or institutional policies. The impact of prolonged and cumulative COVID-19 related is likely applicable to other periods of higher stress, such as intensive care or emergency department rotations. Training programs could consider adaptations to rotation schedules in order to allow periods of recovery after higher-stress rotations. One recent study demonstrated improvement in resident wellness from building non-clinical time into weekly schedules,52 indicating that even short periods of time away from the clinical environment can be beneficial to attend to personal needs. In response to COVID-19, programs have adapted their “time-off” policies. For example, rather than restricting all time off to blocks of vacation time, programs adapted policies to allow single personal days that can be taken as needed. Providing proactive support such as peer support programs have also been beneficial.53 In the context of the pandemic, programs have mobilized these programs to actively reach out to healthcare workers in the highest stress environments, rather than wait for referrals, raising awareness about well-being more broadly and specifically, on reducing the stigma around help-seeking.
There are several limitations of this study. This was a single academic medical center study, and as such, the associations between the outcomes and potential risk factors should not be interpreted as causal. However, the longitudinal nature of this study provides insights on the short-term and extended impact of COVID-19 on trainee wellness. As previously described, further research is needed to ascertain how such exposures may affect the long-term wellness and well-being of trainees. The response rate for the preliminary survey was ~ 29% and is similar to the surveys that have been conducted with trainees.54 There was no determination of the pre-pandemic levels of the considered outcomes. The reported exposure of participants varied over time, complicating the interpretation of the effects. The exposure variable does not capture the degree of exposure of a trainee; for example, trainees who were exposed once to a patient or on a daily basis were both categorized as being exposed. Additionally, the primary exposure variable was related to exposure to patients being tested for COVID-19. However, we also conducted a secondary analysis to evaluate whether a secondary exposure variable related to exposure to patients who were positive for COVID-19 changed the findings. Results from this analysis indicated a positive association between exposure to patients tested positive to COVID-19 and all outcomes, which is consistent with our main findings. The maximum number of possible exposures varied over time (e.g., for survey 1, maximum was 1; for survey 2, maximum was 2; for survey 3, maximum was 3). It is also likely that the persistently exposed group of trainees were working in the emergency or critical care settings, where the likelihood of exposure to COVID-19 patients was high. However, due to changing rotation schedules for trainees and the timing of the surveys, it was not possible to accurately determine the service location of the participants. Additionally, it is potentially possible that there was a response bias; participants who were distressed or whose pandemic-related workload was heavy may not have participated in the survey (or participated initially and dropped out for future surveys). Conversely, it is also likely that participants who were distressed may have participated more as the topic of the survey was relevant to them. As with most self-selected and voluntary surveys, it is impossible to assess or determine the potential bias in our responses.
The high levels of distress experienced by the persistently exposed group underscores the challenges faced by frontline physician trainees. More importantly, the persistently exposed group, by the third survey time point, had potentially “adjusted” to a new normal—albeit, with high levels of stress, anxiety, and burnout—signifying a potential adaptation to a transformed reality of the new clinical practice environment.
Supplementary Information
(DOCX 25 kb)
Declaration
Conflict of interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang J, et al. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Chinese journal of industrial hygiene and occupational diseases. 2020;38:E001–E001. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 2.Lai J, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3):e203976–e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evanoff BA, et al. Work-Related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. Journal of medical Internet research. 2020;22(8):e21366. doi: 10.2196/21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vanhaecht, K., et al., COVID-19 is having a destructive impact on health-care workers’ mental well-being. International Journal for Quality in Health Care, 2020. [DOI] [PMC free article] [PubMed]
- 5.Caruana, E.J., et al., Impact of Covid-19 on training and wellbeing in subspecialty surgery: a national survey of cardiothoracic trainees in the United Kingdom. The Journal of Thoracic and Cardiovascular Surgery, 2020. [DOI] [PMC free article] [PubMed]
- 6.Sanghavi PB, et al. Effect of the coronavirus disease 2019 (COVID-19) pandemic on pediatric resident well-being. Journal of medical education and curricular development. 2020;7:2382120520947062. doi: 10.1177/2382120520947062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shih, G., et al., The Impact of the COVID-19 Pandemic on the Education and Wellness of US Pediatric Anesthesiology Fellows. Pediatric Anesthesia, 2020. [DOI] [PubMed]
- 8.Sneyd, J.R., et al., The impact of the COVID-19 pandemic on anaesthesia trainees and their training. British journal of anaesthesia, 2020. [DOI] [PMC free article] [PubMed]
- 9.Gallagher, T.H. and A.M. Schleyer, “We Signed Up for This!”—Student and Trainee Responses to the Covid-19 Pandemic. New England Journal of Medicine, 2020. [DOI] [PubMed]
- 10.Kannampallil TG, et al. Exposure to COVID-19 patients increases physician trainee stress and burnout. PloS one. 2020;15(8):e0237301. doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanafelt, T., J. Ripp, and M. Trockel, Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 2020. [DOI] [PubMed]
- 12.Ripp, J., L. Peccoralo, and D. Charney, Attending to the Emotional Well-Being of the Health Care Workforce in a New York City Health System During the COVID-19 Pandemic. Academic Medicine, 2020. [DOI] [PMC free article] [PubMed]
- 13.De Brier N, et al. Factors affecting mental health of health care workers during coronavirus disease outbreaks: a rapid systematic review. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo T, et al. Impact of the COVID-19 pandemic on Otolaryngology trainee education. Head & neck. 2020;42(10):2782–2790. doi: 10.1002/hed.26368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coleman, J.R., et al., COVID-19 Pandemic and the Lived Experience of Surgical Residents, Fellows, and Early-Career Surgeons in the American College of Surgeons. Journal of the American College of Surgeons, 2020. [DOI] [PMC free article] [PubMed]
- 16.Hussain R, et al. Impact of COVID-19 on ophthalmic specialist training in the United Kingdom—the trainees’ perspective. Eye. 2020. p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NIOSH (National Institute of Occupational Safety and Health). Quality of work-life questionnaire. 2016 [cited 2020 May 14]; Available from: https://www.cdc.gov/niosh/topics/stress/qwlquest.html.
- 18.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2005;44(2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 19.Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- 20.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Psychology Foundation of Australia; 1996. [Google Scholar]
- 21.Lam T, et al. Psychological well-being of interns in Hong Kong: What causes them stress and what helps them. Medical teacher. 2010;32(3):e120–e126. doi: 10.3109/01421590903449894. [DOI] [PubMed] [Google Scholar]
- 22.Le MTH, et al. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PloS one. 2017;12(7):e0180557. doi: 10.1371/journal.pone.0180557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trockel M, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Academic Psychiatry. 2018;42(1):11–24. doi: 10.1007/s40596-017-0849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maslach C, et al. Maslach burnout inventory. CA: Consulting psychologists press Palo Alto; 1986. [Google Scholar]
- 25.Chew QH, et al. Perceived Stress, Stigma, Traumatic Stress Levels and Coping Responses amongst Residents in Training across Multiple Specialties during COVID-19Pandemic—A Longitudinal Study. International Journal of Environmental Research and Public Health. 2020;17(18):6572. doi: 10.3390/ijerph17186572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cai Z, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. Journal of psychiatric research. 2020;131:132–137. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirten RP, et al. Factors Associated with Longitudinal Psychological and Physiological Stress in Health Care Workers During the COVID-19 Pandemic. medRxiv; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Almeida DM. Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science. 2005;14(2):64–68. doi: 10.1111/j.0963-7214.2005.00336.x. [DOI] [Google Scholar]
- 29.Almeida DM, et al. The speedometer of life: Stress, health and aging, in Handbook of the psychology of aging. Elsevier; 2011. pp. 191–206. [Google Scholar]
- 30.Smyth JM, et al. Everyday stress response targets in the science of behavior change. Behaviour research and therapy. 2018;101:20–29. doi: 10.1016/j.brat.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhaoyang R, et al. Emotional Responses to Stressors in Everyday Life Predict Long-Term Trajectories of Depressive Symptoms. Annals of Behavioral Medicine. 2020;54(6):402–412. doi: 10.1093/abm/kaz057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Neill SC, et al. Affective reactivity to daily interpersonal stressors as a prospective predictor of depressive symptoms. Journal of Social and Clinical Psychology. 2004;23(2):172–194. doi: 10.1521/jscp.23.2.172.31015. [DOI] [Google Scholar]
- 33.Parrish BP, Cohen LH, Laurenceau J-P. Prospective relationship between negative affective reactivity to daily stress and depressive symptoms. Journal of Social and Clinical Psychology. 2011;30(3):270–296. doi: 10.1521/jscp.2011.30.3.270. [DOI] [Google Scholar]
- 34.Wichers M, et al. Transition from stress sensitivity to a depressive state: longitudinal twin study. The British Journal of Psychiatry. 2009;195(6):498–503. doi: 10.1192/bjp.bp.108.056853. [DOI] [PubMed] [Google Scholar]
- 35.Sonnentag S. The recovery paradox: Portraying the complex interplay between job stressors, lack of recovery, and poor well-being. Research in Organizational Behavior. 2018;38:169–185. doi: 10.1016/j.riob.2018.11.002. [DOI] [Google Scholar]
- 36.Sonnentag S. Dynamics of well-being. 2015. [Google Scholar]
- 37.Siltaloppi M, Kinnunen U, Feldt T. Recovery experiences as moderators between psychosocial work characteristics and occupational well-being. Work & Stress. 2009;23(4):330–348. doi: 10.1080/02678370903415572. [DOI] [Google Scholar]
- 38.Rivkin W, Diestel S, Schmidt K-H. Psychological detachment: A moderator in the relationship of self-control demands and job strain. European Journal of Work and Organizational Psychology. 2015. pp. 376–388. [Google Scholar]
- 39.Wendsche J, Lohmann-Haislah A. A meta-analysis on antecedents and outcomes of detachment from work. Frontiers in psychology. 2017. p. 2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stults-Kolehmainen MA, Bartholomew JB, Sinha R. Chronic psychological stress impairs recovery of muscular function and somatic sensations over a 96-hour period. The Journal of Strength & Conditioning Research. 2014;28(7):2007–2017. doi: 10.1519/JSC.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 41.Litwiller B, et al. The relationship between sleep and work: A meta-analysis. Journal of Applied Psychology. 2017;102(4):682. doi: 10.1037/apl0000169. [DOI] [PubMed] [Google Scholar]
- 42.Simbula S. Daily fluctuations in teachers' well-being: A diary study using the Job Demands–Resources model. Anxiety, Stress, & Coping. 2010;23(5):563–584. doi: 10.1080/10615801003728273. [DOI] [PubMed] [Google Scholar]
- 43.Sonnenschein M, et al. Evidence that impaired sleep recovery may complicate burnout improvement independently of depressive mood. Journal of psychosomatic research. 2007;62(4):487–494. doi: 10.1016/j.jpsychores.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 44.Bakker, A.B. and E. Demerouti, Job demands–resources theory. Wellbeing: A complete reference guide, 2014: p. 1-28.
- 45.Bakker, A.B. and E. Demerouti, The job demands-resources model: State of the art. Journal of managerial psychology, 2007.
- 46.Bakker AB, Costa PL. Chronic job burnout and daily functioning: A theoretical analysis. Burnout Research. 2014;1(3):112–119. doi: 10.1016/j.burn.2014.04.003. [DOI] [Google Scholar]
- 47.Sasangohar, F., et al., Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesthesia and analgesia, 2020. [DOI] [PMC free article] [PubMed]
- 48.Morgantini, L.A., et al., Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PloS one, 2020. 15(9): p. e0238217. [DOI] [PMC free article] [PubMed]
- 49.Mehrotra, P., P. Malani, and P. Yadav. Personal protective equipment shortages during COVID-19—supply chain–related causes and mitigation strategies. in JAMA Health Forum. 2020. American Medical Association. [DOI] [PubMed]
- 50.Tawfik, D.S., et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. in Mayo Clinic Proceedings. 2018. Elsevier. [DOI] [PMC free article] [PubMed]
- 51.Shanafelt TD, et al. Burnout and medical errors among American surgeons. Annals of surgery. 2010;251(6):995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 52.Stevens K, Davey C, Lassig AA. Association of weekly protected nonclinical time with resident physician burnout and well-being. JAMA Otolaryngology–Head & Neck Surgery. 2020;146(2):168–175. doi: 10.1001/jamaoto.2019.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Academic Medicine. 2016;91(9):1200–1204. doi: 10.1097/ACM.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 54.Dyrbye LN, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Academic Medicine. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 25 kb)


