Abstract
Severely hypothermic patients, especially suffering cardiac arrest, require highly specialized treatment. The most common problems affecting the recognition and treatment seem to be awareness, logistics, and proper planning. In severe hypothermia, pathophysiologic changes occur in the cardiovascular system leading to dysrhythmias, decreased cardiac output, decreased central nervous system electrical activity, cold diuresis, and noncardiogenic pulmonary edema. Cardiac arrest, multiple organ dysfunction, and refractory vasoplegia are indicative of profound hypothermia. The aim of these narrative reviews is to describe the peculiar pathophysiology of patients suffering cardiac arrest from accidental hypothermia. We describe the good chances of neurologic recovery in certain circumstances, even in patients presenting with unwitnessed cardiac arrest, asystole, and the absence of bystander cardiopulmonary resuscitation. Guidance on patient selection, prognostication, and treatment, including extracorporeal life support, is given.
Keywords: accidental hypothermia, advanced cardiac life support, cardiac arrest, cardiopulmonary resuscitation, extracorporeal membrane oxygenation, extracorporeal life support, rewarming
Hypothermia is defined as a core temperature below 35°C. In healthy young people, hypothermia does not cause cardiac arrest (CA) as a single reason unless the core temperature is below 30°C. However, in old multimorbid persons, hypothermia may contribute to CA below 32°C.1 Deep accidental hypothermia is a specific cause of CA associated with significant morbidity and mortality.2–4 Accidental hypothermia occurs in previously healthy patients exposed to excessive cold, mainly in hostile, harsh environments,2,5,6 induced by a variety of reasons, for example, cold-water immersion and submersion, avalanche burial, falling into a crevasse, overexertion, or prolonged sojourn in a cold or inadequately heated environment. However, accidental hypothermia is also common in urban areas and temperate zones. In such cases, other factors, commonly including alcohol intoxication, drug overdose, multimorbidities, and mental illness, may be causative.2–4,7,8 Especially in regions where the incidence of hypothermia is low, and the knowledge about the pathophysiology is not widespread, the diagnostic process may be underestimated, the treatment delayed and not in compliance with the guidelines.1,3,9,10
The outcome in normothermic unwitnessed out-of-hospital cardiac arrest (OHCA) is poor.11 Several terminations of resuscitation (TOR) rules suggest that after 20 minutes of resuscitation attempts in unwitnessed OHCA without bystander cardiopulmonary resuscitation (CPR), CPR may be terminated if no vital signs were detected and no shockable rhythm was found.12–15 Recommendations for extracorporeal CPR (ECPR) include only selected OHCA patients to sustain perfusion while percutaneous coronary intervention can be performed.16,17 The ECPR protocols include a set of criteria such as witnessed CA, immediate bystander CPR, short no-flow and low-flow time before ECPR, and a shockable rhythm.17,18 While the predictive value of TOR-rules in normothermic CA patients is high and withholding ECPR in these circumstances is sound, current ECPR guidelines do not apply in patients suffering CA from potentially reversible causes such as accidental hypothermia.7,17,19,20
Medical teams are faced with limited up-to-date triage and extracorporeal cardiac life support (ECLS) rewarming algorithms.21–23 It must be emphasized that if the patient is diagnosed and treated properly, an excellent neurologic outcome is often possible even after long-lasting hypothermic cardiac arrest.24 Although the advantage of ECLS over other ways of rewarming in severe hypothermia has been proven,25 it is still not implemented uniformly.7 Based on our experience, we believe that guidance should be provided for ECLS centers covering the eligibility, rewarming, and cardio-pulmonary stabilization of severely hypothermic patients. We would like to provide a concise, practical, and up-to-date recommendation focused on an optimal approach to perform triage and rewarm patients with cardiac arrest in severe accidental hypothermia at an ECLS center.
Pathophysiology
The human body cools gradually and with every fall in 1°C of the core temperature, brain oxygen requirements diminish 6–7%.26 Thus, at 32°C hypothermic CA may be survivable for 10 minutes instead of 5 minutes in normothermia. This results in a metabolism of ~24% and ~16% at 18°C and 15°C, respectively, compared with that at normothermia.26,27 This phenomenon is well known and used commonly during cardiac surgery procedures, where deep hypothermic circulatory arrest is needed, for example, for aortic repair in acute aortic syndromes.28 In contrast, in normothermia, CA lasting for five or more minutes will result in severe brain damage or death.
Hypothermia diminishes vital function long before CA. Cooling will lead to an irritable myocardium, while arrhythmias will ensue below 35°C. Below 32°C, the elderly and multimorbid are at risk of hypothermic CA, while young, healthy people may suffer CA below 30°C.25,29–31 Few still have minimal vital signs below 24°C.25,29–31 The first presenting rhythm may be asystole in 30% of cases.30 Several parameters defined as exclusion criteria for ECPR in normothermic CA are not valid in hypothermic CA (Table 1).32–36 Essential differences between normothermic and hypothermic CA are outlined by Gordon et al.37 In severe hypothermia, end-tidal carbon dioxide (etCO2) is low due to a decreased metabolic rate while a correlation with the partial pressure of carbon dioxide in arterial blood (PaCO2) is lacking. Therefore, etCO2 can neither be used to assess blood flow and not the quality of CPR38 as in normothermic cardiac arrest.39–41 Many hypothermic CA patients suffer from an unwitnessed CA.
Table 1.
| Cardiac Arrest | Normothermic | Hypothermic |
|---|---|---|
| Temperature | >35°C | In healthy adults <30°C (in elderly <32°C) |
| Unwitnessed arrest | Usually, a contraindication for ECPR | Not a contraindication for ECLS Not an independent predictor for survival Not independently associated with worse outcome |
| Initial rhythm | Shockable | Not an independent predictor for survival Asystole not independently associated with worse outcome |
| No flow time | Especially important | Usually unknown, less important |
| Time to cannulation for ECPR | Usually less than 60 minutes | Usually longer than 60 minutes |
| Neurologic outcome in survivors | Variable | Full recovery likelier than in normothermia |
ECLS, extracorporeal cardiac life support; ECPR, extracorporeal cardiopulmonary resuscitation.
Hypothermic patients with asystole may be rewarmed with ECLS until the irritated myocardium resumes electrical activity (usually around 28–30°C), with shockable rhythm defibrillation being required to achieve the return of spontaneous circulations (ROSC). After ROSC, patients often develop multiple organ failure, with cardiac and respiratory failure as a prominent feature requiring advanced organ support such as ECLS.42 This strategy enables recovery while the pulmonary and cardiac functions are being supported.43
Outcomes of Hypothermic CA After ECLS Rewarming
Although CA is likely to occur below 28°C, circulation may even persist below 24°C. Below 20°C, isoelectric ECG and EEG are likely but do not exclude successful ECLS rewarming. The lowest recorded temperature with neurologically intact survival following ECLS rewarming from accidental hypothermia in a pediatric survivor is 11.8°C, while the lowest in an adult survivor is 13.7°C.44,45 The lowest core temperature with neurologically intact survival from induced hypothermia was 4.0°C.46 The threshold of survival for core temperature has not yet been established.
For patients presenting to hospital with hypothermic CA and supported with ECLS, overall survival rates to hospital discharge between 20% and 100% are reported.3 Most notably 61–100% of survivors were neurologically classified as cerebral performance category 1–2.33,35,43,47,48 Respective survival rates are lower for avalanche victims (from 0% to 17%)49 and drowning patients (from 10% to 42%).3,50–54
Apart from the protective effect of hypothermia itself, established protocols of treatment and novel rewarming techniques may influence the outcome.36,55–57 The coordination of the rescue procedures, immediate high-quality CPR (preferably using a mechanical chest compression system), recognition of hypothermia and veno-arterial (VA) ECLS cannulation for rewarming and cardiorespiratory support are crucial for achieving satisfactory survival rates34,55,58–62 and full neurologic recovery.30,61
The Hypothermia Outcome Prediction After ECLS (HOPE) Score
The survival probabilities of in-patients can be determined according to the HOPE score.33
The HOPE score33 allows to perform an in-hospital prediction of the probability of survival after ECLS rewarming in a cardiac arrest patient with accidental hypothermia. The HOPE score is based on six covariates available at hospital admission (Table 2).36 The HOPE score has been externally validated with a cutoff of 10%.35 It showed good calibration as well as excellent discrimination (area under the receiver operating characteristic curve of 0.825) between patients who will survive from those who will die after ECLS rewarming.35 The negative predictive value (defined as the proportion of patients who died among those with a HOPE score <10%) was 97%.33,35
Table 2.
Hypothermia Outcome Prediction after ECLS (HOPE) Score
| HOPE score covariates at hospital admission |
|---|
| - Age - Sex - Core temperature - Serum potassium - Presence of asphyxia (submersion with the head fully covered by water or snow avalanche accident AND in cardiac arrest at extrication) - Duration of cardiopulmonary resuscitation (CPR); since CPR initiation until ECLS cannulation |
An online calculator of the HOPE score is available at: www.hypothermiascore.org
CPR, cardiopulmonary resuscitation; ECLS, extracorporeal cardiac life support.
Problems and Pitfalls in Patient Selection and Qualification for ECLS
There are several problems and pitfalls in qualification for ECLS rewarming and which are notably different from those ECPR for CA in normothermic patients.63
ECLS rewarming is indicated in accidental hypothermic cardiac arrest with a potential for reversibility.21,30,50,61,64–67 Since hypothermic cardiac arrest is a rare medical emergency, EMS as well ED teams may be not familiar with its management. This can lead to fatal mistakes regarding the qualification of a patient for ECLS rewarming and finally patient’s death.68
Since the core temperature measurement is usually unavailable in prehospital settings, all details of patient’s history and clinical signs should be carefully analyzed. A cold trunk, a history of cooling that preceded CA, and the absence of fatal injuries suggest accidental hypothermia cardiac arrest (AHCA).69 Such patients should be transported directly from the scene to an ECLS center to shorten the low-flow time.70
Key instructions may help to identify accidental hypothermia cases and initiate appropriate and adequate treatment. Local protocols in ECLS centers seem to be an ideal way to improve the quality of the initial treatment of hypothermic arrested patients.70 ECLS teams may support emergency teams, being aware of several limitations in equipment and skills in the out-of-hospital setting.
The complete absence of signs of life does not permit clinicians to declare an arrested hypothermic patient dead unless there is an associated fatal illness, fatal traumatic injury, or prolonged asphyxia. Fixed and dilated pupils, pallor, rigor mortis, and nonfixed dependent lividity alone are not reliable signs of death in the arrested severely hypothermic patient. The guiding principle is “no one is dead until they are warm and dead.”
However, the patient can be declared dead if the chest compressions are impossible to perform due to tissue freezing.71
Besides the history of the patient, two important procedures have to be performed simultaneously at hospital admission: the measurement of the core (usually esophageal) temperature to diagnose or confirm significant hypothermia and blood sampling for blood gas analysis including potassium, which is one of the six variables used to calculate the HOPE survival probabilities to select patients for ECLS rewarming.33
Indications for ECLS Rewarming
ECLS rewarming is indicated in AHCA with a mechanism/history compatible with AHCA
AND
HOPE survival probabilities of ≥10% (in adults*)
*Because children may have potentially higher chances of survival as well as a longer life expectancy if they survive, clinicians should exercise caution when using the HOPE survival probabilities with the proposed threshold of 10% to predict children’s outcomes.
An online calculator of the HOPE score is available at: www.hypothermiascore.org (Table 2).
ECLS rewarming should be carefully considered in the following circumstances due to low rates of survival and the high likelihood of major morbidity72,73:
- Core temperature >30°C (consider other factors).30 CA that is solely caused by hypothermia does not occur in patients with a body temperature >30°C.
- Major trauma (Table 3)
- Futile comorbidities
- Chest compressions impossible due to tissue freezing
Table 3.
Problems and Pitfalls in Qualification for ECLS Rewarming
| The clinical factors usually considered as contraindications for ECPR in normothermic CA (asystole, unwitnessed CA, unknown no-flow duration, prolonged CPR duration, advanced age) ARE NOT a contraindication for ECLS rewarming in AHCA patients |
| Blood sampling should avoid hemolysis, and minimize trauma to femoral vessels |
| Inclusion criteria for ECLS rewarming should not be based on a single potassium level. Extreme serum potassium levels are possible. A second blood sample obtained at a different site and verifying measurement may be reasonable |
| If some variables of the HOPE score are not clear (e.g., the presence or absence of asphyxia), taking into account the variable that will lead to the highest survival probabilities when calculating the HOPE score will offer the best chances of survival to the patient |
| Concomitant trauma, especially traumatic brain injury is not an absolute contraindication for ECLS rewarming. Anticoagulation free ECLS run is possible74 |
AHCA, accidental hypothermia cardiac arrest; CPR, cardiopulmonary resuscitation; ECLS, extracorporeal cardiac life support.
In such cases, the decision should be based on a multidisciplinary approach, which should also integrate the value of the HOPE survival probabilities.
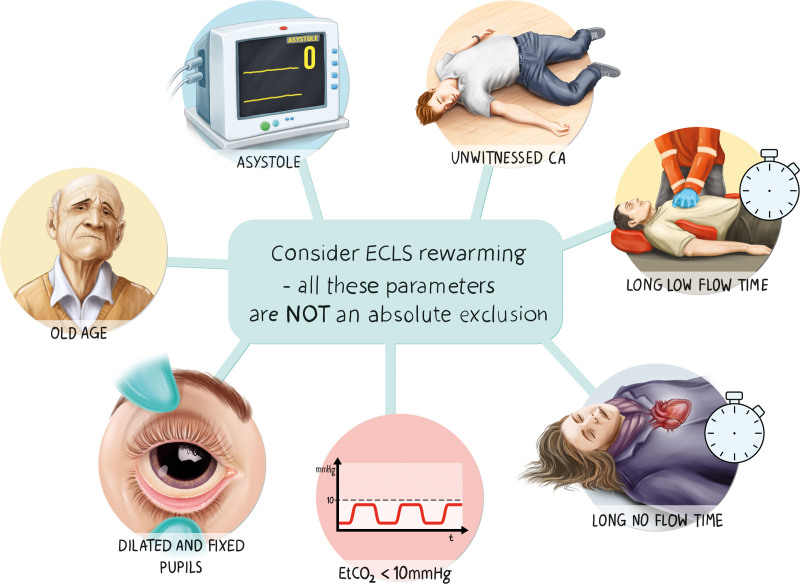
The following parameters considered as exclusion criteria for ECPR in normothermic patients17 DO NOT contraindicate ECLS rewarming (Table 1, Figure 1):
Figure 1.
The following parameters are considered as exclusion criteria for ECPR in normothermic patients. In arrested hypothermic patients, these parameters are not absolute exclusion criteria for ECLS rewarming.
- Asystole
- Unwitnessed CA
- The absolute value of the low-flow duration, provided rewarming with external and alternative internal rewarming if transport to ECLS/CPB is not available within 6 hours (survival with good neurologic outcome has been described with low flow up to 6 hours)75
- The absolute value of the no-flow duration (survival with good neurologic outcome has been described with no flow >1 hour)76
- Elderly77
- Fixed and dilated pupils
End-tidal carbon dioxide (etCO2) <10 mm Hg
Contraindications for ECLS Rewarming
No absolute contraindications for ECLS rewarming in AHCA exist (Figure 1). However, the complications listed in the ELSO General Guideline for all ECLS cases are applicable and balancing the risks versus the potential benefits of the extracorporeal procedure is important, notably in elderly people.17,78
Education of health care professionals in ED and ICU of participating institutions as well as efficient logistic coordination are mandatory for the successful treatment of hypothermic patients.79 As most countries designate specialized centers dedicated to hypothermia treatment using extracorporeal techniques, EMS providers transport potential candidates to these centers.6,10,58,59,61,79
Practical Information on the Management of Patient During ECLS Rewarming
ECLS Mode
Both cardiopulmonary bypass (CPB) and ECLS may be used to provide blood circulation, oxygenation, and warming to hypothermic cardiac arrest patients. ECLS is considered the preferred method due to its lower anticoagulation requirements than CPB and its potential to prolong circulatory support.20 Some patients who have sustained hypothermic cardiac arrest may require this support for several days due to temporary heart failure.42 In hypothermic CA, the VA ECLS mode is preferred.80,81
Initial Patient Management at ECLS Center Before ECLS Cannulation
Continue chest compressions with the best achievable level until sufficient ECLS flow is achieved. Chest compressions can then be terminated.17 In deeply hypothermic patients’ coagulation is impaired, and the risk of blood stasis-related thrombi is negligible (Figure 2).
etCO2 is low due to decreased metabolic rate and cannot be used to assess the quality of CPR.
Core temperature assessment (see also Rewarming Goals)
Blood samples should be obtained with ultrasound-guided puncture or open puncture of the femoral vessels. Cardiopulmonary resuscitation (CPR) may be temporarily stopped.
Final decision to be made by HOPE score calculation (see also Hypothermia Outcome Prediction after ECLS - HOPE score) (Table 2)
Figure 2.
Initial management in accidental hypothermia-related cardiac arrest before ECLS cannulation.
Cannulation
ECLS cannulation in hypothermia-related CA may be challenging due to coagulopathy and a risk of bleeding. It is recommended to choose the method the person who will cannulate the patient is most used to:
-
(1)
the cut-down technique, preferred due to center-specific protocol or in vessels difficult to identify by ultrasound guidance
-
(2)
percutaneously by a vessel puncture, guidewire placement, and dilation (Seldinger technique). Ultrasound guidance82,83 or fluoroscopy is recommended
-
(3)
a combination of the cut-down and Seldinger techniques
-
(4)
by direct cannulation of the right atrium and aorta (children less than 15 kg or in case of unsuccessful peripheral cannulation) for CPB or ECLS
In cases of percutaneous cannulation, the following cannulas may be used: arterial 15–19 French, venous (drainage) 19–25 French. An ultrasound of the vessels, especially arteries, is recommended.82,83 Cannulation-related vessel injury may include unintentional puncture of unidentified vessels, saphenous-femoral junction cannulation, and transfixation of the inguinal ligament during cannulation. Femoral arterial cannulation may be associated with inadequate distal perfusion. A separate retrograde perfusion line (6–8 French) can be introduced in the distal superficial femoral artery by the direct cutdown or Seldinger techniques. Interruptions in chest compression may be aligned at key points of cannulation.
In patients with no contraindications for anticoagulation, unfractionated heparin is given as a bolus (50–100 units per kilogram) at the time of cannulation and by continuous infusion during ECLS.17,78,84 An activated clotting time (ACT) targeted at 150–200 seconds is recommended. In some centers, systemic anticoagulation is waived within the first 24 hours due to hypothermia-related coagulopathy.
Specific Problems and Pitfalls of Cannulation
-
•
Vascular access for ECLS cannulation has the highest priority. Venous and arterial lines for drug administration and monitoring are deemed inferior.
-
•
Repeated attempts to provide blood sampling from femoral vessels may result in hemorrhage and emerged hematoma that aggravate difficult anatomical conditions for vascular access for ECLS
-
•
There is a variability in potassium values between blood sampling sites.85 Central venous blood has been proposed as the preferred site for potassium sampling. It is crucial to avoid iatrogenic trauma to the femoral vessels. Blood samples should be obtained with an ultrasound-guided puncture or open puncture of the femoral vessels. Cardiopulmonary resuscitation (CPR) may be temporarily stopped. Hyperkalemia in deep hypothermia is a sign of a poor prognosis and may disqualify a patient from ECLS rewarming. Thus, it is essential to avoid hemolysis-induced pseudo-hyperkalemia.85 If a patient would not qualify for ECLS rewarming according to the first potassium measurement, a second blood sample may be obtained at a different site to verify the potassium level.
-
•
Inappropriate provision of external rewarming methods during prehospital rescue may result in possible skin damage and even burns. Heat pads placed in the groins increase the risk of difficult vascular access to the femoral vessels.
-
•
Determination of the body position before the rescue and tissue damage to the extremities
-
•
Hypothermia increases blood echogenicity. Very slow flow of hyperechogenic blood in the heart cavities may mimic thrombus formations.
-
•
Factors including alcohol intoxication, drug overdose, and mental illness may cause hypothermia commonly in urban areas. Patients coming from poor social conditions are at risk for hygiene neglect and infectious diseases. This makes them more vulnerable and puts them at risk for infectious complication on ECLS rewarming. Precautionary procedures and high-aseptic standards during cannulation are mandatory.
Circuit Management and Patient Monitoring
Blood flow.
Once cannulation is achieved, blood flow during rewarming is controlled as recommended in the ELSO Guidelines,17,84 usually 2.2–2.4 L/min/m2 to provide adequate blood flow for optimal perfusion of the brain and other end organs.17,84 Blood flow ensures sufficient tissue perfusion targeted by SvO2 >70%. In hypothermia, due to reduced oxygen demand SvO2 may be decided elevated. During the rewarming process, hypothermic patients suffer refractory hypotension due to vasoplegia and fluid shift. This condition may obstacle the adequate blood flow. Fluid resuscitation with isotonic crystalloid and vasopressors are first line of treatment to maintain a mean systemic pressure between 50 and 70 mm Hg and to ensure cerebral perfusion.
Fluids resuscitation.
Patients with hypothermia frequently become disproportionately hypotensive during rewarming from severe dehydration and fluid shifts. High-volume fluid resuscitation with isotonic crystalloid is the first line of treatment. Fluids may be delivered via ECLS tubing in the absence of adequate vascular access.
Ventilation.
Lung function may be deteriorated due to hypothermia, pulmonary vasoconstriction, low perfusion, or no-flow time. Ventilator settings should aim to allow lung protection. During rewarming, massive endothelial damage and lung edema may occur. An initial ventilator setting of FiO2 1.0 may be required, adjusted to the lowest possible FiO2 to avoid the risk of hyperoxia and additional alveolar damage.
Arterial blood gas analysis.
Arterial blood gas analysis according to the alpha-stat-regulation should be repeated. Hypoglycemia, severe acid-base imbalance, and other problems requiring symptom-related treatment may occur.
Cardiac rhythm.
Hypothermic ventricular fibrillation is resistant to pharmacotherapy and defibrillation. Defibrillation delivered in a patient with core temperature below 30°C may be successful if ECLS provides an adequate blood flow and stable rate of rewarming.
Internal cardiac pacing may be considered if bradycardia persists with cardiac instability after normothermia is achieved.
Sedation.
Sedation and analgesia are required to avoid uncontrolled waking up, moving about or coughing. A score of –5 on the Richmond Agitation-Sedation Scale 5 is aimed. Sedation may be reduced and discontinued if normothermia, stable hemodynamic and pulmonary function are achieved.
Neurologic prognostication.
Neurologic exams should be performed once sedation is discontinued. Collaboration with a neurologist is recommended.
Infection.
Asepsis in the operative field during cannulation is a prerequisite to prevent bloodstream infections. Adherence to local protocols of antibiotic prophylaxis to prevent surgical site infection is recommended. Antibiotics are indicated according to further signs of infection.
Rewarming goals.
The optimal targets of rewarming are still unknown.3 A slow rewarming rate has an independent association with survival with good neurologic outcomes in hypothermic cardiac arrest.24 This is consistent with existing evidence and cardiac surgery guidelines suggesting that better neurologic outcome is inversely related to the rewarming rate.86–88 It is postulated that this may be due to a cerebral temperature overshoot that can occur when larger temperature gradients are required by a more rapid ECLS rewarming.
However, the ideal rate of rewarming of hypothermic ECLS patients remains unknown. The maintenance of the core temperature may be cautiously monitored by temperature measurements at several sites, such as the nasopharynx, pulmonary artery, carotid bubble, esophagus, urinary bladder, rectum, and tympanic membrane as well as the venous inflow and arterial outlet.87 However, no single site for measurement and monitoring can be recommended. We do not exactly know how much difference there is between the body compartments during rewarming or how well the temperature of respective sites reflects the brain temperature. A common method of measuring core temperature in patients with hypothermic cardiac arrest is esophageal measurement.
The target position of the tip of the probe is the lower third of the esophagus. The esophageal temperature may not correspond to the core temperature, particularly when high gradients are applied (i.e., high-water bath settings). This may be due to a warmblood outflow in the vicinity of the tip of the esophageal probe.
Therefore, the core temperature should be monitored in at least two sites simultaneously. A temperature gradient between the heat exchanger (water bath) and the core temperature is typically used to monitor the rewarming rate. Continuous oxygenator arterial outlet temperature monitoring is recommended, as well as maintaining a temperature gradient between the venous inflow and arterial outlet of ≤4°C.87 A maximum gradient between the arterial outlet and venous inflow of 10°C should not be exceeded. Failure to comply with these rules may cause serious neurologic complications and hemolysis of blood cells.87
The target rewarming rate during ECLS in accidental hypothermia should be ≤5°C/h.89
It is recommended to start rewarming in 5–10 minutes time intervals after cannulation to ensure the accurate functioning of all devices. The heat exchanger should be set at a maximum of 37°C to prevent cerebral overheating. After ROSC, strict normothermia (35–36°C) is recommended during the first 24 hours. Faster rewarming rates of about 4–5°C per hours until the heart rhythm returns may be recommended, followed by slower rewarming of about 1–2°C per hour.
Weaning.
Weaning may be delayed due to common complications, such as aspiration pneumonia and postresuscitation chest trauma. Normothermia, along with stabilized metabolic, hemodynamic, and pulmonary function, are the requirements for ECLS liberation and decannulation. Repetitive echocardiography is recommended to assess native cardiac output, left ventricular ejection, aortic valve opening, and to exclude major valvular pathologies.17,84 With evidence of improved left ventricular ejection fraction from echocardiography, inotropes, and blood flow may be reduced to 50%, then to 25% of adequate cardiac output.17,84
Medical record.
Data in hypothermic CA patients may be collected according to a checklist template (Figure 3). Required data include out-of-hospital and in-hospital data, namely general and specific data of the patient, the mechanism leading to hypothermic CA, their present condition including core temperature, ECG, mode and duration of CPR, and blood sampling results. These data are used to calculate the probability of survival according to the HOPE score. ECLS rewarming is recommended with HOPE survival probabilities of ≥10%*.33,35,36
Figure 3.
Medical record template for patients suffering accidental hypothermia related cardiac arrest. Data of hypothermic CA patients may be collected according to this checklist template. These data are essential to allow a decision to be made whether the patient qualifies for ECPR. Required data include out-of-hospital and in-hospital data, namely: general and specific data of the patient, the mechanism leading to hypothermic CA, their present condition including core temperature, ECG, mode and duration of CPR and blood sampling results. These data are used to calculate the probability of survival according to the HOPE score. With a HOPE score of ≥ 10 ECPR is recommended.33,35
Practice Points to Remember
-
•
Accidental hypothermia seems to be underdiagnosed and undertreated, especially in those regions where its incidence is a rare condition, while the most common problem affecting the recognition and treatment of hypothermia seems to be logistics and proper planning.
-
•
Since the core temperature measurement is usually unavailable in prehospital settings, all details of patient’s history and clinical signs should be carefully analyzed. Patients with deep hypothermic cardiac arrest should be transported directly from the scene to an ECLS center.
-
•
The Hypothermia Outcome Prediction after ECLS (HOPE) score is recommended for the final qualification for extracorporeal rewarming. A single measurement of the potassium level is not an exclusion criterion for ECLS rewarming.
-
•
VA ECLS enables rewarming and cardiopulmonary stabilization of severely hypothermic patients.
-
•
A favorable neurologic outcome is possible even in prolonged, unwitnessed cardiac arrest related to accidental hypothermia if the patient is diagnosed and treated properly.
-
•
A medical record card (Figure 3) is recommended to collect the data of hypothermic CA patients.
ACKNOWLEDGMENT
The authors thank the Department of Innovation, Research, University and Museums of the Autonomous Province of Bozen/Bolzano for covering the Open Access publication costs.
Footnotes
The authors have no funding and conflicts of interest to report.
Justyna Swol and Tomasz Darocha have equal contribution to this work.
Contributor Information
Tomasz Darocha, Email: tomekdarocha@wp.pl.
Peter Paal, Email: peter.eckman@allina.com.
Hermann Brugger, Email: hermann.brugger@eurac.edu.
Paweł Podsiadło, Email: p.podsiadlo.01@gmail.com.
Sylweriusz Kosiński, Email: kosa@mp.pl.
Mateusz Puślecki, Email: mateuszpuslecki@o2.pl.
Marcin Ligowski, Email: mligowski@icloud.com.
Mathieu Pasquier, Email: mathieu.pasquier@chuv.ch.
References
- 1.Lott C, Alfonzo A, Barelli A, et al. : European resuscitation council guidelines for cardiac arrest in special circumstances 2020. Resuscitation 2021.161: 152–219 [DOI] [PubMed] [Google Scholar]
- 2.Brown DJ, Brugger H, Boyd J, Paal P: Accidental hypothermia. N Engl J Med 2012.367: 1930–1938 [DOI] [PubMed] [Google Scholar]
- 3.Paal P, Gordon L, Strapazzon G, et al. : Accidental hypothermia-an update: The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand J Trauma Resusc Emerg Med 2016.24: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meiman J, Anderson H, Tomasallo C: Centers for disease C, prevention: Hypothermia-related deaths--Wisconsin, 2014, and United States, 2003-2013. MMWR Morb Mortal Wkly Rep 2015.64: 141–143 [PMC free article] [PubMed] [Google Scholar]
- 5.Podsiadło P, Darocha T, Kosiński S, et al. : Severe hypothermia management in mountain rescue: A Survey Study. High Alt Med Biol 2017.18: 411–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wanscher M, Agersnap L, Ravn J, et al. : Outcome of accidental hypothermia with or without circulatory arrest: Experience from the Danish Præstø Fjord boating accident. Resuscitation 2012.83: 1078–1084 [DOI] [PubMed] [Google Scholar]
- 7.Gordon L, Ellerton JA, Paal P, Peek GJ, Barker J: Severe accidental hypothermia. BMJ 2014.348: g1675. [DOI] [PubMed] [Google Scholar]
- 8.Corneli HM: Accidental hypothermia. Pediatr Emerg Care 2012.28: 475–80; quiz 481 [DOI] [PubMed] [Google Scholar]
- 9.Darocha T, Jarosz A, Ziętkiewicz M, et al. : ECMO in treating patients in critical, life-threatening medical condition brought on by severe hypothermia-criterion standard. Ann Emerg Med 2016.67: 558–559 [DOI] [PubMed] [Google Scholar]
- 10.Kosiński S, Darocha T, Gałązkowski R, Drwiła R: Accidental hypothermia in Poland – estimation of prevalence, diagnostic methods and treatment. Scand J Trauma Resusc Emerg Med 2015.23: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sasson C, Rogers MAM, Dahl J, Kellermann AL: Predictors of survival from out-of-hospital cardiac arrest. Circ Cardiovas Qual Outcomes 2010.3: 63–81 [DOI] [PubMed] [Google Scholar]
- 12.Hreinsson JP, Thorvaldsson AP, Magnusson V, Fridriksson BT, Libungan BG, Karason S: Identifying out-of-hospital cardiac arrest patients with no chance of survival: An independent validation of prediction rules. Resuscitation 2020.146: 19–25 [DOI] [PubMed] [Google Scholar]
- 13.Morrison LJ, Verbeek PR, Vermeulen MJ, et al. : Derivation and evaluation of a termination of resuscitation clinical prediction rule for advanced life support providers. Resuscitation 2007.74: 266–275 [DOI] [PubMed] [Google Scholar]
- 14.Morrison LJ: Prehospital termination of resuscitation rule. Curr Opin Crit Care 2019.25: 199–203 [DOI] [PubMed] [Google Scholar]
- 15.Goto Y, Maeda T, Goto YN: Termination-of-resuscitation rule for emergency department physicians treating out-of-hospital cardiac arrest patients: An observational cohort study. Crit Care 2013.17: R235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holmberg MJ, Geri G, Wiberg S, et al. ; International Liaison Committee on Resuscitation’s (ILCOR) Advanced Life Support and Pediatric Task Forces: Extracorporeal cardiopulmonary resuscitation for cardiac arrest: A systematic review. Resuscitation 2018.131: 91–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richardson ASC, Tonna JE, Nanjayya V, et al. : Extracorporeal cardiopulmonary resuscitation in adults. Interim guideline consensus statement from the extracorporeal life support organization. ASAIO J 2021.67: 221–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yannopoulos D, Bartos JA, Aufderheide TP, et al. ; American Heart Association Emergency Cardiovascular Care Committee: The evolving role of the cardiac catheterization laboratory in the management of patients with out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation 2019.139: e530–e552 [DOI] [PubMed] [Google Scholar]
- 19.Bossaert LL, Perkins GD, Askitopoulou H, et al. ; ethics of resuscitation and end-of-life decisions section Collaborators: European resuscitation council guidelines for resuscitation 2015: section 11. The ethics of resuscitation and end-of-life decisions. Resuscitation 2015.95: 302–311 [DOI] [PubMed] [Google Scholar]
- 20.Truhlář A, Deakin CD, Soar J, et al. ; Cardiac arrest in special circumstances section Collaborators: European resuscitation council guidelines for resuscitation 2015: section 4. Cardiac arrest in special circumstances. Resuscitation 2015.95: 148–201 [DOI] [PubMed] [Google Scholar]
- 21.Lavonas EJ, Drennan IR, Gabrielli A, et al. : Part 10: special circumstances of resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015.132(18 suppl 2): S501–S518 [DOI] [PubMed] [Google Scholar]
- 22.Haas NL, Coute RA, Hsu CH, Cranford JA, Neumar RW: Descriptive analysis of extracorporeal cardiopulmonary resuscitation following out-of-hospital cardiac arrest-An ELSO registry study. Resuscitation 2017.119: 56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dow J, Giesbrecht GG, Danzl DF, et al. : Wilderness medical society clinical practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia: 2019 update. Wilderness Environ Med 2019.30: S47–S69 [DOI] [PubMed] [Google Scholar]
- 24.Saczkowski RS, Brown DJA, Abu-Laban RB, Fradet G, Schulze CJ, Kuzak ND: Prediction and risk stratification of survival in accidental hypothermia requiring extracorporeal life support: An individual patient data meta-analysis. Resuscitation 2018.127: 51–57 [DOI] [PubMed] [Google Scholar]
- 25.Morita S, Inokuchi S, Yamagiwa T, et al. : Efficacy of portable and percutaneous cardiopulmonary bypass rewarming versus that of conventional internal rewarming for patients with accidental deep hypothermia. Crit Care Med 2011.39: 1064–1068 [DOI] [PubMed] [Google Scholar]
- 26.Ehrlich MP, McCullough JN, Zhang N, et al. : Effect of hypothermia on cerebral blood flow and metabolism in the pig. Ann Thorac Surg 2002.73: 191–197 [DOI] [PubMed] [Google Scholar]
- 27.McCullough JN, Zhang N, Reich DL, et al. : Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann Thorac Surg 1999.67: 1895–9; discussion 1919 [DOI] [PubMed] [Google Scholar]
- 28.Leshnower BG, Rangaraju S, Allen JW, Stringer AY, Gleason TG, Chen EP: Deep hypothermia with retrograde cerebral perfusion versus moderate hypothermia with antegrade cerebral perfusion for arch surgery. Ann Thorac Surg 2019.107: 1104–1110 [DOI] [PubMed] [Google Scholar]
- 29.Danzl DF, Pozos RS, Auerbach PS, et al. : Multicenter hypothermia survey. Ann Emerg Med 1987.16: 1042–1055 [DOI] [PubMed] [Google Scholar]
- 30.Frei C, Darocha T, Debaty G, et al. : Clinical characteristics and outcomes of witnessed hypothermic cardiac arrest: A systematic review on rescue collapse. Resuscitation 2019.137: 41–48 [DOI] [PubMed] [Google Scholar]
- 31.Pasquier M, Zurron N, Weith B, et al. : Deep accidental hypothermia with core temperature below 24°c presenting with vital signs. High Alt Med Biol 2014.15: 58–63 [DOI] [PubMed] [Google Scholar]
- 32.Chen YS, Lin JW, Yu HY, et al. : Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet 2008.372: 554–561 [DOI] [PubMed] [Google Scholar]
- 33.Pasquier M, Hugli O, Paal P, et al. : Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: The HOPE score. Resuscitation 2018.126: 58–64 [DOI] [PubMed] [Google Scholar]
- 34.Pasquier M, Paal P, Blancher M, Darocha T: Higher survival chances of hypothermic vs. normothermic cardiac arrest patients with ECLS re-warming. Resuscitation 2019.134: 161–162 [DOI] [PubMed] [Google Scholar]
- 35.Pasquier M, Rousson V, Darocha T, et al. : Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: An external validation of the HOPE score. Resuscitation 2019.139: 321–328 [DOI] [PubMed] [Google Scholar]
- 36.Pasquier M, Rousson V, Darocha T, Hugli O: Reply to: The integration of prehospital standard operating procedures and in-hospital HOPE score for management of hypothermic patients in cardiac arrest. Resuscitation 2019.141: 214–215 [DOI] [PubMed] [Google Scholar]
- 37.Gordon L, Paal P: Normothermic and hypothermic cardiac arrest-Beware of Jekyll and Hyde. Resuscitation 2018.129: e10–e11 [DOI] [PubMed] [Google Scholar]
- 38.Darocha T, Kosiński S, Jarosz A, et al. : Should capnography be used as a guide for choosing a ventilation strategy in circulatory shock caused by severe hypothermia? Observational case-series study. Scand J Trauma Resusc Emerg Med 2017.25: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murphy RA, Bobrow BJ, Spaite DW, Hu C, McDannold R, Vadeboncoeur TF: Association between prehospital CPR quality and end-tidal carbon dioxide levels in out-of-hospital cardiac arrest. Prehosp Emerg Care 2016.20: 369–377 [DOI] [PubMed] [Google Scholar]
- 40.Skulec R, Vojtisek P, Cerny V: Correlation between end-tidal carbon dioxide and the degree of compression of heart cavities measured by transthoracic echocardiography during cardiopulmonary resuscitation for out-of-hospital cardiac arrest. Crit Care 2019.23: 334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dennis M, Lal S, Forrest P, et al. : In-depth extracorporeal cardiopulmonary resuscitation in adult out-of-hospital cardiac arrest. J Am Heart Assoc 2020.9: e016521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Darocha T, Sobczyk D, Kosiński S, et al. : New diastolic cardiomyopathy in patients with severe accidental hypothermia after ECMO rewarming: A case-series observational study. Cardiovasc Ultrasound 2015.13: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruttmann E, Weissenbacher A, Ulmer H, et al. : Prolonged extracorporeal membrane oxygenation-assisted support provides improved survival in hypothermic patients with cardiocirculatory arrest. J Thorac Cardiovasc Surg 2007.134: 594–600 [DOI] [PubMed] [Google Scholar]
- 44.Darocha T, Podsiadło P, Polak M, et al. : Prognostic factors for nonasphyxia-related cardiac arrest patients undergoing extracorporeal rewarming - HELP Registry Study. J Cardiothorac Vasc Anesth 2020.34: 365–371 [DOI] [PubMed] [Google Scholar]
- 45.Gilbert M, Busund R, Skagseth A, Nilsen PA, Solbø JP: Resuscitation from accidental hypothermia of 13.7 degrees C with circulatory arrest. Lancet 2000.355: 375–376 [DOI] [PubMed] [Google Scholar]
- 46.Woodhall B, Sealy WC, Hall KD, Floyd WL: Craniotomy under conditions of quinidine-protected cardioplegia and profound hypothermia. Ann Surg 1960.152: 37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Walpoth BH, Walpoth-Aslan BN, Mattle HP, et al. : Outcome of survivors of accidental deep hypothermia and circulatory arrest treated with extracorporeal blood warming. N Engl J Med 1997.337: 1500–1505 [DOI] [PubMed] [Google Scholar]
- 48.Dunne B, Christou E, Duff O, Merry C: Extracorporeal-assisted rewarming in the management of accidental deep hypothermic cardiac arrest: A systematic review of the literature. Heart Lung Circ 2014.23: 1029–1035 [DOI] [PubMed] [Google Scholar]
- 49.Brugger H, Bouzat P, Pasquier M, et al. : Cut-off values of serum potassium and core temperature at hospital admission for extracorporeal rewarming of avalanche victims in cardiac arrest: A retrospective multi-centre study. Resuscitation 2019.139: 222–229 [DOI] [PubMed] [Google Scholar]
- 50.Weuster M, Haneya A, Panholzer B, et al. : The use of extracorporeal membrane oxygenation systems in severe accidental hypothermia after drowning: a centre experience. ASAIO J 2016.62: 157–162 [DOI] [PubMed] [Google Scholar]
- 51.Eich C, Bräuer A, Timmermann A, et al. : Outcome of 12 drowned children with attempted resuscitation on cardiopulmonary bypass: An analysis of variables based on the “Utstein Style for Drowning”. Resuscitation 2007.75: 42–52 [DOI] [PubMed] [Google Scholar]
- 52.Coskun KO, Popov AF, Schmitto JD, et al. : Extracorporeal circulation for rewarming in drowning and near-drowning pediatric patients. Artif Organs 2010.34: 1026–1030 [DOI] [PubMed] [Google Scholar]
- 53.Skarda D, Barnhart D, Scaife E, Molitor M, Meyers R, Rollins M: Extracorporeal cardiopulmonary resuscitation (EC-CPR) for hypothermic arrest in children: Is meaningful survival a reasonable expectation? J Pediatr Surg 2012.47: 2239–2243 [DOI] [PubMed] [Google Scholar]
- 54.Champigneulle B, Bellenfant-Zegdi F, Follin A, et al. : Extracorporeal life support (ECLS) for refractory cardiac arrest after drowning: An 11-year experience. Resuscitation 2015.88: 126–131 [DOI] [PubMed] [Google Scholar]
- 55.Darocha T, Kosiński S, Jarosz A, et al. : The chain of survival in hypothermic circulatory arrest: Encouraging preliminary results when using early identification, risk stratification and extracorporeal rewarming. Scand J Trauma Resusc Emerg Med 2016.24: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pasquier M, Debaty G, Carron PN, Darocha T: Reply to: The importance of pre-hospital interventions for prevention and management of witnessed hypothermic cardiac arrest’. Resuscitation 2019.140: 219–220 [DOI] [PubMed] [Google Scholar]
- 57.Strapazzon G, Forti A, Rauch S, Brugger H: The integration of prehospital standard operating procedures and in-hospital HOPE score for management of hypothermic patients in cardiac arrest. Resuscitation 2019.141: 212–213 [DOI] [PubMed] [Google Scholar]
- 58.Darocha T, Kosinski S, Ziętkiewicz M, et al. : Create a chain of survival: extracorporeal life support treatment of severe hypothermia victims. Artif Organs 2016.40: 812–813 [DOI] [PubMed] [Google Scholar]
- 59.Debaty G, Moustapha I, Bouzat P, et al. : Outcome after severe accidental hypothermia in the French Alps: A 10-year review. Resuscitation 2015.93: 118–123 [DOI] [PubMed] [Google Scholar]
- 60.Forti A, Brugnaro P, Rauch S, et al. : Hypothermic cardiac arrest with full neurologic recovery after approximately nine hours of cardiopulmonary resuscitation: Management and possible complications. Ann Emerg Med 2019.73: 52–57 [DOI] [PubMed] [Google Scholar]
- 61.Khorsandi M, Dougherty S, Young N, et al. : Extracorporeal life support for refractory cardiac arrest from accidental hypothermia: A 10-year experience in Edinburgh. J Emerg Med 2017.52: 160–168 [DOI] [PubMed] [Google Scholar]
- 62.Sawamoto K, Bird SB, Katayama Y, et al. : Outcome from severe accidental hypothermia with cardiac arrest resuscitated with extracorporeal cardiopulmonary resuscitation. Am J Emerg Med 2014.32: 320–324 [DOI] [PubMed] [Google Scholar]
- 63.Podsiadło P, Kosiński S, Darocha T, Hugli O, Pasquier M: Hypothermic cardiac arrest patients’ selection criteria for extracorporeal life support rewarming in extreme cases. Ann Emerg Med 2019.74: 166–167 [DOI] [PubMed] [Google Scholar]
- 64.Kosiński S, Darocha T, Jarosz A, et al. : Difficulties in funding of VA-ECMO therapy for patients with severe accidental hypothermia. Anaesthesiol Intensive Ther 2017.49: 106–109 [DOI] [PubMed] [Google Scholar]
- 65.Jarosz A, Darocha T, Kosiński S, Ziętkiewicz M, Drwiła R: Extracorporeal membrane oxygenation in severe accidental hypothermia. Intensive Care Med 2015.41: 169–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Debaty G, Babaz V, Durand M, et al. : Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation 2017.112: 1–10 [DOI] [PubMed] [Google Scholar]
- 67.Nolan JP, Soar J, Cariou A, et al. : European resuscitation council and European Society of Intensive Care Medicine Guidelines for Post-resuscitation Care 2015: Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 2015.95: 202–222 [DOI] [PubMed] [Google Scholar]
- 68.Daniel N, Weinberg N, Carus F, Church B, Zafren K: Witnessed cardiac arrest in a hypothermic avalanche victim completely buried for 2 hours. Wilderness Environ Med 2021.32: 92–97 [DOI] [PubMed] [Google Scholar]
- 69.Zafren K, Giesbrecht GG, Danzl DF, et al. ; Wilderness Medical Society: Wilderness medical Society practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia: 2014 update. Wilderness Environ Med 2014.25(4 suppl): S66–S85 [DOI] [PubMed] [Google Scholar]
- 70.Brodmann Maeder M, Dünser M, Eberle B, et al. : The bernese hypothermia algorithm: A consensus paper on in-hospital decision-making and treatment of patients in hypothermic cardiac arrest at an alpine level 1 trauma centre. Injury 2011.42: 539–543 [DOI] [PubMed] [Google Scholar]
- 71.Paal P, Milani M, Brown D, Boyd J, Ellerton J: Termination of cardiopulmonary resuscitation in mountain rescue. High Alt Med Biol 2012.13: 200–208 [DOI] [PubMed] [Google Scholar]
- 72.Darocha T, Kosiński S, Jarosz A, Drwila R: Extracorporeal rewarming from accidental hypothermia of patient with suspected trauma. Medicine (Baltimore) 2015.94: e1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mendonca M, Hautz WE, Schucht P, et al. : Extracorporeal life support in hypothermic cardiac arrest: Reconsidering trauma as an absolute contraindication. Resuscitation 2019.135: 228–229 [DOI] [PubMed] [Google Scholar]
- 74.ELSO: ELSO Anticoagulation Guideline. Available from: https://www.elso.org/Portals/0/Files/elsoanticoagulationguideline8-2014-table-contents.pdf.
- 75.Kosinski S, Darocha T, Jarosz A, et al. : The longest persisting ventricular fibrillation with an excellent outcome - 6h 45min cardiac arrest. Resuscitation 2016.105: e21–e22 [DOI] [PubMed] [Google Scholar]
- 76.Althaus U, Aeberhard P, Schüpbach P, Nachbur BH, Mühlemann W: Management of profound accidental hypothermia with cardiorespiratory arrest. Ann Surg 1982.195: 492–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Carlsen AW, Winnerkvist AM, Greiff G: A 95 year-old suffering circulatory arrest after accidental hypothermia: A case report. BMC Geriatr 2017.17: 249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.ELSO: General Guidelines for all ECLS Cases. Available from: https://www.elso.org/Portals/0/ELSO%20Guidelines%20General%20All%20ECLS%20Version%201_4.pdf.
- 79.Aubin H, Lichtenberg A, Albert A: Reply: EMS, HEMS, ECMO Center, ICU team: are you ready for hypothermic patients? Extracorporeal membrane oxygenation in severe accidental hypothermia. JACC Heart Fail 2016.4: 830–831 [DOI] [PubMed] [Google Scholar]
- 80.Mair P RE: Sangalli F PN, Pesenti A. (ed), ECMO for severe accidental hypothermia. in ECMO-Extracorporeal Life Support in Adults. 2014, pp Italia, Springer-Verlag, 163–170. [Google Scholar]
- 81.Swol J, Belohlávek J, Brodie D, et al. : Extracorporeal life support in the emergency department: A narrative review for the emergency physician. Resuscitation 2018.133: 108–117 [DOI] [PubMed] [Google Scholar]
- 82.ELSO: Ultrasound Guidance for Extracorporeal Membrane Oxygenation General Guidelines. Available from: https://www.elso.org/Portals/0/Files/elso_Ultrasoundguideance_ecmogeneral_guidelines_May2015.pdf. Accessed June 2021.
- 83.ELSO: Ultrasound Guidance for Extracorporeal Membrane Oxygenation Veno-Arterial ECMO specific guidelines. Available from: https://www.elso.org/Portals/0/Files/elso_Ultrasoundguidance_vaecmo_guidelines_May2015.pdf. Accessed June 2021.
- 84.ELSO: Guidelines for Adult Cardiac Failure. Available from: https://www.elso.org/Portals/0/IGD/Archive/FileManager/e76ef78eabcusersshyerdocumentselsoguidelinesforadultcardiacfailure1.3.pdf.
- 85.Pasquier M, Blancher M, Buse S, et al. : Intra-patient potassium variability after hypothermic cardiac arrest: A multicentre, prospective study. Scand J Trauma Resusc Emerg Med 2019.27: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Grigore AM, Grocott HP, Mathew JP, et al. ; Neurologic Outcome Research Group of the Duke Heart Center: The rewarming rate and increased peak temperature alter neurocognitive outcome after cardiac surgery. Anesth Analg 2002.94: 4–10, table of contents [DOI] [PubMed] [Google Scholar]
- 87.Engelman R, Baker RA, Likosky DS, et al. ; Society of Thoracic Surgeons; Society of Cardiovascular Anesthesiologists; American Society of ExtraCorporeal Technology: The Society of Thoracic Surgeons, The Society of Cardiovascular Anesthesiologists, and The American Society of ExtraCorporeal Technology: Clinical Practice Guidelines for Cardiopulmonary Bypass–Temperature Management During Cardiopulmonary Bypass. Ann Thorac Surg 2015.100: 748–757 [DOI] [PubMed] [Google Scholar]
- 88.Kawahara F, Kadoi Y, Saito S, Goto F, Fujita N: Slow rewarming improves jugular venous oxygen saturation during rewarming. Acta Anaesthesiol Scand 2003.47: 419–424 [DOI] [PubMed] [Google Scholar]
- 89.Saczkowski R, Kuzak N, Grunau B, Schulze C: Extracorporeal life support rewarming rate is associated with survival with good neurological outcome in accidental hypothermia. Eur J Cardiothorac Surg 2021.59: 593–600 [DOI] [PubMed] [Google Scholar]