Abstract
Objective:
Completing a college degree is associated with success in employment, financial earnings, and life satisfaction. Mental health difficulties, including attention-deficit/hyperactivity disorder (ADHD), can compromise degree completion.
Method:
We examined 4-year academic performance trajectories of 201 college students with ADHD (97 receiving medication [ADHD-Med], 104 not receiving medication [ADHD-NoMed]) relative to 205 non-ADHD Comparison students. Demographic (e.g., sex, race/ethnicity), psychological (e.g., self-reported depression and anxiety symptoms), and service-related (e.g., receipt of academic support) variables were included as predictors of intercept (i.e., Year 1 performance) and slope (yearly change) of semester GPA, progress toward graduation, and self-reported study skill strategies.
Results:
College students with ADHD obtained significantly lower GPAs (Hedge’s g = −0.46 and −0.63) and reported less frequent use of study skills strategies (Hedge’s g range from −1.00 to −2.28) than Comparison students. Significantly more Comparison students (59.1%) persisted through eight semesters relative to ADHD-NoMed students (49%). Multiple variables predicted outcomes with parent education, fewer depressive symptoms, better executive functioning, and receipt of high school Section 504 accommodations and college academic support services among the strongest predictors.
Conclusions.
Findings suggest support services for students with ADHD should begin prior to college matriculation and focus on improving executive functioning skills and depressive symptoms to increase chances of academic success.
Keywords: Attention-deficit/hyperactivity disorder, ADHD, college students, academic achievement
Obtaining a bachelor’s degree confers several distinct advantages over a high school diploma including lower rates of unemployment, higher wages, and greater job and life satisfaction (Bureau of Labor Statistics, 2018; Pew Research Center, 2016). However, only 54.3% of first year college students in the United States will earn their bachelor’s within 6 years of initial enrollment (Espinosa et al., 2019) with 11-21% of students failing to matriculate for two consecutive academic years (National Student Clearinghouse Research Center, 2019). Researchers have investigated success in college for decades (e.g., Lewis & Yates, 2019; Wintraub & Salley, 1945) to identify factors that differentiate successful and unsuccessful students. Many factors predictive of college success have been identified including demographic variables (e.g., sex, minority status, parent education level), psychological functioning (e.g., mental health diagnosis, maladaptive thinking), and the use of support services (e.g., academic services, psychological services).
Predictors of Academic Success in College
With respect to student demographic characteristics, females earn higher grade-point averages (GPAs; D’Limia et al., 2014; Hoffman & Lowitzki, 2005; Kuh et al., 2008) and are more likely to earn bachelor’s degrees relative to males (Musu-Gillette et al., 2017). Regarding differences by race/ethnicity, African American and Hispanic students earn lower GPAs, have diminished persistence into their second year of college, and are less likely to earn a bachelor’s degree relative to White students (Espinosa et al., 2019; Fischer, 2007; Kuh et al., 2008). Finally, first-generation college students are reported to attempt fewer credits and earn lower GPAs relative to students with a family history of college experience (Kuh et al., 2008; Pascarala et al., 2004). These demographic differences are likely due to cultural and historical factors (e.g., disparities in educational opportunity) and do not reflect differences inherent to a specific gender, race, or SES group.
Beyond basic demographic variables, maladaptive cognitions associated with mental health diagnoses (e.g., low perceived control, high perceived stress) have been found to predict both lower GPA and lesser persistence in college students (Haynes et al., 2009; Saunders-Scott et al., 2018). Students with a depressive disorder earn lower GPAs and are at higher risk for drop-out relative to those without depression (Eisenberg et al., 2009). The research concerning anxiety and academic performance is less clear. Al-Qaisy (2011) found a positive relation between anxiety symptomology and academic achievement. Conversely, Van Ameringen, et al. (2003) reported that nearly half of individuals with an anxiety disorder leave school prematurely. Eisenberg and colleagues (2009) also reported that students with anxiety and comorbid depression have particularly negative outcomes for GPA and retention relative to students without a diagnosis.
Despite the rising prevalence and deleterious effects of mental health diagnoses, only 26.1% of adolescents with attention-deficit/hyperactivity disorder (ADHD) are reported by parents to be currently receiving psychosocial treatment (Danielson et al., 2018) and only 18.7% of college students report that they have ever received mental health services (Oswalt et al., 2018). Regarding academic support services, parents report 40.1% of adolescents with ADHD have a current individualized education program (IEP) and 14.2% receive Section 504 educational accommodations (DuPaul et al., 2019). Utilization rates for college academic services are less clear and often are based on small samples or reported in a manner that limits firm conclusions. For example, Chew et al. (2009), reported that only 16% of students with ADHD used available services. More broadly, the most recent National College Learning Center Association survey (Toms, 2016) indicated individual college campuses serve a median of 1,500 students with any disability per year (range = 175 to 18,000). However, research regarding the effectiveness of such support services is scant.
Despite documented efficacy for symptom reduction, the salutary effects of psychosocial treatments are equivocal for key academic variables (e.g., GPA, course withdrawals; Advokat et al., 2011; Anastopoulos & King, 2015; Eisenberg et al., 2009). Medication has been associated with higher college entrance exam scores (Lu et al., 2017) and improved executive functioning and psychosocial functioning in college students (DuPaul et al., 2012). A meta-analysis of academic outcomes among primary school children found medication-related improvements in core academic subjects (e.g., math accuracy; Kortekass-Rijlaarsdam et al., 2019) and such academic improvements may persist for 24 months (Hechtman et al., 2004), with others reporting childhood stimulant treatment improves high school GPA up to 9-years later (Powers et al., 2008).
The literature regarding the effect of academic services is mixed, with some evidence from small trials indicating that academic support services can result in higher course grades and program retention (Matthews et al., 2013; Yeats et al., 2010). Others have reported academic supports alone are insufficient for improving first year GPA (Angrist et al., 2009). Conversely, more comprehensive supports including cognitive behavioral therapy and direct skill instruction have been found to increase academic (e.g., credit hours attempted and earned) and psychological (e.g., significant reductions in ADHD, anxiety, and depressive symptomology) success in a sample of students with ADHD (Anastopoulos et al., 2020). Given the rising number of students with disabilities on college campuses, it is important to investigate malleable factors associated with academic success and progress toward degree completion for this vulnerable student population.
College Students with ADHD
Approximately 11% of college students are identified with one or more disabilities (National Center for Education Statistics, 2016). One of the most common disabilities in the college population is ADHD with 6% of first-year students reporting having received an ADHD diagnosis (Eagan et al., 2014). Students with ADHD may be particularly susceptible to risk factors (e.g., additional psychological disorders, poor executive functioning skills) that predict a lower probability of college success (Anastopoulos et al., 2018, 2020; Weyandt et al., 2017). Young adults with ADHD are less likely to enroll in post-secondary institutions (Barkley et al., 2008) and those who do attend college obtain significantly lower GPAs (DuPaul et al., 2018; Gormley et al., 2016), withdraw from courses more frequently (Advokat et al., 2011), and are less likely to graduate (Hechtman et al., 2016) relative to their non-ADHD peers. These academic performance difficulties appear largely due to the myriad of executive functioning deficits associated with ADHD (Weyandt et al., 2013).
Although it is clear that having ADHD places college students at academic risk, the current knowledge base is limited in several important ways. Available longitudinal studies following children with ADHD into adulthood (e.g., Barkley et al., 2008; Hechtman et al,., 2016) have not focused specifically on college students. Prior studies that have investigated college functioning have been cross-sectional and therefore do not explicate how academic performance is impacted over time and whether trajectories are affected by individual differences (e.g., ADHD symptom severity, receipt of psychotropic medication treatment for ADHD). Relatedly, many of these prior studies have considered college students as a singular group without controlling for or reporting year in college (e.g., Advokat et al., 2010). Also, previous investigations typically have not identified ADHD with sufficient diagnostic rigor, typically relying on a single self-report measure for study inclusion. In addition, studies have employed few measures of academic performance beyond GPA, have not consistently included a non-ADHD comparison group, and have not considered a wide range of other factors (e.g., demographic characteristics, study skills, psychiatric comorbidities) that may impact academic performance in college.
Purpose of Current Study
Although much has been learned about the impact of ADHD on children and adults (Barkley, 2015), relatively less research attention has been directed to the way in which ADHD unfolds among adolescents and young adults transitioning into college. In recent years, colleges and universities have witnessed dramatic increases in their enrollments of students with ADHD (Eagan et al., 2014; Weyandt & DuPaul, 2012). Because ADHD is highly prevalent among college students, is associated with substantial risk for educational difficulties, and its effects on academic performance trajectories of college students have not been investigated, the primary purposes of the current study were to: (a) explicate the academic performance trajectories of college students with and without ADHD, and (b) identify demographic and malleable predictors of academic performance across time to inform future prevention and intervention development. Trajectory differences for students with ADHD who did or did not receive medication also were examined. Multiple academic outcomes were assessed including GPA by semester; progress towards graduation by academic year; self-reported study skills by academic year; and college drop-out status. Fifteen predictors were included: student gender, race, and ethnicity; parent education level; receipt of IEP services, 504 educational accommodations, or psychosocial treatment in high school; anxiety disorder and depression symptom severity; knowledge of and cognitions associated with ADHD; executive functioning skills; and receipt of psychosocial treatment and academic support services in college.
Based upon prior findings, we hypothesized that: (a) college students with ADHD would obtain significantly lower GPAs, report lesser quality study strategies, and show lower rates of persistent enrollment across semesters relative to students without ADHD; (b) pharmacological treatment would result in better academic trajectories; (c) demographic variables (i.e., being female, White, and having parents with higher levels of education) would be associated with better academic outcomes; (d) students meeting criteria for an anxiety or mood disorder would have worse outcomes relative to those without a diagnosis; (e) maladaptive cognitions would be associated with lower academic outcomes; (f) higher executive functioning would predict better academic outcomes; and (g) psychosocial and academic service use would not be associated with improved academic outcomes. We assumed that slopes for all variables would be linear; however, because 4-year trajectories have not been investigated previously, we viewed trend analyses as exploratory.
Method
Participants
Participants were recruited for a longitudinal study examining the long-term outcomes of college students with ADHD across three eastern states in the United States (see Anastopoulos et al., 2018). At baseline, participants were first-year college students (N=456, 220= Male, 236= Female) between 18 to 22 years of age (M = 18.23; SD = 0.52). The full sample of participants was 71.7% Caucasian, 12.3% African American, 5.5% Asian, 3.9% more than one race, and 6.6% other/not reported. By design, at year 1, 228 students met research criteria for the ADHD group and 228 students met research criteria for the Comparison group. The sample of students available for the current four-year analyses ranged from 380-420 students, including 190-216 non-ADHD Comparisons. The ADHD group was subdivided based on self-reported Year 1 ADHD medication status with 94-99 students reporting medication use (ADHD-Med) and 96-105 not receiving medication (ADHD-NoMed). For those participants who completed Year 1 assessment measures, 69.7% of participants with ADHD and 85.1% of control participants completed Year 4 assessment measures. For GPA, the retention rate was 62.4% for participants with ADHD and 72.9% for Comparison participants. The primary reasons for loss of participant cases and fluctuation of sample size across analyses included non-reporting of Year 1 ADHD medication use, complete missingness of dependent variables, or missingness of independent variables. At Year 1, groups did not differ with respect to age and sex. Groups differed regarding ethnicity (χ2 [2] = 12.272, p =.002) with ADHD-Med including significantly fewer Hispanic participants (18.2%) relative to ADHD-NoMed (39%) and Comparison (35.5%) participants. Similarly, parent education level was significantly higher for ADHD-Med participants than students in the other two groups (F [2,422] = 4.17, p < .016).
Screening Measures
Demographic Information
Participants provided a range of demographic information including age, gender, race, ethnicity, parent educational level, and marital status.
ADHD Rating Scale–Self-Report Version (ADHD RS-SRV)
The ADHD RS-SRV, developed specifically for the purposes of this study, is a modified version of the ADHD RS-IV (DuPaul et al., 1998). The scale lists the inattention (IN) and hyperactive-impulsive (HI) symptoms in alternating fashion, which are rated on a 4-point Likert scale (0=never or rarely, 3=very often). Symptom frequency counts for both IN and HI are calculated by summing the number of items scored 2 or 3. The ADHD RS-SRV addresses ADHD symptoms both during childhood and during the past 6 months, also taking into account medication status (i.e., completed regarding symptoms on and off medication for those students receiving pharmacotherapy). Internal consistency reliability data in the current sample suggest acceptable (.74) to excellent (.94) for the childhood and past 6 months reports of both IN and HI symptoms, regardless of medication status.
ADHD Rating Scale-IV: Parent Version.
The ADHD Rating Scale-IV: Parent Version is an existing measure that was sent to parents to obtain multi-respondent diagnostic information (DuPaul et al., 1998). The scale is identical to the ADHD Rating Scale-Childhood and Past 6 Months versions; however, the wording on each item reflects that the questions are asking about the individual’s child. Parents completed the form by indicating two ratings of their child’s behavior when they were not on medication, both from the ages of 5-12 to measure childhood symptoms and in the past 6-months to measure current symptoms. The ADHD Rating Scale-IV: Parent Version has excellent internal consistency (α=.92) and adequate discriminant validity (DuPaul et al., 1998). Internal consistency estimates in the current study were good to excellent (alpha range .89 to .94).
Semi-Structured ADHD Interview
The Semi-Structured ADHD Interview was created for this study to simultaneously address symptom presentation and impairment. The interview is based on DSM-5 adult ADHD criteria and includes nine questions about symptoms of IA and nine questions about symptoms of HI to assess for symptom presence and severity (American Psychiatric Association, 2013). Additional questions explore the degree to which symptoms impair functioning as well as the age of onset of symptoms. Coefficient alphas for both the IN and HI portions of the interview were excellent and good (.90 and .85, respectively).
Structured Clinical Interview for DSM Disorders (SCID-I)
The SCID-I is a computer-based semi-structured interview based on the DSM-IV-TR criteria (American Psychiatric Association, 2000) that is used to test for clinically significant presentations of psychiatric disorders (First et al., 2002). Specifically, the presence of anxiety, mood, and eating disorders was ascertained. Trained graduate assistants in Ph.D. or Masters level clinical and school psychology programs conducted the SCID-I interviews. The SCID-I has adequate inter-rater reliability with kappa levels between .70 and 1.00 (First et al., 2002).
Expert panel classification
The expert panel consisted of four PhD-level psychologists with expertise in the assessment and treatment of ADHD. The panel utilized the data described previously to determine the eligibility for each student enrolled in the current project. Classification of ADHD or non-ADHD comparison for the present study was based on the unanimous decision reached by the four-member expert panel. In addition, the panel made final decisions regarding psychological classifications (e.g., anxiety or mood disorder) that may have been exclusionary or comorbid with ADHD. In instances in which the panel members came to different classifications, the entire panel discussed the case until consensus was reached.
Dependent Measures
GPA
With participant consent, college GPAs were collected from university registrars. For a small number of students (n = 18; 3.9% of the sample) for whom registrar data were not available, self-report of GPA was used. College GPAs were calculated on a four-point scale either ranging from 0.0-4.0 or 0.0-4.3. To adjust for this discrepancy across sites, the range for college GPA was capped at 4.0 (i.e. any value equal to or above 4.0 was recorded as 4.0). GPA was recorded for each of the first four semesters of college.
Progress toward Graduation
Progress toward graduation was assessed by calculating the percentage of credits earned relative to credits needed for graduation at each university.
Learning and Study Strategies Inventory, Second Edition (LASSI)
The LASSI is an 80-item measure used to collect information on students’ awareness about and use of learning and study strategies (Weinstein & Palmer, 2002). Students rate their skill, will, and self-regulation components of strategic learning on a 5-point Likert Scale (a= not at all typical of me, e= very much typical of me). The LASSI is comprised of three factor scores derived from 10 subscales that measure anxiety, attitude, concentration, information processing, motivation, selecting main ideas, self-testing, study aids, test strategies, and time management. Each subscale of the LASSI has demonstrated acceptable to good reliability, with coefficient alphas ranging from .73-.89. Given the relevance to the current study, the LASSI factor scores -Affective Strategies, Comprehension Monitoring Strategies, and Goal Strategies - were included as dependent measures.
Enrollment status
Information regarding enrollment status was collected yearly for each participant. So long as a student was enrolled for at least one academic credit, they were considered as enrolled for a given semester.
Predictor Measures
Beck Anxiety Inventory (BAI)
The BAI is a self-report measure of anxiety symptom severity in adults (Beck & Steer, 1993). The scale includes 21 items that measure symptom severity over the past week. Each item is rated on a four-point Likert scale (0=not at all, 3=severely), with higher scores indicating greater severity of anxiety symptoms. Individuals who score higher on the BAI are more likely to be experiencing more severe symptoms of anxiety. The BAI has excellent levels of internal consistency (α=.92) and adequate concurrent validity (Beck et al., 1988). Internal consistency for the current sample was excellent (alpha = .92).
Beck Depression Inventory- Second Edition (BDI-II)
The BDI-II measures depression symptom severity among adults, where adults report symptom severity over the past two weeks (Beck et al., 1996). The scale includes 21 items, and each item provides response options rated on a four-point scale (0=not at all, 3=severely). Higher ratings on each question indicate greater severity of depression symptoms. The BDI-II has excellent internal consistency (α=.93) and concurrent validity with other depression measures in the assessment of college students (Beck et al., 1996). Internal consistency for the current sample was excellent (alpha = .92).
Behavior Rating Inventory of Executive Function-Adult version
Executive functioning was assessed using the Behavior Rating Inventory of Executive Function - Adult Version (BRIEF-A;Gioia, et al., 2000). The BRIEF-A is a self-report instrument that takes approximately 10 minutes to complete and has adequate psychometric properties (Gioia et al., 2000). Individuals with ADHD have been found to perform more poorly on executive function measures including the BRIEF-A, relative to control participants (Nigg et al., 2005; Toplak et al., 2008; DuPaul et al., 2012). In addition to providing nine specific executive functioning scores, the BRIEF-A generates three general composite scores: Behavior Regulation Index, Metacognition Index, and General Executive Composite the latter of which was used as a predictor measure in the current study. To complete the BRIEF-A, participants rate the frequency of 75 problematic behaviors over the past month on a 3-point scale (1=never; 2=sometimes; 3=often). Higher scores indicate greater degrees of executive dysfunction. The BRIEF-A has demonstrated reliability, validity, and clinical utility as an ecologically sensitive measure of EF in healthy respondents, as well as individuals with a range of psychiatric and neurological conditions (Gioia et al., 2000;. Roth et al., 2005).
Test of ADHD Knowledge
A 40-item test of ADHD knowledge (TOAK) was constructed for use in this study. Items assess the degree to which students agreed with various statements about the nature, assessment, and treatment of ADHD with higher scores indicating greater knowledge. Internal consistency was good (alpha = .82) and test-retest reliability over one year is moderate (r = .58) for the current sample. Greater knowledge of ADHD was associated with higher self-reported use of medication and psychosocial services but not academic supports in this sample (Gormley et al., 2018).
ADHD Cognitions Scale
The 20-item version of the ADHD Cognitions Scale for Adults (ACS; Knouse et al., 2017) was used to assess negative automatic thoughts associated with ADHD. Examples of items are “I’ll just do this one thing first” and “I do better waiting until the last minute.” Participants rate how often each thought occurs to them on a 5-point Likert scale ranging from 1 (not at all) to 5 (all the time). Higher scores indicate more frequent automatic negative thoughts. The ACS has good internal consistency (alpha = .82) and split-half reliability (Spearman-Brown Coefficient for Unequal Length = .84). Moderate correlations with established measures of avoidance, coping, ADHD symptoms, and emotion regulation support the convergent validity of the ACS (Knouse et al.). Internal consistency for the ACS in Year 1 of the current study was good (alpha = .87).
Receipt of Treatment
Students self-reported their receipt of pharmacological, psychological, and academic treatment and supports. Students reported use of medication for both ADHD-related and non-ADHD-related difficulties. Participants with ADHD were placed in the ADHD-Med group if they reported current use (i.e., type and dosage) of one or more medications for treatment of ADHD. It should be noted that 26.7% of ADHD-NoMed participants reported receiving medication in high school but were no longer receiving medication in Year 1 of college. Students were also asked to report the type, if any, of therapy services they had received (i.e., individual, group, or family therapy). Thus, the psychological services variable was coded as 1 (present) or 0 (absent) if students reported receiving at least one therapeutic service in Year 1. Similarly, students were asked about receipt of a range of academic support services (e.g., tutoring, academic skills assistance, writing assistance, career counseling, registered with campus disability office). The academic support services variable was coded as 1 (present) or 0 (absent) if students reported receiving at least one academic support service in Year 1. Finally, students reported their receipt (1 = present, 0 = absent) of individualized education program (IEP) services, Section 504 educational accommodations, and psychological treatment in high school.
Procedure
Study procedures were approved by the institutional review board at all three project sites. Participants were recruited through university disability service offices, summer orientation activities, campus newspapers, social media, and campus postings.
ADHD and Comparison group status was determined via multi-method multi-stage assessment procedures. The first assessment stage included completion of ADHD Rating Scale (DuPaul et al., 1998), modified to address current and past ADHD symptoms, in addition to medication status. If self-report or parent-report indicated frequent displays of four or more symptoms of either inattention or hyperactivity-impulsivity during both childhood and the past 6 months, a semi-structured interview for adult ADHD was administered to address full DSM-5 criteria for ADHD. This same interview was administered to potential Comparison participants if self- and parent-reported responses to the ADHD Rating Scale indicated the presence of three or fewer symptoms for both inattention and hyperactivity-impulsivity during childhood and currently. Participants whose interview responses continued to suggest the presence of three or fewer symptoms from both symptom lists were deemed eligible for the Comparison group. A panel of four ADHD experts (i.e., the three principal investigators and a nationally recognized adult ADHD consultant) reviewed all potentially eligible cases. Unanimous panel agreement was required for determination of ADHD and Comparison group status, in addition to non-ADHD psychiatric comorbidity status.
Once eligible for the study, participants completed a variety of measures in a standardized order across two-to-three meetings conducted by graduate students and doctoral level staff trained on all assessment procedures. Course grades and enrollment status were obtained at the conclusion of each academic year. Participants were provided with monetary incentives at the completion of each annual evaluation.
Statistical Analyses
We used multiple group latent growth curve modeling (LGCM) implemented within Mplus, version 8 (Muthén & Muthén, 2017) to estimate trajectories of change separately for each of the three subgroups (Comparisons, ADHD-Med, ADHD-NoMed) on five dependent measures. Given the consistently spaced annual assessment schedule (or semi-annual in the case of semester GPA), the time metric was set at 1-year (or semester for GPA) intervals and the intercept set at Year 1 (fall semester Year 1 for GPA). Visual inspection of the group means over time suggested non-linear change for semester GPA and progress toward graduation; therefore, both linear and quadratic unconditional growth models were estimated, and change in model fit using the chi-square likelihood ratio test (LRT) was used to determine whether estimation of non-linear trajectories was tenable. Quadratic growth models were estimated for GPA and progress toward graduation, and linear growth models were estimated for LASSI subscales. Due to the non-normal nature of some of the outcome data, we used bootstrapping (10,000 replications) to calculate bias-corrected confidence intervals when making determinations of statistical significance. The threshold for statistical significance of growth factors (i.e., intercepts, slopes, quadratic terms) was set at p < .05, and the threshold for predictors of growth factors was set at p < .10. Within each model, covariates were retained if associations with intercept or slope achieved significance for any of the three groups. Covariate associations with the quadratic term were not considered during model refinement because there were no hypotheses associated with acceleration or deceleration of trajectories. Change in sample-size adjusted Bayesian Information Criteria (BIC) was checked and likelihood ratio tests (LRT) were performed to ensure model fit was not significantly hurt by these refinements. In all cases, model fit was either improved or not significantly changed by dropping covariates from the full model (See Table 1) Overall quality of model fit was determined by examining a combination of fit statistics – Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), and the Standardized Root Mean Square Residual (SRMR) – following guidelines for model acceptability described by Hu and Bentler (1999). Wald tests were used to compare growth parameter means and variabilities across groups within models (Asparouhov & Muthén, 2010).
Table 1.
Model Fit
| Model | BICSSA | RMSEA | CFI | Chi-square | df | LRT p-value |
|---|---|---|---|---|---|---|
| Grade Point Average (GPA) | ||||||
| Full | 5518.74 | 0.06 | 0.89 | 448.69 | 297 | |
| Refined | 5458.49 | 0.06 | 0.90 | 368.70 | 237 | 0.043 |
| Graduation Progress | ||||||
| Full | 7608.34 | 0.03 | 1.00 | 59.95 | 54 | |
| Refined | 7611.23 | 0.01 | 1.00 | 39.92 | 39 | 0.171 |
| LASSI Affective Strategies | ||||||
| Full | 7791.29 | 0.05 | 0.98 | 128.89 | 99 | |
| Refined | 7769.12 | 0.02 | 1.00 | 84.97 | 81 | 0.001 |
| LASSI Comprehension Monitoring | ||||||
| Full | 7835.82 | 0.05 | 0.98 | 129.69 | 101 | |
| Refined | 7870.02 | 0.05 | 0.98 | 118.00 | 89 | 0.471 |
| LASSI Goal Strategies | ||||||
| Full | 7704.65 | 0.05 | 0.97 | 120.01 | 89 | |
| Refined | 7702.29 | 0.06 | 0.98 | 86.96 | 59 | 0.320 |
Note. BIC = Bayesian Information Criteria. RMSEA = Root Mean Square Error of Approximation. CFI = Comparative Fit Index. SRMR = Standardized Root Mean Square Residual. LRT = Likelihood Ratio Test. LASSI = Learning and Study Strategies Inventory.
To evaluate if groups differed with respect to academic persistence (i.e., number of semesters continuously enrolled and/or graduation in eight or fewer semesters), we conducted a survival analysis using Kaplan-Meier survival curves and the Wilcoxon test. The Kaplan-Meier approach was selected due to the presence of censored observations (i.e., data collection ended prior to graduation or non-enrollment for 55.4% of cases; Kleinbaum & Klein, 2012). The Wilcoxon test is useful when early failure is expected as is the case for school dropout with 50% of noncompleters dropping out before their second year (Tinto, 1996).
Results
Group Differences: Predictor Variables
Prior to main analyses, we examined group differences in predictor variables. BRIEF-A, BAI, comorbidity status, and receipt of psychological services differed significantly across groups with both ADHD groups reporting greater executive functioning deficits and anxiety symptoms, higher likelihood of non-ADHD diagnoses, and greater receipt of psychological services at baseline than Comparison participants (all ps < .05). The two ADHD groups did not differ on these variables. In addition, the three groups differed significantly regarding BDI, ADHD Knowledge, ADHD Cognitions, and receipt of psychological services during high school (all ps < .05). ADHD-NoMed participants reported significantly more depressive symptoms on the BDI than ADHD-Med participants who, in turn, reported more symptoms than Comparison participants. ADHD-Med participants received higher ADHD Knowledge scores than ADHD-NoMed participants who, in turn, scored higher than Comparison participants. ADHD-NoMed participants reported more ADHD cognitions than ADHD-Med participants who, in turn, reported more than Comparison participants. ADHD-Med participants were more likely to receive psychological services during high school relative to the ADHD-NoMed participants who, in turn, were more likely to receive high school psychological services relative to Comparison participants. Groups did not differ with respect to receipt of college academic services at baseline. During high school, ADHD-Med participants were more likely to report having an IEP relative to Comparison participants (p <.05) with no differences between the ADHD groups or between ADHD-NoMed and Comparison participants. Finally, ADHD-Med participants were more likely to report a Section 504 plan during high school relative to the ADHD-NoMed participants (p <.01); however, no differences were reported between Comparison participants and either ADHD group.
Intercept and Trajectory Group Differences: GPA
Model fit for GPA was mediocre, with RMSEA = 0.63 (CI90%: 0.05-0.08), CFI = 0.90, and SRMR = .10. Analysis of individual group model fit suggested that the ADHD-Med group drove the misfit (RMSEA = .08, CFI = .76, SRMR = .07), with the other two groups achieving adequate-to-good fit (RMSEA < .05, CFI ≥ .93, SRMR ≤ .11). For semester GPA, Comparison students had a significantly higher mean GPA at intercept compared to ADHD-NoMed and ADHD-Med (fall semester, Year 1; p < .001; Hedge’s g = 0.63 and 0.46 respectively), with no differences between ADHD-Med and ADHD-NoMed (p = .984; see Figure 1). There was a significant negative linear trend to GPA trajectories for Comparisons and ADHD-Med groups; however, the ADHD-NoMed subgroup did not show systematic change over time. Multiple variables were significantly associated with GPA intercept and/or slope for each of the three groups (see Table 2). Notably, higher parent education was associated with higher first-semester GPA for all three groups. High school IEP was associated with lower first semester GPA for ADHD-NoMed participants, and greater ADHD cognitions was correlated with higher initial semester GPA for the ADHD-Med group. Receipt of academic services was positively associated with GPA trajectory for ADHD-NoMed students, and greater ADHD knowledge was correlated with declining GPA trajectory for this group. Counterintuitively, higher BRIEF score was associated with positive GPA slope for ADHD-Med participants. For Comparison participants, greater depressive symptoms and receipt of psychological treatment were negatively associated with GPA trajectory, while higher BRIEF score and high school IEP receipt were positively associated with GPA trajectory.
Figure 1.
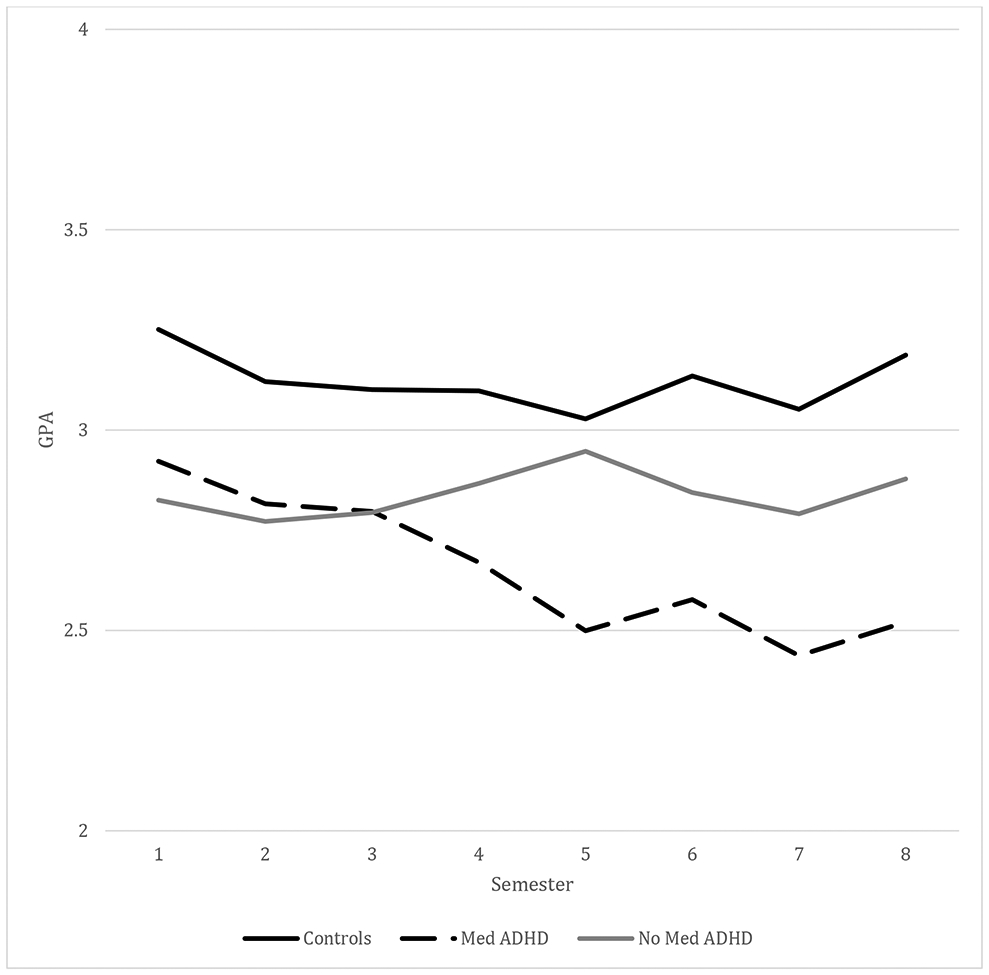
Grade Point Average (GPA) across Eight Semesters for Non-ADHD Comparisons, Non-Medicated Students with ADHD, and Medicated Students with attention-deficit/hyperactivity disorder (ADHD)
Table 2.
Prediction Model for GPA
| GPA | ||||||
|---|---|---|---|---|---|---|
| Intercept | Linear Slope | Quadratic Slope | ||||
| Comparisons | β | CI | β | CI | β | CI |
| Mean | 3.239 | 3.145, 3.327 | −0.099 | −0.151, −0.058 | 0.013 | 0.006, 0.02 |
| Residual Variance | 0.336 | 0.251, 0.475 | 0.028 | 0.004, 0.062 | 0.000 | 0.000-0.001 |
| Sex | ||||||
| Race/Ethnicity | ||||||
| Parent Education | 0.118 | 0.055, 0.176 | −0.016 | −0.039, 0.007 | 0.002 | −0.001, 0.005 |
| HS_IEP | 0.126 | −0.518, 0.811 | 0.192 | 0.031, 0.38 | −0.028 | −0.06, −0.004 |
| HS_504 | ||||||
| HS_PSYTX | 0.081 | −0.084, 0.256 | −0.149 | −0.252, −0.071 | 0.025 | 0.013, 0.04 |
| BRIEF | 0.019 | −0.07, 0.107 | 0.032 | 0, 0.066 | −0.006 | −0.011, −0.002 |
| BDI | 0.121 | 0.008, 0.231 | −0.065 | −0.106, −0.023 | 0.008 | 0.003, 0.013 |
| BAI | ||||||
| Comorbidity | −0.342 | −0.673, −0.051 | 0.114 | −0.05, 0.269 | −0.014 | −0.032, 0.006 |
| Psychological Services | −0.406 | −0.665, −0.121 | 0.081 | −0.085, 0.227 | −0.012 | −0.032, 0.011 |
| Academic Services | 0.098 | −0.008, 0.197 | −0.022 | −0.068, 0.019 | 0.005 | 0, 0.012 |
| ADHD Knowledge | 0.082 | 0.027, 0.142 | −0.017 | −0.041, 0.002 | 0.001 | −0.002, 0.004 |
| ADHD Cognition | −0.079 | −0.158, 0.001 | 0.029 | −0.002, 0.064 | −0.003 | −0.008, 0.001 |
| Intercept | Linear Slope | Quadratic Slope | ||||
| No Medication ADHD | β | CI | β | CI | β | CI |
| Mean | 2.813 | 2.66, 2.958 | −0.029 | −0.113, 0.038 | 0.005 | −0.005, 0.018 |
| Residual Variance | 0.413 | 0.270, 0.716 | 0.014 | 0.006, 0.028 | 0.000 | 0.000,0.000 |
| Sex | ||||||
| Race/Ethnicity | ||||||
| Parent Education | 0.127 | 0.031, 0.226 | −0.019 | −0.06, 0.015 | 0.002 | −0.003, 0.007 |
| HS_IEP | −0.618 | −1.023, −0.266 | −0.015 | −0.23, 0.213 | 0.008 | −0.026, 0.039 |
| HS_504 | ||||||
| HS_PSYTX | 0.149 | −0.168, 0.437 | −0.007 | −0.125, 0.134 | 0.002 | −0.017, 0.017 |
| BRIEF | 0.057 | −0.011, 0.128 | 0.008 | −0.019, 0.038 | −0.002 | −0.006, 0.002 |
| BDI | −0.076 | −0.197, 0.048 | −0.013 | −0.069, 0.04 | 0.001 | −0.007, 0.008 |
| BAI | ||||||
| Comorbidity | −0.031 | −0.335, 0.266 | 0.092 | −0.025, 0.25 | −0.012 | −0.033, 0.005 |
| Psychological Services | 0.162 | −0.263, 0.564 | −0.135 | −0.333, 0.035 | 0.01 | −0.021, 0.043 |
| Academic Services | 0.023 | −0.1, 0.177 | 0.082 | 0.021, 0.144 | −0.012 | −0.021, −0.002 |
| ADHD Knowledge | 0.027 | −0.054, 0.119 | −0.033 | −0.073, 0 | 0.004 | −0.001, 0.01 |
| ADHD Cognition | −0.031 | −0.098, 0.049 | −0.019 | −0.055, 0.013 | 0.003 | −0.002, 0.008 |
| Intercept | Linear Slope | Quadratic Slope | ||||
| Medicated ADHD | β | CI | β | CI | β | CI |
| Mean | 2.928 | 2.756, 3.083 | −0.121 | −0.255, −0.009 | 0.01 | −0.007, 0.029 |
| Residual Variance | 0.393 | 0.255, 0.682 | 0.1 | 0.028, 0.259 | 0.001 | 0.001,0.004 |
| Sex | ||||||
| Race/Ethnicity | ||||||
| Parent Education | 0.148 | 0.049, 0.256 | −0.014 | −0.078, 0.059 | 0.004 | −0.006, 0.012 |
| HS_IEP | −0.231 | −0.611, 0.101 | 0.122 | −0.074, 0.346 | −0.023 | −0.053, 0.003 |
| HS_504 | ||||||
| HS_PSYTX | −0.086 | −0.403, 0.191 | 0.113 | −0.058, 0.321 | −0.015 | −0.044, 0.009 |
| BRIEF | −0.067 | −0.184, 0.043 | 0.087 | 0.012, 0.171 | −0.012 | −0.023, −0.002 |
| BDI | −0.066 | −0.212, 0.062 | −0.043 | −0.128, 0.034 | 0.005 | −0.005, 0.016 |
| BAI | ||||||
| Comorbidity | 0.017 | −0.385, 0.413 | −0.059 | −0.31, 0.186 | 0.021 | −0.011, 0.055 |
| Psychological Services | 0.132 | −0.145, 0.449 | −0.196 | −0.461, 0.034 | 0.024 | −0.005, 0.06 |
| Academic Services | 0.028 | −0.122, 0.161 | −0.024 | −0.122, 0.063 | 0.008 | −0.003, 0.023 |
| ADHD Knowledge | 0.055 | −0.03, 0.164 | −0.039 | −0.096, 0.006 | 0.006 | 0, 0.014 |
| ADHD Cognition | 0.172 | 0.036, 0.311 | −0.036 | −0.12, 0.059 | 0.008 | −0.005, 0.019 |
Note. ADHD = Attention-deficit/hyperactivity disorder. BRIEF-A = Behavior Rating Inventory of Executive Function-Adult version. BDI = Beck Depression Inventory. BAI = Beck Anxiety Inventory. HS = high school. IEP = Individual Education Program. PSY-TX = psychological treatment. Statistically significant values for growth parameters (p < .05) and predictor variables (p < .10) are in bold-face type.
Intercept and Trajectory Group Differences: Progress Toward Graduation
Model fit for progress toward graduation was good, with RMSEA = 0.01 (CI90%: 0.00-0.06), CFI = 0.99, and SRMR = .04. There were no significant differences between groups regarding progress toward graduation at intercept (Year 1). There was greater inter-subject variability in intercepts among students in both ADHD groups than Comparisons (p < .001). There were significant positive linear components to progress toward graduation trajectories for all groups. None of the quadratic slope means were significant. Where they contributed to the models was that all of the residual variances for the quadratic slope parameters were significant (Comparisons p = .016; ADHD-NoMed p = .003; ADHD-Med p = .004). Significant predictors of graduation progress intercept and slope within subgroup are in Table 3. As with GPA, higher parent education was associated with greater initial and trajectory of progress toward graduation, particularly for Comparison and ADHD-Med students. Receipt of academic services and higher ADHD Cognition score were associated with greater initial progress toward graduation for ADHD-Med students. ADHD-Med students who were non-White, received high school IEP services, and reported lower ADHD cognitions exhibited slower progress toward graduation. Conversely, receipt of high school psychological treatment was associated with faster progress toward graduation for ADHD-Med students, while the reverse was true for Comparisons. Male Comparison students showed slower progress toward graduation than female Comparisons.
Table 3.
Prediction Model for Progress to Graduation
| Grad Progress | ||||||
|---|---|---|---|---|---|---|
| Intercept | Linear Slope | Quadratic Slope | ||||
| Comparisons | β | CI | β | CI | β | CI |
| Mean | 25.081 | 24.143, 26.306 | 24.44 | 23.423, 25.36 | −0.11 | −0.41, 0.209 |
| Residual Variance | 51.985 | 22.413, 96.648 | 21.076 | 11.796, 43.480 | 1.25 | 0.495, 2.675 |
| Sex | −2.251 | −4.268, −0.778 | −1.462 | −2.938, −0.11 | 0.23 | −0.229, 0.718 |
| Race/Ethnicity | 2.295 | 0.728, 4.274 | 0.093 | −1.512, 1.784 | 0.01 | −0.508, 0.557 |
| Parent Education | 1.112 | 0.559, 1.799 | 1.244 | 0.656, 1.833 | −0.12 | −0.318, 0.067 |
| HS_IEP | −2.64 | −8.338, 0.975 | 3.701 | −0.465, 11.854 | −1.5 | −7.819, 1.147 |
| HS_504 | −2.171 | −5.099, −0.155 | −0.758 | −4.771, 2.507 | 0.08 | −0.916, 1.46 |
| HS_PSYTX | −2.698 | −5.193, −0.619 | −1.96 | −4.189, −0.142 | 0.46 | −0.036, 1.134 |
| BRIEF | 0.731 | 0.03, 1.578 | 0.021 | −0.646, 0.774 | 0.10 | −0.134, 0.326 |
| BDI | ||||||
| BAI | ||||||
| Comorbidity | ||||||
| Psychological Services | ||||||
| Academic Services | 2.012 | 0.23, 3.909 | 0.29 | −0.789, 1.412 | −0.14 | −0.505, 0.257 |
| ADHD Knowledge | ||||||
| ADHD Cognition | −0.126 | −0.312, 0.032 | 0.031 | −0.111, 0.18 | −0.04 | −0.095, 0.002 |
| Intercept | Linear Slope | Quadratic Slope | ||||
| No Medication ADHD | β | CI | β | CI | β | CI |
| Mean | 25.235 | 23.192, 27.896 | 24.485 | 22.923, 25.91 | −0.294 | −0.778, 0.18 |
| Residual Variance | 136.85 | 66.741, 248.676 | 23.25 | 15.357, 40.709 | 1.542 | 0.879, 3.645 |
| Sex | −3.776 | −8.542, 0.49 | 0.925 | −1.411, 3.509 | 0.13 | −0.632, 0.898 |
| Race/Ethnicity | 1.979 | −3.295, 6.669 | 0.031 | −2.794, 2.638 | 0.033 | −0.799, 0.888 |
| Parent Education | 0.449 | −0.843, 1.835 | 0.963 | 0.229, 1.668 | −0.457 | −0.72, −0.196 |
| HS_IEP | −5.429 | −11.005, 0.083 | −3.344 | −7.895, 0.788 | 0.734 | −0.496, 2.172 |
| HS_504 | 4.599 | −3.053, 14.746 | 1.4 | −2.798, 4.865 | −1.447 | −2.723, −0.081 |
| HS_PSYTX | −2.217 | −6.933, 1.853 | −0.989 | −3.762, 1.52 | 0.714 | −0.09, 1.637 |
| BRIEF | 0.493 | −0.219, 1.503 | 0.278 | −0.281, 0.8 | −0.061 | −0.233, 0.113 |
| BDI | ||||||
| BAI | ||||||
| Comorbidity | ||||||
| Psychological Services | ||||||
| Academic Services | 0.32 | −1.528, 2.116 | 0.203 | −0.924, 1.376 | 0.06 | −0.315, 0.442 |
| ADHD Knowledge | ||||||
| ADHD Cognition | −0.157 | −0.437, 0.076 | −0.112 | −0.27, 0.066 | 0.012 | −0.035, 0.068 |
| Intercept | Linear Slope | Quadratic Slope | ||||
| Medicated ADHD | β | CI | β | CI | β | CI |
| Mean | 25.813 | 23.679, 28.466 | 22.925 | 21.176, 24.349 | −0.326 | −0.957, 0.496 |
| Residual Variance | 120.49 | 67.564, 201.668 | 19.237 | 10.485, 45.599 | 2.334 | 1.439, 7.183 |
| Sex | −1.274 | −5.143, 2.906 | −1.314 | −3.415, 0.822 | −0.146 | −1.109, 0.73 |
| Race/Ethnicity | −5.1 | −13.837, 1.795 | 3.226 | 0.153, 7.169 | −0.25 | −1.974, 1.329 |
| Parent Education | 1.658 | 0.245, 3.203 | 1.457 | 0.648, 2.556 | −0.201 | −0.679, 0.211 |
| HS_IEP | −1.737 | −7.039, 4.013 | −2.804 | −5.358, −0.204 | 0.789 | −0.268, 1.856 |
| HS_504 | 3.879 | −0.964, 9.158 | 2.066 | −0.137, 4.336 | −0.446 | −1.379, 0.482 |
| HS_PSYTX | 1.818 | −2.152, 6.053 | 2.685 | 0.572, 5.276 | −1.543 | −2.569, −0.675 |
| BRIEF | −1.298 | −2.81, 0.074 | 0.046 | −0.624, 0.775 | 0.01 | −0.285, 0.29 |
| BDI | ||||||
| BAI | ||||||
| Comorbidity | ||||||
| Psychological Services | ||||||
| Academic Services | 2.316 | 0.454, 4.682 | −0.373 | −1.524, 0.755 | 0.047 | −0.411, 0.502 |
| ADHD Knowledge | ||||||
| ADHD Cognition | 0.375 | 0.083, 0.708 | 0.201 | 0.013, 0.426 | −0.003 | −0.098, 0.078 |
Note. ADHD = Attention-deficit/hyperactivity disorder. BRIEF-A = Behavior Rating Inventory of Executive Function-Adult version. BDI = Beck Depression Inventory. BAI = Beck Anxiety Inventory. HS = high school. IEP = Individual Education Program. PSY-TX = psychological treatment. Statistically significant values for growth parameters (p < .05) and predictor variables (p < .10) are in bold-face type.
Intercept and Trajectory Group Differences: LASSI Affective Strategies
Model fit was excellent for LASSI Affective Strategies, with RMSEA = 0.02 (CI90%: 0.00-0.05), CFI = 0.99, and SRMR = .05. For LASSI Affective Strategies, Comparisons had a significantly higher score at intercept than ADHD-NoMed and ADHD-Med groups ( p < .001; Hedge’s g = 2.0 and 1.58, respectively), which were also statistically different from each other with ADHD-Med greater than ADHD-NoMed (p = .021; Hedge’s g = 0.43; see Figure 2, top panel). Change over time (i.e., slope) was only statistically significant (with a positive trend) for the ADHD-NoMed group. Multiple variables predicted higher Year 1 scores for ADHD students including White non-Hispanic background, receipt of high school 504 but no receipt of high school IEP services, lower depression symptoms, lower ADHD cognitions, and receipt of academic services (see Table A1 in online supplementary materials). ADHD-NoMed students who did not receive academic services showed a positive trend in scores over time.
Figure 2.
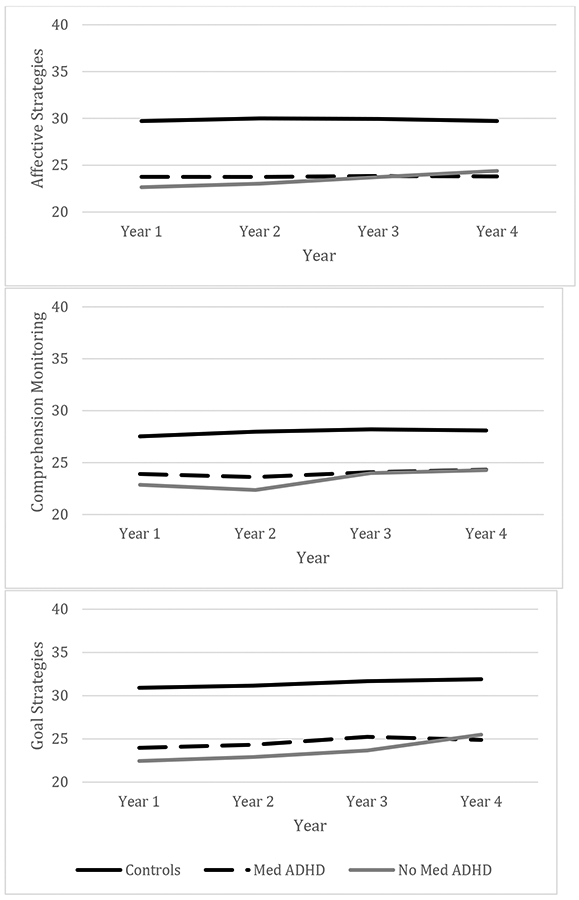
Learning and Study Strategies Inventory (LASSI): Affective Strategies (top), Comprehension Monitoring (middle), and Goal Strategies (bottom) Across Groups
Intercept and Trajectory Group Differences: LASSI Comprehension Monitoring
Model fit was excellent for LASSI Comprehension Monitoring, with RMSEA = 0.03 (CI90%: 0.00-0.06) and CFI = 0.990, and SRMR = .07. For LASSI Comprehension Monitoring Strategies, Comparisons had a significantly higher score at intercept than ADHD-NoMed and ADHD-Med participants ( p < .001; Hedge’s g = 1.35 and 1.0, respectively) who were not different from each other (p = .072; Hedge’s g = 0.32; see Figure 2, middle panel). Linear growth was statistically significant for the Comparison and ADHD-NoMed groups. Variables that predicted higher Year 1 scores included receipt of high school 504 but not IEP services, lower executive functioning deficits, receipt of academic services, and lower depression symptoms (see Table A2 in online supplementary materials). Higher BRIEF scores also predicted positive trend over time for Comparison and ADHD-NoMed students.
Intercept and Trajectory Group Differences: LASSI Goal Strategies
Model fit was good for LASSI Goal Strategies, with RMSEA = 0.05 (CI90%: 0.02-0.07), CFI = 0.98, and SRMR = .07. For LASSI Goal Strategies, Comparisons had a significantly higher score at intercept than ADHD-NoMed and ADHD-Med participants (p < .001; Hedge’s g = 2.28 and 1.87, respectively) than either ADHD group, who were also statistically different from each other (p = .003; Hedge’s g = 0.61; see Figure 2, bottom panel). All three groups showed significant positive growth over time. The ADHD-NoMed group showed significantly greater growth compared to the Comparison participants (p < .001) and the ADHD-Med group (p < .005), while the difference in growth between the ADHD-Med group and the Comparison group was not statistically significant (p = .083). Significant predictors of LASSI subscale intercept and slope are displayed in Table A3 (online supplementary material). For the ADHD-Med group, receipt of high school 504 accommodations but not IEP services, lower anxiety and depression symptoms predicted higher intercept scores, and higher BRIEF scores were correlated with positive trend over time. Receipt of high school psychological treatment was associated with higher Year 1 LASSI Goal Strategies for ADHD-Non Med participants, while comorbidity and non-receipt of college psychological services was associated with positive trend over time. For Comparisons, higher initial Goal Strategies score was predicted by lower BRIEF-A scores and positive trend over time was associated with White non-Hispanic background.
Survival Analysis: Academic Persistence
With respect to academic persistence, 59.1% of Comparison participants persisted through eight semesters or graduated during the study period with a mean of 6.4 semesters persisted. The ADHD-Med group persisted for an average of 5.9 semesters with 54% of students persisting through the entire study or graduating prior to the end of the study. Finally, only 49% of students in the ADHD-NoMed group persisted through the study period with an average of 5.6 semesters persisted (see Figure 3). Results of an omnibus Wilcoxon test indicated differences in survival curves were not statistically significant (χ2 [2]=5.37; p=.068); however, follow-up pairwise comparisons revealed statistically significant differences in survival curves between Comparison students and those in the ADHD-NoMed group (χ2 [1]=5.195; p=.023).
Figure 3.
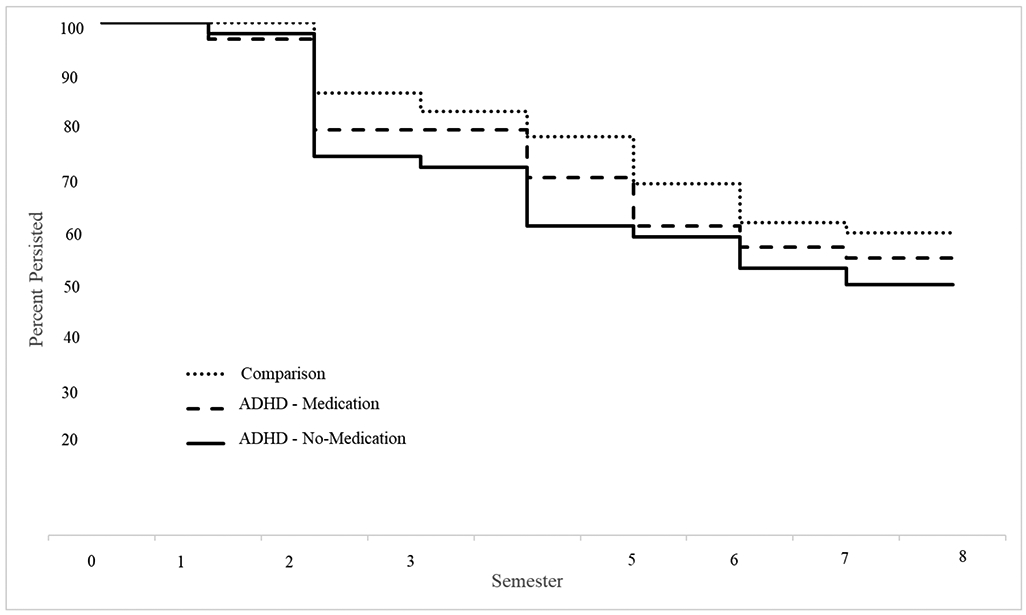
Survival curves across semesters for Comparison Students without attention-deficit/hyperactivity disorder (ADHD), Non-Medicated Students with ADHD, and Medicated Students with ADHD
Discussion
As predicted based on prior studies (e.g., Hechtman et al., 2016), college students with ADHD obtained significantly lower GPAs and reported less frequent use of study skills strategies relative to non-ADHD peers, with differences of medium to large magnitude. Although small differences favoring students with medication were found for affective and goal study skill strategies, ADHD students who did not receive medication showed a positive trend across years for all study skills scores. Academic service receipt was associated with increasing GPA trajectory but only for students with ADHD not receiving medication. Progress toward graduation was similar across groups; however, students with ADHD showed diminished progress over time. Further, students with ADHD not taking medication persisted significantly fewer semesters (i.e., 5.6 semesters, on average) relative to students without ADHD (i.e., 6.4 semesters, on average). These results represent an important advance over prior research in showing academic and study skills deficits were maintained over time, regardless of ADHD medication status or receipt of psychological or academic services. Medication, however, may be associated with persistent enrollment.
Contrary to hypotheses, only a few predictors of academic outcomes for students with ADHD were identified. Higher parent education predicted Year 1 GPA for both ADHD groups, along with receipt of High School IEP for ADHD-NoMed participants and lower ADHD cognitions for ADHD-Med students. Receipt of academic support services and lower ADHD knowledge predicted better performance over time for non-medicated students with ADHD, whereas higher BRIEF-A scores (i.e., poorer executive functioning) predicted positive GPA slope for medicated students with ADHD. All of these findings are consistent with predictions; however, the relationship between executive functioning difficulties and positive trend for ADHD-Med participants is unclear, especially as stimulant medication is associated with improved executive functioning in college students with ADHD (DuPaul et al., 2012). In general, better executive functioning, receipt of high school 504 accommodations, and participation in academic services predicted greater study skills particularly for students with ADHD on medication. Receipt of high school IEP services and depression symptoms predicted inferior study skills; each of these variables could be considered markers of more significant adjustment difficulties. Given that this is the first longitudinal study to examine predictors of academic trajectories for college students with ADHD, these represent novel and unique findings particularly in the relatively ubiquitous association of college academic services with academic functioning and study skills. Controlled studies are necessary to more specifically examine the impact of academic support services on educational outcomes for students with ADHD.
Several predictors of academic trajectories for students with ADHD are particularly compelling given that they may be potential targets for intervention both prior to and during college. For example, executive functioning deficits (e.g., organization skills, assignment tracking and completion) can be addressed by training (e.g., Evans et al., 2018; Sibley et al., 2016, 2020) interventions in secondary school. To the extent that treatment-related gains in executive functioning lead to enhanced study skills that maintain over time, adolescents may be better prepared for college. In similar fashion, cognitive behavior therapy may improve maladaptive cognitions and inattention symptoms in adolescents (Sprich et al., 2016) and emerging adults (e.g., Anastopoulos & King, 2015; Anastopoulos et al., 2020) which could lead to improved comorbid depressive symptoms and better academic performance.
Limitations
Interpretation of our results should be considered in the context of several methodological limitations. First, all participants were students from four-year universities, thus precluding extension of these findings to students with and without ADHD attending 2-year institutions and community colleges. Second, participating universities were from the eastern region of the US and may not represent college outcomes from other regions. Third, medication status for students with ADHD was based on Year 1 medication use and it is possible that their use of medication fluctuated over the 4-year assessment period. Fourth, many of the variables were based on student self-report and could be subject to bias related to social desirability and shared source and method variance. Finally, data retention rates were lower for college students with ADHD relative to their non-ADHD peers, as has been the case for prior longitudinal studies comparing individuals with and without ADHD (e.g., Barkley & Fischer, 2017; Molina et al., 2017). Nevertheless, this study is the largest and most comprehensive to date regarding academic performance and college outcomes for students with ADHD.
Implications for Clinical Practice
There are several important implications of these findings for providing support to youth with ADHD both prior to and following college matriculation. First, depression symptoms play a significant role in academic progress for all students with symptoms of depression requiring specific attention and support to ameliorate negative outcomes. Second, because students with ADHD show significant academic challenges beginning in the first semester, transition support focused on study and self-regulation strategies is critically important for high school students intending to move on to post-secondary education. Developmentally-tailored training interventions focused on organization skills, homework performance, and social interactions should be part of transition support efforts given evidence for their efficacy with adolescents with ADHD (Evans et al., 2018). Third, medication status was not associated with significant advantages for any outcome except for LASSI Affective Strategies and, even then, between-group differences diminished over time. Medicated students with ADHD showed a significant negative linear trend in GPA across years, perhaps indicating that medication status is a marker of symptom severity. Alternatively, receipt of academic support services was associated with better GPA and use of study skills strategies; however, the majority of students with ADHD in this sample did not receive academic skills assistance or tutoring (i.e., 19.7% reported receiving academic skills assistance, 34.2% reported receiving tutoring services, and 58.8% reported meeting with professor or academic advisor). Thus, it is critically important to connect students with ADHD to these services from the onset of their college studies, particularly for those not receiving medication. Fourth, cognitive-behavioral intervention for students with ADHD should focus on improving executive functioning (e.g., organization, planning, and time management skills), challenging and revising maladaptive cognitions, ameliorating depressive symptoms, and improving knowledge about ADHD. Combining cognitive-behavioral intervention with individual mentoring that targets these four areas may enhance academic functioning of college students with ADHD (Anastopoulos et al., 2020).
Conclusion
The results of this large-scale multi-site longitudinal study shed much needed new light on the way in which ADHD impacts young adults during their college years, thereby helping to fill a gap in our understanding of the progression of this disorder across the lifespan. Obtained findings confirm the significant challenges faced by students with ADHD regarding succeeding in and completing college, even among those receiving medical treatment. Importantly, many variables correlated with academic performance are malleable and therefore can be targeted by interventions prior to, and throughout, the college years. Future research should build on these findings to identify additional variables (e.g., student self-advocacy skills, student self-efficacy) that may predict college educational outcomes. It will be critically important to develop and implement evidence-based academic and psychological support strategies that give students with ADHD the knowledge and skills necessary for success, not only during college but also during the transition into their post-college adult years.
Supplementary Material
Acknowledgments
This research was supported by Grant R01MH094435 from the National Institute of Mental Health awarded to Drs. Anastopoulos, DuPaul, and Weyandt. Data were managed using Research Electronic Data Capture (REDCap), supported by a University of Utah College of Nursing grant (8UL1TR000105).
References
- Advokat C, Lane SM, & Lou C (2011). College students with and without ADHD: Comparison of self-report of medication usage, study habits, and academic achievement. Journal of Attention Disorders, 15(8), 656–666. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Anastopoulos AD, DuPaul GJ, Weyandt LL, Morrissey-Kane E, Sommer JL, Rhoads LH, Murphy KR, Gormley MJ, & Gudmundsdottir BG (2018). Rates and patterns of comorbidity among first-year college students with ADHD. Journal of Clinical Child & Adolescent Psychology, 47, 236–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastopoulos AD, & King KA (2015). A cognitive-behavior therapy and mentoring program for college students with ADHD. Cognitive and Behavioral Practice, 22, 141–151. [Google Scholar]
- Anastopoulos AD King KA, Besecker LH, O’Rourke SR, Bray AC, & Supple AJ (2020). Cognitive-behavior therapy for college students with ADHD: Temporal stability of improvements in functioning following active treatment. Journal of Attention Disorders, 24, 863–874. [DOI] [PubMed] [Google Scholar]
- Barkley RA & Fischer M (2017). The Milwaukee Longitudinal Study of Hyperactive (ADHD Children. In Hechtman L (Ed.), Attention deficit hyperactivity disorder: Adult outcome and its predictors (pp. 63–104). Oxford University Press. [Google Scholar]
- Barkley RA, Murphy KR, & Fischer M (2008). ADHD in adults: What the science says. Guilford Press. [Google Scholar]
- Beck AT, & Steer RA (1993). Beck Anxiety Inventory manual. Psychological Corporation. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory–II. Psychological Corporation. [Google Scholar]
- Danielson ML, Visser SN, Chronis-Tuscano A, & DuPaul GJ (2018). A national description of treatment among United States children and adolescents with attention-deficit/hyperactivity disorder. The Journal of Pediatrics, 192, 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Chronis-Tuscano A, Danielson ML, & Visser SN (2019). Predictors of receipt of school services in a national sample of youth with attention-deficit/hyperactivity disorder. Journal of Attention Disorders, 23, 1303–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Franklin MK, Pollack BL, Fletcher KS, Jaffe AR, Gormley MJ, Anastopoulos AD, & Weyandt LL (2018). Predictors and trajectories of educational functioning in college students with and without attention-deficit/hyperactivity disorder. Journal of Postsecondary Education and Disability, 31, 161–178. [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, & Reid R (1998). ADHD rating scale-IV: Checklists, norms, and clinical interpretation. Guilford Press. [Google Scholar]
- DuPaul GJ, Weyandt LL, Rossi JS, Vilardo BA, O’Dell SM, Carson KM, Verdi G, & Swentosky A (2012). Double-blind, placebo-controlled, crossover study of the efficacy and safety of lisdexamfetamine dimesylate in college students with attention-deficit/hyperactivity disorder. Journal of Attention Disorders, 16, 202–220. [DOI] [PubMed] [Google Scholar]
- Eagan MK, Stolzenberg EB, Zimmerman HB, Aragon MC, Whang Sayson H, & Rios-Aguilar C (2017). The American freshman: National norms fall 2016. Higher Education Research Institute, UCLA. [Google Scholar]
- Eisenberg D, Golberstein E, & Hunt JB (2009). Mental health and academic success in college. The B. E. Journal of Economic Analysis & Policy, 9, 1–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinosa LL, Turk JM, Taylor M, & Chessman HM (2019). Race and ethnicity in higher education: A status report. American Council on Education. [Google Scholar]
- Evans SW, Owens JS, Wymbs BT, & Ray RR (2018). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology, 47, 157–198. [DOI] [PubMed] [Google Scholar]
- Fischer EMJ (2007). Settling into campus life: Differences by race/ethnicity in college involvement and outcomes. The Journal of Higher Education, 78, 125–161. 10.1080/00221546.2007.11780871 [DOI] [Google Scholar]
- Gormley MJ, DuPaul GJ, Anastopoulos AD, & Weyandt LL (2016). First year GPA and academic service use among college students with and without ADHD. Journal of Attention Disorders. 10.1177/1087054715623046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hechtman L (2017). Attention deficit hyperactivity disorder: Adult outcome and its predictors. Oxford University Press. [Google Scholar]
- Hechtman L, Abikoff H, Klein RG, Weiss G, Respitz C, Kouri J, Blum C, Greenfield B, Etcovitch J, Fleiss K, & Pollack S (2004). Academic achievement and emotional status of children with ADHD treated with long-term methylphenidate and multimodal psychosocial treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 812–819. doi: 10.1097/01.chi.0000128796.84202.eb [DOI] [PubMed] [Google Scholar]
- Hechtman L, Swanson JM, Sibley MH, Stehli A, Owens EB, Mitchell JT, Arnold LE, Molina BSG, Hinshaw SP, Jensen PS, Abikoff HB, Algorta GP, Howard AS, Hoza B, Etcovitch J, Houssais S, Lakes KD, & Nichols JQ (2016). Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 945–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janisus GM & Weyandt LL (2010). An exploratory study of substance use and misuse among college students with and without ADHD and other disabilities. Journal of Attention Disorders, 14, 205–215. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, & Klein M (2012). Survival analysis: A self-learning text (3rd ed.). Springer. [Google Scholar]
- Knouse LE, Mitchell JT, Kimbrel NA, & Anastopoulos AD (2017). Development and evaluation of the ADHD Cognitions Scale for Adults. Journal of Attention Disorders. Online publication DOI: 10.1177/1087054717707580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortekaas-Rijlaarsdam AF, Luman M, Sonuga-Barke E & Oosterlaan J (2019). Does methlphenidate improve academic performance? A systematic review and meta-analysis. European Child & Adolescent Psychiatry, 28, 155–164. 10.1007/s00787-018-1106-3 [DOI] [PubMed] [Google Scholar]
- Kuh GD, Cruce TM, Shoup R, & Kinzie J (2008). Unmasking the effects of student engagement on first-year college grades and persistence. The Journal of Higher Education, 79, 540–563. [Google Scholar]
- Lu Y, Sjolander A, Cederlof M, D’Onofrio BM, Almqvist C, Larsson H & Lichtenstein P (2017). Association between medication use and performance on higher education entrance tests in individuals with attention-deficit/hyperactivity disorder. JAMA Psychiatry, 74, 815–822. doi: 10.1001/jamapsychiatry.2017.1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill BM, Molina BSG, Coxe S, Gnagy EM, Altszuler AR, Macphee FL, Morrow AS, Trucco EM, & Pelham WE (2020). Functional outcomes of young adults with childhood ADHD: A latent profile analysis. Journal of Clinical Child & Adolescent Psychology, 49, 215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Sibley MH, Pedersen SL, & Pelham WE Jr. (2017). The Pittsburgh ADHD Longitudinal Study (PALS). In Hechtman L (Ed.), Attention deficit hyperactivity disorder: Adult outcome and its predictors. (pp. 105–156). Oxford University Press. [Google Scholar]
- Musu-Gillette L, de Brey C, McFarland J, Hussar W, Sonnenberg W, & Wilkinson-Flicker S (2017). Status and Trends in the Education of Racial and Ethnic Groups 2017 (NCES 2017-051). U.S. Department of Education, National Center for Education Statistics. Washington, DC. Retrieved February/15/2019 from http://nces.ed.gov/pubsearch. [Google Scholar]
- National Center for Education Statistics (2019). Digest of education statistics, 2017. U.S. Department of Education. [Google Scholar]
- National Student Clearinghouse Research Center (2019). High school benchmarks: National college progression rates. Author. [Google Scholar]
- Powers RL, Marks DJ, Miller CJ, Newcorn JH, & Halperin JM (2008). Stimulant treatment in children with attention-deficit/hyperactivity disorder moderates adolescent academic outcomes. Journal of Child and Adolescent Psychopharmacology, 18, 449–459. doi: 10.1089/cap.2008.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth RM, Isquith PK, & Gioia GA (2015). Behavior Rating Inventory of Executive Function-Adult version (BRIEF-A). Psychological Assessment Resources. [Google Scholar]
- Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriquez L, Sanchez F, Derefinko K, Helseth S, & Ward A (2016). Parent-teen behavior therapy + motivational interviewing for adolescents with ADHD. Journal of Consulting and Clinical Psychology, 84, 699–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Morley C, Rodriguez L, Coxe SJ, Evans SW, Morsink S, & Torres F (2020). A peer-delivered intervention for high school students with impairing ADHD symptoms. School Psychology Review, 49, 275–290. [Google Scholar]
- Sprich SE, Safren SA, Finkelstein D, Remmert JE, & Hammerness P (2016). A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. Journal of Child Psychology and Psychiatry, 57, 1218–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinto V (1996). Reconstructing the first year of college. Planning for Higher Education, 25, 1–6. [Google Scholar]
- Torpey E (2018, April). Measuring the value of education. Career Outlook, US Bureau of Labor Statistics [Google Scholar]
- U.S. Department of Labor, Bureau of Labor Statistics. (2018). Unemployment rates and earnings by educational attainment, 2017. Retrieved from: https://www.bls.gov/emp/chart-unemployment-earnings-education.htm
- Weinstein CE, & Palmer DR (2002). Learning and Study Strategies Inventory-second edition: User’s manual. H&H Publishing Company, Inc. [Google Scholar]
- Weyandt LL, DuPaul GJ, Verdi G, Rossi JS, Swentosky A, Vilardo BS, O’Dell S, & Carson KS (2013). The performance of college students with and without ADHD: Neuropsychological, academic, and psychosocial functioning. Journal of Psychopathology and Behavioral Assessment, 35, 421–435. doi: 10.1007/s10862-013-9351-8 [DOI] [Google Scholar]
- Weyandt LL, Oster D, Gudmundsdottir G, DuPaul GJ, & Anastopoulos AD (2017). Neuropsychological functioning in college students with and without ADHD. Neuropsychology, 31, 160–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


