Abstract
The ongoing pandemic of COVID-19 is a threat to various routine healthcare services. India’s routine immunization (RI) campaign is one of largest ever known. In this review, we discuss the magnitude of disruption of RI activities due to COVID-19 pandemic, various causes of it and recommend ways to reduce the disruptions. Prominent literature databases were searched till April 30, 2021 for articles reporting disruptions of RI due to COVID-19. One study from India and numerous from outside India reported significant declines in the vaccine coverage rates during the lockdown period, which ranged from March 2020 till August 2020 in different regions of the world. Some reported disruptions for all vaccines, while a few reported sparing of birth doses. Shortage of healthcare workers due for them being diverted to patient care services and their reduced movement due to lockdowns and non-availability of public transport were prominent causes. Parents avoided RI sessions as they feared them or their children getting infected. They also faced travel restrictions, just like the healthcare workers. Children of school entry age and those from poorer socio-demographic profile appeared to miss the doses more frequently. Ministry of Health and Family Welfare, India has issued guidelines for conducting fixed and outreach RI sessions while following COVID-appropriate behavior. Promptly identifying missed out children and scheduling catch-up sessions is required to sustain the gains made over the decades by the immunization program of India.
Keywords: COVID-19 pandemic, developing countries, routine immunization, vaccine policy, vaccine-preventable diseases
Introduction
India’s path towards achieving Sustainable Development Goals (SDG) would include reduction in the incidence of various vaccine preventable diseases (VPDs).[1] Universal Immunization Program of India, one of the largest public health programs in the world, provides free vaccination against 12 VPDs, 11 nationally [Diphtheria, Pertussis, Tetanus, Polio, Measles, Rubella, severe form of Childhood Tuberculosis, Hepatitis B and Meningitis and Pneumonia caused by Hemophilus Influenza type B, Rota Virus Diarrhea, Pneumonia (PCV under expansion)] and one sub-nationally (Japanese Encephalitis- for endemic areas). As one of the most effective public health interventions, every US$1 spent on immunization returned US$ 26 from savings on healthcare costs and expenses from illness.[2]
The World Health Organization (WHO) on March 11, 2020, declared the novel coronavirus (COVID-19) outbreak a global pandemic. India reported its first case on January 30, 2020 and first confirmed death from COVID on March 12, 2020. After a ‘one-day janta curfew’ on March 22, 2020, India went into nationwide lockdown on March 25, 2020, which went till April 14, 2020 and extended till May 17. The National Health Mission’s Health Management Information System (HMIS) reported that just after a week of implementing lockdown routine health services were severely affected, based on month-on-month comparison with previous year’s data.[3] India’s routine immunization (RI) campaign was at risk as well. After years of infrastructure building, organizational work, social marketing, garnering financial support and goodwill of the people of India, all was in jeopardy. Childhood vaccines are time sensitive and thus even a small gap in the vaccination coverage of millions of children will put the gains reaped by decades of work in danger. Indicator 19 of SDG 3.2 measures percent of children receiving full immunization (as recommended by national vaccination schedules). Thus, disruption of RI would directly impact India’s ability to achieve SDGs. Some experts argued that physical distancing measures may decrease the transmission of some infectious diseases like measles.[4] However, there is a risk of resurgence in unimmunized children once normalcy returns. In this review, we discuss the magnitude of disruption of RI activities, various aspects of it and what could be the way ahead.
Relevance of this Review
On May 5, 2021 India reported 4,12,618 new cases of COVID-19 in 24 hours.[5] With daily rising cases, similar disruptions will happen again, as witnessed in 2020. In our compelling need to focus on COVID-19, health authorities may lose sight of other existing VPDs. Thus, it is believed that knowledge from this article can help the policy makers in determining the type of response required in such situations.
Objectives
In this review, we aim to present the magnitude of RI disruptions caused by COVID in India and developing countries in general. We also want to highlight the reasons behind these disruptions and recommend ways in which these disruptions can be settled.
Methodology
Literature search was done in MEDLINE using Medical Subject Headings terms like ‘pandemics’, coronavirus’, ‘COVID-19’, ‘immunization’ and ‘vaccination’. Other databases searched were Cochrane, EMBASE, CINAHL, Scopus and Google Scholar. All searches were done in English language till April 30, 2021. References of the selected articles were searched as well. The authors did not include articles about adult immunization. Since it was a narrative review, ethical approval was not required.
Findings and Discussion
Impact of COVID-19 pandemic on routine immunization services in India
According to media reports, schools remain shut in many parts of India even after the unlocking process started in July 2020.[6] Anganwadis and schools for children lower than fourth grade remained shut throughout India since the start of pandemic. This is worrisome as these places are important points for imparting many health services to young children, including immunizations. In addition, lockdown in the main urban areas has triggered a mass migration of people, especially those living in informal settlements and slums, back to their hometowns and other rural areas.[7] Due to this, their children most likely missed their scheduled immunizations, resulting in reduced coverage. Not only this, a large number of new migrated residents to these rural areas would put a strain on the existing health facilities.
Agrawal et al.[8] analyzed the impact of COVID-19 pandemic on RI during the post lockdown period at a tertiary care center of Meerut, Uttar Pradesh. They found that the number of beneficiaries receiving RI during August and December 2020 were significantly lower as compared to February 2020. The least affected were the birth doses. The authors reported that the first booster of DPT and second dose of MR was the worst affected. Another set of data coming from Rajasthan, India reported significant lapses in the timeliness of administration of RI doses.[9] Subgroup analysis found that children in less educated and poorer households already had lower pre-COVID levels of immunization and were subject to greater declines in RI coverage during and after lockdown. The authors analyzed government’s administrative data obtained from HMIS and commented that increase in post-lockdown numbers may not reflect an increased RI coverage but may be due to seasonal fluctuations or migration of people. Shet et al.[10] found a 50% decline in vaccination services in the month of June 2020 as reported by 83% of the 424 surveyed pediatricians. The authors also reported that 76% of the pediatricians expressed concerns about the gap in the coverage of RI.
Impact of COVID-19 pandemic on routine immunization services in other countries
The WHO’s Strategic Advisory Group of Experts on Immunization issued a broader call, recommending that all preventive mass vaccination campaigns for other diseases be postponed because of social distancing issues.[11] The Global Polio Eradication Initiative recommended suspending polio vaccination campaigns until the second half of 2020. Harris et al.[12] reported disruptions to RI in 95% of the South East Asia Region countries. A WHO survey found that outreach services were affected in 70% of the 91 countries surveyed and facility based disruptions in 61%.[13] Following the suspension of RI activities, there has been a new polio outbreak of vaccine-derived polio virus in Niger.[14] In Pakistan and Afghanistan, wild poliovirus Type 1 have been reported, and cases of Type 2 poliovirus, mutated from the oral vaccine, have appeared in Chad, Ethiopia, Ghana, and Pakistan.[15] On June 19, 2020, 54 cases of polio were detected, of which 42 were from Pakistan and rest were from Afghanistan.[16] Diphtheria has recently resurged in countries like Venezuela, Pakistan, Nepal, Bangladesh, and Yemen where conflict and/or population displacement have significantly stressed public health systems.[17] Cholera is now present in Bangladesh, Cameroon, Mozambique, South Sudan, and Yemen.[17]
The WHO, United Nations International Children’s Emergency Fund (UNICEF), and Global Alliance for Vaccines and Immunisation (GAVI), the Vaccine Alliance have reported that RI programs have been substantially disrupted in at least 68 countries, affecting around 80 million children.[18] Of the 129 countries in which data were available, more than half reported moderate to severe disruptions, or total suspension of vaccination services during March to April 2020.[19] The Vaccine Tracking System of the US Centers for Disease Control and Prevention (CDC) shows that US health care providers ordered about quarter a million fewer doses of Vaccines for Children (VFC) Program-funded measles-containing vaccines and about 2.5 million fewer doses of non-influenza vaccines from mid-March to mid-April, 2020 compared to the same period in 2019.[20] Chandir et al.[21] analyzed immunization records from the Sindh province of Pakistan and reported a 52% decline in mean daily beneficiaries vaccinated. During lockdown, over 8000 children were missing their vaccinations. This is worrisome as Pakistan is endemic to wild polio virus and circulating vaccine derived polio virus (VDPV). All Supplementary Immunization Activities (SIA), the cornerstone of the polio eradication strategy, were suspended after the last scheduled SIA on March 24, 2020 to deal with the COVID-19 crises.[22] Another report from Pakistan reported higher measles cases from January 2020 till March 2020 as compared to the same period in the previous year.[23] Mansour and colleagues assessed the impact of COVID-19 on RI services in Lebanon. By interviewing public and private pediatricians, the authors reported that greatest decline was in the utilization of oral polio vaccine (OPV), hepatitis A, followed by measles and pneumococcal conjugate vaccine (PCV)- containing vaccines. During the first 3 weeks of the lockdown, the number of measles mumps rubella (MMR) vaccines delivered in England fell by 20%. In New York City, vaccinations have been down 63% overall, and by 91% for children older than two years of age.[24]
The details of reported disruptions to RI across the globe are described in Table 1.
Table 1.
Reduced vaccine coverage due to COVID-19 in different parts of the world
| Authors | Site | Comparison | Vaccine of concern | Vaccine coverage (as number of beneficiaries) |
|---|---|---|---|---|
| Agrawal et al.[8] | India | February 2020 vs August 2020 | Birth dose-BCG, OPV, Hep B | Decline of 27.9% |
| MR-1 | Decline of 68.42% | |||
| MR-2 | Decline of 84.3% | |||
| DPT b2 | Decline of 57.4% | |||
| Chandir et al.[21] | Pakistan | Baseline (September 23, 2019 to March 22, 2020) vs Lockdown (March 23, 2020 to May 9, 2020) | BCG | Decline of 56.6% |
| OPV-0 | Decline of 51.6% | |||
| Penta-1 | Decline of 56.4% | |||
| OPV-1 | Decline of 56.2% | |||
| PCV-1 | Decline of 56.4% | |||
| Rota-1 | Decline of 56.1% | |||
| Penta-2 | Decline of 51% | |||
| OPV-2 | Decline of 50.7% | |||
| PCV-2 | Decline of 51.1% | |||
| Rota-2 | Decline of 50.7% | |||
| Penta-3 | Decline of 49.5% | |||
| OPV-3 | Decline of 49.2% | |||
| IPV | Decline of 51.6% | |||
| PCV-3 | Decline of 49.7% | |||
| Measles-1 | Decline of 47.4% | |||
| Measles-2 | Decline of 48.2% | |||
| Mansour et al.[25] | Lebanon | October 2019 vs March 2020 | OPV | Decline of 28% |
| IPV | Decline of 17% | |||
| Measles | Decline of 38% | |||
| Penta | Decline of 14% | |||
| PCV13 | Decline of 14% | |||
| Bramer et al.[26] | United States | Baseline (May 2016 to May 2019) vs May 2020 | Recommended vaccines for children aged ≤24 months | Decline of 15.5% |
| Buonsenso et al.[27] | Sierra Leone | Baseline (March 1, 2019 to April 26, 2019) vs Lockdown (March 1, 2020 to April 26, 2020) | BCG | Decline of 52.7% |
| OPV-0 | Decline of 52.7% | |||
| OPV-1 | Decline of 70.7% | |||
| Penta-1 | Decline of 70.7% | |||
| PCV-1 | Decline of 70.7% | |||
| Rota-1 | Decline of 70.7% | |||
| OPV-2 | Decline of 78.9% | |||
| Penta-2 | Decline of 78.9% | |||
| PCV-2 | Decline of 78.9% | |||
| Rota-2 | Decline of 78.9% | |||
| Penta-3 | Decline of 77.6% | |||
| PCV-3 | Decline of 77.6% | |||
| IPV | Decline of 77.6% | |||
| Measles | Decline of 65.6% | |||
| Langdon-Embry et al.[28] | Unites States | April 5 to 11, 2019 vs April 5 to 11, 2020 | Recommended vaccines for children aged <24 months | Decline of 62% |
| McDonald et al.[29] | Canada | Week 1 to 17, 2019 vs Week 1 to 17, 2020 | Hexavalent | Decline of 3.5% |
| MMR-1 | Decline of 3.7% | |||
| Harris et al.[12] | SEAR/WPR region | 2019 vs 2020 | DPT | Decline of 42% |
| OPV-infancy | Decline of 79% | |||
| OPV-school entry | Decline of 4% | |||
| IPV | Decline of 29% | |||
| Measles | Decline of 9% | |||
| Tessier et al.[30] | England | First four weeks 2019 vs first four weeks 2020 | Hexvalent-1 | Decline of 11.6% |
| MMR-1 | Decline of 7.5% | |||
| First four weeks 2020 vs first four weeks 2021 | Hexvalent-1 | Decline of 14.2% | ||
| MMR-1 | Decline of 19.3% |
BCG: Bacillus Calmette-Guérin; OPV: Oral polio vaccine; Hep: Hepatitis; MR: Measles Rubella vaccine; DPT: Diphtheria, Pertussis Tetanus vaccine; b: booster; PCV: pneumococcal conjugate vaccine; Penta: Pentavalent vaccine; Rota: Rotavirus vaccine; IPV: inactivate poliovirus vaccine; MMR: measles, mumps, and rubella vaccine
Causes of disruption [Figure 1]
Figure 1.
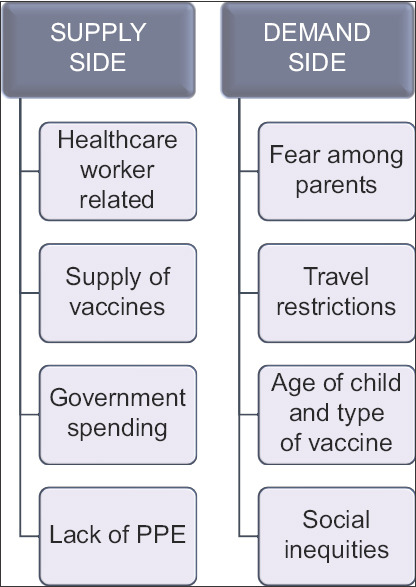
Causes of disruption to routine immunization activities
Supply side issues
Healthcare workers related
Healthcare services in India are stretched and directed to other priorities like contact tracing, care of COVID-patients and now COVID vaccination campaign. In addition, HCW have fallen ill or died as a result of COVID infection. Moreover, there have been reports of misdirected acts of violence against them as well.[31] As a result, there are higher levels of anxiety, depression, stress, fear, anger, and insomnia has been observed among HCW during the pandemic.[32] Furthermore, public transport was also not available and increase in commuting costs made it difficult for millions of HCWs to commute from home to work.
Supply chain of vaccines
Domestic as well international transport of vaccines was affected during and after lockdown, as there were flight cancellations, trade restrictions and even border closures by some countries. Vaccine stock-outs was a genuine concern as the manufacturing units and supply chain was disrupted.[33]
Government spending
When COVID was rapidly spreading in March and April 2020, the Government was struggling to provide personal protective equipment (PPE) kits, ventilators and other medicines required to manage piles of patients admitting to hospitals.
Lack of personal protective equipment (PPE)
This was especially true during the early weeks of pandemic. Adapting to work long hours with PPE has been another challenge for the HCWs.
Demand side issues
Fear among parents
Hesitancy in receiving vaccines for a variety of reasons is not new and refusal has become a serious concern in recent years.[34] After the start of pandemic, parents feared them or their children getting infected while visiting a healthcare facility for RI. A dataset from Rajasthan showed that of the 2081 households surveyed, parents’ fear of getting COVID-19 was the most common cause of RI disruption (20%), while 15% reported cancellation of immunization sessions and 10% reported travel restrictions. This coupled fear of contracting COVID-19 in addition to pre-existing hesitancy made things worse.
Travel restriction for general public
Public transport was not available or safe without masks to travel during the pandemic. This discouraged the parents from bringing their children for RI. This along with complete halt of outreach activities led to decreased RI coverage.
Age of the child
Birth cohort was relatively spared as access to vaccines was maintained in institutional deliveries. As a result, no significant gap was observed in birth doses. However, infants and children of school entry age were the most affected.[26]
Mistrust in health facilities
During these testing times, HCWs were hesitant to treat patients due to the lack of PPE. This led to distress in physicians and mistrust among patients.
Social inequities
Social factors have always affected the role out of health services. Data from Karachi, Pakistan showed that slums and densely packed settlements were worst affected.[21]
Problems with outreach sessions
Social distancing recommendations made it very difficult to conduct not only outreach activities but fixed hospital based sessions as well.
Type of vaccine
Problem with multi-dose vial is that vaccinators refrain from opening them when very few beneficiaries arrive. It is especially true for those vaccines without an open-vial policy (example BCG, MR and JE vaccines).
Way forward
Mathematical modelling from the London School of Hygiene and Tropical Medicine suggests that for each excess COVID-19 death due to an infection acquired during the vaccination visit (predominantly among elderly household members), around 29 to 347 future child deaths could be prevented with sustained RI.[35] For this reason, ensuring the continuation of RI is vitally important for all countries, particularly since it is not known how long the pandemic will last.
Ministry of Health and Family Welfare (MoHFW), India released a guidance document regarding RI services during the pandemic.[36] The guidance suggests that in the containment and buffer zones, birth doses will continue, while health facility based RI sessions and outreach sessions will discontinue. In areas beyond the buffer zone, birth doses and health facility based RI sessions should continue, while outreach sessions should be discontinued. For the outreach sessions, a staggered approach to be employed to avoid crowding. It is suggested that these decisions are to be taken by the district administration. While these guidelines are helpful, it is suggested that district health officials generate area specific lists of children who missed their vaccinations during the pandemic. Chandir and colleagues demonstrated how this can be done with the help of electronic data.[21] Quickly identifying cohorts of susceptible children of under-five age group is needed for which catch up vaccination can be done proactively. Intensified Mission Indradhanush (IMI) 3.0 was rolled out on 8 Feb, 2021 to sustain the gains made RI and previous Mission Indradhanush campaigns and to close the immunization gaps that might have emerged due to the ongoing COVID-19 pandemic.[37]
At the time of writing of this article, the two COVID-vaccines in India, Covishield and Covaxin, are not approved for children less than 18 years. However, their parents who will receive the vaccine should be provided with targeted messages and reminders for childhood RI. Here, primary care physicians can play an important role. They are usually the first point of contact for majority of the patients, especially at a time when general masses would want to avoid crowded hospitals for minor ailments. Their office visits can be used to educate parents about the importance of minimizing gaps in RI and allay fears among them. A state-wide survey from Canada reported greater disruption of RI in a pediatrician’s office as compared to that of a primary care physician.[38] This suggests greater responsibility and a bigger role for primary care physicians and family medicine practitioners in restoring RI services during a pandemic. In addition, linking RI campaigns with the COVID-19 vaccine sessions, could prove beneficial. Based on the published literature and above discussion, some of our recommendations are listed in Table 2.
Table 2.
Recommendations to reduce disruptions in routine immunization campaign due to COVID-19 pandemic
| Routine Immunization should be continued as much as possible while following the guidelines issued by the Ministry of Health and Family Welfare (MoHFW), India. |
| Real-time data would be helpful in identifying missed out children. In addition, it can help monitor vaccinators' attendance as well. |
| Reinforcing and maintaining surveillance of vaccine preventable diseases surveillance. |
| Home based or drive-through RI services could be implemented. |
| Explaining the importance of vaccines and risk of missing out on RI and conducting RI sessions following COVID appropriate behavior can help reduce apprehensions among parents. Virtual engagement with the parents can help alleviate some of their fears. |
| Using this pandemic as a teaching moment, the communication skills of vaccinators can be refreshed. |
| Development of innovative digital tools to track migratory population. |
| Supplies to conduct a RI session need to be ensured like adequate vaccines, logistics, personal protective equipment etc. |
| Filling out any vacancies in RI related services can help strengthen the immunization program. Additional contractual staff can be hired if needed. |
| Collaboration and capacity building of private health sector and non-governmental organizations may help in achieving the objective. |
The dynamic and evolving nature of the pandemic makes the assessment of the daily situation difficult. However, to the best of our knowledge, this is the latest account of RI during COVID -19 pandemic.
Conclusion
COVID-19 pandemic represents one of the most challenging public health crisis of this generation. COVID-19 vaccination program commenced in India from January 16, 2021. One of the most important ways to control the pandemic is to vaccinate the populations as quickly as possible. Strengthening the RI services will give strength to the COVID vaccination program as well. While governments, healthcare professionals and researchers are rightly focusing on the immediate response to the COVID-19 pandemic, we must ensure that sufficient resource and consideration is given to delivery of routine vaccinations. Anticipating similar pandemic/disaster in future, an emergency preparedness plan may be prepared to avoid such disruption to RI program.
Key messages
Routine immunization coverage rates have declined globally during the first wave of COVID pandemic (March to August 2020).
Routine immunization should continue as much as possible, while following COVID appropriate behavior. Decision to conduct outreach immunization sessions should be made by local health authorities after assessing the ground situation.
Identifying missed children and doing catch-up vaccination at the earliest in these children should be priority.
Primary care physicians should utilize every outpatient visit to educate parents about the importance of RI and allay fears among them. The current review discusses various causes and suggests recommendations for primary care physicians to minimize RI disruptions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Decouttere C, De Boeck K, Vandaele N. Working Papers of Department of Decision Sciences and Information Management. Leuven: 2020. Advancing sustainable development goals through immunization:A literature review; p. 654671. [Google Scholar]
- 2.Restrepo-Méndez MC, Barros AJ, Requejo J, Durán P, Serpa LA, Franca GV, et al. Progress in reducing inequalities in reproductive, maternal, newborn,'and child health in Latin America and the Caribbean:An unfinished agenda. Rev Panam Salud Pública. 2015;38:9–16. [PubMed] [Google Scholar]
- 3.Health Management Information System Standard Reports [online], 2021. [Last accessed on 2021 Sep 7]. Available from: https://hmis.nhp.gov.in/downloadfile?filepath=publications/Hmis-Report/State-wise_four%20time%20point%20cumulative%20figure_April%20-June%202020.pdf .
- 4.Hungerford D, Cunliffe N. Coronavirus disease (COVID-19) –impact on vaccine preventable diseases. Euro Surveill. 2020;25:2000756. doi: 10.2807/1560-7917.ES.2020.25.18.2000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Total coronavirus cases in India [online], 2021. [Last accessed on 2021 May 06]. Available from: https://www.worldometers.info/coronavirus/country/india/#graph-cases-daily .
- 6.Unlock 4:Schools, colleges to remain shut till 30 September [online], 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.livemint.com/news/india/unlock-4-0-schools-colleges-to-remain-shut-till-30-september-11598713639432.html .
- 7.Coronavirus lockdown sparks mass migration in India [online], 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.bbc.com/news/av/world-asia-india-52096729 .
- 8.Agrawal AD, Gupta G, Bhasin A, Singh A, Rathi A. Impact of COVID-19 pandemic on routine childhood immunisation services post lockdown in a tertiary care centre in Meerut district of western U.P. Int J Contemp Pediatr. 2021;8:219–24. [Google Scholar]
- 9.Jain R, Chopra A, Falezan C, Patel M, Dupas P. COVID-19 related immunization disruptions in Rajasthan, India:A retrospective observational study. medRxiv. 2020 doi: 10.1016/j.vaccine.2021.06.022. doi:10.1101/2020.12.04.20244327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shet A, Dhaliwal B, Banerjee P, Carr K, DeLuca A, Britto C, et al. COVID-19-related disruptions to routine vaccination services in India:Perspectives from pediatricians. medRxiv. 2021 doi: 10.1136/bmjpo-2021-001060. doi:10.1101/2021.01.25.21250040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Covid-19 strategic update [online], 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf .
- 12.Harris RC, Chen Y, Côte P, Ardillon A, Nievera MC, Ong-Lim A, et al. Impact of COVID-19 on routine immunisation in South-East Asia and Western Pacific:Disruptions and solutions. Lancet Reg Health-West Pac. 2021:100140. doi: 10.1016/j.lanwpc.2021.100140. doi:10.1016/j.lanwpc. 2021.100140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Pulse survey on continuity of essential health services during the COVID-19 pandemic; 2020. Interim report [online] 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
- 14.Niger reports new polio outbreak [online], 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.afro.who.int/news/niger-reports-new-polio-outbreak .
- 15.Polio Global Eradication Initiative website, Polio this week as of 31 March 2021 [online]. 2021. [Last accessed on 2021 Sep 7]. Available from: https://reliefweb.int/report/pakistan/polio-week-31-march-2021 .
- 16.Chard AN, Datta SD, Tallis G, Burns CC, Wassilak SG, Vertefeuille JF, et al. Progress toward polio eradication—worldwide, January 2018–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:784–9. doi: 10.15585/mmwr.mm6925a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffman J, Maclean R. Slowing the Coronavirus is speeding the spread of other diseases. New York Times [online] 2020. [Last accessed on 2021 Apr 05]. Available from: https://www.nytimes.com/2020/06/14/health/coronavirus-vaccines- measles.html .
- 18.At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn Gavi, WHO and UNICEF [online]; 2020. [Last accessed 29. on 2021 Sep 7]. Available from: https://www.who.int/news/item/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef .
- 19.Roberts L. Global polio eradication falters in the final stretch. Science. 2020;367:14–5. doi: 10.1126/science.367.6473.14. [DOI] [PubMed] [Google Scholar]
- 20.Santoli JM, Lindley MC, DeSilva MB, Kharbanda EO, Daley MF, Galloway L, et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration —United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:591–3. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 21.Chandir S, Siddiqi DA, Setayesh H, Khan AJ. Impact of COVID-19 lockdown on routine immunisation in Karachi, Pakistan. Lancet Glob Health. 2020;8:e1118–20. doi: 10.1016/S2214-109X(20)30290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.EOC Sindh. Postponement of fIPV Campaign, Karachi, March 2020. March 17, 2020. [Google Scholar]
- 23.Rana MS, Usman M, Alam MM, Mere MO, Ikram A, Zaidi SSZ, et al. Impact of COVID-19 pandemic on Measles surveillance in Pakistan. J Infect. 2021;82:414–51. doi: 10.1016/j.jinf.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernandez M. Vaccinations are plummeting amid coronavirus pandemic [online] 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.axios.com/children-coronavirus-vaccinations-d2e86bd2-034e-4cc9-82b9-156fb9621f4f.html .
- 25.Mansour Z, Arab J, Said R, Rady A, Hamadeh R, Gerbaka B, et al. Impact of COVID-19 pandemic on the utilization of routine immunization services in Lebanon. PLoS One. 2021;16:e0246951. doi: 10.1371/journal.pone.0246951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bramer CA, Kimmins LM, Swanson R, Kuo J, Vranesich P, Jacques-Carroll LA, et al. Decline in child vaccination coverage during the COVID-19 pandemic—Michigan Care Improvement Registry, May 2016-May 2020. Am J Transplant. 2020;20:1930–1. doi: 10.1111/ajt.16112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buonsenso D, Cinicola B, Kallon MN, Iodice F. Child healthcare and immunizations in sub-Saharan Africa during the COVID-19 pandemic. Front Pediatr. 2020;8:517. doi: 10.3389/fped.2020.00517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Langdon-Embry M, Papadouka V, Cheng I, Almashhadani M, Ternier A, Zucker JR. Notes from the field:Rebound in routine childhood vaccine administration following decline during the COVID-19 pandemic—New York City, March 1–June 27, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:999–1001. doi: 10.15585/mmwr.mm6930a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDonald HI, Tessier E, White JM, Woodruff M, Knowles C, Bates C, et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. 2020;25:2000848. doi: 10.2807/1560-7917.ES.2020.25.19.2000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tessier E, Rai Y, White J, Roy P, Ramsay M. Impact of COVID-19 on childhood vaccination counts to week 4 in 2021, and vaccine coverage to December 2020 in England:Interim analyses:Health Protection Report. 2021;15 [Google Scholar]
- 31.Iyengar KP, Jain VK, Vaishya R. Current situation with doctors and healthcare workers during COVID-19 pandemic in India. Postgrad Med J. 2020 doi: 10.1136/postgradmedj-2020-138496. doi:10.1136/postgradmedj-2020-138496. [DOI] [PubMed] [Google Scholar]
- 32.Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers:A scoping review. Int J Emerg Med. 2020;13:40–8. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Unicef. Impact of COVID-19 on vaccine supplies. UNICEF [online] 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.unicef.org/supply/stories/impact-covid-19-vaccine-supplies .
- 34.Hotez PJ, Nuzhath T, Colwell B. Combating vaccine hesitancy and other 21st century social determinants in the global fight against measles. Curr Opin Virol. 2020;41:1–7. doi: 10.1016/j.coviro.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Abbas K, Procter SR, van Zandvoort K, Clark A, Funk S, Mengistu T, et al. Routine childhood immunisation during the COVID-19 pandemic in Africa:A benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. 2020;8:e1264–72. doi: 10.1016/S2214-109X(20)30308-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Immunization services during and post-COVID 19. MoHFW website [online] 2020. [Last accessed on 2021 Sep 7]. Available from: https://www.mohfw.gov.in/pdf/3ImmunizationServicesduringCOVIDOutbreakSummary150520202.pdf .
- 37.Intensified Mission Indradhanush 3.0 website [online], 2020. [Last accessed on 2021 Sep 7]. Available from: https://imi3.nhp.gov.in .
- 38.Piché-Renaud PP, Ji C, Farrar DS, Friedman JN, Science M, Kitai I, et al. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario, Canada. Vaccine. 2021;39:4373–82. doi: 10.1016/j.vaccine.2021.05.094. [DOI] [PMC free article] [PubMed] [Google Scholar]


