Abstract
Background:
Even though vitamin A (Vit A) is one of the essential vitamins required for bone growth and development, it is still uncertain whether its effect on bone mineral density (BMD) is beneficial or harmful.
Aim:
To assess Vit A’s effect and its derivatives on BMD and the risk of developing osteoporosis.
Data sources:
PubMed, Cochrane Library, Science Direct, Embase, and Google Scholar were searched in February 2019 and updated in November 2020.
Methods:
Conducted following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.
Results:
A total of 13 studies were included in this report out of 9,124 citations. Five of them were cross-sectional studies, and nine were cohort studies. Three out of five cross-sectional studies showed an increase in BMD, while two showed a decrease in BMD. Four out of eight cohort studies found an increase in BMD; two studies found no association between vitamin A level and BMD; one showed an inverse U-shape association of vitamin A with BMD, suggesting that both the increase or decrease levels of vitamin A affect BMD, while only one study showed a decrease in BMD.
Conclusion:
Although most of the included studies showed a favorable effect of Vit A on BMD, Vit A’s role or its derivatives on BMD change remains unclear.
Keywords: Bone mineral density (BMD), osteoporosis, Vit A, vitamin A derivatives, vitamin A supplements vitamin
Introduction
Vitamin A (Vit A) plays a role in bone growth and development,[1] influencing osteoclast and osteoblast. It is one of the fat-soluble vitamins and an antioxidant. It is an essential nutrient required to maintain many biological activities.[2] The daily required need for Vit A for adults is 900 micro g/d in males and 700 micro g/d in females.[3] Our diet is found in two forms, either as retinal esterase/retinol, which is found in eggs, milk, fortified cereals, and liver or as carotenoids/beta-carotene, which is found in vegetables. It is also found in over-the-counter multivitamins and some medications as Isotretinoin.[2]
There is a debate over whether increased consumption of Vit A is linked to skeletal fragility promotion. Since the 1920s, this relationship was demonstrated in different clinical animal and observational human studies.[3] M. Mata-Granados found that women with higher retinol levels were more at risk of osteoporosis than women with low retinol levels.[4]
On the other hand, some studies have shown Vit A to be beneficial for bone health by promoting osteoblasts differentiation and bone formation.[3] In an Italian case-control study of 75 women with osteoporosis and another 75 women without osteoporosis, a positive correlation between femoral neck BMD and plasma retinol level has been found.[5]
Other studies showed no link between increased Vit A intake and osteoporosis or fractures.
A recent meta-analysis of the prospective cohort studies about dietary intake of vitamins: A, C, E and the subsequent fracture risk at various sites found that increased Vit A intake did not increase the risk.[6] On the other hand, a 2017 systematic review and meta-analysis suggested that Vit A intake and level may differentially influence the risks of total and hip fractures.[7]
Since the significance of knowledge about Vit A’s role on bone health in dealing with patients with increased risk of osteoporosis and fractures in primary care and the current knowledge about its role on bone health is inconclusive, we aim in this study to assess the evidence of the effect of Vit A on BMD and the risk of developing osteoporosis.
Method
This systematic review was conducted following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines to explore the association of vitamin A use and BMD change.[8]
Study strategy
We performed a comprehensive literature search in February 2019 and an updated one in November 2020. The searched databases were PubMed, Cochrane Library, Science Direct, Embase, and Google Scholar using Vit A, Retinol, Fracture, Osteoporosis, BMD, bone health as the keywords. All published articles (cohort, case-control, cross-sectional, and randomized control trials [RCTs]) discussing the influence of oral Vit A or its derivatives on bone tissue health were extracted. Unpublished literature was searched by looking into the clinical trial registry.[9]
Inclusion and exclusion criteria
All studies fulfilled the inclusion criteria: (1) Population: Adolescents and adults, males and females. Animal studies were excluded (2) Exposure: Circulating levels of Vit A and retinol in the blood (either from supplements or diet), but all treatment forms were excluded (3) Outcomes: BMD and the osteoporosis risks were detected by radiological evidence. (4) Study type: Cross-sectional, case-control, cohort studies and RCTs (5) Timing: Studies published after 2000. All languages were included.
Study selection
Two reviewers (SR and QK) separately scanned the titles and abstracts, and when required, the full text was recovered and reviewed to identify all the relevant articles. A third author (GR) resolved the disagreements.
Risk of bias and quality assessment
The Newcastle–Ottawa scale (NOS) is a scale used for evaluating the quality of nonrandomized studies involved in a systematic review and/or meta-analyses.[10,11] Three factors were evaluated for scoring the quality of the studies, selection, comparability and outcome. The studies’ quality was graded by awarding stars in each subset with a total score of 9. The studies that scored seven or more were considered high quality. In contrast, those that scored lower than seven were considered low quality.[10,11] QK and SR, two independent reviewers, assessed the quality of the included studies using NOS. A third reviewer resolved the disagreements.
Data extraction
For the selected studies, we used Covidence software,[12] a systematic review production tool for the title, abstract and full-text screening.[13] After searching, using the keywords, two reviewers (SR, QK) extracted the data separately using pretested data extraction form; any conflicts were resolved by a third reviewer (GR). The extracted information included author, year, study design, setting, patient’s age, sample size, confounders, and exposure. The outcomes including osteoporosis (a common skeletal disorder characterized by decreased bone density, compromised bone strength, and increased fracture risk[14]) were based on the BMD measures for the two groups, exposed and nonexposed.
Dealing with missing data
The mean, P values, standard deviations (SD) of the mean difference were missing in the selected studies. Consequently, we contacted the authors of each study with no response received, so we could not pool the results. The present study was approved after review under the ethical standards by King Abdullah International Medical Research Center (KAIMRK) IRB Committee on Feb 3, 2019 (research number RC19/024/R).
Results
Literature search
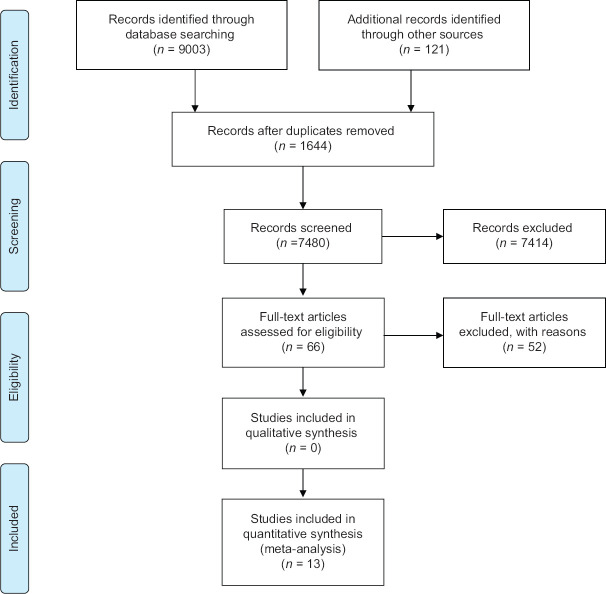
A total of 9,124 citations were identified by searching the databases and manual search of references. After screening the titles and abstracts, 1,644 duplicates and 7,414 irrelevant studies were removed. Sixty-six studies met our criteria; after full article reviews and assessment for eligibility, 53 studies were excluded. A total of 14 studies are included in this report. Figure 1 shows a PRISMA flowchart depicting the process of selection and exclusion.
Figure 1.
A PRISMA flowchart depicting the process of selection and exclusion (http://prisma-statement.org/prismastatement/flowdiagram).
Quality of evidence
The overall quality of evidence on the association between Vit A and its derivatives was moderate and high. Most studies were graded seven points or above on the nine-point Newcastle–Ottawa scale for quality. Only two studies had lower grades.[14,15]
Study characteristics
The 14 included studies were a mixture of cross-sectional and cohort studies, which reported the association between Vit A or its derivatives’ use and change in BMD, and these were in English. The studies were conducted in the USA, Brazil, Denmark, Korea, Spain, Norway, China, Thailand, and the Netherlands. Overall, the data for 71,078 participants, including adults, age groups ranging between 20 and 80, were used in this systematic review. Half of the included studies used both genders; the other half included females only, three of which were postmenopausal. The enrolled articles either study the effect of Vit A, retinol, or beta-carotene on BMD. The BMD change was measured by DXA. Most of the included studies’ results were adjusted for age, sex, and BMI [Table 1].[4,15,16,17,18,19,20,21,22,23,24,25,26]
Table 1.
Included study results
| Study first author, year (country) | study name | study design | Setting | Number of patients | Supplement, type, dose | Gender | results/outcomes | summary of the result | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Thais R. Silval, 2015 (brazil) | Associations between body composition and lifestyle (actors with bone mineral density according to time since menopause in women from Southern Brazil: a cross- sectional study | Cross- sectional | hospital baaed (Gynecologc al Endocrinol og yUnitl | 99 | distry vitamin A | Females | vitamin A appears tobt less consumed among women with lower bone mass, Considering all sample, vitamin A intake lower tban 700 meg a day, that is the recommended amount for dietary reference intakes | increase BMD |
| 2 | Sahni S, 2009(USA) | Inverse association ot carotenoid intakes with 4-y change in bone mineral density in elderly men and women: the Framingham Osteoporosis Study 2009 | Cohort | population based | 874 | a-carotene, b-carotene, b-cryptoxanthi n, lycopene, and luteinl zeaxanthin | both | Carotenoids showed protective role against 4 year BMD loss in older men and women. | increase BMD |
| 3 | C Ballew,2009 (USA) | High Serum Retlnyl Esters Are Not Associated with Reduced Bone Mineral Density in the Third National Health and Nutrition Examination Surrey, 1988-1994 | cohort | population based | 68 to 374 for men and from 597 to 602 for women | Retinyl Esters | both | no associations between physiological indicators of potential excess vitamin A intake and either BMD or osteopenia/osteoporosis | No association |
| 4 | Kristina L Penniston, 2006(USA) | Serum retinyl esters are not elevated in postmenopausal women with and without osteoporosis whose preformed vitamin A intakes are highl | Cohort | population based | GO | Retinol /Retinyl esters/NS Total VA /Retinyl esters | Females | Sentm retinyl esters were not elevated in these postmenopausal women despite intakes of total VA that were nearly two-fold the Recommended Dietary Allowance. How- ever, retinyl ester concentration (percentage of total VA) was marginally associated with osteoporosis | marginal decrease BMD |
| 5 | JOANNE H. E. PROMISLOW, 2002(USA) | Retlnol Intake and Bone Mineral Density In the Elderly: The Rancho Bernardo Study | Cohort | population based | 968 | RETINOL | Both | Both sexes, increasing retinal became negatFety associated with skeletal heal that in takes not far beyond the recommended daily allowance (RDA), intakes reached predominately by supplement users, inverse U" shaped association of retiool intake irkhEM) and bone maintenance observed in this cohort raises the concent that either loo lilk or too much retinol may adversely affect bone health | both increase or decrease lerelof Vitamin A affect BMD |
| 6 | L Reinmark, 2004 (Denmark) | No effect of vitamin A intake on bone mineral density and fracture risk in perimenopausal women | cohort | multicenterl c | 1869 | Females | no associations between intake of vitamin A and BMD of the femoral neck or lumbar spine | No association | |
| 7 | Nam-Seok Joo, 2015(Korea) | Serum Vitamin D and Bone Mineral Density: Analysis of the Korea National Health and Nutrition Examination Survey {KNHANES, 2008-2011) | Cross- sectional | population based | 6481 (2907 men and 3574 women) | Dietary vitamin A | both | Total hip and femoral neck BMD in men and lumbar spine BMD in women were both positively correlated with dietary vitamin A intake (Mean dietary vitamin A intakes were 737 and 600 pg RE (Retinol Equivalents) in men and women, respectively) in subjects with serum 25(OH)D >75 nmol/L. | increase BMD |
| 8 | J. M. Mala - Granados, 2013(Spain) | Vitamin D insufficiency together with high serum levels of vitamin A increases the risk for osteoporosis in postmenopausal women | Cross- secbonal | 232 | Females | Bone density measurements revealed that the risk of osteoporosis was -8 times higher in women with the highest retinol levels, as compared with women with the lowest retinol levels. | decrease BMD | ||
| 9 | Kristin Holvik, 2015(N orway) | No increase in risk of hip fracture at high serum retinol concentrations in community- dwelling older Norwegians: the Norwegian Epidemiologic Osteoporosis Studies | cohort | multicenter populatioin based study | 21774 | s-retinol | both | inverse association between s-retinol and risk of hip fracture, which was statistically significant in women but not in men | increase BMD |
| 10 | GO Chen, 2015(china) | Association of dietary consumption and serum levels of vitamin A and β-carotene with bone mineral density in Chinese adults β-carotene with bone mineral density in Chinese adults | Cohort | population based | 3154 | Serum levels of retinol and P-carotene | both | greater levels of serum retinol, β-carotene, and the β-carotene-lo-retinol ratio were associated with a higher BMD | increase BMD |
| 11 | Ml-Ja Choi,2007(Ko rea) | Relationship of nutrient intakes and bone mineral density of elderly women in | Cross- sectional | clinic center | 101 | Dietary Vitamin A | Females | Vitamin A, vitamin B1, and vitamin B2 intakes of participants in the osteoporosis group were lower than those in the normal group | increase BMD |
| 12 | Chupeerach C, 2011(Thialand) | Decreased retinol transport proteins in Thai post-menopausal women with osteoporosis | Cross- sectional | OBGYN clinic | 144 | Females | this study showed lower TTR, BMI and serum calcium in osteoporotic patients than controls. Malnutrition Is a risk factor for osteoporosis and TTR may be a marker for osteoporosis | decrease BMD | |
| 13 | de Jonge, 2015(Netherlands) | Dietary vitamin A intake and bone health In the elderly: the Rotterdam Study | cohort | Population based | 5288 | Ditary Intake | both | a plausible favourable relation between high vitamin A intake from the diet and fracture risk in overweight subjects, whereas the association between vitamin A and BMD is mainly explained by BMI. | Increase fracture |
Primary outcomes
Five of the included studies were cross-sectional to look for the relation between dietary Vit A and BMD. Four of those showed an increase in BMD, while one showed a decrease in BMD in all sites (lumbar spine, femoral neck, and trochanter).
The eight cohort studies used supplemental Vit A derivatives (retinol or retinal esterase or beta-carotene). Of them, four found an increase in the BMD with greater levels of supplementary Vit A. While only one study showed a decrease in BMD, two studies found no association between these levels and BMD; another one showed an inverse U-shape association of Vit A with BMD, suggesting that both increased or decreased levels of vitamin A affect BMD.
Discussion
This systematic review of observational studies that aimed to explore the association between Vit A and its effect on BMD revealed mixed results. Although most of the incorporated studies revealed a favorable effect, uncertainty remains over Vit A’s role or its derivatives on BMD change.
Most of the included studies have confirmed that a higher Vit A intake may increase BMD in all positions, which can be explained by the fact that Vit A acts as an antioxidant that reduces bone resorption by decreasing oxidative stress.[27] However, the exact underlying mechanism remains unclear as hypervitaminosis A is associated with adverse bone effects by disrupting the calcium-regulating hormone metabolism and decreasing vitamin D activity.[7]
A recent meta-analysis by Zhang et al.[7] found that a higher beta-carotene intake may increase total fracture risk. They also observed a positive influence of lower blood retinol levels on total and hip fracture risk. Additionally, a high intake of Vit A had slightly increased the risk of hip fracture but decreased total fracture risk in their results. The difference in retinol absorption could explain this variability in the fracture risk.[7] Houtkooper et al.[27] measured BMD at lumbar vertebrae 2–4, femur neck, Ward’s triangle, and trochanter. A positive association between retinol intake and BMD at all bone sites except for the femoral neck was found.
In another recent systematic review by Zhou et al.[6] on the dietary vitamin intake effect on fracture risk, no harmful impact of Vit A was found. They explained their results by their included study sites of fractures which were not differentiated, and the effect estimates for the fractures in different sites might have been neutralized. The sources of Vit A differ between studies in previous meta-analyses.
These contradictive results regarding vitamin A intake, absorption, and role in fracture risk suggest that an increase in BMD is not a guaranteed protector against fracture risk. Other factors may have a role in increasing such a risk. For example, the Iowa Women’s Health Study followed up over 34,000 postmenopausal women for an average of 9.5 years and found a no-dose-response relationship demonstrated between Vit A and fracture risk at all sites.[28]
Bone fragility and fracture risk are dependent on bone mass and quality; in animal studies, it has been shown that an excess Vit A has a negative effect on the cortical bone. On the other hand, human epidemiologic studies only used the DEXA scan to assess BMD, which is a two-dimensional technique providing measurements of a real (mg/cm2) rather than volumetric (mg/cm3) BMD.[29,30] DXA fails to assess Vit A’s independent changes on the trabecular and cortical bone or the important components of bone microarchitecture.[31]
All the cross-sectional studies showed a protective role of Vit A on BMD if the participants took the vitamin’s daily allowance from the diet. However, the exact level of Vit A either from the diet or supplement to cause a beneficial bone effect or prevent harm, cannot yet be determined from the available evidence. As most of the studies assessed the dietary intake based on a different questionnaire regarding food frequency; the semi-quantitative instrument might have errors classifying that intake. Moreover, concurrent ingestions of other nutritional substances may affect the relationship between Vit A ingestion, absorption, and health outcomes.[15] For example, fatty meals increase the absorption of Vit A and Vit D as well. Moreover, other antioxidants, vitamins, and minerals consumed from the diet affect bone health.
Most of the included studies were carried over the aging population, and as it is known that aging is a risk factor for a poor diet and weight loss; both may contribute to osteoporosis.
In this review, only observational studies (cross-sectional and cohort) were included because there have been very few RCTs and case-control studies in humans, which did not fulfill our inclusion criteria. All cross-sectional studies showed a protective role on BMD if the participants took the daily allowance of Vit A from the diet. In contrast, the included cohort studies that used supplemental Vit A were not all consistent with this role. This may be assigned to the fact that a healthy balanced diet rich in nutrients, minerals, and antioxidants other than Vit A positively affect bone health.
Our study did not involve a meta-analysis because the pooling of results was not possible due to the missing data. Moreover, we only studied the effect of Vit A on BMD as the previous systematic reviews on the fracture risk did not illustrate this role. Also, their results were inconsistent, which merited further investigation.
Thus, taking Vit A in doses higher than required for bone health benefits cannot be encouraged until a dose-response relationship is further studied where the exact mechanism and possible harms are illustrated. This relationship should be further investigated by large-scale prospective studies considering other confounders. More studies are required to clarify the reasons for the increased hip fracture with increased Vit A intake despite the decrease in all site fracture risk. The effect of Isotretinoin (high-dose Vit A), which is one of the most common used dermatologic treatment for several conditions, like acne, on BMD should be investigated.
This systematic review has several remarkable strengths, such as the comprehensive search, strict inclusion criteria that focused only on the relationship between the Vit A use and BMD change, and the included studies published with no language restrictions. Nevertheless, only observational studies’ involvement carries the possibility of unmeasured residual confounding, which cannot be excluded. Moreover, observational studies cannot clarify if the observation is a causal effect or a result of unmeasured variables.
Conclusion
Our study reviewed the risk and benefit of Vit A on BMD; we revealed a favorable effect, where most of the included studies have shown that a higher Vit A intake may increase BMD in all sites. However, we still have inconclusive evidence of this positive relationship due to a lack of quantitative data. Therefore, well-controlled observational and RCTs are recommended to convey more valuable results. Aging is a risk factor for a poor diet and weight loss; both may contribute to osteoporosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Publishing HH. Vitamin A and your bones [Internet] Harvard Health. Available from: https://www.health.harvard.edu/newsletter_article/vitamin-a-and-your-bones .
- 2.Henning P, Conaway HH, Lerner UH. Retinoid receptors in bone and their role in bone remodeling. Front Endocrinol (Lausanne) 2015;6:31. doi: 10.3389/fendo.2015.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conaway HH, Henning P, Lerner UH. Vitamin A metabolism, action, and role in skeletal homeostasis. Endocr Rev. 2013;34:766–97. doi: 10.1210/er.2012-1071. [DOI] [PubMed] [Google Scholar]
- 4.Mata-Granados JM, Cuenca-Acevedo JR, de Castro ML, Holick MF, Quesada-Gomez JM. Vitamin D insufficiency, together with high serum levels of vitamin A, increases the risk for osteoporosis in postmenopausal women. Arch Osteoporos. 2013;8:124. doi: 10.1007/s11657-013-0124-5. [DOI] [PubMed] [Google Scholar]
- 5.Maggio D, Barabani M, Pierandrei M, Polidori MC, Catani M, Mecocci P, et al. Marked decrease in plasma antioxidants in aged osteoporotic women:Results of a cross-sectional study. J Clin Endocrinol Metab. 2003;88:1523–7. doi: 10.1210/jc.2002-021496. [DOI] [PubMed] [Google Scholar]
- 6.Zhou P, Shao R, Wang H, Miao J, Wang X. Dietary vitamin A, C, and E intake and subsequent fracture risk at various sites:A meta-analysis of prospective cohort studies. Medicine (Baltimore) 2020;99:e20841. doi: 10.1097/MD.0000000000020841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang X, Zhang R, Moore JB, Wang Y, Yan H, Wu Y, et al. The effect of vitamin A on fracture risk:A meta-analysis of cohort studies. Int J Environ Res Public Health. 2017;14:1043. doi: 10.3390/ijerph14091043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses:The PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 9. Available from: https://www.who.int/clinical-trials-registry-platform .
- 10.Petticrew M, Altman DJ. Evaluating nonrandomized intervention studies. Health Technol Assess. 2003;7:1–79. doi: 10.3310/hta7270. [DOI] [PubMed] [Google Scholar]
- 11.Wells GA, Shea B, O’Connell DA, Peterson J, Welch V, Losos M, et al. The Ottawa Hospital Research Institute [Internet]. Ottawa Hospital Research Institute. cited 2021 Aug 18. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 12. Available from: https://www.covidence.org .
- 13.Lorenzetti DL, Ghali WA. Reference management software for systematic reviews and meta-analyses:An exploration of usage and usability. BMC Med Res Methodol. 2013;13:141. doi: 10.1186/1471-2288-13-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359–81. doi: 10.1007/s00198-014-2794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chupeerach C, Harnroongroj T, Phonrat B, Tungtrongchitr A, Schweigert FJ, Tungtrongchitr R, et al. Decreased retinol transport proteins in Thai postmenopausal women with osteoporosis. Southeast Asian J Trop Med Public Health. 2011;42:1515–20. [PubMed] [Google Scholar]
- 16.Silva TR, Franz R, Maturana MA, Spritzer PM. Associations between body composition and lifestyle factors with bone mineral density according to time since menopause in women from Southern Brazil:A cross-sectional study. BMC Endocr Disord. 2015;15:71. doi: 10.1186/s12902-015-0072-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahni S, Hannan MT, Blumberg J, Cupples LA, Kiel DP, Tucker KL. Inverse association of carotenoid intakes with 4-y change in bone mineral density in elderly men and women:The Framingham Osteoporosis Study. Am J Clin Nutr. 2009;89:416–24. doi: 10.3945/ajcn.2008.26388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ballew C, Galuska D, Gillespie C. High serum retinyl esters are not associated with reduced bone mineral density in the Third National Health and Nutrition Examination Survey, 1988–1994. J Bone Miner Res. 2001;16:2306–12. doi: 10.1359/jbmr.2001.16.12.2306. [DOI] [PubMed] [Google Scholar]
- 19.Penniston KL, Weng N, Binkley N, Tanumihardjo SA. Serum retinyl esters are not elevated in postmenopausal women with and without osteoporosis whose preformed vitamin A intakes are high. Am J Clin Nutr. 2006;84:1350–6. doi: 10.1093/ajcn/84.6.1350. [DOI] [PubMed] [Google Scholar]
- 20.Promislow JH, Goodman - Gruen D, Slymen DJ, Barrett - Connor E. Retinol intake and bone mineral density in the elderly:The Rancho Bernardo Study. J Bone Miner Res. 2002;17:1349–58. doi: 10.1359/jbmr.2002.17.8.1349. [DOI] [PubMed] [Google Scholar]
- 21.Rejnmark L, Vestergaard P, Charles P, Hermann AP, Brot C, Eiken P, et al. No effect of vitamin A intake on bone mineral density and fracture risk in perimenopausal women. Osteoporos Int. 2004;15:872–80. doi: 10.1007/s00198-004-1618-1. [DOI] [PubMed] [Google Scholar]
- 22.Joo NS, Yang SW, Song BC, Yeum KJ. Vitamin A intake, serum vitamin D and bone mineral density:Analysis of the Korea National Health and Nutrition Examination Survey (KNHANES, 2008–2011) Nutrients. 2015;7:1716–27. doi: 10.3390/nu7031716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holvik K, Ahmed LA, Forsmo S, Gjesdal CG, Grimnes G, Samuelsen SO, et al. No increase in the risk of hip fracture at high serum retinol concentrations in community-dwelling older Norwegians:The Norwegian epidemiologic osteoporosis studies. Am J Clin Nutr. 2015;102:1289–96. doi: 10.3945/ajcn.115.110528. [DOI] [PubMed] [Google Scholar]
- 24.Chen GD, Zhu YY, Cao Y, Liu J, Shi WQ, Liu ZM, et al. Association of dietary consumption and serum levels of vitamin A and b-carotene with bone mineral density in Chinese adults. Bone. 2015;79:110–5. doi: 10.1016/j.bone.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 25.Choi MJ, Park EJ, Jo HJ. Relationship of nutrient intakes and bone mineral density of elderly women in Daegu, Korea. Nutr Res Pract. 2007;1:328–34. doi: 10.4162/nrp.2007.1.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Jonge EA, Kiefte-de Jong JC, Campos-Obando N, Booij L, Franco OH, Hofman A, et al. Dietary vitamin A intake and bone health in the elderly:The Rotterdam study. Eur J Clin Nutr. 2015;69:1360–8. doi: 10.1038/ejcn.2015.154. [DOI] [PubMed] [Google Scholar]
- 27.Houtkooper LB, Ritenbaugh C, Aickin M, Lohman TG, Going SB, Weber JL, et al. Nutrients, body composition, and exercise are related to change in bone mineral density in premenopausal women. J Nutr. 1995;125:1229–37. doi: 10.1093/jn/125.5.1229. [DOI] [PubMed] [Google Scholar]
- 28.Lim LS, Harnack LJ, Lazovich D, Folsom AR. Vitamin A intake and the risk of hip fracture in postmenopausal women:The Iowa Women's health study. Osteoporos Int. 2004;15:552–9. doi: 10.1007/s00198-003-1577-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bahtiri E, Islami H, Hoxha R, Qorraj-Bytyqi H, Rexhepi S, Hoti K, et al. Esomeprazole use is independently associated with significant reduction of BMD:1-year prospective comparative safety study of four proton pump inhibitors. J Bone Miner Metab. 2016;34:571–9. doi: 10.1007/s00774-015-0699-6. [DOI] [PubMed] [Google Scholar]
- 30.Stathopoulos KD, Zoubos AB, Papaioannou NA, Mastrokalos D, Galanos A, Papagelopoulos PJ, et al. Differences of bone mineral mass, volumetric bone mineral density, geometrical and structural parameters and derived strength of the tibia between premenopausal and postmenopausal women of different age groups:A peripheral Quantitative Computed Tomography (pQCT) study. J Musculoskelet Neuronal Interact. 2016;16:113–21. [PMC free article] [PubMed] [Google Scholar]
- 31.Aleraij S, Alhowti S, Ferwana M, Abdulmajeed I. Effect of proton pump inhibitors on bone mineral density:A systematic review and meta-analysis of observational studies. Bone Rep. 2020;13:100732. doi: 10.1016/j.bonr.2020.100732. [DOI] [PMC free article] [PubMed] [Google Scholar]