Abstract
Background:
Caesarean section (C-section) delivery is a serious maternal health concern in the long run. Notedly, there is a lack of studies dealing with understanding the ways and reasons of C-section deliveries becoming a public health issue in today’s time in India and the measures to reduce the unnecessary caesarean sections. We have conducted this study to study the changes in the state-wise prevalence of C-section deliveries in India and understand C-section delivery’s socioeconomic and biomedical predictors.
Materials and Methods:
The study uses data from the fourth and fifth rounds of the National Family Health Surveys (NFHS). The per cent differences in the C-section deliveries from NFHS-4 to NFHS-5 across the states were measured through relative changes. The association between the C-section delivery and socioeconomic and biomedical factors were assessed using multiple logistic regression.
Results:
This study revealed that the C-section deliveries are higher in the southern states than in the other parts of India. Literacy plays a vital role in C-section deliveries. The probabilities of C-section deliveries are more in 30–40 and 40 + years. The women belonging to the median wealth index category were more likely (OR–CI, 1.62 [1.55–1.66]) to undergo the C-section followed by the women from wealthy households (OR–CI, 1.46 [1.41–1.52]).
Conclusion:
The Government’s health policymakers should take the initiative to reduce the C-section section delivery by means of building maternal health literacy and awareness among women and the community so that its future implications can be minimised. It is crucial to formulate a mandate and implement it in the states where C-sections are too high through community health workers and primary care providers.
Keywords: C-section, maternal health, multiple logistic regression, out-of-pocket expenditure, private health facility, socio-economic status
Introduction
Caesarean delivery (C-section) delivers a baby through surgery through a laceration in the mother’s abdomen and uterus. According to the World Health Organisation (WHO), a caesarean section is a surgical procedure that can save the life of a woman and her baby when undertaken for medical reasons. Thus, the procedure should only be used in complicated pregnancies.[1] However, C-sections have gradually become common in developing countries, and it is already quite common in the developed countries for a long time. In terms of the developing countries, in India, the C-section rates have crossed the WHO threshold of 15%, a severe public health concern.[2] Other developing countries like Bangladesh, China, Sri Lanka have also seen increments in the C-section in the past two decades. One of the most crucial reasons for this growing rate of C-sections is the increase of institutional births and other attributable factors like unregulated health facilities, mainly private institutions and an increasing trend of women opting for it.[3,4] These factors are regarded as non-clinical factors which need to be explored more to understand the increasing rates of caesarean deliveries.[5] The conceptual framework provided in Figure 1 investigates the various factors affecting the increasing C-section deliveries as per the WHO recommendations and guidelines.[6]
Figure 1.
Factors affecting increasing rate of C-section deliveries
From this conceptual framework, it can be understood that the livelihood of women and their families in the context of developing countries plays a significant role in making decisions related to the delivery procedures. Lifestyle is an integral part of livelihood and with an increasing rate of obesity in women due to the lack of physical activities especially in the urban areas and due to dietary habits, they are prone to caesarean deliveries. Moreover, the secondary infertile women on becoming pregnant fear normal delivery as it might lead to losing a chance of live birth.[7,8,9] In terms of expenditure, it is known that the C-section delivery costs more than a normal delivery. There is no doubt that a caesarean delivery takes less time and effort, and pays more than the normal vaginal delivery.[10,11] The private sector health facilities promote caesarean delivery for their benefit of revenues thereby leading to an unregulated market.[12,13]
It is also to be noted that increasing education and literacy among women has led to their apprehension towards normal delivery due to the fear of pain and fear of medical litigations.[14,15] Certain religions practice multiple births which is also an important non-clinical factor that needs to be addressed to reduce unnecessary caesarean sections.[16]
A considerable number of studies have shown that there is an inverse relationship between the rates of C-section and maternal and child mortality in low-income countries where large sectors of the population lack access to basic obstetric care.[14,17,18] However, the C-section rates above a central limit have not shown additional benefit for the mother or child, and some studies have shown that the high rates of the C-section could be linked to negative repercussions in maternal and child health. According to the WHO statement in 1985, the international healthcare community has considered a range of 10–15% to be the ideal rate for C-sections in a country.[19] Since then, C-section rates have become increasingly common in both developed and developing countries. A C-section can efficaciously prevent maternal and perinatal mortality and morbidity. However, no evidence has been shown of the benefits of caesarean delivery for women or infants who are fit for normal delivery and do not require the procedure.
In terms of the global scenario, the previous studies show that in both the developed and developing countries, there is a large increment in the rate of C-section as a country shifts from lower to higher Human Development Index (HDI). However, it can be seen that the rates are consistently rising even within the HDI categories. Currently, no internationally accepted classification system for the C-section is available to allow meaningful and relevant comparisons of C-section rates across different facilities, regions or cities.[20] Among the pre-existing systems used to classify C-sections, in recent years, the 10-group classification (Robson classification) has been widely used in many countries. In the Indian context, 17% of live births, as per the National Family Health Survey (NFHS-4), in the 5 years before the survey were C-section deliveries. Moreover, 45% of the C-section deliveries were reportedly planned after the onset of labour pains (NFHS-4).[21] The prevalence of the C-section in India was 8.5% in NFHS-3 while data in NFHS-4 show that it has increased to 17.2%.[22] Thus, almost 9% has increased over 10 years. This study thus delves deep into understanding the change in the rate of the C-section deliveries and identifying the various factors affecting the increment in the C-section rates.
In the current times, unnecessary caesarean deliveries are of public health concern in India. This study is needed to understand the possible factors of the high C-section rates in India. India, being a diverse country, there have been quite wide differences across the geographies, religions, castes and other socioeconomic characteristics which eventually are correlated with women’s education, literacy, livelihood and health. Education, awareness on caesarean deliveries and importance of institutional deliveries and increased healthcare access plays a significant role in the higher C-section deliveries. A few global studies have mentioned the physician factor contributing to the rise in C-section rates in terms of preferring a C-section because of the doctors’ ability to schedule C-section at their convenience, the shorter duration of the delivery by C-section compared to vaginal delivery, inadequate training of the physicians in vaginal delivery and financial incentives.[23,24] Not many studies have been done to understand how C-section deliveries have become a public health concern in today’s time and what to do to reduce the unnecessary C- sections. This study tries to understand the relationship between the various factors affecting the increase in caesarean deliveries in health facilities and their co-relation and also shows the geographical prevalence of caesarean deliveries across the states of India. Thus, the main objectives of this study are (a) to study the changes in the state-wise prevalence of C-section deliveries in India; (b) to understand the socioeconomic and biomedical predictors of the C-section delivery.
Methods and Materials
Data and material
For this study, the data used are the compilation of the fourth round of NFHS (NFHS-4, 2015–2016) and state-level fact sheets of the fifth round (NFHS-5, 2019–2020). The NFHS is the Indian version of the Demographic and Health Survey (DHS) which is a survey consistently conducted over 90 countries with over 300 surveys worldwide. The NFHS-4 was coordinated by the International Institute for Population Sciences (IIPS) with the financial support of the Ministry of Health and Family Welfare, Government of India.[25] The survey provides information on the important indicators of maternal and child health, fertility and mortality. Both NFHS-4 and NFHS-5 covered all the 29 states and 7 union territories and also provided information on the district level (all 640 districts in India as per the census 2011) estimates for important indicators.
The details of the sampling procedure and data collection protocol can be found elsewhere (IIPS, 2020). The information provided in all state-level factsheets were brought together in an excel sheet. The relevant indicators of nutrition and other socioeconomic indicators were used for data analysis. The data were properly filtered and cleaned before they were used for analysis.
Outcome and predictor variables
We have taken ‘C-section delivery’ as the outcome variable. The pre-existing variable in the NFHS-4 data, i.e. ‘delivery by caesarean section’ was dichotomised into ‘C-section = 1’ and ‘non-C-section = 0’. The variables age, place of residence, education, wealth index, place of delivery, out-of-pocket expenditure (OOPE), anti-natal care (ANC) visit, birth order, maternal body mass index (BMI) and size of the child were used as predictors. The variable ‘respondent current age was categorised into ‘15–20’, ‘20–30’, ‘30–40’ and ‘40+’. The variable ‘wealth index’ which was categorised as ‘poorest’, ‘poorer’, ‘middle’, ‘richer’ and ‘richest’ in the existing data (NFHS-4) was recategorised as ‘poor’, middle’ and ‘rich’. We have categorised the maternal BMI into ‘underweight (<18.5)’, ‘normal (18.5–24.9) and overweight/obese (>25.0) as per the guidelines of the WHO. The variable out-of-OOPE was categorised into ‘No expense = 0’, ‘<25000 = 1’, ‘> =25000 = 2’, similarly, the birth order was categorised into ‘1-2 = 1’, ‘3-5 = 2, ‘>5 = 3’.
Data analysis
The analyses were done after removing list-wise cases of missing, flagged and no information from the NFHS-4 data. The state-wise percentages were taken from the extracted factsheets of NFHS-5. We have calculated absolute and relative per cent changes to understand the changes in the prevalence of C-section deliveries. State-wise maps based on the prevalence of C-section deliveries were created in the STATA software through the packages ‘shp2dta’ (package used to convert.shp file into.dta format) and ‘spmap’ (specially designed to visualise spatial data). The multiple logistic regression was done to understand the associated predictors with the C-section deliveries in India. The statistical formulation of the multiple logistic regression model is given below:
log((Pk/(1-Pk)) =
α0 × β1* × 1 + β2* × 2 + β3* × 2 + ..... + β10* × 1
where, Pi = Probability of C-section delivery (k = 1, 2, 3,…, 10)
xj, (j = 1, 2, 3,…., 10) are predictors
β1 ..........β j are coefficients, j = 1, 2,3, …10
ɑ0 is intercept
All statistical analyses were done in the STATA software (version: 13.0).
Results
Scenario of the C-section deliveries across the Indian states over 5 years (2015–2020)
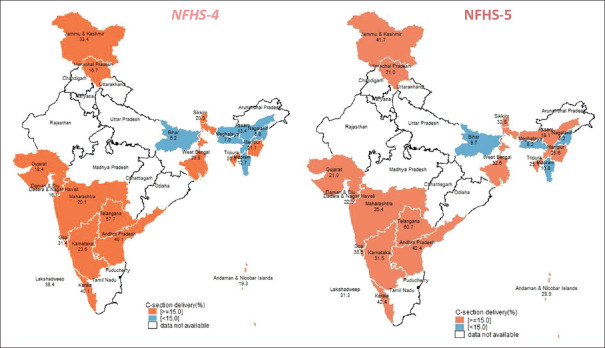
The heat maps show the spatial variations of the C-section deliveries across the selected Indian states. The C-section deliveries have increased from 2015 to 2020. More than half of the states show high C-section deliveries. The highest C-section deliveries was found in Telangana (60.7%), while the lowest was observed in Nagaland (5.2%) in the first round of NFHS-5, 2019–2020.
The top five states showing higher C-section deliveries in NFHS-5 were Kerala (42.4%), Andhra Pradesh (42.4%), Lakshadweep (31.3%), Jammu and Kashmir (41.7%) and Goa (39.5%), respectively. The bottom five states showing lower C-section deliveries were Meghalaya (8.2%), Bihar (9.7%), Mizoram (10.8%), Assam (18.1%) and Himachal Pradesh (21.0%), respectively [Figure 2].
Figure 2.
Spatial distribution of percentage of caesarean section delivery across Indian States, NFHS
The relative change in the C-section deliveries provided us with a basis to compare the changes in terms of the ratio of differences in the current to the previous percentages divided by the previous percentage. The relative change in the C-section deliveries was found the highest in Ladakh (133.5%) followed by Sikkim (56.9%), Bihar (56.5%), Andaman and Nicobar (54.9%) and Dadra Nagar Haveli and Daman Diu (42.2%), while the lower changes were observed in states like Telangana (5.2%) followed by Kerala (5.7%), Andhra Pradesh (5.7%), Nagaland (10.3%), Mizoram (15.0%) and Lakshadweep (18.5%), respectively [Table 1].
Table 1.
Changes in C-section deliveries across the Indian states, NFHS (2015-2020)
| States/UTs | NFHS-4 (2015-2016) | NFHS-5 (2019-2020) | AC | RC |
|---|---|---|---|---|
| Lakshadweep | 38.4 | 31.3 | -7.1 | -18.5 |
| Mizoram | 12.7 | 10.8 | -1.9 | -15.0 |
| Nagaland | 5.8 | 5.2 | -0.6 | -10.3 |
| Telangana | 57.7 | 60.7 | 3.0 | 5.2 |
| Andhra Pradesh | 40.1 | 42.4 | 2.3 | 5.7 |
| Kerala | 40.1 | 42.4 | 2.3 | 5.7 |
| Meghalaya | 7.6 | 8.2 | 0.6 | 7.9 |
| Gujarat | 18.4 | 21.0 | 2.6 | 14.1 |
| Manipur | 21.1 | 25.6 | 4.5 | 21.3 |
| Tripura | 20.5 | 25.1 | 4.6 | 22.4 |
| Jammu and Kashmir | 33.4 | 41.7 | 8.3 | 24.9 |
| Himachal Pradesh | 16.7 | 21.0 | 4.3 | 25.7 |
| Goa | 31.4 | 39.5 | 8.1 | 25.8 |
| Maharashtra | 20.1 | 25.4 | 5.3 | 26.4 |
| Karnataka | 23.6 | 31.5 | 7.9 | 33.5 |
| Assam | 13.4 | 18.1 | 4.7 | 35.1 |
| West Bengal | 23.8 | 32.6 | 8.8 | 37.0 |
| Dadra and Nagar Haveli and Daman and Diu | 16.1 | 22.9 | 6.8 | 42.2 |
| Andaman and Nicobar | 19.3 | 29.9 | 10.6 | 54.9 |
| Bihar | 6.2 | 9.7 | 3.5 | 56.5 |
| Sikkim | 20.9 | 32.8 | 11.9 | 56.9 |
| Ladakh | 16.1 | 37.6 | 21.5 | 133.5 |
AC: Absolute change, RC: Relative change
Associated predictors with C-section deliveries in India
The results of the multiple logistic regression show that socioeconomic and biomedical factors were significantly associated with ‘Caesarean (outcome variable)’. The women belonging to the age group 40–49 were more likely (OR–CI, 1.7 [1.52–2.05]) to undergo C-section as compared to the women of age group 15–20, followed by age group 30–40 (OR–CI, 1.39 [1.32–1.48]) and 20–30 (OR–CI, 1.08 [1.03–1.14]), respectively. Women belonging to the rural areas were less likely (OR–CI, 0.84 [0.82–0.86]) to undergo C-sections as compared to women of the urban area. Highly educated women were more likely to undergo caesarean as compared to the uneducated women (OR–CI, 1.64 [1.6–1.76]). The odds of the C-section delivery were significantly higher in the private hospital as compared to the public hospital (OR–CI, 4.45 [4.34, 4.57]).
The women belonging to the middle wealth index category were more likely (OR–CI, 1.62 [1.55–1.66]) to undergo C-section followed by the women from the rich households (OR–CI, 1.46 [1.41–1.52]) as compared to the poor households. The women who have completed more than five ANC visits to the healthcare facilities were more likely to undergo the C-section (OR–CI 2.10 [2.04–2.17]) as compared to the women who have done less than five or no visits. The predictors birth order, OOPE and the size of the child were also significantly associated with the outcome variable (C-section). The overweight women were more likely to go for the C-section as compared to the underweight women (OR–CI, 2.45 [2.36–2.55]) followed by the women having normal weight [Table 2].
Table 2.
Result of multiple logistic regression showing association between C-section delivery and selected predictors, NFHS-4
| Caesarean (outcome variable) | Odds Ratio | Sth. Err | 95% Confidence interval | |
|---|---|---|---|---|
|
| ||||
| LL | UL | |||
| Age group (in years) | ||||
| 15-20® | 1 | |||
| 20-30 | 1.08*** | 0.03 | 1.03 | 1.14 |
| 30-40 | 1.39*** | 0.04 | 1.32 | 1.48 |
| 40+ | 1.77*** | 0.13 | 1.52 | 2.05 |
| Place of residence | ||||
| Urban® | 1 | |||
| Rural | 0.84*** | 0.01 | 0.82 | 0.86 |
| Education | ||||
| No education® | 1 | |||
| Primary | 1.40*** | 0.04 | 1.36 | 1.5 |
| Secondary | 1.57*** | 0.03 | 1.54 | 1.66 |
| Higher | 1.64*** | 0.04 | 1.6 | 1.76 |
| Place of delivery | ||||
| Public® | 1 | |||
| Private | 4.45*** | 0.06 | 4.34 | 4.57 |
| ANC visit | ||||
| No visit® | 1 | |||
| 1-4 | 1.38*** | 0.02 | 1.34 | 1.43 |
| >5 | 2.10*** | 0.03 | 2.04 | 2.17 |
| Birth order | ||||
| 1-2® | 1 | |||
| 3-5 | 0.39*** | 0.01 | 0.37 | 0.4 |
| >5 | 0.17*** | 0.01 | 0.15 | 0.2 |
| Wealth index | ||||
| Poor® | 1 | |||
| Middle | 1.62*** | 0.03 | 1.55 | 1.66 |
| Rich | 1.46*** | 0.03 | 1.41 | 1.52 |
| OOPE | ||||
| No expenses® | 1 | |||
| <25000 | 0.79*** | 0.02 | 0.76 | 0.82 |
| >=25000 | 1.70*** | 0.04 | 1.62 | 1.78 |
| BMI | ||||
| Underweight® | 1 | |||
| Normal | 1.26*** | 0.02 | 1.22 | 1.31 |
| Overweight/obese | 2.45*** | 0.05 | 2.36 | 2.55 |
| Size of the child | ||||
| Large® | 1 | |||
| Average | 0.77*** | 0.01 | 0.75 | 0.8 |
| Small | 0.87*** | 0.03 | 0.81 | 0.94 |
| Others | 0.50*** | 0.04 | 0.43 | 0.58 |
®Reference category, P***< 0.0001, LL: Lower limit, UL: Upper limit, OOPE: Out-of-pocket expenditure. Note: Author’ estimation on NFHS-4 data (2015-2016)
Discussion
The findings suggest that more than one-fifth of the institutional deliveries are C-section deliveries in most of the states of India. Moreover, C-section deliveries are performed mostly in the southern states of India (Telangana, Kerala, Andhra Pradesh).[15,25,26] Based on the analysis in this study, states like Uttar Pradesh, Bihar and Rajasthan show a low prevalence of caesarean deliveries compared to the other states. These findings of the C-section rates will enable effective health policy changes.[27,28] The rate of C-section deliveries is the highest in Telangana and lowest in Bihar. Literacy plays an important role in the C-section deliveries, i.e. the higher the literacy, the higher is the chance of C-section delivery.[15] However, only literacy will not help in reducing the incidence of unnecessary C-section deliveries. Maternal and child health literacy is also important as is being implemented by many health programmes.[29,30,31] Additionally, increasing age at birth is also directly proportionate to the increasing rate of C-section deliveries.[32,33] These kinds of deliveries, reportedly, are prevalent more in the urban areas than rural areas. Moreover, private institutions are performing more C-section deliveries than public health institutions. Studies have shown that clinical leadership in promoting normal birth can become a major contributing factor to reducing the C-section rates.[24,34] Among the North-Eastern states, most of the C-section deliveries are performed in the private institutions of Tripura (87.1%). When it comes to the wealth factor, it has an integral connection with livelihood and lifestyle. Overweight or obese women are commonly found in middle-class households and rich households and as the findings suggest, they are more prone to C-section deliveries than poor households.[26,35]
The study’s main limitation was that it was not feasible to compare the national estimates of C-section deliveries due to the unavailability of raw data of NFHS-5. Also, we cannot establish any causal relationship because of a cross-sectional study.
Training the community health workers on the knowledge of the obstetric danger signs and importance of normal deliveries for mothers not facing any complications during pregnancy along with clinical leadership among the primary care physicians on promoting healthy deliveries and raising awareness on post-partum maternal health outcomes of normal deliveries among healthy mothers could be some of the immediate implementation strategies as part of Maternal, Newborn, and Child Health (MNCH) health programmes.
Conclusion
The Government should take a primary initiative of raising awareness on the importance of normal deliveries for healthy pregnant mothers which will result in maternal health literacy among women. This can be done with the help of the frontline workers like the community health workers and primary care physicians who are the first point of contact of the pregnant mothers for ante-natal care, check-ups, or any health problems. During these check-up sessions, the primary care providers can raise awareness on the deliveries and their medical implications so that the mothers can decide for themselves before labour and the incidences of sudden decisions of unnecessary C-section deliveries are reduced in future. Sensitisation of the importance of normal delivery when no medical complications are seen in women also needs to be conducted by awareness campaigns through various modes of communication. Therefore, it is crucial to formulate a mandate where it should be noted that C-section deliveries should only be executed when medically necessary and implement the directives at the states where C-section is too high. It is also needed to be looked into that the private hospitals do not compel the patients for C-section delivery for their revenue prospects.
Key points
C-section deliveries are more prevalent in the South Indian states compared to the North Indian states. Additionally, these kinds of deliveries are performed more in the urban areas than the rural areas.
Literacy and increasing age at birth of women play an important role in C-section deliveries, i.e. they are directly proportionate to the increasing rate of C-section deliveries.
Private institutions are performing more C-section deliveries than public health institutions. And this is associated with women belonging to the upper-middle class and wealthy households who mostly opt for deliveries in private institutions due to a perception of better service provision and better quality of care.
Spreading awareness on the importance of normal delivery when no medical complications are seen in women is important and can be done through primary care providers and frontline workers who are the first point of contact of the pregnant women for ANC care, routine check-ups and visits related to any complications in pregnancy.
The Government should formulate a mandate and implement the directives at the states where the C-section is too high.
Compliance with ethical standards
This research article does not contain any studies with human participants performed by the authors. The secondary data used in this study is publicly available on the website of Demographic and Health Surveys (DHS). Author has received access of data on request from DHS.
Declaration of patient consent
Authors have given their consents for publication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: Analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21:98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- 2.Ronsmans C, Holtz S, Stanton C. Socioeconomic differentials in caesarean rates in developing countries: A retrospective analysis. Lancet. 2006;368:1516–23. doi: 10.1016/S0140-6736(06)69639-6. [DOI] [PubMed] [Google Scholar]
- 3.Belizán JM, Althabe F, Cafferata ML. Health consequences of the increasing caesarean section rates. Epidemiology. 2007;18:485–6. doi: 10.1097/EDE.0b013e318068646a. [DOI] [PubMed] [Google Scholar]
- 4.Villar J, Valladares E, Wojdyla D, Zavaleta N, Shah A, Campodónico L, et al. Caesarean delivery rates and pregnancy outcomes: The 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367:1819–29. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Informed decisions and maternal health literacy could reduce caesarean section numbers. Maternal and newborn health. Regional office for Europe. January 16. 2019. Available from URL: https://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/news/news/2019/01/informed-decisions-and-maternal-health-literacy-could-reduce-caesarean-section-numbers .
- 6.Appropriate technology for birth. Lancet. 1985;2:436–7. PMID: 2863457. Accessed from URL: https://pubmed.ncbi.nlm.nih.gov/2863457/ [PubMed] [Google Scholar]
- 7.Kirchengast S, Hartmann B. Recent lifestyle parameters are associated with increasing caesarean section rates among Singleton term births in Austria. Int J Environ Res Public Health. 2018;16:14. doi: 10.3390/ijerph16010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chavarro JE, Martín-Calvo N, Yuan C, Arvizu M, Rich-Edwards JW, Michels KB, et al. Association of birth by cesarean delivery with obesity and type 2 diabetes among adult women. JAMA Netw Open. 2020;3:e202605. doi: 10.1001/jamanetworkopen.2020.2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organisation. WHO European Regional Office Health for all database. [Last accessed on 2010 May 10]. Available from: http://data.euro.who.int/hfadb .
- 10.Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. Comparative performance of private and public healthcare systems in low- and middle-income countries: A systematic review. PLoS Med. 2012;9:e1001244. doi: 10.1371/journal.pmed.1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zakerihamidi M, Latifnejad Roudsari R, Merghati Khoei E. Vaginal delivery vs. cesarean section: A focused ethnographic study of women's perceptions in the North of Iran. Int J Community Based Nurs Midwifery. 2015;3:39–50. [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson E, Marit R. Physicians treating physicians: Information and incentives in childbirth. Am Econ J Econ Policy. 2016;8:115–141. [Google Scholar]
- 13.Dongre A, Surana M. C-section deliveries and the role of the private health sector in India. [Last accessed on 2021 Feb 3];Blog Post Date 23 July, 2018. URL: C-section deliveries and the role of the private health sector in India (ideasforindia.in) [Google Scholar]
- 14.Hofberg K, Ward MR. Fear of pregnancy and childbirth. Postgrad Med J. 2003;79:505–10. doi: 10.1136/pmj.79.935.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mishra VK. Geo-Spatial Analysis of Caesarean Section in India. OAJ Gerontol Geriatric Med. 2019;5:555658. [Google Scholar]
- 16.World Health Organisation. World Health Report 2005. [Last accessed on 2010 May 10]. Available from: http://www.who.int/whr/2005/annex . Published 2005.
- 17.Demographic and Health Surveys. [Last accessed on 2010 Mar 10]. Available from: http://www.measuredhs.com .
- 18.Vogel JP, Betrán AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J, et al. Use of the robson classification to assess caesarean section trends in 21 countries: A secondary analysis of two WHO multicountry surveys. Lancet Glob Health. 2015;3:e260–70. doi: 10.1016/S2214-109X(15)70094-X. [DOI] [PubMed] [Google Scholar]
- 19.Betran AP, Torloni MR, Zhang JJ, Gülmezoglu AM. WHO Working Group on Caesarean Section. WHO Statement on Caesarean Section Rates. BJOG. 2016;123:667–70. doi: 10.1111/1471-0528.13526. doi: 10.1111/1471-052813526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12:57. doi: 10.1186/s12978-015-0043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Women's Healthcare Australia 2016. Women's Healthcare Australia Benchmarking Report: Maternity Care 2014/2015 [Google Scholar]
- 22.Torloni MR, Betran AP, Souza JP, Widmer M, Allen T, Gulmezoglu M, et al. Classifications for cesarean section: A systematic review. PLoS One. 2011;6:e14566. doi: 10.1371/journal.pone.0014566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elnakib S, Abdel-Tawab N, Orbay D, Hassanein N. Medical and non-medical reasons for cesarean section delivery in Egypt: A hospital-based retrospective study. BMC Pregnancy Childbirth. 2019;19:411. doi: 10.1186/s12884-019-2558-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goyert GL, Bottoms SF, Treadwell MC, Nehra PC. The physician factor in cesarean birth rates. N Engl J Med. 1989;320:706–9. doi: 10.1056/NEJM198903163201106. [DOI] [PubMed] [Google Scholar]
- 25.IIPS. National Family Health Survey, India. [Last accessed on 2021 Feb 9]; URL: National Family Health Survey (rchiips.org) [Google Scholar]
- 26.Press Information Bureau, Ministry of Health and Family Welfare, Government of India. (2018) Regulating Caesarean Sections conducted by Private Hospitals [Press Release] Retrieved from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=177374 .
- 27.Bhartia A, Sen Gupta Dhar R, Bhartia S. Reducing caesarean section rate in an urban hospital serving women attending privately in India – A quality improvement initiative. BMC Pregnancy Childbirth. 2020;20:556. doi: 10.1186/s12884-020-03234-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sandall J, Tribe RM, Avery L, Mola G, Visser GH, Homer CS, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. 2018;392:1349–57. doi: 10.1016/S0140-6736(18)31930-5. [DOI] [PubMed] [Google Scholar]
- 29.Bahl R, Qazi S, Darmstadt GL, Martines J. Why is continuum of care from home to health facilities essential to improve perinatal survival? Semin Perinatol. 2010;34:477–85. doi: 10.1053/j.semperi.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Saggurti N, Atmavilas Y, Porwal A, Schooley J, Das R, Kande N, et al. Effect of health intervention integration within women's self-help groups on collectivization and healthy practices around reproductive, maternal, neonatal and child health in rural India. PLoS One. 2018;13:e0202562. doi: 10.1371/journal.pone.0202562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahmad D, Mohanty I, Hazra A, Niyonsenga T. The knowledge of danger signs of obstetric complications among women in rural India: Evaluating an integrated microfinance and health literacy program. BMC Pregnancy Childbirth. 2021;21:79. doi: 10.1186/s12884-021-03563-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ecker JL, Chen KT, Cohen AP, Riley LE, Lieberman ES. Increased risk of cesarean delivery with advancing maternal age: Indications and associated factors in nulliparous women. Am J Obstet Gynecol. 2001;185:883–7. doi: 10.1067/mob.2001.117364. [DOI] [PubMed] [Google Scholar]
- 33.Rydahl E, Declercq E, Juhl M, Maimburg RD. Cesarean section on a rise-Does advanced maternal age explain the increase? A population register-based study. PloS One. 2019;14:e0210655. doi: 10.1371/journal.pone.0210655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ji H, Jiang H, Yang L, Qian X, Tang S. Factors contributing to the rapid rise of caesarean section: A prospective study of primiparous Chinese women in Shanghai. BMJ Open. 2015;5:e008994. doi: 10.1136/bmjopen-2015-008994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Srivastava S, Chaurasia H, Singh JK, Chaudhary P. Exploring the spatial patterns of cesarean section delivery in India: Evidence from National family health survey-4. Clin Epidemiol Glob Health. 2020;8:414–22. [Google Scholar]