Abstract
Cervical radiculopathy is a neurologic condition caused by nerve root compression in the cervical spine, resulting in pain, numbness, sensory or motor dysfunction in the upper extremities. We present the case of a 57-year-old woman working as an insurance agent who suffered from chronic neck pain and numbness in the left arm for six months. Cervical radiographs revealed a reverse in natural lordotic curve. The patient was diagnosed with left C6 radiculopathy due to cervical spondylosis. Since cervical traction, rehabilitative exercise, acupuncture, and pain medicines previously failed to provide a long-lasting relief of symptoms, the patient sought chiropractic care. She was treated with spinal manipulation in combination with intermittent motorized cervical traction for three months. As a result of care, the patient experienced complete relief of symptoms, full cervical mobility, and high WHO Quality of Life score. A restoration of cervical lordosis was demonstrated on the 4-year follow-up radiograph.
Keywords: Cervical lordosis, cervical radiculopathy, chiropractic manipulation
Introduction
Cervical radiculopathy is a neurologic condition resulting from compression or inflammation of the cervical nerve roots.[1] The nerve compression is caused by narrowing of the neural foramen due to cervical spondylosis, disc herniation, trauma, or an abnormal curve of the spine. The majority of cases of cervical radiculopathy stem from degenerative disease in the cervical spine. Disc desiccation can lead to decreased disc height, hypertrophy of the uncinate joint, foraminal stenosis and cervical radiculopathy.[1] Disc degeneration and herniation trigger a pro-inflammatory cascade mediated by tumor necrosis factor-alpha, interleukin factor-6, and extracellular matrix-degrading enzyme.[2] This cascade leads to further sensitization and increased pain in the area. Conservative treatment should be the initial treatment for patients with compressive cervical radiculopathy. Many nonsurgical treatment options are available, ranging from different types of physiotherapy, cervical traction, non-steroidal anti-inflammatory drugs, manipulative therapies, and epidural steroid injection.[3] Operative intervention is indicated if conservative measures fail.
The primary goal of surgery for cervical radiculopathy is to relieve symptoms by neural decompression and to prevent the progression of debilitating symptoms. According to the North American Spine Society Evidence-Based Clinical Guideline, surgical intervention is suggested for the rapid symptom relief of cervical radiculopathy from degenerative diseases when compared with medical or interventional treatment (Grade B recommendation).[4] This case report describes chiropractic care of cervical radiculopathy associated with spondylosis in a 57-year-old woman. The patient had a resolution of neck pain and numbness of the left arm with a concomitant of correction of cervical curvature following chiropractic interventions.
This case report has been prepared after obtaining written informed consent from the patient to have the case details and accompanying images published. Owing to the nature of the retrospective chart review, IRB approval is not required.
Case Report
A 57-year-old woman insurance agent presented with chronic neck pain and numbness of the left arm for 6 months. She described her neck pain as deep, dull aching accompanied by a sensation of numbness over the lateral aspect of her left arm. She denied any history of trauma. The pain was rated at 8/10 in numeric pain scale (0 being none and 10 being the worst pain imaginable), which had negatively impacted her sleep pattern and social life. In addition, the symptoms were induced by lack of sleep and sleeping on the left side, therefore the provocative cycle severely impaired the patient’s quality of life. The patient was previously diagnosed with left C6 radiculopathy associated with cervical spondylosis. She was treated with cervical traction, rehabilitative exercise, acupuncture, and pain medication which only provided temporary relief of her symptoms. She sought chiropractic care for the conditions.
On examination, the patient presented with a forward head, stooping posture, and mild thoracic hyperkyphosis. Physical examination identified motion restriction at the C2/3, C5/6 and C6/7 segments. Muscular hypertonicity was palpated at the left trapezius, left sternocleidomastoid, and right splenius capitis. A hand-held dynamometer was used to measure the cervical range of motion quantitatively. Neck motion was limited by pain at 20°/70° active extension, 45°/80° active flexion, and 45°/90° of bilateral rotations. The Spurling test (by applying axial compression of the cervical spine to induce radicular pain) was positive for left nerve root pain. Sensory deficit was also noted along the left C6 dermatome. Motor strength of the left biceps was decreased and rated 4/5 on neurological examination. Cervical radiographs demonstrated narrowed interspaces from C4/C5 through C7/T1, anterior osteophytic lipping of cervical vertebrae and reversed cervical lordosis [Figure 1]. Left foraminal narrowing due to osteophyte encroachment at C5/C6 and C6/C7 levels was evident on the oblique views [Figure 2]. The clinical findings were consistent with cervical radiculopathy secondary to spondylosis and foraminal narrowing.
Figure 1.
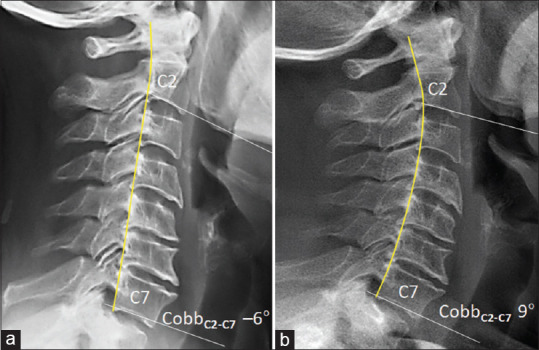
Sagittal cervical radiographs. (a) At initial assessment, posterior vertebral line (yellow line) depicted a reverse in cervical lordosis. C2-7 Cobb angle minus 6°, narrowed interspaces from C4/C5 through C7/T1, and anterior osteophytic lipping of lower vertebrae were noted. (b) 4 years follow-up, the cervical curvature improved as compared with initial radiograph. The mean C2-C7 angle in asymptomatic women is 9.11° ± 10.4°
Figure 2.
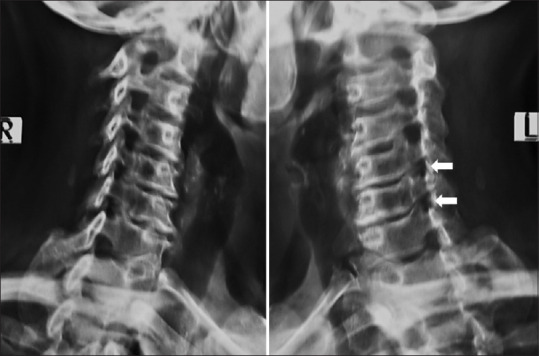
Oblique radiographs of the cervical spine. Oblique imaging at initial assessment revealed foraminal stenosis at left C5/6 and C6/7 segments (white arrows), evidence of cervical spondylosis and interspace narrowing at C4/C5 through C7/T1 levels
After assessing for appropriateness of the manual technique, the patient underwent a high-velocity and low-amplitude (HVLA) cervical manipulation. The initial treatments focused on adjusting the cervical mobility, and correcting cervical misalignment and vertebral instability. The patient started treatment session 3 times a week. She reported 50% relief of neck pain and radiculopathy symptoms and was able to maintain the head in an upright posture after four weeks of treatment. Subsequently an intermittent motorized traction for cervical decompression was added to release intervertebral space and retrieve neurological function. Treatment frequency was reduced to 2 times a week for 2 months. The patient reported complete resolution of symptoms, full cervical mobility, and stopping pain medications three months after the beginning of treatment. She entered an elective spinal rehabilitation program once monthly for continuing care for up to four years. As a result of care, the restoration of cervical lordosis was demonstrated on the follow-up radiograph [Figure 1b].
Discussion
Cervical hypolordosis describes a deficient front-to-back spinal curvature in the neck.[5] Radiculopathy is a potential problem in patients with a loss of lordosis or reversed lordosis of the cervical spine, since nerve root impingement can result from foraminal narrowing. In the current report, the patient suffering from cervical radiculopathy experienced a positive outcome after chiropractic care consisting of HVLA cervical manipulation and intermittent motorized traction. After 3 months of treatment, the patient reported complete resolution of primary symptoms with a concomitant retrieve of head posture and cervical lordosis, which was evident in the post-treatment radiograph [Figure 1b]. She was followed up for 4 years and showed no relapsing symptoms and lived a healthy life. Chiropractic manipulation in treating people with cervical radiculopathy is an emerging practice with evidence.[5,6,7] Correction of cervical misalignment itself can substantially help alleviate radiculopathy symptoms probably by mobilizing of restricted tissues, decompressing the entrapped nerve roots, and facilitating nuchal muscle strength.
Despite the existence of conflicting medical views, many authors have reported that chiropractic manipulative therapy is safe and beneficial for patients with cervical radiculopathy.[6,7] In a study conducted by Haldeman et al.[8] the potential risk of cerebrovascular insult associated with cervical manipulation was estimated to be 1 in 5.85 million while possible risk of serious gastrointestinal complications with non-steroidal anti-inflammatory drugs estimated by Sostres et al.[9] was 2% of the users. The overall neurological complications of posterior approach cervical surgery were estimated to range from about 15% to 25% in the current literature.[10] Chiropractic manipulation in this regard seems to be far safer than pharmacological or surgical intervention.
Randomized clinical trials have demonstrated spinal manipulation to be an effective treatment for cervical radiculopathy. In a study conducted by Christensen and Buswell[7] on the clinical outcomes of 162 patients with cervical radiculopathy treated with a chiropractic protocol, 85.5% had resolution of their radicular complaints in a mean of 9 treatment sessions. An investigation[11] of the efficacy of spinal manipulation for 50 patients with cervical radiculopathy from disc herniation, 85.7% reported significant improvement at 3 months with no adverse events. A systematic review by Galindez-Ibarbengoetxea et al.[12] on the effects of spinal manipulation in relation to neck pain showed that cervical HVLA manipulation resulted in improved cervical range of motion, increased mouth opening and increased pain-free handgrip strength, with large effect sizes. In a prospective cohort observational study[13] of 529 patients underwent cervical manipulation for neck pain with 1 year follow-up, the common adverse events were pain related, but rarely severe in intensity. Most of the patients report recovery in the long term. Rubinstein et al.[13] concluded that the benefits of chiropractic care for neck pain outweighed the potential risks associated with it.
Surgery, by nature, involves substantial injury of the tissues and peripheral nerves in the area (s) to be operated on. Persistent pain and functional limitations following surgery have been acknowledged since the advent of spinal surgery.[14] Surgery is typically reserved to be the treatment option of last resort if conservative treatments fail or neurological deficits worsen.[14] Nevertheless, the underlying biological mechanisms of spinal manipulation remain elusive.[15] There is a need of additional high-quality studies and much larger trials demonstrating the efficacy and safety of spinal manipulation for cervical radiculopathy and its comparison with other modalities which would do much to address the issues.
Primary care physicians are generally the first contact of any type of illness including cervical radiculopathy. Both the pandemic and continuous population aging have intensified an ongoing shortage of physicians. There is accentuated emphasis on task sharing between physicians and non-physician clinicians for shifting of non-communicable disease burden. Primary care physicians can make judicious decisions about the appropriate complementary approaches used together in a collaborative way. A broad understanding of each other’s scope of practice is important to make integrative healthcare more efficient.
Ethical statement
This article does not contain any studies with human or animal subjects performed by the author. The author attests that this case report was determined not to require Institutional Review Board/Ethics Committee review, and the corresponding protocol/approval number is not applicable as this was a retrospective case report.
Owing to the nature of the retrospective chart review, IRB approval is not required.
Declaration of patient consent
The author certify that he have obtained all appropriate patient consent forms. In the form, the patient has given their consent for their clinical information to be reported in the journal. The patient understands that his/her name and initials will not be published and due efforts will be made to conceal their identity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Iyer S, Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med. 2016;9:272–80. doi: 10.1007/s12178-016-9349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Geer CM. Cytokine involvement in biological inflammation related to degenerative disorders of the intervertebral disk: A narrative review. J Chiropr Med. 2018;17:54–62. doi: 10.1016/j.jcm.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benditz A, Brunner M, Zeman F, Greimel F, Florian V, Boluki D, et al. Effectiveness of a multimodal pain management concept for patients with cervical radiculopathy with focus on cervical epidural injections. Sci Rep. 2017;7:7866. doi: 10.1038/s41598-017-08350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bono CM, Ghiselli G, Gilbert TJ, Kreiner DS, Reitman C, Summers JT, et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011;11:64–72. doi: 10.1016/j.spinee.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 5.Chu ECP, Lim T, Mak KC. Cervical radiculopathy alleviating by manipulative correction of cervical hypolordosis. J Med Cases. 2018;9:139–41. [Google Scholar]
- 6.Murphy DR, Hurwitz EL, Gregory A, Clary R. A nonsurgical approach to the management of patients with cervical radiculopathy: A prospective observational cohort study. J Manipulative Physiol Ther. 2006;29:279–87. doi: 10.1016/j.jmpt.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Christensen KD, Buswell K. Chiropractic outcomes managing radiculopathy in a hospital setting: A retrospective review of 162 patients. J Chiropr Med. 2008;7:115–25. doi: 10.1016/j.jcm.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haldeman S, Carey P, Townsend M, Papadopoulos C. Arterial dissections following cervical manipulation: The chiropractic experience. CMAJ. 2001;165:905–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Sostres C, Gargallo CJ, Lanas A. Nonsteroidal anti-inflammatory drugs and upper and lower gastrointestinal mucosal damage. Arthritis Res Ther. 2013;15(Suppl 3(Suppl 3)):S3. doi: 10.1186/ar4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badiee RK, Mayer R, Pennicooke B, Chou D, Mummaneni PV, Tan LA. Complications following posterior cervical decompression and fusion: A review of incidence, risk factors, and prevention strategies. J Spine Surg. 2020;6:323–33. doi: 10.21037/jss.2019.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peterson CK, Schmid C, Leemann S, Anklin B, Humphreys BK. Outcomes from magnetic resonance imaging-confirmed symptomatic cervical disk herniation patients treated with high-velocity, low-amplitude spinal manipulative therapy: A prospective cohort study with 3-month follow-up. J Manipulative Physiol Ther. 2013;36:461–7. doi: 10.1016/j.jmpt.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Galindez-Ibarbengoetxea X, Setuain I, Andersen LL, Ramírez-Velez R, González-Izal M, Jauregi A, et al. Effects of cervical high-velocity low-amplitude techniques on range of motion, strength performance, and cardiovascular outcomes: A review. J Altern Complement Med. 2017;23:667–75. doi: 10.1089/acm.2017.0002. [DOI] [PubMed] [Google Scholar]
- 13.Rubinstein SM, Leboeuf-Yde C, Knol DL, de Koekkoek TE, Pfeifle CE, van Tulder MW. The benefits outweigh the risks for patients undergoing chiropractic care for neck pain: A prospective, multicenter, cohort study. J Manipulative Physiol Ther. 2007;30:408–18. doi: 10.1016/j.jmpt.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Daniell JR, Osti OL. Failed back surgery syndrome: A review article. Asian Spine J. 2018;12:372–9. doi: 10.4184/asj.2018.12.2.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gyer G, Michael J, Inklebarger J, Tedla JS. Spinal manipulation therapy: Is it all about the brain? A current review of the neurophysiological effects of manipulation. J Integr Med. 2019;17:328–37. doi: 10.1016/j.joim.2019.05.004. [DOI] [PubMed] [Google Scholar]


