Abstract
Since the appearance in the late of December 2019, SARS-CoV-2 is rapidly evolving and mutating continuously, giving rise to various variants with variable degrees of infectivity and lethality. The virus that initially appeared in China later mutated several times, wreaking havoc and claiming many lives worldwide amid the ongoing COVID-19 pandemic. After Alpha, Beta, Gamma, and Delta variants, the most recently emerged variant of concern (VOC) is the Omicron (B.1.1.529) that has evolved due to the accumulation of high numbers of mutations especially in the spike protein, raising concerns for its ability to evade from pre-existing immunity acquired through vaccination or natural infection as well as overpowering antibodies-based therapies. Several theories are on the surface to explain how the Omicron has gathered such a high number of mutations within less time. Few of them are higher mutation rates within a subgroup of population and then its introduction to a larger population, long term persistence and evolution of the virus in immune-compromised patients, and epizootic infection in animals from humans, where under different immune pressures the virus mutated and then got reintroduced to humans. Multifaceted approach including rapid diagnosis, genome analysis of emerging variants, ramping up of vaccination drives and receiving booster doses, efficacy testing of vaccines and immunotherapies against newly emerged variants, updating the available vaccines, designing of multivalent vaccines able to generate hybrid immunity, up-gradation of medical facilities and strict implementation of adequate prevention and control measures need to be given high priority to handle the on-going SARS-CoV-2 pandemic successfully.
Keywords: Omicron, Immune escape, Variant of concern, Vaccine failure, Omicron origin, Prevention and control
1. Introduction
It has been almost two years since the start of the coronavirus disease (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus – 2 (SARS-CoV-2), leading to more than 5.5 million deaths out of over 340 million confirmed cases reported worldwide as of January 21, 2022 (WHO, 2022). The virus has shaken the world economy, restricted the free movements, affecting millions of people and putting a burden on medical staff, that made them tired both mentally and physically, and emotionally fragile (Kutscher, 2021). The World Health Organization (WHO) is collaborating continuously with the public health institutions and scientists, and closely ministering the evolution and emergence of SARS-CoV-2 since January 2020 (WHO 2021a; WHO 2021b). In May 2021, WHO proposed nomenclature as variants of concern (VOC) and variants of interest (VOI) for classification of SARS-CoV-2 emerging variants for easy-to-pronounce and non-stigmatizing labels along with the scientific nomenclature that is used by researchers and academicians (WHO 2021b). The continuous emergence of several variants and mutants of SARS-CoV-2 from time to time has led to increased morbidity and mortality amidst different waves of pandemic within the ongoing pandemic resulting into high global health concerns and panics (Boehm et al., 2021; Thakur et al., 2021). After Alpha, Beta, Gamma and Delta SARS-CoV-2 variants, Omicron (B.1.1.529) variant has emerged recently during November 2021 as a highly mutated virus variant, classified as VOC by WHO on 26 November 2021, that is now attaining position of a dominant strain in several countries owing to its very high transmissibility (NewsNodes, 2022; WHO, 2021a; WHO, 2021c). The pattern of infection rate, higher transmissibility, and cases of immune evasion against acquired immunity with breakthrough infections in vaccinated individuals are so impulsive that Omicron spread rapidly worldwide in a short period of few weeks (Rahmani and Rezaei, 2021).
As per WHO, the VOI is a variant that contains the genetic changes that could be possibly linked to enhanced transmissibility, immune or diagnostic evasion, disease severity, identified as the cause of significant community transmission and increased prevalence, and having epidemiological impacts. On the other hand, a SARS-CoV-2 VOC is a variant that fulfills all the requirements of VOI, however, upon comparative assessment with other variants, it poses a threat of enhanced transmissibility, detrimental impacts on epidemiology, increased virulence or variability in clinical presentation, and decreased diagnostic, therapeutic, and vaccine interventions (WHO 2021a). The WHO established a group of experts as Technical Advisory Group on SARS-CoV-2 Virus Evolution (TAG-EV) to track, monitor, and evaluate the evolving situation on the pandemic virus, the WHO COVID-19 reference laboratory network, members of GISAID, Nextstrain, Pango, and scientific representatives from several nations and institutions. One of the tasks given to this group is to introduce non-stigmatizing and simplified labels of VOI and VOC into public audiences. Based on its easy-to-pronounce and practicability, the use of Greek Alphabet letters such as Alpha, Beta, Gamma, Delta, and presently Omicron, in the SARS-CoV-2 nomenclature, have been proposed by this expert group to mediate non-scientific public discussions, so as to improve public health awareness (WHO, 2021b).
The present article highlights the emergence of SARS-CoV-2 Omicron variant, its salient features and high global health concerns, and strategies to tackle it amid the ongoing COVID-19 pandemic. Various mutations present in Omicron that lead to enhanced transmissibility and immune evasion from vaccine induced or natural immunity obtained post infection have been discussed. We have done comparative analysis between other VOCs and Omicron in order to understand the similarities and differences. Various computational models have been developed to predict the mutants that might escape the immunity and were found efficient (Greaney et al., 2021; Miller et al., 2021). Escape mutants brings threat of rendering convalescent serum, vaccine and monoclonal antibodies (mAbs) ineffective (Planas et al., 2021; Dejnirattisai et al., 2021; Taylor et al., 2021), and this is true in case of Omicron also, it is found that after two doses of SARS-CoV-2 vaccine the Omicron neutralization is far less than Delta or parent SARS-CoV-2 virus (Garcia-Beltran et al., 2021; Natario, 2021; Barda et al., 2021). The experimental trials conducted by different groups of scientists and commercial companies revealed that the third dose of the vaccine (booster) significantly enhance neutralization of the Omicron (Nemet et al., 2021; Garcia-Beltran et al., 2021). Various diagnostic advances have been discussed here along with various therapeutic advances like ribonucleoside analogs, antivirals and monoclonal antibodies (Ferré et al., 2022; Graham, 2021; Wang and Yang, 2021, Falcone et al., 2021; Cameroni et al., 2021). Experimental evidences are suggestive of 70 times faster replication of Omicron in human bronchus while ten times slower in human lung tissue (Chi-wai, 2021; Dyer, 2021) that probably results in low disease severity. Despite presenting low disease severity, its higher transmissibility might present a threat for co-morbid patients (WHO, 2021a). Various strategies to tackle the rising Omicron pandemic that encompass the involvement of government organizations to ensure effective implementation of prevention, control and preparedness interventions (Luo et al., 2021), tie-ups with both public and private sectors to enhance the number of testings (CDC, 2021b) and introduction of strict measures and decisions by government based on scientific facts (Queen, 2022) are also discussed.
2. Emergence of omicron
The most recent novel SARS-CoV-2 variant was first reported from a specimen collected on 9 November 2021, which was initially named B.1.1.529 and later, on 26 November 2021, WHO designated the variant B.1.1.529 a VOC namely ‘Omicron” (WHO 2021c). Omicron is the most mutated SARS-CoV-2 variant with nearly 50 mutations accumulated in its genome, and is of particular interest and concerns since 26–32 mutations are in the viral spike (S) protein region (WHO 2021c), and out of these, 15 are in the receptor-binding domain (RBD) (ECDC, 2021a). Just three days after announcing the Omicron as VOC, on 29 November 2021, it was detected in Austria, Australia, Belgium, Canada, Czech Republic, Denmark, France, Germany, Italy, the Netherlands and the United Kingdom, and most of the cases being travel-associated (Petersen et al., 2022; Maxmen, 2021). Recently in Japan Omicron has been detected in two international travellers who travelled to Omicron undetected areas (Maruki et al., 2022). Subsequently, this newer variant rapidly spread to many countries, and as of January 22, 2022, Omicron has been reported from 150 countries and territories with nearly 0.5 million confirmed cases and 115 deaths (ECDC, 2021b; Mohapatra et al., 2021; NewsNodes, 2022). The effective (instantaneous) reproduction number of Omicron has been found to be 3.19 (95% CI 2.82–3.61) times higher than that of the Delta variant, therefore a rapid increase in Omicron cases may be observed in the coming time owing to its considerable advantage of higher transmissibility (Ito et al., 2021).
In addition, Omicron presents a shorter incubation period and clinical symptoms similar to or milder than the previous variants (Jansen et al., 2021). Preliminary data from disease surveillance program in Japan conducted by National Institute of Infectious Diseases, suggested that the viral RNA amount peaks at three to six days after onset of symptoms (NIID, 2022). This issue becomes particularly important when the isolation period in several countries such as England is reduced from 10 days to 7 days (Torjesen, 2022).
Though it appears that this variant has replaced older variants in South Africa, however, such reports could be biased considering that the virus characterization increased with the increase in the number of cases and remained primarily confined to the Omicron infected areas. Furthermore, a comparison of various Omicron strains revealed its origin in late September or early October, indicating that it is probably spreading more slowly than as being considered presently (Kupferschmidt, 2021a; Quarleri et al., 2021). In South Africa, since the start of the SARS-CoV-2 pandemic, children aged 10–19 years accounted for 9.2% of total COVID-19 cases, and this population is vulnerable to Omicron risk also (Lima et al., 2021).
Preliminary evidence from South African clinical study suggested a potential of Omicron variant to escape from immune responses and possess higher transmissibility that could lead to severe consequences (Cele et al., 2021; Vaughan, 2021). The possibility of such immune evasion by the Omicron variant is supported by an in vitro data obtained by Chinese scientist's that mutations at N440K, T478K, and N501Y sites attribute to ten times and two times higher infectivity to Omicron in comparison to initial SARS-CoV-2 variant and Delta variant, respectively (Chen et al., 2021a). In absence of Omicron specific vaccine, already approved vaccines form competent authorities might be used as countermeasure to reduce the circulating Omicron infection (Thakur and Kanta Ratho, 2021). Later, several researchers have reported evidences that Omicron variant could reduce the efficacy of COVID-19 vaccines and neutralization antibodies (antibodies-based immunotherapies) owing to its vast mutations (Callaway, 2021a; Cele et al., 2021; Chen et al., 2021a; Kozlov, 2021; Lu et al., 2021; Torjesen, 2021; Dejnirattisai et al., 2021; Kannan et al., 2022; X. Zhang et al., 2021, L. Zhang et al., 2021).
An artificial intelligence (AI) model, trained and validated with good number of experimental data point revealed that the Omicron variant could be ten times more contagious and twice more infectious than the Delta variant (Chen et al., 2021a). Since it is a common biological phenomenon to get mutations in virus and have multiple variants with ability to escape immune responses, it is too early to tell that Omicron is more benign than its previous variants. In fact, early indications are there revealing less severe symptoms than those of previous one and doctors attended larger number of mild cases in comparison to earlier waves. Also, current data as on 6th December 2021, indicated lesser number of patients seeking medical care with serious lung damage and demand of oxygen support than previous waves of COVID-19 pandemic (Vogel and Kupferscgmidt, 2021). However, as of 20 December, 132 hospitalized persons were diagnosed as confirmed Omicron, 17 of them had received a booster vaccine (a total of three doses), 74 had received two doses, eight had just got one dosage, 27 had not been vaccinated, and the vaccine status of 6 people was unknown. Additionally, within 28 days of omicron diagnosis, 14 patients from 52 to 96 years old died (Mahase, 2021a).
3. Where omicron fits in classical virology?
Coronaviruses (CoVs) are indifferent from other RNA viruses and are highly adaptable to the changing ecological niche through the high mutation rates attributed to several factors. Low fidelity RNA dependent RNA polymerase enzyme that accumulates mutations in the RNA genome (approximately 10-4 nucleotide substitution/site/year) and even higher mutation rates are present in SARS-CoV-2 that is causing the virus to adapt under even unfavorable conditions and may perpetuate to stay in the human host (Banoun, 2021). Further diversity in the genome is added by unique mechanism of viral replication, which is mediated through the “copy-choice” method and viral recombination (Terada et al., 2014). RNA-dependent RNA polymerase forms nascent cRNA and nascent RNA in the copy-choice model. Then, it dissociates from the original template and again binds to another RNA template at the identical or near-identical position and RNA synthesis is reinitiated, leading to recombination (Herrewegh et al., 1998). Template switching may occur at various sites. This template-switching results in the synthesis of new viruses as in case of Feline Coronavirus Type II Strains (viruses 79–1683 and 79–1146), which originated by event of dual recombination between Feline Coronavirus Type I and Canine Coronavirus (Herrewegh et al., 1998). It is clear that recombination in CoVs is possible between two genetically different parent viruses and progeny viruses may differ in cell culture and receptor usage (Terada et al., 2014). The emergence of VOC is very much likely due to the circulation of various strains. This Omicron variant picked up at least one mutation from another virus, presumably one that causes the common cold that makes it appear “more human,” helps it to escape from the human immune system and transmitted more easily while inducing a mild form of the disease (Lapid, 2021).
Generally, fitness and virulence attributes are considered a coupled phenomenon, but significant deviations have also been reported. If we take examples of vesicular stomatitis virus (VSV) and most RNA viruses having compact genomes, these are susceptible to point mutations and adaptability changes by only a few substitutions (Holmes, 2008; Domingo and Perales, 2018). On the other hand, viral fitness and virulence have complex determinants and are affected by complex cell specificities, viral-host, and virus-virus interactions. In a study done by Furio et al. (2012), quantification of the fitness and virulence of 21 single- or double-nucleotide mutants of the VSV was done, and a positive correlation between virulence and fitness was observed, however in a few mutants, both of these traits are independent. These workers found both the mutants with reduced fitness but unaffected virulence (single mutant) and high within-host fitness and low virulence (double mutant). Due to mutations owing to immune pressures, changing environment, or simply by error-prone replication machinery, viral quasispecies, which are well-defined mutants resulting from the complex mutation-selection process, are always present in a host cell niche. Out of them, it is likely to have the emergence of VOC, which are both high in fitness and virulence. In the case of Omicron, enhanced fitness is reported as evidenced by high transmissibility (WHO, 2021a); however, data on enhanced virulence is not so evident in the present scenario, which is somewhat relieving.
4. Theories on omicron emergence
A preliminary population-level unpublished study of Pulliam et al. (2021) indicated substantial immune evasion by the Omicron variant. However, the variant displays a decrease in the hazard coefficient for primary infection and an increase in reinfection hazard coefficient. The occurrence of mutations is common in viruses, and SARS-CoV-2 is not an exception; however, the scientific community's main concern owes to the accumulation of such a high number of mutations in the genome of Omicron variant (Kupferschmidt, 2021b).
Phylogenetic analysis of the Omicron variant was done by sequence alignment, pair-wise comparison, and identity matrix was generated. Evaluated using different model, Kimura model was found to make an entirely new monophyletic clade distant from other SARS-CoV-2 variants, however Jukes-Cantor model revealed a close relationship between alpha and Omicron variant, and it might be predicted that Omicron is between us possibly longer than we assume (Kandeel et al., 2021).
Sequence analysis of the Omicron variant revealed that mutagenic pressure is more significant on S1 than on S2, and is free from backbone hydrogen bonds, which increases the mutability. This fact may serve to predict the future possible mutation sites and be helpful in vaccine designing (Penner et al., 2021). Recently, Omicron has been classified into two different lineages BA.1 and BA.2, and few of the variations are unique while few are common to both. Both the BA.1 and BA.2 lineages contain 51 mutations, and among them, 32 are common in both while each lineage has 19 signature mutations. Among the 19 unique mutations in the S glycoprotein region, BA.1 include 13, whereas BA.2 contained seven unique mutations (Majumdar and Sarkar, 2021). One more lineage BA.3 is reported now (Desingu et al., 2022).
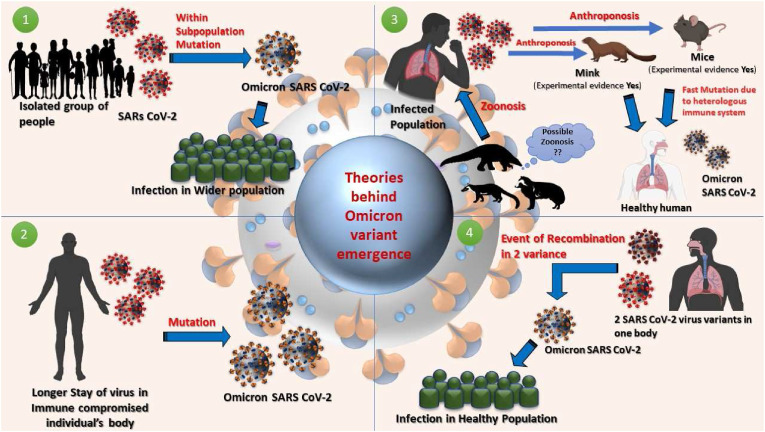
There are four possible theories/hypotheses behind the emergence of Omicron like VOC (Du et al., 2022; Lennerstrand et al., 2022; Sun et al., 2022). The first one is that virus started circulating and mutating in an isolated group of people, where it changes itself dramatically to be very different from the variants outside of that group and then it introduced itself into the wider population (Naveca et al., 2019, Sarah, 2021). Alternatively, the virus could have significantly remained for a more extended period in an immune-compromised person as in the case reported by Karim et al., (2021), where SARS-CoV-2 infection persisted longer than six months in a patient with advanced Human Immunodeficiency Virus (HIV) presented with antiretroviral treatment failure. Also, in the same patient, the emergence of the E484K substitution associated with immune escape and the N501Y substitution associated with most VOC were reported, strengthening the hypothesis of intra-host evolution of VOCs (Kupferschmidt, 2021c). mRNA- and non-mRNA-based vaccines may have a role in generating Omicron variants in a chronically infected COVID-19 patient, offering the chance for the virus to evolve and mutate, and acquire the ability to escape the body's immune response (breakthrough vaccine-induced immunity) (Li, 2021).
Another possibility of getting mutations so fast could be the back spillage of the virus into animals from the human host as it was reported by Oreshkova et al. (2020), where mink received the infection from humans, and the viral sequences from both the mink and human isolates were closely related. Zooanthroponotic transmission and implications of reintroduction into human populations, and zoonotic concerns of SARS-CoV-2 require deeper investigations, mink-to-human transmission of the virus has already been reported, and studies are underway to trace the origin of this pandemic virus (Banerjee et al., 2021; Holmes et al., 2021; Korath et al., 2021; Sharun et al., 2021a, 2021b). In different species, immune pressure might be different, which might contribute to the enhanced mutation rate. It is to be noted that SARS-CoV-2 emerging variants including delta variant have been reported from animals (Bonilla-Aldana and Rodriguez-Morales, 2021; Karikalan et al., 2021). SARS-CoV-2 vaccines for animals have also been developed recently, which could tackle this pandemic virus at the human-animal interface by reducing its circulation in animal population along with implementing one health strategies holistically (Chavda et al., 2021; Sharun et al., 2021c; Vandeputte et al., 2021). Moreover, one more theory is that if a person is infected with two coronaviruses, the chances of recombination are there, and Omicron could have gained so many mutations. Though the theory is skeptical, recombination events between SARS-CoV-2 variants are evident (Le Page, 2021). Insertional mutation ins214EPE is found in Omicron only and is absent in any of the previous SARS-CoV-2 lineage. Possibly this insertion has arose due to template switching during co-infection in the same host cell with other or SARS-CoV-2 virus (Venkatakrishnan et al., 2021). Recently, Wei et al. (2021) proposed a theory of mice origin of Omicron. The scientists explained molecular spectra of mutations, the relative frequency of 12 kinds of base substitutions. The phenomenon may be understood well with the example of G > U transversion that occurs in reactive oxygen species while cytidine deamination results in C > U transitions. Poliovirus, Ebola virus, and SARS-CoV-2 have shown similar molecular spectra of mutations if these mutations occur in the same host species, while different molecular spectra are exhibited if the species changes (Shan et al., 2021). Since the molecular spectrum of mutations is highly host-specific, the host for the Omicron virus can be determined by analysing the spectrum of mutations in Omicron. Upon investigation whether the mutational spectra of Omicron is consistent with the human cellular environment, a dissimilarity has been observed in the molecular mutation spectra of Omicron, and mutational molecular spectra in viruses evolved in human. Further investigation based on a comparison of molecular mutation spectra of various host species and then molecular docking revealed that pre outbreak Omicron mutations in the Spike protein significantly match the mutations present in mouse-adapted SARS-CoV-2, which could promote adaptation to mouse as a host, particularly via enhanced S protein binding affinity for the mouse cell entry receptor (Wei et al., 2021). The findings of this study suggest that the progenitor of Omicron might have jumped from humans to mice, gained mutations rapidly that facilitated the virus to infect the mice, then the virus jumped back into humans, reflecting an inter-species (human-mice-human) evolutionary trajectory to be responsible for the current outbreak of the Omicron variant.
The hypotheses concerning the emergence of Omicron are given in Fig. 1 .
Fig. 1.
SARS-CoV-2 variant (1) In a closed subgroup of the population, the virus circulates and mutates, which further infects the large population (Naveca et al., 2019); (2) In an immune-compromised individual the virus stays for a more extended period resulting in the accumulation of a more significant number of mutations (Karim et al., 2021); (3) From an infected individual, the virus transmits to animals, where the fast mutation occurs due to heterologous immune system, which could then possibly may infect a healthy human population (Wei et al., 2021); and (4) If one person, infected with two SARS-CoV-2 variants, there is a chance of recombination, and as a result, Omicron managed to gain so many mutations (Le Page, 2021).
5. Mutations in omicron and their biological consequences
Previously the deadly combination of K417N + E484K + N501Y mutations reported in beta and gamma were found to increase the transmissibility by 50% and resulted in higher hospitalization rates, ICU admissions, and deaths (Wahid et al., 2021). The Omicron variant contains at least 30 mutations (Kupferschmidt and Vogel, 2021) in spike protein, which includes Ala67Val, Δ69-70, Thr95Ile, Gly142Asp, Δ143-145, Δ211, Leu212Ile, Gly339Asp, Ser371Leu, Ser373Pro, Ser375Phe, Lys417Asn, Asn440Lys, Gly446Ser, Ser477Asn, Thr478Lys, Glu484Ala, Gln493Arg, Gly496Ser, Gln498Arg, Asn501Tyr, Tyr505His, Thr547Lys, Asp614Gly, His655Tyr, Asn679Lys, Pro681His, Asn764Lys, Asp796Tyr, Asn856Lys, Gln954His, Asn969Lys, and Leu981Phe, where 15 (residues 319–541) of these modifications reside in the RBD (Saxena et al., 2021). These mutations might affect the transmissibility of Omicron. Asn501Tyr enhances ACE2 receptor binding (Ali et al., 2021), thereby may help in transmission. D614G, N501Y, and K417 will likely make the Omicron more infectious (Poudel et al., 2022). D614G mutation is present in all the VOCs, and N501Y is also present in all VOCs, excluding the Delta variant (Shanmugaraj et al., 2021; Corum and Zimmer, 2021). Omicron contains several deletions and mutations those overlap with other VOCs (Dhawan et al., 2022).
While N501Y is associated with increased transmissibility, other mutations also enhance the affinity of spike towards ACE2 like in the B.1.429 lineage, the L452R showed higher ACE2 interaction (Gong et al., 2021). Kinases including PI3K/AKT are imperative to signalling in SARS-CoV-2 entry. Structure-prediction-based molecular docking analysis revealed that epidermal growth factor receptor might act as another potential acceptor in mutants having N501Y. Since several kinases are elevated in cancer patients, N501Y mutation containing lineages might have more detrimental consequences (Kazybay et al., 2021).
Furthermore, His655Tyr is adjacent to the furin cleavage point that can fasten the spike cleavage and help in transmission (Chen et al., 2021b). The mutations at position N679K, and P681H, which also exist in Alpha and Delta variants, could also increase the transmission ability of the virus (CDC, 2021a, Poudel et al., 2022, Thakur and Kanta Ratho, 2021). Asn679Lys present near the furin cleavage site enhances the polybasic nature and, therefore, might enhance cleavage and help in transmission (Tao et al., 2021). Pawłowski (2021) proposed that electrogenic mutations that cause the changes in the electrostatic force between the RBD of spike protein and ACE2 might be used as a strategy by the virus and resultant Coulomb attraction is higher and stronger in Omicron in comparison to the ancestral SARS-CoV-2 virus. Since ACE2 possesses patches of negative electrostatic surface potential, it is evident that higher positive potential of RBD will enhance the virus tropism, and indeed, the relationship between positive electrostatic potential and affinity of Delta variant for ACE2 has been evidenced by multiple replacements of neutral or negatively charged amino acids with positively charged amino acid (Pascarella et al., 2021a). If any direct relationship between the electrostatic potential and receptor affinity and infectivity persists, Omicron is anticipated to have more transmissibility and interact with other molecules like antibodies (Pascarella et al., 2021b). In-vivo studies must support this in-vitro data since the interaction between ACE2 and RBD is a complex process and is affected by the presence of several other mutations present in the spike protein, including a unique insertion at position 214 that might significantly affect the structure and function (Venkatakrishnan et al., 2021). Cryo-EM structural analysis of the Omicron variant spike protein complexed with human ACE2 showed formation of new salt bridges and hydrogen bonds involving the mutations at R493, S496 and R498 in RBD. These mutations possibly compensate for the other Omicron mutations like K417N known to reduce the affinity between the ACE2 and S protein (Mannar et al., 2022).
All the above data point towards the increased transmissibility potential of the Omicron variant. RNA-dependent RNA polymerase (Nsp12) and nonstructural protein 14 (Nsp14) are the proteins indispensable for viral replication, and it is still questionable whether mutations in these regions might confer higher mutation rates of Omicron (Gao et al., 2021). Omicron also possess mutations in the nucleocapsid protein (R203K and G204R), which are though not unique to the Omicron but are linked with enhanced subgenomic RNA expression (Leary et al., 2021) and viral replication (Mourier et al., 2021 Quarleri et al., 2021). The original SARS-CoV-2 has an R0 of 2.5, while Delta variant had an R0 below 7. The Omicron variant is suspected to have an R0 value as high as 10 (Burki, 2021) and its high doubling time is every 2–3 days which is making contact tracing difficult. The interaction between wild type ACE2-RBD and ACE-2-Omicron RBD was modelled using the CHARMM36 force fields. Atomistic molecular dynamics simulation studies was carried out using the GROMACS 5.1.2 package and mutations on RBD Omicron variant have been reported to result in stronger binding to human ACE2 receptor than wild type virus (Lupala et al., 2022). A comparative computational analysis between the Omicron and Delta variants showed that Omicron has a higher affinity for ACE2 receptors than the delta variant. Docking studies revealed that Q493R, N501Y, S371L, S373P, S375F, Q498R, and T478K are the mutations that contribute to higher affinity for ACE2 receptors. The Omicron variant possesses many hydrophobic amino acids such as leucine and phenylalanine in the RBD region that are essential for structural stability. Disordered regions of viral proteins are linked to viral pathogenicity and infectivity. Disorder scores more than 0.5 suggest inherent disorder, while scores between 0.2 and 0.5 are considered flexible. According to the intrinsic disorder score predicted by PONDR® VLXT, the Omicron variant has less disordered area than other variants and exhibits the disorder-to-order transition. In Omicron, this disorder-order transition region lies between 468 and 473 amino acid of spike protein (Kumar et al., 2021). The sequence analysis by Wang and Cheng (2021) revealed that the variant has two subclades and possibly it has arisen from clade 20B instead of currently circulating delta variant and alterations in the sequence might affect ACE2 receptor and/or antibody bindings. One more phylogenetic analysis based on the relative abundance of signature mutations revealed that Omicron is closely related to the Gamma variant. The analysis used the MAFFT program, and ten sequences were taken for each of the alpha, Beta, Gamma, Delta, and Mu variants (Kannan et al., 2022).
6. Major public health concerns related to omicron
Since the appearance of SARS-CoV-2, numerous mutations have been identified in different variants of this pandemic virus reported across the world. Modelling results of (ECDC 2021d) indicated that, by March 1, 2022, the Omicron VOC would become the majority variant (>50%) of SARS-CoV-2 infections in the European Union and European Economic Area (EU/EEA) countries. In the Kingston, Frontenac, Lennox & Addington (KFL&A) region of Canada, initial modelling estimated revealed the Re for Omicron at 1.5 (A. Li et al., 2021). The emergence of Omicron variant has raised high concerns owing it to be a most mutated SARS-CoV-2 variant with nearly 50 mutations being gathered in its genome and mainly because it had at least 30 mutations in the viral spike (S) region, particularly at the receptor binding domain (RBD). This increases the likelihood of reducing the efficacy of neutralizing antibodies obtained through infection with previous SARS-CoV-2, its variants or vaccination (Callaway, 2021b). The preliminary data is suggestive of the increased rate of reinfection in South Africa. Emerging evidence are there stating the reduced neutralization of some SARS-CoV-2 variants by post-vaccination serum (Harvey et al., 2021) as well as evasion of immunity from a prior infection in contrast to the Beta and Delta variants of SARS-CoV-2 (Pulliam et al., 2021). Contact tracing studies for Omicron conducted in Israel among multiple patients and healthcare workers exposed to a pre-symptomatic physician, who was triple vaccinated with BNT162b2 vaccine, revealed that out of 51 contacts, 88% were boosted (3 doses) with BNT162b2 vaccine and 92% were masked. And among all 51 contacts only one boosted primary contact was infected with Omicron. This shows the efficacy of vaccine and importance of infection preventive measures like masks (Leshem et al., 2022). Hereby in the below section the immune escape form natural infection induced immunity, vaccine induced immunity, mAbs and immune escape in presence of selective pressure have been discussed.
6.1. Natural immunity escape
When the convalescent sera of early strains infected subjects and Delta strain-infected patients were neutralized with pseudotyped Omicron S protein-expressing virus, the neutralizing antibody titre was 36 times lower for convalescent sera obtained from patients infected with early strains and 39 times lower for convalescent sera obtained from patients infected with Delta strain, suggestive of natural immune escape by Omicron (X. Zhang et al., 2021). A testing of 115 sera from vaccine recipients or convalescent individuals, revealed that Omicron partially or completely escape neutralization (Planas et al., 2021).
6.2. Evasion against vaccine-induced immunity
Even the vaccine-induced immunity can be evaded by Omicron variant, causing breakthrough infections in COVID-19 vaccinated individuals that are mainly characterized by either asymptomatic or mild symptoms. For example, within three weeks of the Omicron-emerged wave in South Africa, epidemiological surveillance concluded that two vaccine doses still protected individuals from severe disease (SAMRC, 2021). However, a little protection against infection with the Omicron variant was reported by two doses of the AstraZeneca or Pfizer-BioNTech vaccines (Dejnirattisai et al., 2021). The patients infected with multiple spike variant produce wider breadth of protection in cross neutralizing the Omicron and hence contribute knowledge towards booster strategies (Laurie et al., 2021). In a live virus microneutralization assay, Omicron variant strains HKU691, and HKU344-R346K were tested with sera from 25 BNT162b2 and 25 Coronavac vaccine recipients. In 20% and 24% of BNT162b2 recipients, detectable neutralizing antibodies against HKU691 and HKU344-R346K were observed, respectively, while none of the Coronavac recipients showed detectable neutralizing antibodies against any of these two Omicron variant strains (Lu et al., 2021). The UK Health Security Agency suggested that 25 weeks post-vaccination with two shots of SARS-CoV-2 vaccine, the protection against symptomatic infection is only 10% compared to 40% protection against Delta variant (Burki, 2021). More details have been presented in the later section “SARS-Cov-2 vaccine efficacy against Omicron” of this review.
6.3. Immune escape against monoclonal antibodies
A computational analysis revealed that insertions and deletions in the N3 and N5 domains of spike protein hinder the binding of neutralizing antibodies (NAbs) (Andreano et al., 2021b). Andreano et al. (2021b) experimented with taking serum from 10 vaccinated donors with BNT162b2 mRNA vaccine. In the experiment, scientists attempted to evaluate the virus neutralization against different VOC by B cells and antibody response generated against vaccines at the individual cell level. Approximately 6000 cells were sorted, and near 3000 cells could produce monoclonal antibodies (MAbs) against S protein. Antibodies from more than 400 cells neutralized the wild-type SARS-CoV-2 virus that originated in Wuhan. However, variants showed variable degrees of neutralization and escaped from neutralization. The beta and gamma variants escaped 70% antibodies compared, while comparatively a smaller portion of antibodies are escaped by Alpha and Delta (Andreano et al., 2021b). Nine mAbs those are either clinically approved or in development for treatment (Taylor et al., 2021), completely failed to neutralize Omicron (Planas et al., 2021). For the mutations at E484A and K417N, many of the commercial mAbs preparations are ineffective, and greater resistance is exhibited (Ai et al., 2021). The lower level of protection could be attributed to the immune escape since several of the mutations in the Omicron are present in the area likely to bind neutralization antibodies and compromise the immune defence against Omicron (Callaway and Ledford, 2021). Casirivimab and Imdevimab mAbs presented robust neutralization against Delta variant but remained ineffective against Omicron when assessed using a peusotyped SARS-CoV-2 virus-like particles having mutations in all four structural proteins (Syed et al., 2022). A panel of anti-RBD mAbs encompassing S309 (parent mAb of sotrovimab), COV2-2196, COV2-2130 (parent mAbs of AZD8895, AZD1061), REGN10933, REGN10987, LY-CoV555 LY-CoV016 and Celltrion (CT-P59) intended for clinical use were tested for Omicron neutralization. LY-CoV555, LY-CoV016, REGN10933, REGN10987 and CT-P59 mAbs were completely ineffective against Omicron in both Vero-TMPRSS2 and Vero-hACE2-TMPRSS2 cells while combination of COV2-2196 and COV2-2130 or S309 were minimally effective (VanBlargan et al., 2022).
More details about effectiveness of different mAbs have been discussed in the later section “Therapeutic advances against Omicron” of this review.
6.4. Immune escape in presence of selective pressure of antibodies
How could the selective pressure of polyclonal immunity in convalescent or vaccinated people, responsible for generating variants that could be VOC, tested? Immune escape against natural To determine whether the currently available vaccines will remain efficacious against the emerging VOCs, an experiment was conducted by Andreano et al. (2021a) to estimate the escape of viral particles from herd immunity and antibody treatment. In the experiment, plasma from 20 convalescent patients was collected and incubated with the virus isolated from Wuhan for three months. Up to seven passages, the serum was able to neutralize the virus; however, after 45 days, the deletion of F140 in the spike protein resulted in a partial reduction in neutralization. On day 73rd, E484K substitution in the RBD and on day 80th, an insertion led to the generation of a new glycosylation site resulting in an entirely new variant that was completely resistant towards plasma neutralization (Andreano et al., 2021a). This E484K substitution is present in Omicron (Kupferschmidt, 2021c).
7. Prediction of escape mutants through bioinformatics analysis
Deep mutational scanning experiments facilitate to measure the impact of viral mutations on antibody binding or neutralization. Greaney et al. (2021) developed an escape calculator based on experimental data obtained for 33 monoclonal antibodies to assess antigenic effects of various mutations in the RBD region of SARS-CoV-2. An interactive version of the calculator is at https://jbloomlab.github.io/SARS2_RBD_Ab_escape_maps/escape-calc/, and the calculator suggests that extensive changes are present in the new omicron variant. Furthermore, the results of the escape calculator are correlated well with the neutralization assays of human polyclonal sera (Greaney et al., 2021). Miller et al. (2021) described the mutational landscape of the Omicron variant using amino acid interaction (AAI) networks, and the study revealed that antibody escape breadth is increased in the Omicron owing to the mutations in class 3 and 4 antibody epitopes and simultaneously escape depth is also increased owing to the mutations in the class 1 antibody epitopes. In particular, subclades bearing R346 S/K mutations are advised to be taken care of for escape.
8. Is natural infection followed by vaccination provides superior protection against omicron?
Reports are there which are stating that vaccination post natural infection (hybrid immunity) generates more NAbs against Omicron variant (Callaway, 2021a; Schmidt et al., 2021a) instead in vaccinated people who don't have previous infection history. Similar results were obtained by Cele et al. (2021), who performed a focus reduction neutralization test (FRNT50) with plasma obtained from BNT162b2 vaccinated and both BNT162b2 vaccinated and previously infected patients either with Delta variant or ancestral strains. They found that the Omicron live virus neutralization was 22 folds less than the ancestral D614G strain for the vaccinated and prior infected people. Using the same FRNT50 assay, BNT162b2 vaccine efficacy was estimated in preventing Omicron symptomatic infection, and the vaccine efficacy was 73% (95% CI 58–83%) for vaccinated and prior infected individuals and 35% (95% CI 20–50%) for vaccinated only participants.
9. Booster shots of vaccines
The importance of third vaccination with BNT162b2 is underscored, owing to at least 100 factors high neutralization efficacy after a third shot against the omicron variant (Nemet et al., 2021); and other researchers have also obtained similar results (Garcia-Beltran et al., 2021), who revealed that the vaccine's ability is compromised in protecting against infection (Cele et al., 2021). In accordance with the results of Cele et al. (2021), Schmidt et al. (2021b) also found that the sera from people who had been vaccinated with two mRNA vaccine doses were 30- to 180- fold less effective in neutralization against Omicron, while the sera from patients previously infected or patients vaccinated with three doses of mRNA vaccine showed 38–154 fold increase in the neutralization of Omicron. Doria-Rose et al. (2021) reported 49–84 folds less neutralization than the initial SARS-CoV-2 strain in serum samples obtained from subjects vaccinated with 100 μg mRNA-1273. All the results suggest the importance of boosting doses in increasing the neutralization against Omicron (Garcia-Beltran et al., 2021; Natario, 2021; Barda et al., 2021). There is a requirement for vaccine manufacturer to be alert to customize the vaccine as per need of heavily mutated coronavirus strains. Such preparedness programs will help in mitigating the serious consequences arose due to emergence of new mutated variants. Both the Pfizer and BioNTech have claimed after necessary laboratory testing that the three doses of their mRNA vaccine are able to contest Omicron variant effectively (Sohan et al., 2022). A data driven analysis using a library of 132 known antibody and S protein complexes, binding free energy changes for 15 RBD mutations on these complexes were evaluated to determine the possible impact of Omicron mutations on vaccine efficacy. The study revealed that Omicron RBD mutations might significantly change the binding patterns of known antibodies and overall analysis indicated that the changes that reduced the binding between the antibody and RBD complexes were more prominent than those enhanced the binding, indicative of severe disruptive impacts. It further suggests that the changes occurred in Omicron are favoring vaccine escape. Among the 15 RDB mutation, K417N (a mutation common with beta variant), and E484A are the mutations that lead to overwhelmingly disruptive effects to many known antibodies (Chen et al., 2021a). The sera from the individuals vaccinated by two doses of inactivated whole-virion vaccines (BBIBP-CorV) showed reduced neutralization by Omicron, however homologous or heterologous vaccination with protein subunit vaccine (ZF 2001) enhance neutralization against the Omicron (Wang et al., 2022). Homologous boosting with BBIBP-CorV vaccine 9 months post two dose vaccination schedule in a cohort of 292 participants, revealed that in 78.08% participants Omicron got neutralized (Yu et al., 2022). Nevertheless, this increased protection against Omicron may decrease more quickly than against Delta, with a 15–25% reduction in protection after ten weeks following the booster (Mahase, 2021a). Vesicular stomatitis virus (VSV) pseudoparticles expressing spike of SARS-CoV-2 was used to evaluate the magnitude and breadth of the neutralizing antibodies in infected and vaccinated individuals with mRNA-vaccine. The analysis revealed that though boosting with third dose enhanced the neutralization capacity, however Omicron is most resistant to neutralization in comparison to other VOCs and the boosting remained unable to evoke high response in pregnant vaccinated women. The findings are suggestive of considerable heterogeneity in the magnitude and breadth of neutralization responses of Omicron in different groups (Sievers et al., 2022). After 2 doses of Heterologous vaccination with CoronaVac vaccine there was no detectable Omicron neutralization but when boosted with BNT162b2, it showed 1.4 fold higher neutralization in comparison to 2 doses of mRNA vaccine (Pérez-Then et al., 2022).
10. What if neutralizing antibodies are partially effective against omicron
Multiple evidences are reflecting that Omicron variant escape neutralizing antibodies and therefore less neutralizing abilities of convalescent serum is observed. However immune system still can fight Omicron owing to the opsonizing function of non-neutralizing antibodies and cell mediated immunity.
10.1. Efficacy of non-neutralizing antibodies
Neutralizing antibodies at one hand target limited region of viral spike specifically involved in attachment and/or fusion, while on the other hand antibodies mediating Fc activity may bind across the entire antigenic area. The Fc activity only requires the antigen-antibody complex in such a manner that Fc region of antibodies are accessible to immune cells. Thus even in the absence of neutralizing antibodies, non-neutralizing antibodies may continue to opsonize the Omicron and Omicron infected cells. The three vaccines viz. BNT162b2 and mRNA-1273 mRNA vaccines, and CoronaVac presented a persisting higher opsonophagocytic FcγR2a and cytotoxic FcγR3a receptor binding activity that continued to recognize, bind, and clear the virus even in the absence of antibody mediated neutralizing activity (Bartsch et al., 2021).
10.2. T cell immunity obtained from natural infection and vaccination
While it is critical to know the extent to which humoral response will be effective against Omicron, it is generally difficult for the virus to escape T cell response due to a broad response generated and a variety of HLA haplotypes present. T cell response lasts longer after infection or vaccination than antibodies, and the T cells recognize more sites on S protein than antibodies, this present greater ability to recognize altered variants (Ledford, 2022). In an analysis of estimating the impact of Omicron mutations on the binding of CD4+ and CD8+ T to epitopes present on S protein, over two third of the immune response remained unaffected from mutations. Since Omicron mutations are mainly present in Spike protein, over 95% T cell epitopes present in other genes remained unaffected by mutations (May et al., 2021). In one of the experiments conducted by Redd et al. (2021) in the direction of determining the T cell immune response escape, it was found that out of 52 potential epitopes specific against CD8+ T cell responses, only one epitope showed cross over and only 2/30 individuals contained the change in amino acid present in Omicron. It indicated that in virtually all the participants, Omicron had been recognized by existing anti-SARS-CoV-2 CD8+ T-cell responses, which eliminates the possibilities of T cell immunity escape during the evolution of the SARS-CoV-2 virus. SARS-CoV-2 spike-specific CD4+ and CD8+ T cells have been found to be elicited during natural infection or vaccination with BNT162b2, and cross recognized Omicron at 84% and 91% levels in SARS-CoV-2 infected and vaccinated subjects, respectively. Examination of 454 major histocompatibility complex (MHC) class I-restricted CD8+ T cell epitopes identified through activation-induced marker assays, revealed 96.7% epitopes to be fully conserved in Omicron variant (Tarke et al., 2021). Examination of 280 MHC class II-restricted CD4+ T cell epitopes revealed conservancy of 90.0% of CD4+ T cell epitopes (Choi et al., 2022). Overall examination revealed that T cell epitopes of SARS-CoV-2 proteins are highly conserved in Omicron, suggestive of possible protection imparted through T cell memory during reinfection or breakthrough infection with Omicron (Gao et al., 2022; Faraz Ahmed et al., 2022).
11. Is the severity for omicron is less than its other VOC cousins?
Early studies revealed that Omicron is less severe than other variants, with a risk of hospitalization ranging from 15% to 80% lower than the Delta variant (Christie, 2021; Wolter et al., 2021). Omicron possibly not causing severe illness, especially in vaccinated people and those administered a booster shot (Burki, 2021; Garcia-Beltran et al., 2021; Khan et al., 2022; Mahase, 2021d ; Tanne, 2021b). Most of the reported cases are confined within the term of clinically asymptomatic or mild cases (ECDC, 2021b; NewsNodes, 2022). The symptoms of the Omicron variant are runny nose, headache, fatigue (either mild or severe), sneezing, and sore throat (Iacobucci, 2021a; Mohiuddin and Kasahara, 2021). However, the children have been involved in the Omicron-led fourth wave in South Africa, where the preliminary data suggested that children's risk of hospital admission is 20% higher than the D614G-led first wave (SAMRC, 2021). Hong Kong University researchers revealed in ex vivo culture studies that Omicron replicates 70 times faster than Delta in human bronchus while ten times slower in human lung tissue, and possibly it explains the lower severity of disease in Omicron infected patients (Chi-wai, 2021; Dyer, 2021).
Omicron variant replicates at lower levels in Calu3 and Caco2 cell lines. Also Omicron is inefficient in using transmembrane serine protease 2 (TMPRSS2) in comparison to other VOCs. In the Omicron infected K18-hACE2 mice, virus replication is low in upper and lower respiratory tract resulting in ameliorated lung pathology (Shuai et al., 2022). In the lung cells (expressing TMPRSS2), and lung organoids, Omicron virus appeared to replicate at a lower level in comparison to Delta (Meng et al., 2021; Kozlov, 2022). Experimental infection with Omicron live virus in C57BL/6 mice, BALB/c mice, K18-hACE2 transgenic mice (expressing hACE2 under an epithelial cytokeratin promoter) and Syrian hamsters, showed clinically less severe morbidity in comparison to Beta and Delta variants (Diamond et al., 2021). Similarly, hamsters infected with wild type SARS-CoV-2, Alpha, Beta, or Delta strains showed a weight loss upto 10–17% by day 6 of infection, while hamsters infected with Omicron did not result in detectable weight loss despite higher challenge doses (McMahan et al., 2022). With pseudotyped Omicron particles bearing all the S mutation with HIV virus backbone, a lower entry efficacy and less proteases cleavage have been observed in Omicron, suggestive of low replicative efficacy in HEK293T cells or ACE2 receptor expressing A549 cells (Hu et al., 2022). While using the SARS-CoV-2 virus-like particles (VLPs) harbouring all the mutations present in the four structural genes of Omicron revealed an increase in infectivity (Syed et al., 2022). The difference in results between the pseudotyped Omicron particles (Hu et al., 2022) that exhibit a lower entry efficacy and in SARS-CoV-2 like VLPs having Omicron like mutations that exhibited increased infectivity, possibly owing to the types of mutations incorporated in the said viruses and the cell line used for assay. E484K mutation is present in Beta and Gamma variants (Kannan et al., 2022), while it is mutated to E484A in Omicron. The E484K substitution in Gamma variant is found to be associated with the capacity to cause reinfection (Resende et al., 2021). This altered ability of Gamma variant to be more efficient in causing reinfection possibly is attributed to the change of negatively charged, hydrophilic residue (glutamic acid) to positively charged, relatively high hydrophilic amino acid (lysine). The Omicron presents different reinfection ability possibly owing to change of amino acid from Glutamic acid to hydrophobic amino acid (alanine), which may change the interactive forces between ACE2 receptor and might play a role in altering the interaction between ACE2 receptor and RBD. The electrostatic potential of RBD domain of Omicron is higher than in comparison to Delta resulting in reduced affinity for the ACE2 receptor. Omicron N terminal domain has also poor affinity for lipid rafts that made Omicron less fusogenic and low pathogenic (Fantini et al., 2022). In spike protein, Omicron is having 5 additional positively charged amino acids in comparison to wild type virus that is enhancing the binding of Omicron virus with the cellular targeted drug development (Nie et al., 2022).
So far, the clinical characteristics of reinfection cases with Omicron are mild (Vogel and Kupferscgmidt, 2021). On 14 December, the South African private health insurer Discovery Health in Johannesburg declared that the risk of hospitalization is 29% lower in Omicron infection than the person infected with previous strains (Ledford, 2021), and this is something a glimmer of hope.
12. Diagnosis of omicron
Antigen-based tests are less sensitive than RT-PCR-based tests; however, when the viral load is high, they quickly detect the positive individuals and hence are of utility in clinical settings and are approved in many countries for self-testing. Deerain et al. (2021) evaluated ten commercial kits for their diagnostic potential, and they found that all the ten kits were able to detect both the Delta and Omicron variants. The detection limit was 6.50 log10 copies per mL and 6.39 log10 copies per mL for Delta and Omicron, respectively (Deerain et al., 2021). SARS-CoV-2 has undergone a broad process of recombination and mutation since its detection and has generated wide varieties of both the VOIs and VOCs. Due to variations in the targeted area, S gene dropouts have been reported, and hence reliability of currently used detection systems is also under question. The immunoassays based on coated antigens with prototype SARS-CoV-2 virus may not necessarily detect the antibodies against currently circulating variants and hence there is a compelling need of regular re-evaluation and revalidation of live virus neutralization assays based on emerging VOIs and VOCs (Lippi et al., 2021).
The Omicron is detectable by the current RT-PCR test (ThermoFisher TaqPathTm kit available by Applied Biosystems). However, reports are there for S gene target failure (SGTF), giving a false negative result; though, a sudden enhancement in the SGTF (S gene dropout) might be taken as an indicator of the appearance of Omicron with a reduced circulation of other variants. We have evidentiary proofs from the field from Switzerland and Liechtenstein. Data of most frequently used SARS-CoV-2 PCR tests targeting different sites (including the ORF1ab region (N = 16), the RdRp gene (N = 13), the S gene (N = 8), the E gene (N = 11), the N gene (N = 32) and, M gene (1) have been collected by Metzger et al. (2021). When S gene dropouts were considered, out of 8 assays available, out, only two assays showed S gene drop out for Omicron hence still, S gene dropout cannot be considered as a marker for the presence of Omicron and confirmation of the presence of Omicron should be supported by the gene sequencing data analysis (Metzger et al., 2021; Torjesen, 2021).
Neopane et al. (2021) developed a TaqMan SARS-CoV-2 mutation panel molecular genotyping assay that was able to differentiate variants B.1.617.2 (Delta), B.1.1.7 (Alpha), B.1.526 (Iota), B.1.351 (Beta), P.1 (Gamma), P.2 (Zeta), B.1.617.1 (Kappa) and B.1.427/B.1.429 (Epsilon). The assay is highly useful in the present scenario and can be used in surveillance and epidemic control. However, the challenges still remain for the rapid development of the testing kit to fulfil the extensive requirements of the pandemic. To accelerate the assay development and attaining its approval, in the United States, the emergency use authorization (EUA) has made the approval workflow easier. Such efforts have enabled governments to significantly increase the number of testing in the emergence of new variants (Thomas et al., 2021). Next-generation sequencing (NGS) of the whole genome of Omicron might serve as the gold standard for diagnosis and variant identification despite being time consuming and costly. When the data of Allplex SARS-CoV-2 Master Assay and Variants I Assay were compared with NGS as reference for 115 samples, the sensitivity for detection of spike mutations were 98.7% and 100%, respectively for Allplex Master Assay and Variants I Assay (Fu et al., 2022). Multiplex RT-PCR to detect SARS-CoV-2 VOCs and spike variant PCR assays can have the utility to quickly monitor selected VOCs in resource-limited settings, however may require updates as new variants emerge (Fu et al., 2022). During the SARS-CoV-2 genomic surveillance in the state of Georgia, a combination of Spike SNP PCR assay (taking only 2 h and 12 min run time) and genome sequencing and lineage classification (72 h) provided an on time diagnosis for Omicron. Additionally, the SNP analysis enabled the assay to distinguish between the other VOCs and Omicron and the assay may be further modified as per the requirements to detect new mutations if required (Sexton et al., 2022). Omicron has been detected in an aircraft wastewater sample using the CDC N1, CDC N2, and del (69–70) RT-qPCR assays per guidance from the WHO and sequencing further confirmed the presence of Omicron belonging to BA.1 sub-lineage (Ahmed et al., 2022).
Testing strategies should be flexible to changes in the epidemiological situation and local epidemiology, population dynamics, and resource availability. In addition, appropriate sample and technique selection are critical to the testing strategy's effectiveness, and it is highly reliant on the testing strategy's specific public health objectives such as assessment of different variant circulation and outbreaks, selection of representative samples for sequencing, monitoring the virus evolution and vaccine efficacy assessment. Therefore, on 20th December 2021, the European Center for disease prevention and control (ECDC) and the WHO Regional Office for Europe developed the first update for methods and strategies for detecting and characterizing SARS-CoV-2 variants (ECDC, 2021c).
13. Is previous SARS-CoV-2 infection increase susceptibility to omicron?
In UK analysis published in 23 December 2021, people who had previously been infected with SARS-CoV-2 were more likely to get infected with omicron than with earlier variants, with 9.5% of those affected having a history of infection (Mahase, 2021a). Moreover, Mahase (2021a) suggested that this statistic is likely to be underestimated because some patients are unaware that they have had past asymptomatic infections. As a result, they are not counted in the total tally. While studying the transmission dynamics of Omicron in immunocompetent and immunosuppressed populations, it was found that in comparison to other VOCs, asymptomatic carriage is increased to 16% in both people living with HIV and people living with HIV/AIDS in comparison to 2.6% during the Beta and Delta outbreaks (Garrett et al., 2022).
14. SARS-Cov-2 vaccine efficacy against omicron
A study encompassing a small group of subjects (n = 12) observed that the efficacy of the Pfizer-BioNTech vaccine is 41 folds lesser for Omicron against classical SARS-CoV-2 (Cele et al., 2021). Pfizer Company obtained similar results, who reported that the third dose of vaccine could prove the similar level of neutralizing antibodies obtained after two doses against the classical virus (Mahase, 2021b).
In late November 2021, Omicron caused an outbreak in Norway suggestive of high transmissibility despite complete vaccination. In a party attended by 117 people, an attack rate of 74% was observed with Omicron, and all developed symptoms. However, none of them required hospitalization. Ninety-six percent of the attendees were fully vaccinated and still developed the symptoms (Brandal et al., 2021) that are evidentiary proof of the vaccination failure on Omicron infection. As of 9 December 2021, 785 Omicron cases have been reported in Denmark. 76% were fully vaccinated, while 7.1% were boosted with the third dose. In 76% of cases, symptoms were reported with the requirement of hospitalization in 9 patients, and no death was reported (Espenhain et al., 2021). In South Africa, two doses of the Pfizer-BioNTech vaccine provided 70% protection against hospitalization and 33% protection against infection instead of 93% and 80%, respectively, for the Delta variant (SAMRC, 2021). A robust IgA and IgG response has been evoked in individuals receiving either BNT162b2 (Pfizer/BioNTech) or mRNA-1273 (Moderna) vaccination (n = 578). The neutralization was higher in mRNA-1273 vaccinees those previously had symptomatic SARS-CoV-2 infection (Moncunill et al., 2022). Though the Omicron variant compromised the effectiveness of 2 doses of mRNA vaccination and reduced overall protection, it can still protect against severe consequences (Tanne, 2021a). Previous viral infection or vaccination is however partially protecting against hospitalization and severe consequences during Omicron infection, as per Singhal (2022), though there is no notable impact of vaccines against spread of Omicron. Serum samples from infected and then vaccinated (convalescent–vaccinated) or been vaccinated and then gained infection (vaccinated–convalescent) were tested for neutralizing antibodies. Both the convalescent–vaccinated or vaccinated–convalescent samples showed Omicron neutralization, though to a lesser extent than Delta; however in above case Omicron neutralization was little higher in case of convalescent–vaccinated serum (Rössler et al., 2022). An antibody waning has been observed 6 months post second vaccination dose and prior to third boosting dose, especially those receiving two doses of AstraZeneca ChAdOx1 nCoV-19 (Faustini et al., 2022). In addition, a mouse-adapted strain containing all the five mutations present in Omicron also (K417, E484, Q493, Q498, N501) in spike region when expressed from the highly attenuated, replication-competent vaccinia virus vector NYVAC-KC, it provided 100% protection from death but not from symptoms (Kibler et al., 2021). A single dose ChAdOx1 nCoV-19 vaccine is able to elicit a greater level of antibody response with prior infection and it was comparable with that of two vaccine doses (Gelanew et al., 2022). This data is important and helpful in reducing the requirement of vaccine doses for resource-limited countries. In cancer patients, mRNA vaccines showed 4.2-fold and 21.3-fold lower efficacy against Delta and Omicron variants, and after boosting it was 3.6-fold and 5.1-fold lower for Delta and Omicron, respectively. It showed the effectiveness of boosting strategies in immunocompromised groups including cancer patients (Zeng et al., 2021). In multivariable Cox proportional hazards regression analysis in the previously infected subjects, significant lower risk of infection with Omicron was not demonstrated but in vaccinated individuals it was reported (Shrestha et al., 2022).
15. Readiness for omicron specific vaccine
Since the previously developed vaccines are not entirely efficacious, Pfizer-BioNTech and Moderna, the manufacturers of the two mRNA vaccines, claimed that they could make an mRNA-based vaccine against Omicron in 100 days (Burki, 2021). Encouraging updates from Pfizer and BioNTech as well as Moderna in the preparation of Omicron-specific vaccine (Mahase, 2021c) could lead to an optimistic future to combat the Omicron variant of SARS-CoV-2.The continuous evolution of SARS-CoV-2 and the situation being out of control contributes to the COVID-19 pandemic's prolongation, putting the entire world at risk of COVID-19 and its devastating impacts on global health and severe economic consequences (Petersen et al., 2022). However, opinion of evolutionary biologist Jesse Bloom is somewhat relieving who is telling that Omicron would not be eradicated, rather it will permanently establish itself in human like other seasonal CoVs and have been circulating in human being since decades (Callaway, 2021c).
16. Therapeutic advances against omicron
Several repurposed drugs including antivirals and immunotherapies (antibodies-based) have been suggested for use in emergency purposes to ameliorate the disease severity in patients with COVID-19, while many drugs and therapies are still under investigations and trials, however most appropriate choices are still awaited to define optimal COVID-19 treatment (Bae et al., 2021; Rabaan et al., 2021; Zou et al., 2021; NIH, 2022). In this section, we are presenting some recent advances in drugs and therapies which could be suitable for Omicron.
16.1. Ribonucleoside analog
Presently a ribonucleoside analog and a protease inhibitor are being used against SARS-CoV-2. The mode of action of these two antivirals seems to remain unaffected since the target of these two antivirals are NSP14 and NSP5 genes, and Omicron showed only one mutation in each of these genes. However, the efficacy of these antivirals has not been proven yet, even for Delta variants (Ferré et al., 2022). Also, recently, a candidate drug named ResCovidin™ was developed that blocks all the ports of SARS-CoV-2 entry, and it may prevent the infectivity of Omicron (Fang and Shi, 2021).
16.2. Antivirals
Recently, an oral antiviral drug with anti-RNA polymerase activity, Molnupiravir (Lagevrio®), has been approved by the FDA's Antimicrobial Drugs Advisory Committee as first oral antiviral drug for COVID-19 and others are also likely to appear shortly (Fan et al., 2021; Lee et al., 2021; Persad et al., 2021; Pourkarim et al., 2022). Apart from Molnupiravir, one more antiviral drug nirmatrelvir/ritonavir [PaxlovidTM (PF-07321332 + ritonavir), Pfizer] has shown promising results in clinical trials to protect from serious COVID-19 illness, and FDA has recently granted emergency use authorization (EUA) for this oral antiviral drug (Graham, 2021; Mahase, 2021e; Wang and Yang, 2021). Such antiviral oral drugs and pills have raised new hopes of COVID-19 treatment and slashing hospitalization amid threats of Omicron and other variants such as Delta, and could be helpful in changing the ongoing pandemic's course (Fan et al., 2021; Couzin-Frankel, 2021; Graham, 2021; Parums, 2022).
16.3. Monoclonal antibodies
As of now, eight authorized or approved mAbs are there for the treatment; out of them, seven Mabs (bamlanivimab, etesevimab, casirivimab, imdevimab, cilgavimab, tixagevimab and regdanvimab) block binding of viral S protein to ACE2. Omicron variants showed that mutations in the virus affected antibody binding of authorized therapeutic antibodies, including Casirivimab + imdevimab combination and Bamlanivimab + etesevimab combination (Falcone et al., 2021). Early modelling studies have predicted that the REGN-COV2 (Casirivimab and Imdevimab), as well as the Rockefeller University antibody C135 are still efficacious against the omicron (Chen et al., 2021a; Aleem et al., 2022). NA8 and NE12 are the prophylactic and therapeutic antibodies that are developed using combinatorial antibody phage-display library methodology, and are effective against Omicron in picomolar concentrations (Chen et al., 2022). Future strategy to combat Omicron requires high potency drugs which could reduce viral replication and spreading, and be effective against all the circulating variants, including any possible variants that could emerge (Fang and Shi, 2021; Mohiuddin and Kasahara, 2021). Omicron mutations did not affect the binding of Sotrovimab (S309) or Tixagevimab + Cilgavimab combination (Miller et al., 2021). Similar results were obtained by Hoffmann et al. (2021), who reported resistance of Omicron spike towards many commercial therapeutic antibodies but susceptibility towards inhibition by sotrovimab. Recent in vitro data demonstrated the promising use of sotrovimab, a MAb antibody produced by GSK, against the Omicron spike protein (Mahase, 2021b). Broadly neutralizing Sarbecovirus mAbs recognizes the site outside of the receptor-binding motif. In this class, three mAbs fall, namely sotrovimab, S2X259, and S2H97, identifying conserved epitopes and neutralizing Omicron (Cameroni et al., 2021). A panel of 44 mAbs when investigated for neutralizing Omicron belonging to cognate RBD binding sites (I, I, IV, and V) and few of the antibodies among them targeting the conserved epitopes were found to be broadly neutralizing; these will be beneficial in targeting Omicron being resilient against antigenic shift associated with virus evolution (Cameroni et al., 2021), and might help control the ongoing pandemic. A panel of neutralizing antibodies have been recovered using the linking B cell receptor to antigen specificity through sequencing (LIBRA-seq) technology that allows simultaneous report of B cell receptor and antigen reactivity at the single-cell level. Five neutralizing antibodies were screened precisely to SARS-CoV-2 only and not for any other coronavirus. The 54042-4 was the most potent and targeted RBD region among them. Shotgun alanine-scanning mutagenesis of the SARS-CoV-2 RBD showed that currently circulating VOCs' neutralization is not affected if 54042-4 antibody is used. 54042-4 uses a distinct S protein recognition mode and possesses a distinctive genetic signature, differentiating it from other SARS-CoV-2 neutralizing antibodies. Its ability to neutralize Alpha, Beta, Gamma, and Delta VOCs and conservancy of its epitope among currently circulating isolates make it a potential therapeutic and diagnostic target (Kramer et al., 2021).
17. Strategies to tackle emerging SARS-CoV-2 variants
The pandemic virus is rapidly evolving and poses a severe threat to human health. The emergence of the omicron variant serves as a harsh reminder that, while we've made headway against covid-19 in the last two years, there's still a lot more work to be done (Rae, 2021). There are requirements for prompt diagnosis, extensive surveillance, and monitoring of the emerging SARS-CoV-2 variants (Rahimi et al., 2021; Raman et al., 2021; Khan et al., 2022). There is an urgent demand to reduce the vaccine hesitancy and simultaneous development of even more efficacious vaccines (Blasi et al., 2021; Fiolet et al., 2021). Such an efficacious vaccine is required to reach to the entire world's population. The safety measures adopted during the initial waves of SARS-CoV-2, like the implementation of quarantine, wearing masks, and other advanced protective equipment, with good hygiene practices need to be followed up continuously (Dhama et al., 2021; Zhou et al., 2021). Attempts to upgrade medical facilities and efforts to make these upgraded facilities available and accessible to the virus infected patients, especially the ones residing in the most affected areas, need to be one of the top priorities in each Omicron-affected countries. Apart from developing therapeutics against the emerging variants, much of the research should be directed towards drug repurposing where drugs that are already developed, evaluated for safety and efficacy, and already being used for treatment for another ailment may be implemented in the treatment of SARS-CoV-2 (Dhama et al., 2020).
At present, a very low proportion of people residing in low-income countries had been vaccinated against COVID-19 (Anonymous, 2021; Tareq et al., 2021). The challenge in the drive of vaccination is the less likelihood of vaccination in ethnic minority groups and less vaccination in financially deprived groups (Rae, 2021). As vaccination has been proven quite effective in the management of COVID-19 and to prevent high burden of disease severity (Nainu et al., 2020; Liu et al., 2021), people residing in low-income and less-developed countries should be a top priority subject for mass vaccination (He et al., 2021). During the time of pandemic when many variants are appearing one after one with variable disease severity and transmissibility, clarity of messages is essential which have been changed time to time from “stay home” to “stay alert,” and many people may find it quite puzzling and it could be explained as “Alert Fatigue” (McKee, 2021). Moreover, there is a decline in the adherence to guidelines and trust in government when government officials in charge of making rules breach the rules and are called the Cummings effect when we see all the situations as per behavioral aspects (McKee, 2021). Also, despite complete vaccination, the spread of the Omicron variant is generating anxiety and fear in public, fuelled by misinformation on social media platforms. Medical staff is also stressed due to difficulty being faced in managing the interactions with anti-vaxers, and the situation worsens while handling aggressive psychiatric patients (Jain and Jolly, 2021). After the emergence of SARS-CoV-2, China has adjusted a series of policies to ensure effective implementation of prevention and control interventions and integrated the public health concept (Luo et al., 2021). The government is set to establish Nightingale hubs at the start of the first week of 2022 as a part of the preparedness program, and here the patients will be kept, those are not fit for discharge but require minimal nursing support and are not going to serve as a source of infection and does not require oxygen support (Mahase, 2021f).
A fully coordinated and targeted operation of mass vaccination support can be managed by high-income and more developed countries. Vaccines need to be donated to the people residing in low-income countries to promote vaccination equity and global access, since the longer the vaccine inequity persists, the more the virus will gain opportunity to perpetuate, mutate and evolve (Vaughan, 2021). Hence, in response to this, more than 100 countries and thousands of organizations came up together and are supporting a campaign, initiated and led by India and South Africa (Wouters et al., 2021) and backed up by the WHO, to temporarily waive intellectual-property (IP) rights to COVID-19 vaccines and drugs (Anonymous, 2021). Formulations of better strategies to design superior vaccine candidates with longer shelf life, higher stability, and ease of immunization like an oral or nasal vaccine are to be opted (Snehota et al., 2021). Presently when there is a high requirement of protecting the population from emerging SARS-CoVB-2 VOCs and VOIs, many mRNA based vaccines might be efficiently designed to meet the pace of emerging variants; however, there is a quest to develop a much more experimental one-shot universal vaccine that can protect individuals for the entire lifetime (Li, 2021).
Yaesoubi et al. (2021) suggested decision rules based on current hospital occupancy surveillance data and the weekly rate of new hospitalization. This might be helpful to policymakers to keep a close eye on current and changing situations and make decision rules (Yaesoubi et al., 2021). Among some safety measures, on arrival at the airport, thermal screening for infection is advocated, along with the social spacing. In addition, passengers from high-risk countries should be subjected to RT-PCR testing, and routine safety protocol should be followed. If these are found positive, the sample should be sent for genome sequencing (Thakur and Kanta Ratho, 2021).
Government organizations may tie-up with private organizations to enhance the number of testings and tracking of SARS-CoV-2 and its emerging variants (CDC, 2021b). Genome sequencing facilities need to be enhanced to monitor the real-time emergence of new variants so that the timely strategies can be designed to mitigate the forthcoming issues related to the pandemic. Much is yet to be known and explored about the most recently emerged Omicron SARS-CoV-2 variant, its threat assessment, and therefore, high vigilance, needful public health alerts, collaborative efforts, action plans and preparedness plans in advance while translating the entire knowledge gained on COVID-19 into prevention and control of emerging variants to be best feasible ways are the utmost need of the present time to tackle this VOC too that is seeming to pose high global health concerns amid the ongoing COVID-19 pandemic (Anonymous, 2021; Choudhary et al., 2021; Daria et al., 2021; Gao et al., 2021; Karim and Karim, 2021; Wang et al., 2021; Ingraham and Ingbar, 2021).
18. What can be done in the present scenario?
Presently Omicron VOC has knocked on the door of 150 countries as of January 22, 2022 with nearly 0.5 million confirmed cases and 115 deaths worldwide, and is spreading into the population of all the affected countries with its faster transmission rates (ECDC, 2021b; NewsNodes, 2022), therefore the number of cases are likely to increase quickly as a massive surge in COVID-19 cases at global level. Provided we have limited information related to the Omicron variant, a multi-layered approach is required to be adopted, mainly when immune escape and possible vaccine failure are posing a significant concern (ECDC, 2021e). Delta variant circulation among the countries forced authorities to make people vaccinated on top priority, especially those who are unvaccinated or not fully vaccinated. For example, in the USA, the significance of receiving vaccines is stressed even for children over five years and getting booster shots to people over 18 years of age (Tanne, 2021b). Some travel-related restrictions also may be implemented and extended until the epidemiological situation is fully understood. To slow the spread of Omicron, more than 50 countries have tightened border controls by 02 December 2021 (Mallapaty, 2021). Though, travel restrictions are imposed in response to a newly discovered coronavirus strain, according to researchers' speculations, we are too late and may even hinder Omicron research. Therefore, to prevent viral spread, the WHO advocated against travel bans and suggested quarantining new arrivals and testing travellers for SARS-CoV-2 before and after their trips (WHO 2021d). Moreover, in the meeting of Scientific Advisory Group for Emergencies (SAGE, 2021) in England on 16 December, they advised government of England to introduce more strict measures, like those in place after step 2 or step 1 of the government's roadmap, very soon to lower infection levels in the public and prevent the expected high levels of hospital admissions and deaths across the UK. The decisions by government should be based on scientific facts rather on political issues (Queen, 2022). Moreover, they stressed that delaying such initiatives until 2022 would considerably diminish their effectiveness and make it less probable that they will prevent significant pressure on health and care settings.
Lubin et al. (2021) provided a structural model based on binding of Omicron RBD to its corresponding ACE2 and neutralizing and therapeutic antibodies based on computational analysis. A multi-residue interaction network was formed between R493, S496, Y501, R498, and ACE2 residues. This interaction network suggested positive co-operation between residues to enhance the binding of Omicron RBD and ACE2, while binding of Barnes Class 1 and Class 2 neutralizing antibodies against Omicron RBD showed overall reductions in interfacial interactions. Furthermore, few of the substitutions in Omicron are known to dampen the antibody binding (e.g., K417N). An improved model named as extended WKDE model has been made that performs the retrospective analysis based on the spatiotemporal information to infer the date of infection for individual cases and predict the risk of disease onset in the future (Tong et al., 2021). Such more data-driven spatial prediction models need to be developed to reduce the dependence of theoretical assumptions and accurately predict the future disease onset, especially when we are combating Omicron having very high infection rates.
The Monte Carlo modelling revealed that now higher proportion of infected individuals is acting as super-emitters. For wild type virus, the ratio was 1 in 1000, while for Omicron it is 1 in 20 or 10 (Riediker et al., 2022). This data suggest that surgical masks alone are not able to protect fully, in fact well fitted FFP2 respirators are able to provide sufficient protection. Various non-pharmaceutical interventions have proven their efficacy in preventing the transmission related to delta variant VOC. Also, measures such as social distancing, maintaining adequate ventilation, and good hand and respiratory hygiene also play a significant role in lowering the SARS-CoV-2 associated morbidity and mortality. Wearing masks even with complete vaccination is urgent and necessary and need to be clubbed with the non-pharmaceutical interventions to curb the pandemic. Many mathematical models are suggesting that current vaccination rate is not sufficient to fully prevent the spread of virus (Brüssow and Zuber, 2021). It was reported that the Omicron variant (B.1.1.529) was found in an asymptomatic, fully vaccinated traveller in a quarantined hotel in Hong Kong, China, and had been transmitted to another fully vaccinated traveller staying in a room across the corridor from the index patient, indicating transmission of this virus variant despite strict quarantine precautions (Gu et al., 2021). Smoke tests in designated quarantine hotels revealed that aerosols could leak out may move to guest rooms and corridors and infectious aerosols may be inhaled when the doors of the rooms are opened (Wong et al., 2021). Classical Wells-Riley model is widely used model to estimate transmission risk of airborne pathogens in indoor spaces. spatiotemporal distribution of airborne pathogens is determined using computational fluid dynamics (CFD) simulations of airflow and aerosol transport and it revealed that a combination of proper ventilation along with PPE kit are necessary for preventing the transmission risk at hospital wards (X. Li et al., 2021). Experts suggest that the governments should implement strict restrictions based on modelling, which indicates that without posing additional restrictions, hospital admission could peak 3000 and 10000 a day, with a death toll between 600 and 6000 a day (Iacobucci, 2021b).
Early genomic detection, field investigation, and laboratory assessments will remain helpful in understanding the epidemiological trends, virus characteristics, disease severity, the effectiveness of public health and social interventions, diagnostic procedures, immunological responses, as well as vaccine effectiveness and taking adequate steps necessary to prevent further dissemination could be crucial in slowing down the Omicron VOC establishment (Wang and Powell, 2021).
19. Conclusions and future perspective
Despite the global massive vaccination drives and high efforts to restrain SARS-CoV-2 spread, COVID-19 pandemic continues as the virus evolves into several variants and mutants. SARS-CoV-2 pandemic has hit the world with its devastating global health impacts and severely affecting the economy worldwide. After almost two years of the initial emergence of the virus and its different variants, an exceptional accumulation of high numbers of mutations have given rise to the newly emerged most mutated SARS-CoV-2 Omicron variant. The emergence of Omicron variant could be attributed to either accumulation of mutations in a closed group of people and then its dissemination in a larger group of people or due to long term persistence in immune-compromised patients that led to the continuous evolution in virus resulting in a variant with higher mutations. Alternatively, the hypothesis of epizootic transfer of virus from human to animals and then again bouncing back to humans also need appropriate attention to be in-depth investigated to reach any conclusion. Whatever could be the reason behind the emergence of Omicron, it presently created havoc and imposed high public health concerns at global level. Until its complete etiology is understood regarding infectivity, neutralization through immune sera and effectiveness against currently available vaccines and immunotherapies, safety measures such as quarantine, social distancing, wearing of face masks, hand hygiene, respiratory hygiene, medical facility upliftment, development of highly efficacious vaccines and universal vaccine effective against all variants of SARS-CoV-2, and exploring drug repurposing should be given due priority to limit the speed of spread of this most recently emerged Omicron variant. The primary concerns related to the emergence of any virus include infectivity, the efficacy of therapeutics against the pathogen and the efficacy of pre-existing immunity obtained via natural infection or immunization via vaccines against the emerging virus, and possible health hazards associated with the emergence of immune escape. Hence strengthening of research, enhancing genomic surveillance and tracking, developing highly effective vaccines and immunotherapies, designing appropriate strategies, action plans and future preparedness plans need to be emphasized on priority and executed promptly at global levels to mitigate the high global health concerns associated with this new Omicron variant emergence well before it could make high surges in COVID-19 cases worldwide.
Authors contributions
All the authors contributed significantly to this manuscript. RK, SS, TA, MAK, NAE, FN, PAD and KD conceptualized the manuscript. RKM wrote the first draft with input from SS, TA, MAK, NAE, FN, PAD. All Authors updated the manuscript. KD and RK updated, reviewed and edited the manuscript. All authors contributed to revisions and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments:
The authors are grateful to all the respective Universities and Institutes.
References
- Ahmed W., Bivins A., Smith W.J.M., Metcalfe S., Stephens M., Jennison A.V., Moore F.A.J., Bourke J., Schlebusch S., McMahon J., Hewitson G., Nguyen S., Barcelon J., Jackson G., Mueller J.F., Ehret J., Hosegood I., Tian W., Wang H., Yang L., Bertsch P., Tynan J., Thomas K.V., Bibby K., Graber T.E., Ziels R., Simpson S.L. Detection of the Omicron (B.1.1.529) variant of SARS-CoV-2 in aircraft wastewater. Sci. Total Environ. 2022;153171 doi: 10.1016/J.SCITOTENV.2022.153171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ai J., Zhang H., Zhang Yi, Lin K., Zhang Yanliang, Wu J., Wan Y., Huang Y., Song J., Fu Z., Wang H., Guo J., Jiang N., Fan M., Zhou Y., Zhao Y., Zhang Q., Liu Q., Lv J., Li P., Qiu C., Zhang W. Omicron variant showed lower neutralizing sensitivity than other SARS-CoV-2 variants to immune sera elicited by vaccines after boost. Emerg. Microb. Infect. 2021:1–24. doi: 10.1080/22221751.2021.2022440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleem A., Akbar Samad A.S., Slenker A.K. 2022. Emerging Variants of SARS-CoV-2 and Novel Therapeutics against Coronavirus (COVID-19) - PubMed.https://www.ncbi.nlm.nih.gov/books/NBK570580/ [PubMed] [Google Scholar]
- Ali F., Kasry A., Amin M. The new SARS-CoV-2 strain shows a stronger binding affinity to ACE2 due to N501Y mutant. Med. Drug Discov. 2021;10 doi: 10.1016/J.MEDIDD.2021.100086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreano E., Paciello I., Piccini G., Manganaro N., Pileri P., Hyseni I., Leonardi M., Pantano E., Abbiento V., Benincasa L., Giglioli G., De Santi C., Fabbiani M., Rancan I., Tumbarello M., Montagnani F., Sala C., Montomoli E., Rappuoli R. Hybrid immunity improves B cells and antibodies against SARS-CoV-2 variants. Nature. 2021 doi: 10.1038/S41586-021-04117-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreano E., Piccini G., Licastro D., Casalino L., Johnson N.V., Paciello I., Monego S.D., Pantano E., Manganaro N., Manenti A., Manna R., Casa E., Hyseni I., Benincasa L., Montomoli E., Amaro R.E., McLellan J.S., Rappuoli R. SARS-CoV-2 escape from a highly neutralizing COVID-19 convalescent plasma. Proc. Natl. Acad. Sci. U. S. A. 2021;118 doi: 10.1073/PNAS.2103154118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous Omicron is bad but the global response is worse, 2021. Nature. 2021;600:190. doi: 10.1038/D41586-021-03616-X. [DOI] [PubMed] [Google Scholar]
- Bae E.Y., Sanders J.M., Johns M.L., Lin K., Ortwine J.K., Wei W., Mang N.S., Cutrell J.B. Therapeutic options for coronavirus disease 2019 (COVID-19): where are we now? Curr. Infect. Dis. Rep. 2021;2312 23(2021):1–15. doi: 10.1007/S11908-021-00769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee A., Mossman K., Baker M.L. Zooanthroponotic potential of SARS-CoV-2 and implications of reintroduction into human populations. Cell Host Microbe. 2021;29:160. doi: 10.1016/J.CHOM.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banoun H. Evolution of SARS-CoV-2: review of mutations, role of the host immune system. Nephron Clin. Pract. 2021;145:392. doi: 10.1159/000515417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barda N., Dagan N., Cohen C., Hernán M.A., Lipsitch M., Kohane I.S., Reis B.Y., Balicer R.D. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–2100. doi: 10.1016/S0140-6736(21)02249-2/ATTACHMENT/588607F0-89F7-4E80-8E48-FB7CE8C7F7EC/MMC1.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartsch Y., Tong X., Kang J., Avendaño M.J., Serrano E.F., García-Salum T., Pardo-Roa C., Riquelme A., Medina R.A., Alter G. Preserved Omicron Spike specific antibody binding and Fc-recognition across COVID-19 vaccine platforms. medRxiv Prepr. Serv. Health Sci. 2021 doi: 10.1101/2021.12.24.21268378. [DOI] [Google Scholar]
- Blasi F., Gramegna A., Sotgiu G., Saderi L., Voza A., Aliberti S., Amati F. SARS-CoV-2 vaccines: a critical perspective through efficacy data and barriers to herd immunity. Respir. Med. 2021;180:106355. doi: 10.1016/J.RMED.2021.106355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm E., Kronig I., Neher R.A., Eckerle I., Vetter P., Kaiser L. Novel SARS-CoV-2 variants: the pandemics within the pandemic. Clin. Microbiol. Infect. 2021;27:1109. doi: 10.1016/J.CMI.2021.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Aldana D.K., Rodriguez-Morales A.J. The threat of the spread of SARS-CoV-2 variants in animals. Vet. Q. 2021;41:321. doi: 10.1080/01652176.2021.2008046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandal L.T., MacDonald E., Veneti L., Ravlo T., Lange H., Naseer U., Feruglio S., Bragstad K., Hungnes O., Ødeskaug L.E., Hagen F., Hanch-Hansen K.E., Lind A., Watle S.V., Taxt A.M., Johansen M., Vold L., Aavitsland P., Nygård K., Madslien E.H. Outbreak caused by the SARS-CoV-2 omicron variant in Norway, november to december 2021. Euro Surveill. 2021;26 doi: 10.2807/1560-7917.ES.2021.26.50.2101147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brüssow H., Zuber S. Can a combination of vaccination and face mask wearing contain the COVID-19 pandemic? Microb. Biotechnol. 2021 doi: 10.1111/1751-7915.13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burki T.K. Omicron variant and booster COVID-19 vaccines. Lancet Respir. Med. 2021 doi: 10.1016/S2213-2600(21)00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway E. Omicron likely to weaken COVID vaccine protection. Nature. 2021 doi: 10.1038/D41586-021-03672-3. [DOI] [PubMed] [Google Scholar]
- Callaway E. Heavily mutated Omicron variant puts scientists on alert. Nature. 2021;600 doi: 10.1038/D41586-021-03552-W. [DOI] [PubMed] [Google Scholar]
- Callaway E. Beyond Omicron: what's next for COVID's viral evolution. Nature. 2021;600:204–207. doi: 10.1038/D41586-021-03619-8. [DOI] [PubMed] [Google Scholar]
- Callaway E., Ledford H. How bad is Omicron? What scientists know so far. Nature. 2021;600:197–199. doi: 10.1038/D41586-021-03614-Z. [DOI] [PubMed] [Google Scholar]
- Cameroni E., Bowen J.E., Rosen L.E., Saliba C., Zepeda S.K., Culap K., Pinto D., VanBlargan L.A., De Marco A., di Iulio J., Zatta F., Kaiser H., Noack J., Farhat N., Czudnochowski N., Havenar-Daughton C., Sprouse K.R., Dillen J.R., Powell A.E., Chen A., Maher C., Yin L., Sun D., Soriaga L., Bassi J., Silacci-Fregni C., Gustafsson C., Franko N.M., Logue J., Iqbal N.T., Mazzitelli I., Geffner J., Grifantini R., Chu H., Gori A., Riva A., Giannini O., Ceschi A., Ferrari P., Cippà P.E., Franzetti-Pellanda A., Garzoni C., Halfmann P.J., Kawaoka Y., Hebner C., Purcell L.A., Piccoli L., Pizzuto M.S., Walls A.C., Diamond M.S., Telenti A., Virgin H.W., Lanzavecchia A., Snell G., Veesler D., Corti D. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature. 2021 doi: 10.1038/D41586-021-03825-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cele S., Jackson L., Khan K., Khoury D., Moyo-Gwete T., Tegally H., Scheepers C., Amoako D., Karim F., Bernstein M., Lustig G., Archary D., Smith M., Ganga Y., Jule Z., Reedoy K., San J.E., Hwa S.-H., Giandhari J., Blackburn J.M., Gosnell B.I., Karim S.A., Hanekom W., NGS S.A., Team C.-K., Gottberg A. von, Bhiman J., Lessells R.J., Moosa M.-Y.S., Davenport M., Oliveira T. de, Moore P.L., Sigal A. medRxiv; 2021. SARS-CoV-2 Omicron Has Extensive but Incomplete Escape of Pfizer BNT162b2 Elicited Neutralization and Requires ACE2 for Infection. 2021.12.08.21267417. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2021. Science Brief: Omicron (B.1.1.529) Variant.https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/scientific-brief-omicron-variant.html [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2021. Science Brief: Emerging SARS-CoV-2 Variants.https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/scientific-brief-emerging-variants.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F201,%209-ncov%2Fmore%2Fscience-and-research%2Fscientific-brief-emerging-variants.html [PubMed] [Google Scholar]
- Chavda V.P., Feehan J., Apostolopoulos V. vol. 9. Vaccines; 2021. A Veterinary Vaccine for SARS-CoV-2: the First COVID-19 Vaccine for Animals. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Wang R., Gilby N.B., Wei G.W. 2021. Omicron (B.1.1.529): Infectivity, Vaccine Breakthrough, and Antibody Resistance.https://arxiv.org/abs/2112.01318 ArXiv [Preprint]. arXiv: 2112.01318v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R.E., Zhang X., Case J.B., Winkler E.S., Liu Y., VanBlargan L.A., Liu J., Errico J.M., Xie X., Suryadevara N., Gilchuk P., Zost S.J., Tahan S., Droit L., Turner J.S., Kim W., Schmitz A.J., Thapa M., Wang D., Boon A.C.M., Presti R.M., O'Halloran J.A., Kim A.H.J., Deepak P., Pinto D., Fremont D.H., Crowe J.E., Corti D., Virgin H.W., Ellebedy A.H., Shi P.Y., Diamond M.S. Resistance of SARS-CoV-2 variants to neutralization by monoclonal and serum-derived polyclonal antibodies. Nat. Med. 2021;27:717–726. doi: 10.1038/S41591-021-01294-W. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Zhang P., Matsuoka Y., Tsybovsky Y., West K., Santos C., Boyd L.F., Nguyen H., Pomerenke A., Stephens T., Olia A.S., De Giorgi V., Holbrook M.R., Gross R., Postnikova E., Garza N.L., Johnson R.F., Margulies D.H., Kwong P.D., Alter H.J., Buchholz U.J., Lusso P., Farci P. Extremely potent monoclonal antibodies neutralize Omicron and other SARS-CoV-2 variants. medRxiv Prepr. Serv. Health Sci. 2022 doi: 10.1101/2022.01.12.22269023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi-wai C.M. 2021. HKUMed Finds Omicron SARS-CoV-2 Can Infect Faster and Better than Delta in Human Bronchus but with Less Severe Infection in Lung.https://www.med.hku.hk/en/news/press/20211215-omicron-sars-cov-2-infection [Google Scholar]
- Choi S.J., Kim D.-U., Noh J.Y., Kim S., Park S.-H., Jeong H.W., Shin E.-C. T cell epitopes in SARS-CoV-2 proteins are substantially conserved in the Omicron variant. Cell. Mol. Immunol. 2022 doi: 10.1038/S41423-022-00838-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhary O.P., Dhawan M., None P. Omicron variant (B.1.1.529) of SARS-CoV-2: threat assessment and plan of action. Int. J. Surg. 2021;97:106187. doi: 10.1016/J.IJSU.2021.106187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie B. Covid-19: early studies give hope omicron is milder than other variants. BMJ. 2021;375:n3144. doi: 10.1136/BMJ.N3144. [DOI] [PubMed] [Google Scholar]
- Corum J., Zimmer C. 2021. Tracking Omicron and Other Coronavirus Variants - the New York Times.https://www.nytimes.com/interactive/2021/health/coronavirus-variant-tracker.html [Google Scholar]
- Couzin-Frankel J. Antiviral pills could change pandemic's course. Science. 2021;374:799–800. doi: 10.1126/SCIENCE.ACX9605. [DOI] [PubMed] [Google Scholar]
- Daria S., Bhuiyan M.A., Islam M.R. Detection of highly muted coronavirus variant Omicron (B.1.1.529) is triggering the alarm for South Asian countries: associated risk factors and preventive actions. J. Med. Virol. 2021 doi: 10.1002/JMV.27503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deerain J., Druce J., Tran T., Batty M., Yoga Y., Fennell M., Dwyer D.E., Kok J., Williamson D.A. Assessment of the analytical sensitivity of ten lateral flow devices against the SARS-CoV-2 omicron variant. J. Clin. Microbiol. 2021 doi: 10.1128/JCM.02479-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejnirattisai W., Shaw R.H., Supasa P., Liu C., Stuart A.S., Pollard A.J., Liu X., Lambe T., Crook D., Stuart D.I., Mongkolsapaya J., Nguyen-Van-Tam J.S., Snape M.D., Screaton G.R. Reduced neutralisation of SARS-CoV-2 omicron B.1.1.529 variant by post-immunisation serum. Lancet. 2021 doi: 10.1016/S0140-6736(21)02844-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desingu P.A., Nagarajan K., Dhama K. Emergence of Omicron third lineage BA.3 and its importance. J. Med. Virol. 2022 doi: 10.1002/JMV.27601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhama K., Khan S., Tiwari R., Sircar S., Bhat S., Malik Y.S., Singh K.P., Chaicumpa W., Bonilla-Aldana D.K., Rodriguez-Morales A.J. Coronavirus disease 2019-COVID-19. Clin. Microbiol. Rev. 2020;33:1–48. doi: 10.1128/CMR.00028-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhama K., Patel S.K., Yatoo M.I., Tiwari R., Sharun K., Dhama J., Natesan S., Malik Y.S., Singh K.P., Harapan H. SARS-CoV-2 existence in sewage and wastewater: a global public health concern? J. Environ. Manag. 2021;280:111825. doi: 10.1016/J.JENVMAN.2020.111825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond M., Halfmann P., Maemura T., Iwatsuki-Horimoto K., Iida S., Kiso M., Scheaffer S., Darling T., Joshi A., Loeber S., Foster S., Ying B., Whitener B., Floyd K., Ujie M., Nakajima N., Ito M., Wright R., Uraki R., Li R., Sakai Y., Liu Y., Larson D., Osorio J., Hernandez-Ortiz J., ÄŒiuoderis K., Florek K., Patel M., Bateman A., Odle A., Wong L.-Y., Wang Z., Edara V.V., Chong Z., Thackray L., Ueki H., Yamayoshi S., Imai M., Perlman S., Webby R., Seder R., Suthar M., Garcia-Sastre A., Schotsaert M., Suzuki T., Boon A., Kawaoka Y., Douek D., Moliva J., Sullivan N., Gagne M., Ransier A., Case J., Jeevan T., Franks J., Fabrizio T., DeBeauchamp J., Kercher L., Seiler P., Singh G., Warang P., Gonzalez-Reiche A.S., Sordillo E., van Bakel H., Simon V. The SARS-CoV-2 B.1.1.529 Omicron virus causes attenuated infection and disease in mice and hamsters. Res. Sq. 2021 doi: 10.21203/RS.3.RS-1211792/V1. [DOI] [Google Scholar]
- Domingo E., Perales C. Quasispecies and virus. Eur. Biophys. J. 2018;47:443–457. doi: 10.1007/S00249-018-1282-6. [DOI] [PubMed] [Google Scholar]
- Doria-Rose N.A., Shen X., Schmidt S.D., O'Dell S., McDanal C., Feng W., Tong J., Eaton A., Maglinao M., Tang H., Atmar R.L., Lyke K.E., Wang L., Zhang Y., Gaudinski M.R., Black W.P., Gordon I., Guech M., Ledgerwood J.E., Misasi J.N., Widge A., Roberts P.C., Beigel J., Korber B., Pajon R., Mascola J.R., Montefiori D.C. Booster of mRNA-1273 vaccine reduces SARS-CoV-2 omicron escape from neutralizing antibodies. medRxiv. 2021;12(2021) doi: 10.1101/2021.12.15.21267805. 15.21267805. [DOI] [Google Scholar]
- Du P., Gao G.F., Wang Q. 2022. The Mysterious Origins of the Omicron Variant of SARS-CoV-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer O. Covid-19: omicron is causing more infections but fewer hospital admissions than delta, South African data show. BMJ. 2021;375:n3104. doi: 10.1136/BMJ.N3104. [DOI] [PubMed] [Google Scholar]
- Espenhain L., Funk T., Overvad M., Edslev S.M., Fonager J., Ingham A.C., Rasmussen M., Madsen S.L., Espersen C.H., Sieber R.N., Stegger M., Gunalan V., Wilkowski B., Larsen N.B., Legarth R., Cohen A.S., Nielsen F., Lam J.U.H., Lavik K.E., Karakis M., Spiess K., Marving E., Nielsen C., Wiid Svarrer C., Bybjerg-Grauholm J., Olsen S.S., Jensen A., Krause T.G., Müller L. Epidemiological characterisation of the first 785 SARS-CoV-2 Omicron variant cases in Denmark. Euro Surveill. 2021;26 doi: 10.2807/1560-7917.ES.2021.26.50.2101146. December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC) 2021. Threat Assessment Brief: Implications of the Emergence and Spread of the SARS-CoV-2 B.1.1. 529 Variant of Concern (Omicron) for the EU/EEA.https://www.ecdc.europa.eu/en/publications-data/threat-assessment-brief-emergence-sars-cov-2-variant-b.1.1.529 [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC) 2021. Weekly Epidemiological Update: Omicron Variant of Concern (VOC) – Week 50.https://www.ecdc.europa.eu/en/news-events/weekly-epidemiological-update-omicron-variant-concern-voc-week-50-data-19-december-2021 (data as of 19 December 2021) [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC) Methods for the detection and characterisation of SARS-CoV-2 variants - first update. 2021. https://www.ecdc.europa.eu/en/publications-data/methods-detection-and-characterisation-sars-cov-2-variants-first-update
- European Centre for Disease Prevention and Control (ECDC) ECDC; Stockholm: 2021. Implications of the Spread of the SARS-CoV-2 B.1.1.529 Variant of Concern (Omicron) for the EU/EEA – First Update. 2 December 2021.https://www.ecdc.europa.eu/en/publications-data/covid-19-threat-assessment-spread-omicron-first-update 2021. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC) 2021. Threat Assessment Brief: Implications of the Further Emergence and Spread of the SARS CoV 2 B.1.1.529 Variant of Concern (Omicron) for the EU/EEA First Update.https://www.ecdc.europa.eu/en/publications-data/covid-19-threat-assessment-spread-omicron-first-update [Google Scholar]
- Falcone M., Tiseo G., Valoriani B., Barbieri C., Occhineri S., Mazzetti P., Vatteroni M.L., Suardi L.R., Riccardi N., Pistello M., Tacconi D., Menichetti F. Efficacy of bamlanivimab/etesevimab and casirivimab/imdevimab in preventing progression to severe COVID-19 and role of variants of concern. Infect. Dis. Ther. 2021;10:2479. doi: 10.1007/S40121-021-00525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan H., Lou F., Fan J., Li M., Tong Y. The emergence of powerful oral anti-COVID-19 drugs in the post-vaccine era. Lancet. Microb. 2021 doi: 10.1016/S2666-5247(21)00278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang F. “Flora”, Shi P.-Y. Omicron: a drug developer's perspective. Emerg. Microb. Infect. 2021:1–10. doi: 10.1080/22221751.2021.2023330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fantini J., Yahi N., Colson P., Chahinian H., Bernard |, Scola L., Raoult | Didier. The puzzling mutational landscape of the SARS-2-variant Omicron. J. Med. Virol. 2022 doi: 10.1002/JMV.27577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraz Ahmed S., Abdul Quadeer A., McKay M.R. SARS-CoV-2 T cell responses elicited by COVID-19 vaccines or infection are expected to remain robust against omicron. Viruses. 2022;14(2022):79. doi: 10.3390/V14010079. Page 79 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faustini S., Shields A., Banham G., Wall N., Al-Taei S., Tanner C., Ahmed Z., Efstathiou E., Townsend N., Goodall M., Plant T., Perez-Toledo M., Jasiulewicz A., Price R., McLaughlin J., Farnan J., Moore J., Robertson L., Nesbit A., Curry G., Black A., Cunningham A., Harper L., Moore T., Drayson M., Richter A. Cross reactivity of spike glycoprotein induced antibody against Delta and Omicron variants before and after third SARS-CoV-2 vaccine dose in healthy and immunocompromised individuals. J. Infect. 2022 doi: 10.1016/J.JINF.2022.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferré V.M., Peiffer-Smadja N., Visseaux B., Descamps D., Ghosn J., Charpentier C. Omicron SARS-CoV-2 variant: what we know and what we don't. Anaesthesia, Crit. Care Pain Med. 2022;41:100998. doi: 10.1016/J.ACCPM.2021.100998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiolet T., Kherabi Y., MacDonald C.-J., Ghosn J., Peiffer-Smadja N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review. Clin. Microbiol. Infect. 2021 doi: 10.1016/J.CMI.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu J.Y.L., Chong Y.M., Sam I.-C., Chan Y.F. SARS-CoV-2 multiplex RT-PCR to detect variants of concern (VOCs) in Malaysia, between January to May 2021. J. Virol. Methods. 2022;301:114462. doi: 10.1016/J.JVIROMET.2022.114462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furio V., Garijo R., Duran M., Moya A., Bell J.C., Sanjuan R. Relationship between within-host fitness and virulence in the vesicular stomatitis virus: correlation with partial decoupling. J. Virol. 2012;86:12228–12236. doi: 10.1128/JVI.00755-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao S., Guo H., Luo G. Omicron variant (B.1.1.529) of SARS-CoV-2, a global urgent public health alert. J. Med. Virol. 2021 doi: 10.1002/JMV.27491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y., Cai C., Grifoni A., Müller T.R., Niessl J., Olofsson A., Humbert M., Hansson L., Österborg A., Bergman P., Chen P., Olsson A., Sandberg J.K., Weiskopf D., Price D.A., Ljunggren H.-G., Karlsson A.C., Sette A., Aleman S., Buggert M. Ancestral SARS-CoV-2-specific T cells cross-recognize the Omicron variant. Nat. Med. 2022 doi: 10.1038/S41591-022-01700-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Beltran W.F., Denis K.J. St, Hoelzemer A., Lam E.C., Nitido A.D., Sheehan M.L., Berrios C., Ofoman O., Chang C.C., Hauser B.M., Feldman J., Gregory D.J., Poznansky M.C., Schmidt A.G., Iafrate A.J., Naranbhai V., Balazs A.B. 2021. mRNA-Based COVID-19 Vaccine Boosters Induce Neutralizing Immunity against SARS-CoV-2 Omicron Variant. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett N., Tapley A., Andriesen J., Seocharan I., Fisher L.H., Bunts L., Espy N., Wallis C.L., Randhawa A.K., Ketter N., Yacovone M., Goga A., Bekker L.-G., Gray G.E., Corey L. High rate of asymptomatic carriage associated with variant strain omicron. medRxiv Prepr. Serv. Health Sci. 2022 doi: 10.1101/2021.12.20.21268130. [DOI] [Google Scholar]
- Gelanew T., Mulu A., Abebe M., Bates T.A., Wassie L., Tefer M., Fentahun D., Alemu A., Tamiru F., Assefa G., Bayih A.G., Taffesse F.G., Mihret A., Abdissa A. A single dose ChAdOx1 nCoV-19 vaccine elicits high antibody responses in individuals with prior SARS-CoV-2 infection comparable to that of double dose vaccinated SARS-CoV-2 infection naïve individuals. Res. Sq. 2022 doi: 10.21203/RS.3.RS-1250175/V1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong S.Y., Chatterjee D., Richard J., Prévost J., Tauzin A., Gasser R., Bo Y., Vézina D., Goyette G., Gendron-Lepage G., Medjahed H., Roger M., Côté M., Finzi A. Contribution of single mutations to selected SARS-CoV-2 emerging variants spike antigenicity. Virology. 2021;563:134. doi: 10.1016/J.VIROL.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham F. Daily briefing: Pfizer's COVID pill looks promising. Nature. 2021 doi: 10.1038/D41586-021-03379-5. [DOI] [PubMed] [Google Scholar]
- Greaney A.J., Starr T.N., Bloom J.D. An antibody-escape calculator for mutations to the SARS-CoV-2 receptor-binding domain. 2021. bioRxiv. [DOI] [PMC free article] [PubMed]
- Gu H., Krishnan P., Ng D.Y.M., Chang L.D.J., Liu G.Y.Z., Cheng S.S.M., Hui M.M.Y., Fan M.C.Y., Wan J.H.L., Lau L.H.K., Cowling B.J., Peiris M., Poon L.L.M. Probable transmission of SARS-CoV-2 omicron variant in quarantine hotel, Hong Kong, China, november 2021. Emerg. Infect. Dis. 2021;28 doi: 10.3201/EID2802.212422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey W.T., Carabelli A.M., Jackson B., Gupta R.K., Thomson E.C., Harrison E.M., Ludden C., Reeve R., Rambaut A., Peacock S.J., Robertson D.L. SARS-CoV-2 variants, spike mutations and immune escape. Nat. Rev. Microbiol. 2021;19:1. doi: 10.1038/S41579-021-00573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X., Hong W., Pan X., Lu G., Wei X. SARS-CoV-2 Omicron variant: characteristics and prevention. MedComm. 2021;2:838–845. doi: 10.1002/MCO2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrewegh A.A.P.M., Smeenk I., Horzinek M.C., Rottier P.J.M., de Groot R.J. Feline coronavirus type II strains 79-1683 and 79-1146 originate from a double recombination between feline coronavirus type I and canine coronavirus. J. Virol. 1998;72:4508–4514. doi: 10.1128/JVI.72.5.4508-4514.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Krüger N., Schulz S., Cossmann A., Rocha C., Kempf A., Nehlmeier I., Graichen L., Moldenhauer A.-S., Winkler M.S., Lier M., Dopfer-Jablonka A., Jäck H.-M., Behrens G.M.N., Pöhlmann S. The Omicron variant is highly resistant against antibody-mediated neutralization: implications for control of the COVID-19 pandemic. Cell. 2021 doi: 10.1016/J.CELL.2021.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.C. Comparative studies of RNA virus evolution. Orig. Evol. Virus. 2008:119–134. doi: 10.1016/B978-0-12-374153-0.00005-9. [DOI] [Google Scholar]
- Holmes E.C., Goldstein S.A., Rasmussen A.L., Robertson D.L., Crits-Christoph A., Wertheim J.O., Anthony S.J., Barclay W.S., Boni M.F., Doherty P.C., Farrar J., Geoghegan J.L., Jiang X., Leibowitz J.L., Neil S.J.D., Skern T., Weiss S.R., Worobey M., Andersen K.G., Garry R.F., Rambaut A. The origins of SARS-CoV-2: a critical review. Cell. 2021;184:4848–4856. doi: 10.1016/J.CELL.2021.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu J., Peng P., Cao X., Wu K., Chen J., Wang K., Tang N., Huang A.-L., Cao X. Increased immune escape of the new SARS-CoV-2 variant of concern Omicron. Cell. Mol. Immunol. 2022:1–3. doi: 10.1038/s41423-021-00836-z. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobucci G. Covid-19: government ignores scientists' advice to tighten restrictions to combat omicron. BMJ. 2021;375:n3131. doi: 10.1136/BMJ.N3131. [DOI] [PubMed] [Google Scholar]
- Iacobucci G. Covid-19: runny nose, headache, and fatigue are commonest symptoms of omicron, early data show. BMJ. 2021;375:n3103. doi: 10.1136/BMJ.N3103. [DOI] [PubMed] [Google Scholar]
- Ingraham N.E., Ingbar D.H. The omicron variant of SARS-CoV-2: understanding the known and living with unknowns. Clin. Transl. Med. 2021;11:e685. doi: 10.1002/CTM2.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito K., Piantham C., Nishiura H. Relative instantaneous reproduction number of omicron SARS-CoV-2 variant with respect to the delta variant in Denmark. J. Med. Virol. 2021 doi: 10.1002/JMV.27560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain A., Jolly T.S. Omicron (B.1.1.529) COVID-19 variant: a mental health perspective on lessons learned and future challenges. Prim. Care Compan. CNS Dis. 2021;23:38797. doi: 10.4088/PCC.21COM03206. [DOI] [PubMed] [Google Scholar]
- Jansen L., Tegomoh B., Lange K., Showalter K., Figliomeni J., Abdalhamid B., Iwen P.C., Fauver J., Buss B., Donahue M. Investigation of a SARS-CoV-2 B.1.1.529 (omicron) variant cluster - Nebraska, november-december 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:1782–1784. doi: 10.15585/MMWR.MM705152E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandeel M., Mohamed M.E.M., Abd El‐Lateef H.M., Venugopala K.N., El‐Beltagi H.S. Omicron variant genome evolution and phylogenetics. J. Med. Virol. 2021 doi: 10.1002/JMV.27515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannan S.R., Spratt A.N., Sharma K., Chand H.S., Byrareddy S.N., Singh K. Omicron SARS-CoV-2 variant: unique features and their impact on pre-existing antibodies. J. Autoimmun. 2022;126:102779. doi: 10.1016/J.JAUT.2021.102779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karikalan M., Chander V., Mahajan S., Deol P., Agrawal R.K., Nandi S., Rai S.K., Mathur A., Pawde A., Singh K.P., Sharma G.K. Natural infection of Delta mutant of SARS-CoV-2 in Asiatic lions of India. Transbound. Emerg. Dis. 2021 doi: 10.1111/TBED.14290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim S.S.A., Karim Q.A. vol. 398. Lancet; London, England: 2021. (Omicron SARS-CoV-2 Variant: a New Chapter in the COVID-19 Pandemic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim F., Moosa M., Gosnell B., Cele S., Giandhari J., Pillay S., Tegally H., Wilkinson E., San J., Msomi N., Mlisana K., Khan K., Bernstein M., Manickchund N., Singh L., Ramphal U., Team C.-K., Hanekom W., Lessells R., Sigal A., Oliveira T. de. medRxiv; 2021. Persistent SARS-CoV-2 Infection and Intra-host Evolution in Association with Advanced HIV Infection. 2021.06.03.21258228. [DOI] [Google Scholar]
- Kazybay B., Ahmad A., Mu C., Mengdesh D., Xie Y. Omicron N501Y mutation among SARS-CoV-2 lineages: in-silico analysis of potent binding to tyrosine kinase and hypothetical repurposed medicine. Trav. Med. Infect. Dis. 2021;102242 doi: 10.1016/J.TMAID.2021.102242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan N.A., Al-Thani H., El-Menyar A. The emergence of new SARS-CoV-2 variant (Omicron) and increasing calls for COVID-19 vaccine boosters-The debate continues. Trav. Med. Infect. Dis. 2022;45:102246. doi: 10.1016/J.TMAID.2021.102246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kibler K.V., Szczerba M., Lake D., Roeder A.J., Rahman M., Hogue B.G., Wong L.-Y.R., Perlman S., Li Y., Jacobs B.L. 2021. Intranasal Immunization with a Vaccinia Virus Vaccine Vector Expressing Pre-fusion Stabilized SARS-CoV-2 Spike Fully Protected Mice against Lethal Challenge with the Heavily Mutated Mouse-Adapted SARS2-N501YMA30 Strain of SARS-CoV-2. bioRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korath A.D.J., Janda J., Untersmayr E., Sokolowska M., Feleszko W., Agache I., Adel Seida A., Hartmann K., Jensen-Jarolim E., Pali-Schöll I. 2021. One Health: EAACI Position Paper on Coronaviruses at the Human-Animal Interface, with a Specific Focus on Comparative and Zoonotic Aspects of SARS-Cov-2. Allergy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlov M. Omicron overpowers key COVID antibody treatments in early tests. Nature. 2021 doi: 10.1038/D41586-021-03829-0. [DOI] [PubMed] [Google Scholar]
- Kozlov M. Omicron's feeble attack on the lungs could make it less dangerous. Nature. 2022;601 doi: 10.1038/D41586-022-00007-8. 177–177. [DOI] [PubMed] [Google Scholar]
- Kramer K.J., Johnson N.V., Shiakolas A.R., Suryadevara N., Periasamy S., Raju N., Williams J.K., Wrapp D., Zost S.J., Walker L.M., Wall S.C., Holt C.M., Hsieh C.L., Sutton R.E., Paulo A., Nargi R.S., Davidson E., Doranz B.J., Crowe J.E., Bukreyev A., Carnahan R.H., McLellan J.S., Georgiev I.S. Potent neutralization of SARS-CoV-2 variants of concern by an antibody with an uncommon genetic signature and structural mode of spike recognition. Cell Rep. 2021;37 doi: 10.1016/J.CELREP.2021.109784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Thambiraja T.S., Karuppanan K., Subramaniam G. 2021. Omicron and Delta Variant of SARS-CoV-2: A Comparative Computational Study of Spike Protein. bioRxiv 2021.12.02.470946. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K. 2021. ‘Patience Is Crucial’: Why We Won't Know for Weeks How Dangerous Omicron Is.https://www.science.org/content/article/patience-crucial-why-we-won-t-know-weeks-how-dangerous-omicron [Google Scholar]
- Kupferschmidt K. Scientists see a ‘really, really tough winter’ with Omicron. Science. 2021;17(374(6574)):1421–1422. doi: 10.1126/science.acz9834. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K. Where did “weird” Omicron come from? Science. 2021;374:1179. doi: 10.1126/SCIENCE.ACX9738. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K., Vogel G. How bad is Omicron? Some clues are emerging. Science (80- 2021;374:1304–1305. doi: 10.1126/SCIENCE.ACX9782. [DOI] [PubMed] [Google Scholar]
- Kutscher E. Preparing for Omicron as a covid veteran. BMJ. 2021;375:n3021. doi: 10.1136/BMJ.N3021. [DOI] [PubMed] [Google Scholar]
- Lapid N. Reuters; 2021. Omicron Variant May Have Picked up a Piece of Common-Cold Virus.https://www.reuters.com/business/healthcare-pharmaceuticals/omicron-variant-may-have-picked-up-piece-common-cold-virus-2021-12-03/ [Google Scholar]
- Laurie M.T., Liu J., Sunshine S., Peng J., Black D., Mann S.A., Pilarowski G., Zorn K.C., Rubio L., Bravo S., Marquez C., Sabatino J.J., Jr., Mittl K., Petersen M., Havlir D., Francisco Graduate Program in S., DeRisi J. medRxiv; 2021. SARS-CoV-2 Variant Exposures Elicit Antibody Responses with Differential Cross-Neutralization of Established and Emerging Strains Including Delta and Omicron. 2021.09.08.21263095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Page M. Stopping coronavirus variants. New Sci. 2021;252:8. doi: 10.1016/S0262-4079(21)02230-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leary S., Gaudieri S., Parker M.D., Chopra A., James I., Pakala S., Alves E., John M., Lindsey B.B., Keeley A.J., Rowland-Jones S.L., Swanson M.S., Ostrov D.A., Bubenik J.L., Das S.R., Sidney J., Sette A., de Silva T.I., Phillips E., Mallal S. Generation of a novel SARS-CoV-2 sub-genomic RNA due to the R203K/G204R variant in nucleocapsid: homologous recombination has potential to change SARS-CoV-2 at both protein and RNA level. Pathog. Immun. 2021;6:27. doi: 10.20411/PAI.V6I2.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford H. How severe are Omicron infections? Nature. 2021;600:577–578. doi: 10.1038/D41586-021-03794-8. [DOI] [PubMed] [Google Scholar]
- Ledford H. “Killer” immune cells still recognize Omicron variant. Nature. 2022;601 doi: 10.1038/D41586-022-00063-0. 307–307. [DOI] [PubMed] [Google Scholar]
- Lee C.C., Hsieh C.C., Ko W.C. Molnupiravir—a novel oral anti-SARS-CoV-2 agent. Antibiotics. 2021;10 doi: 10.3390/ANTIBIOTICS10111294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennerstrand J., Svensson L., Lundkvist A. How did omikron originate and why does it spread so fast? 2022. https://lakartidningen.se/klinik-och-vetenskap-1/artiklar-1/klinisk-oversikt/2022/01/hur-har-omikron-uppstatt-och-varfor-sprider-den-sig-sa-snabbt/ [PubMed]
- Leshem E., Gonen T., Hoffman T., Barsisat A., Kreiss Y., Regev-Yochay G. Low rate of transmission to triple-vaccinated contacts of an imported case of SARS-CoV-2 omicron infection: a contact tracing study in Israel. J. Trav. Med. 2022 doi: 10.1093/JTM/TAAC003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X. Omicron: call for updated vaccines. J. Med. Virol. 2021 doi: 10.1002/JMV.27530. [DOI] [PubMed] [Google Scholar]
- Li A., Maier A., Carter M., Hugh Guan T. Omicron and S-gene target failure cases in the highest COVID-19 case rate region in Canada - december 2021. J. Med. Virol. 2021 doi: 10.1002/JMV.27562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Lester D., Rosengarten G., Aboltins C., Patel M., Cole I. A spatiotemporally resolved infection risk model for airborne transmission of COVID-19 variants in indoor spaces. Sci. Total Environ. 2021;812:152592. doi: 10.1016/J.SCITOTENV.2021.152592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima D.G.S., Figueiredo T.M.R., Pereira Y.T.G., Almino M.A.F.B., Pereira L.M., de Menezes H.L., Araújo J.E.B., Junior J.G., Vieira N.B., de Carvalho S.M.F., Machado S.S.F., de Matos Cassiano C.J., Dionizio B.S., Pinheiro R.C.F., Feitosa P.W.G., Filho F.H.P., Lima N.N.R., Neto M.L.R. The effects of the silence on south African children and adolescents against a global alert on the newly identified coronavirus variant: Omicron. J. Pediatr. Nurs. 2021 doi: 10.1016/J.PEDN.2021.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Adeli K., Plebani M. Commercial immunoassays for detection of anti-SARS-CoV-2 spike and RBD antibodies: urgent call for validation against new and highly mutated variants. Clin. Chem. Lab. Med. 2021 doi: 10.1515/CCLM-2021-1287. 0. [DOI] [PubMed] [Google Scholar]
- Liu Q., Qin C., Liu M., Liu J. Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: a systematic review and meta-analysis. Infect. Dis. Povert. 2021;10 doi: 10.1186/S40249-021-00915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L., Mok B.W.-Y., Chen L.-L., Chan J.M.-C., Tsang O.T.-Y., Lam B.H.-S., Chuang V.W.-M., Chu A.W.-H., Chan W.-M., Ip J.D., Chan B.P.-C., Zhang R., Yip C.C.-Y., Cheng V.C.-C., Chan K.-H., Jin D.-Y., Hung I.F.-N., Yuen K.-Y., Chen H., To K.K.-W. Neutralization of SARS-CoV-2 Omicron variant by sera from BNT162b2 or Coronavac vaccine recipients. Clin. Infect. Dis. 2021 doi: 10.1093/CID/CIAB1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubin J.H., Markosian C., Balamurugan D., Pasqualini R., Arap W., Burley S.K., Khare S.D. Structural models of SARS-CoV-2 Omicron variant in complex with ACE2 receptor or antibodies suggest altered binding interfaces. bioRxiv. 2021;2021 doi: 10.1101/2021.12.12.472313. 12.12.472313. [DOI] [Google Scholar]
- Luo M., Liu Q., Wang J., Gong Z. From SARS to the Omicron variant of COVID-19: China's policy adjustments and changes to prevent and control infectious diseases. Biosci. Trend. 2021;2021 doi: 10.5582/BST.2021.01535. [DOI] [PubMed] [Google Scholar]
- Lupala C.S., Ye Y., Chen H., Su X.-D., Liu H. Mutations on RBD of SARS-CoV-2 Omicron variant result in stronger binding to human ACE2 receptor. Biochem. Biophys. Res. Commun. 2022;590:34. doi: 10.1016/J.BBRC.2021.12.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. Covid-19: hospital admission 50-70% less likely with omicron than delta, but transmission a major concern. BMJ. 2021;375:n3151. doi: 10.1136/BMJ.N3151. [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: omicron and the need for boosters. BMJ. 2021;375:n3079. doi: 10.1136/BMJ.N3079. [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: do vaccines work against omicron-and other questions answered. BMJ. 2021;375:n3062. doi: 10.1136/BMJ.N3062. [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: UK approves monoclonal antibody sotrovimab for over 12s at high risk. BMJ. 2021;375:n2990. doi: 10.1136/BMJ.N2990. [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: Pfizer's paxlovid is 89% effective in patients at risk of serious illness, company reports. BMJ. 2021;375:n2713. doi: 10.1136/BMJ.N2713. [DOI] [PubMed] [Google Scholar]
- Mahase E. Omicron: NHS is on “war footing” as Nightingale hubs are announced in England. BMJ. 2021;375:n3159. doi: 10.1136/BMJ.N3159. [DOI] [PubMed] [Google Scholar]
- Majumdar S., Sarkar R. Mutational and phylogenetic analyses of the two lineages of the Omicron variant. J. Med. Virol. 2021 doi: 10.1002/JMV.27558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallapaty S. Omicron-variant border bans ignore the evidence, say scientists. Nature. 2021;600 doi: 10.1038/D41586-021-03608-X. [DOI] [PubMed] [Google Scholar]
- Mannar D., Saville J.W., Zhu X., Srivastava S.S., Berezuk A.M., Tuttle K.S., Marquez A.C., Sekirov I., Subramaniam S. SARS-CoV-2 Omicron variant: antibody evasion and cryo-EM structure of spike protein-ACE2 complex. Science. 2022 doi: 10.1126/SCIENCE.ABN7760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruki T., Iwamoto N., Kanda K., Okumura N., Yamada G., Ishikane M., Ujiie M., Saito M., Fujimoto T., Kageyama T., Saito T., Saito S., Suzuki T., Ohmagari N. Two cases of breakthrough SARS-CoV-2 infections caused by the Omicron variant (B.1.1.529 lineage) in international travelers to Japan. Clin. Infect. Dis. 2022 doi: 10.1093/CID/CIAB1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxmen A. Omicron blindspots: why it's hard to track coronavirus variants. Nature. 2021;600 doi: 10.1038/D41586-021-03698-7. 579–579. [DOI] [PubMed] [Google Scholar]
- May D.H., Rubin B.E.R., Dalai S.C., Patel K., Shafiani S., Elyanow R., Noakes M.T., Snyder T.M., Robins H.S. 2021. Immunosequencing and Epitope Mapping Reveal Substantial Preservation of the T Cell Immune Response to Omicron Generated by SARS-CoV-2 Vaccines; p. 21267877. medRxiv 2021.12.20. [DOI] [Google Scholar]
- McKee M. Public health and politics are inseparable, as Omicron and the UK's response remind us. BMJ. 2021;375:n3055. doi: 10.1136/BMJ.N3055. [DOI] [PubMed] [Google Scholar]
- McMahan K., Giffin V., Tostanoski L.H., Chung B., Siamatu M., Suthar M.S., Halfmann P., Kawaoka Y., Piedra-Mora C., Martinot A.J., Kar S., Andersen H., Lewis M.G., Barouch D.H. bioRxiv; 2022. Reduced Pathogenicity of the SARS-CoV-2 Omicron Variant in Hamsters. 2022.01.02.474743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng B., Ferreira I.A.T., Abdullahi A., Saito A., Kimura I., Yamasoba D., Kemp S.A., Goonawardane N., Papa G., Fatihi S., Rathore S., Ikeda T., Toyoda M., Tan T.S., Kuramochi J., Mitsunaga S., Ueno T., Charles O.J., Collaboration C.-N.B.C.-19, Consortium, T.G. to P.J. (G2P-J. Consortium E.-C., Smith K.G.C., Bradley J., Choi J., Madissoon E., Meyer K., Mlcochova P., Doffinger R., Teichmann S.A., James L., Lee J.H., Thukral L., Sato K., Gupta R.K. SARS-CoV-2 Omicron spike mediated immune escape, infectivity and cell-cell fusion. bioRxiv. 2021 doi: 10.1101/2021.12.17.473248. 2021.12.17.473248. [DOI] [Google Scholar]
- Metzger C.M.J.A., Lienhard R., Seth-Smith H.M.B., Roloff T., Wegner F., Sieber J., Bel M., Greub G., Egli A. PCR performance in the SARS-CoV-2 Omicron variant of concern? Swiss Med. Wkly. 2021;151 doi: 10.4414/SMW.2021.W30120. [DOI] [PubMed] [Google Scholar]
- Miller N.L., Clark T., Raman R., Sasisekharan R. bioRxiv; 2021. Insights on the Mutational Landscape of the SARS-CoV-2 Omicron Variant. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohapatra R.K., Sarangi A.K., Kandi V., Azam M., Tiwari R., Dhama K. Omicron (B.1.1.529 variant of SARS-CoV-2); an emerging threat: current global scenario. J. Med. Virol. 2021 doi: 10.1002/JMV.27561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohiuddin M., Kasahara K. Investigating the aggressiveness of the COVID-19 Omicron variant and suggestions for possible treatment options. Respir. Med. 2021;191:106716. doi: 10.1016/J.RMED.2021.106716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moncunill G., Aguilar R., Ribes M., Ortega N., Rubio R., Salmerón G., Molina M.J., Vidal M., Barrios D., Mitchell R.A., Jiménez A., Castellana C., Hernández-Luis P., Rodó P., Méndez S., Llupià A., Puyol L., Rodrigo Melero N., Carolis C., Mayor A., Izquierdo L., Varela P., Trilla A., Vilella A., Barroso S., Angulo A., Engel P., Tortajada M., García-Basteiro A.L., Dobaño C. Determinants of early antibody responses to COVID-19 mRNA vaccines in a cohort of exposed and naïve healthcare workers. EBioMedicine. 2022;75:103805. doi: 10.1016/J.EBIOM.2021.103805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mourier T., Shuaib M., Hala S., Mfarrej S., Alofi F., Naeem R., Alsomali A., Jorgensen D., Subudhi A.K., Rached F. Ben, Guan Q., Salunke R.P., Ooi A., Esau L., Douvropoulou O., Nugmanova R., Perumal S., Zhang H., Rajan I., Al-Omari A., Salih S., Shamsan A., Mutair A. Al, Taha J., Alahmadi A., Khotani N., Alhamss A., Mahmoud A., Alquthami K., Dageeg A., Khogeer A., Hashem A.M., Moraga P., Volz E., Almontashiri N., Pain A. medRxiv; 2021. Saudi Arabian SARS-CoV-2 Genomes Implicate a Mutant Nucleocapsid Protein in Modulating Host Interactions and Increased Viral Load in COVID-19 Patients. 2021.05.06.21256706. [DOI] [Google Scholar]
- Nainu F., Abidin R.S., Bahar M.A., Frediansyah A., Emran T. Bin, Rabaan A.A., Dhama K., Harapan H. SARS-CoV-2 reinfection and implications for vaccine development. Hum. Vaccines Immunother. 2020;16:3061–3073. doi: 10.1080/21645515.2020.1830683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natario N. 2021. UTMB Study Shows Unvaccinated, Natural Immunity Offers Little Protection against Omicron - ABC13 Houston.https://abc13.com/houston-coronavirus-utmb-research-omicron-variant-protecting-against/11372883/ [Google Scholar]
- National Institute of Infectious Diseases, Japan, (NIID . 2022. Active Epidemiological Investigation on SARS-CoV-2 Infection Caused by Omicron Variant (Pango Lineage B.1.1.529.https://www.niid.go.jp/niid/en/2019-ncov-e/10884-covid19-66-en.html in Japan: preliminary report on infectious period. [Google Scholar]
- National Institutes of Health (NIH) 2022. COVID-19 Treatment Guidelines.https://www.covid19treatmentguidelines.nih.gov/ [Google Scholar]
- Naveca F., Costa da C., Nascimento V., Souza V., Corado A., Nascimento F., Costa A., Duarte D., Silva G., Mejía M., Pessoa K., Gonçalves L., Brandão M.J., Jesus M., Pinto R., Silva M., Mattos T., Abdalla L., Santos J.H., Costa-Filho R., Wallau L.G., Siqueira M.M., Delatorre E., Gräf T., Bello G., Resende P.C. 2019. SARS-CoV-2 Reinfection by the New Variant of Concern (VOC) P.1 in Amazonas, Brazil - SARS-CoV-2 Coronavirus/nCoV-2019 Genomic Epidemiology – Virological.https://virological.org/t/sars-cov-2-reinfection-by-the-new-variant-of-concern-voc-p-1-in-amazonas-brazil/596 [Google Scholar]
- Nemet I., Kliker L., Lustig Y., Zuckerman N., Erster O., Cohen C., Kreiss Y., Alroy-Preis S., Regev-Yochay G., Mendelson E., Mandelboim M. Third BNT162b2 vaccination neutralization of SARS-CoV-2 omicron infection. N. Engl. J. Med. 2021 doi: 10.1056/NEJMC2119358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neopane P., Nypaver J., Shrestha R., Beqaj S.S. SARS-CoV-2 variants detection using TaqMan SARS-CoV-2 mutation panel molecular genotyping assays. Infect. Drug Resist. 2021;14:4471. doi: 10.2147/IDR.S335583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NewsNodes . 2022. Newsnodes - Omicron Tracker.https://newsnodes.com/nu_tracker [Google Scholar]
- Nie C., Sahoo A.K., Herrmann A., Ballauff M., Netz R.R., Haag R. Charge matters: mutations in omicron variant favor binding to cells. Chembiochem. 2022 doi: 10.1002/CBIC.202100681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreshkova N., Molenaar R.J., Vreman S., Harders F., Oude Munnink B.B., Van Der Honing R.W.H., Gerhards N., Tolsma P., Bouwstra R., Sikkema R.S., Tacken M.G.J., De Rooij M.M.T., Weesendorp E., Engelsma M.Y., Bruschke C.J.M., Smit L.A.M., Koopmans M., Van Der Poel W.H.M., Stegeman A. SARS-CoV-2 infection in farmed minks, The Netherlands. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.23.2001005. April and May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parums D.V. Editorial: current status of oral antiviral drug treatments for SARS-CoV-2 infection in non-hospitalized patients. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2022;28 doi: 10.12659/MSM.935952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascarella S., Ciccozzi M., Zella D., Bianchi M., Benedetti F., Benvenuto D., Broccolo F., Cauda R., Caruso A., Angeletti S., Giovanetti M., Cassone A. SARS-CoV-2 B.1.617 Indian variants: are electrostatic potential changes responsible for a higher transmission rate? J. Med. Virol. 2021;93:6551–6556. doi: 10.1002/JMV.27210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascarella S., Ciccozzi M., Bianchi M., Benvenuto D., Cauda R., Cassone A. The electrostatic potential of the Omicron variant spike is higher than in Delta and Delta-plus variants: a hint to higher transmissibility? J. Med. Virol. 2021 doi: 10.1002/JMV.27528. [DOI] [PubMed] [Google Scholar]
- Pawłowski P. SARS-CoV-2 variant Omicron (B.1.1.529) is in a rising trend of mutations increasing the positive electric charge in crucial regions of the spike protein S. Acta Biochim. Pol. 2021 doi: 10.18388/ABP.2020_6072. [DOI] [PubMed] [Google Scholar]
- Penner R.C., Elisabete M., Oliveira C.D.R., Gomes A., Sampaio P., Lucio M. Mutagenic distinction between the receptor-binding and fusion subunits of the SARS-CoV-2 spike glycoprotein and its upshot. Vaccines. 2021;9(2021):1509. doi: 10.3390/VACCINES9121509. Page 1509 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Then E., Lucas C., Monteiro V.S., Miric M., Brache V., Cochon L., Vogels C.B.F., Malik A.A., De la Cruz E., Jorge A., De los Santos M., Leon P., Breban M.I., Billig K., Yildirim I., Pearson C., Downing R., Gagnon E., Muyombwe A., Razeq J., Campbell M., Ko A.I., Omer S.B., Grubaugh N.D., Vermund S.H., Iwasaki A. Neutralizing antibodies against the SARS-CoV-2 Delta and Omicron variants following heterologous CoronaVac plus BNT162b2 booster vaccination. Nat. Med. 2022 doi: 10.1038/S41591-022-01705-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persad G., Peek M.E., Shah S.K. Fair allocation of scarce therapies for COVID-19. Clin. Infect. Dis. 2021 doi: 10.1093/CID/CIAB1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen E., Ntoumi F., Hui D.S., Abubakar A., Kramer L.D., Obiero C., Tambyah P.A., Blumberg L., Yapi R., Al-Abri S., Pinto T. de C.A., Yeboah-Manu D., Haider N., Asogun D., Velavan T.P., Kapata N., Bates M., Ansumana R., Montaldo C., Mucheleng’anga L., Tembo J., Mwaba P., Himwaze C.M., Hamid M.M.A., Mfinanga S., Mboera L., Raj T., Aklillu E., Veas F., Edwards S., Kaleebu P., McHugh T.D., Chakaya J., Nyirenda T., Bockarie M., Nyasulu P.S., Wejse C., Muyembe-Tamfum J.-J., Azhar E.I., Maeurer M., Nachega J.B., Kock R., Ippolito G., Zumla A. Emergence of new SARS-CoV-2 Variant of Concern Omicron (B.1.1.529) - highlights Africa's research capabilities, but exposes major knowledge gaps, inequities of vaccine distribution, inadequacies in global COVID-19 response and control efforts. Int. J. Infect. Dis. 2022;114:268–272. doi: 10.1016/J.IJID.2021.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planas D., Veyer D., Baidaliuk A., Staropoli I., Guivel-Benhassine F., Rajah M.M., Planchais C., Porrot F., Robillard N., Puech J., Prot M., Gallais F., Gantner P., Velay A., Le Guen J., Kassis-Chikhani N., Edriss D., Belec L., Seve A., Courtellemont L., Péré H., Hocqueloux L., Fafi-Kremer S., Prazuck T., Mouquet H., Bruel T., Simon-Lorière E., Rey F.A., Schwartz O. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021;2021 5967871 596:276–280. doi: 10.1038/s41586-021-03777-9. [DOI] [PubMed] [Google Scholar]
- Poudel S., Ishak A., Perez-Fernandez J., Garcia E., León-Figueroa D.A., Romaní L., Bonilla-Aldana D.K., Rodriguez-Morales A.J. Highly mutated SARS-CoV-2 Omicron variant sparks significant concern among global experts – what is known so far? Trav. Med. Infect. Dis. 2022;45:102234. doi: 10.1016/J.TMAID.2021.102234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourkarim F., Pourtaghi-Anvarian S., Rezaee H. Molnupiravir: a new candidate for COVID-19 treatment. Pharmacol. Res. Perspect. 2022;10 doi: 10.1002/PRP2.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhawan M., Priyanka, Choudhary O.P. Omicron SARS-CoV-2 variant: reasons of emergence and lessons learnt. Int. J. Surg. 2022;97:106198. doi: 10.1016/J.IJSU.2021.106198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulliam J.R.C., Schalkwyk C. van, Govender N., Gottberg A. von, Cohen C., Groome M.J., Dushoff J., Mlisana K., Moultrie H. medRxiv; 2021. Increased Risk of SARS-CoV-2 Reinfection Associated with Emergence of the Omicron Variant in South Africa. 2021.11.11.21266068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quarleri J., Galvan V., Delpino · M Victoria. Omicron variant of the SARS-CoV-2: a quest to define the consequences of its high mutational load. GeroScience. 2021 doi: 10.1007/S11357-021-00500-4. 2021 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Queen D. Another year another variant: covid 3.0—Omicron. Int. Wound J. 2022;19:5. doi: 10.1111/IWJ.13739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabaan A.A., Al-Ahmed S.H., Garout M.A., Al-Qaaneh A.M., Sule A.A., Tirupathi R., Mutair A. Al, Alhumaid S., Hasan A., Dhawan M., Tiwari R., Sharun K., Mohapatra R.K., Mitra S., Emran T. Bin, Bilal M., Singh R., Alyami S.A., Ali Moni M., Dhama K. Diverse immunological factors influencing pathogenesis in patients with COVID-19: a review on viral dissemination, immunotherapeutic options to counter cytokine storm and inflammatory responses. Pathogens. 2021;10 doi: 10.3390/PATHOGENS10050565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rae M. Omicron: a failure to act with a global focus will continue the proliferation of new variants of covid-19. BMJ. 2021;375:n3095. doi: 10.1136/BMJ.N3095. [DOI] [PubMed] [Google Scholar]
- Rahimi F., Kamali N., Abadi A.T.B. The Mu strain: the last but not least circulating ‘variant of interest’ potentially affecting the COVID-19 pandemic. Future Virol. 2021;17:5–8. doi: 10.2217/FVL-2021-0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahmani S., Rezaei N. Omicron (B.1.1.529) variant: development, dissemination, and dominance. J. Med. Virol. 2021 doi: 10.1002/JMV.27563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raman R., Patel K.J., Ranjan K. COVID-19: unmasking emerging SARS-CoV-2 variants, vaccines and therapeutic strategies. Biomolecules. 2021;11:993. doi: 10.3390/BIOM11070993. 2021Page 993 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redd A.D., Nardin A., Kared H., Bloch E.M., Abel B., Pekosz A., Laeyendecker O., Fehlings M., Quinn T.C., Tobian A.A. bioRxiv; 2021. Minimal Cross-Over between Mutations Associated with Omicron Variant of SARS-CoV-2 and CD8+ T Cell Epitopes Identified in COVID-19 Convalescent Individuals. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resende P.C., Delatorre E., Gräf T., Mir D., Motta F.C., Appolinario L.R., Paixão A.C.D. da, Mendonça A.C. da F., Ogrzewalska M., Caetano B., Wallau G.L., Docena C., Santos M.C. dos, de Almeida Ferreira J., Sousa Junior E.C., Silva S.P. da, Fernandes S.B., Vianna L.A., Souza L., da C., Ferro J.F.G., Nardy V.B., Santos C.A., Riediger I., do Carmo Debur M., Croda J., Oliveira W.K., Abreu A., Bello G., Siqueira M.M. Evolutionary dynamics and dissemination pattern of the SARS-CoV-2 lineage B.1.1.33 during the early pandemic phase in Brazil. Front. Microbiol. 2021;11:3565. doi: 10.3389/FMICB.2020.615280/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riediker M., Briceno-Ayala L., Ichihara G., Albani D., Poffet D., Tsai D.-H., Iff S., Monn C. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med. Wkly. 2022;152:w30133. doi: 10.4414/SMW.2022.W30133. [DOI] [PubMed] [Google Scholar]
- Rössler A., Riepler L., Bante D., von Laer D., Kimpel J. SARS-CoV-2 omicron variant neutralization in serum from vaccinated and convalescent persons. N. Engl. J. Med. 2022 doi: 10.1056/NEJMC2119236/SUPPL_FILE/NEJMC2119236_DISCLOSURES.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMRC . 2021. Discovery Health, South Africa's Largest Private Health Insurance Administrator, Releases At-Scale, Real-World Analysis of Omicron Outbreak Based on 211 000 COVID-19-Positive Test Results in South Africa, Including Collaboration with the South Africa.https://dsycloud.zoom.us/rec/share/F90e3WwsG3hnWohegHBLZ794OqtadWO 5wNTEMh-5BE7uIG-G_Rlex4WT0wtBJHtM.jBJNHyH9YLBdybjJ Johannesburg, 14 December 2021. [Google Scholar]
- Sarah Wild. 2021. How the Omicron Variant Got So Many Scary Mutations So Quickly - Scientific American.https://www.scientificamerican.com/article/how-the-omicron-variant-got-so-many-scary-mutations-so-quickly/ [Google Scholar]
- Saxena S.K., Kumar S., Ansari S., Paweska J.T., Maurya V.K., Tripathi A.K., Abdel-Moneim A.S. Characterization of the novel SARS-CoV-2 omicron (B.1.1.529) variant of concern and its global perspective. J. Med. Virol. 2021 doi: 10.1002/JMV.27524. [DOI] [PubMed] [Google Scholar]
- Schmidt F., Weisblum Y., Rutkowska M., Poston D., Da Silva J., Zhang F., Bednarski E., Cho A., Schaefer-Babajew D.J., Gaebler C., Caskey M., Nussenzweig M.C., Hatziioannou T., Bieniasz P.D. High genetic barrier to SARS-CoV-2 polyclonal neutralizing antibody escape. Nature. 2021;2021 6007889 600:512–516. doi: 10.1038/s41586-021-04005-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt F., Muecksch F., Weisblum Y., Silva J. Da, Bednarski E., Cho A., Wang Z., Gaebler C., Caskey M., Nussenzweig M.C., Hatziioannou T., Bieniasz P.D. medRxiv; 2021. Plasma Neutralization Properties of the SARS-CoV-2 Omicron Variant. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scientific Advisory Group for Emergencies (SAGE) 2021. SAGE 99 Minutes: Coronavirus (COVID-19) Response, 16 December 2021.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1042189/S1437_SAGE_99_Minute.pdf [Google Scholar]
- Sexton M.E., Waggoner J.J., Carmola L.R., Nguyen P.-V., Wang E., Khosravi D., Taz A., Arthur R., Patel M., Edara V.-V., Foster S.L., Moore K.M., Gagne M., Roberts-Torres J., Henry A.R., Godbole S., Douek D.C., Rouphael N., Suthar M.S., Piantadosi A. Rapid detection and characterization of SARS-CoV-2 omicron variant in a returning traveler. Clin. Infect. Dis. 2022 doi: 10.1093/CID/CIAC032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan K.J., Wei C., Wang Y., Huan Q., Qian W. Host-specific asymmetric accumulation of mutation types reveals that the origin of SARS-CoV-2 is consistent with a natural process. Innovation. 2021;2:100159. doi: 10.1016/J.XINN.2021.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanmugaraj B., Malla A., Khorattanakulchai N., Phoolcharoen W. SARS-CoV-2 omicron variant: could it be another threat? J. Med. Virol. 2021 doi: 10.1002/JMV.27532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharun K., Dhama K., Pawde A.M., Gortázar C., Tiwari R., Bonilla-Aldana D.K., Rodriguez-Morales A.J., de la Fuente J., Michalak I., Attia Y.A. SARS-CoV-2 in animals: potential for unknown reservoir hosts and public health implications. Vet. Q. 2021;41:181–201. doi: 10.1080/01652176.2021.1921311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharun K., Tiwari R., Natesan S., Dhama K. SARS-CoV-2 infection in farmed minks, associated zoonotic concerns, and importance of the One Health approach during the ongoing COVID-19 pandemic. Vet. Q. 2021;41:50. doi: 10.1080/01652176.2020.1867776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharun K., Tiwari R., Saied A.R.A., Dhama K. SARS-CoV-2 vaccine for domestic and captive animals: an effort to counter COVID-19 pandemic at the human-animal interface. Vaccine. 2021;39:7119–7122. doi: 10.1016/J.VACCINE.2021.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha N.K., Burke P.C., Nowacki A.S., Terpeluk P., Gordon S.M. Necessity of COVID-19 vaccination in persons who have already had COVID-19. Clin. Infect. Dis. 2022 doi: 10.1093/CID/CIAC022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuai H., Chan J.F.-W., Hu B., Chai Y., Yuen T.T.-T., Yin F., Huang X., Yoon C., Hu J.-C., Liu H., Shi J., Liu Y., Zhu T., Zhang J., Hou Y., Wang Y., Lu L., Cai J.-P., Zhang A.J., Zhou J., Yuan S., Brindley M.A., Zhang B.-Z., Huang J.-D., To K.K.-W., Yuen K.-Y., Chu H. 2022. Attenuated Replication and Pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nat. 2022 1–1. [DOI] [PubMed] [Google Scholar]
- Sievers B.L., Chakraborty S., Xue Y., Gelbart T., Gonzalez J.C., Cassidy A.G., Golan Y., Prahl M., Gaw S.L., Arunachalam P.S., Blish C.A., Boyd S.D., Davis M.M., Jagannathan P., Nadeau K.C., Pulendran B., Singh U., Scheuermann R.H., Frieman M.B., Vashee S., Wang T.T., Tan G.S. Antibodies elicited by SARS-CoV-2 infection or mRNA vaccines have reduced neutralizing activity against Beta and Omicron pseudoviruses. Sci. Transl. Med. 2022 doi: 10.1126/SCITRANSLMED.ABN7842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhal T. 2022. The Emergence of Omicron: Challenging Times Are Here Again! Indian J. Pediatr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snehota M., Vlckova J., Cizkova K., Vachutka J., Kolarova H., Klaskova E., Kollarova H. Acceptance of a vaccine against COVID-19 - a systematic review of surveys conducted worldwide. Bratisl. Lek. Listy. 2021;122:538–547. doi: 10.4149/BLL_2021_086. [DOI] [PubMed] [Google Scholar]
- Sohan M., Hossain M.J., Islam M.R. The SARS-CoV-2 Omicron (B.1.1.529) variant and effectiveness of existing vaccines: what we know so far. J. Med. Virol. 2022 doi: 10.1002/JMV.27574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Lin W., Dong W., Xu J. Origin and evolutionary analysis of the SARS-CoV-2 Omicron variant. J. Biosaf. Biosec. 2022;4:33–37. doi: 10.1016/J.JOBB.2021.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed A.M., Ciling A., Khalid M.M., Sreekumar B., Chen P.-Y., Kumar G.R., Silva I., Milbes B., Kojima N., Hess V., Shacreaw M., Lopez L., Brobeck M., Turner F., Spraggon L., Taha T.Y., Tabata T., Chen I.P., Ott M., Doudna J.A. Omicron mutations enhance infectivity and reduce antibody neutralization of SARS-CoV-2 virus-like particles. medRxiv Prepr. Serv. Health Sci. 2022 doi: 10.1101/2021.12.20.21268048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanne J.H. Covid 19: omicron is a cause for concern, not panic, says US president. BMJ. 2021;375:n2956. doi: 10.1136/BMJ.N2956. [DOI] [PubMed] [Google Scholar]
- Tanne J.H. Covid 19: US cases rise amid omicron fears but booster shots offer protection, experts say. BMJ. 2021;375:n3098. doi: 10.1136/BMJ.N3098. [DOI] [PubMed] [Google Scholar]
- Tao K., Tzou P.L., Nouhin J., Gupta R.K., de Oliveira T., Kosakovsky Pond S.L., Fera D., Shafer R.W. The biological and clinical significance of emerging SARS-CoV-2 variants. Nat. Rev. Genet. 2021;2212 22(2021):757–773. doi: 10.1038/s41576-021-00408-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tareq A.M., Emran T. Bin, Dhama K., Dhawan M., Tallei T.E. 2021. Impact of SARS-CoV-2 Delta Variant (B.1.617.2) in Surging Second Wave of COVID-19 and Efficacy of Vaccines in Tackling the Ongoing Pandemic. https://doi.org/10.1080/21645515.2021.1963601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarke A., Sidney J., Kidd C.K., Dan J.M., Ramirez S.I., Yu E.D., Mateus J., da Silva Antunes R., Moore E., Rubiro P., Methot N., Phillips E., Mallal S., Frazier A., Rawlings S.A., Greenbaum J.A., Peters B., Smith D.M., Crotty S., Weiskopf D., Grifoni A., Sette A. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. Cell Rep. 2021;2 doi: 10.1016/J.XCRM.2021.100204. Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor P.C., Adams A.C., Hufford M.M., de la Torre I., Winthrop K., Gottlieb R.L. Neutralizing monoclonal antibodies for treatment of COVID-19. Nat. Rev. Immunol. 2021;216 21:382–393. doi: 10.1038/s41577-021-00542-x. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terada Y., Matsui N., Noguchi K., Kuwata R., Shimoda H., Soma T., Mochizuki M., Maeda K. Emergence of pathogenic coronaviruses in cats by homologous recombination between feline and canine coronaviruses. PLoS One. 2014;9 doi: 10.1371/JOURNAL.PONE.0106534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur V., Kanta Ratho R. Omicron (B.1.1.529): a new SARS-CoV-2 variant of concern mounting worldwide fear. J. Med. Virol. 2021 doi: 10.1002/JMV.27541. [DOI] [PubMed] [Google Scholar]
- Thakur V., Bhola S., Thakur P., Patel S.K.S., Kulshrestha S., Ratho R.K., Kumar P. Waves and variants of SARS-CoV-2: understanding the causes and effect of the COVID-19 catastrophe. Infection. 2021;1:1. doi: 10.1007/S15010-021-01734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas E., Delabat S., Carattini Y.L., Andrews D.M. SARS-CoV-2 and variant diagnostic testing approaches in the United States. Viruses. 2021;13 doi: 10.3390/V13122492. 2021Page 2492 13, 2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong C., Shi W., Zhang A., Shi Z. Tracking and controlling the spatiotemporal spread of SARS-CoV-2 Omicron variant in South Africa. Trav. Med. Infect. Dis. 2021;102252 doi: 10.1016/J.TMAID.2021.102252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torjesen I. Covid-19: omicron may be more transmissible than other variants and partly resistant to existing vaccines, scientists fear. BMJ. 2021;375:n2943. doi: 10.1136/BMJ.N2943. [DOI] [PubMed] [Google Scholar]
- Torjesen I. Covid-19: peak of viral shedding is later with omicron variant, Japanese data suggest. BMJ. 2022;376:o89. doi: 10.1136/BMJ.O89. [DOI] [PubMed] [Google Scholar]
- VanBlargan L.A., Errico J.M., Halfmann P.J., Zost S.J., Crowe J.E., Purcell L.A., Kawaoka Y., Corti D., Fremont D.H., Diamond M.S. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat. Med. 2022:1–6. doi: 10.1038/s41591-021-01678-y. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandeputte J., Van Damme P., Neyts J., Audonnet J.C., Baay M., Neels P. Animal experiments show impact of vaccination on reduction of SARS-CoV-2 virus circulation: a model for vaccine development? Biologicals. 2021;73:1–7. doi: 10.1016/J.BIOLOGICALS.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan A. Omicron emerges. New Sci. 2021;252:7. doi: 10.1016/S0262-4079(21)02140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatakrishnan A., Anand P., Lenehan P.J., Suratekar R., Raghunathan B., Niesen M.J.M., Soundararajan V. Omicron variant of SARS-CoV-2 harbors a unique insertion mutation of putative viral or human genomic origin. 2021. [DOI]
- Vogel G., Kupferscgmidt K. 2021. Early Lab Studies Hint Omicron May Be Milder. But Most Scientists Reserve Judgment - Science.https://www.science.org/content/article/early-lab-studies-hint-omicron-may-be-milder-most-scientists-reserve-judgment [Google Scholar]
- Wahid M., Jawed A., Mandal R.K., Dailah H.G., Janahi E.M., Dhama K., Somvanshi P., Haque S. Variants of SARS-CoV-2, their effects on infection, transmission and neutralization by vaccine-induced antibodies. Eur. Rev. Med. Pharmacol. Sci. 2021;25:5857–5864. doi: 10.26355/EURREV_202109_26805. [DOI] [PubMed] [Google Scholar]
- Wang L., Cheng G. Sequence analysis of the emerging sars-CoV-2 variant omicron in South Africa. J. Med. Virol. 2021 doi: 10.1002/JMV.27516. [DOI] [PubMed] [Google Scholar]
- Wang X., Powell C.A. How to translate the knowledge of COVID-19 into the prevention of Omicron variants. Clin. Transl. Med. 2021;11 doi: 10.1002/CTM2.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Yang L. In the age of Omicron variant: paxlovid raises new hopes of COVID-19 recovery. J. Med. Virol. 2021 doi: 10.1002/JMV.27540. [DOI] [PubMed] [Google Scholar]
- Wang P., Nair M.S., Liu L., Iketani S., Luo Y., Guo Y., Wang M., Yu J., Zhang B., Kwong P.D., Graham B.S., Mascola J.R., Chang J.Y., Yin M.T., Sobieszczyk M., Kyratsous C.A., Shapiro L., Sheng Z., Huang Y., Ho D.D. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature. 2021;593:130–135. doi: 10.1038/S41586-021-03398-2. [DOI] [PubMed] [Google Scholar]
- Wang X., Zhao X., Song J., Wu J., Zhu Y., Li M., Cui Y., Chen Y., Yang L., Liu J., Zhu H., Jiang S., Wang P. Homologous or heterologous booster of inactivated vaccine reduces SARS-CoV-2 omicron variant escape from neutralizing antibodies. Emerg. Microb. Infect. 2022:1–18. doi: 10.1080/22221751.2022.2030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei C., Shan K.-J., Wang W., Zhang S., Huan Q., Qian W. Evidence for a mouse origin of the SARS-CoV-2 Omicron variant. J. Genet. Genom. 2021 doi: 10.1016/J.JGG.2021.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolter N., Jassat W., Walaza S., Welch R., Moultrie H., Groome M., Amoako D.G., Everatt J., Bhiman J.N., Scheepers C., Tebeila N., Chiwandire N., Plessis M. du, Govender N., Ismail A., Glass A., Mlisana K., Stevens W., Treurnicht F.K., Makatini Z., Hsiao N., Parboosing R., Wadula J., Hussey H., Davies M.-A., Boulle A., Gottberg A. von, Cohen C. vol. 21. medRxiv; 2021. p. 21268116. (Early Assessment of the Clinical Severity of the SARS-CoV-2 Omicron Variant in South Africa). 2021.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.C., Au A.K.W., Chen H., Yuen L.L.H., Li X., Lung D.C., Chu A.W.H., Ip J.D., Chan W.M., Tsoi H.W., To K.K.W., Yuen K.Y., Cheng V.C.C. Transmission of Omicron (B.1.1.529) - SARS-CoV-2 Variant of Concern in a designated quarantine hotel for travelers: a challenge of elimination strategy of COVID-19. Lancet Reg. Health. 2021:100360. doi: 10.1016/J.LANWPC.2021.100360. West. Pacific 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (WHO) 2021. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern.https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern [Google Scholar]
- World Health Organisation (WHO) 2021. Tracking SARS-CoV-2 Variants.https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ [Google Scholar]
- World Health Organisation (WHO) 2021. Enhancing Readiness for Omicron (B.1.1.529): Technical Brief and Priority Actions for Member States.https://www.who.int/publications/m/item/enhancing-readiness-for-omicron-(b.1.1.529)-technical-brief-and-priority-actions-for-member-states [Google Scholar]
- World Health Organisation (WHO) 2021. Policy and Technical Considerations for Implementing a Risk-Based Approach to International Travel in the Context of COVID-19.https://www.who.int/news-room/articles-detail/policy-and-technical-considerations-for-implementing-a-risk-based-approach-to-international-travel-in-the-context-of-covid-19 [Google Scholar]
- World Health Organisation (WHO) WHO coronavirus (COVID-19) dashboard | WHO coronavirus (COVID-19) dashboard with vaccination data. 2022. https://covid19.who.int/
- Wouters O.J., Shadlen K.C., Salcher-Konrad M., Pollard A.J., Larson H.J., Teerawattananon Y., Jit M. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397:1023–1034. doi: 10.1016/S0140-6736(21)00306-8/ATTACHMENT/414172BD-59F4-4348-B632-944257A3BAA4/MMC3.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaesoubi R., You S., Xi Q., Menzies N.A., Tuite A., Grad Y.H., Salomon J.A. medRxiv; 2021. Simple Decision Rules to Predict Local Surges in COVID-19 Hospitalizations during the Winter and Spring of 2022. [DOI] [Google Scholar]
- Yu X., Wei D., Xu W., Li Y., Li X., Zhang X., Qu J., Yang Z., Chen E. Reduced sensitivity of SARS-CoV-2 Omicron variant to antibody neutralization elicited by booster vaccination. Cell Discov. 2022;81 8(2022):1–4. doi: 10.1038/s41421-022-00375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng C., Evans J.P., Chakravarthy K., Qu P., Reisinger S., Song N.-J., Rubinstein M.P., Shields P.G., Li Z., Liu S.-L. COVID-19 mRNA booster vaccines elicit strong protection against SARS-CoV-2 Omicron variant in patients with cancer. Cancer Cell. 2021 doi: 10.1016/J.CCELL.2021.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Li Q., Liang Z., Li T., Liu S., Cui Q., Nie J., Wu Q., Qu X., Huang W., Wang Y. The significant immune escape of pseudotyped SARS-CoV-2 Variant Omicron. Emerg. Microb. Infect. 2021:1–11. doi: 10.1080/22221751.2021.2017757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Wu S., Wu B., Yang Q., Chen A., Li Y., Zhang Y., Pan T., Zhang H., He X. SARS-CoV-2 Omicron strain exhibits potent capabilities for immune evasion and viral entrance. Signal Transduct. Target. Ther. 2021;61 6(2021):1–3. doi: 10.1038/s41392-021-00852-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L., Ayeh S.K., Chidambaram V., Karakousis P.C. Modes of transmission of SARS-CoV-2 and evidence for preventive behavioral interventions. BMC Infect. Dis. 2021;21:1–9. doi: 10.1186/S12879-021-06222-4/PEER-REVIEW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou H., Yang Y., Dai H., Xiong Y., Wang J.-Q., Lin L., Chen Z.-S. Recent updates in experimental research and clinical evaluation on drugs for COVID-19 treatment. Front. Pharmacol. 2021;12 doi: 10.3389/FPHAR.2021.732403. [DOI] [PMC free article] [PubMed] [Google Scholar]